To the Editor: Auditory verbal hallucination (AVH) is defined as the hearing of voices in the absence of any external auditory stimulus.[1–3] Most AVH content is related to the experiencer, and these events usually cause serious distress. AVHs can occur in patients with a broad range of mental disorders and neurological diseases, such as schizophrenia, bipolar disorder (BP), major depressive disorder (MDD), post-traumatic stress disorder (PTSD), borderline personality disorder (BPD), and in healthy individuals.[2–4] They are most prevalent in schizophrenic patients, affecting more than 70% of this population. Beyond schizophrenia, up to 46% of patients with BPD, 11.3% to 62.8% of persons with BP, 5.4% to 40.6% of those with MDD, and 4.2% of individuals in the general population experience AVHs.[1–4]
Given its broad prevalence, AVH can be misdiagnosed and mistreated in the early stage, increasing the occurrence of side effects and enhancing affected individuals’ physical and mental suffering. AVH can also increase the risks of violence, suicidal behavior, and self-mutilation in affected patients. Hence, a means to facilitate early, precise diagnosis and treatment is urgently needed.[5–7]
Many scholars have emphasized the urgent need to explore the pathological features of AVHs (especially those common and specific to different subject categories) using multiple techniques and to identify precise treatment targets.[8,9] As language and speech are specific to human beings, no small animal model is available for the assessment of AVHs; due to the complexity and human specificity of AVH, it can be studied only in living experiencers.
Currently, we can depend only on new techniques in neuroscience to explore the pathological features and specific therapeutic targets of AVH in individuals with different disorders from multiple perspectives.[8,9] Multi-disciplinary research approaches, such as those combining genomics with human connectome techniques, are needed.[8,9]
In the last 3 years, many notable scholars have emphasized the importance of multi-modal and multi-disciplinary approaches to the exploration of AVH and its treatment in subjects with different mental disorders, particularly the early features of AVH in those with schizophrenia.[8,9] Using the full network of mutually interacting brain states and causal reasoning software, AVHs have been linked to abnormal activity in salience network components in patients with schizophrenia.[8,9] A study employing non-trend analysis revealed brain functional connectivity changes after treatment with clozapine in schizophrenic patients with AVHs.[8,9] Using linear support vector machines, the characteristics of AVHs in patients with schizophrenia have been explored with functional magnetic resonance imaging.[8,9] Electroencephalography (EEG) and diffusion tensor imaging have shown changes in the gamma-band synchronization and anisotropy of stimulated white matter in the auditory cortices of schizophrenic patients experiencing AVHs.[10] Moreover, AVHs were associated with specific dysfunctions in the default-mode and language-processing networks in such patients.[11] In a recent study, Mallikarjun et al[12] found that AVHs in patients with first-episode schizophrenia were correlated strongly with abnormal functioning of the salience network. Recently, Chen et al[13] demonstrated the presence of theta wave alterations in patients with AVHs. According to EEG-based studies, healthy individuals with AHVs are more likely to perform abnormal self-generated vocalization.[14] Overall, neuroimaging studies suggest that the human connectome method is useful for the identification of AVH pathological features and potential treatment targets in patients with schizophrenia, and that machine learning techniques (which reveal cognition patterns) can be used to establish predictive models for AVHs in subjects with various mental disorders.
At the same time, researchers have identified specific genes associated with AVH. Forkhead-box protein 2 (FOXP2)[15] has been reported to confer susceptibility to AVHs in patients with schizophrenia. The catechol-O-methyltransferase (COMT) and neuregulin 1 (NRG1) genes have been reported to influence the effects of AVH treatment in these patients.[16] Taken together, these findings suggest that AVHs are associated to some extent with genetic features. The intrinsic pathological features of AVHs may be elucidated on the genetic level. With the development of high-throughput and gene sequencing technology, neural circuits and brain networks have been shown to be regulated by gene networks (including RNA) in patients with mental disorders and in healthy individuals.[17] These studies provide important clues for the exploration of common and specific neuroimaging-genetic co-alteration features among those with mental disorders and healthy individuals.[17]
Pattern recognition methods have been used to establish predictive models for some diseases, and have enabled the achievement of many better effects.[18,19] For example, Yin et al[19] developed a novel method for AVH pattern recognition in schizophrenic patients, with 73.9% specificity. Findings of such research support the use of pattern recognition to establish a predictive model for AVH development in individuals with different mental disorders.
