Abstract
Context
Patellar tendinopathy (PT) is a degenerative condition known to affect athletes who participate in sports such as basketball and volleyball. Patellar tendinopathy is a challenging condition to treat and may cause an athlete to prematurely retire from sport. The prevalence of PT in male collegiate basketball players is unknown.
Objective
To determine the prevalence of PT and patellar tendon abnormality (PTA) in a population of male collegiate basketball players.
Design
Cross-sectional study.
Setting
National Collegiate Athletic Association Divisions II and III, National Association of Intercollegiate Athletics, and Northwest Athletic Conference male collegiate basketball teams were assessed in a university laboratory setting.
Patients or Other Participants
Ninety-five male collegiate basketball players (age = 20.0 ± 1.7 years).
Main Outcome Measure(s)
A diagnostic ultrasound image of an athlete's patellar tendon was obtained from each knee. Patellar tendinopathy was identified based on a player's symptoms (pain with palpation) and the presence of a hypoechoic region on an ultrasonographic image.
Results
A majority of participants, 53 of 95 (55.8%), did not present with pain during palpation or ultrasonographic evidence of PTA. Thirty-two basketball players (33.7%) displayed ultrasonographic evidence of PTA in at least 1 knee; 20 of those athletes (21.1%) had PT (pain and tendon abnormality). Nonstarters were 3.5 times more likely to present with PTA (odds ratio = 3.5, 95% confidence interval = 1.3, 9.6; P = .017) and 4 times more likely to present with PT (odds ratio = 4.0, 95% confidence interval = 1.1, 14.8; P = .038) at the start of the season.
Conclusions
One in 3 male collegiate basketball players presented with either PT or PTA. Sports medicine professionals should evaluate basketball athletes for PT and PTA as part of a preseason screening protocol.
Keywords: diagnostic ultrasound, jumper's knee, knee
Key Points
More than 20% of male collegiate basketball players presented with patellar tendinopathy before the start of sanctioned practices.
Thirty-three percent of male collegiate basketball players presented with ultrasonographic evidence of a hypoechoic region (eg, patellar tendon abnormality) in at least 1 patellar tendon.
Basketball players categorized as nonstarters were more likely to present with patellar tendon abnormalities and patellar tendinopathy than their starter counterparts.
Other potential risk factors (eg, age, height, weight, body mass index, and player position) were not associated with a greater risk of patellar tendon abnormality or patellar tendinopathy.
Patellar tendinopathy (PT) is a degenerative condition marked by histopathologic changes in the tendon.1–5 Patellar tendinopathy, also commonly referred to as jumper's knee, is experienced primarily by active individuals (age range = 14–40 years),2,6–8 especially basketball and volleyball athletes.6–10 The prevalence of PT has been reported to be as high as 32% in elite male basketball players (mean age = 24.1 ± 5.1 years) and as high as 50% in high-level male volleyball players (Norwegian teams, age range not provided).8,11 Patellar tendinopathy is a challenging condition to treat: many athletes miss prolonged periods of play or must retire prematurely from sport participation.12,13
The clinical diagnosis of PT has historically been based on a patient's symptoms (eg, pain with tendon loading during jumping), musculoskeletal examination, and pain with palpation of the tendon (ie, the portion of the tendon distal to the patella) or the inferior pole of the patella.3,5,8,14 The Victorian Institute of Sport Assessment–Patella questionnaire has also been used as part of the diagnostic process to categorize injury severity and track rehabilitation progress.15 Diagnostic ultrasound imaging of the patellar tendon can be performed to confirm the diagnosis of PT in patients who present with the aforementioned clinical findings.1,3,5 Ultrasound imaging is considered the criterion standard test for diagnosing patellar tendon abnormality (PTA).5,16 An ultrasonographic image of the PTA shows a hypoechoic region (Figure 1). However, clinical findings are not always associated with PT, and PTA is not always associated with symptoms. For example, palpation of the patellar tendon alone offers little diagnostic utility.1 Patellar tendon abnormality on an ultrasound image in the absence of other clinical findings also has limited diagnostic utility. Previous authors7 identified PTA in asymptomatic athletes with no known history of the disease. To appreciate the health status of the patellar tendon, studies of prevalence should include measures of both PTA (via ultrasound imaging) and PT (diagnosis based on clinical signs and symptoms confirmed by ultrasound imaging).
