Background
The proportion of women in medicine is increasing,1,2 and female medical graduates outnumber males everywhere, apart from Japan and Switzerland.3
This development is of concern to some health-care systems. Tokyo Medical University systematically capped female entrants at 30%.4–6 Rather than addressing excessive working hours,7 lack of flexibility in training, poor childcare provision and open a dialogue with unsupportive senior doctors,8 the Tokyo medical school selected for men, who they thought were more likely to stay in the workplace. Similarly, a recent editorial in the British Medical Journal9 also argued for a change in the intake criteria of medical schools to select doctors with the ‘correct motivation and attributes’ to work in the NHS without taking any time out rather than consider workforce planning to allow for different preferences and working patterns.
Women remain underrepresented in surgery where the training curriculum must accommodate both the acquisition of knowledge and the development of practical skills.10–14 However, research has shown that women possess equal desire to pursue surgery early on in their careers.15 Few studies have looked at gastroenterology training from a gender perspective.16,17 However, female gastroenterologists have lower engagement in leadership roles,18 earn less money than male gastroenterologists,19 are more likely to remain childless and receive significantly less training in endoscopy.20
In 2018, the UEG Week included a Symposium on the topic of women in endoscopy. In preparation, we conducted a survey to explore the barriers encountered by women during endoscopy training. Because some studies have suggested that women may be more ‘risk-averse’,21 we also set out to compare attitudes to risk.
Methods
In October 2018, using Twitter and Facebook, female gastroenterologists were invited to take part in an online survey asking about perceived obstacles during endoscopy training under the headings ‘confidence’, ‘part-time working’, ‘self-advocacy’, ‘patriarchy’ and ‘childbearing’.
In a second linked survey, we compared attitudes to risk between male and female fully trained endoscopists describing themselves as ‘primarily diagnostic endoscopists’ versus ‘primarily therapeutic endoscopists’. The invitation was open to all trained gastroenterologists, regardless of annual number of procedures or years of practise. To gauge attitude to risk, we presented respondents to seven real-life endoscopic scenarios asking respondents to select a solution with which they would feel the most comfortable. Three options were given to each scenario: (a) a cautious approach associated with more inconvenience to the patient, (b) a less cautious approach linked with greater risks but less inconvenience to the patient and (c) an option between the two extremes. Details of the endoscopic case scenarios are available on the UEG website. The statistical analyses were carried out using SPSS version 26.
Results
A total of 225 endoscopists with a median age of 29 years completed the survey from 35 countries (84% from high-income countries, with the largest single group from the UK which constituted 38% of respondents). Almost half (100/225) regarded themselves as ‘therapeutic’ (interventional) endoscopists, and of these, 30 were women (see Table 1). There was little difference in the range of endoscopic procedures carried out by male versus female mainly diagnostic endoscopists and therapeutic endoscopists.
Table 1.
Endoscopic procedures carried out by respondents.
| Gastroscopy | Colonoscopy | ERCP | EUS | Enteroscopy | |
|---|---|---|---|---|---|
| Male mainly diagnostic endoscopists (n = 46) | 46 (100%) | 43 (93%) | 3 (6%) | – | 4 (15%) |
| Female mainly diagnostic endoscopists (n = 69) | 58 (84%) | 61 (88%) | 2 (3%) | 7 (10%) | – |
| Male mainly therapeutic endoscopists (n = 80) | 78 (97%) | 78 (97%) | 44 (55%) | 29 (36%) | 19 (23%) |
| Female mainly therapeutic endoscopists (n = 30) | 29 (97%) | 29 (97%) | 10 (33%) | 11 (37%) | 5 (17%) |
ERCP: endoscopic retrograde cholangiopancreatography; EUS: endoscopic ultrasound.
