Abstract
Introduction
Labial frenectomy is a common procedure in the oral surgery specialty. Nowadays, laser surgery seems to provide better post-operative results than scalpel surgery. Thus, the aim of this study was to analyze whether trans-surgical and postoperative variables of labial frenectomy are better when performed with laser than with conventional scalpel.
Materials and Methods
A systematic review has been performed based on PRISMA criteria. The search included three databases, with no limitations of time or language. After screening, seven papers were included in qualitative analysis and six in meta-analysis. Bias analysis was performed according to Cochrane Handbook. Pain during the first (MD − 3.18, 95% CI − 4.03 to − 2.32) and seventh post-surgical days (MD − 1.04, 95% CI − 1.45 to − 0.64); discomfort during speech on the first (MD − 2.15, 95% CI − 3.94 to − 0.37) and the seventh post-surgical days (MD − 1.60, 95% CI − 1.96 to − 1.24); discomfort during chewing on the first (MD − 2.90, 95% CI − 3.35 to − 2.45) and the seventh days (MD − 1.56, 95% CI − 2.21 to − 0.91); and average surgery time (MD − 1.84, 95% CI − 3.22 to − 0.46) were lower in the laser group than in the scalpel group.
Conclusion
The results of this systematic review have shown better results to laser group in the following variables: pain, discomfort during speech and chewing. However, the evidence is limited due the high risk of bias.
Keywords: Labial frenectomy, Labial frenulum, Laser, Laser surgery, Oral surgery
Introduction
The labial frenal attachment is a fibrous tissue covered with mucosa that comes from the lip and cheek to the alveolar periosteum [1]. Generally, labial frenal attachments do not present problems, but in some circumstances the presence of an abnormal attachment can become a hindrance. Frenectomy is a surgical procedure that aims to eliminate excessive interdental tissue and reduce the tension of marginal gingiva tissues [2]. There are many discussions about the usefulness of labial frenectomy. However, this procedure is indicated in some situations such as diastema, gingival recession, difficulties in oral hygiene, interference in labial movements, and prosthetic needs [3, 4]. After the lip frenectomy procedure, as in many oral surgical procedures, pain, discomfort, edema, and bleeding are common complications [5, 6]. Once the need for a lip frenectomy is determined, there are multiple effective surgical techniques used to perform it. Among those are the simple excision technique, using the scalpel, and laser-assisted frenectomy [7].
There are several types of lasers that have been used in dentistry, including the neodymium-doped yttrium aluminum garnet (Nd:YAG), the diode, carbon dioxide (CO2), erbium-doped yttrium aluminum garnet laser (Er: YAG), and the erbium, chromium: yttrium: scandium gallium-garnet (Er, Cr: YSGG) laser [8]. Each one emits light at a specific wavelength that is determined by the gain medium (solid, liquid, or gas). Laser treatment is indicated for some oral tissue procedures, such as frenectomies, gingivectomies, gingivoplasties, operculum removal, and biopsies of benign lesions [7].
One of the main benefits of using dental lasers is the ability to interact selectively and precisely with diseased tissues. This characteristic can explain the lesser degree of injury to the surrounding tissue, no significant complications, limited scarring and contraction, and probable biostimulation effect of the laser [9]. Because lasers provide excellent hemostasis, the need for suturing is significantly reduced. Some lasers can even be used to attach the edges of tissue together, and this itself provides less need for suturing [10]. Furthermore, lasers are used in surgery because they can execute precise surgical incisions and offer hemostatic control. The results of laser interaction depend on the type of laser used and the targeted tissue [4].
Despite the literature indicating that the clinical standards of patients submitted to labial frenectomies with an Nd:YAG laser are consistently superior to those of conventional techniques, comparative studies are still scarce [11]. Thus, the aim of this study was to compare whether trans-surgical and post-operative variables of labial frenectomy are better when performed with laser than with conventional scalpel.
Methods
This review was performed based on PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analysis) [12]. As this study is a systematic review of the literature, ethical committee approval was not necessary once it was established that neither human beings nor animals were involved.
Focused PICOS Question
The outcomes, pain, bleeding, time spent to perform the surgery, suture necessity, analgesics consumption, discomfort during speaking and chewing formed the parameter to determine the following PICO question:
Is laser more effective than conventional scalpel to perform incisions during labial frenectomy?
P (Population)—People who underwent labial frenectomy.
