Abstract
Objectives
The aim of this study was to assess the initial outcome of non-operative, conservative management in selective penetrating abdominal injury in a tertiary care hospital.
Material and Methods
This was a cross sectional study done on purposively selected 36 patients with penetrating abdominal injuries of all ages admitted within 6 hours of the incident. All patients confirmed peritoneal breach and standard algorithm of management was followed. Closed monitoring was ensured with repeated investigations at regular intervals. Outcome parameters included surgical site infection (SSI), fever, hypothermia, wound dehiscence, fecal fistula, length of stay, pulmonary complication and death.
Results
A total of 36 patients with a mean age of 30 years (SD= 6.7), consisting all males, mostly (58%) from rural areas and 73% from low socioeconomic condition. Site of injury was noted in the epigastrium (42%) and right iliac region (22%). Among them, 33 (92%) patients were successfully managed with non-operative management and 3 (8%) patients needed laparotomy. Routine imaging and clinical observation could detect hollow viscus injury within 36 hours in 3 patients. Hospital stay was significantly lower ( <7 days) in conservative management.
Conclusion
Clinical examination alone and/or together with different diagnostic methods could reduce the number of negative laparotomies and associated morbidities. Single surgeon must closely monitor a patient of penetrating abdominal injury and take vital decisions from the time of admission until discharge.
Keywords: Penetrating abdominal injury, non-operative management, conservative management
Introduction
Penetrating abdominal trauma is an important public health problem accounting for a substantial proportion of all trauma admissions at tertiary care hospitals, and it continues to be a major cause of homicidal injury in Bangladesh, and even in the United States. Among penetrating abdominal injuries (PAI) stab wounds (SW) are about three times more often than gunshot wounds (GSW). It is mentioned in many literatures that PAI was being managed conservatively until the early 1900s (1-3). Laparotomy became the standard practice during “World War I” with evidence of a better chance of survival than conservative management. But in 1960, Shaftan, reported a high rate of negative laparotomies and managed 125 of 180 patients with PAI without surgery, with a mortality rate less than 1% (4). Since then, pendulum started to shift towards selective non-operative management (SNOM) for PAI. Nowadays, with the advent of minimal access surgery and modern imaging tools such as high resolution ultrasonogram, computed tomography (CT) scan laparotomy is almost avoidable because of its improved diagnostic facility, great therapeutic role and least surgical stress as well.
Current guideline allows to delay laparotomy with close observation for hemodynamically stable patients with no signs of peritonitis for PAIs even GSWs (5-6). In the United States, SNOM has become the standard care in abdominal SWs, and up to 55% of anterior abdominal SWs could be managed conservatively (7). Even with peritoneal breach, a considerable number of patients might have no other major intra-abdominal injury that necessitates operative management (3).
Among all trauma patients, many of them with penetrating abdominal injuries are admitted in Dhaka Medical College Hospital from all over the country every day. Most of them are transported from very far and get delayed. Majority of those patients do not have any primary management or resuscitation on the way. After admission, many of them cannot afford treatment cost. After negative exploratory laparotomy, patients might become the victims of anesthetic hazard, followed by wound infection, longer stay, increased treatment cost, higher morbidity and even death. These morbidity and mortality could be reduced by choosing selective criteria for conservative management when possible. Our observational study evaluated the outcome of non-operative management in selective PAIs with close monitoring.
Patients and Methods
This cross-sectional study was performed at the casualty unit of Dhaka Medical College Hospital Bangladesh over a period of one year (February 2011 to January 2012) in the accident center of a hospital. The study included a total of 36 penetrating abdominal injury patients of all ages, presented within 6 hours of the incident according to our selection criteria (Table 1). Institutional ethical committee clearance for collection of data and informed written consent was taken from the selected patients for conservative management.
Table 1. Inclusion and exclusion criteria for conservative approach in our study.