Figure 1.
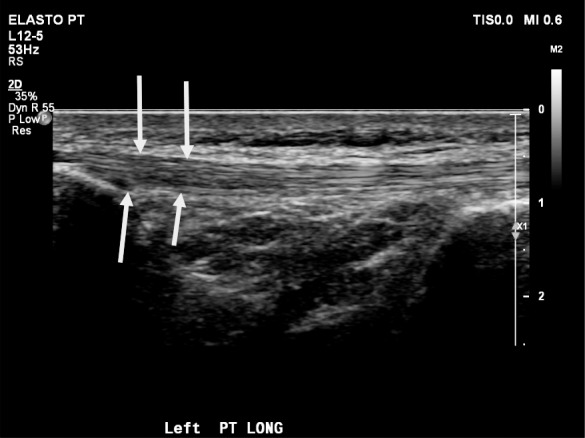
Diagnostic ultrasound image of a left patellar tendon (longitudinal view). Arrows illustrate hypoechoic region of the tendon.
The reported preseason prevalence of PT and PTA varies widely across athletic populations and is unknown for some groups of athletes. As mentioned earlier, the prevalence of PT has been reported in male elite basketball and volleyball players; however, the prevalence of PTA in those populations is unknown.8,11 Researchers have reported the PT and PTA prevalence among elite teenage basketball players (tendinopathy = 7%, tendon abnormality with or without pain = 26%), elite junior volleyball players (tendinopathy = 18%, tendon abnormality with or without pain = 36%), and adult volleyball players (tendinopathy = 30.2%, tendon abnormality without pain = 26.6%).7,14,17 Among younger athletes, investigators7,14,17 demonstrated a range of tendinopathy prevalence rates and tendon abnormalities. The prevalence of PTA (in which an athlete may be asymptomatic) and the diagnosis of PT display a disconnect. Evaluating tendon health in additional populations is warranted to appreciate the prevalence of abnormalities among those who may be experiencing this condition or at risk for worsening of the condition.
An abnormal ultrasound finding in asymptomatic individuals may indicate that symptoms are likely to develop and, therefore, may motivate preseason screening and prevention. In a sample of asymptomatic, teenage elite basketball players, a hypoechoic region in the patellar tendon was associated with a fourfold (relative risk = 4.2) increased risk of symptoms.6 Interestingly, male athletes were more likely to experience PTA than their female counterparts.6 A subsequent study14 supported the association between symptom onset and tendon abnormalities at the start of the season. The risk of developing PT was low in junior volleyball players who started the season with normal diagnostic ultrasound findings.14 The presence of PT or PTA at the start of the season is important for athletic trainers and other sports medicine professionals to document. Athletes with an asymptomatic tendon abnormality may go on to develop PT, and athletes with PT may benefit from an evidence-based therapeutic exercise program.
As noted, the prevalence of PTA (26% in teenage basketball players) and PT (7% in teenage basketball players and 32% in Norwegian elite-level basketball players) has been reported in a few basketball populations; however, the prevalence of PT and PTA in male collegiate basketball players is unknown.7,8 Therefore, the primary purpose of our study was to identify the prevalence of PT and PTA in a population of male collegiate basketball athletes. The secondary purpose was to compare the prevalence of PT and PTA based on age, anthropometric measures, starter status, player position, and level of competition. We hypothesized that the following characteristics would be associated with greater odds of having PT and PTA: older age; taller, heavier, or overweight athletes; forwards or centers; starters; and athletes who played for universities or colleges that offered scholarships.
