Abstract
Purpose
To evaluate the therapeutic efficacy and complications of microneedling (dermaroller) therapy as a treatment modality in the treatment of facial scars resulting from acne, trauma and surgery.
Materials and Methods
Fifty patients with facial acne scar, traumatic scar, hypertrophic scars and scars with skin discoloration reporting to our institute were included in the study. Microneedling procedure was performed with the help of dermaroller. Postoperative wound was evaluated by three evaluators by comparing preoperative and postoperative clinical photographs.
Results
Seven out of the total 50 patients (14%) showed an excellent response to dermaroller treatment, while 26 patients (52%) had a good response. Fourteen patients (28%) had fair response, and 3 patients (6%) had poor response.
Conclusion
Microneedling therapy with dermaroller is one of the simplest, yet most effective skin treatments for scars, stretch marks, deep wrinkles, etc. The dermaroller is a definitive credit crunch skin rescue option. It is simple yet effective and suitable for all skin types and skin tones.
Keywords: Microneedling, Traumatic scar, Acne scar, Hypertrophic scar, Dermaroller
Introduction
Beauty or aesthetics plays an important role in a person’s life. An ever-increasing demand and desire to look more beautiful and attractive has become a primary concern. The human face plays an important role in a person’s identity, communication and self-confidence. The chances of developing adequate social skills are considerably higher for the “attractive” than for the “unattractive” and that a collective bias exists which says “beautiful is good and ugly is bad” [1].
Patient with a facial scar becomes a high degree functional, emotional and social handicap. A variety of studies have shown that patients suffer from low self-esteem and embarrassment when carrying visible scars on the face, neck, arms and hands. Such despair may result in decreased patient’s self-esteem, poor body image, poor job performance and diminished overall quality of life [2].
In this era of perfection, cosmetic procedures have altered people’s outlook toward life in general. The appearance of an unpleasant scar can definitely be improved, even if not erased. The cosmetic procedures for scar management can be divided into two categories—“Noninvasive techniques” and “Invasive techniques.” The Noninvasive techniques include pressure/compression therapy, silicone gel, topical steroids, microporous tape, polyurethane patches, acrylic casts, chemical peels. The Invasive techniques include surgical scar revision, intralesional corticosteroid injection, radiotherapy, laser therapy, cryotherapy, intralesional fluorouracil, interferon gamma, dermabrasion, percutaneous collagen induction with microneedling therapy [3–12].
Microneedling therapy is minimally invasive non-surgical and non-ablative procedure used for facial rejuvenation. This procedure involves the use of a microneedling device to create controlled skin injury. There are various skin needling devices including Dermaroller® (Dermaroller GmbH); Dermapen™ (Equipmed, Australia) Derma-Stamps™ (Dermaroller, USA) and radial disks incorporating fine microneedles of various diameters and lengths, fabricated from a wide range of materials such as silicon, glass, metals and polymers. As each fine needle punctures the skin, it creates a channel or micro-wound. The controlled injury triggers the body to fill these micro-wounds by producing new collagen and elastin in the papillary dermis. In addition, new capillaries are formed. This neovascularization and neocollagenesis following treatment leads to reduction of scars and skin rejuvenation which improved skin texture, firmness and hydration.
In this rapidly advancing field which is getting rapidly popular, it is necessary to keep a clear and rational perspective. As we encounter patients with traumatic scars, surgical scars and depressed scars in day-to-day practice, we should have a holistic approach to treat such patients. In the literature on microneedling therapy, we have found that most of the studies have used dermarollers with 192 needles but in the following study we have used dermaroller with 540 needles.
Aim
To evaluate the therapeutic efficacy and complications of microneedling (dermaroller) therapy as a treatment modality in correction of facial scars resulting from acne, trauma and surgery.
Materials and Methods
Study Design
It is a prospective randomized study consisting 50 patients with facial acne scar, traumatic scar, hypertrophic scars and scars with skin discoloration reporting to our institute.
