Abstract
Formalin or formaldehyde is commonly used for cadaver fixation, which is, however, not suitable for endoscopic transnasal skull base approach because of consequent hardening of the soft tissue. Several alternatives have been reported, but each of them also has some limitations. We applied a novel fixation method using N-vinyl-2-pyrrolidone (NVP), a precursor of the water-soluble macromolecular polymer, for endoscopic transnasal skull base approach in six donated cadaver specimens. In four cadavers, elasticity of the soft tissue in the nasal cavity was almost similar to that of living tissue, and a surgical approach similar to the real surgical field was possible. However, the soft tissue was moderately stiffer than living tissue in two specimens so that surgical manipulation was hindered to some extent while NVP concentration was 10% in all the cadavers. Since the brain tissue was too soft and pliable for surgical manipulation in NVP, more careful surgical manipulation than real surgical field was mandatory in order to prevent damage in the brain tissue. Therefore, this concentration of NVP was considered to be appropriate. In conclusion, NVP embalming was effective for endoscopic transnasal skull base approach in cadaver dissection, providing environment similar to the real surgical field.
Keywords: cadaver dissection, endoscopic transnasal skull base approach, N-vinyl-2-pyrrolidone
Introduction
In the recent neurosurgical settings, endoscopic transnasal approach has been widely applied to several skull base lesions, and its indication has rapidly growing as a less-invasive option.1,2) Due to its anatomical complexity, needs for cadaveric surgical training for this approach are also increasing and has continuously been performed worldwide.3)
For cadaver fixation, formalin or formaldehyde is commonly used.4) Because of consequent stiffness of the soft tissue, however, formalin-fixed cadaver is not suitable for transnasal skull base approach unless soft tissue structures in the nasal cavities are completely removed. In addition, because of its possible carcinogenesis,5,6) forced-air ventilation equipment in the dissection room is required in Japan. Several methods by which the body remains pliable and flexible have been devised such as the fresh-frozen method,7) the use of Thiel solution,8) and saturated saline.9) Our colleagues (M.N., G.M., and others) recently invented and reported the usefulness of a novel fixation method using N-vinyl-2-pyrrolidone (NVP),10) which is an organic compound with a five-membered lactam ring and a vinyl group. Hereby the authors report the usefulness of NVP embalming for endoscopic transnasal skull base approach in cadaver dissection.
Materials and Methods
Source of cadavers
All the six cadavers used in this study were donated to our institution (aged 72–96 years; 5 males, one female) (Table 1). Written comprehensive consent was obtained from the donors in advance, and from the families prior to and at donation, agreeing to body donation and its use for anatomical education, research, and clinical skill training.
Table 1.
Characteristics of six cadavers studied
| No. | Age | Sex | Body weight (kg) | Interval between death and injection | Interval between injection and dissection | Cause of death | Status of soft tissue | Status of the brain |
|---|---|---|---|---|---|---|---|---|
| 1 | 96 | M | 28 | 8 days | 7 months | Senility | Equivalent to living tissue | Too soft |
| 2 | 72 | M | 44 | 8 days | 7 months | Cancerous pleurisy | Equivalent to living tissue | Too soft |
| 3 | 88 | M | 47 | 1 day | 3 months | Aspiration pneumonia | Equivalent to living tissue | Too soft |
| 4 | 88 | F | 30 | 1 day | 2 months | Colon cancer | Equivalent to living tissue | Too soft |
| 5 | 88 | M | 40 | 2 days | 11 months | Rectal cancer | Moderately hard | Too soft |
| 6 | 85 | M | 65 | 2 days | 4 days | Metastatic liver cancer Rectal cancer | Moderately hard | Too soft |
M: male, F: female.
The research protocol was developed in strict accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects, and was approved by the Ethics Committee of our institution (approval number: 1112).
