Abstract
Drawing on discussions at a workshop hosted by the National Cancer Policy Forum, current challenges in pathology are reviewed and practical steps to facilitate high‐quality cancer diagnosis and care through improved patient access to expertise in oncologic pathology are highlighted
Delivery of high‐quality health care depends on accurate and timely diagnosis [1]. In cancer care, diagnostic tests are critical for developing treatment plans and also to inform prognosis, prediction, and assessment of treatment response, disease progression, and recurrence [1], [2]. Pathologists are essential physicians on the oncology care team because they have specialized knowledge to inform diagnostic test selection, performance, and interpretation, as well as communication of results and the implications for subsequent care decisions.
Drawing on discussions at a workshop hosted by the National Cancer Policy Forum [3], we review current challenges in pathology and outline practical steps to facilitate high‐quality cancer diagnosis and care through improved patient access to expertise in oncologic pathology.
Challenges
The development of more sophisticated approaches to diagnostic testing and the growth in precision therapies are transforming cancer diagnosis and care [4], [5]. In the traditional paradigm of pathology testing, a clinician orders diagnostic testing, a clinical laboratory/pathologist performs the ordered tests and returns results, and an individual clinician collates and interprets the information [6]. Now, however, there is an increasingly large, complex, and rapidly expanding menu of diagnostic testing options for clinicians to consider, with few evidence‐based guidelines and limited clinical decision support (CDS) to help with test selection and interpretation. For example, for lung cancer, several molecular, cytogenetic, and immunohistochemical tests serve as companion diagnostics for various targeted therapies. Laboratories have a variety of platform options for a particular test and might apply different outputs and cutoffs for interpretation of results as positive or actionable. Test selection may also vary by histologic subtype, stage of disease, and response to conventional therapy.
Furthermore, complex diagnostic tests generally do not provide yes‐or‐no or discrete numerical results and may have widely accepted reference ranges and thresholds for interpretation. Thus, expert interpretation is essential to inform clinical decisions. New cancer prevention strategies also require knowledge about which cancer detection tests, alone or in combination with primary prevention strategies such as vaccines, are best utilized at which age and how to follow up abnormal test results based on an individual person's risk. Cervical cancer prevention has been a paradigm in this respect [7], [8].
In addition to morphology, diagnostic pathology reports now comprise multiple types of information, such as mRNA expression and genomic DNA data, as well as histology and immunohistochemical results [9]. Molecular testing has added complexity to cancer diagnosis and care by expanding the number of distinct cancer subtypes (e.g., >150 for hematopoietic neoplasms) that can be identified by specific abnormalities and facilitating selection of precision oncology therapies that target those abnormalities in a patient's cancer. This complexity continues to increase as molecular testing has shifted from individual genes to multiplex “omics” panels with hundreds of genes [10]. To maximize the clinical utility of these high dimensional data sets, integrated information management systems are being developed to incorporate structured genomic sequence data into secure, interoperable electronic health record (EHR) platforms [11]. Such systems, which are being deployed in some larger, tertiary care settings, can facilitate incorporation of data into integrated reports, and the results may be discussed in team‐based multidisciplinary tumor boards. However, although widespread implementation of such systems remains an aspirational goal, this paradigm has not yet been implemented in the vast majority of cancer care settings.
No test has perfect sensitivity or specificity, but the diagnostic uncertainty, interobserver variability, and potential for diagnostic errors introduced by the subjective nature of test interpretation are often underappreciated. Gray zones exist in pathology, as in any area of medical practice. Correlation with clinical and radiologic findings and the use of ancillary tests and second reviews can help to improve accuracy and limit nondefinitive diagnosis. For example, one study of second‐opinion surgical pathology reviews found major diagnostic disagreements in 2.3% of cases and minor disagreements in 9.0% of cases [12]. Training and skills may vary among clinicians in different practice settings, and even pathologists who have undertaken subspecialty training in specific areas of pathology might not stay current in that subspecialty if they practice as a “generalist” in nonacademic settings.
Accurately conveying complex diagnostic testing results to patients and clinicians who may be unfamiliar with emerging technologies is also challenging. Accurate, timely diagnosis may be hampered by a lack of interoperability of EHR systems and poor collaboration and communication among pathologists, radiologists, and oncologists on a patient's care team [1].
Disparities in patient access to pathology expertise and technologies can affect the timeliness and accuracy of cancer diagnosis and thus the quality of care patients receive. Smaller community hospitals, especially those in low‐resource areas, may lack pathologists with adequate specialty‐focused training in oncologic pathology as well as ancillary support, equipment, and resources to provide the complex diagnostic testing and interpretation necessary for precision oncology care. Technology innovation can also exacerbate health disparities because care facilities with limited resources may lag behind in technology adoption, creating new inequities in patient care. In addition, many new tests and technologies are expensive and may not be covered by payers initially.
