Abstract
The purpose of this study was to examine the association between oral health literacy, preventive orientation and behaviors, and chronic medical conditions—specifically, hypertension and diabetes. A cross-sectional study was conducted with dental school patients attending the dental clinics in Los Angeles, California, and Baltimore, Maryland. Their health literacy levels were measured using the short Test of Functional Health Literacy in Adults (Short-TOFHLA) and the Rapid Estimate of Adult Literacy in Medicine and Dentistry (REALM-D). The medical history and existing medical conditions—specifically, hypertension and diabetes status—were extracted from patient health history and electronic records. Ten items were asked about preventive behaviors (e.g., brushing teeth in evening, smoking, exercise, drinking soda) and 3 preventive health services (dental checkup, flu shot, medical checkup). Six locus of control items were asked (e.g., good health is a matter of good fortune, what happens to my health is God’s will). Out of 793 subjects, 221 had a documented history of hypertension, 88 with diabetes. There was an association between Short-TOFHLA scores and both diabetes and hypertension, but after controlling for sociodemographic and preventive variables, the association was no longer significant. In multivariate analysis, women, people with at least some college, Asians or non-Hispanic Whites, younger people, those who spoke English as a child, those who sought health information from the Internet or health care professionals, and those who smoked reported lower utilization of preventive health services, and those who had less locus of control reported higher Short-TOFHLA scores. There were no significant differences in mean REALM-D scores between patients who had hypertension or diabetes versus not having the condition. Multivariate models showed that people with higher REALM-D scores had at least some college, were other race/ethnicity or non-Hispanic White, spoke English as a child, and sought health information via the Internet.
Knowledge Transfer Statement: The results of this study show that dental school patients exhibit a range of health literacy abilities and preventive behaviors, and health literacy measures positively correlated with some preventive behaviors but not others. Dental schools receive a significant number of patients with chronic diseases, and students should be educated to use effective patient communication skills to reinforce positive health behaviors among these patients.
Keywords: diabetes, hypertension, Short-TOFHLA, REALM-D, adults, knowledge measures
Introduction
Chronic diseases such as diabetes and hypertension require patient education to achieve adequate control and prevent adverse health outcomes. Hypertension affects approximately 77 million individuals in the United States (Go et al. 2014). Despite effective therapies, only 37% of patients with hypertension achieve their target blood pressure, well below the goal of 50% set by Healthy People 2010 (US Department of Health and Human Services 2010). Diabetes is one of the more common diseases in the United States, affecting more than 30 million people, accounting for 9.4% of the US population (Centers for Disease Control and Prevention [CDC] 2017). Outcomes for diabetes care are frequently unsatisfactory for unknown reasons, despite high rates of health care access and use, but inadequate health literacy was identified as one of the factors (Schillinger et al. 2002; Bailey et al. 2014; CDC 2016). Control of hypertension and diabetes, both chronic diseases, often requires people to engage in multiple complex tasks, including medication adherence, frequent medical visits, and diet and lifestyle modifications (Poureslami et al. 2017). These tasks may be more difficult for people with limited health literacy (Al Sayah et al. 2013; Eyüboğlu and Schultz 2016). Early evidence indicates that deficits in health literacy are associated with poorer health outcomes and higher health-related costs for both individuals and systems and are an independent predictor of outcomes distinct from education attainment and other measures of socioeconomic status (SES) (Sudore et al. 2006; Berkman et al. 2011).
Health literacy includes the ability to understand instructions on prescription drug bottles, appointment slips, medical education brochures, doctor’s directions and consent forms, and the ability to negotiate complex health care systems. Low health literacy is found in many different health care settings (Williams et al. 1995; Gazmararian et al. 2003; Berkman et al. 2014) and is most common in older patients, those with lower education levels, immigrants, and racial minorities (Wilson 2003). According to the most recent national assessment of health literacy, 36% of American adults do not have the skills necessary to effectively manage their health and navigate the health care system (Powers et al. 2008). Studies that evaluated the relationship between health literacy and blood pressure control have shown that patients’ functional health literacy strongly correlated with knowledge of their illness (McNoughton et al. 2014) and that patients with hypertension and inadequate functional health literacy had higher systolic blood pressure readings than health-literate patients. Similarly, patients with diabetes and inadequate literacy had higher HbA1c levels (Williams et al. 1998; Friis et al. 2016).
The goal of this study was to examine the relationship between multiple health literacy assessments, preventive orientation and behaviors, and hypertension and diabetes among diverse, dental care–seeking individuals.
Methods
Study data were extracted from the Multi-Site Oral Health Literacy Research Study (MOHLRS), a 4-y National Institutes of Health (NIH)/National Institute of Dental and Craniofacial Research (NIDCR)–sponsored project that investigated the relationships between health literacy and oral health conducted among dental patients in California and Maryland. The study has been previously described and will be summarized here (Macek et al. 2016).
Questionnaire Development
The research team developed the questionnaire to accommodate a wide range of literacy levels and so that an individual’s ability to read would not prevent him or her from responding to non-literacy-type questions (e.g., patient characteristics, health behaviors), as was previously reported by our group (Macek et al. 2016). To accomplish this objective, the research team designed the consent forms and each section of the survey to be read aloud to participants. Survey instructions and transitional text were written in clear language, aiming toward a lower reading level. Response categories for selected items were reproduced onto Microsoft PowerPoint slides and loaded onto a tablet device. This approach allowed participants to see response choices at the same time interviewers read them aloud, eliminating the need for participants to recall a list of responses while answering questions. The entire survey took approximately 40 min to complete.
Study Recruitment and Data Collection
The target population included English-speaking, initial care-seeking, adult patients older than 18 y presenting to the screening, oral surgery, and urgent care clinics affiliated with schools of dentistry at the University of Maryland and the University of California Los Angeles (UCLA) (Macek et al. 2016). “Initial care-seeking” patients were defined as new patients or patients who had no more than 4 total visits to the respective clinic sites during the preceding 5 y because low-income adults may use dental school clinics episodically, for emergency care.
Participants were recruited from dental clinic waiting rooms by trained members of the research team. Individuals who expressed interest were handed a recruitment card with a telephone number so people could choose to participate immediately or to call to schedule data collection. Patients who did not speak English, who had notable vision and/or hearing disabilities, and who were trained or employed as nurses, physicians, or dental personnel were not eligible to participate. Before data collection commenced, written informed consent and permission to subsequently access the participant’s dental chart were obtained. Research methods were reviewed and approved by the institutional review boards at the University of Maryland, Baltimore and UCLA.