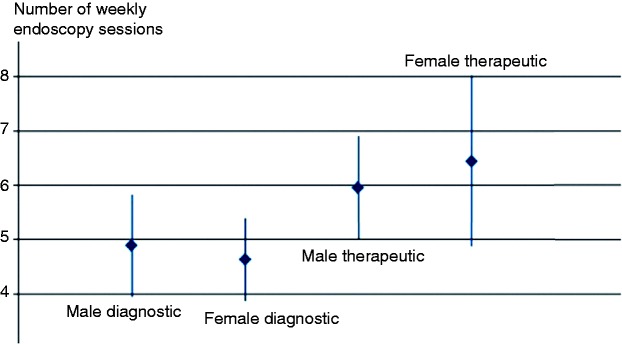
There was no statistically significant difference in the number of weekly sessions spent in the endoscopy unit between male versus female non-interventional and interventional endoscopists (Figure 1).
Figure 1.
Mean number of weekly endoscopy sessions.
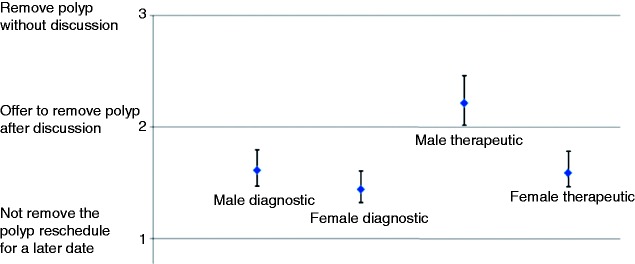
However, there was a difference in attitude to risk between diagnostic and therapeutic endoscopists, with diagnostic endoscopists being more risk averse in most clinical scenarios. The only clinical scenario in which a female interventional endoscopist was likely to be significantly more cautious than their male counterpart was that regarding informed consent. This scenario described the unexpected encounter of a 15 mm pedunculated polyp in a young man in whom no consent had been sought for polypectomy before colonoscopy. Male therapeutic endoscopists were significantly more likely to go ahead and remove the polyp at the index examination (See Figure 2). Diagnostic endoscopists and female therapeutic endoscopists were more likely to reschedule the polypectomy for a later date or attempt to discuss the options with the patient at the time of the procedure.
Factors perceived to be holding women back in training
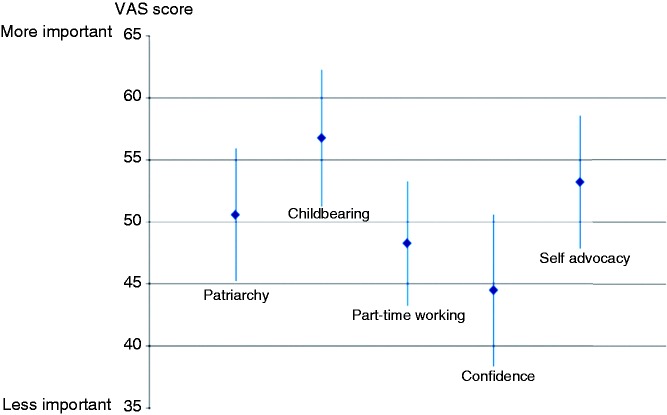
Female gastroenterologists were asked to give examples of barriers they had encountered in their endoscopy training. Responses were grouped under the following five headings: ‘confidence’, ‘part-time working’, ‘self-advocacy’, ‘patriarchy’ and ‘childbearing’. Trainees were asked to grade items according to importance on the following visual analogue scale: 0 = ‘no importance’ and 100 = ‘extremely important’.
Confidence
Confidence was regarded as the least important issue for female trainees, significantly less important than childbearing with a median VAS score of 44 (95% confidence interval (CI) 38–50) (Figure 3).
Female trainees seemed to process setbacks differently from men. A female trainee recalled telling her trainer that she had failed to reach the caecum. ‘As my trainer took over, he explained that I didn’t “fail” but that my colonoscopy was just incomplete. With these words, I realised that my “framing” had been wrong!’ In addition, several female trainees reported that they felt more unsettled by minor adverse events such as bleeding after polypectomy. ‘Endoscopic complications do affect me, whereas my male colleagues seem less concerned’.