METHODS
Participants
A total of 95 male collegiate basketball players (mean age = 20.0 ± 1.7 years) representing 7 teams participated in this study. Teams were recruited from the Portland, Oregon region. The sample consisted of basketball players representing the National Collegiate Athletic Association (NCAA) Division II (DII; n = 14), NCAA Division III (DIII; n = 43), National Association of Intercollegiate Athletics (NAIA; n = 21), and community college (n = 17) levels of competition. An athlete was excluded from the study if he was (a) restricted from sport participation by the team physician or the team's certified athletic trainer due to injury, (b) was unable to fully participate in practice, (c) was unable to complete a drop vertical jump from 76.2 cm, or (d) under the age of 17 years at the time of testing. The 76.2-cm drop vertical jump was included in the testing as a part of a larger study. The Institutional Review Board of George Fox University (Newberg, OR) approved this investigation. Informed consent was obtained from each participant before data collection.
Testing Protocol
Demographic and anthropometric information and diagnostic ultrasound imaging were collected during the athletes' off-season period, just before the official (ie, sanctioned) start of their collegiate preseason. Demographic information was obtained from each athlete before imaging. Age was requested from the athlete when he completed the informed consent. Height was collected using a cloth tape affixed to a wall. Weight was measured when the athlete stood on a force plate (model BP 600600; AMTI, Watertown, MA). Body mass index (BMI) was calculated from the height and weight measures. Player position and starter or nonstarter status were determined by reviewing each team's roster and season statistics.
Ultrasonography was performed by 2 clinicians (M.K.H., J.H.) with 27 and 31 years of experience, respectively. Interrater reliability for diagnostic ultrasound images of the patellar tendon is excellent.18–20 Participants were positioned supine on a treatment plinth with the knees flexed to approximately 110°. Four ultrasound images, a longitudinal view and 3 transverse views, were captured for each patellar tendon. For the longitudinal view, the image consisted of the tendon from the distal pole of the patella to its insertion on the proximal tibia (ie, tibial tuberosity). Transverse views (3 images) were captured at the proximal (near the apex of the patella) and distal (near the tibial tuberosity) insertion points and midpoint between these structures. An ultrasound machine (model Affinity 50G; Phillips Healthcare, Andover, MA) fitted with a 50-mm linear array probe was used at a depth of 2.5 cm for all images.
Ultrasound images were reviewed for the presence of PTA independently by M.K.H. and a second researcher (J.B., with 19 years of experience). A tendon was identified as having a PTA based on the presence of a hypoechoic region (Figure 1). We categorized individuals as having PTA in the right patellar tendon only, the left patellar tendon only, or both patellar tendons or none in either tendon. A κ statistic was performed to determine agreement between researchers. The κ value was 0.828 (P < .001) with 91.6% agreement between raters.21 The subsequent statistical analysis was based on the PTA prevalence established by M.K.H.
One researcher (J.B.), who was blinded to the diagnostic ultrasound findings at the time of testing, palpated both tendons of each athlete. Palpation was performed along the length of each patellar tendon from its origin on the patella to its insertion site on the tibial tuberosity.
Statistical Analysis
Descriptive statistics (mean ± standard deviation) were calculated for the athletes' age, height, weight, and BMI and compared using analysis of variance. An athlete was diagnosed with PT if he presented with a hypoechoic region on diagnostic ultrasound imaging and pain with palpation of the involved tendon. An athlete was categorized as having a PTA only if he had sonographic evidence of tendon abnormality but did not experience pain during palpation. Participants were also categorized as having pain with palpation (but no tendon abnormality) or as having no pain and no PTA. Logistic regression was performed to calculate the prevalence odds ratios (ORs) for potential risk factors. The 7 risk factors analyzed in this study were age, height, weight, BMI, player position, starter status, and level of competition. Each factor was dichotomized into an at-risk and a lesser-risk (ie, reference) group. Age was dichotomized based on mean scores from this sample: 19 years and younger (reference) or 20 years and older (at risk).8,11 Taller, heavier, and overweight (BMI ≥ 25.0 kg/m2) athletes were categorized as at risk, and shorter, lighter, and normal-weight (BMI = 18.5–24.9 kg/m2) athletes served as the reference groups. Prior reports22,23 have suggested that weight and BMI may be risk factors for tendinopathy. Player position was categorized as either a guard (eg, point guard, guard, wing) or a forward or center (eg, forward, post, center). Forwards and centers were categorized as at risk, and guards served as the reference group. Forwards and centers, who are usually taller and heavier than guards, jump at a greater frequency during sport due to positional requirements.24 Starters were identified from season statistics as the players who started a majority of games for their team. Starters were categorized as at risk, and nonstarters served as the reference group. We hypothesized that starters might be at greater risk because of more exposure to injury due to more minutes played in practices and games. A total of 34 starters were identified (for the 7 teams, 35 starters would have been expected; however, 1 starter did not attend testing). Athletes were dichotomized into 2 groups by level of competition: NCAA DII, NAIA, and community college athletes were categorized as at risk, and NCAA DIII athletes served as the reference group. This dichotomization was based on programs that could offer athletic scholarships (eg, NCAA DII, NAIA, community college programs) and those that could not (NCAA DIII).