Answers to survey questions were entered into a secure, Internet-based electronic database (Qualtrics software program). Each participant was then given a printed folder containing dental education materials, answers to selected knowledge-based questions, and a copy of the consent form. Participants received a cash payment or a cash payment with parking voucher (value dependent on recruitment site).
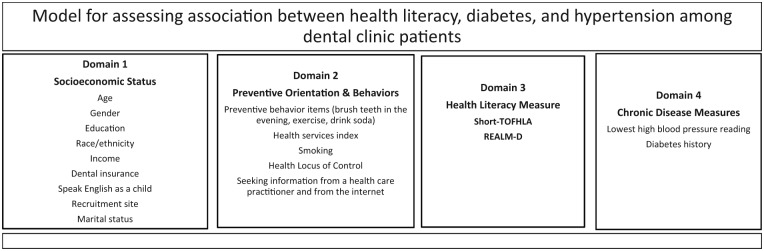
The Figure shows the conceptual model used as the framework for this analysis linking health literacy with hypertension and diabetes after accounting for sociodemographic factors and preventive orientation and behaviors. The model included 4 domains: SES covariates (domain 1), preventive orientation and behaviors (domain 2), health literacy (domain 3), and health measures (domain 4).
Figure.
Model for assessing association between health literacy, hypertension, and diabetes among dental clinic patients.
Sociodemographic covariates (domain 1)
This category included 9 variables: age, sex, race/ethnicity, education level, annual household income, language spoken now and language spoken as a child, marital status, dental insurance status, and the subject’s recruitment site.
Participants were asked to self-identify the following sociodemographics: their age, sex (male/female), race and ethnicity (non-Hispanic White, Hispanic, non-Hispanic Black, non-Hispanic Asian, and other/mixed race), whether they currently had dental insurance (yes/no), their marital status (married, living with partner, widowed, divorced, separated, never married), and their estimated annual household income ($0 to $11,000, $11,001 to $22,000, $22,001 to $33,000, $33,001 to $44,000, $44,001 to $55,000, and >$55,000). Participants identified their highest grade or year of completed school, which was then categorized as <12th grade, grade 12, some college, and college graduate. Subjects were asked what languages they speak and which language they spoke as a child. These items were combined as a proxy for acculturation to 4 categories (speaks multiple languages now/spoke English as a child, speaks only English now/spoke English as a child, speaks multiple languages now/spoke English and 1 or more other languages as a child, speaks multiple languages now/did not speak English as a child) (Marin et al. 1987).
Preventive orientation and behaviors (domain 2)
This domain reflected an individual’s orientation toward seeking preventive health information, preventive services, and adopting healthful activities. The subjects were asked how much information they sought about topics, such as diet, exercise, prevention, and specific health conditions, from health care professionals such as doctors, nurses, therapists, and psychologists and separately, from the Internet (1 = a lot, 2 = some, 3 = a little, or 4 = none). Preventive behaviors included the following three 3-point ordinal measures (2 = every day, 1 = sometimes, 0 = never): brush teeth in the evening, exercise, and drink soda. A preventive health services score was created by summing the following 3 binary items: got a flu shot, had a checkup from a medical doctor, and visited a dentist in the past year. The smoking information was obtained from the patient history as current, past, or never. Scoring for 4 preventive behavior items—seek information from health professionals, brush teeth in the evening, exercise, and drink soda—were reversed to go in a positive direction for the analysis.
Health locus of control (HLOC) refers to the belief that one has control over one’s health (such as being able to effect weight loss) rather than it being dependent upon external factors such as God’s will (Wallston et al. 1976). The HLOC summary score was obtained as the sum of six 5-point ordinal measures for assessing locus of control, where, after reversal, higher scores equaled less control. The questions included the following: people’s ill health results from their own carelessness; when I feel ill, I know it is because I have not been getting the proper exercise or eating right; no matter what I do, if I am going to get sick, I will get sick; good health is largely a matter of good fortune; I can only do what my doctor tells me to do; and whatever happens to my health is God’s will.
Health literacy and knowledge measures (domain 3)
Health literacy was measured using the short Test of Functional Health Literacy in Adults (Short-TOFHLA (Baker et al. 1999) and the Rapid Estimate of Adult Literacy in Medicine and Dentistry (REALM-D) (Atchison et al. 2010). The Short-TOFHLA is a 36-item health literacy instrument that tests an individual’s ability to use reading context to replace selected missing words from 2 medical intake forms. Participants replaced blanks with multiple-choice options of medical and health terms. The final score was determined by summing the number of correctly filled in blanks out of 36 and was calculated manually and then entered into the database. The REALM-D is an 84-item dental/medical health literacy word recognition instrument, in which the final score is a summation of words pronounced correctly.
Objective measures (domain 4)
The signed informed consent included the information that the research team would access his or her electronic dental record for a period of up to 2 y beyond the initial interview to collect information. The primary outcomes of interest were hypertension, or uncontrolled blood pressure, and a reported history of diabetes. Uncontrolled blood pressure (hypertension) was defined as 140/90 mm Hg (Go et al. 2014). Blood pressure measurements were extracted from patients’ dental electronic record, where they had been recorded by the patients’ treating dental student(s) in the dental clinic. If the first blood pressure measurement was high, additional measurements were taken and the lowest blood pressure measurement was recorded. These values were obtained manually by the dental student, using an appropriate-sized cuff while the patient was seated. Diabetes was self-reported by the patients and recorded in their dental record as diabetes type I or II; the majority of diabetes reported was type II.
Data Management
Survey responses and chart review data were merged into an analytical file with a unique identifier assigned to each respondent. Once survey and chart data were combined, all personal identifying information was removed from the analytical file to maintain participant anonymity. The SAS statistical software program for Windows (SAS Institute) was used to code variables, clean data, and conduct the analyses in this report.
Statistical Methods
Bivariate analyses
Short-TOFHLA and REALM-D scores were compared by each demographic variable and by smoking status using the Kruskal-Wallis test. The correlations between Short-TOFHLA and the REALM-D score versus other preventive measures were assessed using the Spearman method.
Multivariable analyses
The relationship between the health literacy outcomes (Short-TOFHLA and REALM-D) versus diabetes or hypertension (predictors) was evaluated nonparametrically using linear regression models with bootstrapping before and after adjusting for covariates. Regression model 1 then adjusted for the demographic variables (domain 1). The demographic variables considered were age, sex, education, race/ethnicity, income, dental insurance, did not speak English as child, and marital status. Site of recruitment was eliminated from the model to concentrate our interest on specific patient characteristics. Regression model 2 adjusted for demographics and the prevention orientation and behavior variables. These included seeking information about health by talking to health professionals and on the Internet; smoking; daily preventive activities of brushing teeth in evening, exercise, and drinking soda; the preventive health services score; and locus of control score (domain 2). Missing values for the covariates were singly imputed using regression imputation for the purpose of the multivariable analyses.