Part-time working
The mean VAS score for part-time working was 48 (95% CI 43–53). Many trainees pointed out that simply being around less meant that it was difficult to maintain the connections required to be considered for a therapeutic training programme.
Furthermore, many women highlighted the issues linked with staffing an endoscopy list versus for example an outpatient clinic. This was most concisely put by a female trainee from the UK: ‘If they phone from school to say that my child is poorly and I have to cancel with short notice, it’s far easier for me to find someone to cover my outpatient clinic than my ERCP list …’.
Self-advocacy
Self-advocacy, whereby women are less likely to put themselves forward, has previously been identified as a reason for seeing fewer women in leadership roles. In our survey, it was also seen as an important factor, with a mean VAS score of 53 (95% CI 47–58). Comments included: ‘Women generally prefer their achievements to speak for themselves’, ‘men are better able to “disguise” insecurity or lack of confidence in order to not look unprepared’ and ‘Women feel that they have to prove that they are far better than “good enough” before putting themselves forward for training in interventional endoscopy’.
Patriarchy
As expected, patriarchy was recognised as an important issue, with a mean VAS score of 50 (95% CI 45–55). This was unsurprising, as a US study22 of surgical training found that women often felt excluded from the ‘dominant culture’, that is, the one that establishes values, rules and norms of behaviour.
In our survey, words such as ‘stitch-up’, ‘conspiracy’ and ‘male club’ were often used to describe circumstances. Most agreed that ‘unconscious bias’ was at play, together with a lack of female role models. Comments included: ‘When a male training lead considers trainees for the endoscopy training post, they will look for someone like themselves’. Similarly, female trainees often commented that they were more likely to be given tasks such as organising staffing rotas, teaching or seeing referrals than learning therapeutic skills. They attributed this to a perception that they had better negotiation and communication skills. This was summed up by a female trainee as follows: ‘Spending my first year of specialist training dealing with rostering issues and teaching medical students whilst my male counterparts were learning endoscopy made me doubt my endoscopy abilities’.
Our findings indicate that unless exposed to hands-on endoscopy at an early stage and encouraging role models in their training, women are unlikely to consider a career in therapeutic endoscopy seriously.
Pregnancy and childcare
A small study of Canadian gastroenterologists23 found that women’s spouses were more likely to be physicians or other professionals, whereas men’s spouses were more likely to be housewives. It was therefore not surprising that childbearing was regarded as the most important issue by our respondents, with a mean VAS score of 56 (95% CI 51–62). Many female trainees also highlighted that endoscopy training programmes start at a point in a trainee’s career when they also want to start a family.
Many institutions reportedly lacked sufficient job-sharing opportunities, as the expectation was that everyone works full time. Furthermore, many countries offered no protection of training placements during maternity leave. US legislation does not even mandate paid maternity leave.
Being pregnant also puts women at a direct disadvantage. Many women reported feeling tired during long endoscopy lists, not being able to use the colonoscopy imager, having concerns about radiation as well as fatigue and back pain being exacerbated by heavy lead protection.
Discussion
Gender discrimination has a negative effect beyond damage to individual women’s careers.24 Organisations miss out on gender-balanced leadership. Patients miss out on the more effective communication skills of women25 and may also suffer worse outcomes.26–29 Finally, female patients have a preference for a female endoscopist30,31 and may even decline screening colonoscopy if a female is not available.32
Women in medicine face similar challenges to those in other professions, including access to childcare, flexible working, loss of confidence following pregnancy and lack of female role models. Unfortunately, training programmes rarely attempt any formal evaluation of the experience training provides, let alone develop a plan for dealing with these barriers.33,34
There are several limitations to our study. Our tool for assessing attitude to risk in endoscopy has not been independently validated. Our study includes the opinions of self-selected individuals. Finally, the distribution of respondents was highly skewed. Most came from countries classified by the World Bank as high-income countries.35 This limitation reduces the generalisability of our findings.