Thus, several important discoveries have been made in AVH-related research in the past 2 years. Previous studies have laid a solid foundation and provided new clues for the exploration of AVH features from neuroimaging and genetics perspectives. However, additional efforts are needed to elucidate the characteristics of this disorder at the micro- and macro-scales (from genetic to neuroimaging features). Cohort studies are needed to dynamically characterize the pathological features of AVH development and disease trajectory in persons with different mental disorders and healthy individuals. The exploration of dynamic neuroimaging and genetic features of AVHs in healthy individuals can provide especially important information that contributes to our understanding of the pathological mechanism of this disorder. Cohort studies are also needed to identify alterations in neuroimaging features that accompany AVH treatment progress, which will aid the establishment of specific treatment targets for patients with different mental disorders. The application of pattern recognition based on identified neuroimaging-genetic co-alterations can contribute to the establishment of a model which can provide an objective index to help clinical doctors increase the rate of early and accurate AVH diagnosis and develop precise treatment strategies.
We propose the following pathway for future AVH research, with two main components. First, researchers should examine subjects with first-episode untreated schizophrenia, BP, PTSD, BPD, and MDD, and healthy individuals experiencing first AVH episodes, using high-throughput sequencing techniques (central in genomics)[17] and human connectome techniques[17] to identify common and specific neuroimaging-genetic co-alteration features of AVHs, which could guide the development of specific treatment strategies. Given that the content, type, and effects of AVHs can vary significantly among mental disorders,[1–4] researchers should distinguish the neuroimaging-genetic co-alteration features of AVHs in terms of characteristics shared by, and specific to, schizophrenia, BP, PTSD, BPD, and MDD. Many studies have confirmed that the combined use of these techniques provides important information in neuroscience research.[17] Second, based on the data on AVH features acquired in such work, researchers should adopt machine learning techniques to identify qualitative factors enabling early diagnosis and to establish predictive models for treatment outcomes in individuals with different mental disorders. Using advanced pattern recognition, these classifiers and the predictive model can be integrated into a single logic algorithm model. The use of such modeling is a current trend in psychiatric research.[19]
The first novel aspect of the proposed research pathway is that it is based on the hypotheses, inspired by previous findings, that common and specific pathological features of AVHs will be found among subjects with different mental disorders and healthy individuals, and that neuroimaging-genetic co-alterations can form the basis of the development of a relatively stable and accurate index. In patients with AVHs, neuroimaging-genetic co-alteration may reflect intrinsic genetic/genomic features, neuropathological (endophenotype) features, and/or clinical manifestations (phenotypes). Brain abnormality (the endophenotype) may serve as a “bridge” between endogenous genomic differences and exogenous clinical features, regulated by specific genes and associated with the clinical manifestation of AVH in different subjects. This “bridge” can be detected using current technologies and can be used as a visual biomarker reflecting the relationships among the endogenous and exogenous features and the therapeutic target [Figure 1]. The identification of an abnormal “bridge” can provide evidence for early diagnosis, before an AVH episode, and enable prediction of the treatment outcome.
Figure 1.
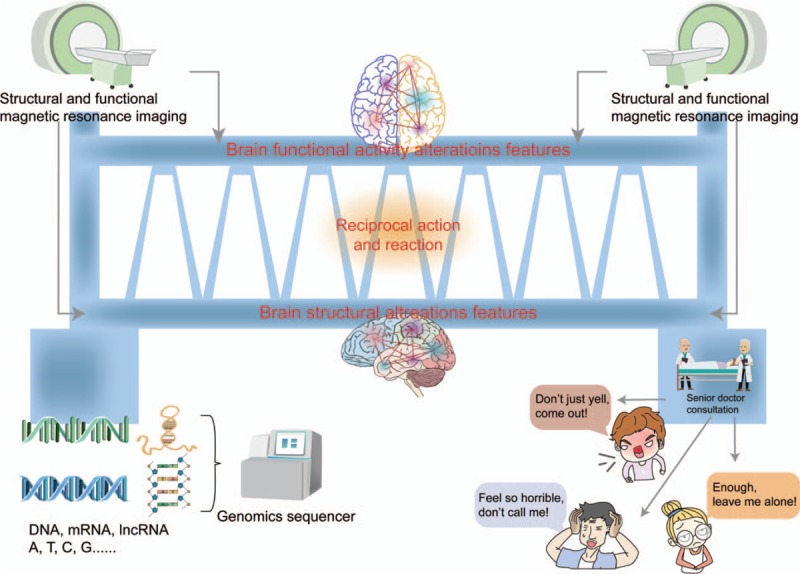
Potential pathological features (genetic, neurological, and clinical) in subjects experiencing AVHs. We propose the hypothesis of “pathological feature bridge of AVHs.” Patients with different diagnostic types of AVHs all have “pathological features bridge of AVHs.” This diagnostic specific “bridge” is comprised of three parts: endogenous genitic features, brain featurs regulated by genetic features, and clinical features of AVHs. The left end of “bridge” is endogenous genetic features, the middle part of “bridge” is brain features, and the right end of “bridge” is clinical features of AVHs. From left to right, the susceptibility to AVHs, which is determined by the endogenous genes, combined with early environmental factors lead to the gradual change of brain features (including structural and functional features) in the development of an individual, which eventually develops AVHs with different clinical features. AVHs: Auditory verbal hallucinations.