The models allowed for the relationship between each health literacy score versus diabetes or hypertension to vary by education, marital status, and acculturation (speak English as a child) by including the appropriate interaction terms to the above models (effect modification). Final models were selected using the backward procedure for variable selection and liberal P < 0.15 cutoff as the retention criterion since this was an exploratory study and we did not wish to miss any potentially important variables and/or risk biasing the results by excluding any potentially important variables from the models (Bendel and Afifi 1977). Interaction effects were considered significant if P < 0.10.
Results
After removal of 104 subjects who were excluded from the analysis due to missing values for diabetes and hypertension, and an additional 26 subjects were excluded due to missing Short-TOFHLA scores analysis was conducted on 793 subjects.
Table 1 presents the Short-TOFHLA and the REALM-D scores in relation to patient demographics. Results for the Short-TOFHLA show variation in scores across the age groups, with younger people having higher scores than older people (P = 0.00). More educated persons had higher scores compared to those subjects who reported less than a 12th-grade education (mean, 35 for college graduate vs. mean 30 for <12th-grade education; P = 0.00). With regard to ethnicity, Short-TOFHLA scores were highest for non-Hispanic (NH) Asians (mean, 35.1), followed by NH Whites (mean, 33.8), NH Blacks (mean, 32.1), other ethnic groups (mean, 31.8). and Hispanics (mean, 31.6; P = 0.000). For the REALM-D, people who were other or NH White (both with a mean score of 79.5) demonstrated the highest scores, whereas Hispanics had the lowest scores (mean, 75.9; P < 0.001). People with the highest reported income (P = 0.00) and who spoke English as a child (P = 0.00) had the highest mean health literacy scores. Both health literacy scores showed significant differences for the place of recruitment.
Table 1.
Short-TOFHLA and REALM-D Scores in Relation to Patient Demographics (n = 793 Subjects).
| Short-TOFHLA |
REALM-D |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Range | Median | Mean | P Value | n | Range | Median | Mean | P Value | |
| Age, y | ||||||||||
| Unknown | 6 | 24–36 | 29.5 | 30.2 | 0.00 | 6 | 29–80 | 77.5 | 69.7 | 0.78 |
| 18–24 | 65 | 24–36 | 35.0 | 34.5 | 65 | 38–84 | 81.0 | 77.4 | ||
| 25–44 | 280 | 10–36 | 35.0 | 33.9 | 288 | 14–84 | 81.0 | 78.7 | ||
| 45–64 | 345 | 0–36 | 34.0 | 32.1 | 359 | 0–84 | 81.0 | 77.6 | ||
| 65+ | 97 | 9–36 | 34.0 | 30.3 | 100 | 31–84 | 81.0 | 78.4 | ||
| Sex | ||||||||||
| Unknown | 2 | 35–36 | 35.5 | 35.5 | 0.26 | 3 | 80–84 | 82.0 | 82.0 | 0.50 |
| Male | 397 | 0–36 | 35.0 | 32.3 | 409 | 0–84 | 81.0 | 77.8 | ||
| Female | 394 | 9–36 | 35.0 | 33.1 | 406 | 14–84 | 81.0 | 78.2 | ||
| Education | ||||||||||
| Unknown | 6 | 14–36 | 35.5 | 31.5 | 0.00 | 6 | 72–84 | 80.5 | 79.2 | 0.00 |
| Less than grade 12 | 63 | 6–36 | 33.0 | 30.0 | 66 | 14–84 | 78.0 | 73.7 | ||
| Grade 12 | 212 | 0–36 | 34.0 | 31.5 | 215 | 0–84 | 79.0 | 76.6 | ||
| Some college | 239 | 7–36 | 35.0 | 33.1 | 243 | 29–84 | 81.0 | 78.1 | ||
| College graduate | 273 | 9–36 | 35.0 | 34.0 | 288 | 22–84 | 82.0 | 79.9 | ||
| Race/ethnicity | ||||||||||
| Hispanic | 100 | 6–36 | 34.0 | 31.6 | 0.00 | 102 | 27–84 | 79.0 | 75.9 | 0.00 |
| NH Black | 312 | 0–36 | 34.0 | 32.1 | 318 | 14–84 | 80.0 | 77.0 | ||
| NH Asian | 27 | 31–36 | 35.0 | 35.1 | 30 | 48–84 | 81.0 | 77.2 | ||
| Other | 56 | 5–36 | 34.0 | 31.8 | 58 | 65–84 | 81.0 | 79.5 | ||
| NH White | 298 | 9–36 | 35.0 | 33.8 | 310 | 0–84 | 82.0 | 79.5 | ||
| Income | ||||||||||
| $0–$11,000 | 116 | 14–36 | 35.0 | 32.8 | 0.01 | 121 | 14–84 | 79.0 | 75.6 | 0.00 |
| $11,001–$22,000 | 136 | 12–36 | 35.0 | 33.0 | 141 | 38–84 | 80.0 | 77.5 | ||
| $22,001–$33,000 | 132 | 0–36 | 34.0 | 31.7 | 137 | 40–84 | 81.0 | 78.8 | ||
| $33,001–$44,000 | 101 | 6–36 | 35.0 | 32.5 | 104 | 29–84 | 81.0 | 78.0 | ||
| $44,001–$55,000 | 65 | 9–36 | 35.0 | 32.6 | 66 | 49–84 | 80.0 | 78.3 | ||
| >$55,000 | 149 | 5–36 | 35.0 | 33.9 | 154 | 56–84 | 81.5 | 79.8 | ||
| Unknown | 94 | 6–36 | 34.5 | 32.2 | 95 | 0–84 | 81.0 | 77.7 | ||
| Have dental insurance | ||||||||||
| Unknown | 4 | 14–36 | 33.0 | 28.8 | 0.52 | 4 | 70–84 | 75.5 | 75.0 | 0.30 |
| No | 483 | 0–36 | 35.0 | 32.7 | 494 | 0–84 | 81.0 | 78.1 | ||
| Yes | 306 | 5–36 | 35.0 | 32.8 | 320 | 14–84 | 81.0 | 77.9 | ||
| Multiple languages spoken now/language spoken as child | ||||||||||
| Unknown | 7 | 14–36 | 32.0 | 29.9 | 0.00 | 7 | 72–84 | 81.0 | 80.1 | 0.00 |
| No/English only | 530 | 0–36 | 35.0 | 32.7 | 549 | 14–84 | 81.0 | 78.4 | ||
| Yes/English only | 92 | 28–36 | 35.0 | 34.6 | 94 | 22–84 | 81.0 | 79.4 | ||
| Yes/English and other | 71 | 15–36 | 35.0 | 33.6 | 72 | 58–84 | 81.0 | 78.6 | ||
| Yes/other than English | 93 | 6–36 | 34.0 | 30.8 | 96 | 0–84 | 78.0 | 73.7 | ||
| State | ||||||||||