RESULTS
Of the 95 male collegiate basketball players, 32 (33.7%) presented with ultrasound findings associated with PTA (Table 1). Twenty players were diagnosed as having PT, and another 12 presented with PTA only (ie, no pain with palpation of the tendon). Ten players reported pain with palpation of a tendon; however, these players had no PTA. The remaining 53 athletes presented with no pain and no PTA. Patellar tendon abnormality was present in the right knee only of 14 participants, the left knee only of 13, and bilaterally in 5 (Figure 2). No differences in demographic characteristics existed between participants based on the presence of PTA or pain with palpation (or both).
Table 1.
Baseline Characteristics of Male Collegiate Basketball Players With Patellar Tendinopathy (PT)a or Patellar Tendon Abnormality (PTA)
| Variable |
Basketball Players, Mean ± SD |
P Valueb |
||||
| All (n = 95) |
With PT (n = 20) |
With PTA Only (n = 12) |
With Pain Only (n = 10) |
With No Pain and No PTA (n = 53) |
||
| Age, y | 20.0 ± 1.7 | 20.6 ± 2.1 | 19.5 ± 1.3 | 19.8 ± 1.2 | 20.0 ± 1.6 | .266 |
| Height, m | 1.90 ± 0.08 | 1.90 ± 0.06 | 1.88 ± 0.08 | 1.88 ± 0.07 | 1.91 ± 0.09 | .551 |
| Weight, kg | 87.4 ± 11.4 | 87.8 ± 8.8 | 85.2 ± 13.9 | 85.9 ± 9.6 | 88.0 ± 12.1 | .873 |
| Body mass index, kg/m2 | 24.2 ± 2.5 | 24.4 ± 2.3 | 24.1 ± 2.7 | 24.3 ± 2.1 | 24.1 ± 2.6 | .977 |
Pain on palpation and a hypoechoic region on ultrasound imaging.
Analysis of variance.
Figure 2.
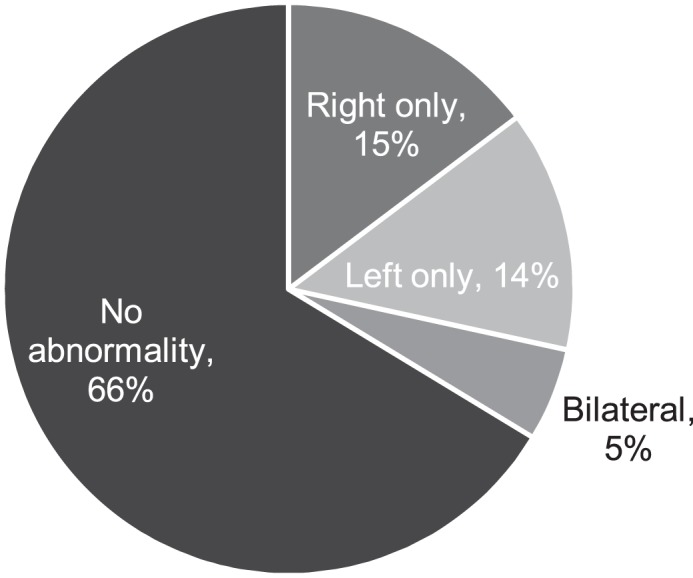
Distribution of patellar tendon abnormality by lower extremity.
