Abstract
Vitamin B12 deficiency can cause extensive hematologic alterations such as pancytopenia, macrocytosis, hypersegmentation of neutrophils, and hypercellular bone marrow with blastic differentiation. These dysplastic changes can sometimes be so profound that they mimic myelodysplastic syndromes or even acute leukemia, leading to extensive workup and aggressive treatment measures. We present a patient who was referred to our tertiary care medical center for treatment of suspected acute myeloid leukemia on the basis of peripheral smear and bone marrow biopsy findings, and induction chemotherapy was considered. However, the patient was found to have vitamin B12 deficiency, with improvement in pancytopenia and blastic changes with parenteral vitamin B12 supplementation. This highlights the importance of recognizing that dysplastic changes in patients with vitamin B12 deficiency could be misleading.
Keywords: Acute leukemia, megaloblastic anemia, myelodysplastic syndrome, pancytopenia, vitamin B12 deficiency
Early identification and prompt treatment of vitamin B12 deficiency is of utmost importance, because it is a reversible cause of ineffective hematopoiesis,1 in contrast to myelodysplastic syndrome or acute myeloid leukemia, which are irreversible disorders of ineffective hematopoiesis. Deficiency of vitamin B12 causes impaired nucleic acid metabolism, resulting in asynchrony between the cytoplasm and nuclear maturation, leading to megaloblastic anemia.2 Characteristic findings include red cell macrocytosis, hypersegmented neutrophils in the peripheral blood, and hypercellular bone marrow with giant bands and proerythroblasts.3 These findings can sometimes result in the misdiagnosis of myelodysplastic syndrome due to nuclear cytoplasmic asynchrony or even acute leukemia due to increased proerythroblasts.4,5 Some of these patients also end up receiving extensive workup and are treated with aggressive measures.6 In this report, we present a patient who was referred to our hospital with concerns for acute leukemia but in fact had vitamin B12 deficiency.
CASE DESCRIPTION
A 57-year-old nonvegetarian man presented to an outside facility with a 3-week history of progressive generalized weakness and dyspnea on exertion. He had a previous history of alcohol abuse about 3 years earlier. Physical examination was significant for pallor. Initial laboratory results showed pancytopenia with peripheral blood differential counts of 73.2% neutrophils, 21% lymphocytes, 1.7% monocytes, and no basophils or eosinophils. His laboratory workup is summarized in Table 1. His hemoglobin 2 weeks prior to this presentation was 9 g/dL. A basic metabolic panel and coagulation studies were within normal limits. Coombs test was negative, thyroid-stimulating hormone was normal, and a hepatitis panel, stool for occult blood, and HIV screen were negative. The patient received two units of packed red blood cells and was started on oral vitamin B12 1000 μg/day. However, his pancytopenia continued to worsen and bone marrow biopsy was performed. The preliminary biopsy reported an elevated blast percentage. Induction chemotherapy was considered and the patient was transferred to our tertiary care center due to suspected acute myeloid leukemia.
Table 1.
