Abstract
Patient: Female, 78
Final Diagnosis: Gall bladder volvulus
Symptoms: Abdominal pain
Medication: —
Clinical Procedure: Cholecystectomy
Specialty: Surgery
Objective:
Rare disease
Background:
Gall bladder volvulus is a rare clinical entity, with only around 500 cases reported in the literature. It is defined as the rotation of the gallbladder on its mesentery along the axis of the cystic pedicle, although cases of torsion of the gallbladder fundus itself have been reported.
Case Report:
A 78-year-old woman presented for severe right upper-quadrant abdominal pain that began acutely 3 days prior. Her pain was accompanied by nausea and vomiting. She also reported feeling chills. Abdominal X-ray revealed a 7-cm-diameter subhepatic opacity containing gas. Abdominal ultrasound and CT scan revealed a distended and displaced gallbladder located below the liver, in contact with the right kidney. Subsequently, open cholecystectomy was performed, and a distended, necrotic gallbladder was found twisted on its pedicle; thus, a gall bladder volvulus was diagnosed.
Conclusions:
In our patient, the classic patient characteristics of an elderly thin female with kyphosis were present. However, the rest of the presentation was not typical of gallbladder volvulus due to the patient’s delay in seeking treatment, and was representative of the necrotic phase of gallbladder torsion, in which the patient becomes ill-appearing, with fever and chills, with significant abdominal rigidity.
MeSH Keywords: Abdominal Pain; Cholecystectomy; Cholecystitis, Acute
Background
Gallbladder volvulus is a rare clinical entity with only around 500 cases reported in the literature [1]. It is defined as the rotation of the gallbladder on its mesentery along the axis of the cystic pedicle, although cases of torsion of the gallbladder fundus itself have been reported [2]. Since its initial description in an 1898 case report, this condition has proven to be difficult to diagnose, at least prior to the discovery of a twisted gallbladder in the abdomen intraoperatively. However, with increasing awareness of the condition, advancements in medical imaging, and more accurate knowledge coming from the collection of published case reports, it is increasingly possible for this condition to be diagnosed preoperatively and managed appropriately. This paper presents a case report followed by a discussion and a literature review of the components of preoperative diagnosis and management.
Case Report
A 78-year-old woman presented for severe right upper-quadrant abdominal pain that began acutely 3 days prior. Her pain was accompanied by nausea and vomiting. She also reported feeling chills. Her past medical history included hypertension and peptic ulcer disease. On presentation, she was tachycardic and febrile. On physical exam, she appeared thin and ill; her abdomen was rigid and significantly tender to palpation, with rebound tenderness. No mass could be palpated due to the rigidity of the abdomen.
Her lab test results revealed leukocytosis with a left shift, and liver and pancreatic enzymes were within normal limits.
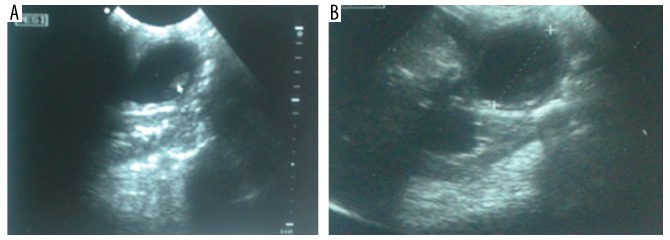
An abdominal X-ray revealed a 7-cm-diameter subhepatic opacity containing gas, and the hepatic flexure was lower than expected (Figure 1). An abdominal ultrasound revealed a distended and displaced gallbladder located below the liver, in contact with the right kidney (Figure 2A, 2B). A CT scan confirmed prior observations of a distended, subhepatic gallbladder with fluid in the gallbladder fossa and intestinal ileus (Figure 3).
Figure 1.

Abdominal X-ray revealing a 7-cm-diameter subhepatic opacity containing gas.
Figure 2.
(A, B) Abdominal ultrasound revealed a distended and displaced gallbladder located below the liver, in contact with the right kidney.
Figure 3.
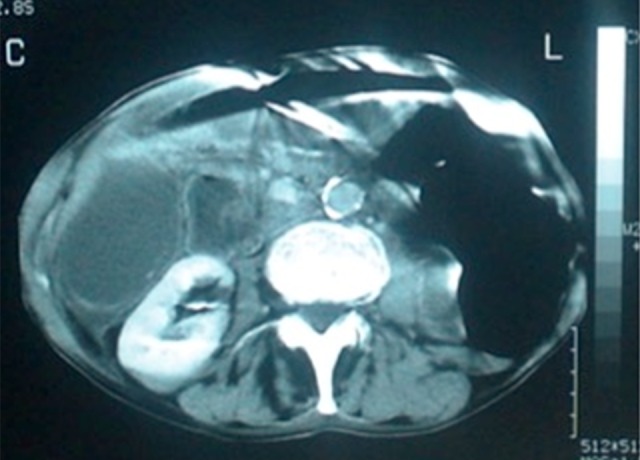
CT scan showing a distended, subhepatic gallbladder with fluid-filled gallbladder fossa and intestinal ileus.