Similarly, no difference in PT or PTA prevalence was found by age or anthropometric measures (eg, height, weight, BMI; Table 2). Forwards and centers were no more likely to demonstrate PT or PTA than guards. Starters were less likely to have PT (OR = 0.25, 95% confidence interval [CI] = 0.07, 0.92; P = .038) or PTA (OR = 0.29, 95% CI = 0.10, 0.80; P = .017). In other words, nonstarters were 4 times (95% CI = 1.1, 14.8; P = .038) more likely to present with PT and were 3.5 times (95% CI = 1.3, 9.6; P = .017) more likely to present with PTA. The highest percentage of PT by level of competition was in NAIA athletes (28.6%), followed by community college (23.5%), DII (21.4%), and DIII (16.2%) players. The highest percentage of PTA (with or without pain during palpation) by level of competition was observed in NAIA (42.9%), followed by DII (35.7%), DIII (30.2%), and then community college (29.4%) players. Prevalence did not differ based on competition-level dichotomization.
Table 2.
Relationships Between Age, Anthropometric Measures, and Sport-Related Demographics and Patellar Tendinopathy or Patellar Tendon Abnormality
| Characteristic |
No. per Category |
Patellar Tendinopathy, No. (%) |
Odds Ratio (95% CI) |
Patellar Tendon Abnormality, No. (%) |
Odds Ratio (95% CI) |
| Age, y | |||||
| ≤19 | 42 | 7 (16.7) | Reference | 12 (28.6) | Reference |
| ≥20 | 53 | 13 (24.5) | 1.6 (0.58, 4.5) | 20 (37.7) | 1.5 (0.64, 3.6) |
| Height, m | |||||
| ≤1.89 | 48 | 8 (16.7) | Reference | 16 (33.3) | Reference |
| ≥1.90 | 47 | 12 (25.5) | 1.7 (0.63, 4.7) | 16 (34.0) | 1.0 (0.44, 2.4) |
| Weight, kg | |||||
| ≤87.39 | 49 | 9 (18.4) | Reference | 16 (32.7) | Reference |
| ≥87.40 | 46 | 11 (23.9) | 1.4 (0.52, 3.8) | 16 (34.8) | 1.1 (0.47, 2.6) |
| Body mass index, kg/m2 | |||||
| Normal (18.5–24.9) | 62 | 12 (19.4) | Reference | 21 (33.9) | Reference |
| Overweight (25–29.9) | 33 | 8 (24.2) | 1.3 (0.48, 3.7) | 11 (33.3) | 0.98 (0.40, 2.4) |
| Position | |||||
| Guard | 59 | 11 (18.6) | Reference | 21 (35.6) | Reference |
| Forward or center | 36 | 9 (25.0) | 1.5 (0.54, 4.0) | 11 (30.6) | 0.80 (0.32, 1.9) |
| Starter status | |||||
| Starter | 34 | 3 (8.8) | 0.25 (0.07, 0.92)b | 6 (17.6) | 0.29 (0.10, 0.80)c |
| Nonstarter | 61 | 17 (27.9) | Reference | 26 (42.6) | Reference |
| Level of competitiona | |||||
| NCAA DII/NAIA/CC | 52 | 13 (25.0) | 1.7 (0.62, 4.8) | 19 (36.5) | 1.3 (0.56, 3.1) |
| NCAA DIII | 43 | 7 (16.3) | Reference | 13 (30.2) | Reference |
Abbreviations: CC, community college; CI, confidence interval; DII, Division II; DIII, Division III; NAIA, National Association of Intercollegiate Athletics; NCAA, National Collegiate Athletic Association.
Dichotomization was based on competition levels eligible to offer athletic scholarships.
Starters were hypothesized to be at greater risk than nonstarters but nonstarters had a 4.0-fold increased risk of patellar tendinopathy (95% CI = 1.1, 14.8; P = .038).
Starters were hypothesized to be at greater risk than nonstarters but nonstarters had a 3.5-fold increased risk of patellar tendon abnormality (95% CI = 1.3, 9.6; P = .017).