I (Intervention)—The use of laser technique to perform labial frenectomy
C (Comparison)—The use of a conventional scalpel to perform labial frenectomy.
O (Outcome)—Laser technique is more effective than conventional scalpel for the following variables: pain, bleeding, time spent to perform the surgery, suture necessity, analgesics consumption, discomfort during speaking and chewing.
S (Type of study)—Randomized or quasi-randomized controlled clinical trials.
Search Strategy
The search for the articles was performed in the following databases: PubMed (https://www.ncbi.nlm.nih.gov/pubmed), VHL—Virtual Health Library—LILCAS, IBECS, MEDLINE, The Cochrane Library and Scielo (http://bvsalud.org/), Web of Science (http://webofknowledge.com), and OVID (http://ovidsp.ovid.com/). For each database, three search steps were performed (Chart I). The grey literature was also searched for relevant ongoing trials in Google Scholar.
Eligibility Criteria
Eligibility criteria were determined before screening the articles. The following inclusion criteria were adopted: randomized clinical trials, clinical trials, and comparative studies that compared the use of lasers and scalpels to perform labial frenectomy. The exclusion criteria included: studies that considered only one of the techniques (laser only or scalpel only), patients with systemic diseases (bleeding disorders, continuous use of medicines, arterial hypertension, diabetes of metabolic diseases), observational studies, case reports, technical notes, letters to the editor, abstracts, and papers indexed in databases with no abstracts and case series.
Study Selection
The study selection was performed with a rigid protocol fulfilled by two independent authors (ACRP and ELG). Firstly, the authors read the title and abstract. At this moment, the articles that did not fulfill the inclusion criteria were excluded. The articles that did fulfill inclusion criteria were selected for reading in full. After reading the full papers, differences in opinion about inclusion and exclusion of the papers were solved by consent between authors. When an agreement could not be reached, a third author gave a decision vote.
Data Extraction and Meta-analysis
The following data were extracted from the papers after they were elected to be included in this review: (1) author and year of publication, (2) country of publication, (3) study design, (4) type of laser used, (5) sample size for each group, (6) total sample size, (7) follow-up days, (8) sample age in intervention groups, and (9) gender (Table 1). Furthermore, the following clinical data were also extracted for each group: (1) trans-operative bleeding, (2) suture necessity, (3) analgesic consumption, (4) surgical time, (5) pain on the first post-operative day, (6) pain on the seventh post-operative day, (7) discomfort during speaking on the first post-operative day, (8) discomfort during speaking on the seventh post-operative day, (9) discomfort during chewing on the first post-operative day, (10) discomfort during chewing on the seventh post-operative day, and (11) fear (Table 2). When papers provided insufficient data for inclusion in the analysis, the first or corresponding authors were contacted to determine whether additional data could be provided.
Table 1.
Characteristics of the studies included in the systematic review
| References | Country | Study design | Tipo de laser | Scalpel (n) | Laser (n) | Sample | Follow-up (days) | Age (mean, years) | Gender | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Scalpel | Laser | Female | Male | ||||||||
| Patel et al. [16] | India | RCT | Diode laser | 10 | 10 | 20 | 90 | 32.4 ± 7.75 | 12 | 8 | |
| Akpınar et al. [7] | Turkey | RCT | Nd:YAG | 44 | 45 | 89 | 7 | 28.75 ± 11.32 | 29.75 ± 11.58 | 51 | 38 |
| Butchibabu et al. [17] | India | RCT | Diode laser | 5 | 5 | 10 | 7 | 18–30 | 4 | 6 | |
| Medeiros Jr et al. [11] | Brazil | Intervention study | Nd:YAG | 22 | 18 | 40 | 15 | 20.7 ± 9.4 | 21.2 ± 11.5 | 24 | 16 |
| Kara [18] | Turkey | RCT | Nd:YAG | 20 | 20 | 40 | 7 | 16.2 ± 1.9 | 16.7 ± 2.3 | 16 | 24 |
| Janas [6] | Poland | Intervention study | CO2 laser | 52 | 66 | 118 | – | 5–58 | 5–62 | NR | NR |
| Haytac et al. [5] | Turkey | Intervention study | CO2 laser | 20 | 20 | 40 | 7 | 18–26 | 18–26 | 24 | 16 |
Table 2.