The second novel aspect of the proposed pathway is the performance of a large cohort study with a 2-year follow-up period from the first AVH episode, involving the combined use of machine learning, genomic, and brain connectome methods, as well as consideration of subjects’ sociodemographic characteristics and treatment outcomes, to establish a model for early diagnosis and treatment outcome prediction in different subject groups. The examination of dynamic alterations in AVHs (plastic changes in neuroimaging-genetic co-alteration features) with therapy in different subjects will also enable the identification of specific treatment targets. The resulting integrated model can aid the exploration of precise therapeutic strategies according to potential disease-specific targets [Figure 2].[20] Limited by our knowledge, this proposed pathway may have some flaws, and we invite international scholars to help us improve the concept and design appropriate studies to test it.
Figure 2.
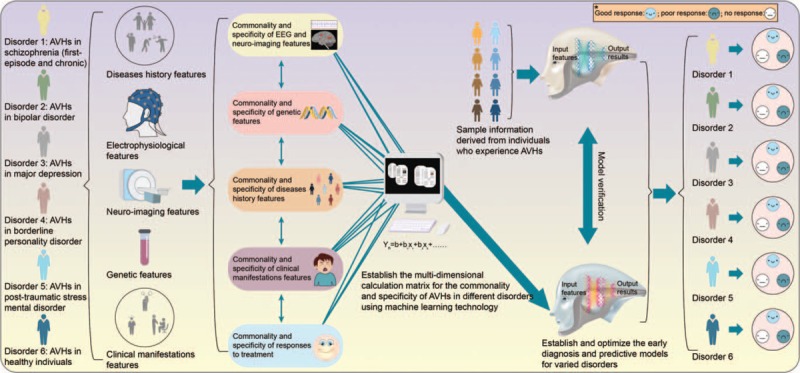
Integrated classification and predictive model based mainly on neuroimaging-genetic co-alteration features. We speculate that there are some common and specific characteristics influenced by neuroimaging-genetic basis and environmental factors in AVHs with different diagnostic types. These common and specific characteristics can provide information for early qualitative diagnosis and characterize the therapeutic targets of diseases. The common and specific neuroimaging-genetic features, as well as their dynamic change mode, can be investigated in AVHs with different diseases for the first episode through high-throughput sequencing and brain connectome. Based on the information, the early accurate diagnosis and treatment prediction model can be established and validated by pattern recognition technology. This prediction model can be applied in clinical practice to assist clinicians to identify the type as well as the prognosis of AVHs in the early stage, thus help clinicians optimize the treatment in the early stage. AVHs: Auditory verbal hallucinations.
Funding
This work was supported by grants from the Tianjin Health Bureau Foundation (No. 2014KR02), the National Natural Science Foundation of China (No. 81871052), the Key Projects of the Natural Science Foundation of Tianjin, China (No. 17JCZDJC35700), and Key Projects of Wenzhou Bureau of Science and Technology (No. ZS2017011).
Conflicts of interest
None.
Footnotes
How to cite this article: Cheng LL, Wang GW, Zhang YC, Li GY, Tian HJ, Wang LN, Sun XH, Zhou CH, Zhuo CJ. Exploring neuroimaging-genetic co-alteration features of auditory verbal hallucinations in different subjects for the establishment of a predictive model. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000385
References
- 1.Upthegrove R, Broome MR, Caldwell K, Ives J, Oyebode F, Wood SJ. Understanding auditory verbal hallucinations: a systematic review of current evidence. Acta Psychiatr Scand 2016; 133:352–367. doi: 10.1111/acps.12531. [DOI] [PubMed] [Google Scholar]
- 2.Laroi F, Sommer IE, Blom JD, Fernyhough C, Ffytche DH, Hugdahl K, et al. The characteristic features of auditory verbal hallucinations in clinical and nonclinical groups: state-of-the-art overview and future directions. Schizophr Bull 2012; 38:724–733. doi: 10.1093/schbul/sbs061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Waters F, Aleman A, Fernyhough C, Allen P. Report on the inaugural meeting of the International Consortium on Hallucination Research: a clinical and research update and 16 consensus-set goals for future research. Schizophr Bull 2012; 38:258–262. doi: 10.1093/schbul/sbr181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sommer IE, Daalman K, Rietkerk T, Diederen KM, Bakker S, Wijkstra J, et al. Healthy individuals with auditory verbal hallucinations; who are they? Psychiatric assessments of a selected sample of 103 subjects. Schizophr Bull 2010; 36:633–641. doi: 10.1093/schbul/sbn130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas N, Rossell SL, Waters F. The changing face of hallucination research: the International Consortium on Hallucination Research (ICHR) 2015 meeting report. Schizophr Bull 2016; 42:891–895. doi: 10.1093/schbul/sbv183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Toh WL, Castle DJ, Thomas N, Badcock JC, Rossell SL. Auditory verbal hallucinations (AVHs) and related psychotic phenomena in mood disorders: analysis of the 2010 Survey of High Impact Psychosis (SHIP) data. Psychiatry Res 2016; 243:238–245. doi: 10.1016/j.psychres.2016.06.035. [DOI] [PubMed] [Google Scholar]