| Maryland | 434 | 0–36 | 35.0 | 32.3 | 0.00 | 442 | 14–84 | 81.0 | 78.2 | 0.00 |
| California | 359 | 6–36 | 35.0 | 33.2 | 376 | 0–84 | 80.0 | 77.7 | ||
| Marital status | ||||||||||
| Unknown | 6 | 14–36 | 35.0 | 31.5 | 0.00 | 6 | 72–84 | 80.0 | 79.0 | 0.50 |
| Married | 178 | 0–36 | 35.0 | 31.7 | 182 | 0–84 | 80.0 | 77.2 | ||
| Living with partner | 106 | 5–36 | 35.0 | 32.9 | 109 | 31–84 | 81.0 | 78.0 | ||
| Widowed | 28 | 16–36 | 33.0 | 31.3 | 30 | 53–84 | 78.5 | 77.1 | ||
| Divorced | 122 | 7–36 | 34.5 | 32.5 | 126 | 27–84 | 81.0 | 78.0 | ||
| Separated | 42 | 14–36 | 35.0 | 32.5 | 43 | 60–84 | 81.0 | 79.0 | ||
| Never married | 311 | 8–36 | 35.0 | 33.5 | 322 | 14–84 | 81.0 | 78.4 | ||
Statistically significant associations (P < 0.05) are listed in bold.
NH, non-Hispanic; REALM-D, Rapid Estimate of Adult Literacy in Medicine and Dentistry; Short-TOFHLA, short Test of Functional Health Literacy in Adults.
Comparing the results for the 2 health literacy measures, for the Short-TOFHLA, people who were recruited to participate in California (mean, 33.2; P = 0.00) had higher scores, while for the REALM-D, people from Maryland had higher scores (mean, 78.2; P = 0.00). Two other variables demonstrated significant differences for the Short-TOFHLA, with an increasing score from oldest (mean, 30.3 points) to people 18 to 24 y of age (34.5 points; P = 0.00), and those who were never married (mean, 33.5; P = 0.00) had the highest Short-TOFHLA scores, but these variables were not associated with the REALM-D. Moving forward to the multivariate regression, the 3 categories in which people spoke English as a child were combined and compared to people who did not speak English as a child.
Table 2 shows that Short-TOFHA scores were associated with seeking health information on the Internet, the preventive health services score, and the HLOC score. Scores for people who reported no use of the Internet to find health information and lower preventive health services scores (having a flu shot, seeing a medical doctor for a checkup, and seeing the dentist within the past year) were associated with having lower Short-TOFHLA scores (P = 0.00). A higher HLOC score, meaning the individual feels she or he has less control over one’s actions, was associated with lower Short-TOFHLA scores (P = 0.01). Similarly, lower REALM-D scores were associated with no seeking of health information on the Internet and a higher (meaning less control) HLOC score.
Table 2.
REALM-D and Short-TOFHLA by Preventive Measures.
| Short-TOFHLA |
REALM-D |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | n | Range | Median | Mean | P Value | n | Range | Median | Mean | P Value |
| Smoking | ||||||||||
| Current | 187 | 10–36 | 35.0 | 33.0 | 0.38 | 194 | 31–84 | 80.5 | 77.9 | 0.20 |
| Former | 96 | 6–36 | 35.0 | 32.2 | 100 | 22–84 | 81.0 | 79.0 | ||
| Never | 510 | 0–36 | 35.0 | 32.8 | 524 | 0–84 | 81.0 | 77.9 | ||
| Seek information from health professionals | ||||||||||
| Missing | 60 | 14–36 | 35.0 | 32.8 | 0.40 | 60 | 48–84 | 80.0 | 77.3 | 0.64 |
| A lot | 282 | 8–36 | 35.0 | 33.0 | 292 | 0–84 | 81.0 | 77.6 | ||
| Some | 307 | 5–36 | 35.0 | 33.1 | 318 | 27–84 | 81.0 | 79.2 | ||
| A little | 114 | 0–36 | 35.0 | 32.0 | 118 | 31–84 | 80.0 | 77.0 | ||
| None | 30 | 6–36 | 34.0 | 29.4 | 30 | 40–84 | 79.0 | 75.0 | ||
| Seek information from the Internet | ||||||||||
| Missing | 52 | 14–36 | 35.0 | 32.4 | 0.01 | 52 | 48–84 | 80.0 | 77.2 | 0.01 |
| A lot | 392 | 5–36 | 35.0 | 33.4 | 406 | 14–84 | 81.0 | 78.5 | ||
| Some | 188 | 6–36 | 35.0 | 33.4 | 195 | 22–84 | 81.0 | 79.0 | ||
| A little | 71 | 0–36 | 35.0 | 32.0 | 74 | 40–84 | 81.0 | 78.0 | ||
| None | 90 | 6–36 | 33.0 | 29.3 | 91 | 0–84 | 78.0 | 74.1 | ||
| Brush teeth in the evening | ||||||||||
| Missing | 54 | 14–36 | 35.0 | 32.6 | 0.57 | 54 | 48–84 | 80.0 | 77.5 | 0.69 |
| Never | 66 | 5–36 | 34.0 | 31.6 | 69 | 31–84 | 80.0 | 75.5 | ||
| Sometimes | 309 | 0–36 | 35.0 | 33.0 | 318 | 0–84 | 81.0 | 78.3 | ||
| Every day | 364 | 6–36 | 35.0 | 32.75 | 377 | 14–84 | 81.0 | 78.3 | ||
| Exercise | ||||||||||
| Missing | 49 | 14–36 | 35.0 | 32.45 | 0.83 | 49 | 48–84 | 79.0 | 76.9 | 0.62 |
| Never | 61 | 17–36 | 34.0 | 32.7 | 63 | 27–84 | 81.0 | 76.8 | ||
| Sometimes | 416 | 5–36 | 35.0 | 33.0 | 432 | 0–84 | 81.0 | 78.2 | ||
| Every day | 267 | 0–36 | 35.0 | 32.35 | 274 | 14–84 | 81.0 | 78.1 | ||
| Drink soda | ||||||||||
| Missing | 51 | 14–36 | 35.0 | 32.55 | 0.86 | 51 | 48–84 | 79.0 | 76.8 | 0.22 |
| Every day | 112 | 16–36 | 34.5 | 32.8 | 119 | 31–84 | 81.0 | 78.1 | ||
| Sometimes | 384 | 0–36 | 35.0 | 32.9 | 392 | 22–84 | 81.0 | 78.3 | ||
| Never | 246 | 9–36 | 35.0 | 32.5 | 256 | 0–84 | 81.0 | 77.7 | ||
| Preventive health services (higher is better) | ||||||||||
| Missing | 3 | 32–35 | 33.0 | 33.3 | 0.00 | 3 | 77–84 | 82.0 | 80.7 | 0.85 |
| 0 | 118 | 14–36 | 35.0 | 33.8 | 122 | 0–84 | 81.0 | 78.5 | ||
| 1 | 225 | 0–36 | 35.0 | 32.6 | 232 | 22–84 | 81.0 | 78.2 | ||
| 2 | 279 | 6–36 | 35.0 | 32.6 | 286 | 14–84 | 80.0 | 77.2 | ||