Inclusion Criteria
Patients with post-acne scars/burn scars/post-traumatic scars in maxillofacial region.
Patients with post-herpetic scars/post-varicella scars in maxillofacial region.
Patients with facial scars and discoloration.
Exclusion Criteria
Patients on iso-tretinoin, corticosteroid or aspirin therapy for past 1 year.
Patients with keloids, family history of keloids.
Patients with bleeding disorder.
Patients with active viral or bacterial infection, evolving dermatosis or active inflammatory lesions of face.
Patients with malignant tumors of face.
Preoperative Preparation
Participants were counseled for the procedure, informed and explained about the complications of the procedure and about the local anesthesia. Informed written consent was taken.
Post-operatively, all the participants were informed to avoid sun exposure for at least 1 month and sunscreen (SPF 30 or greater) is used diligently. Patients were not given any preoperative antimicrobial drugs that might influence healing.
Procedure
Patient Preparation
The complete procedure was performed under all aseptic conditions and precautions using eutectic mixture of local anesthetic (EMLA) as topical anesthetic for 60–90 min.
The skin needling procedure was performed by rolling a preformed tool on the skin areas affected by scars. To treat scars, the device used was equipped with a rolling barrel 20 mm wide and 540 needles in 8 rows. The needles used had a length of 1.5 mm and a diameter of 0.25 mm. Depending on the applied pressure (pressing too hard is not necessary for excellent results and if needling is done on the face, the rolling barrel should not be used on the eyelids or lips), they penetrate the scar tissue between 0.1 and 1.3 mm.
Rolling consisted of moving dermaroller with same pressure, 4 times in 4 directions: horizontally, vertically and diagonally to the right and left. This ensured an even pricking pattern resulting in about 700–750 pricks per square centimeter.
The treatment time ranged from 10 to 60 min, depending on the size of the area being treated. The skin bleeding was observed for a short time, but that soon stopped.
After the Procedure
Wound dressing with soframycin ointment was given. Postoperative instructions were given to the patients, and they were informed that edema, erythema and crusting are normal sequelae. Redness of the skin subsided within 3–4 days and re-epithelization occurred by the 7–10th postoperative day. Patients were also advised application of moisturizer with vitamins A, C and E and sunscreen lotion (SPF 30 or greater) to prevent sun damage to skin.
Analysis of Data
Patients were recalled for follow-up after 7 days post-treatment for assessment of healing. Clinical evaluation of all the cases was carried out on every follow-up visit, but in order to make the study more reproducible and substantial extra-oral photographic record was made. All the photographs were recorded by same person using same device.
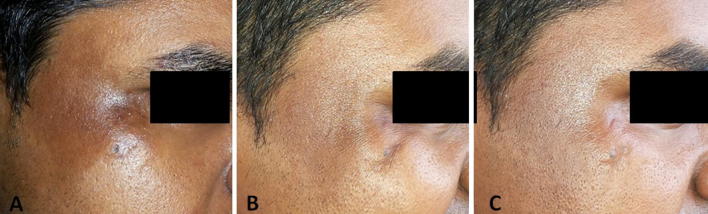
The photographic data of each patient were printed on photographic sheet. Photographs of each patient were presented on photographic sheet, i.e., preoperative and postoperative (Figs. 1, 2).
Fig. 1.
Patient with traumatic scar. a Preoperative clinical photograph. b Clinical photograph 1 week after initiation of the procedure. c Postoperative clinical photograph
Fig. 2.
Patient with acne scar. a Preoperative clinical photograph. b Clinical photograph 1 week after initiation of the procedure. c Postoperative clinical photograph
All the photographs of total 50 patients were mixed for randomization before evaluation and numbered from 1 to 50. The evaluation was done by three evaluators, i.e., plastic surgeon, periodontist and a beautician.