Our empirical survey has revealed several explanations for women being underrepresented in advanced endoscopy. Clearly, the issues are more intractable than can be solved by sending training leads to ‘implicit bias training’36 or female trainees on courses to develop resilience, negotiation or assertiveness skills.37 Our task is to understand the barriers and create a service where all trainees feel valued and supported.
Figure 2.
What do do with an unexpected 15mm polyp encountered at colonoscopy in a young patient.
Figure 3.
Relative importance of issues encountered by female trainees.
References
- 1.Ramakrishnan A, Sambuco D, Jagsi R. Women’s participation in the medical profession: insights from experiences in Japan, Scandinavia, Russia, and Eastern Europe. J Womens Health (Larchmt) 2014; 23: 927–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NHS digital. Narrowing of NHS gender divide but men still the majority in senior roles, https://digital.nhs.uk/news-and-events/latest-news/narrowing-of-nhs-gender-divide-but-men-still-the-majority-in-senior-roles (2018, accessed 13 May 2019).
- 3.Organisation for Economic Cooperation and Development. Graduation rates in tertiary education by gender, www.oecd.org/gender/data/graduationratesintertiaryeducationbysex.htm (2015, accessed 22 November 2018).
- 4.The Guardian. Tokyo medical school ‘changed test scores to keep women out’, https://www.theguardian.com/world/2018/aug/02/tokyo-medical-school-changed-test-scores-to-keep-women-out (2018, accessed 13 May 2019).
- 5.Shoji H. A Tokyo medical school rigged exam results to favour men. But Japan’s sexism problem runs even deeper, http://time.com/5374353/japan-sexismme-too/ (2018, accessed 13 May 2019).
- 6.Nationwide probe after Tokyo medical school excluded women, https://www.france24.com/en/20180810-japan-nationwide-probe-tokyo-medical-schoolexcludes-women (2018, accessed 13 May 2019).
- 7.Nomura K, Yamazaki Y, Gruppen LD, et al. The difficulty of professional continuation among female doctors in Japan: a qualitative study of alumnae of 13 medical schools in Japan. BMJ Open 2015; 5: e005845–e005845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Takata H, Nagata H, Nogawa H, et al. The current shortage and future surplus of doctors: a projection of the future growth of the Japanese medical workforce. Hum Resour Health 2011; 9: 14–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cleland J, Simpson J, Johnston P. Doctors opt out of training after foundation years. BMJ 2019; 365: l1509–l1509. [DOI] [PubMed] [Google Scholar]
- 10.Van Heest AE, Agel J. The uneven distribution of women in orthopaedic surgery resident training programs in the United States. J Bone Joint Surg Am 2012; 94: e9–e9. [DOI] [PubMed] [Google Scholar]
- 11.Rohde RS, Wolf JM, Adams JE. Where are the women in orthopaedic surgery? Clin Orthop Relat Res 2016; 474: 1950–1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muffly TM, Weterings R, Barber MD, et al. Discrepancies in the female pelvic medicine and reconstructive surgeon workforce. Female Pelvic Med Reconstr Surg 2015; 21: 99–105. [DOI] [PubMed] [Google Scholar]
- 13.Benzil DL, Abosch A, Germano I, et al. The future of neurosurgery: a white paper on the recruitment and retention of women in neurosurgery. J Neurosurg 2008; 109: 378–386. [DOI] [PubMed] [Google Scholar]
- 14.Renfrow JJ, Rodriguez A, Liu A, et al. Positive trends in neurosurgery enrollment and attrition: analysis of the 2000–2009 female neurosurgery resident cohort. J Neurosurg 2016; 124: 834–839. [DOI] [PubMed] [Google Scholar]
- 15.Report of the Chair of the National Working Group on Women in Medicine. Women doctors: making a difference, https://www.nwpgmd.nhs.uk/sites/default/files/WIMreport.pdf (2009, accessed 13 May 2019).