Treatment characteristics and outcomes
| References | Trans -operative bleeding | Suture n (%) | Analgesic consumption n (%) | Surgical time** | Pain first day** | Pain seventh day** | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| L | S | L | S | L | S | L | S | L | S | L | S | |
| Patel et al. [16] | 0.25 ± 0.46 | 2.37 ± 0.51 | NR | NR | 1.87 ± 0.83* | 4.25 ± 0.7* | NR | NR | 2.25 ± 1.035 | 4.87 ± 1.24 | 0.375 ± 0.51 | 2.25 ± 1.83 |
| Akpınar et al. [7] | NR | NR | No | Yes | NR | NR | 8.84 ± 3.11 | 9.93 ± 3.32 | 1 ± NR | 2 ± NR | 0 ± NR | 0 ± NR |
| Butchibabu et al. [17] | NR | NR | No | Yes | 1 (20) | 3 (60) | NR | NR | 6.5 ± 0.43 | 8.76 ± 5.59 | 1.38 ± 0.38 | 3.7 ± 0.46 |
| Medeiros Jr et al. [11] | Absent 17(94.4%) | Absent 0 | No | Yes | 13 (72.2) | 16 (72.7) | 7.7 ± 1.9 | 10.2 ± 1.8 | NR | NR | NR | NR |
| Scarce 1 (5.6%) | Scarce 11 (50%) | |||||||||||
| Abundant 0 | Abundant 11(50%) | |||||||||||
| Kara [18] | No | Yes | No | Yes | 2 (5.0) | 37 (92.5) | NR | NR | 1.46 ± 0.98 | 5.38 ± 0.55 | 0.15 ± 0.33 | 1.14 ± 0.97 |
| Janas [6] | No | Yes | No | Yes | NR | NR | NR | NR | NR | NR | NR | NR |
| Haytac et al. [5] | NR | NR | No | Yes | 7 (33.3) | 17 (85) | NR | NR | 3.4 ± 1.1 | 6.2 ± 1.8 | 0.1 ± 0.3 | 3.3 ± 1.5 |
| References | Discomfort speaking first day** | Discomfort speaking seventh day** | Discomfort chewing first day** | Discomfort chewing seventh day** | Fear | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| L | S | L | S | L | S | L | S | L | S | |
| Patel et al. [16] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Akpınar et al. [7] | 1 ± NR | 1 ± NR | 0 ± NR | 0 ± NR | 0 ± NR | 1 ± NR | 0 ± NR | 0 ± NR | NR | NR |
| Butchibabu et al. [17] | 5.38 ± 0.48 | 8.18 ± 0.49 | 0.74 ± 0.24 | 2.10 ± 0.29 | 5.38 ± 0.48 | 8.18 ± 0.49 | 0.74 ± 0.24 | 2.10 ± 0.29 | NR | NR |
| Medeiros Jr et al. [11] | NR | NR | NR | NR | NR | NR | NR | NR |
Mild 04 (22.2) Moderate 14 (77.8) Severe 0 |
Mild 06 (27.3) Moderate 15 (68.2) Severe 01 (4.5) |
| Kara [18] | 2.51 ± 0.69 | 3.01 ± 0.77 | 0.04 ± 0.36 | 1.98 ± 0.69 | 1.99 ± 0.45 | 4.65 ± 0.57 | 0.07 ± 0.25 | 1.14 ± 0.78 | 6.45 ± 0.88 | 6.67 ± 0.64 |
| Janas [6] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Haytac et al. [5] | 0.8 ± 0.7 | 4.0 ± 1.4 | 0.1 ± 0.2 | 1.6 ± 0.9 | 1.7 ± 0.9 | 5.2 ± 1.4 | 0.1 ± 0.3 | 2.4 ± 1.0 | NR | NR |
L Laser, S Scalpel and NR Not related
*Number of analgesic; **Mean VAS ± SD
The software R was used for meta-analysis. The packages “meta” and “metafor” were activated to perform the meta-analysis. The heterogeneity of the results was assessed using the I2 test [13]. When homogeneity was present (I2 = 0.00), the fixed effect model was used for performing meta-analysis and forest plot. When heterogeneity was present (I2 > 0.00), the random effect model was used. For continuous variables, differences between averages were assessed. For the analgesic consumption variable, the odds ratio (OR) was assessed. Risk measures, 95% confidence interval (CI), and p value were described in forest plots.