Results
In this study, results were analyzed by three evaluators. They evaluated clinical improvement in facial scars with microneedling therapy based on the comparison of pre- and postoperative photographs of patients. In all the patients, evaluators gave the score according to the percentage of improvement that they observe in the scar and then depending on the scores given by the evaluators, (score 5-poor, score 1-best), we used our criteria of improvement for assessing the results. To avoid the bias, an individual sheet was given for assessment to each evaluator and no evaluator was shown the assessment results of other evaluator.
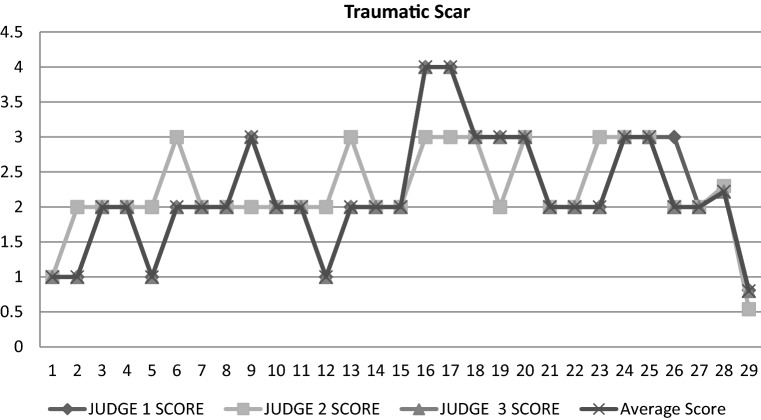
Out of 27 patients with traumatic scar (Fig. 3), on an average, 4 patients had score “1,” 15 patients had score “2,” 6 patients had score “3,” and remaining two had score of “4.” In traumatic scar patients, the pre-treatment score was “5” and the average score given for improvement in the scar by the three evaluators was “2.22”; the average score of standard deviation is “0.80,” and the average coefficient of variation is “36.04.” So, considering the variability and results given by evaluators the success rate is 64% in trauma scar patients.
Fig. 3.
As the scores of judge 1 and judge 3 are identical, the graph lines for these judge are overlapping
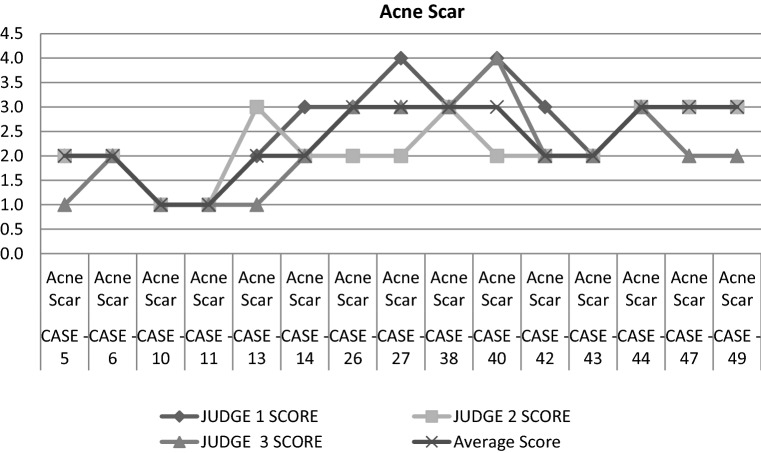
Total 15 patients with acne scars (Fig. 4) were evaluated, out of which on an average, 2 patients had the score of “1,” 6 patients had score “2,” and remaining 7 had score “3.” In acne scar patients, the pre-treatment score was “5” and the average score given for improvement in the scar by the three evaluators was “2.33.” The standard deviation was “0.72,” and average coefficient of variation was “31.02.” So, considering the variability and the scores given by evaluators the success rate in acne scar patient is 69%.
Fig. 4.