Subsequently, open cholecystectomy was performed, and a distended, necrotic gallbladder was found twisted on its pedicle, completely rotated at more than 180 degrees (Figure 4). The gallbladder contained no gallstones. Histopathology reported a hemorrhagic, necrotic, and gangrenous gallbladder wall with significant leukocytic infiltration.
Figure 4.

Open cholecystectomy showing necrotic gallbladder twisted at its pedicle, completely rotated at more than 180 degrees.
Discussion
Gallbladder volvulus can affect patients of any age, with case reports of patients ranging from 5 days to 100 years, but appears to have a concentrated bimodal distribution with a small peak in the pediatric age group (0–18 years old) and a much larger peak in the elderly (70–100 years old). In a literature review of 324 patients, 84% of the patients were adults with a 4: 1 female-to-male ratio, while the rest were pediatric with a 1: 2.5 female-to-male ratio [1].
The mechanism underlying torsion of the gallbladder is poorly understood. It is thought that there must be an underlying defect of gallbladder attachment, most commonly the gall bladder hanging from the liver on a congenital mesentery of variable length, connecting to the gallbladder and cystic duct along their length, or connecting to the cystic duct alone, leaving a freely moving gallbladder [3]. Very rarely, a hypermobile gallbladder is due to a hypermobile liver secondary to absence of coronary and triangular ligaments [4]. Another reported anatomical variation that may be an underlying defect is an aberrantly proximal origin of the cystic duct from the right hepatic duct, constituting a very narrow cystic pedicle [5]. The predominance of torsion among the elderly is likely correlated with the diminishing supportive visceral fat and elastic tissue, with resulting visceroptosis and freeing of the gallbladder, as well as liver atrophy that further increases the motility of the gallbladder [3]. Low BMI is likely contributory through a similar mechanism of decreased visceral fat. Kyphosis has been cited as a possibly contributor due to placing the gallbladder in a more dependent position [6]. Atherosclerosis with hardening of the cystic artery has also been thought to be a possible contributing factor [6].
Along with a predisposition to torsion, there must be a final trigger for the twisting. It has been postulated that the final twisting may be secondary to gastrointestinal tract peristaltic movements whereby a stomach peristaltic wave goes from left to right and rotates the gallbladder in a clockwise manner, while the peristalsis of the transverse colon moving from right to left would account for the cases of counterclockwise torsions [7,8]. Percutaneous manipulation of the gallbladder has also been reported as a cause of torsion [9]. Torsion can also be classified as incomplete, in which rotation is 180°, or complete, in which rotation is >180°.
While cholelithiasis has been identified as a major culprit in most gall-bladder pathologies, this is not the case for gallbladder torsion. Gallstones were reportedly present in only 24.4–32% of patients (Reilly 2012), which has cast significant doubt on their role in torsion of the organ; however, it is still a higher prevalence of gall stones than the 7% estimated for the general population, although this number is not corrected for age [1,10,11]. It has been suggested that gallstones can increase the weight of the organ, increasing its risk of undergoing torsion, or to transiently increase pressure in the gallbladder, or to promote gallbladder peristalsis, thus acting as a risk factor by any of these mechanisms [12].
The clinical presentation is challengingly similar to that of acute cholecystitis, but a correct diagnosis is possible. A memorable triad of triads has been described to alarm and stimulate clinical suspicion for the presence gallbladder volvulus [13]. A triad of patient characteristics is elderly female, thin, and kyphotic or with chronic lung disease. A triad of symptoms is early presentation, typical pain, and early vomiting and nausea. A triad of physical signs is palpable abdominal mass, absence of toxemia and jaundice, and pulse-temperature discrepancy [13]. The typical pain is right upper-quadrant, sudden, sharp, and intense, but may in fact localize, along with the palpable mass, if present, to the middle or right lower quadrant due to the displaced gallbladder [14–16]. The pain may also begin as visceral pain and progress to localized somatic pain, even to the right iliac fossa such as appendicitis would present [14,15]. Guarding may, however, preclude identifying an abdominal mass [17]. An important clue to the diagnosis is an acute cholecystitis patient who does not improve on supportive management and antibiotics [11].