- 7.Toh WL, Thomas N, Rossell SL. Auditory verbal hallucinations in bipolar disorder (BD) and major depressive disorder (MDD): a systematic review. J Affect Disord 2015; 184:18–28. doi: 10.1016/j.jad.2015.05.040. [DOI] [PubMed] [Google Scholar]
- 8.The 4th International Consortium on Hallucination Research. Available from: https://ichr2017.sciencesconf.org/resource [Accessed November 11, 2017]. [Google Scholar]
- 9.The 5th International Consortium on Hallucination Research. Available from: https://hallucinationconsortium.org/conferences/2018-conference-kyoto-japan/ [Accessed August 11, 2018]. [Google Scholar]
- 10.Steinmann S, Amselberg R, Cheng B. The role of functional and structural interhemispheric auditory connectivity for language lateralization – a combined EEG and DTI study. Sci Rep 2018; 8:15428.doi: 10.1038/s41598-018-33586-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scheinost D, Tokoglu F, Hampson M, Hoffman R, Constable RT. Data-driven analysis of functional connectivity reveals a potential auditory verbal hallucination network. Schizophr Bull 2019; 45:415–424. doi: 10.1093/schbul/sby039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mallikarjun PK, Lalousis PA. Aberrant salience network functional connectivity in auditory verbal hallucinations: a first episode psychosis sample. Transl Psychiatry 2018; 8:69.doi: 10.1038/s41398-018-0118-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen X, Ji GJ, Zhu C, Bai X, Wang L, He K, et al. Neural correlates of auditory verbal hallucinations in schizophrenia and the therapeutic response to theta-burst transcranial magnetic stimulation. Schizophr Bull 2019; 45:474–483. doi: 10.1093/schbul/sby054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pinheiro AP, Schwartze M, Kotz SA. Voice-selective prediction alterations in nonclinical voice hearers. Sci Rep 2018; 8:14717.doi: 10.1038/s41598-018-32614-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCarthy-Jones S, Green MJ, Scott RJ, Tooney PA, Cairns MJ, Wu JQ, et al. Preliminary evidence of an interaction between the FOXP2 gene and childhood emotional abuse predicting likelihood of auditory verbal hallucinations in schizophrenia. J Psychiatr Res 2014; 50:66–72. doi: 10.1016/j.jpsychires.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 16.Chhabra H, Shivakumar V, Subbanna M, Kalmady SV, Bose A, Agarwal SM, Sreeraj VS. Gene polymorphisms and response to transcranial direct current stimulation for auditory verbal hallucinations in schizophrenia. Acta Neuropsychiatr 2018; 30:218–225. doi: 10.1017/neu.2018.4. [DOI] [PubMed] [Google Scholar]
- 17.Radulescu E, Jaffe AE, Straub RE, Chen Q, Shin JH, Hyde TM, et al. Identification and prioritization of gene sets associated with schizophrenia risk by co-expression network analysis in human brain. Mol Psychiatry 2018; 23:1–14. doi: 10.1038/s41380-018-0304-1. [DOI] [PubMed] [Google Scholar]
- 18.Cui LB, Liu L, Guo F, Chen YC, Chen G, Xi M, et al. Disturbed brain activity in resting-state networks of patients with first-episode schizophrenia with auditory verbal hallucinations: a cross-sectional functional MR imaging study. Radiology 2017; 283:810–819. doi: 10.1148/radiol.2016160938. [DOI] [PubMed] [Google Scholar]
- 19.Xia M, He Y. Functional connectomics from a “big data” perspective. Neuroimage 2017; 160:152–167. doi: 10.1016/j.neuroimage.2017.02.031. [DOI] [PubMed] [Google Scholar]
- 20.Sommer IE, Kleijer H, Hugdahl K. Toward personalized treatment of hallucinations. Curr Opin Psychiatry 2018; 31:237–245. doi: 10.1097/YCO.0000000000000416. [DOI] [PubMed] [Google Scholar]