Risk of Bias (Quality) Assessment
The quality of included studies was assessed by two reviewers (ELG and SGMF) using the Cochrane Collaboration’s tool for assessing risk of bias [14]. The criteria were divided into five main domains. For each study, these criteria were rated as exhibiting low, unclear, or high risk of bias. For the final classification of risk of bias, disagreements between reviewers were resolved by consensus. Blinding of the evaluators and patients is not possible in this type of intervention study, which requires a surgical procedure to be performed. Therefore, to judge the blindness, the studies considered as “low risk” were the ones in which the variables depended only on patients reports, and “high risk” studies were those that considered the perception of the evaluator, such as the amount of trans-operative bleeding. Regarding the ethical aspects, those studies that mentioned the consent of the participants but did not report on the submission of the work to the judgment of an ethics committee were considered to have “unclear risk.” When evaluating selective reporting, a description of some variable data collection with no results displayed was considered “high risk.”
Results
Study Selection
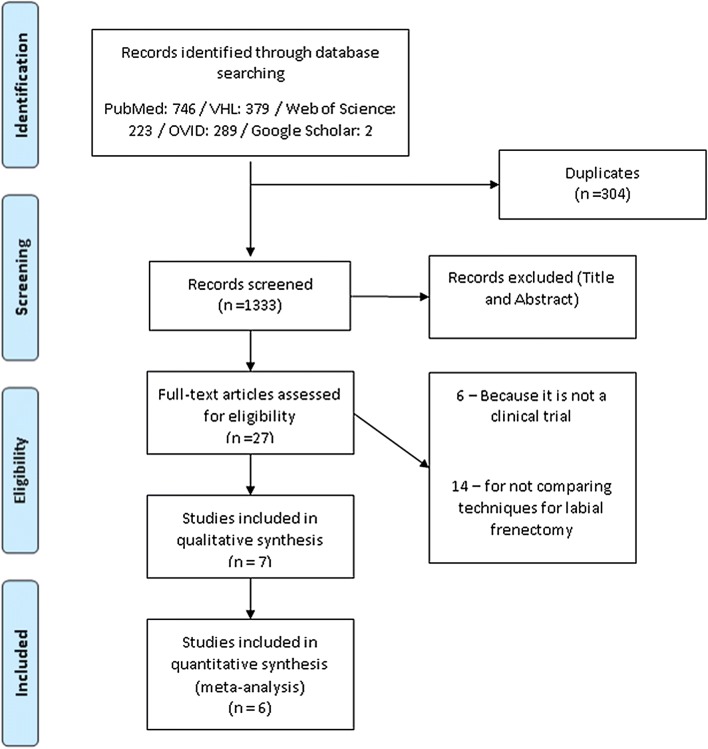
The literature search resulted in the identification of 1639 studies. After screening titles and abstracts by three reviewers, we retrieved 27 full-text studies. The reference lists of selected papers and hand search revealed no additional relevant paper.
A total of seven studies were included in the qualitative synthesis, and six were included in the meta-analysis. The process of study selection and the reasons for exclusion are summarized in (Fig. 1). One study was not included in the global meta-analysis due to the absence of evaluation of the same variables [6]. It was possible to include in the meta-analysis the variables analgesic consumption, pain and discomfort during speech and chewing, which were assessed during the first and seventh post-operative days. Even though the pain variable was reported by two authors, it was not presented in the same way, disallowing its inclusion in the meta-analysis.
Fig. 1.
PRISMA flowchart showing the article selection process
Study Characteristics
The main characteristics of the included studies and of the patients are presented in Table 1.
Among included studies, four were randomized trials [7, 15–17], one reported no randomization [11], and two were intervention studies with no description of randomization [5, 6, 11]. Three of the selected studies were conducted in Turkey [5, 7, 15], one in Brazil [11], two in India [16, 17], and one in Poland [6]. The average age of participants of studies varied from 16.2 [15] to 32.4 years [7]. The Nd:YAG laser was utilized in three studies [7, 11, 15], CO2 [5, 6] and diode laser [16, 17] were each used in two studies.
The summarized treatment characteristics and outcomes are shown in Table 2. Six studies reported having used local anesthesia during frenectomy [6, 7, 11, 15–17]. One study reported having considered surface anesthesia, infiltration anesthesia, number of anesthetics used, surgical technique, bleeding during surgery, pain during and after surgery, suturing, surgery duration, post-operational swelling, wound healing, necessity to be operated on again, potential swallowing of oral vestibule, and patient’s personal feelings [6]. However, these results were unavailable.
