Abstract
The initiation of polymorphic ventricular tachycardia in long QT syndrome type 2 (LQT2) has been associated with a characteristic ECG pattern of short-long RR intervals. We hypothesize that this characteristic pattern increases APD dispersion in LQT2, thereby promoting arrhythmia. We investigated APD dispersion and its dependence on two previous cycle lengths (CLs) in transgenic rabbit models of LQT2, LQT1, and their littermate controls (LMC) using random stimulation protocols. The results show that the short-long RR pattern was associated with a larger APD dispersion in LQT2 but not in LQT1 rabbits. The multivariate analyses of APD as a function of two previous CLs (APDn = C + α1CLn−1 + α2CLn−2) showed that α1 (APD restitution slope) is largest and heterogeneous in LQT2 but uniform in LQT1, enhancing APD dispersion under long CLn−1 in LQT2. The α2 (short-term memory) was negative in LQT2 while positive in LQT1, and the spatial pattern of α1 was inversely correlated to α2 in LQT2, which explains why a short-long combination causes a larger APD dispersion in LQT2 but not in LQT1 rabbits. In conclusion, short-long RR pattern increased APD dispersion only in LQT2 rabbits through heterogeneous APD restitution and the short-term memory, underscoring the genotype-specific triggering of arrhythmias in LQT syndrome.
Subject terms: Arrhythmias, Cardiovascular diseases
Introduction
Long-QT syndrome (LQTS) is an inherited disease associated with prolongation of QT interval and sudden cardiac death (SCD)1. The two most common forms of LQTS are caused by mutations in the KCNQ1 (LQT1) and KCNH2 genes (LQT2), which encode the α subunits of the slowly activating (IKs) and rapidly activating (IKr) voltage-gated potassium channels, respectively. Clinical studies have documented that pause-dependent initiation of polymorphic ventricular tachycardia (pVTs) is associated with either congenital LQT22,3 or acquired LQT24, and is classically referred to as the short-long-short RR interval sequence of R-on-T early afterdepolarization (EAD)2,3,5.
The ‘pause’, or short-long initiation pattern, can cause excessive APD prolongation in LQTS to promote EADs, leading to pVTs. In addition, ‘pause’ may increase APD dispersion, a substrate vulnerable to reentry by causing conduction blocks in LQT syndromes6,7. Indeed, several groups have shown that a pause can increase APD dispersion in drug-induced experimental animal models of LQTS7,8. In addition to well-recognized role of APD dispersion in reentry formation, our group also reported that the enhanced APD dispersion could promote the spontaneous genesis of premature ventricular complexes (PVCs) by electrotonic current flow in the steep repolarization gradient area9,10, suggesting that APD dispersion can act as both substrate and trigger for pVT initiation in LQTS.
Despite the importance of APD dispersion in LQT-related arrhythmias, it is not clear whether the short-long cycle length (CL) pattern increases APD dispersion as well as how varied CL can effect on behavior of APD dispersion. To understand how APD dispersion is modulated under alternating CL pattern, the effect of previous multiple CL changes on APDs should be considered. A typical APD restitution curve as a function of a single diastolic interval from a S1S2 protocol is significantly limited in this case, since it does not account for the effect of short-long alternating CL. Previous studies using two premature stimuli (S1-S2-S3 intervals) showed that the APD dynamics of S3 is markedly different from the APD restitution curve of the S2 beat11–13.
Several groups have introduced the term ‘short-term cardiac memory’ which refers to the effects of pacing history on APD14–18. Theoretical and experimental studies used random CL pacing19 or stochastic pacing protocol20–22 to investigate APD modulation by pacing history and its influence on alternans. The adaptation of APD to history of CL change can be attributed to the activation/inactivation and recovery kinetics of ionic currents and Ca2+ handling, and changes in intracellular and extracellular ion concentration. Ion channel kinetics most likely underlies short-term cardiac memory and it is possible that prior heart rate variations such as short-long CL may greatly influence APD dynamics in LQTS lacking IKs or IK r and is probably an important factor in determining APD dispersion under characteristic short-long RR intervals as seen in LQT2 but not in LQT1 patients. However, most of studies on short-term memory focused on modulation of APD dynamics and alternans by pacing history and its effect on APD dispersion in LQTS in a genotype-specific manner is not fully elucidated.
Telemetry recordings from LQT2 rabbits showed characteristic short-long CL variation before the onset of pVT and sudden cardiac death23,24 similar to LQT2 patients2,3. We therefore used these transgenic rabbits to investigate the mechanisms underlying CL–dependent APD dispersion in LQTS. APD dispersion dynamics from littermate control (LMC), LQT1 and LQT2 rabbits were studied using randomly varying CLs and short-long CL pacing protocol and we found that APD dispersion in LQT2 rabbits is highly dependent on a previous history of heart rate variation due to heterogeneous restitution and short-term cardiac memory.
Results
CL patterns preceding maximum APD dispersion
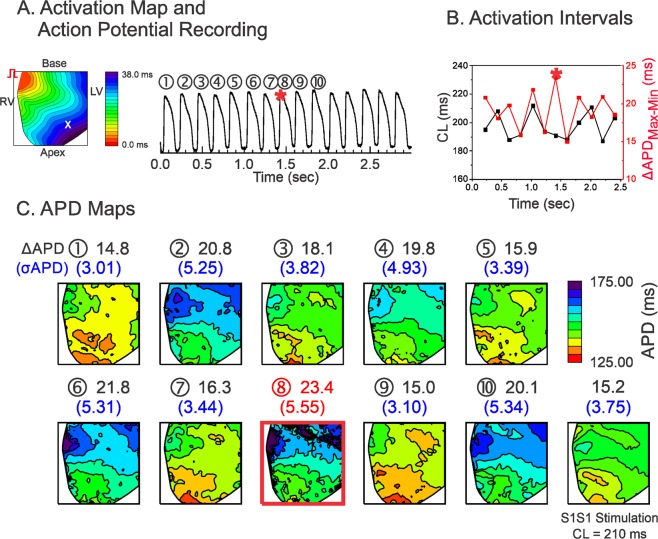
Hearts of all three genotypes (LMC, LQT1, and LQT2) were stimulated using a series of computer-generated random CLs in the range of tissue refractoriness plus 50 ms to investigate dynamics of APD dispersion under various CL combinations (see Methods). Figure 1 shows typical examples of activation map, APD traces, CL variation, and APD maps from a LMC rabbit. Figure 1A shows an activation map and an AP trace from one mapping site (x), and Fig. 1B shows the CLs measured from the same site. Figure 1C shows the series of APD maps and APD dispersion for 10 consecutive beats. In this case, the maximum APD dispersion occurred at the 8th beat (marked with a red star in panels A–C). The last panel in Fig. 1C is the APD map from constant rate pacing at CL = 210 ms (=averaged CL of random pacing).
Figure 1.
Influence of CL variation on APD dispersion in LMC. (A) Activation map and sample trace of action potentials during random stimulation. (B) Corresponding mean CLs (black) and ΔAPDmax-min (red) in panel (A,C) APD maps corresponding to the action potentials shown in panel A. ΔAPDmax-min and the standard deviations of the APDs (σAPD) are shown above the corresponding maps. The beat with maximum APD dispersion is marked with a red square (the 8th beat, ΔAPDmax-min = 23.4 ms). The corresponding beat of the maximum ΔAPDmax-min is marked with a red star in panels A and B. The APD map from S1S1 stimulation at the closest average CL of random stimulation protocol is also shown at the end for comparison (CL = 210 ms in this scan, ΔAPDmax-min = 15.2 ms, σAPD = 3.75 ms).
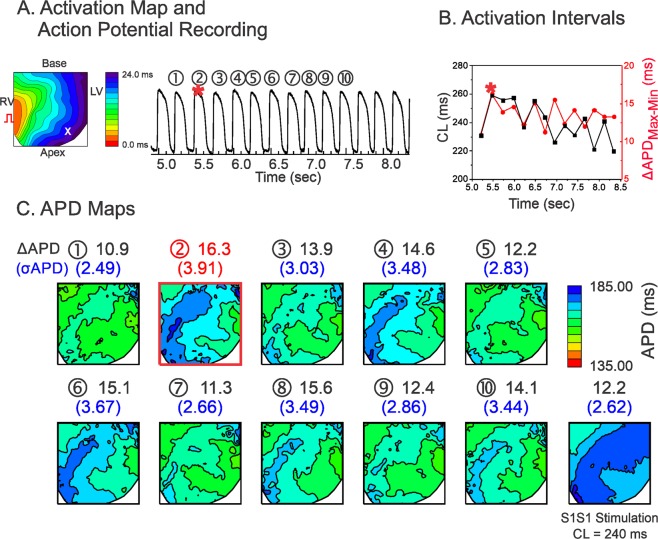
Figure 2 shows a representative result from a LQT1 heart. APD dispersion in the LQT1 hearts was smaller overall than that in the LMC hearts. Long CLs repeatedly produced higher APD dispersion in LQT1. Figure 3 shows an example from a LQT2 heart. The maximum dispersion in LQT2 (σAPD = 10.9 ms, ΔAPDmax-min = 38.0 ms) occurred at the 10th beat. The dispersion under ramp pacing (panel C, last APD map at CL = 270 ms, σAPD = 7.2 ms, ΔAPDmax-min = 26.0 ms) was smaller than that under random pacing, suggesting that CL variations were more likely to promote APD dispersion as compared to fixed CL.