DISCUSSION
To our knowledge, we are the first to use diagnostic ultrasound imaging to confirm the presence of PT and to identify PTA in a population of male collegiate basketball players during the off-season, just before the start of the preseason. More than 20% of basketball players presented with PT, and another 12% displayed ultrasonographic evidence of PTA.
Several important findings were revealed. First, approximately 1 in 3 male collegiate basketball players had either PT or ultrasonographic evidence of PTA in at least 1 tendon during the off-season. The presence of PTA, whether or not the athlete has pain with palpation, should be concerning to ATs and sports medicine professionals who work with male collegiate basketball teams. Basketball players who were asymptomatic at the time of testing might become symptomatic as training volumes increased during the season.6,17 As previously mentioned, asymptomatic athletes with PTA were 4 times more likely to develop PT.6,25 In addition, athletes with normal tendons may develop PT as the season progresses.6,17
A second important finding was the lack of a difference in the prevalence of PT or PTA by level of competition. We assessed athletes from the DII, DIII, NAIA, and community college levels of competition. Comparisons among all 4 levels of competition were difficult due to the sample size of each group. However, dichotomizing the athletes into 2 groups based on whether programs could offer athletic scholarships resulted in no difference in prevalence rates. It must be noted that, despite efforts to collect measures on DI basketball players, we were unable to test athletes from either DI team in the Portland, Oregon region. Thus, the prevalence of PT or PTA in this population is currently unknown.
The third important finding relates to player position and starter status. We hypothesized that forwards and centers might be at greater risk for PTA due to positional requirements: shooting, offensive and defensive rebounding, and blocking shots. However, in this sample, forwards and centers were no more likely to have PTA or PT than their counterparts at the guard position. We proposed that starters might be more likely to develop PT because of more time on the court during both practices and games. Yet nonstarters were more likely to present with PTA than starters. This is an interesting result that warrants exploration in future studies. Nonstarters may demonstrate kinetic or kinematic differences when jumping; whether these differences are a cause of PT or an adaptation to the disease is unknown.26–29
Study Limitations
Two limitations were associated with this study. First, studies of prevalence can identify potential relationships between disease and risk factors; however, they do not provide strong evidence of causality. Second, we only evaluated male athletes. Although the sexes appear to display different injury rates, the prevalence of PTA or PT in female collegiate basketball players is unknown.6 Future researchers should prospectively evaluate potential risk factors (including but not limited to player position, starter status, and presence of PTA) for developing PT in a population of male collegiate basketball players. A longitudinal prevalence study, collecting sonographic images of the tendon at the start of the preseason, the midseason, and the end of the season would illustrate tendon changes in response to exposure. Evaluating the prevalence of PTA and PT in female collegiate basketball players is warranted.
Clinical Implications
Athletic trainers and other sports medicine professionals who work with male collegiate basketball players should recognize the potential for 1 in 3 male collegiate basketball players to start the season with either a diagnosis of PT or the presence of a PTA. Many of the athletes who present with an asymptomatic hypoechoic region may develop symptomatic PT. As previously mentioned, elite teenage basketball players who presented with PTA but were asymptomatic at the time of testing were 4 times more likely to develop PT.6
CONCLUSIONS
More than 20% of male collegiate basketball players presented with PT during the off-season period, just before the start of officially sanctioned practices. Another 12% had PTA without symptoms. The prevalence of jumper's knee in this population is consistent with that of other populations of basketball athletes. Athletic trainers and sports medicine professionals who provide medical care to male collegiate basketball teams should consider assessing patellar tendon health in players as part of a preseason screening protocol.
