Correction to: Heart and Vessels 10.1007/s00380-019-01425-x
In the original publication of the article, the Figure 2b and the Tables 2 and 3 were published incorrectly.
The corrected Figure 2b and Tables 2 and 3 are provided below. 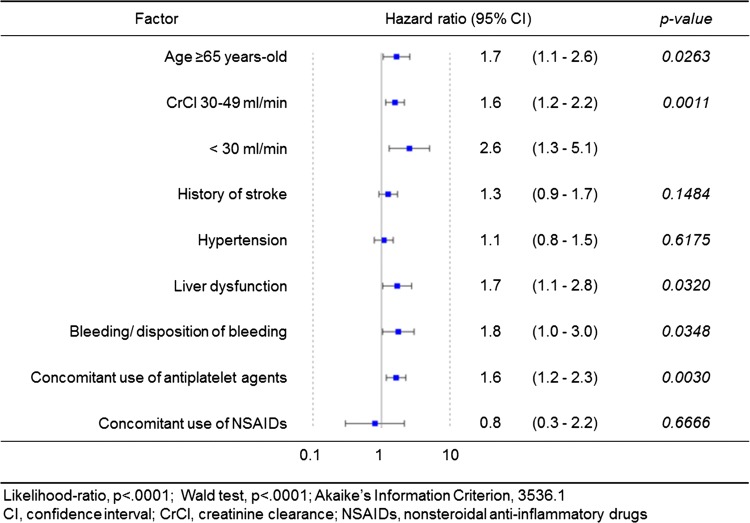
Table 2.
Incidence rate and univariate analysis by Cox proportional hazards analysis of stroke/systemic embolism
| No. of event (%/year) | HR | 95% CI | p value | |
|---|---|---|---|---|
| Overall | 176 (1.0) | |||
| Sex | ||||
| Male | 115 (1.0) | Reference | 0.5283 | |
| Female | 61 (1.1) | 1.1 | 0.8, 1.5 | |
| Age class 1 (years-old) | ||||
| < 65 | 23 (0.7) | Reference | 0.0176 | |
| ≥ 65 | 153 (1.1) | 1.7 | 1.1, 2.6 | |
| Age class 2 (years-old) | ||||
| < 65 | 23 (0.7) | Reference | 0.0022 | |
| 65–74 | 60 (0.9) | 1.3 | 0.8, 2.2 | |
| ≥ 75 | 93 (1.3) | 2.0 | 1.3, 3.2 | |
| Body weight (kg) | ||||
| ≥ 60 | 84 (0.8) | Reference | 0.0250 | |
| 50–59 | 50 (1.1) | 1.3 | 0.9, 1.9 | |
| < 50 | 33 (1.4) | 1.7 | 1.1, 2.6 | |
| Systolic blood pressure (mmHg) | ||||
| < 160 | 156 (1.0) | Reference | 0.0928 | |
| ≥ 160 | 12 (1.6) | 1.6 | 0.9, 3.0 | |
| CrCl (mL/min) | ||||
| ≥ 50 | 112 (0.9) | Reference | 0.0026 | |
| 30–49 | 49 (1.5) | 1.8 | 1.3, 2.5 | |
| < 30 | 3 (1.0) | 1.2 | 0.4, 3.7 | |
| Comorbiditya | ||||
| Congestive heart failure | ||||
| – | 129 (1.0) | Reference | 0.8550 | |
| + | 47 (1.0) | 1.0 | 0.7, 1.4 | |
| Hypertension | ||||
| – | 44 (0.9) | Reference | 0.2768 | |
| + | 132 (1.1) | 1.2 | 0.9, 1.7 | |
| Angina pectoris | ||||
| – | 157 (1.0) | Reference | 0.7193 | |
| + | 19 (0.9) | 0.9 | 0.6, 1.5 | |
| Diabetes mellitus | ||||
| – | 121 (0.9) | Reference | 0.0227 | |
| + | 55 (1.3) | 1.4 | 1.1, 2.0 | |
| Aortic aneurysm | ||||
| – | 174 (1.0) | Reference | 0.7916 | |
| + | 2 (0.8) | 0.8 | 0.2, 3.3 | |
| Deep vein thrombosis | ||||
| – | 175 (1.0) | Reference | 0.9718 | |
| + | 1 (1.0) | 1.0 | 0.2, 7.4 | |
| Pulmonary embolism | ||||
| – | 175 (1.0) | Reference | 0.4012 | |
| + | 1 (2.2) | 2.3 | 0.3, 16.2 | |
| Dyslipidemia | ||||
| – | 105 (1.0) | Reference | 0.6278 | |
| + | 71 (1.0) | 0.9 | 0.7, 1.3 | |
| Liver dysfunction | ||||
| – | 167 (1.0) | Reference | 0.6999 | |
| + | 9 (0.9) | 0.9 | 0.5, 1.7 | |
| Renal dysfunction | ||||
| – | 176 (1.0) | Reference | 0.6995 | |
| + | 0 (0.0) | < 0.001 | < 0.001 | |
| Medical historya | ||||
| Stroke (ischemic/hemorrhagic) | ||||
| – | 91 (0.7) | Reference | < 0.0001 | |
| + | 85 (2.3) | 3.6 | 2.7, 4.8 | |
| Transient ischemic attack | ||||
| – | 169 (0.9) | Reference | 0.4721 | |
| + | 7 (1.3) | 1.3 | 0.6, 2.8 | |
| Systemic embolism | ||||
| – | 174 (1.0) | Reference | 0.6643 | |
| + | 2 (1.4) | 1.4 | 0.3, 5.5 | |
| Vascular disease (MI/PAD) | ||||
| – | 158 (1.0) | Reference | 0.0352 | |
| + | 18 (1.6) | 1.7 | 1.0, 2.7 | |
| Malignant tumor | ||||
| – | 159 (1.0) | Reference | 0.7657 | |
| + | 17 (1.1) | 1.1 | 0.7, 1.8 | |