| 3 | 168 | 5–36 | 34.5 | 32.4 | 175 | 40–84 | 81.0 | 78.7 | ||
| Locus of control (higher score is less control) | ||||||||||
| Missing | 3 | 32–35 | 33.0 | 33.3 | 0.01 | 3 | 77–84 | 82.0 | 80.7 | 0.01 |
| Quartile 1 | 118 | 14–36 | 35.0 | 33.8 | 122 | 0–84 | 81.0 | 78.5 | ||
| Quartile 2 | 225 | 0–36 | 35.0 | 32.6 | 232 | 22–84 | 81.0 | 78.2 | ||
| Quartile 3 | 279 | 6–36 | 35.0 | 32.6 | 286 | 14–84 | 80.0 | 77.2 | ||
| Quartile 4 | 168 | 5–36 | 34.5 | 32.4 | 175 | 40–84 | 81.0 | 78.7 | ||
Statistically significant associations (P < 0.05) are listed in bold.
REALM-D, Rapid Estimate of Adult Literacy in Medicine and Dentistry; Short-TOFHLA, short Test of Functional Health Literacy in Adults.
Table 3 shows the regression models between Short-TOFHLA and diabetes and hypertension. The variables for income, dental insurance, marital status and brushing in the evening, exercising, and drinking soda were not significant at P < 0.15 and were excluded from the final models. In unadjusted analysis, patients who reported having diabetes had a Short-TOFHLA score of 31.43 compared to 32.89 for those who did not report having diabetes (mean change, –1.46; P = 0.03). The relationship between diabetes and the Short-TOFHLA was greatly diminished and was no longer statistically significant after the adjustment for demographic factors. There was no evidence that the relationship between Short-TOFHLA and diabetes significantly differed by education, marital status, or language spoken as child (not shown). The final multivariable model for diabetes, including both demographic and preventive orientation and behavior variables, indicated 10 significant predictors of the Short-TOFHLA scores. Women had higher Short-TOFHLA scores compared to men by an average of about 1 point after controlling for the other covariates (mean change, 0.93; P = 0.01). People with more years of schooling had higher scores compared to less educated persons controlling for other covariates. For example, people with some college and college graduates had scores that were greater by 2.56 and 3.50 points on average, respectively, compared to those who had less than high school education with P < 0.001 in the adjusted analysis. With regard to ethnicity, Short-TOFHLA scores were highest for Asians, and scores from both Asians (by 2.36 points) and NH Whites (by 1.39 points) were significantly higher than the reference group of NH Blacks after controlling for the other factors. Older individuals had lower scores compared to younger individuals. For example, persons who were 65 y or older had scores that were smaller by over 4 points on average, and those aged 45 to 64 y scored less by 2.37 points compared to persons who were aged 18 to 24 y with P < 0.01 in the adjusted analysis. Persons who did not speak English as a child had smaller scores by about 3 points on average compared to native English speakers with P < 0.01 in the adjusted analysis.
Table 3.
Multivariable Regression Models for Short-TOFHLA.
| Diabetes |
Hypertension |
|||||||
|---|---|---|---|---|---|---|---|---|
| Mean Change | Lower CL | Upper CL | P Value | Mean Change | Lower CL | Upper CL | P Value | |
| Unadjusted | ||||||||
| Yes vs. no | −1.46 | −2.76 | −0.16 | 0.03 | −1.28 | −2.23 | −0.34 | 0.01 |
| Adjusted model 1a | ||||||||
| Yes vs. no | −0.11 | −1.39 | 1.18 | 0.87 | 0.23 | −0.71 | 1.17 | 0.62 |
| Adjusted model 2b | ||||||||
| Yes vs. no | 0.13 | −1.15 | 1.41 | 0.84 | 0.44 | −0.52 | 1.40 | 0.37 |
| Female vs. male | 0.93 | 0.25 | 1.61 | 0.01 | 0.92 | 0.19 | 1.65 | 0.01 |
| Education | ||||||||
| <12th grade | Reference | Reference | ||||||
| Grade 12 | 1.07 | −0.54 | 2.69 | 0.19 | 1.05 | −0.45 | 2.55 | 0.17 |
| Some college | 2.56 | 1.07 | 4.06 | 0.00 | 2.55 | 1.03 | 4.08 | 0.00 |
| College graduate | 3.50 | 1.93 | 5.08 | 0.00 | 3.51 | 1.98 | 5.04 | 0.00 |
| Race/ethnicity | ||||||||
| NH Black | Reference | Reference | ||||||
| Hispanic | 0.38 | −0.98 | 1.74 | 0.59 | 0.41 | −0.94 | 1.76 | 0.55 |
| NH Asian | 2.36 | 1.17 | 3.56 | 0.00 | 2.36 | 1.17 | 3.55 | 0.00 |
| Other | −0.94 | −2.63 | 0.75 | 0.28 | −0.93 | −2.63 | 0.78 | 0.29 |
| NH White | 1.36 | 0.56 | 2.16 | 0.00 | 1.39 | 0.59 | 2.19 | 0.00 |
| Age, y | ||||||||
| 18–24 | Reference | Reference | ||||||
| 25–44 | −0.51 | −1.36 | 0.34 | 0.24 | 0.52 | −1.39 | 0.34 | 0.24 |
| 45–64 | −2.37 | −3.36 | −1.37 | 0.00 | 2.49 | −3.51 | −1.47 | 0.00 |
| 65+ | −4.20 | −5.71 | −2.69 | 0.00 | 4.39 | −5.97 | −2.81 | 0.00 |
| Language spoken as child | ||||||||
| Not English | −3.02 | −4.32 | −1.72 | 0.00 | −3.00 | −4.31 | −1.70 | 0.00 |
| Seek health information on Internet | ||||||||
| A lot | Reference | Reference | ||||||
| Some | 0.41 | −0.35 | 1.18 | 0.29 | 0.43 | −0.29 | 1.15 | 0.24 |
| A little | −0.63 | −2.13 | 0.87 | 0.41 | −0.68 | −2.29 | 0.94 | 0.41 |
| None | −1.53 | −3.02 | −0.04 | 0.04 | −1.56 | −3.08 | −0.05 | 0.04 |
| Speak to health care professionals | ||||||||