Figure 2.
Influence of CL variation on APD dispersion in LQT1. (A) Activation map and sample trace of action potentials. (B) Corresponding mean CLs (black) and ΔAPDmax-min (red) in panel (A,C) APD maps for each stimulation in A. The beat with maximum APD dispersion are marked with a red square (2nd beat, ΔAPDmax-min = 16.3 ms, σAPD = 3.91 ms). Prior to the maximum APD dispersion, CLs did not show a short-long CL pattern.
Figure 3.
Influence of CL variation on APD dispersion in LQT2. (A) Activation map and sample trace of action potentials. (B) Corresponding mean CLs (black) and ΔAPDmax-min (red) in panel (A,C) APD maps. The beat with the maximum APD dispersion is marked with a red square (10th beat). Note that short-long alternating CL precedes the maximum APD dispersion.
Overall, the APD dispersion is largest in LQT2 and smallest in LQT1. The beat-to-beat APD variation was greatest in LQT2, medium in LMC, and lowest in LQT1 hearts (see Supplementary Fig. S1 for expanded traces and Table 1 for summary of APD dispersion from three genotypes).
Table 1.
Summary of statistical data analysis.
| LMC | LQT1 | LQT2 | |
|---|---|---|---|
|
Max σAPD |
Fig. 1. Under Random Stimulation: σAPD = 5.55 ms ΔAPDmax-min = 23.4 ms Under S1S1 Stimulation: CL = 210 ms σAPD = 3.75 ms ΔAPDmax-min = 15.2 ms |
Fig. 2. Under Random Stimulation: σAPD = 3.91 ms ΔAPDmax-min = 12.2 ms Under S1S1 Stimulation: CL = 240 ms σAPD = 2.62 ms ΔAPDmax-min = 12.2 ms |
Fig. 3. Under Random Stimulation: σAPD = 10.9 ms ΔAPDmax-min = 38.0 ms Under S1S1 Stimulation: CL = 270 ms σAPD = 7.2 ms ΔAPDmax-min = 26.0 ms |
|
Beat-to-beat APD variation (standard deviation of APD during random stimulation,σbeat-to-beat) |
5.8 ± 1.2 ms n = 5 hearts in Fig. 1 |
3.2 ± 0.9 ms n = 5 hearts in Fig. 2 |
8.8 ± 2.0 ms LMC vs. LQT2, p < 0.05 LQT1 vs. LQT2, p < 0.05 (Student’s t-test respectively) |
|
ΔCL = CLn−1 – CLn−2 at maximum APD dispersion (paired t-test between CLn−1 and CLn−2) (Fig. 4A) |
5.3 ± 17.7 ms p = 0.2084 n = 5 hearts, 10 scans |
5.0 ± 18.6 ms p = 0.2084 n = 5 hearts, 10 scans |
17.7 ± 14.1 ms CLn−1 > CLn−2, p < 0.01 n = 5 hearts, 10 scans |
|
Correlation of σAPD vs. ΔCL under random stimulation (Fig. 4B) |
0.008 ± 0.002 r = 0.23 ± 0.14 n = 4 hearts LMC vs. LQT1, p < 0.05 |
0.002 ± 0.004 r = 0.10 ± 0.16 n = 4 hearts |
0.022 ± 0.008 r = 0.51 ± 0.17 n = 4 hearts LMC vs. LQT2, p < 0.05 LQT1 vs. LQT2, p < 0.05 (Student’s t-test respectively) |
|
Correlation between ΔCL and σAPD under S1S2S3 stimulation (Fig. 4C) |
r = 0.68 ± 0.09 p < 0.05 n = 4 hearts |
N/A |
r = 0.79 ± 0.14 p < 0.01 n = 4 hearts |
|
Slope of σAPD vs. ΔCL under S1S2S3 stimulation (Fig. 4C) |
0.005 ± 0.001 n = 4 hearts |
N/A |
0.035 ± 0.020 LMC vs. LQT2, p < 0.01 n = 4 hearts (Student’s t-test) |
|
Coefficient α1 under random stimulation in Fig. 5C (Statistical differences were found by one-way ANOVA test at p = 0.05 level) |
0.23 ± 0.06 n = 6 hearts |
0.17 ± 0.02 n = 6 hearts LMC vs LQT1, p = 0.029 (Student’s t-test) |
0.32 ± 0.06 n = 6 hearts LMC vs LQT2, p = 0.039 LQT1 vs LQT2, p < 0.00003 (Student’s t-test respectively) |
|
Coefficient α2 under random stimulation in Fig. 5C (Statistical differences were found by one-way ANOVA test at p = 0.05 level) |
−0.068 ± 0.04505 n = 6 hearts |
0.007 ± 0.051 n = 6 hearts LMC vs LQT1, p = 0.023 (Student’s t-test) |
−0.053 ± 0.021 n = 6 hearts LQT1 vs LQT2, p = 0.025 LMC vs LQT2, p = 0.461 (Student’s t-test) |
|
Standard deviation of restitution slope map under random stimulation in Fig. 5D |
0.030 ± 0.014 n = 4 hearts |
0.029 ± 0.008 n = 4 hearts |
0. 064 ± 0.025 n = 4 hearts LMC vs. LQT2, p < 0.05 (Student’s t-test) |
|
Correlation between α1 and α2 in Fig. 5E |
−0.07 ± 0.15 n = 6 hearts |
N/A |
−0.27 ± 0.10 n = 6 hearts |
Short-long alternating CL increases APD dispersion only in LQT2 hearts
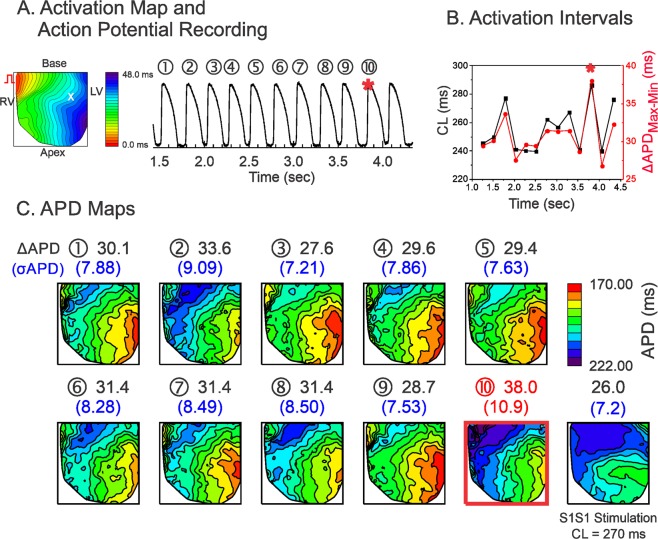
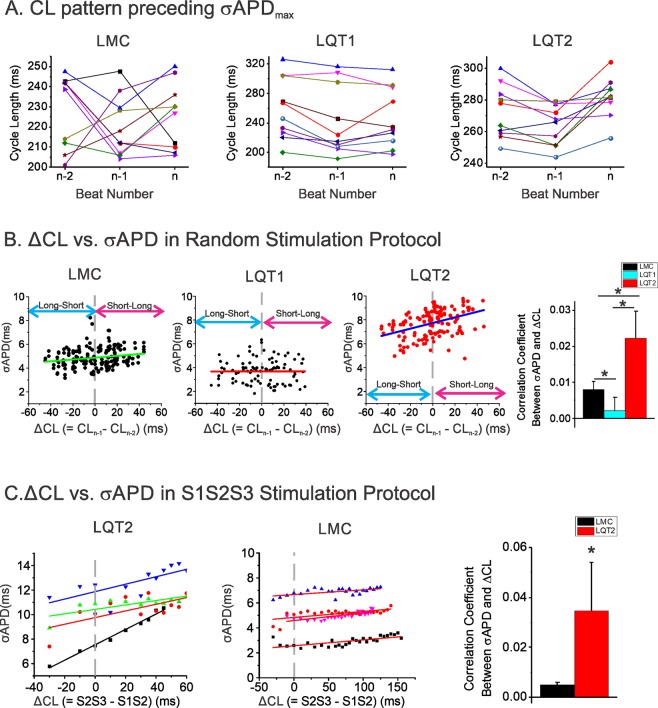
Figure 4A shows CLs from the three previous CLs preceding the beat exhibiting maximum APD dispersion from LMC, LQT1, and LQT2 hearts. LQT2 hearts exhibited a long-short-long CL sequence (short-long if only two previous CLs included) that preceded the beat with maximum APD dispersion, while LMC and LQT1 hearts did not show clear CL dependent patterns (Table 1). To further quantify the effect of alternating CL on APD dispersion, we investigated whether there is any correlation between CL difference (ΔCL = CLn−1 − CLn−2, a degree of CL change from short to long) and APD dispersion. Panel B shows typical examples of APD dispersion (σAPD, see Methods) vs. ΔCL from 20-second scans in LMC, LQT1, and LQT2 hearts. The results show a positive correlation between ΔCL and APD dispersion in LQT2 but negligible correlation in LMC and LQT1 (Table 1). APD dispersion in LQT2 is more dependent on a degree of CL change.