Certain ultrasonographic findings can help identify the abdominal pathology. Findings include the presence of the gallbladder inferior to the liver or outside its fossa, the gallbladder long axis lying horizontally, and seeing a twisted pedicle as an echogenic conical structure connecting the gallbladder to the liver [18]. Other signs include a markedly distended gallbladder, and a thickened multilayered wall with a continuous hypoechoic zone separating 2 echogenic layers [19,20]. It has also been suggested that under the suspicion of cholecystitis, the absence of cholelithiasis is supportive of volvulus as an alternative diagnosis [5]. Absence of blood flow on Doppler ultrasonography can also support the diagnosis [21].
Computed tomography (CT) findings indicative of gallbladder torsion have been described and vary in specificity [22–24]. More specific findings include a change in anatomical orientation of the gallbladder from vertical to horizontal, gallbladder location away from its fossa, the “beak” sign, and the “whirl” sign, the latter 2 being representative of the angulation of the twisted pedicle [22–24]. Other findings include a well-enhanced cystic duct to the right of the gallbladder, fluid collection separating the gallbladder from its fossa, significant gallbladder distention, and gallbladder wall thickening with hyperdensity and poor enhancement on IV contrast [22–24].
Other adjunct imaging test findings have been reported. Hydroxy iminodiacetic acid (HIDA) scans can show a “bulls-eye” image representing focal accumulation of activity in a blocked cystic duct with photopenic nonfilling of the gallbladder [25]. Magnetic resonance cholangiopancreatography (MRCP) findings have been described and include a v-shaped distortion of the extrahepatic bile ducts secondary to traction by the cystic duct, a tapered and twisted cystic duct, a distended and irregularly located gallbladder, and a difference in intensity of gallbladder and extrahepatic bile ducts [26].
The mortality rate of gallbladder volvulus is estimated to be 6%, notably in elderly with comorbidities and a delay in diagnosis [1]. Early diagnosis is crucial due to its therapeutic implications. The most common working diagnosis in such patients is acute cholecystitis, which is often managed conservatively with antibiotics, especially in the elderly. However, gallbladder torsion needs prompt surgical detorsion and cholecystectomy prior to the progression to ischemia, necrosis, rupture, and biliary peritonitis, which can be fatal. Laparoscopic cholecystectomy is recommended and can often be facilitated by the minimal adherence of the gallbladder to the liver bed [11]. Detorsion prior to resection, with careful dissection of the susceptible common bile duct, is recommended to prevent iatrogenic injury, especially in such a setting of anatomic twisting [17].
Conclusions
In our patient, the classic patient characteristics of elderly thin female with kyphosis were present. However, the rest of the presentation was not typical of gallbladder volvulus due to the patient’s delay in seeking treatment and was representative of the necrotic phase of gallbladder torsion, in which the patient becomes ill-appearing with fever and chills, with significant abdominal rigidity. The imaging findings were most useful in reaching the diagnosis, as they revealed the classic description of gallbladder torsion with a distended and inferiorly displaced gallbladder. The most important part of reaching the diagnosis is keeping a high index of suspicion, as well as knowledge of the typical findings of gallbladder volvulus in order to direct the management towards an emergent cholecystectomy as opposed to conservative management.
Footnotes
Conflict of interests
None.
References:
- 1.Reilly DJ, Kalogeropoulos G, Thiruchelvam D. Torsion of the gallbladder: A systematic review. HPB. 2012;14(10):669–72. doi: 10.1111/j.1477-2574.2012.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aharoni D, Hadas-Halpern I, Fisher D, Hiller N. Torsion of the fundus of gallbladder demonstrated on ultrasound and treated with ERCP. Abdom Imaging. 2000;25(3):269–71. doi: 10.1007/s002610000031. [DOI] [PubMed] [Google Scholar]
- 3.Gross RE. Congenital anomalies of the gallbladder: A review of one hundred and forty-eight cases, with report of a double gallbladder. Arch Surg. 1936;32(1):131–62. [Google Scholar]