| A lot | Reference | Reference | ||||||
| Some | −0.16 | −0.91 | 0.59 | 0.68 | −0.14 | −0.84 | 0.55 | 0.69 |
| A little | −1.36 | −2.46 | −0.26 | 0.02 | −1.33 | −2.42 | −0.24 | 0.02 |
| None | −2.76 | −5.45 | −0.06 | 0.05 | −2.68 | −5.26 | −0.09 | 0.04 |
| Smoking | ||||||||
| Current | Reference | Reference | ||||||
| Former | −1.42 | −2.84 | 0.00 | 0.05 | −1.46 | −2.92 | 0.00 | 0.05 |
| Never | −0.96 | −1.76 | −0.15 | 0.02 | −0.97 | −1.78 | −0.16 | 12.76 |
| Preventive health service score (higher is better) | ||||||||
| 0 points | Reference | Reference | ||||||
| 1 point | −1.29 | −2.25 | −0.33 | 0.01 | −1.30 | −2.28 | −0.32 | 0.01 |
| 2 points | −1.12 | −2.12 | −0.13 | 0.03 | −1.14 | −2.09 | −0.18 | 0.02 |
| 3 points | −1.37 | −2.52 | −0.21 | 0.02 | −1.39 | −2.55 | −0.24 | 0.02 |
| Health locus of control (higher score is less control) | ||||||||
| Quartile 1 | Reference | Reference | ||||||
| Quartile 2 | −0.70 | −1.51 | 0.11 | 0.09 | −0.71 | −1.59 | 0.16 | 0.11 |
| Quartile 3 | −0.05 | −0.99 | 0.88 | 0.91 | −0.06 | −0.96 | 0.84 | 0.90 |
| Quartile 4 | −1.18 | −2.18 | −0.19 | 0.02 | −1.22 | −2.20 | −0.24 | 0.02 |
Statistically significant associations (P < 0.05) are listed in bold.
CL, confidence limit; NH, non-Hispanic; Short-TOFHLA, short Test of Functional Health Literacy in Adults.
Model 1 adjusted for demographic variables only.
Model 2 adjusted for demographic variables and preventive variables.
With respect to the preventive orientation and behavior variables, individuals who never sought health information from the Internet had scores that were smaller by 1.5 points on average with P = 0.04, and those who reported never talking (–2.76, P = 0.05) or talking only a little to health care professionals had lower Short-TOFHLA scores (by 1.36 points; P = 0.02) compared to those who reported talking a lot after controlling for the other factors. Both never smokers and former smokers had lower health literacy scores (by 0.96 points [P = 0.02] and 1.42 points [P = 0.05], respectively) compared to current smokers. Patients with higher (better) total preventive health services scores had smaller Short-TOFHLA scores on average after adjusting for the other factors. For example, patients who reported having all 3 services (a flu shot, a doctor checkup, and a visit to the dentist within a year) had lower Short-TOFHLA scores by an average of about 1.37 points compared to those who reported none of the above factors with P = 0.02 in the adjusted analysis. Individuals who reported having HLOC scores and who felt they had less control over their health had lower health literacy scores on average compared to the reference group in quartile 1 control (mean change, –1.18 from first to last quartile; P = 0.02) after adjusting for the covariates.
In unadjusted analysis, patients who reported having hypertension had a mean Short-TOFHLA score of 31.80 compared to 33.09 for those who did not report having hypertension in the unadjusted analysis (mean change, –1.28; P = 0.01). The relationship between hypertension and the Short-TOFHLA was greatly diminished and was no longer statistically significant after the adjustment for demographic factors. There was no evidence that the relationship between Short-TOFHLA and hypertension significantly differed by education, marital status, or language spoken as child (not shown). Other significant sociodemographic and preventive variables were the same as for diabetes, with people who were female, having some college or being a college graduate, being Asian or NH White, being younger in age, having spoken English as a child, seeking a lot or some health information from the Internet, speaking a lot to health care professionals, smoking, having fewer or no preventive health services, and reporting they have more control over their health having higher Short-TOFHLA scores.
Table 4 shows the regression models between REALM-D scores and diabetes and hypertension. There were no significant differences in mean REALM-D scores between patients who had hypertension or diabetes versus not having the condition. The variables for income, dental insurance, marital status, brushing in the evening, exercising, and drinking soda were not significant at P < 0.15 and were excluded from the final models. The diabetes model for the REALM-D scores showed that people with higher REALM-D scores had some college (3.40 points with P = 0.04 vs. <12th grade) or were a college graduate (mean change, 5.17 points; P = 0.00 vs. <12th grade). With regard to ethnicity, REALM-D scores for both other race/ethnicity (by 2.39 points with P = 0.01) and NH Whites (by 2.03 points with P = 0.00) were significantly higher than the reference group of NH Blacks after controlling for the other factors. Those who did not speak English as a child had lower REALM-D scores (mean change, –5.67; P = 0.00). Those who sought no health information via the Internet had lower REALM-D scores (mean change, –3.23; P = 0.01).
Table 4.