Figure 4.
CL patterns preceding the maximum APD dispersion. (A) Three previous CLs (CLn−3 − CLn−2 − CLn−1) preceding ΔAPDmax in LMC, LQT1, and LQT2 (n = 10 stimulation protocols from 5 hearts per group). Note that long-short-long CL patterns precede ΔAPDmax in LQT2 (paired t-test between CLn−2 and CLn−1, p = 0.0017), while no clear pattern was found in LMC (p = 0.1836) or LQT1 (p = 0.2084). (B) Correlation analysis of alternating CL and APD dispersion in random stimulation protocol. CL difference (ΔCL = CLn−1 − CLn−2) vs. APD dispersion (σAPD) shows a clear positive association in LQT2, unlike LMC & LQT1. Correlation coefficient between APD dispersion (σAPD) and ΔCL in LQT2 greater than others under random stimulations (slope = 0.00797 ± 0.00237 in LMC, 0.0022 ± 0.0037 in LQT1, and 0.02218 ± 0.00759 in LQT2 n = 4 hearts each. p = 0.039, 0.012, and 0.003 in LMC VS. LQT1, LMC VS LQT2 and LQT1 VS. LQT2 respectively, Student’s t-test where appropriate). APD dispersion of LQT2 is more dependent on CL difference. (C) Correlation of CL difference (ΔCL = S2S3 − S1S2) with APD dispersion (σAPD) in S1S2S3 Protocol replicating short-long CL pattern. In LQT2, there is a positive relationship (slope = 0.035 ± 0.020, n = 4 hearts) between short-long cycle and APD dispersion (σAPD), but of much smaller size in LMC (slope = 0.003 ± 0.003, n = 4 hearts, p = 0.02 LQT2 VS. LMC, Student’s t-test where appropriate).
To further verify that a short-long CL increases APD dispersion in LQT2, we applied an S1S2S3 pacing protocol in which S2S3 was fixed while S1S2 was variable (see Methods). This stimulation protocol evaluates the effect of S1S2 on APD dispersion of the S3 beat, since S2S3 is fixed. Figure 4C shows the results of APD dispersion of the S3 beat from LMC and LQT2 (n = 4 per group). To be consistent with panel B, we used ΔCL = S2S3 − S1S2 for the x-axis, and S2S3 was fixed at 320 ms. Both LQT2 and LMC demonstrated statistically significant correlation between ΔCL and σAPD (Table 1). The linear regression of σAPD vs. ΔCL showed a steeper slope in LQT2 (Table 1). Thus, shortening S1S2 by 100 ms increased APD dispersion by 19 ms in LQT2 but only 2.7 ms in LMC. These results strongly suggest that S1S2 alone has a significant influence on APD dispersion of the S3 in LQT2 rabbits, setting the stage for the generation of pVTs.
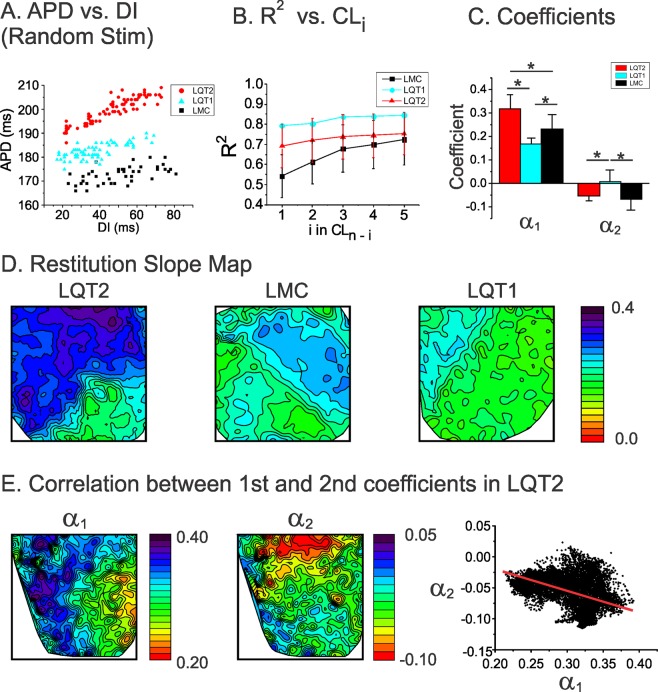
Genotypic specific restitution kinetics of APD and short-term memory
Since the previous two CLs have greater impact on APD dispersion in LQT2 hearts, we hypothesized that short-term cardiac memory is greater in LQT2 hearts to cause large APD dispersion under the characteristic short-long CL pattern. We investigated the short-term memory effect, specifically how much the second previous CL (CLn−2) influences APD, using multivariate regression analysis (see Methods). Figure 5A shows typical examples of APD vs. diastolic interval (DI) scatter plots using the random pacing protocol in LMC, LQT1, and LQT2 hearts. The goodness of fit (R2) increases with increasing the number of previous CLs included in the multivariate analysis (panel B). The coefficients from the multivariate regression analysis are shown in panel C. The results show that the coefficient α1 for the first CL was greatest in LQT2, meaning that APD restitution is steepest in LQT2. The coefficient α2 (representing the short-term memory effect) for the second CL of LMC and LQT2 were negative (details are in Table 1) while the coefficient for LQT1 is close to zero (Table 1), meaning that shorter CLn−2 is associated with longer APDn in LMC and LQT2.
Figure 5.
APD restitution and short-term memory effect on APD dispersion. (A) Examples of APD restitution from LMC, LQT1, and LQT2 hearts using random stimulation protocol. Note that the restitution slope is greatest in LQT2 followed by LMC and LQT1. (B) Goodness of fit (R2) of multivariate analysis using where k is the kth previous beats. R2 including previous 10 beats were 0.848 ± 0.043, 0.85 ± 0.002, and 0.792 ± 0.093 for LMC, LQT1, and LQT2 respectively. (C) Coefficients (α1 & α2) from multivariate regression analysis (* indicates p < 0.05, One-Way ANOVA tests were performed between three groups and significant difference were founded at the 0.05 level. The differences of α1 in LMC vs LQT1, LQT1 vs LQT2 and LMC vs LQT2 are significant at the 0.05 level by Fisher test and the differences of α2 in LMC vs LQT1 and LQT1 vs LQT2 are significant at the 0.05 level by Fisher test). (D) Spatial patterns of 1st coefficients (α1) in LMC, LQT1, and LQT2 hearts. Note that the map of α1 from LQT2 shows greater spatial heterogeneities (0.09–0.39) compared to that of LMC and LQT1 hearts (standard deviation of slope map = 0. 064 ± 0.025 in LQT2 vs. 0.029 ± 0.008 and 0.030 ± 0.014 in LQT1 and LMC, n = 4 hearts each, p < 0.05, Student’s t-test where appropriate). (E) Spatial patterns of 1st and 2nd coefficients (α1 & α2) in LQT2. The map of α2 shows a spatial gradient with higher slope at the apex than the base, different from the α2 map. The α1 vs. α2 plot in the right panel shows negative correlation (−0.27 ± 0.10 in LQT2 vs. −0.07 ± 0.15 in LQT1, p < 0.05, n = 6 hearts, Student’s t-test where appropriate), indicating that the gradient direction in α2 is opposite that in α1.