As the scores of judge 1 and judge 3 are identical, the graph lines for these judge are overlapping
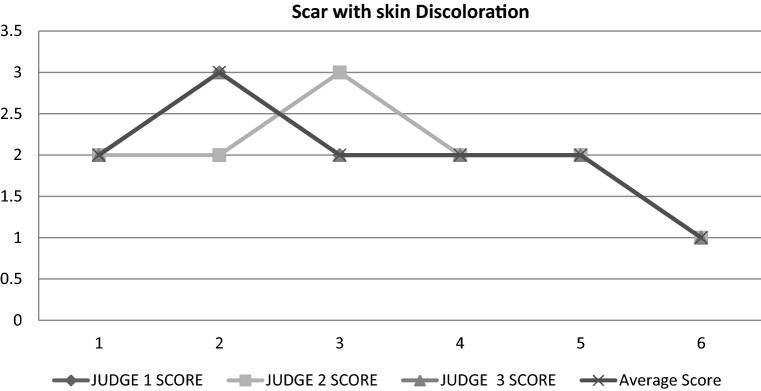
Out of our 6 patients with facial scar with discoloration (Fig. 5), one patient had score “1,” 4 patients had score “2,” and remaining 1 patient had score “3”; the pre-treatment score was “5,” and the average score given for improvement in the scar by the three evaluators was “2.0.” Average score of standard deviation was “0.63,” and average score of the coefficient of variation was “31.62.” So, considering the variability and the scores given by evaluators the success rate is 68% in scar with discoloration patient.
Fig. 5.
As the scores of judge 1 and judge 3 are identical, the graph lines for these judge are overlapping
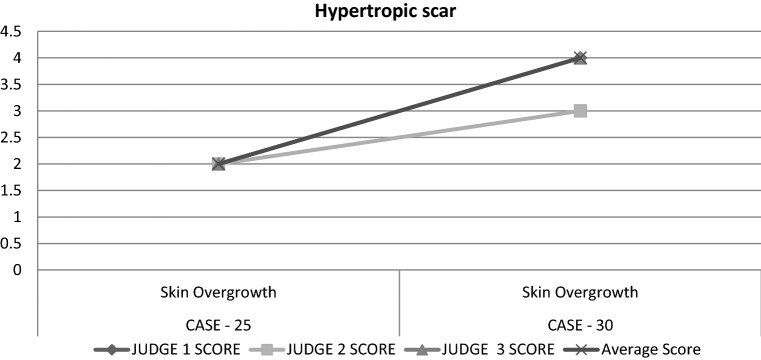
In 2 patients with hypertrophic scar (Fig. 6), one patient had an average score “4” and second patient had an average score of “2”; the pre-treatment score was “5,” and the average score given for improvement in the scar by the three evaluators was “3.” The average score of standard deviation is “1.41,” and the coefficient of variation is “47.00.” So, considering the variability and the score given by the evaluators in patients with hypertrophic scar the success rate is 53%.
Fig. 6.
As the scores of judge 1 and judge 3 are identical, the graph lines for these judge are overlapping
Overall, 7 out of the total of 50 patients (14%) showed an excellent response to dermaroller treatment, while 26 patients (52%) had a good response. Fourteen patients (28%) had fair response, and 3 patients (6%) had poor response.
Correlating the response with the morphological type of scarring present, we found a good-to-excellent response in rolling and boxcar scars, while pitted scars showed only moderate improvement. Linear scars, deep tunnels and other thick and complicated scars showed a less response to treatment.
Discussion
The development of microneedling occurred in 1994. Electroridopuncture (ERP) for skin aging and acne scars was practiced in cosmetic dermatology since 1995 when Orentreich and Orentreich [13] described subcision or dermal needling for scars. Camirand and Doucet in 1997 described needle dermabrasion using a “tattoo pistol” to treat scars. [14] Recently in 2006, Fernandes developed a more cost-effective management by introducing percutaneous collagen induction therapy with the dermaroller [15].
Various modalities have been used for the treatment of acne scars like punch excision, subcision, peels, microdermabrasion and lasers. The latest in the treatment armamentarium is microneedling [16].