Multivariable Models for REALM-D.
| Diabetes |
Hypertension |
|||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted |
Unadjusted |
|||||||
| Mean Change | Lower CL | Upper CL | P Value | Mean Change | Lower CL | Upper CL | P Value | |
| Yes vs. no | −0.45 | −2.15 | 1.25 | 0.60 | 0.16 | −1.22 | 1.53 | 0.82 |
| Adjusted Model 1a | Adjusted Model 1a | |||||||
| Mean Change | Lower CL | Upper CL | P Value | Mean Change | Lower CL | Upper CL | P Value | |
| Yes vs. no | −0.60 | −2.21 | 1.00 | 0.46 | 0.33 | −0.91 | 1.58 | 0.60 |
| Adjusted Model 2b | Adjusted Model 2b | |||||||
| Mean Change | Lower CL | Upper CL | P Value | Mean Change | Lower CL | Upper CL | P Value | |
| Yes vs. no | −0.15 | −1.81 | 1.51 | 0.86 | 0.73 | −0.55 | 2.01 | 0.26 |
| Education | ||||||||
| <12th grade | Reference | Reference | ||||||
| Grade 12 | 2.11 | −1.48 | 5.70 | 0.25 | 2.03 | −1.47 | 5.54 | 0.26 |
| Some college | 3.40 | 0.13 | 6.67 | 0.04 | 3.35 | −0.01 | 6.71 | 0.05 |
| College graduate | 5.17 | 1.97 | 8.38 | 0.00 | 5.11 | 1.84 | 8.39 | 0.00 |
| Race/ethnicity | ||||||||
| NH Black | Reference | Reference | ||||||
| Hispanic | 0.70 | −1.62 | 3.02 | 0.56 | 0.78 | −1.54 | 3.11 | 0.51 |
| NH Asian | 0.53 | −2.33 | 3.39 | 0.72 | 0.64 | −2.24 | 3.53 | 0.66 |
| Other | 2.32 | 0.61 | 4.04 | 0.01 | 2.39 | 0.66 | 4.12 | 0.01 |
| NH White | 1.95 | 0.58 | 3.32 | 0.01 | 1.25 | 0.69 | 3.38 | 0.00 |
| Language spoken as child | ||||||||
| Not English | −5.67 | −8.28 | −3.06 | 0.00 | −5.63 | −8.16 | −3.10 | 0.00 |
| Seek health information from Internet | ||||||||
| A lot | Reference | Reference | ||||||
| Some | 0.25 | −1.13 | 1.63 | 0.72 | 0.22 | −1.06 | 1.50 | 0.74 |
| A little | −0.51 | −2.46 | 1.45 | 0.61 | −0.64 | −2.75 | 1.46 | 0.55 |
| None | −3.23 | −5.76 | −0.70 | 0.01 | −3.44 | −5.93 | −0.95 | 0.01 |
Statistically significant associations (P < 0.05) are listed in bold.
CL, confidence limit; NH, non-Hispanic; REALM-D, Rapid Estimate of Adult Literacy in Medicine and Dentistry.
Model 1 adjusted for demographic variables only.
Model 2 also adjusted for preventive variables.
The hypertension model for the REALM-D scores was almost identical, with people with higher REALM-D scores among those who had some college (3.35 points, P = 0.05, vs. <12th grade) or were a college graduate (mean change, 5.11 points, P = 0.01, vs. <12th grade). Both other race/ethnicity (mean change, 2.39; P = 0.01) and NH Whites (mean change, 2.03; P = 0.00) had significantly higher REALM-D scores (P < 0.01) compared to NH Blacks. Those who did not speak English as a child had lower REALM-D scores (mean change, –5.63; P = 0.00). Those who sought no health information via the Internet had lower REALM-D scores (mean change, –3.44; P = 0.01).
Discussion
This study confirmed existing information and added new information on characteristics associated with health literacy. It highlighted new information on health associations with health literacy and highlighted differences between health literacy measures.
Two systematic reviews regarding health literacy and health outcomes provide relevant comparison to this study. Berkman et al. (2011) examined the evidence of an association between low (compared to adequate) health literacy and over 30 outcomes. There were 3 relevant health outcomes and 4 relevant prevention-related outcomes. The 3 health outcomes were prevalence of chronic disease, diabetes control and complications, and hypertension control. In 3 health outcomes cases, they found there was insufficient evidence to confirm an association between health literacy because of inconsistent results. In this study, the Short-TOFHLA scores for 2 health measures, diabetes and hypertension, were significantly different in unadjusted analysis but became nonsignificant after controlling for multiple demographic variables. The study also confirmed the previous findings that there could be no association found between a health literacy measure, in this case the REALM-D scores, and those who had diabetes or hypertension and those who did not.
We focused on patients with hypertension and diabetes, because in addition to being prevalent, these chronic diseases require daily attention to self-care and have standard markers of disease control (levels of HbA1c and blood pressure). Both are chronic diseases characterized by a high level of complexity that requires extensive self-care management, including translation of guidelines into everyday life (Friis et al. 2016). In addition, uncontrolled diabetes has been associated with periodontal disease progression (Casanova et al. 2014). The demands for people with these diseases are complicated because self-care of a chronic disease often relies on information in printed educational materials, verbal instructions, and patient education courses. Having adequate health literacy is critical for patients for managing their condition and navigating the health care environment. The inconsistent findings, between a health literacy measure (Short-TOFHLA) and an oral health literacy measure (REALM-D), emphasize the need for controlled studies to use multiple measures of health literacy and to try to identify the specific type of health literacy measure that would be most effective in assessing not only disease status but also elements of patient nonunderstanding that could preclude the patient from being able to manage chronic conditions.
Regarding the association between health literacy and preventive factors, the systematic review by Berkman et al. (2011) reported there were 4 preventive outcomes: seeking health-related information, healthy lifestyle behaviors, influenza immunization, and smoking. Regarding the seeking of health information, they reported no difference, and they rated the evidence as low. For the healthy lifestyle, there were 5 cross-sectional studies, and the association with low health literacy was inconsistent. Four studies provided moderate evidence of an association between low health literacy and lower likelihood of influenza immunizations. Two cross-sectional studies tested the association of smoking with low health literacy, and the findings were inconsistent. A review of health literacy and diabetic health outcomes among diabetic patients (Al Sayah et al. 2013) reviewed 4 cross-sectional studies not included in the Berkman review and found moderate evidence of no association between health literacy and self-care behaviors (diet, exercise, blood sugar testing, foot care, smoking cessation, and medication adherence). They stated that they rated it as moderate evidence because the study adequately controlled for confounders and the results were consistent. Our study also found inconsistent findings between health literacy measures but not across disease entities. Both the Short-TOFHLA and the REALM-D identified seeking health information from the Internet, as well as other patient sociodemographic variables. However, the Short-TOFHLA also identified seeking health information from health care professionals, smoking, seeking fewer preventive health services (an intriguing observation), and HLOC as additional findings to consider for the future. Thus, although the finding of having a chronic disease did not matter with respect to health literacy scores, the use of a comprehensive model did expand our knowledge on associations with preventive behaviors such as seeking health information from health professionals or from the Internet, use of preventive health services, and one’s orientation toward behavior—the HLOC.