Heterogeneous restitution and short-term memory increases APD dispersion under short-long CL combination in LQT2
We previously reported that LQT2 hearts exhibited heterogeneous APD restitution associated with increased vulnerability to discordant alternans and reentry formation25. Heterogeneous restitution was also observed during the random stimulation protocol, manifesting as steeper APD restitution slope at the base than that at the apex in LQT2 (left panel in Fig. 5D). In contrast, LMC and LQT1 show much less slope dispersion (middle and right maps in panel D), indicating that APD restitution is more heterogeneous in LQT2.
We further examined whether the short-term cardiac memory effect was heterogeneous in LQT2. Figure 5E shows the α1 and α2 maps from multivariate analysis (see Methods). The α2 map (middle) shows heterogeneity between apex and base, indicating that the short-term cardiac memory effect in LQT2 is also heterogeneous. Interestingly, the gradient pattern of the α2 map (middle) is not the same as that of the α1 map (left). The correlation between α1 and α2 is negative, indicating that the region of steep APD restitution has a larger short-term memory effect that can dampen the APD prolongation caused by a pause.
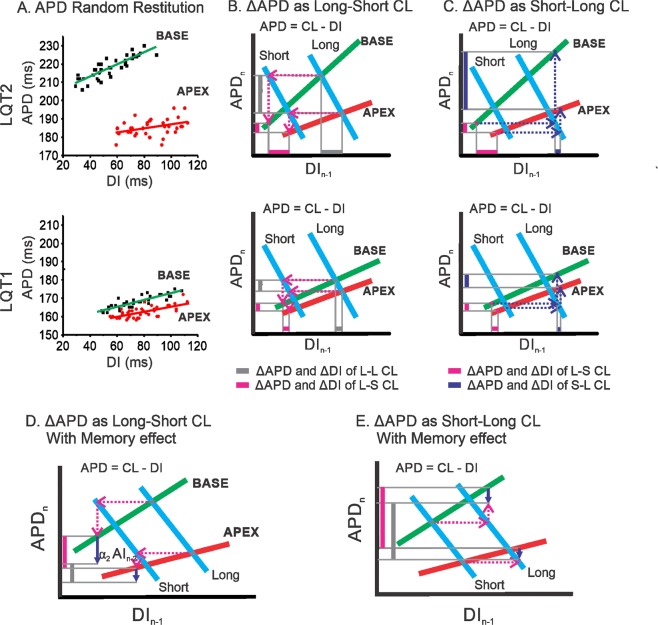
The gradient pattern of APD dispersion is determined mainly by APD restitution slope of the first beat (α1). Since α2 inversely correlates with α1, α2 (short-term memory) negatively impact on APD, dampening APD dispersion in LQT2. When the 2nd previous CL is short, this dampening effect is abolished, leaving full exposure of APD dispersion in LQT2 rabbits (see Fig. 7 and discussion for detail).
Figure 7.
Mechanisms of short-long CL enhancing APD dispersion in LQT2 (top) but not in LQT1 (bottom). (A) Scatter plot of APD vs. DI from base and apex showing heterogeneous restitution in LQT2, while heterogeneity in restitution is small in LQT1. (B) Illustration of enhanced APD dispersion under long-short CL. The red/green lines represent apex and base APD restitution curves, and the blue lines are the plots of the functional relation between APD and DI for a fixed CL, i.e., APD = CL − DI. The vertical bars indicate APD dispersion from long-long (grey) followed by a single short CL (magenta). (C) Enhanced APD dispersion in LQT2 under short-long CL changes due to heterogeneous restitution (purple vertical bar). (D) Illustration of APD dispersion reduced by the short-term memory effect in short-long CL. (E) Illustration of APD dispersion reduced by the short-term memory effect in long-short CL. The purple downward arrows indicate the APD adaptation direction and magnitude by the short-term memory effect of the previous CL (). In short-long CL, APD dispersion is less reduced by the short-term memory effect than in long-short CL. The step-by-step animation for this figure is available as a supplementary movie.
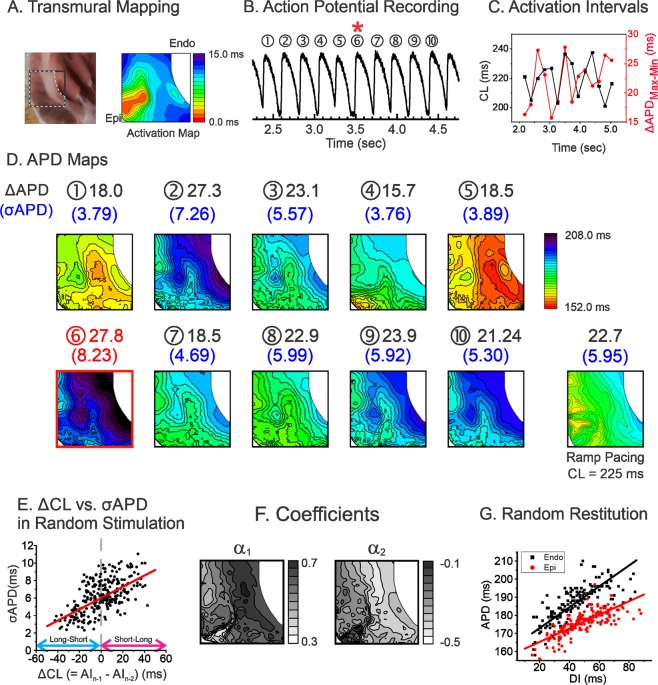
We further investigated APD dispersion dynamics under CL variations across the endocardium to the epicardium in the left ventricles (LV) of LQT2 hearts (n = 3). Figure 6 shows an example of APD dispersion recorded from LV wedge preparation during the random pacing protocol. The maximum APD dispersion of LV wedge preparation was also associated with a short-long CL pattern (Fig. 6C). The multivariate analysis revealed that the coefficient α1 was 0.502 ± 0.130 and α2 was negative (−0.213 ± 0.100, Fig. 6F). The heterogeneities of α1 and α2 were also present transmurally; see Fig. 6G, endocardium = 0.578 (black) vs. epicardium (red) = 0.375. The spatial correlation between α1 and α2 was negative (−0.847 ± 0.067), indicating that the region with a steeper APD restitution (endocardium) has a larger short-term cardiac memory effect than the region with a shallower APD restitution (epicardium). The combined epicardial and transmural mappings show that a short CLn−2 weakens the short-term memory effect that decreases APD dispersion caused by large APD restitution heterogeneity in LQT2.
Figure 6.
Influence of CL variation on APD dispersion across epicardium and endocardium of LV wedge preparation of LQT2 heart. (A) Location of transmural mapping and a typical example of activation map paced from the epicardium. (B) Trace of action potentials during random stimulation. (C) Corresponding mean CLs (black) and ΔAPDmax-min (red) in panel (B,D) APD maps corresponding to the action potentials shown in panel B. The beat with maximum APD dispersion is marked with a red square (the 6th beat, ΔAPDmax-min = 27.8 ms, σAPD = 8.23 ms). The corresponding beat of the maximum APD dispersion is marked with a red star in panels B and C. The APD map from S1S1 pacing at a CL closest to the average CLs of random stimulation protocol is shown in the last panel (CL = 225 ms in this scan, ΔAPDmax-min = 22.7 ms, σAPD = 5.95 ms). (E) Correlation analysis of alternating CL preceding σAPD in random stimulation protocol. ΔCL vs. σAPD shows a positive association similar to the result from the anterior region of LQT2 in Fig. 3. (F) Spatial patterns of 1st and 2nd coefficients (α1 & α2) in the transmural region of LQT2. (G) Scatter plot of APD vs. DI from the base and apex showing heterogeneous restitution in LQT2. The random restitution slope of the endocardium (0.58) is steeper than that of the epicardium (0.37).
Discussion
APD dispersion and steep restitution have long been suspected as mechanisms underlying long QT-related arrhythmias in clinical, drug/transgenic animal and computation modeling studies7,9,10,23,26–30. We investigated rate-dependent APD dispersion dynamics in transgenic rabbit models of LQTS using a comprehensive stimulation protocol and found that LQT2 rabbits (but not LQT1 rabbits) show enhanced APD dispersion in response to short-long CL changes due to heterogeneous APD restitution and the short-term cardiac memory effect.
Different types of LQTS may have different mechanisms of initiation and maintenance of arrhythmias31,32. Sympathetic tone such as exercise is a predominant trigger in LQT1, while majority of cardiac events in LQT2 patients occur during rest/sleep or sympathetic surge such as an auditory stimulus32. The majority of documented arrhythmias in congenital long QT syndrome patients were ‘pause’ dependent. LQT2 patients show short-long-short initiation pattern preceding pVTs, while increasing CLs are found in LQT1 patients2,3, associate with differential sympathetic trigger conditions. We previously reported that the short-long pattern preceded pVT initiation in LQT2 but not in LQT1 rabbits23,24, suggesting that ‘pause’ is a unique feature of pVT initiation in LQT2.