Potential Solutions
Leaders in pathology and the broader health care community need to develop and implement strategies to address these challenges and improve the care of patients with cancer (Box 1). Patient access to expertise in cancer diagnostics could be expanded through improved collaboration among pathologists, radiologists, oncologists, and informaticians; enhanced education and training as well as initial and continuing certification; increased use of expert consultations, including whole‐slide imaging and teleconsultation; and dissemination of appropriate clinical CDS tools.
Box 1. Strategies to improve patient access to high‐quality oncologic pathology.
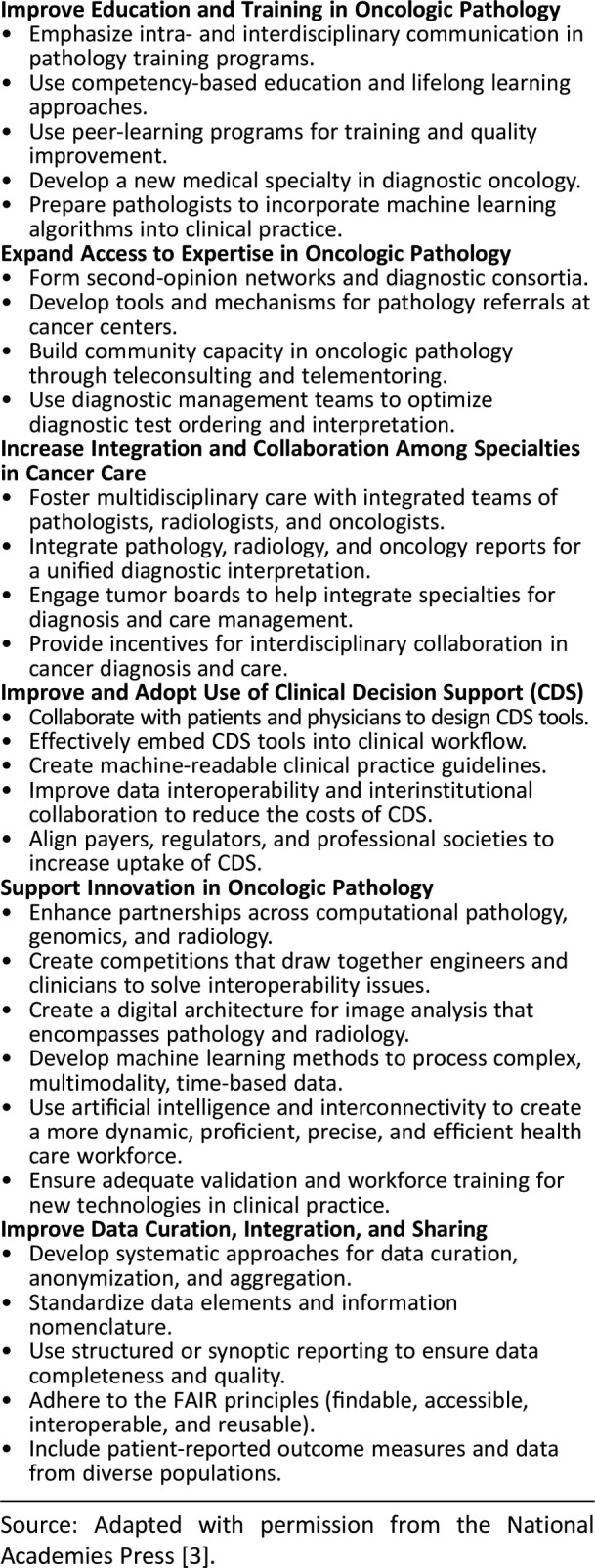
Source: Adapted with permission from the National Academies Press [3].
The growing overlap between the fields of radiology and pathology, along with advances in bioinformatics, represents an opportunity to improve diagnostic oncology. Greater integration of pathology and radiology reports in oncology would provide a more unified and complete interpretation of a patient's disease and the implications for treatment planning and management, as well as for monitoring response to therapy. For example, at the Memorial Sloan Kettering Cancer Center, an integrated report is prepared for bone cancer patients via tumor boards. Increased use of multispecialty tumor conferences is a critical opportunity to promote such interdisciplinary collaboration, but this is a time‐intensive process and requires participation of multiple specialists. Current reimbursement mechanisms and work cultures in clinical settings often do not reward this type of teamwork across specialties or among health care professionals. New payment models, such as the Merit‐Based Incentive Payment System [13], and new informatics technologies could also help incentivize this collaboration and facilitate the integration of patient‐centric diagnostic reports.
