Abstract
Introduction
Sebaceous gland carcinoma of the eyelid is an uncommon but highly malignant tumour. Post-tumour excisional defect reconstruction must aim in restoration of function and aesthetics. Prompt diagnosis and adequate treatment is of paramount for successful outcome of disease.
Case Report
A 61-year-old female patient underwent surgery for sebaceous gland carcinoma of right lower eyelid 3 years back and reported to us with recurrence. On examination, an exophytic mass was seen over right conjunctiva adjacent to the eyelid margin. With the objective of restoring form and aesthetics, immediate reconstruction was carried out using superiorly pedicled nasolabial flap to cover the lower eyelid defect and non-vascularised buccal mucosal flap for bulbar and palpebral conjunctival reconstruction.
Conclusion
The tumour is notorious to cause local recurrence and metastases; hence, an early and accurate diagnosis, surgical and adjunctive chemoradiation and regular periodic follow-ups are of utmost importance for the successful management of sebaceous gland carcinoma of eyelids.
Introduction
Sebaceous gland carcinoma of the eyelid is an uncommon but a highly malignant neoplasm. It is the second most common eyelid neoplasm, first being basal cell carcinoma [1]. The incidence is approximately 0.2–0.8% of all eyelid tumours and 1.0–5.5% of all eyelid malignancies [2]. A higher incidence is seen among Asian individuals [2]. The tumour shows a female predilection and affects adults mainly between sixth to seventh decades of life [3]. The tumour may arise from meibomian glands, glands of Zeis or sebaceous glands of the eyelid skin [2]. The upper eyelid is affected more than the lower eyelid [2]. The tumour poses challenge in diagnosing both clinically and histologically as it closely mimics features of other pathologies [3]. Post-tumour excisional defect reconstruction must aim in restoration of function and aesthetics.
Case Report
A 61-year-old female patient underwent surgery for sebaceous gland carcinoma of right lower eyelid 3 years back and reported to us with recurrence.
On examination, an exophytic mass was seen over right conjunctiva adjacent to the eyelid margin. It measured 2.5 × 1.5 cm, occupying the entire lower eyelid except the medial one-third and extended to the lateral canthus (Fig. 1). The mass had fine septations, freely mobile without any globe movement restriction and bled easily. The mass moulded to the shape of the globe and inferior conjunctival fornix. There was loss of eyelashes and skin attachment at the eyelid margin overlying tumour. There was no globe displacement or proptosis. No lymph nodes were palpable.
Fig. 1.

Exophytic mass over lower right eyelid
High-resolution ultrasonography of face and neck showed no parotid and cervical lymphadenopathy. Incisional biopsy of the lesion confirmed recurrent sebaceous gland carcinoma.
The treatment executed was wide excision of the lateral two-thirds of the lower and lateral one-third of the upper eyelid down to the periosteum with 5-mm normal margins. The conjunctiva of the inferior fornix and lower one-third of the bulbar conjunctiva were excised along with the lid mass. The lower lid retractors were transected deep to the orbital rim (Fig. 2a, b).
Fig. 2.
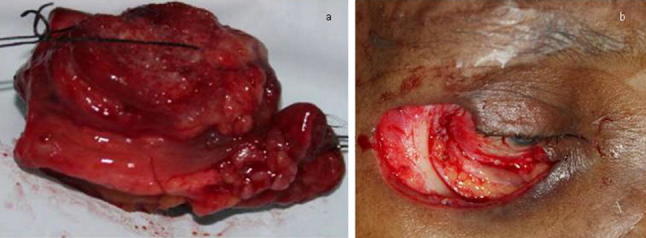
a Tumour excisional specimen. b Post-tumour excisional defect
With the objective of restoring form and aesthetics, immediate reconstruction was carried out using superiorly pedicled nasolabial flap to cover the lower eyelid defect and non-vascularised buccal mucosal flap for bulbar and palpebral conjunctival reconstruction.
Both flap healing were uneventful (Fig. 3). The flap was also well attached to the lower eyelid retractors. The functional result (lid closure, ocular movements) and cosmesis achieved were satisfactory. Final histopathology report revealed lower eyelid sebaceous gland carcinoma with all margins being negative. Since it was a recurrent lesion, the patient was subjected to external beam radiation therapy to neck 50 Gy in 25 fractions and surface mould brachytherapy to right lower eyelid 28 Gy in 14 fractions. The patient has been followed up periodically for 12 months and is found to be disease free.
Fig. 3.

Post-operative healing of nasolabial and buccal mucosal flaps
Discussion
The treatment of sebaceous gland carcinoma of the eyelid often gets delayed as it is frequently misdiagnosed with chalazion, blepharoconjunctivitis or basal cell carcinoma [2]. The tumour can spread directly by orbital invasion, regional lymph nodes via lymphatogenous and distant spread via haematogenous routes [3].
Microscopically, the lesion was composed of tumour cells with foamy cytoplasm and fine vacuoles signifying sebaceous differentiation [4] (Fig. 4). Histologically, it is commonly misdiagnosed as basal cell carcinoma [3]. Thus, multiple full-thickness biopsies from representative areas are required [2]. The diagnosis is further complicated by the tendency of the tumour to spread intraepithelially referred to as pagetoid spread [2]. Metastasis occurs in approximately 8–25% cases. Local metastasis involves parotid, submandibular and cervical lymph nodes. Distant metastasis involves liver, lung, brain and bones [5].
Fig. 4.