Computer modeling and experimental data7,33–35 suggest that the post-pause prolongation of APD is a major reason for EAD formation through providing time for the recovery and the reactivation of L-type Ca2+ current, which generates depolarizing currents of EADs. In addition to the effect of the immediate pause on APD, our multivariate analysis of APD restitution shows the importance of two previous CLs, short-long CLs, that prolong APD even more. The prolongation of APD by short-long CLs may further increase the risk for EAD formation in LQT2.
The hallmark of substrates for arrhythmias is dispersion of repolarization, which allows unidirectional conduction block and reentry formation36–40. In addition, large APD dispersion can initiate tissue-scale PVCs9,10, suggesting large APD dispersion itself can act as both reentrant substrate and trigger. Indeed, dispersion of repolarization has been implicated as an underlying mechanism of LQT-related arrhythmias in both previous pharmacological and transgenic animal models6,23,27,41–43. Ikr blockade using E-4031 or sotalol increases the transmural APD gradient in canine hearts8,44 and between the apex and base in rabbit hearts41 and LQT transgenic mice27.
APD dispersion in LQTS can be dynamic, and several groups have shown a close correlation between ‘pause’ and greater APD dispersion in drug-induced animal models of LQTS7,8. The current study investigates the dynamic modulation of APD dispersion in the heart with varying heart rates. In addition to a simple ‘pause’-dependent increase of APD dispersion, we found that short CL before the pause can further enhance APD dispersion in LQT2. Compared to LQT1, APD and its dispersion in LQT2 are largely dependent on multiple previous CLs (Fig. 4A–C). Although LQT1 had longer APD than LMC in our transgenic models, LQT1 did not show short-long CL-dependent APD dispersion, in line with clinical observations that the short-long pattern was limited to LQT2 patients2,3.
The short-term cardiac memory effect can be considered an additional factor enhancing APD dispersion in LQT2 as well as heterogeneous APD restitution (Fig. 5D). Our experimental results show that APDs are dependent on at least two previous CLs (Fig. 5A–C). The coefficients from multivariate regression analysis show that 1) two previous CLs are enough to account for most of APD variation (R2 > 0.7); 2) LMC and LQT2, but not LQT1, are inversely influenced by the second previous CLs (α2 < 0); and 3) the α2 map does not resemble the α1 map, suggesting a heterogeneous short-term memory effect.
Figure 7 illustrates how heterogeneities in APD restitution and short-term memory develop greater APD dispersion in LQT2 by short-long RR intervals but not in LQT1 (the step-by-step progress of the iterations from basal CL to short and long CL changes is available as an online supplementary movie). Two restitution curves are shown in Fig. 7A, representing heterogeneous APD restitution from base (green) and apex (red) in LQT2 (top) and LQT1 (bottom). LQT2 shows greater APD and restitution slope dispersion between the base and apex than LQT1. Panel B shows APD dispersion dynamics from the basic long-long CL (grey) followed by a short CL (magenta). The short CL shortens APD in both apex and base, resulting in smaller APD dispersion. Therefore, it creates a uniform DI distribution for the following beat. When CL increases again, a uniform DI distribution (purple) creates a larger APD gradient between apex and base (purple bar in the Y axis) due to steep APD restitution in the base. In addition, the heterogeneous short-term memory effect modulates APD dispersion through further shortening of APD at the base (blue arrows in Fig. 7D,E). Since APD dispersion is reduced by |Δα2CLn−2|, APD dispersion is greater under short-long CL than long-short CL in LQT2 (see Fig. 7D,E).
The magnitude of α2 is about 13% of α1 and when large CLs variation occurs such as characteristic short-long RR intervals found during pVT initiation in LQT2 rabbits, its contribution can be estimated to be 28 ms (α2 × 700 ms CL = 0.04 × 700 ms), which is a significant impact on APDs in rabbits. If LQT1 and LQT2 are compared, the estimated APD changes by α2 by ΔCL = 700 ms will be −7 ms in LQT1 vs. 28 ms in LQT2, showing a greater effect of short-term memory on APDs in LQT2 rabbits.
The heterogeneous short-term memory effect (largest at the base, where APD is largest) can reduce APD dispersion by . Therefore, when CLn−2 is larger (long-long CL case), APD dispersion can be reduced by short-term memory effect and conversely, short CLn-2 eliminates the dampening effect by short-term memory to increase APD dispersion. These results indicate that APD dispersion is enhanced under short-long alternating cycles in LQT2 because of small short-term cardiac memory effect caused by short .
APD dispersion is determined by intrinsic heterogeneity of ion channel expressions. it is well documented that several ionic currents are heterogeneous in the heart, – apico-basal heterogeneity of IKs, Ito and IKr45,46, transmural heterogeneity of IKs47,48 and Ito49, and RV-LV heterogeneity of Ito50. These ion channel expression patterns can greatly influence short-term cardiac memory and APD dispersion.
The larger short-term cardiac memory effect in LQT2 compared to LQT1 can be linked to the role of IKs as a dominant repolarizing current when IKr is absent. Due to its slow activation and inactivation kinetics, IKs has been linked to short-term cardiac memory51–53 and can dynamically create APD dispersion54. This is in agreement with the negligible α2 in LQT1, where IKs is lacking. Interestingly, the short-term memory effect is stronger in LMC than LQT2, potentially due to the small reduction of IKs (~20%) in our transgenic animal model of LQT223. The correlation analysis between the first and the second coefficients also shows a similar tendency, i.e., largest in LMC (−0.41), followed by LQT2 (−0.26), and negligible in LQT1 (−0.07). Under short CL, IKs (a major determinant of short-term cardiac memory) accumulates due to incomplete deactivation, causing shortening of the APD. Following the long CL, IKs channels are deactivated, resulting in APD prolongation. Since the expression of IKs is reported to be heterogeneous46, Iks heterogeneity may contribute to enhanced APD dispersion under short-long CL.
Another potential source of short-term cardiac memory is Ito. The heterogeneous expression of Ito has been well documented and influence APD dispersion transmurally, RV vs. LV, and apex-base direction. Due to its relatively rapid turnover of expression, it has been linked to pacing-induced T-wave memory55,56. Ito has been also implicated in the genesis of APD alternans57 and EAD-induced complex APD instability through its modulation of short-term cardiac memory58. In our current stimulation protocol with short-long CLs, the short CLn−2 can accelerate inactivation of Ito and the long CLn−1 can provide the sufficient time to recover from the inactivation, which exposes the largest impact of Ito heterogeneity on APD and may increase APD dispersion. However, the interpretation should be cautious because Ito can influence APD indirectly by modulating other ionic currents and its consequence is difficult to predict. Further studies are needed to delineate its exact roles in cardiac short-term memory and APD dispersion in long QT syndrome.
Conclusions
In the present study, we demonstrate that APD in LQT2 rabbits is highly dynamic and depends on preceding CL changes. Combined with heterogeneous APD restitution, this property of CL-dependent APD adaptation, known as short-term cardiac memory, promotes greater APD dispersion in LQT2 compared to LQT1 and LMC rabbits. Our results suggest that rate-dependent APD dispersion dynamics plays an important role in determining the genotype-specific initiation of malignant arrhythmias in LQTS.
Study limitations
Our study was limited to APD dispersion from the anterior surface and transmural mapping of LV without sympathetic stimulation in a narrow short diastolic interval range (<50 ms). This range was chosen to finish pacing protocol without conduction block and tissue-scale PVCs9,10 (1/12 random stimulation caused ventricular tachycardia in n = 1/6 LQT2 hearts) and to have relatively linear restitution curve for multivariate analysis. LQT1 hearts demonstrated frequent EADs and pVT induction under isoproterenol, and LQT2 hearts showed time-dependent adaptation of APD under isoproterenol59, which makes it difficult to investigate APD dispersion dynamics under isoproterenol with the random CL stimulation protocol. Previous studies60,61 indicated that sympathetic nerve stimulation increases APD dispersion due to heterogeneous distribution of sympathetic nerve endings, which cannot be reproduced pharmacologically with isoproterenol. Our study focused on APD dispersion dynamics in a short diastolic interval range (<50 ms) to apply multivariate analysis; however, the relationship between APD dispersion and arrhythmogenesis including reentry or EAD formation remains unclear. Further studies are required to understand the role of APD dispersion in arrhythmogenesis.