Initial laboratory findings
| Test | Result | Reference range |
|---|---|---|
| Hemoglobin (g/dL) | 4.3 | 13–17 |
| White blood cells (/mm3) | 3400 | 4500–10,800 |
| Platelet count (cells/mm3) | 92,000 | 150,000–450,000 |
| Mean corpuscular volume (fl) | 102 | 80–94 |
| Red blood cell distribution width | 16.2% | 11.5%–15% |
| Haptoglobin (mg/dL) | <8 | 30–200 |
| Reticulocyte index | 0.16 | 0.5–2.5 |
| Total bilirubin (mg/dL) | 2.3 | 0–1.5 |
| Direct bilirubin (mg/dL) | 1.2 | <0.3 |
| Lactate dehydrogenase (U/L) | 2510 | 100–220 |
| Serum vitamin B12 (pg/mL) | 68 | 200–700 |
| Serum folic acid (ng/mL) | 7.8 | >4 |
| Ferritin (ng/mL) | 110 | 12–300 |
| Total iron-binding capacity (μg/dL) | 325 | 240–450 |
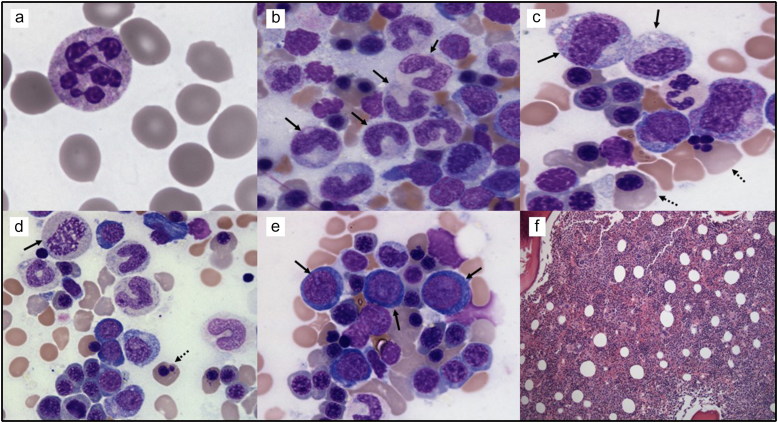
In our facility, the patient’s peripheral smear showed scattered hyperlobated neutrophils, normocytic normochromic anemia with mild anisopoikilocytosis including scattered macrocytes, rare nucleated red blood cells, and marked thrombocytopenia. A repeat bone marrow biopsy showed 90% cellularity with trilineage hematopoiesis and was notable for numerous giant band forms, left-shifted erythroid hyperplasia, and dyspoietic features in all three lineages (Figure 1). The flow cytometry analysis and acute myeloid leukemia panel by fluorescence in situ hybridization did not show any evidence of acute leukemia. Cytogenetics showed a normal male karyotype. The patient received daily parenteral vitamin B12 injections with rapid bone marrow recovery, as evidenced by improvement in the blood counts and reticulocyte index. He was discharged 6 days later and continued to receive vitamin B12 injections once weekly as an outpatient. Upon 45-day follow-up in the clinic, laboratory work revealed improvement in all cell counts, resolution of macrocytosis, and return of lactate dehydrogenase to a normal level (Table 2). The patient tested negative for antiparietal cell antibodies and intrinsic factor antibody.
Figure 1.
(a) Peripheral blood smear showing a hypersegmented neutrophil and macrocytes. Bone marrow aspirate showing (b) numerous giant bands (arrows); (c, d) myeloid precursors with nuclear cytoplasmic asynchrony (solid black arrow) and erythroid precursor showing nuclear cytoplasmic asynchrony, nuclear budding, and multinucleation (dashed black arrow); (e) erythroid precursors including scattered proerythroblasts that may erroneously be labeled as blasts. (f) Bone marrow biopsy showing hypercellularity (>95% cellularity).
Table 2.