The study has limitations. First, this is a cross-sectional study, and the sample was derived from university-based dental clinic patients, that is, people who chose to seek dental care and sought care in a school-based clinic. These individuals may have had specific dental problems that drove them to the dentist; thus, our results are not generalizable to the general public. Second, people who choose a dental school may be different from the general population of people who seek dental care. Our sample also included relatively few individuals with less than a high school level of education. Those with low levels of education are expected to face the greatest health literacy challenges within the health care system, and their data would have been most informative. A large number of health histories had missing data on diabetes and high blood pressure. Finally, we did not differentiate participants based on their reason for visiting the dental clinic (e.g., for a dental emergency or for routine care). It is likely that patients who presented for acute care may have been different from those who presented for routine preventive dental services.
There are also strengths to the study. The sample included a diverse sample from 2 large US cities in different parts of the country using the identical methodology. A robust set of covariates was included in the multivariate analysis to adequately control for the consistent association found between health literacy and sociodemographic factors. Lack of health literacy may lead to multiple strains on the health care system as well as for patients, including medication errors, missed appointments, adverse medical outcomes, and lower patient satisfaction. The future of patient education requires ingenuity and commitment of necessary resources to improve outcomes for low-literate patients with chronic diseases.
Author Contributions
D.V. Messadi, contributed to conception, design, and data interpretation, drafted and critically revised the manuscript, M.D. Macek, contributed to design, data acquisition, and analysis, critically revised the manuscript, D. Markovic, contributed to conception, data analysis, and interpretation, critically revised the manuscript, K.A. Atchison, contributed to conception, design, data analysis, and interpretation, drafted and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Acknowledgments
We would like to acknowledge the valuable contribution of Dr. Jennifer Holtzman, Leslie Hanson, and Jessica Richards.
Footnotes
This project was funded by the National Institute of Dental and Craniofacial Research (R01 DE020858).
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Al Sayah F, Majumdar SR, Williams B, Robertson S, Johnson JA. 2013. Health literacy and health outcomes in diabetes: a systematic review. J Gen Intern Med. 28(3):444–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atchison KA, Gironda MW, Messadi D, Der-Martirosian C. 2010. Screening for oral health literacy in an urban dental clinic. J Public Health Dent. 70(4):269–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. 1999. Development of a brief test to measure health literacy. Patient Educ Couns. 38(1):33–42. [DOI] [PubMed] [Google Scholar]
- Bailey SC, Brega AG, Crutchfield TM, Elasy T, Herr H, Kaphingst K, Karter AJ, Moreland-Russell S, Osborn CY, Pignone M, et al. 2014. Update on health literacy and diabetes. Diabetes Educ. 40(5):581–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendel RB, Afifi AA. 1977. Comparison of stopping rule in forward stepwise regression. J Am Stat Assoc. 72(357):46–53. [Google Scholar]
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. 2011. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 155(2):97–107. [DOI] [PubMed] [Google Scholar]
- Casanova L, Hughes FJ, Preshaw PM. 2014. Diabetes and periodontal disease: a two-way relationship. Br Dental J. 217(8):433–437. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Learn about health literacy. 2016. https://www.cdc.gov/healthliteracy/index.html
- Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017. Atlanta (GA): Centers for Disease Control and Prevention, US Department of Health and Human Services. [Google Scholar]
- Eyüboğlu E, Schulz PJ. 2016. Do health literacy and patient empowerment affect self-care behaviour? A survey study among Turkish patients with diabetes. BMJ Open. 6(3):e010186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friis K, Vind BD, Simmons RK, Maindal HT. 2016. The relationship between health literacy and health behaviour in people with diabetes: a Danish population-based study. J Diabetes Res. 2016:7823130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gazmararian JA, Williams MV, Peel J, Baker DW. 2003. Health literacy and knowledge of chronic disease. Patient Educ Counsel. 51(3):267–277. [DOI] [PubMed] [Google Scholar]
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, et al. ; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. 2014. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 129(3):e28–e292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macek MD, Atchison KA, Watson MR, Holtzman J, Wells W, Braun B, Aldoory L, Messadi D, Gironda M, Haynes D, et al. 2016. Assessing health literacy and oral health: preliminary results of a multi-site investigation. J Public Health Dent. 76(4):303–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. 1987. Development of a short acculturation scale for Hispanics. Hisp J Behav Sci. 9(2):183–205. [Google Scholar]
- McNaughton CD, Jacobson TA, Kripalani S. 2014. Low literacy is associated with uncontrolled blood pressure in primary care patients with hypertension and heart disease. Patient Educ Counsel. 96(2):165–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poureslami I, Nimmon L, Rootman I, Fitzgerald MJ. 2017. Health literacy and chronic disease management: drawing from expert knowledge to set an agenda. Health Promot Int. 32(4):743–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powers BJ, Olsen MK, Oddone EZ, Thorpe CT, Bosworth HB. 2008. Literacy and blood pressure—do healthcare systems influence this relationship? A cross-sectional study. BMC Health Serv Res. 8:219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. 2002. Association of health literacy with diabetes outcomes. JAMA. 288(4):475–482. [DOI] [PubMed] [Google Scholar]
- Sudore RL, Mehta KM, Simonsick EM, Harris TB, Newman AB, Satterfield S, Rosano C, Rooks RN, Rubin SM, Ayonayon HN, et al. 2006. Limited literacy in older people and disparities in health and healthcare access. J Am Geriatr Soc. 54(5):770–776. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services (DHHS). 2010. Healthy People 2010. Washington (DC): Government Printing Office. [Google Scholar]
- Wallston BS, Wallston KA, Kaplan GD, Maides SA. 1976. Development and validation of the health locus of control (HLC) scale. J Consult Clin Psychol. 44(4):580–585. [DOI] [PubMed] [Google Scholar]
- Williams MV, Baker DW, Parker RM, Nurss JR. 1998. Relationship of functional health literacy to patients’ knowledge of their chronic disease: a study of patients with hypertension and diabetes. Intern Med. 158(2):166–172. [DOI] [PubMed] [Google Scholar]
- Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, Nurss JR. 1995. Inadequate functional health literacy among patients at two public hospitals. JAMA. 4(21):1677–1682. [PubMed] [Google Scholar]
- Wilson JF. 2003. The crucial link between literacy and health. Ann Intern Med. 39(10):875–878. [DOI] [PubMed] [Google Scholar]