| Bleeding/disposition of bleeding | ||||
| – | 169 (1.0) | Reference | 0.9900 | |
| + | 7 (1.0) | 1.0 | 0.5, 2.1 | |
| Rivaroxaban dosage | ||||
| 15 mg/day | 87 (0.9) | Reference | 0.0658 | |
| 10 mg/day | 89 (1.2) | 1.3 | 1.0, 1.8 | |
| Amount of drinking (unit/week) | ||||
| No | 105 (1.1) | Reference | 0.1202 | |
| < 8 | 47 (0.8) | 0.7 | 0.5, 1.0 | |
| ≥ 8 | 24 (1.0) | 0.9 | 0.6, 1.4 | |
| History of smoking | ||||
| No | 99 (0.9) | Reference | 0.2940 | |
| In the past | 54 (1.1) | 1.1 | 0.8, 1.6 | |
| Current | 23 (1.3) | 1.4 | 0.9, 2.2 | |
| Type of AF | ||||
| PAF | 67 (0.9) | Reference | 0.0799 | |
| Non-PAFb | 109 (1.1) | 1.3 | 1.0, 1.8 | |
| Using concomitant anti-plateletsa | ||||
| – | 138 (0.9) | Reference | 0.0046 | |
| + | 38 (1.5) | 1.7 | 1.2, 2.4 | |
| Using concomitant NSAIDsa | ||||
| – | 172 (1.0) | Reference | 0.9525 | |
| + | 4 (1.0) | 1.0 | 0.4, 2.8 | |
| CHADS2 score | ||||
| < 3 | 76 (0.7) | Reference | < 0.0001 | |
| ≥ 3 | 100 (1.7) | 2.7 | 2.0, 3.6 | |
| CHA2DS2-VASc score | ||||
| < 4 | 58 (0.6) | Reference | < 0.0001 | |
| ≥ 4 | 118 (1.5) | 2.5 | 1.9, 3.5 | |
| HAS-BLED score | ||||
| < 2 | 60 (0.6) | Reference | < 0.0001 | |
| ≥ 2 | 106 (1.7) | 2.8 | 2.0, 3.8 |
HR hazard ratio, CI confidence interval, CrCl creatinine clearance, MI myocardial infraction, PAD peripheral arterial disease, AF atrial fibrillation, PAF paroxysmal atrial fibrillation, NSAIDs non-steroidal anti- inflammatory drugs
aReference; without factor
bPersistent and permanent atrial fibrillation
Table 3.
Incidence rate and univariate analysis by Cox proportional hazards analysis of ISTH major bleeding
| ISTH major bleeding | ||||
|---|---|---|---|---|
| No. of event (%/year) | HR | 95% CI | p value | |
| Overall | 215 (1.2) | |||
| Sex | ||||
| Male | 147 (1.2) | Reference | 0.8223 | |
| Female | 68 (1.2) | 1.0 | 0.7, 1.3 | |
| Age class 1 (years-old) | ||||
| < 65 | 26 (0.7) | Reference | 0.0027 | |
| ≥ 65 | 189 (1.4) | 1.9 | 1.2, 2.8 | |
| Age class 2 (years-old) | ||||
| < 65 | 26 (0.7) | Reference | < 0.0001 | |
| 65–74 | 66 (1.0) | 1.3 | 0.8, 2.1 | |
| ≥ 75 | 123 (1.7) | 2.4 | 1.6, 3.6 | |
| Body weight (kg) | ||||
| ≥ 60 | 125 (1.3) | Reference | 0.7249 | |
| 50–59 | 52 (1.1) | 0.9 | 0.7, 1.3 | |
| < 50 | 31 (1.3) | 1.1 | 0.7, 1.6 | |
| Systolic blood pressure (mmHg) | ||||
| < 160 | 199 (1.3) | Reference | 0.2772 | |
| ≥ 160 | 6 (0.8) | 0.6 | 0.3, 1.4 | |
| CrCl (mL/min) | ||||
| ≥ 50 | 138 (1.1) | Reference | < 0.0001 | |
| 30–49 | 59 (1.8) | 1.8 | 1.3, 2.4 | |
| < 30 | 9 (2.9) | 2.9 | 1.5, 5.6 | |
| Comorbiditya | ||||
| CHF | ||||
| – | 149 (1.2) | Reference | 0.1140 | |
| + | 66 (1.4) | 1.3 | 1.0, 1.7 | |
| Hypertension | ||||
| – | 53 (1.1) | Reference | 0.1770 | |
| + | 162 (1.3) | 1.2 | 0.9, 1.7 | |
| Angina pectoris | ||||
| – | 181 (1.2) | Reference | 0.0543 | |
| + | 34 (1.7) | 1.4 | 0.9, 2.1 | |
| Diabetes mellitus | ||||