Most articles reported pain while chewing and speaking using the visual analogic scale [7, 11, 15–17].
Although Medeiros Jr et al. [11] mention the collection of variables of pain and discomfort for oral functions, these results appear synthesized in the fear variable. This study reports pain reduction and optimization of speech in patients operated on with a conventional scalpel on the third post-operative day. It does not present the found results, most likely because the researchers did not value the intervention of interest (laser). This study also reports that the discomfort in mastication was similar among the groups.
The post-operative bleeding variable was cited by only two authors [7, 11]. Akpınar et al. [7] report that there was no post-operative bleeding in either group.
Medeiros Jr et al. [11] show that three patients (7.5%) experienced post-surgical complications. One patient treated with conventional surgery presented mild post-operative hemorrhage. Two patients treated with the Nd:YAG laser developed superficial bone exposure in the attached gingiva [11].
A study selected patients with both maxillary and mandibular labial frenums in which two different techniques were used on the same patient. They divided patients into two groups: Group 1 included 20 patients (the first labial frenum was treated with conventional surgery, and 1 week later the other frenum was treated with Nd:YAG laser surgery); group 2 also included 20 subjects (first, one labial frenum was treated with Nd:YAG laser surgery, and 1 week later the other frenum (maxillary or mandibular) was treated with conventional surgery) [15]. For this meta-analysis, we considered the results related to the first intervention of each patient.
Quality and Risk of Bias Assessment
The consensus judgments by the authors for the domains of risk of bias for studies included in the systematic review are given in Table 3. Risk of bias was unclear in 40% of all items across studies. Similarly, risk was low in 40% and was high in 20% of all items. The risk of bias for blindness, according to our analysis, was considered high in 40% of the studies.
Table 3.
Quality evaluation studies
| Criteria | Studies | ||||||
|---|---|---|---|---|---|---|---|
| Patel et al. [16] | Akpınar et al. [7] | Butchibabu et al. [17] | Medeiros Jr et al. [11] | Kara [18] | Janas [6] | Haytac et al. [5] | |
| Concealment of treatment allocation | Low risk | Unclear risk | Unclear risk | High risk | High risk | Unclear risk | Unclear risk |
| Double-blind | High risk | Low risk | Low risk | High risk | High risk | Unclear risk | Low risk |
| Incomplete outcome data (attrition bias) | Unclear risk | Unclear risk | Unclear risk | Unclear risk | Unclear risk | Unclear risk | Unclear risk |
| Selective reporting (reporting bias) | Low risk | Low risk | Low risk | High risk | Low risk | High risk | Low risk |
| Ethical criteria | Low risk | Low risk | Unclear risk | Low risk | Low risk | Unclear risk | Low risk |
Meta-analysis Results
Intra-operative bleeding was assessed in four studies [6, 11, 15, 16]. However, each author evaluated this variable in a different way, making it impossible for us to complete the meta-analysis. In all groups that used the conventional scalpel technique, post-operative bleeding was observed. There was no need for suturing labial frenectomies performed by a laser, while surgeries performed with conventional scalpel required suture in most studies [5–7, 11, 15]. Pain and discomfort during speech and chewing were analyzed during the first and seventh days, using a visual analog scale with values ranging from 1 to 10. Fear was evaluated by two studies included in this meta-analysis [11, 15]. It was also not possible to perform meta-analysis of this variable due to heterogeneity among the measurement methods used.