NVP embalming
“Preserve” solution, consisting of 100% NVP and <0.1% N,N′-dibutyl-phenylenediamine, was purchased from Nippon Medical and Chemical Instruments (Osaka, Japan). The femoral artery and contralateral common carotid artery were cannulated with a T-shaped cannula connected to Tygon tubes (6475-25; Yamato Scientific, Tokyo, Japan). Each cadaver was perfused with diluted “Preserve” solution via the cannula using a peristaltic pump (Masterflex L/S; Yamato Scientific; 8 mL/min, total 12 L). “Preserve” solution was diluted so that the final concentrations of NVP were 10% of the body weight. When the infusion was complete, the arteries were ligated and the body was immersed in 5 L of 5% “Preserve” solution in a sealed plastic bag and then stored at 4°C.10) Above-mentioned procedures are protected by several patents (patent No. 4374435, Tissue fixation method with hydrophilic macromolecule; patent No. 4956839, Tissue fixation method with monomer compound of hydrophilic macromolecule; patent No. 5840193, Infusion solution for cadaveric preservation).
Cadaver dissection
Two days before dissection, red silicone was injected into the bilateral common carotid and vertebral arteries, and blue one into the bilateral jugular veins. Transnasal approach using the NVP-embalmed cadavers were performed by an experienced neurosurgeon (K.M.) and an otolaryngologist (H.Y.) with rigid neuroendoscope with a diameter of 4 mm (Olympus Co., Tokyo, Japan). Following approaches and procedures were performed; standard transsphenoidal approach to the pituitary gland and the cavernous sinus; transtuberculum sellae approach to the suprasellar region; clivectomy and transclival approach to the basilar artery and the anterior aspect of the brainstem; pituitary transposition and approach to the basilar tip; lateral approach to the orbit; and transpterygopalatine fossa approach to the trigeminal nerve lateral to the internal carotid artery. After all the approaches, pedicled nasoseptal flap was harvested and placed to the sella turcica as previously reported.11)
Hardness of the cadaveric specimens in comparison to that of the living tissue was classified into five levels as follows: “too hard”, too hard to dissect and not appropriate for use; “moderately hard”, harder than the living tissue but applicable for use; “equivalent”, equivalent to the living tissue; “moderately soft”, softer than the living tissue but applicable for use; “too soft”, too soft to dissect and not appropriate for use, which was evaluated by both the neurosurgeon (K.M.) and the otolaryngologist (H.Y.).
Results
In four cadaveric specimens embalmed using NVP, the hardness of the soft tissue of the nasal cavity including nostril, superior, middle, and inferior turbinate was “equivalent”, and these were almost similarly soft and flexible in comparison to the living tissue (Table 1). Thus, these structures could be kept unremoved and were only retracted for various surgical approaches, and all the scheduled approaches were possible. Dissection environment was quite similar to the real surgical field in all the six cadaveric specimens. The pituitary gland and the cavernous sinus could be smoothly exposed via standard transsphenoidal approach (Fig. 1A). Transtuberculum sellae approach provided access to the suprasellar region (Fig. 1B). After clivectomy, we could approach the basilar artery and the anterior aspect of the brainstem by transclival approach (Fig. 1C). Pituitary transposition enabled access to the basilar tip (Fig. 1D). Via lateral approach, we could also obtain a corridor into the orbit. After transpterygopalatine fossa approach, the trigeminal nerve could be exposed (Figs. 2A and 2B). Pedicled nasoseptal flap could be easily and successfully harvested and placed to the sella turcica (Fig. 2C). During intradural manipulation in transtuberculum sellae approach and transclival approach, the brain tissue and the pituitary gland was “too soft”, pliable and easily damaged when compressed or retracted, while morphology of the brain was kept while it was untouched. Therefore, more careful surgical manipulation than that for real surgical field was mandatory inside the dura mater in order to prevent damage in the brain tissue.
Fig. 1.