Microscopic view revealed tumour tissue showing cells arranged in lobules, nests and sheets that are separated by fibrous septa. Cells were pleomorphic and had round to oval nuclei. Occasional mitotic cells were seen
Surgical excision is the mainstay of treatment [2]. Tumour without orbital involvement involves wide local excision, with the margins checked in both frozen and permanent sections in combination with conjunctival map surgeries [2]. Margin of 5–6 mm of normal appearing tissue is required to prevent recurrence. Total parotidectomy, cervical node dissection and radiotherapy are required in cases of lymph node involvement [6]. Orbital exenteration is reserved for patients with extensive orbital involvement [2]. Radiotherapy is considered as an adjunctive to surgery in cases of recurrences and long-standing cases, patients refusing surgery or as palliative treatment in inoperable cases [2]. Chemotherapy has been used to manage recurrent or metastatic lesion, but there is no evidence-based regimen [3].
Indicators of poor prognosis include poor differentiation of tumour, involvement of both eyelids, tumour diameter > 10 cm, duration of symptoms > 6 months, orbital, vascular, lymphatic invasion and pagetoid invasion [7].
Skin and subcutaneous tissue of eyelid can be reconstructed using full-thickness skin grafts, pedicled flaps like superior eyelid skin flap, supraorbital skin flap, midforehead flap, nasolabial flap, cervical tubed flap [8], cheek rotation flap (Mustarde) and bipedicled musculocutaneous Tripier flap. Conjunctival reconstruction can be done using tarso-conjunctival grafts, buccal mucosa, hard palate mucosa, temporalis fascia and amniotic membrane [9].
We used the superiorly pedicled subcutaneous nasolabial flap because of excellent colour match, proximity to lesion, ease of harvesting and primary closure of donor defect. The flap is highly versatile as it can be advanced, rotated or transposed. The flap thickness harvested depends upon the reconstructive requirement. When a thin pliable eyelid skin is required, the flap can be thinned at the level of dermis and epidermis or can be maintained thick as in reconstruction for full-thickness lip defects. Despite the flap has random pattern of blood supply, it acts as an axial flap, due to extensive vascularisation of the face.
In 1983, van der Meulen first described use of buccal mucosal graft for conjunctival reconstruction, but Anderson [10] observed lower lid laxity with thin buccal mucosal grafts. Therefore, we preferred to use thick buccal mucosa flap to provide excellent movement and support and avoid lid laxity.
Conclusion
The tumour is notorious to cause local recurrence and metastases; hence, an early and accurate diagnosis, surgical and adjunctive chemoradiation and regular periodic follow-ups are of utmost importance for the successful management of sebaceous gland carcinoma of eyelids.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
The procedure performed in studies involving human participants was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from the participant included in the study.
Contributor Information
Badrinath Talwar, Email: kanachurcraniofacial@gmail.com, Email: badrinath.talwar@gmail.com.
Mustafa Khader, Email: drmustafamaxfax@gmail.com.
Prashanth Lowell Monis, Email: monislowell@gmail.com.
Aafreen Aftab, Email: aafreenaftab@gmail.com.
References
- 1.Saito A, Tsutsumida A, Furukawa H, Saito N, Yamamoto Y. Sebaceous carcinoma of the eyelids: a review of 21 cases. J Plast Reconstr Aesthet Surg. 2008;61(11):1328–1331. doi: 10.1016/j.bjps.2007.09.016. [DOI] [PubMed] [Google Scholar]
- 2.Callahan EF, Appert DL, Roenigk RK, Bartley GB. Sebaceous carcinoma of the eyelid: a review of 14 cases. Dermatol Surg. 2004;30(8):1164–1168. doi: 10.1111/j.1524-4725.2004.30348.x. [DOI] [PubMed] [Google Scholar]
- 3.Kan LW, Leu YS, Tzen CY, Wu CH. Recurrent sebaceous gland carcinoma of eyelid previously diagnosed as basal cell carcinoma: case report. Am J Otolaryngol. 2011;32(6):620–623. doi: 10.1016/j.amjoto.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Costea CF, Petraru D, Dumitrescu G, Sava A. Sebaceous carcinoma of the eyelid: anatomoclinical data. Rom J Morphol Embryol. 2013;54(3):665–668. [PubMed] [Google Scholar]
- 5.Lan MC, Lan MY, Lin CZ, Ho DM, Ho CY. Sebaceous carcinoma of the eyelid with neck metastasis. Otolaryngol Head Neck Surg. 2007;136(4):670–671. doi: 10.1016/j.otohns.2006.08.019. [DOI] [PubMed] [Google Scholar]
- 6.Husain A, Blumenschein G, Esmaeli B. Treatment and outcomes for metastatic sebaceous cell carcinoma of the eyelid. Int J Dermatol. 2008;47(3):276–279. doi: 10.1111/j.1365-4632.2008.03496.x. [DOI] [PubMed] [Google Scholar]
- 7.Shields JA, Demirci H, Marr BP, Eagle RC, Jr, Shields CL. Sebaceous carcinoma of the ocular region: a review. Surv Ophthalmol. 2005;50(2):103–122. doi: 10.1016/j.survophthal.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 8.Paletta FX. Lower eyelid reconstruction. Plast Reconstr Surg. 1973;51(6):653–657. doi: 10.1097/00006534-197306000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Copcu E, Sivrioglu N. The new reconstruction technique in the treatment of the skin cancers located on the eyelid: posterior temporalis fascia composite graft. Int Semin Surg Oncol. 2004;1:5. doi: 10.1186/1477-7800-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whitehouse GM, Francis IC. Eyelid reconstruction using a monopedicle flap and buccal mucosa: report of 15 cases. Aust N Z J Ophthalmol. 1988;16(4):295–301. doi: 10.1111/j.1442-9071.1988.tb01231.x. [DOI] [PubMed] [Google Scholar]