| – | 159 (1.2) | Reference | 0.4925 | |
| + | 56 (1.3) | 1.1 | 0.8, 1.5 | |
| Aortic aneurysm | ||||
| – | 210 (1.2) | Reference | 0.2144 | |
| + | 5 (2.1) | 1.7 | 0.7, 4.2 | |
| DVT | ||||
| – | 212 (1.2) | Reference | 0.0823 | |
| + | 3 (3.1) | 2.6 | 0.9, 8.3 | |
| PE | ||||
| – | 214 (1.2) | Reference | 0.5833 | |
| + | 1 (2.2) | 1.7 | 0.2, 12.3 | |
| Dyslipidemia | ||||
| – | 125 (1.2) | Reference | 0.9155 | |
| + | 90 (1.2) | 1.0 | 0.8, 1.3 | |
| Liver dysfunction | ||||
| – | 195 (1.2) | Reference | 0.0252 | |
| + | 20 (2.0) | 1.7 | 1.1, 2.7 | |
| Renal dysfunction | ||||
| – | 215 (1.2) | Reference | 0.6682 | |
| + | 0 (0.0) | < 0.001 | < 0.001, > 999.9 | |
| Medical history | ||||
| Stroke (ischemic/hemorrhagic) | ||||
| – | 154 (1.1) | Reference | 0.0065 | |
| + | 61 (1.7) | 1.5 | 1.1, 2.0 | |
| Transient ischemic attack | ||||
| – | 208 (1.2) | Reference | 0.8415 | |
| + | 7 (1.3) | 1.1 | 0.5, 2.3 | |
| Systemic embolism | ||||
| – | 215 (1.2) | Reference | 0.1736 | |
| + | 0 (0.0) | < 0.001 | < 0.001, > 999.9 | |
| Vascular disease (MI/PAD) | ||||
| – | 196 (1.2) | Reference | 0.1345 | |
| + | 19 (1.7) | 1.4 | 0.9, 2.3 | |
| Malignant tumor | ||||
| – | 189 (1.2) | Reference | 0.1145 | |
| + | 26 (1.7) | 1.4 | 0.9, 2.1 | |
| Bleeding/disposition of bleeding | ||||
| – | 200 (1.2) | Reference | 0.0240 | |
| + | 15 (2.1) | 1.8 | 1.1, 3.1 | |
| Rivaroxaban dosage | ||||
| 15 mg/day | 108 (1.1) | Reference | 0.0635 | |
| 10 mg/day | 107 (1.4) | 1.3 | 1.0, 1.7 | |
| Amount of drinking (unit/week) | ||||
| No | 128 (1.4) | Reference | 0.0649 | |
| < 8 | 57 (1.0) | 0.7 | 0.5, 1.0 | |
| ≥ 8 | 30 (1.3) | 0.9 | 0.6, 1.4 | |
| History of smoking | ||||
| No | 126 (1.2) | Reference | 0.4144 | |
| In the past | 71 (1.4) | 1.2 | 0.9, 1.6 | |
| Current | 18 (1.0) | 0.9 | 0.5, 1.4 | |
| Type of AF | ||||
| PAF | 89 (1.1) | Reference | 0.3453 | |
| Non-PAFb | 126 (1.3) | 1.1 | 0.9, 1.5 | |
| Using concomitant anti-plateletsa | ||||
| – | 166 (1.1) | Reference | 0.0003 | |
| + | 49 (2.0) | 1.8 | 1.3, 2.5 | |
| Using concomitant NSAIDsa | ||||
| – | 211 (1.2) | Reference | 0.7265 | |
| + | 4 (1.0) | 0.8 | 0.3, 2.3 | |
| CHADS2 score | ||||
| < 3 | 121 (1.0) | Reference | 0.0009 | |
| ≥ 3 | 94 (1.6) | 1.6 | 1.2, 2.1 | |
| CHA2DS2-VASc score | ||||
| < 4 | 92 (1.0) | Reference | 0.0001 | |
| ≥ 4 | 123 (1.6) | 1.7 | 1.3, 2.2 | |
| HAS-BLED score | ||||
| < 2 | 92 (0.9) | Reference | < 0.0001 | |
| ≥ 2 | 111 (1.7) | 1.9 | 1.4, 2.5 | |
HR hazard ratio, CI confidence interval, ISTH International Society on Thrombosis and Haemostasis, CrCl creatinine clearance, MI myocardial infraction, PAD peripheral arterial disease, AF atrial fibrillation, PAF paroxysmal atrial fibrillation, NSAIDs non-steroidal anti-inflammatory drugs
aReference; without factor
bPersistent and permanent atrial fibrillation
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.