REFERENCES
- 1.Cook JL, Khan KM, Kiss ZS, Purdam CR, Griffiths L. Reproducibility and clinical utility of tendon palpation to detect patellar tendinopathy in young basketball players: Victorian Institute of Sport tendon study group. Br J Sports Med. 2001;35(1):65–69. doi: 10.1136/bjsm.35.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gisslén K, Alfredson H. Neovascularization and pain in jumper's knee: a prospective clinical and sonographic study in elite junior volleyball players. Br J Sports Med. 2005;39(7):423–428. doi: 10.1136/bjsm.2004.013342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Malliaras P, Cook J, Purdam C, Rio E. Patellar tendinopathy: clinical diagnosis, load management, and advice for challenging case presentations. J Orthop Sports Phys Ther. 2015;45(11):887–898. doi: 10.2519/jospt.2015.5987. [DOI] [PubMed] [Google Scholar]
- 4.Peers KHE, Lysens RJJ. Patellar tendinopathy in athletes: current diagnostic and therapeutic recommendations. Sports Med. 2005;35(1):71–87. doi: 10.2165/00007256-200535010-00006. [DOI] [PubMed] [Google Scholar]
- 5.Mendonça Lde M, Ocarino JM, Bittencourt NF, Fernandes LM, Verhagen E, Fonseca ST. The accuracy of the VISA-P questionnaire, single-leg decline squat, and tendon pain history to identify patellar tendon abnormalities in adult athletes. J Orthop Sports Phys Ther. 2016;46(8):673–680. doi: 10.2519/jospt.2016.6192. [DOI] [PubMed] [Google Scholar]
- 6.Cook JL, Khan KM, Kiss ZS, Purdam CR, Griffiths L. Prospective imaging study of asymptomatic patellar tendinopathy in elite junior basketball players. J Ultrasound Med. 2000;19(7):473–479. doi: 10.7863/jum.2000.19.7.473. [DOI] [PubMed] [Google Scholar]
- 7.Cook JL, Khan KM, Kiss ZS, Griffiths L. Patellar tendinopathy in junior basketball players: a controlled clinical and ultrasonographic study of 268 patellar tendons in players aged 14–18 years. Scand J Med Sci Sports. 2000;10(4):216–220. doi: 10.1034/j.1600-0838.2000.010004216.x. [DOI] [PubMed] [Google Scholar]
- 8.Lian OB, Engebretsen L, Bahr R. Prevalence of jumper's knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33(4):561–567. doi: 10.1177/0363546504270454. [DOI] [PubMed] [Google Scholar]
- 9.Ito E, Iwamoto J, Azuma K, Matsumoto H. Sex-specific differences in injury types among basketball players. Open Access J Sports Med. 2015;6:1–6. doi: 10.2147/OAJSM.S73625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Witvrouw E, Bellemans J, Lysens R, Danneels L, Cambier D. Intrinsic risk factors for the development of patellar tendinitis in an athletic population. Am J Sports Med. 2001;29(2):190–195. doi: 10.1177/03635465010290021201. [DOI] [PubMed] [Google Scholar]
- 11.Lian O, Holen KJ, Engebretsen L, Bahr R. Relationship between symptoms of jumper's knee and the ultrasound characteristics of the patellar tendon among high level male volleyball players. Scand J Med Sci Sports. 1996;6(5):291–296. doi: 10.1111/j.1600-0838.1996.tb00473.x. [DOI] [PubMed] [Google Scholar]
- 12.Cook JL, Khan KM, Harcourt PR, Grant M, Young DA, Bonar SF. A cross sectional study of 100 athletes with jumper's knee managed conservatively and surgically. The Victorian Institute of Sport Tendon Study Group. Br J Sports Med. 1997;31(4):332–336. doi: 10.1136/bjsm.31.4.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kettunen JA, Kvist M, Alanen E, Kujala UM. Long-term prognosis for jumper's knee in male athletes: a prospective follow-up study. Am J Sports Med. 2002;30(5):689–692. doi: 10.1177/03635465020300051001. [DOI] [PubMed] [Google Scholar]