In this study, microneedling therapy was performed on 50 patients with facial scars with the help of dermaroller (540 needles, 1.5 mm in length). Out of the total 50 patients, 27 patients had traumatic scar, 15 patients had acne scars, 6 patients had scar with skin discoloration, and 2 patients had hypertrophic scar. The results were assessed after four sessions of treatment. The age of the patients ranged from 18 to 40 years, with the mean age of 24.6 years. All patients tolerated the procedure well, and except for a temporary erythema and post-inflammatory skin discoloration, no adverse effects were noted in any patient.
Martin Schwarz (June 2011) in a prospective controlled assessment of microneedling with the dermaroller device (192 stainless steel needles and 1.5 mm length) treated eleven patients with post-traumatic scars. Author explained that all subjects were pleased with the results and acknowledged that they would undergo another dermaroller treatment [17].
In a study by Prof. Pholin for management of atrophic acne scar in 31 Thai patients (2006), usually the mild cases were treated once, while in severe cases 3–4 treatments were given. The mean clinical scores decreased from 4.24 to 2.33 at 6 months of follow-up. Five cases (16.13%) had improvement more than 75%, while 21 cases (67.74%) had improvement more than 50%. Two cases (6.45%) developed folliculitis within a few days after treatments, which cleared rapidly after oral antibiotics [18].
In our 50 patients, we have noticed that superficial scar of less than 1 mm depth had 80–90% improvement and was removed easily and in less visits. In deeper scar with depth more than 1 mm, scar reduction was seen 40–60% of total initial scar in 4 visits. So, deeper scars needed more time and visits to completely remove the scar.
Microneedling with dermaroller has emerged as an effective treatment option for scars, as it is a simple, easy-to-do, cost-effective, non-ablative, and minimally invasive procedure with excellent results, minimal social downtime and side effects. As a result, more and more women and men are choosing cosmetic procedures, making it more popular and acceptable with every passing year.
Conclusion
Microneedling therapy with dermaroller is one of the simplest, yet most effective skin treatment for scars, stretch marks, deep wrinkles, fine lines on skin, sun damaged skin, rough skin texture, hair loss, aging skin, hyper-pigmentation marks. Microneedling therapy also results in skin tightening, skin texture improvement, pore size reduction and improved capillary blood supply. It is simple yet effective and suitable for all skin types and skin tones. The dermaroller has laser-like results at a fraction of the cost. The healing is rapid, without any skin damage and requires less time. The process is virtually painless and in turn patient will start noticing a clear, new skin forming which will help them look younger and feel better about their facial skin appearance. Microneedling is a well-understood procedure with established preoperative and postoperative management with highly predictable results. Healing is prompt with minimal morbidity and rare complications.
The results can be optimized by careful patient selection, skin preparation; protection and choice of an appropriate device are important variables. The cost of the equipment is within reach of any practitioner or patient. Consequently, microneedling offers a practical complement to other methods of skin resurfacing. Managing patient expectations, however, is the most important component to treat any scars. Further studies need to be carried out on a larger sample size and also considering skin type of individual for more conclusive results.
As oral and maxillofacial surgeons, we have the skills to provide microneedling therapy at an exceptional level. Our forefathers in the specialty paved the way for us, and that is why we have privilege to practice our specialty. Each of us must obtain the proper training and continually update our knowledge in this area so that we can continue to advance the specialty of oral and maxillofacial surgery.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no competing interests.
Ethical Approval
This study was approved by the ethics committee of the Institution. All procedures performed in the study were in accordance with the ethical standards of the institutional ethics committee.
Informed Consent
Informed consent was obtained from the patients included in the study.