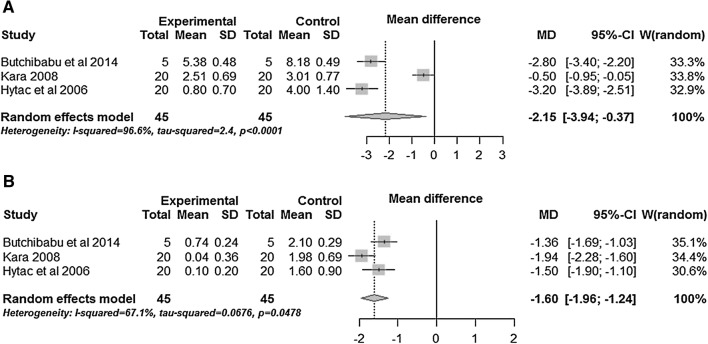
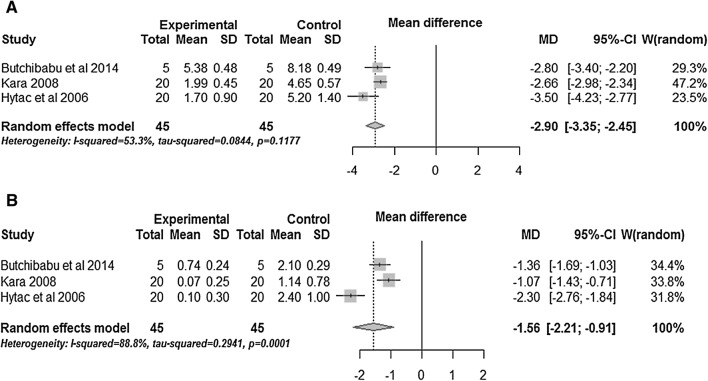
The pain variable, assessed on the first post-operative day (POD), was significantly lower in groups that underwent frenectomy with laser compared with the technique using the conventional scalpel (MD − 3.18, 95% CI − 4.03 to − 2.32). This difference was also found on the seventh post-operative day (MD − 1.04, 95% CI − 1.45 to − 0.64) (Fig. 2). In relation to discomfort during speech on the first post-operative day post-operative, the laser group showed better results with a reduction in average discomfort (MD − 2.15, 95% CI − 3.94 to − 0.37), as well as on the seventh day after surgery (MD − 1.60, 95% CI − 1.96 to − 1.24) (Fig. 3). Discomfort while chewing on the first day after surgery was significantly lower in the group operated on with a laser (MD − 2.90, 95% CI − 3.35 to − 2.45) and on the seventh post-operative day (MD − 1.56 95% CI − 2.21 to − 0.91) (Fig. 4). The average time of surgery was also reduced when the frenectomy was performed with a laser (MD − 1.84, 95% CI − 3.22 to − 0.46). There was no significant difference regarding analgesic consumption among groups (OR 12:09, 95% CI 0:01 to 1:01).
Fig. 2.
a Box plots comparing the variable pain between laser and scalpel 1 day after the post-operative. b Box plots comparing variable pain between laser and scalpel 7 days after the post-operative
Fig. 3.
a Box plots comparing the variable discomfort during speech between laser and scalpel on the first day after the post-operative. b Box plots comparing the variable discomfort during speech between laser and scalpel on the seventh day after the post-operative
Fig. 4.
a Box plots comparing the variable discomfort while chewing between laser and scalpel on the first day after the post-operative. b Box plots comparing the variable discomfort while chewing between laser and scalpel on the seventh day after the post-operative
Discussion
The incorporation of less invasive methods to minimize the pain and discomfort of the patient during and after operations has been evolving in dentistry [18]. Therefore, the use of lasers in dental surgery is already established as an effective and reliable option [19]. This review showed that the groups in which frenectomies were performed using laser showed better results than those who underwent the conventional technique with a scalpel. The variables measured included surgical time, pain, discomfort while chewing on the first and seventh post-operative days, and discomfort during speech on the first and seventh post-operative days.
The use of a high-intensity laser presents significant advantages for performing oral surgical procedures, including the ability to cut while performing hemostasis and coagulation [20], and significant reduction in the need for sutures [10]. The use of this technique in the studies included in this review avoided the need for sutures and the presence of trans-operative bleeding in 100% of the cases.
The meta-analysis showed a significant difference in discomfort during speech (first and seventh post-operative days) and during mastication (first and seventh post-operative days) between the groups submitted to labial frenectomy with a laser or conventional scalpel. This can be explained by the accuracy of surgical procedures performed with a laser. There are no major adverse effects on the surrounding tissues. In addition, the laser could seal lymphatic and nerve ending channels, which reduced post-operative swelling and the inflammatory response [9].
Among the advantages of laser-assisted surgery are the possibility of reducing or avoiding the use of analgesics and reducing post-operative pain [20, 21]. Reduction in post-operative pain (first and seventh post-operative days) was significantly different among groups, and it was lower in groups that underwent frenectomy with a laser. Although the use of a surgical laser has shown a reducing effect of the analgesic consumption compared with the use of conventional scalpel, this difference was not significant in the meta-analysis.