- 4.Chiavarini RL, Chang SF, Westerfield JD. The wandering gallbladder. Radiology. 1975;115(1):47–48. doi: 10.1148/115.1.47. [DOI] [PubMed] [Google Scholar]
- 5.Kozman MA, Parikh RN, Fisher OM. Interesting anatomical anomaly predisposing to gallbladder torsion. ANZ J Surg. 2018;88(11):E794. doi: 10.1111/ans.13830. [DOI] [PubMed] [Google Scholar]
- 6.McHenry CR, Byrne MP. Gallbladder volvulus in the elderly. An emergent surgical disease. J Am Geriatr Soc. 1986;34(2):137–39. doi: 10.1111/j.1532-5415.1986.tb05482.x. [DOI] [PubMed] [Google Scholar]
- 7.Barber AH. Acute torsion of the gall-bladder. BMJ. 1939;2(4121):1272–73. doi: 10.1136/bmj.2.4121.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Case TC. Acute torsion of gallbladder. Am J Surg. 1951;82(6):749–53. doi: 10.1016/0002-9610(51)90402-3. [DOI] [PubMed] [Google Scholar]
- 9.Cave RK, Rose SC, Miller FJ. Gallbladder volvulus as a complication of percutaneous manipulation. J Vasc Interv Radiol. 1990;1(1):117–19. doi: 10.1016/s1051-0443(90)72515-8. [DOI] [PubMed] [Google Scholar]
- 10.Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology. 1999;117(3):632–39. doi: 10.1016/s0016-5085(99)70456-7. [DOI] [PubMed] [Google Scholar]
- 11.Nakao A, Matsuda T, Funabiki S, et al. Gallbladder torsion: Case report and review of 245 cases reported in the Japanese literature. J Hep Bil Pancr Surg. 1999;6(4):418–21. doi: 10.1007/s005340050143. [DOI] [PubMed] [Google Scholar]
- 12.Levene A. Acute torsion of the gall-bladder post-mortem findings in two cases. Br J Surg. 1958;45(192):338–40. doi: 10.1002/bjs.18004519207. [DOI] [PubMed] [Google Scholar]
- 13.Lau WY, Fan ST, Wong SH. Acute torsion of the gall bladder in the aged: A re-emphasis on clinical diagnosis. ANZ J Surg. 1982;52(5):492–94. doi: 10.1111/j.1445-2197.1982.tb06036.x. [DOI] [PubMed] [Google Scholar]
- 14.Christensen E. Torsion of the gallbladder. BMJ. 1956;2(5002):1160. doi: 10.1136/bmj.2.5002.1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bauman Z, Ruggero J, Lim J. Gallbladder volvulus presenting as acute appendicitis. Case Rep Surg. 2015;2015:629129. doi: 10.1155/2015/629129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tarhan OR, Barut I, Dinelek H. Gallbladder volvulus: Review of the literature and report of a case. Turk J Gastroenterol. 2006;17(3):209–11. [PubMed] [Google Scholar]
- 17.Pottorf BJ, Alfaro L, Hollis HW. A clinician’s guide to the diagnosis and management of gallbladder volvulus. Perm J. 2013;17(2):80–83. doi: 10.7812/TPP/12-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Safadi RR, Abu-Yousef MM, Farah AS, et al. Preoperative sonographic diagnosis of gallbladder torsion: Report of two cases. J Ultrasound Med. 1993;12(5):296–98. doi: 10.7863/jum.1993.12.5.296. [DOI] [PubMed] [Google Scholar]
- 19.Merine D, Meziane M, Fishman EK. CT diagnosis of gallbladder torsion. J Comput Assist Tomogr. 1987;11(4):712–13. doi: 10.1097/00004728-198707000-00032. [DOI] [PubMed] [Google Scholar]
- 20.Cameron EW, Beale TJ, Pearson RH. Case report: Torsion of the gall-bladder on ultrasound – differentiation from acalculous cholecystitis. Clin Radiol. 1993;47(4):285–86. doi: 10.1016/s0009-9260(05)81142-0. [DOI] [PubMed] [Google Scholar]
- 21.Hiroko N, Hideaki I, Tomoya K, et al. Color Doppler diagnosis of gallbladder torsion: A case report. J Med Ultrasonics. 1998;25(2):103–6. [Google Scholar]
- 22.Kitagawa H, Nakada K, Nakada M, et al. Two cases of torsion of the gall-bladder diagnosed preoperatively. J Ped Surg. 1997;32(11):1567–69. doi: 10.1016/s0022-3468(97)90454-1. [DOI] [PubMed] [Google Scholar]
- 23.Layton B, Rudralingam V, Lamb R. Gallbladder volvulus: It’s a small whirl. BJR Case Rep. 2016;2(3):20150360. doi: 10.1259/bjrcr.20150360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chou C, Chen R, Yang A, Wu H. Gallbladder torsion: Preoperative diagnosis by MDCT. Abdom Imaging. 2007;32(5):657–59. doi: 10.1007/s00261-006-9160-6. [DOI] [PubMed] [Google Scholar]
- 25.Wang GJ, Colln M, Crossett J, Holmes RA. “Bulls-eye” image of gallbladder volvulus. Clin Nuc Med. 1987;12(3):231–32. doi: 10.1097/00003072-198703000-00019. [DOI] [PubMed] [Google Scholar]
- 26.Usui M, Matsuda S, Suzuki H, Ogura Y. Preoperative diagnosis of gallbladder torsion by magnetic resonance cholangiopancreatography. Scand J Gastroenterol. 2000;35(2):218–22. doi: 10.1080/003655200750024425. [DOI] [PubMed] [Google Scholar]