- 16.Gerson LB, Twomey K, Hecht G, et al. Does gender affect career satisfaction and advancement in gastroenterology? Results of an AGA institute-sponsored survey. Gastroenterology 2007; 132: 1598–1606. [DOI] [PubMed] [Google Scholar]
- 17.Perera S, Bistritz L, Beaton MD. Equity and gender issues among members of the Canadian Association of Gastroenterology. J Can Assoc Gastroenterol 2018; 13 May 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moleiro J, Ilie M, Fitzgerald R. Leadership roles for women in gastroenterology: new initiatives for the new generation of gastroenterologists. United European Gastroenterol J 2016; 4: 815–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh A, Burke CA, Larive B, et al. Women in Gastroenterology Committee of American College of Gastroenterology. Do gender disparities persist in gastroenterology after 10 years of practice? Am J Gastroenterol 2008; 103: 1589–1595. [DOI] [PubMed] [Google Scholar]
- 20.Arlow FL, Raymond PL, Karlstadt RG, et al. Gastroenterology training and career choices. Am J Gastroenterol 2002; 97: 459–469. [DOI] [PubMed] [Google Scholar]
- 21.Byrnes JP, Miller DC, Schafer WD. Gender differences in risk taking: a meta-analysis. Psychol Bull 1999; 125: 367–383. [Google Scholar]
- 22.Cochran A, Hauschild T, Elder WB, et al. Perceived gender-based barriers to careers in academic surgery. Am J Surg 2013; 206: 263–268. [DOI] [PubMed] [Google Scholar]
- 23.Heathcote J, Cauch-Dudek K, Rhyne D. The professional lives of women in gastroenterology: a Canadian comparison study with men. Gastroenterology 1997; 113: 669–674. [DOI] [PubMed] [Google Scholar]
- 24.DeFilippis EM. Putting the ‘she’ in doctor. JAMA Intern Med 2018; 178: 323–324. [DOI] [PubMed] [Google Scholar]
- 25.Hall JA, Blanch-Hartigan D, Roter DL. Patients’ satisfaction with male versus female physicians: a meta-analysis. Med Care 2011; 49: 611–617. [DOI] [PubMed] [Google Scholar]
- 26.Greenwood BN, Carnahan S, Huang L. Patient–physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci U S A 2018; 115: 8569–8574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsugawa Y, Jena AB, Figueroa JF, et al. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med 2017; 177: 206–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wallis CJD, Ravi B, Coburn N, et al. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ 2017; 359: j4366–j4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mehrotra A, Morris M, Gourevitch RA, et al. Physician characteristics associated with higher adenoma detection rate. Gastrointest Endosc 2018; 87: 778–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shah DK, Karasek V, Gerkin RD, et al. Sex preferences for colonoscopists and GI physicians among patients and health care professionals. Gastrointest Endosc 2011; 74: 122–127. [DOI] [PubMed] [Google Scholar]
- 31.Menees SB, Inadomi JM, Korsnes S, et al. Women patients’ preference for women physicians is a barrier to colon cancer screening. Gastrointest Endosc 2005; 62: 219–223. [DOI] [PubMed] [Google Scholar]
- 32.Denberg TD, Melhado TV, Coombes JM, et al. Predictors of nonadherence to screening colonoscopy. J Gen Intern Med 2005; 20: 989–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Snyder RA, Tarpley MJ, Phillips SE, et al. The case for on-site child care in residency training and afterward. J Grad Med Educ 2013; 5: 365–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garza RM, Weston JS, Furnas HJ. Pregnancy and the plastic surgery resident. Plast Reconstr Surg 2017; 139: 245–252. [DOI] [PubMed] [Google Scholar]
- 35.World Bank. Country and lending groups 2015, http://data.worldbank.org/about/country-and-lending-groups (accessed 13 May 2019).
- 36.Phillips NA, Tannan SC, Kalliainen LK. Understanding and overcoming implicit gender bias in plastic surgery. Plast Reconstr Surg 2016; 138: 1111–1116. [DOI] [PubMed] [Google Scholar]
- 37.Kang SK, Kaplan S. Working toward gender diversity and inclusion in medicine: myths and solutions. Lancet 2019; 393: 579–586. [DOI] [PubMed] [Google Scholar]