It was not possible to perform meta-analysis for the “fear” variable because of the heterogeneity among the assessment methods used. However, none of the studies that assessed this variable found a significant difference between the groups operated on with a laser or conventional scalpel [11, 15]. Because the patients usually have no prior experience with either procedure, it is justifiable that there is no difference between the fear experienced by patients prior to the frenectomy in both techniques.
The fact that the average operating time was significantly shorter in the meta-analysis when frenectomy was performed with a laser might be related to laser energy. Lasers can make incisions in the tissue without causing bleeding and without the need for sutures which allows for a simple and fast outpatient procedure [12].
Despite these findings, most of the studies included in this review were methodologically limited by some degree of bias. Only one study presented a description of a randomized sequence and allocation concealment of patients, yet this seemed to be inappropriate [15]. Some studies have not reported intended results in the method, such as pain and discomfort, which restricted the comparison. Another limitation is related to the size of samples, ranging from 10 to 118 participants. It should be noted that three of the seven studies used a sample of 40 participants, highlighting the need for further studies with greater scientific rigor. In addition, none of the studies reported the sample calculation for setting of the sample size. Moreover, the blinding in this type of study was impaired because the surgical technique could not be masked for the surgeon and could be recognized by the participants. These situations can lead to an induced response by operators and participants because they can think that more modern technique may be better than older or vice versa.
Considering the small number of studies included in this analysis, subgroup analysis was not possible in relation to the type of laser used (Nd:YAG and CO2). These two types of lasers are different regarding the biological effect on tissues. Thus, post-operative complications can be different between them. For this reason, the authors recognize it as a great limitation of this review. The types of lasers and their indications and limitations should be known by the professionals that use them within dental surgery [22]. The heterogeneity of the results of meta-analysis calculated using the I2 ranged from 25.4 to 96.6%. These results can be attributed to the different types of lasers included in these analyses, which shows that the results of this meta-analysis should be interpreted with caution.
The few studies included also prevented the completion of the Egger test for publication bias analysis, as well as the use of the funnel plot. However, the non-indexed literature (Opengrey) was consulted, minimizing the chance of such bias. In this consultation, were found two non-indexed articles, and they were included in this review [16, 17]. As strengths of this meta-analysis, we highlight the lack of restriction for search of publications only in English, and the theme originality, gathering all the studies that compared the use of a laser and a conventional scalpel in labial frenectomies. A protocol was used to guide the search strategy, study selection, and data collection. However, the strength of evidence of this review was shaken by the low methodological quality of the studies included and the heterogeneity of the results. More research is needed and with better methodological quality to either corroborate or refute these findings.
This systematic review suggests that labial frenectomies performed with high-intensity surgical lasers are faster and offer better prognosis in terms of pain and discomfort during speech and chewing, than those performed with conventional scalpels. However, these results should be viewed with caution because of the high risk of bias found. Therefore, there is still insufficient evidence to conclude that the use of lasers is better than the use of conventional scalpels in frenectomies. Other randomized trials using the two techniques are necessary to allow the dentist to safely choose between either of the techniques.