- 14.Gisslén K, Gyulai C, Nordström P, Alfredson H. Normal clinical and ultrasound findings indicate a low risk to sustain jumper's knee patellar tendinopathy: a longitudinal study on Swedish elite junior volleyball players. Br J Sports Med. 2007;41(4):253–258. doi: 10.1136/bjsm.2006.029488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Visentini PJ, Khan KM, Cook JL, Kiss ZS, Harcourt PR, Wark JD. The VISA score: an index of severity of symptoms in patients with jumper's knee (patellar tendinosis). Victorian Institute of Sport Tendon Study Group. J Sci Med Sport. 1998;1(1):22–28. doi: 10.1016/s1440-2440(98)80005-4. [DOI] [PubMed] [Google Scholar]
- 16.Woodley BL, Newsham-West RJ, Baxter GD. Chronic tendinopathy: effectiveness of eccentric exercise. Br J Sports Med. 2007;41(4):188–198. doi: 10.1136/bjsm.2006.029769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Malliaras P, Cook J, Ptasznik R, Thomas S. Prospective study of change in patellar tendon abnormality on imaging and pain over a volleyball season. Br J Sports Med. 2006;40(3):272–274. doi: 10.1136/bjsm.2005.023846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Black J, Cook J, Kiss ZS, Smith M. Intertester reliability of sonography in patellar tendinopathy. J Ultrasound Med. 2004;23(5):671–675. doi: 10.7863/jum.2004.23.5.671. [DOI] [PubMed] [Google Scholar]
- 19.Gellhorn AC, Carlson MJ. Inter-rater, intra-rater, and inter-machine reliability of quantitative ultrasound measurements of the patellar tendon. Ultrasound Med Biol. 2013;39(5):791–796. doi: 10.1016/j.ultrasmedbio.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 20.Del Baño-Aledo ME, Martínez-Payá JJ, Ríos-Díaz J, Mejías-Suárez S, Serrano-Carmona S, de Groot-Ferrando A. Ultrasound measures of tendon thickness: intra-rater, inter-rater and inter-machine reliability. Muscles Ligaments Tendons J. 2017;7(1):92–199. doi: 10.11138/mltj/2017.7.1.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Petrie A, Sabin C. Medical Statistics at a Glance 2nd ed. Malden, MA: Blackwell Publishing; 2005. [Google Scholar]
- 22.Franeschi F, Papalia R, Paciotti M, et al. Obesity as a risk factor for tendinopathy: a systematic review. Int J Endocrinol. 2014;2014:670262. doi: 10.1155/2014/670262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Crossley KM, Thancanamootoo K, Metcalf BR, Cook JL, Purdam CR, Warden SJ. Clinical features of patellar tendinopathy and their implications for rehabilitation. J Orthop Res. 2007;25(9):1164–1175. doi: 10.1002/jor.20415. [DOI] [PubMed] [Google Scholar]
- 24.Brumitt J, Engilis A, Mattocks A, Ellis N, Reyes J. Comparison of jump and hop test measures between NAIA and Division III male collegiate basketball players. Athl Train Sports Health Care. 2018;10(5):208–216. [Google Scholar]
- 25.McAuliffe S, McCreesh K, Culloty F, Purtill H, O'Sullivan K. Can ultrasound imaging predict the development of Achilles and patellar tendinopathy? A systematic review and meta-analysis. Br J Sports Med. 2016;50(24):1516–1523. doi: 10.1136/bjsports-2016-096288. [DOI] [PubMed] [Google Scholar]
- 26.Fietzer AL, Chang YJ, Kulig K. Dancers with patellar tendinopathy exhibit higher vertical and braking ground reaction forces during landing. J Sports Sci. 2012;30(11):1157–1163. doi: 10.1080/02640414.2012.695080. [DOI] [PubMed] [Google Scholar]
- 27.Elvin N, Elvin A, Scheffer C, Arnoczky S, Dillon E, Erasmus PJ. A preliminary study of patellar tendon torques during jumping. J Appl Biomech. 2009;25(4):360–368. doi: 10.1123/jab.25.4.360. [DOI] [PubMed] [Google Scholar]
- 28.Cook JL, Kiss ZS, Khan KM, Purdam CR, Webster KE. Anthropometry, physical performance, and ultrasound patellar tendon abnormality in elite junior basketball players: a cross-sectional study. Br J Sports Med. 2004;38(2):206–209. doi: 10.1136/bjsm.2003.004747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Vries AJ, Koolhaas W, Zwerver J, et al. The impact of patellar tendinopathy on sports and work performance in active athletes. Res Sports Med. 2017;25(3):253–265. doi: 10.1080/15438627.2017.1314292. [DOI] [PubMed] [Google Scholar]