Laboratory test results over time
| Variable | Reference range | With oral B12 supplementation |
With parenteral B12 supplementation |
|||||
|---|---|---|---|---|---|---|---|---|
| Day 1 | Day 3 | Day 5 | Day 7 | Day 9 | Day 11 (discharged) | Day 52 (clinic) | ||
| Hemoglobin (g/dL) | 13–17 | 4.3 | 7a | 7.5 | 6.7 | 7.6 | 9 | 11 |
| White cell count (cells/mm3) | 4500–10,800 | 3400 | 2400 | 800 | 3920 | 2600 | 9220 | 4510 |
| Differential count (%) | ||||||||
| Neutrophils | 40–75% | 73.2% | 74% | 82% | 81.4% | 56.5% | 86.7% | 67.4% |
| Lymphocytes | 20–45% | 21% | 23% | 13% | 6.9% | 16.8% | 4.4% | 17.1% |
| Monocytes | 2–10% | 1.7% | 1.5% | 3% | 7.1% | 16.9% | 5.3% | 13.5% |
| Basophils | 0–2% | 0 | 0 | 0 | 0 | 0.4% | 0.9% | 1.3% |
| Absolute neutrophil count (cells/mm3) | 1400–6000 | 2500 | 1776 | 650 | 3200 | 1500 | 8000 | 3000 |
| Platelet count (cells/mm3) | 150,000–450,000 | 92,000 | 61,000 | 39,000 | 42,000 | 75,000 | 193,000 | 328,000 |
| Mean corpuscular volume (fl) | 80–94 | 102 | 91 | 90 | 91.6 | 93.1 | 95.5 | 85.2 |
| Reticulocyte index | 0.16 | 0.19 | 4.2 | |||||
| Total bilirubin (mg/dL) | 0–1.5 | 2.3 | 13 | 3.8 | 3.8 | 0.4 | ||
| Direct bilirubin (mg/dL) | <0.3 | 1.2 | 6.9 | 2 | 1.4 | — | ||
| Lactate dehydrogenase (U/L) | 100–220 | 2510 | 1,187 | 687 | 482 | 147 | ||
After transfusion.
DISCUSSION
Vitamin B12 deficiency is easily treatable but is often underrecognized.7 Its symptoms can be clinically subtle, with hematological abnormalities ranging from an incidentally discovered increase in mean corpuscular volume in asymptomatic patients to full-blown megaloblastic anemia.3 Less commonly, patients have life-threatening hematological manifestations including pancytopenia and hemolytic anemia.6 The patient discussed in this case report had vitamin B12 deficiency with macrocytosis, pancytopenia, and concurrent hemolysis (elevated lactate dehydrogenase and indirect bilirubin and low haptoglobin). The patient also had a low reticulocyte count, indicating an inadequate bone marrow response to the anemia. Hemolysis in patients with vitamin B12 deficiency has been attributed to intramedullary destruction of red blood cells due to ineffective erythropoiesis.
Deficiency of vitamin B12 is more commonly caused by malabsorption,8 although nutritional insufficiency is frequently seen in older patients,9 alcoholics,10 and vegans and vegetarians.11 We speculate that our patient’s previous history of alcohol abuse combined with chronic malabsorption could have contributed to this deficiency. This could also explain his initial lack of response to oral vitamin B12 supplementation but excellent response with complete normalization of cell counts with parenteral supplementation. A serum B12 level <200 pg/mL along with clinical evidence of disease is consistent with deficiency, and no further confirmatory testing is needed. However, in symptomatic patients with borderline B12 levels from 200 to 300 pg/mL, deficiency is possible and verification with serum methylmalonic acid and/or serum homocysteine level may be necessary.12
Though bone marrow biopsy is not typically needed for the diagnosis of B12 deficiency, many patients with severe pancytopenia undergo this procedure.13 Not only does this sometimes result in complicating the initial assessment but it could also lead to missing the diagnosis and further expensive workup. In a case series reported by Kim et al, 12 patients with pancytopenia were initially diagnosed as having myelodysplastic syndrome, but they responded rapidly to a 7-day parenteral vitamin B12 treatment with complete normalization of blood counts, proving that they, in fact, had B12 deficiency.14
The patient discussed in this report was referred to us for concerns of acute myeloid leukemia, because he had pancytopenia and results of bone marrow aspiration cytology showed markedly hypercellular marrow with accelerated erythropoiesis with megaloblastic changes that were believed to be secondary to acute leukemia. However, his repeat bone marrow biopsy findings in our institute showed no evidence of blasts, with normal flow cytometry and cytogenetics, supported by a low serum vitamin B12 level and normalization of blood counts after parenteral vitamin B12 supplementation, which favors the diagnosis of vitamin B12 deficiency.