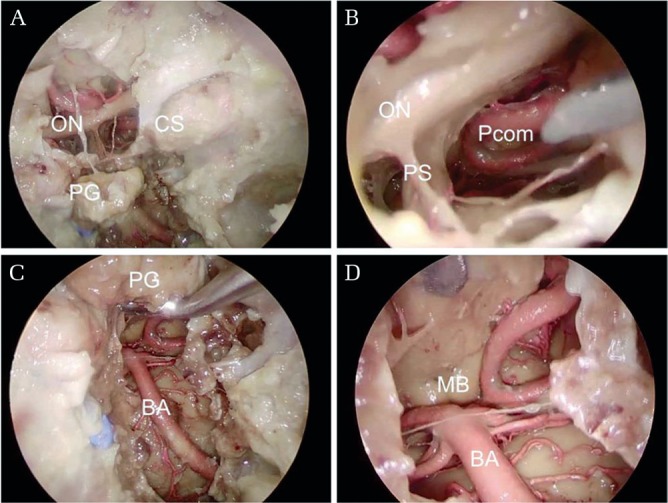
Dissection around the pituitary gland via endoscopic transnasal skull base approach in the NVP-embalmed cadavers (No. 3 in Table 1). (A) The pituitary gland (PG), the cavernous sinus (CS), and the optic nerves (ON) are visible after standard transsphenoidal approach and transtuberculum sellae approach. (B) Deep in the suprasellar area, the posterior communicating artery (Pcom) and the pituitary stalk (PS) are under direct vision. (C) Transposition of the pituitary gland and clivectomy provides exposure of full length of the basilar artery (BA). (D) Deeply, the bilateral mammillary bodies (MB) can be observed. Injection of blue silicone was insufficient probably because of insufficient irrigation and removal of thrombi inside the vessels before silicone injection, or hypoplasty of the internal jugular vein. NVP: N-vinyl-2-pyrrolidone.
Fig. 2.
Dissection around the pituitary gland (continued) via endoscopic transnasal skull base approach in the NVP-embalmed cadavers (No. 3 in Table 1). (A) Transpterygopalatine fossa approach provides access lateral to the internal carotid (IC) artery. (B) Enlarged view shows the trigeminal verve (V). (C) Nasoseptal flap (NF) can be placed to the sella turcica. NVP: N-vinyl-2-pyrrolidone.
In the remaining two specimens, soft tissue of the nasal cavity was “moderately hard” so that surgical manipulation was hindered to some extent. Hardness of the brain tissue was “too soft”, which was almost similar to the above-mentioned four specimens. Evaluation of the status of the tissue was concurrent between the neurosurgeon (K.M.) and the otolaryngologist (H.Y.) throughout the cadaveric specimens. In comparison of these two specimens and the others, no specific relationship was found in body weight at the time of death, interval between the time of death and the time of injecting NVP, interval between the time of injection and the time of dissection, and cause of death (Table 1).
Discussion
We found NVP embalming, as an alternative to formalin, was effective for endoscopic transnasal skull base approach in cadaver dissection, providing environment similar to the real surgical field. NVP has not only fixative effect, but also disinfectant and preservative effects.10) It has no carcinogenesis,5) is completely free of formalin, and requires no expensive ventilation equipment.10) Formalin alternatives also have following limitations. Fresh-frozen method does entail risks of infection and decomposition and requires large freezers.7) It also has limitation in preservation period (a few weeks at the most). In contract, NPV enabled long preservation period up to 11 months. The Thiel and saturated saline methods still involve low concentrations of formalin. In this manner, embalming using NVP is promising having great advantages, which are summarized in Table 2.
Table 2.
Advantage and disadvantage of several embalming methods
| Embalming methods | Advantage | Disadvantage |
|---|---|---|
| Formalin | Widespread | Stiffness of soft tissue |
| Easy to handle | Forced air ventilation required | |
| Fresh frozen | No stiffness | Large freezer required |
| Limited preservation period | ||
| Saturated saline | No stiffness | Preservation period unknown |
| Contain formalin (low concentration) | ||
| Thiel | No stiffness | Contain formalin (low concentration) |
| NVP | No stiffness | Softness of brain tissue |
| Long preservation period |
NVP: N-vinyl-2-pyrrolidone.