Material and Methods
Heart preparations
Littermate control (LMC), LQT1, and LQT2 rabbits of both sexes, averaging 16.5 months old/4.2 kg body weight/9.14 g heart weight, were euthanized with buprenorphene (0.03 mg/kg IM), acepromazine (0.5 mg.kg−1 IM), xylazene (15 mg.kg−1 IM), ketamine (60 mg.kg−1 IM), pentothal (35 mg.kg−1 IV), and heparin (200 U.kg−1). This investigation conformed to the current Guide for Care and Use of Laboratory Animals published by the National Institutes of Health (NIH Publication No. 85-23, revised 1996) and approved by the Lifespan Animal Welfare Committee at Rhode Island Hospital. Hearts were excised and retrogradely perfused through the aorta in a Langendorff perfusion system (Radnoti Glass Technology, Monrovia) with (in mmol.L−1) 130 NaCl, 24 NaHCO3, 1.0 MgCl2, 4.0 KCl, 1.2 NaH2PO4, 5 Dextrose, 25 Mannitol, 1.25 CaCl2, at pH 7.4, and gassed with 95% O2 and 5% CO2. In total, 23 rabbits were studied: LMC (n = 9), LQT1 (n = 5) and LQT2 (n = 9). Blebbistatin (5 μmol.L−1) was perfused to reduce movement artifact62.
Optical mapping
The optical apparatus has been previously described63. Fluorescence images from the anterior surface and LV free wall of the heart were captured using a CMOS camera (100 × 100 pixels, Ultima-L, SciMedia, Japan), and the field of view was set to 2.0 × 2.0 cm2 (spatial resolution of 200 × 200 μm2, Fig. 8A). The sampling rate was set to 1,000 frames.s−1, and data were analyzed with a custom-built software program developed in Interactive Data Language (Exelis, Inc., Boulder). Hearts were stained with a voltage-sensitive dye, di-4-ANEPPS (Invitrogen, Carlsbad), using 25 μL of stock solution (1 mg.ml−1 of dimethyl sulfoxide, DMSO) delivered through a bubble trap, above the aortic cannula. ECG and perfusion pressure were continuously monitored (PowerLab, ADInstruments, Colorado Springs).
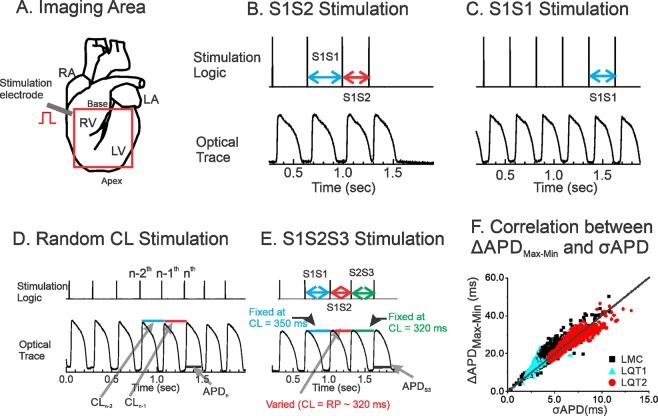
Figure 8.
Experimental method. (A) Schematics of imaging area and stimulation site. (B) S1S2 protocol. (C) Ramp pacing. (D) Random interval stimulation. CLn − 1; Activation Interval between nth and n−1th beats. (E) S1S2S3 protocol. S1S2 was progressively shortened from 320 ms to the refractory period, while S2S3 was fixed at CL = 320 ms. (F) Correlation between σAPD and ΔAPDmax-min from LMC (black), LQT1 (blue), LQT2 rabbit hearts (red). ΔAPDmax-min and σAPD were calculated from n = 5 hearts per group, about 315 beats per heart during random stimulation. σAPD, equivalent to 0.25 times of ΔAPDmax-min (R2 = 0.99), is used to estimate APD dispersion to normalized recording region because of robustness to variation in pixel numbers after removing outliers and low-amplitude signals.
Stimulation protocol
S1S2 pacing protocol: A conventional S1S2 pacing protocol was applied to measure refractoriness and APD restitution. Typically, 20 beats of constant CL (S1S1 = 350 ms) were applied, followed by a shorter (S1S2) interval. The S1S2 interval was decreased from 300 ms in 10-ms increments until it missed capture (Fig. 8B).
Ramp pacing protocol: After S1S2 and random CL pacing, the hearts were given 10 min to recover prior to ramp pacing (Fig. 8C). Hearts were paced at CLs that were successively decreased by 10 ms until loss of 1:1 capture or induction of ventricular fibrillation or ventricular tachycardia23,64,65.
Random CL pacing protocol: The pacing CLs were computer generated using a uniform random number generator, which varied within a 50-ms interval extending from the tissue refractory period measured from S1S2 protocol as described earlier19. The 50 ms range of DI was chosen because the dynamic APD restitution curve in this range can be assumed to be linear [19 and see Fig. 8D]. In addition, this range of short DI did not allow additional triggered activity such as early afterdepolarizations, so that multiple linear regression analysis can be applied (Fig. 8D).
S1S2S3 pacing protocol: To quantify the short-term memory effect on APD and APD dispersion, the S1S2 stimulation protocol was extended to include S2S3 stimulation, in which the S2S3 interval was fixed at 320 ms but the S1S2 was varied. Similar to S1S2 pacing, 20 beats of constant CL (S1S1 = 350 ms) were applied, followed by a variable S1S2 (from 300 ms to the refractory period with a 10 ms increment) and a fixed S2S3 at 300 or 320 ms, and the APD and APD dispersion of beat S3 were plotted as a function of S1S2. Since S2S3 is fixed, this pacing protocol measures the effect of S1S2 on APDn and its dispersion exclusively without the influence from CLn−1 (Fig. 8E).
Data analysis
The activation and repolarization time points at each site were determined from fluorescence (F) signals by calculating (dF/dt)max and (d2F/dt2)max. Data were filtered using a spatial Gaussian filter (3 × 3 pixel), and first/second derivatives were calculated using a temporal polynomial filter (3rd order, 13 points). Pixels with low signal-to-noise ratio determined by (dF/dt)max (lower than 3 × σ of baseline) and outliers of pixels determined by Grubbs’ test were removed from analysis.
APD dispersion was defined as standard deviation of APD (σAPD), because the standard deviation was robust to variation in pixel numbers after removing outliers and low-amplitude signals. σAPD and the ΔAPDmax-min, which was defined as differences between 99% quartile (APDmax) and 1% quartile (APDmin) of spatial APD distributions, have positive correlation with 4.01 coefficient value as shown in Fig. 8F, and σAPD is equivalent to 1/4th of ΔAPDmax-min.
Multivariate analysis of APD and previous CLs
Multivariate analysis of APD from random CL stimulation was carried out as previously described19 to quantify the short-term cardiac memory effect. Briefly, CLs were calculated by subtracting the previous activation time from the next activation time. APDs were measured from individual pixels and as a result, series of CLs (CL1, CL2, …, CLn) and APDs (APD1, APD2, …, APDn) were calculated (see Fig. 8D). Then each APD was curve-fitted to the previous CLs using a linear regression model19. For example, each APD was fitted to its previous kth CLs as:
| 1 |
A minimum of 80 APs were analyzed for each multivariate linear regression model. At least three independent scans were analyzed from the same heart to verify reproducibility of the curve fitting.
Supplementary information
Mechanisms of short-long CL enhancing APD dispersion in LQT2
Acknowledgements
This work was supported by the National Heart, Lung, and Blood Institute at the National Institutes of Health [Grant number R01 HL-096669 to B.C. and R01 HL114784-01A2 and R01 HL110791-03 to G.K.].
Author Contributions
B.-R.C. and Z.Q. contributed to experimental design and B.-R.C. contributed to implementation of experiments. T.Y.K., P.J., J.M.H., Z.P., D.P., L.L.C., K.K. and B.-R.C. contributed to data acquisition. T.Y.K. and B.-R.C. contributed to data analysis. J.C. contributed to animal handling and genotyping L.Q.T. rabbits. X.P. and G.K. contributed to maintaining the colonies of transgenic L.Q.T. rabbits. T.Y.K., G.K., Z.Q. and B.-R.C. contributed to the writing of the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1038/s41598-019-51230-9.