References
- 1.Brons R. Esthetics. Textbook of facial harmony standards for orthognathic surgery and orthodontics. London: Quintessence Publishing Co; 1998. pp. 13–15. [Google Scholar]
- 2.Bock O, Schmid-Ott G, Malewski P, Mrowietz U. Quality of life of patients with keloid and hypertrophic scarring. Arch Dermatol Res. 2006;297(10):433. doi: 10.1007/s00403-006-0651-7. [DOI] [PubMed] [Google Scholar]
- 3.Kempiak SJ, Uebelhoer N. Superficial chemical peels and microdermabrasion for acne vulgaris. In Seminars in cutaneous medicine and surgery 2008 Sep 1, vol 27, no 3, pp 212–220. Frontline Medical Communications [DOI] [PubMed]
- 4.Tanzi EL, Aister TS. Laser treatment of scars—advances in dermatologic surgery. Skin Ther Lett. 2004;9(1):4–7. [PubMed] [Google Scholar]
- 5.Robertson JC, Hodgson B, Druett JE, Druett J. Pressure therapy for hypertrophic scarring: preliminary communication. J R Soc Med. 1980;73(5):348–354. doi: 10.1177/014107688007300509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hatamipour E, Mehrabi S, Hatamipour M, Shirazi HR. Effects of combined intralesional 5-fluorouracil and topical silicone in prevention of keloids: a double blind randomized clinical trial study. Acta Med Iran. 2011;49(3):127. [PubMed] [Google Scholar]
- 7.Gauglitz GG. Management of keloids and hypertrophic scars: current and emerging options. Clin Cosmet Investig Dermatol. 2013;6:103. doi: 10.2147/CCID.S35252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rivera AE. Acne scarring: a review and current treatment modalities. J Am Acad Dermatol. 2008;59(4):659–676. doi: 10.1016/j.jaad.2008.05.029. [DOI] [PubMed] [Google Scholar]
- 9.Basta-Juzbašić A. Current therapeutic approach to acne scars. Acta Dermatovenerol Croat. 2010;18(3):171–175. [PubMed] [Google Scholar]
- 10.O’Sullivan ST, O’Shaughnessy M, O’Connor TP. Aetiology and management of hypertrophic scars and keloids. Ann R Coll Surg Engl. 1996;78(3 Pt 1):168. [PMC free article] [PubMed] [Google Scholar]
- 11.Anitha B. Prevention of complications in chemical peeling. J Cutan Aesthet Surg. 2010;3(3):186. doi: 10.4103/0974-2077.74500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sarkarat F, Bohluli B, Kahali R (2013) Office-based facial cosmetic procedures. In: A textbook of advanced oral and maxillofacial surgery. InTech
- 13.Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;21(6):543–549. doi: 10.1111/j.1524-4725.1995.tb00259.x. [DOI] [PubMed] [Google Scholar]
- 14.Aust MC, Reimers K, Repenning C, Stahl F, Jahn S, Guggenheim M, Schwaiger N, Gohritz A, Vogt PM. Percutaneous collagen induction: minimally invasive skin rejuvenation without risk of hyperpigmentation—fact or fiction? Plast Reconstr Surg. 2008;122(5):1553–1563. doi: 10.1097/PRS.0b013e318188245e. [DOI] [PubMed] [Google Scholar]
- 15.Patnaik VVG, Singla R, Bala S. Anatomy of ‘a beautiful face & smile’. J Anat Soc India. 2003;52(1):74–80. [Google Scholar]
- 16.Sharad J. Combination of microneedling and glycolic acid peels for the treatment of acne scars in dark skin. J Cosmet Dermatol. 2011;10(4):317–323. doi: 10.1111/j.1473-2165.2011.00583.x. [DOI] [PubMed] [Google Scholar]
- 17.Schwarz M, Laaff H. A prospective controlled assessment of microneedling with the Dermaroller device. Plast Reconstr Surg. 2011;127(6):146e–148e. doi: 10.1097/PRS.0b013e3182131e0f. [DOI] [PubMed] [Google Scholar]
- 18.Niwat P. Percutaneous collagen induction with dermaroller for management of atrophic acne scars in 31 Thai patients. J Cosmet Dermatol. 2009;2(1):1–13. [Google Scholar]