In conclusion, it is important to recognize that bone marrow biopsy in patients with vitamin B12 deficiency could be misleading, because it may appear to show dysplastic changes mimicking myelodysplastic syndrome or acute leukemia. Vitamin B12 deficiency should be ruled out in all suspected diagnosis of myelodysplastic syndrome and acute myeloid leukemia in clinically relevant settings. Parenteral vitamin B12 supplementation should be considered in patients with vitamin B12 deficiency and pancytopenia.
References
- 1.Stabler SP. Clinical practice. Vitamin B12 deficiency. N Engl J Med. 2013;368:149–160. [DOI] [PubMed] [Google Scholar]
- 2.Aslinia F, Mazza JJ, Yale SH. Megaloblastic anemia and other causes of macrocytosis. Clin Med Res. 2006;4:236–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Briani C, Dalla Torre C, Citton V, et al. Cobalamin deficiency: clinical picture and radiological findings. Nutrients. 2013;5:4521–4539. doi: 10.3390/nu5114521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh N, Qayyum S, Wasik MA, Luger SM. Combined B12 and folate deficiency presenting as an aggressive hematologic malignancy. Am J Hematol. 2015;90:964–965. doi: 10.1002/ajh.23987. [DOI] [PubMed] [Google Scholar]
- 5.Aitelli C, Wasson L, Page R. Pernicious anemia: presentations mimicking acute leukemia. South Med J. 2004;97:295–297. doi: 10.1097/01.SMJ.0000082003.98003.88. [DOI] [PubMed] [Google Scholar]
- 6.Andres E, Affenberger S, Zimmer J, et al. Current hematological findings in cobalamin deficiency. A study of 201 consecutive patients with documented cobalamin deficiency. Clin Lab Haematol. 2006;28:50–56. doi: 10.1111/j.1365-2257.2006.00755.x. [DOI] [PubMed] [Google Scholar]
- 7.Dharmarajan TS, Adiga GU, Norkus EP. Vitamin B12 deficiency. Recognizing subtle symptoms in older adults. Geriatrics. 2003;58:30–38. [PubMed] [Google Scholar]
- 8.Andres E, Vogel T, Kaltenbach G, Lang PO. Food-cobalamin malabsorption and vitamin B12 deficiency in adults and in elderly patients: what is the problem? Rev Med Interne. 2016;37:511–513. [DOI] [PubMed] [Google Scholar]
- 9.Baik HW, Russell RM. Vitamin B12 deficiency in the elderly. Annu Rev Nutr. 1999;19:357–377. doi: 10.1146/annurev.nutr.19.1.357. [DOI] [PubMed] [Google Scholar]
- 10.Laufer EM, Hartman TJ, Baer DJ, et al. Effects of moderate alcohol consumption on folate and vitamin B(12) status in postmenopausal women. Eur J Clin Nutr. 2004;58:1518–1524. doi: 10.1038/sj.ejcn.1602002. [DOI] [PubMed] [Google Scholar]
- 11.Pawlak R, Lester SE, Babatunde T. The prevalence of cobalamin deficiency among vegetarians assessed by serum vitamin B12: a review of literature. Eur J Clin Nutr. 2014;68:541–548. doi: 10.1038/ejcn.2014.46. [DOI] [PubMed] [Google Scholar]
- 12.Hannibal L, Lysne V, Bjorke-Monsen AL, et al. Biomarkers and algorithms for the diagnosis of vitamin B12 deficiency. Front Mol Biosci. 2016;3:27. doi: 10.3389/fmolb.2016.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Randhawa J, Ondrejka SL, Setrakian S, Taylor H. What should I know before ordering a bone marrow aspiration/biopsy in patients with vitamin B12 deficiency? BMJ Case Rep. 2013;2013 pii: bcr2013010200. doi: 10.1136/bcr-2013-010200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim M, Lee SE, Park J, et al. Vitamin B(12)-responsive pancytopenia mimicking myelodysplastic syndrome. Acta Haematol. 2011;125:198–201. doi: 10.1159/000322941. [DOI] [PubMed] [Google Scholar]