References
- 1.Dessertenne F. La tachycardie ventricularire à deux foyers opposés variables. Arch Mal. Coeur. 1966;59:263–272. [PubMed] [Google Scholar]
- 2.Noda T, et al. Classification and mechanism of Torsade de Pointes initiation in patients with congenital long QT syndrome. Eur Heart J. 2004;25:2149–2154. doi: 10.1016/j.ehj.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 3.Tan HL, et al. Genotype-specific onset of arrhythmias in congenital long-QT syndrome: possible therapy implications. Circulation. 2006;114:2096–2103. doi: 10.1161/CIRCULATIONAHA.106.642694. [DOI] [PubMed] [Google Scholar]
- 4.Mazur A, Anderson ME, Bonney S, Roden DM. Pause-dependent polymorphic ventricular tachycardia during long-term treatment with dofetilide: a placebo-controlled, implantable cardioverter-defibrillator-based evaluation. J Am Coll Cardiol. 2001;37:1100–1105. doi: 10.1016/s0735-1097(01)01106-8. [DOI] [PubMed] [Google Scholar]
- 5.Viskin S, et al. Mode of onset of torsade de pointes in congenital long QT syndrome. J Am Coll Cardiol. 1996;28:1262–1268. doi: 10.1016/s0735-1097(96)00311-7. [DOI] [PubMed] [Google Scholar]
- 6.Restivo M, Caref EB, Kozhevnikov DO, El-Sherif N. Spatial dispersion of repolarization is a key factor in the arrhythmogenicity of long QT syndrome. J Cardiovasc Electrophysiol. 2004;15:323–331. doi: 10.1046/j.1540-8167.2004.03493.x. [DOI] [PubMed] [Google Scholar]
- 7.Liu J, Laurita KR. The mechanism of pause-induced torsade de pointes in long QT syndrome. J Cardiovasc Electrophysiol. 2005;16:981–987. doi: 10.1111/j.1540-8167.2005.40677.x. [DOI] [PubMed] [Google Scholar]
- 8.Shimizu W, Antzelevitch C. Cellular basis for long QT, transmural dispersion of repolarization, and torsade de pointes in the long QT syndrome. J Electrocardiol. 1999;32:177–184. doi: 10.1016/S0022-0736(99)90077-8. [DOI] [PubMed] [Google Scholar]
- 9.Huang X, Kim TY, Koren G, Choi BR, Qu Z. Spontaneous initiation of premature ventricular complexes and arrhythmias in type 2 long QT syndrome. Am J Physiol Heart Circ Physiol. 2016;311:H1470–H1484. doi: 10.1152/ajpheart.00500.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu W, et al. Mechanisms linking T-wave alternans to spontaneous initiation of ventricular arrhythmias in rabbit models of long QT syndrome. J Physiol. 2018;596:1341–1355. doi: 10.1113/JP275492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kobayashi Y, Gotoh M, Mandel WJ, Karagueuzian HS. Increased temporo-spatial dispersion of repolarization during double premature stimulation in the intact ventricle. Pacing Clin Electrophysiol. 1992;15:2194–2199. doi: 10.1111/j.1540-8159.1992.tb03046.x. [DOI] [PubMed] [Google Scholar]
- 12.Kobayashi Y, Peters W, Khan SS, Mandel WJ, Karagueuzian HS. Cellular mechanisms of differential action potential duration restitution in canine ventricular muscle cells during single versus double premature stimuli. Circulation. 1992;86:955–967. doi: 10.1161/01.CIR.86.3.955. [DOI] [PubMed] [Google Scholar]
- 13.Shimizu S, et al. Temporal and spatial dispersion of repolarization during premature impulse propagation in human intact ventricular muscle: comparison between single vs double premature stimulation. Europace. 2000;2:201–206. doi: 10.1053/eupc.2000.0100. [DOI] [PubMed] [Google Scholar]
- 14.Baher A, et al. Short-term cardiac memory and mother rotor fibrillation. Am J Physiol Heart Circ Physiol. 2007;292:H180–189. doi: 10.1152/ajpheart.00944.2005. [DOI] [PubMed] [Google Scholar]
- 15.Banville I, Chattipakorn N, Gray RA. Restitution dynamics during pacing and arrhythmias in isolated pig hearts. J Cardiovasc Electrophysiol. 2004;15:455–463. doi: 10.1046/j.1540-8167.2004.03330.x. [DOI] [PubMed] [Google Scholar]
- 16.Fox JJ, Bodenschatz E, Gilmour RF., Jr. Period-doubling instability and memory in cardiac tissue. Phys Rev Lett. 2002;89:138101. doi: 10.1103/PhysRevLett.89.138101. [DOI] [PubMed] [Google Scholar]
- 17.Otani NF, Gilmour RF., Jr. Memory models for the electrical properties of local cardiac systems. J Theor Biol. 1997;187:409–436. doi: 10.1006/jtbi.1997.0447. [DOI] [PubMed] [Google Scholar]
- 18.Watanabe MA, Koller ML. Mathematical analysis of dynamics of cardiac memory and accommodation: theory and experiment. Am J Physiol Heart Circ Physiol. 2002;282:H1534–1547. doi: 10.1152/ajpheart.00351.2001. [DOI] [PubMed] [Google Scholar]
- 19.Choi BR, Liu T, Salama G. Adaptation of cardiac action potential durations to stimulation history with random diastolic intervals. J Cardiovasc Electrophysiol. 2004;15:1188–1197. doi: 10.1046/j.1540-8167.2004.04070.x. [DOI] [PubMed] [Google Scholar]
- 20.Prudat Yann, Madhvani Roshni V., Angelini Marina, Borgstom Nils P., Garfinkel Alan, Karagueuzian Hrayr S., Weiss James N., de Lange Enno, Olcese Riccardo, Kucera Jan P. Stochastic pacing reveals the propensity to cardiac action potential alternans and uncovers its underlying dynamics. The Journal of Physiology. 2016;594(9):2537–2553. doi: 10.1113/JP271573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dvir H, Zlochiver S. Stochastic pacing effect on cardiac alternans–simulation study of a 2D human ventricular tissue. Conf Proc IEEE Eng Med Biol Soc. 2013;2013:1514–1517. doi: 10.1109/EMBC.2013.6609800. [DOI] [PubMed] [Google Scholar]
- 22.Wilson D, Ermentrout B. Stochastic Pacing Inhibits Spatially Discordant Cardiac Alternans. Biophys J. 2017;113:2552–2572. doi: 10.1016/j.bpj.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brunner M, et al. Mechanisms of cardiac arrhythmias and sudden death in transgenic rabbits with long QT syndrome. J Clin Invest. 2008;118:2246–2259. doi: 10.1172/JCI33578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Odening KE, et al. Pharmacogenomics of anesthetic drugs in transgenic LQT1 and LQT2 rabbits reveal genotype-specific differential effects on cardiac repolarization. Am J Physiol Heart Circ Physiol. 2008;295:H2264–2272. doi: 10.1152/ajpheart.00680.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ziv O, et al. Origin of complex behaviour of spatially discordant alternans in a transgenic rabbit model of type 2 long QT syndrome. J Physiol. 2009;587:4661–4680. doi: 10.1113/jphysiol.2009.175018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Antzelevitch C, Shimizu W, Yan GX, Sicouri S. Cellular basis for QT dispersion. J Electrocardiol. 1998;30:168–175. doi: 10.1016/S0022-0736(98)80070-8. [DOI] [PubMed] [Google Scholar]
- 27.London B, et al. Dispersion of repolarization and refractoriness are determinants of arrhythmia phenotype in transgenic mice with long QT. J Physiol. 2007;578:115–129. doi: 10.1113/jphysiol.2006.122622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Napolitano C, Priori SG, Schwartz PJ. Significance of QT dispersion in the long QT syndrome. Prog Cardiovasc Dis. 2000;42:345–350. doi: 10.1053/pcad.2000.0420345. [DOI] [PubMed] [Google Scholar]
- 29.Shimizu W, Antzelevitch C. Cellular and ionic basis for T-wave alternans under long-QT conditions. Circulation. 1999;99:1499–1507. doi: 10.1161/01.CIR.99.11.1499. [DOI] [PubMed] [Google Scholar]
- 30.Zareba W, Moss AJ. Dispersion of repolarization. Relation to heart rate and repolarization duration. J Electrocardiol. 1995;28(Suppl):202–206. doi: 10.1016/s0022-0736(95)80057-3. [DOI] [PubMed] [Google Scholar]
- 31.Shimizu W, Aiba T, Antzelevitch C. Specific therapy based on the genotype and cellular mechanism in inherited cardiac arrhythmias. Long QT syndrome and Brugada syndrome. Curr Pharm Des. 2005;11:1561–1572. doi: 10.2174/1381612053764823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schwartz PJ, et al. Genotype-phenotype correlation in the long-QT syndrome: gene-specific triggers for life-threatening arrhythmias. Circulation. 2001;103:89–95. doi: 10.1161/01.CIR.103.1.89. [DOI] [PubMed] [Google Scholar]