The reason for the difference in hardness of soft tissues between specimens is speculative. It might be due to individual variation of body fat percentage or muscle mass. Since these parameters were not collected, body weight of six specimens was shown instead. However, we found any significant difference in body weight was found between two stiffer specimens and the others (Table 1). Interval between the time of death and time of injection was also not significantly different between these two groups. Thus, the mechanisms for the difference in hardness remain as the issue to be solved.
N-vinyl-2-pyrrolidone also have several drawbacks. Flexibility tended to decrease with increasing NVP concentration, and the brain tissue was too soft for dissection even with highest concentration of 20%.10) Because the brain tissue was too soft for dissection in all our specimens, NVP would not be appropriate for the dissection of the brain parenchyma including fiber dissection. Because the soft tissue in the nasal cavity in our specimens could be hardened even without increasing the NVP concentration, increasing the concentration more than 20% to maintain hardness of the brain would lead to further hardness of the soft tissue. Thus, 10%, which was used in this study, would be the appropriate concentration.
Hereby we only reported initial experience with qualitative results by subjective assessment. Quantitative assessment by objective method to describe the status of soft tissue including elastography or ultrasonic examination to assess tissue stretch ability would be necessary in the future.
Conclusion
N-vinyl-2-pyrrolidone embalming, as an alternative to formalin, was effective for endoscopic transnasal skull base approach in cadaver dissection, providing environment similar to the real surgical field.
Footnotes
Conflicts of Interest Disclosure
All authors have no conflicts of interest.
References
- 1).Kassam AB, Gardner P, Snyderman C, Mintz A, Carrau R: Expanded endonasal approach: fully endoscopic, completely transnasal approach to the middle third of the clivus, petrous bone, middle cranial fossa, and infratemporal fossa. Neurosurg Focus 19: E6, 2005 [PubMed] [Google Scholar]
- 2).Zwagerman NT, Zenonos G, Lieber S, et al. : Endoscopic transnasal skull base surgery: pushing the boundaries. J Neurooncol 130: 319–330, 2016 [DOI] [PubMed] [Google Scholar]
- 3).Dallan I, Castelnuovo P, Seccia V, et al. : Combined transnasal transcervical robotic dissection of posterior skull base: feasibility in a cadaveric model. Rhinology 50: 165–170, 2012 [DOI] [PubMed] [Google Scholar]
- 4).Blum F: [The formaldehyde as a fixation agent]. Z Wiss Mikrosk 10: 314–315, 1893. (in German) [Google Scholar]
- 5).International Agency for Research on Cancer: Formaldehyde, 2-Butoxyethanol and 1-tert-Butoxy-2-propanol. Lyon, International Agency for Research on Cancer Monographs on the evaluation of carcinogenic risks to humans, Vol. 88, 2006 [PMC free article] [PubMed] [Google Scholar]
- 6).Nielsen GD, Larsen ST, Wolkoff P: Re-evaluation of the WHO (2010) formaldehyde indoor air quality guideline for cancer risk assessment. Arch Toxicol 91: 35–61, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7).Macchi V, Munari PF, Brizzi E, Parenti A, De Caro R: Workshop in clinical anatomy for residents in gynecology and obstetrics. Clin Anat 16: 440–447, 2003 [DOI] [PubMed] [Google Scholar]
- 8).Thiel W: [The preservation of the whole corpse with natural color]. Ann Anat 174: 185–195, 1992. (in German) [PubMed] [Google Scholar]
- 9).Hayashi S, Homma H, Naito M, et al. : Saturated salt solution method: a useful cadaver embalming for surgical skills training. Medicine (Baltimore) 93: e196, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10).Haizuka Y, Nagase M, Takashino S, Kobayashi Y, Fujikura Y, Matsumura G: A new substitute for formalin: application to embalming cadavers. Clin Anat 31: 90–98, 2018 [DOI] [PubMed] [Google Scholar]
- 11).Hadad G, Bassagasteguy L, Carrau RL, et al. : A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope 116: 1882–1886, 2006 [DOI] [PubMed] [Google Scholar]