Creating a new integrative medical specialty in diagnostic oncology, with training in pathology, radiology, cancer biology, and new computational methods is another opportunity to develop cancer‐specific diagnostic expertise. Developing an overall digital architecture that supports pathology, radiology, and informatics could play a critical role in merging diagnostic training programs. Other changes to education and training could also improve expertise in oncologic pathology. For example, entrustable professional activities, which are observable, measurable units of work that require the integration of many competencies, may correlate better with clinical practice than traditional approaches to training metrics [14], [15]. Recent surveys of pathology residents also indicated that training programs need a greater emphasis on molecular and genomic diagnostics and pathology informatics [16]. Improved methods of ensuring that physicians are staying current with rapid advances in health care, via meaningful continuing certification geared toward “assessment of learning, for learning,” is a priority of the American Board of Medical Specialties and the American Board of Pathology [17], [18].
Nonetheless, pathologists in community practices may not have access to cutting‐edge diagnostic technologies, and it may not always be feasible for them to maintain current knowledge in these rapidly evolving fields. New tools and platforms could enable community clinicians to obtain expert consultation. Telemedicine, as well as clinician‐to‐clinician teleconsulting and telementoring partnerships, can help disseminate knowledge and build capacity in regions lacking specialty or subspecialty medical care [19]. Digitization is changing the field of pathology in ways that will facilitate telemedicine and expert consultations. The U.S. Food and Drug Administration recently approved the first digital pathology system to review and interpret whole‐slide images prepared from biopsied tissue, and some institutions are starting to use real‐time digital pathology strategies, including telepathology, within their institutions as well as for expert consultation outside their systems [20]. This is one potential approach to implementing a recent recommendation to improve the accuracy of pathology reports via second review for selected cases [21].
CDS tools can also help clinicians appropriately order, interpret, and act on diagnostic test results [22]. For example, diagnostic management teams can develop standard test ordering algorithms to reflect the appropriate diagnostic testing for specific diseases. This approach entails a collaboration among experts in diagnostic testing, treating clinicians, and biomedical informaticians to develop and iteratively refine standard test ordering algorithms and then to create a single, evidence‐based, comprehensive report of integrated diagnostic data to guide treatment and disease monitoring [23].
Applications of artificial intelligence (AI) could help clinicians overcome cognitive overload from diagnostic information. In the case of digital pathology, AI can also highlight areas of interest in a specimen so that pathologists can focus more attention on potentially invasive or metastatic lesions. A recent study found that some deep‐learning algorithms can effectively detect lymph node metastases in women with breast cancer [24]. Digitization in pathology will also enable compilation of large digital pathology data sets that can be analyzed with AI to facilitate development and validation of computational diagnostic methods.
With the evolution of precision oncology, the essential role for precise diagnostics to guide care management decisions is growing. The potential for harm when patients lack access to high‐quality oncologic pathology and integrated diagnostics cannot be ignored. Policy makers and leaders in pathology and oncology should take action to address these critical gaps in cancer care.
Acknowledgments
We thank the speakers and participants for their contributions to the workshop. The activities of the National Cancer Policy Forum are supported by its sponsoring members, which currently include the Centers for Disease Control and Prevention, the National Institutes of Health/National Cancer Institute, the American Association for Cancer Research, the American Cancer Society, the American College of Radiology, the American Society of Clinical Oncology, the Association of American Cancer Institutes, the Association of Community Cancer Centers, Bristol‐Myers Squibb, the Cancer Support Community, the CEO Roundtable on Cancer, Flatiron Health, Helsinn Therapeutics (U.S.) Inc., the LIVESTRONG Foundation, Merck, the National Comprehensive Cancer Network, Novartis Oncology, the Oncology Nursing Society, and Pfizer Inc. The responsibility for the content of this article rests with the authors and does not necessarily represent the views of the National Academies of Sciences, Engineering, and Medicine, its committees, its sponsors, or its convening activities.