- 33.Viskin S, et al. Arrhythmias in the congenital long QT syndrome: how often is torsade de pointes pause dependent? Heart. 2000;83:661–666. doi: 10.1136/heart.83.6.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Viswanathan PC, Rudy Y. Pause induced early afterdepolarizations in the long QT syndrome: a simulation study. Cardiovasc Res. 1999;42:530–542. doi: 10.1016/S0008-6363(99)00035-8. [DOI] [PubMed] [Google Scholar]
- 35.January CT, Riddle JM. Early afterdepolarizations: mechanism of induction and block. A role for L-type Ca2+ current. Circ Res. 1989;64:977–990. doi: 10.1161/01.RES.64.5.977. [DOI] [PubMed] [Google Scholar]
- 36.Poelzing S, Rosenbaum DS. Nature, significance, and mechanisms of electrical heterogeneities in ventricle. The anatomical record. Part A, Discoveries in molecular, cellular, and evolutionary biology. 2004;280:1010–1017. doi: 10.1002/ar.a.20103. [DOI] [PubMed] [Google Scholar]
- 37.Janse MJ. Vulnerability to ventricular fibrillation. Chaos. 1998;8:149–156. doi: 10.1063/1.166295. [DOI] [PubMed] [Google Scholar]
- 38.Yuan S, et al. Dispersion of repolarization following double and triple programmed stimulation. A clinical study using the monophasic action potential recording technique. Eur Heart J. 1996;17:1080–1091. doi: 10.1093/oxfordjournals.eurheartj.a015005. [DOI] [PubMed] [Google Scholar]
- 39.Antzelevitch C, Fish J. Electrical heterogeneity within the ventricular wall. Basic Res Cardiol. 2001;96:517–527. doi: 10.1007/s003950170002. [DOI] [PubMed] [Google Scholar]
- 40.Gilmour RF, Jr., Gelzer AR, Otani NF. Cardiac electrical dynamics: maximizing dynamical heterogeneity. J Electrocardiol. 2007;40:S51–55. doi: 10.1016/j.jelectrocard.2007.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Choi BR, Burton F, Salama G. Cytosolic Ca2+ triggers early afterdepolarizations and Torsade de Pointes in rabbit hearts with type 2 long QT syndrome. J Physiol. 2002;543:615–631. doi: 10.1113/jphysiol.2002.024570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Antzelevitch C. Molecular biology and cellular mechanisms of Brugada and long QT syndromes in infants and young children. J Electrocardiol. 2001;34(Suppl):177–181. doi: 10.1054/jelc.2001.28865. [DOI] [PubMed] [Google Scholar]
- 43.Baker LC, London B, Choi BR, Koren G, Salama G. Enhanced dispersion of repolarization and refractoriness in transgenic mouse hearts promotes reentrant ventricular tachycardia. Circ Res. 2000;86:396–407. doi: 10.1161/01.RES.86.4.396. [DOI] [PubMed] [Google Scholar]
- 44.Shimizu W, Antzelevitch C. Sodium channel block with mexiletine is effective in reducing dispersion of repolarization and preventing torsade des pointes in LQT2 and LQT3 models of the long-QT syndrome. Circulation. 1997;96:2038–2047. doi: 10.1161/01.CIR.96.6.2038. [DOI] [PubMed] [Google Scholar]
- 45.Szentadrassy N, et al. Apico-basal inhomogeneity in distribution of ion channels in canine and human ventricular myocardium. Cardiovasc Res. 2005;65:851–860. doi: 10.1016/j.cardiores.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 46.Cheng J, et al. Heterogeneous distribution of the two components of delayed rectifier K+ current: a potential mechanism of the proarrhythmic effects of methanesulfonanilideclass III agents [see comments] Cardiovasc Res. 1999;43:135–147. doi: 10.1016/S0008-6363(99)00061-9. [DOI] [PubMed] [Google Scholar]
- 47.Liu DW, Antzelevitch C. Characteristics of the delayed rectifier current (IKr and IKs) in canine ventricular epicardial, midmyocardial, and endocardial myocytes. A weaker IKs contributes to the longer action potential of the M cell. Circ Res. 1995;76:351–365. doi: 10.1161/01.RES.76.3.351. [DOI] [PubMed] [Google Scholar]
- 48.Nerbonne JM, Guo W. Heterogeneous expression of voltage-gated potassium channels in the heart: roles in normal excitation and arrhythmias. Journal of cardiovascular electrophysiology. 2002;13:406–409. doi: 10.1046/j.1540-8167.2002.00406.x. [DOI] [PubMed] [Google Scholar]
- 49.Litovsky SH, Antzelevitch C. Rate dependence of action potential duration and refractoriness in canine ventricular endocardium differs from that of epicardium: role of the transient outward current. J Am Coll Cardiol. 1989;14:1053–1066. doi: 10.1016/0735-1097(89)90490-7. [DOI] [PubMed] [Google Scholar]
- 50.Choi BR, et al. Transient Outward K(+) Current (Ito) Underlies the Right Ventricular Initiation of Polymorphic Ventricular Tachycardia in a Transgenic Rabbit Model of Long-QT Syndrome Type 1. Circ Arrhythm Electrophysiol. 2018;11:e005414. doi: 10.1161/CIRCEP.117.005414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zeng J, Laurita KR, Rosenbaum DS, Rudy Y. Two components of the delayed rectifier K+ current in ventricular myocytes of the guinea pig type. Theoretical formulation and their role in repolarization. Circ Res. 1995;77:140–152. doi: 10.1161/01.res.77.1.140. [DOI] [PubMed] [Google Scholar]
- 52.Rudy Y. Molecular basis of cardiac action potential repolarization. Ann N Y Acad Sci. 2008;1123:113–118. doi: 10.1196/annals.1420.013. [DOI] [PubMed] [Google Scholar]
- 53.Rudy Y. Cardiac repolarization: insights from mathematical modeling and electrocardiographic imaging (ECGI) Heart Rhythm. 2009;6:S49–55. doi: 10.1016/j.hrthm.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 54.Viswanathan PC, Shaw RM, Rudy Y. Effects of IKr and IKs heterogeneity on action potential duration and its rate dependence: a simulation study. Circulation. 1999;99:2466–2474. doi: 10.1161/01.CIR.99.18.2466. [DOI] [PubMed] [Google Scholar]
- 55.Shvilkin A, et al. Evolution and resolution of long-term cardiac memory. Circulation. 1998;97:1810–1817. doi: 10.1161/01.CIR.97.18.1810. [DOI] [PubMed] [Google Scholar]
- 56.Geller JC, Rosen MR. Persistent T-wave changes after alteration of the ventricular activation sequence. New insights into cellular mechanisms of ‘cardiac memory’. Circulation. 1993;88:1811–1819. doi: 10.1161/01.CIR.88.4.1811. [DOI] [PubMed] [Google Scholar]
- 57.Qu Z, Xie Y, Garfinkel A, Weiss JN. T-wave alternans and arrhythmogenesis in cardiac diseases. Front Physiol. 2010;1:154. doi: 10.3389/fphys.2010.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Landaw J, Qu Z. Memory-induced nonlinear dynamics of excitation in cardiac diseases. Physical review. E. 2018;97:042414. doi: 10.1103/PhysRevE.97.042414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liu GX, et al. Differential conditions for early after-depolarizations and triggered activity in cardiomyocytes derived from transgenic LQT1 and LQT2 rabbits. J Physiol. 2012;590:1171–1180. doi: 10.1113/jphysiol.2011.218164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mantravadi R, et al. Autonomic nerve stimulation reverses ventricular repolarization sequence in rabbit hearts. Circ Res. 2007;100:e72–80. doi: 10.1161/01.RES.0000264101.06417.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ng GA, et al. Sympathetic nerve stimulation produces spatial heterogeneities of action potential restitution. Heart Rhythm. 2009;6:696–706. doi: 10.1016/j.hrthm.2009.01.035. [DOI] [PubMed] [Google Scholar]
- 62.Fedorov V, et al. Application of blebbistatin as an excitation-contraction uncoupler for electrophysiologic study of rat and rabbit hearts. Heart Rhythm. 2007;4:619–626. doi: 10.1016/j.hrthm.2006.12.047. [DOI] [PubMed] [Google Scholar]
- 63.Choi BR, Jang W, Salama G. Spatially discordant voltage alternans cause wavebreaks in ventricular fibrillation. Heart Rhythm. 2007;4:1057–1068. doi: 10.1016/j.hrthm.2007.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Banville I, Gray RA. Effect of action potential duration and conduction velocity restitution and their spatial dispersion on alternans and the stability of arrhythmias. Journal of cardiovascular electrophysiology. 2002;13:1141–1149. doi: 10.1046/j.1540-8167.2002.01141.x. [DOI] [PubMed] [Google Scholar]
- 65.Hayashi H, et al. Dynamic origin of spatially discordant alternans in cardiac tissue. Biophys J. 2007;92:448–460. doi: 10.1529/biophysj.106.091009. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Mechanisms of short-long CL enhancing APD dispersion in LQT2