Acknowledgements
Endi Lanza Galvão would like to thank FAPEMIG—Fundação de Amparo a Pesquisa do Estado de Minas Gerais for her Ph.D. scholarship.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mishima K, Shiraishi M, Kawai Y, Harada K, Ueyama Y. Frenum-like synechiae of the lip and vestibule. Oral Maxillofac Surg. 2016;20:219–222. doi: 10.1007/s10006-015-0544-z. [DOI] [PubMed] [Google Scholar]
- 2.Chaubey KK, Arora VK, Thakur R, Narula IS. Perio-esthetic surgery: using LPF with frenectomy for prevention of scar. J Indian Soc Periodontol. 2015;15:265–269. doi: 10.4103/0972-124X.85672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gontijo I, Navarro RS, Naypek P, Ciamponi AL, Haddad AE. The application of diode and Er:YAG lasers in labial frenectomies in infants. J Dent Child. 2005;72:10–15. [PubMed] [Google Scholar]
- 4.Olivi G, Chaumanet G, Genovese MD, Beneduce C, Andreana S. The Er, Cr:YSGG laser labial frenectomy: a clinical retrospective evaluation of 156 consecutive cases. Gen Dent. 2010;58:e-126–e-133. [PubMed] [Google Scholar]
- 5.Haytac MC, Ozcelik O. Evaluation of patient perceptions after frenectomy operations: a comparison of carbon dioxide laser and scalpel techniques. J Periodontol. 2006;77:1815–1819. doi: 10.1902/jop.2006.060043. [DOI] [PubMed] [Google Scholar]
- 6.Janas A (2007) Use of carbon dioxide laser in frenuloplasty of upper and lower lip and tongue. In: Proceedings of SPIE 6598, laser technology VIII: applications of lasers, p 659805–1
- 7.Akpınar A, Toker H, Lektemur Alpan A, Çalışır M. Postoperative discomfort after Nd:YAG laser and conventional frenectomy: comparison of both genders. Aust Dent J. 2016;61:71–75. doi: 10.1111/adj.12333. [DOI] [PubMed] [Google Scholar]
- 8.Aoki A, Sasaki KM, Watanabe H, Ishikawa I. Lasers in nonsurgical periodontal therapy. Periodontology. 2004;36:59–97. doi: 10.1111/j.1600-0757.2004.03679.x. [DOI] [PubMed] [Google Scholar]
- 9.Aldelaimi TN, Khalil AA. Clinical application of diode laser (980 nm) in maxillofacial surgical procedures. J Craniofac Surg. 2015;26:1220–1223. doi: 10.1097/SCS.0000000000001727. [DOI] [PubMed] [Google Scholar]
- 10.Garg N, Verma S, Chadha M, Rastogi P. Use of carbon dioxide laser in oral soft tissue procedures. Natl J Maxillofac Surg. 2015;6:84–88. doi: 10.4103/0975-5950.168218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Medeiros R, Jr, Gueiros LA, Silva IH, de Albuquerque Carvalho A, Leao JC. Labial frenectomy with Nd:YAG laser and conventional surgery: a comparative study. Lasers Med Sci. 2015;30:851–856. doi: 10.1007/s10103-015-1764-z. [DOI] [PubMed] [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Götzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analysis of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 13.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 14.Higgins JPT, Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration
- 15.Kara C. Evaluation of patient perceptions of frenectomy: a comparison of Nd: YAG laser and conventional techniques. Photomed Laser Surg. 2008;26:147–152. doi: 10.1089/pho.2007.2153. [DOI] [PubMed] [Google Scholar]
- 16.Patel RM, Varma S, Suragimath G, Abbayya K, Zope AS, Vishwajeet K. Comparison of labial frenectomy procedure with conventional surgical technique and diode laser. J Dent Lasers. 2015;9:94–99. doi: 10.4103/0976-2868.170565. [DOI] [Google Scholar]
- 17.Butchibabu K, Koppolu P, Mishra A, Pandey R, Swapna LA, Uppada UK. Evaluation of patient perceptions after labial frenectomy procedure: a comparison of diode laser and scalpel techniques. Eur J Gen Dent. 2014;3:129–133. doi: 10.4103/2278-9626.134839. [DOI] [Google Scholar]
- 18.Cavalcanti TM, Almeida-Barros RQ, Catão MH, Feitosa AP, Lins RD. Knowledge of the physical properties and interaction of laser with biological tissue in dentistry. An Bras Dermatol. 2011;86:955–960. doi: 10.1590/S0365-05962011000500014. [DOI] [PubMed] [Google Scholar]
- 19.Martens LC. Laser physics and a review of laser applications in dentistry for children. Eur Arch Paediatr Dent. 2011;12:61–67. doi: 10.1007/BF03262781. [DOI] [PubMed] [Google Scholar]
- 20.Fornaini C, Rocca JP, Bertrand MF, Merigo E, Nammour S, Vescovi P. Nd:yAG and diode laser in the surgical management of soft tissues related to orthodontic treatment. Photomed Laser Surg. 2007;25:381–392. doi: 10.1089/pho.2006.2068. [DOI] [PubMed] [Google Scholar]
- 21.Devishree SK, Gujjari SK, Shubhashini PV. Frenectomy: a review with the reports of surgical techniques. J Clin Diagn Res. 2012;6:1587–1592. doi: 10.7860/JCDR/2012/4089.2572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gomes ASL, Lopes MWF, Ribeiro CMB. Radiação laser: aplicações em cirurgia oral. Int J Dent. 2007;6:16–19. [Google Scholar]