Disclosures
Sharyl J. Nass: National Cancer Policy Forum (RF); Ritu Nayar: American Board of Pathology (C/A); Erin P. Balogh: National Cancer Policy Forum (RF), Bristol‐Myers Squibb, Flatiron Health, Helsinn Therapeutics, Merck, Novartis Oncology, Pfizer (RF—institutional); Richard L. Schilsky: AstraZeneca, Bayer, Bristol‐Myers Squibb, Genentech, Eli Lilly & Co., Merck, Pfizer (RF—institutional); Hedvig Hricak: IBA (SAB). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1.Institute of Medicine . Improving Diagnosis in Health Care. Washington, D.C.: National Academies Press; 2015. [PubMed] [Google Scholar]
- 2.Harris TJ, McCormick FJ. The molecular pathology of cancer. Nat Rev Clin Oncol 2010;7:251–265. [DOI] [PubMed] [Google Scholar]
- 3.National Academies of Sciences, Engineering, and Medicine . Improving Cancer Diagnosis and Care: Patient Access to Oncologic Imaging and Pathology Expertise and Technologies: Proceedings of a Workshop. Washington, D.C.: National Academies Press; 2018. [PubMed] [Google Scholar]
- 4.Lowy DR, Collins FS. Aiming high—changing the trajectory for cancer. N Engl J Med 2016;374:1901–1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Institute of Medicine . Biomarker Tests for Molecularly Targeted Therapies: Key to Unlocking Precision Medicine. Washington, D.C.: National Academies Press; 2016. [PubMed] [Google Scholar]
- 6.Seegmiller AC, Kim AS, Mosse CA et al. Optimizing personalized bone marrow testing using an evidence‐based, interdisciplinary team approach. Am J Clin Pathol 2013;140:643–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vaccine recommendations and Guidelines of the ACIP: HPV. Centers for Disease Control and Prevention Web site. Available at https://www.cdc.gov/vaccines/hcp/acip‐recs/vacc‐specific/hpv.html. Updated November 21, 2014. Accessed March 8, 2019.
- 8.Schiffman M, Wentzensen N, Khan MJ et al. Prepare for the next round of ASCCP‐sponsored cervical screening and management guidelines. J Low Genit Tract Dis 2017;21:87–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Louis DN, Feldman M, Carter AB et al. Computational pathology: A path ahead. Arch Pathol Lab Med 2016;140:41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Institute of Medicine . Evolution of Translational Omics: Lessons Learned and the Path Forward. Washington, D.C.: National Academies Press; 2012. [PubMed] [Google Scholar]
- 11.Masys DR, Jarvik GP, Abernethy NF et al. Technical desiderata for the integration of genomic data into Electronic Health Records. J Biomed Inform 2012;45:419–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manion E, Cohen MB, Weydert J. Mandatory second opinion in surgical pathology referral material: Clinical consequences of major disagreements. Am J Surg Pathol 2008;32:732–737. [DOI] [PubMed] [Google Scholar]
- 13.MIPS overview. CMS, 2019. Centers for Medicare and Medicaid Services Web site. Available at https://qpp.cms.gov/mips/overview. Accessed March 8, 2019.
- 14.ten Cate O. Entrustability of professional activities and competency‐based training. Med Educ 2005;39:1176–1177. [DOI] [PubMed] [Google Scholar]
- 15.ten Cate O. Nuts and bolts of entrustable professional activities. J Grad Med Educ 2013;5:157–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Black‐Schaffer WS, Gross DJ, Crawford JM et al. Evidence‐based alignment of pathology residency with practice: Methodology and general consideration of results. Acad Pathol 2018;5:2374289518790501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.ABPath CertLink ‐ General overview. American Board of Pathology Web site. Available at www.abpath.org/index.php/abpath-certlink. Accessed March 8, 2019.
- 18.CertLink delivers longitudinal assessment online. American Board of Medical Specialties Web site. Available at https://www.abms.org/initiatives/certlink-platform-and-pilot-programs/. Accessed March 8, 2019.
- 19.Arora S, Thornton K, Murata G et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med 2011;364:2199–2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Volynskaya Z, Chow H, Evans A et al. Integrated pathology informatics enables high‐quality personalized and precision medicine: Digital pathology and beyond. Arch Pathol Lab Med 2017;142:369–382. [DOI] [PubMed] [Google Scholar]
- 21.Nakhleh RE, Nosé V, Colasacco C et al. Interpretive diagnostic error reduction in surgical pathology and cytology: Guideline from the College of American Pathologists Pathology and Laboratory Quality Center and the Association of Directors of Anatomic and Surgical Pathology. Arch Pathol Lab Med 2016;140:29–40. [DOI] [PubMed] [Google Scholar]
- 22.Khorasani R, Hentel K, Darer J et al. Ten commandments for effective clinical decision support for imaging: Enabling evidence‐based practice to improve quality and reduce waste. AJR AM J Roentgenol 2014;203:945–951. [DOI] [PubMed] [Google Scholar]
- 23.Seegmiller AC, Kim AS, Mosse CA et al. Data‐driven iterative refinement of bone marrow testing protocols leads to progressive improvement in cytogenetic and molecular test utilization. Am J Clin Pathol 2016;146:585–593. [DOI] [PubMed] [Google Scholar]
- 24.Bejnordi BE, Veta M, Van Diest PJ et al. Diagnostic assessment of deep learning algorithms for detection of lymph node metastases in women with breast cancer. JAMA 2017;318:2199–2210. [DOI] [PMC free article] [PubMed] [Google Scholar]