| Inclusion criteria |
| • Penetrating injury inanterior abdominal wall. • Hemodynamically stable patients. • Patients notdeveloped the signs ofperitonitis. • Patient admitted tohospital within 6 hours ofinjury |
| Exclusion criteria |
| • Poly trauma patients(head injury, limbfractures and perineal injuries. • Presence ofperitoneal collectiondetected by FAST • Patient’s with previoushistory of majorabdominal surgery. • Patients with gunshotinjury. • Patient’s with knowncase diabetes mellitus,chronic liver, renal, & cardiovascular disease. |
| FAST: Focused assessment with sonography for trauma. |
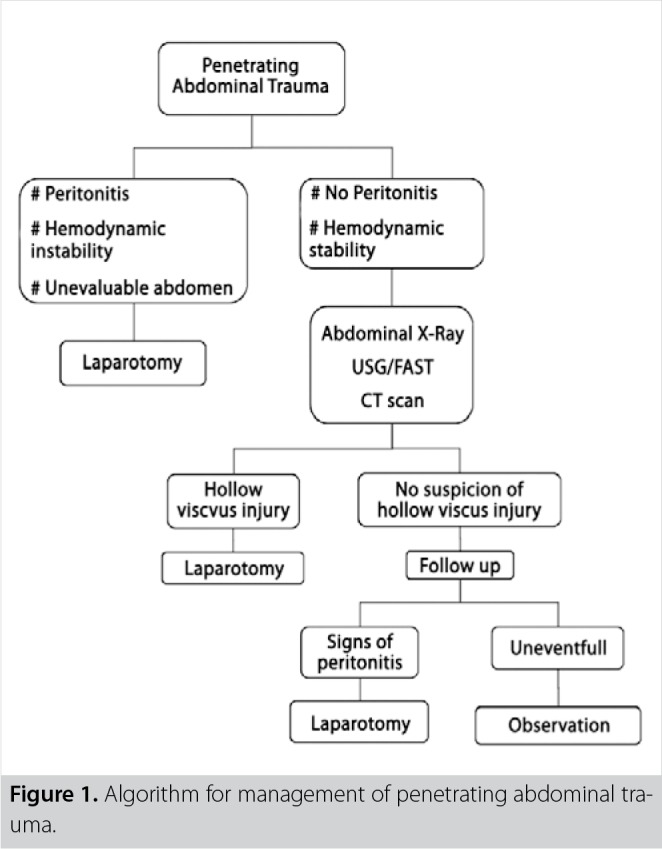
The selected patients were evaluated by standard ATLS protocol and side by side resuscitated and then routine hematological, biochemical, focused assessment with sonography for trauma (FAST) and other common radiological imaging studies were performed. We didn’t routinely practice computed tomography (CT) scan in our study because CT is generally a poor predictor of intestinal injury and pneumoperitoneum is often missed. Moreover, contrast material is not safe because of the risk of aspiration, hypersensitivity, nephrotoxicity and delay of the procedure. All patients underwent surgical toileting of the penetrating wound under local anesthesia and peritoneal breach was confirmed and repaired with or without drain. Standard algorithm of management was followed (Figure 1) (3).
Figure 1. Algorithm for management of penetrating abdominal tra- uma.
All patients were managed initially by nothing per oral (NPO) with continued nasogastric suction, urinary bladder catheterization, maintenance intravenous fluids, tetanus prophylaxis, prophylactic broad-spectrum antibiotics with metronidazole, adequate analgesics and regular motoring of hemodynamic status and vital signs with date and time were recorded and complete physical examination was done to see the associated injuries and neurological status. Plain abdominal radiograph in erect posture was done 12 hourly and abdominal ultrasonogram (USG) daily for the first 48 hours. Routine hematological and biochemical studies were repeated if needed. Oral feeding was resumed on the 3rdday in responding patients. Non-responding patients, developing any feature of peritonitis including abdominal rigidity, tenderness, fever, unresolved and progressive pneumoperitoneum or peritoneal collection or significant drop of hematocrit requiring blood transfusion were explored surgically immediately. Otherwise, the patients were discharged from the 3rdday onwards unless further inpatient care required.
Outcome parameters included number of patients managed conservatively and the rate of surgical site infection (SSI), fever, hypothermia, wound dehiscence, fecal fistula, length of stay, pulmonary complication and death. Other multivariables were studied as age, sex, occupation, socioeconomic condition, types of weapon, mode of injury and time interval between incident and admission.
Statistical Analysis
No software program was used for statistical analysis. Continuous variables were analyzed using median and range. All the data were expressed in frequency and percentage. Collected data were tabulated in numerical tables. Some are expressed in graph and Pie chart.
Results
Thirty-six patients of PAI were selected with mild or no signs of hemodynamic instability for our study in Casualty Unit, Dhaka Medical College Hospital from February 2011 to January 2012 and managed as per designed algorithm.
Multivariable Analysis
In our series, we noted that the age incidence ranged from 19 to 62 years and the highest incidence was in between 21-40 years. Mean age was 30 years (SD= 6.7), all patients were males, mostly (58%) from rural areas and 73% from lower socioeconomic conditions. No patient could arrive within the first 2 hours and, we found maximum 33 patients arriving within 4-6 hours. Cause of injury was mostly homicidal 91.7% and sharp metallic weapons were mostly used 89%. Site of injury was most commonly noted over the epigastrium (42%) and then the right iliac region (22%) (Table 2). Among them, thirty-three patients (92%) were successfully managed with non-operative management and 3 patients (8%) needed laparotomy.
Table 2. Multivariable analysis in our study.
| Category | Value | Percentage |
| Age | Mean (30 years) SD= 6.7 |
|
| Sex | ||
| Male | 36 | 100% |
| Female | 0 | 0% |
| Occupation | ||
| Farmer | 6 | 16.7% |
| Businessman | 4 | 11% |
| Service holder | 5 | 14% |
| Rickshaw puller | 8 | 22.3% |
| Day laborer | 13 | 36% |
| Habitat | ||
| Urban | 15 | 42% |
| Rural | 21 | 58% |
| Socioeconomic condition | ||
| Lower | 26 | 72.2% |
| Middle | 10 | 27.8% |
| Higher | 0 | 0% |
| Time of arrival after injury (hours) | ||
| 1-2 | 0 | 0% |
| 2-4 | 3 | 8.3% |
| 4-6 | 33 | 91.7% |
| Cause of injury | ||
| Accidental | 2 | 5.5% |
| Homicidal | 33 | 91.7% |
| RTA | 1 | 2.8% |
| Type of weapon | ||
| Sharp metallic | 32 | 89% |
| Nonmetallic (glass, bamboo) | 4 | 11% |
| Fire arms | 0 | |
| Site of injury | ||
| Epigastrium | 15 | 42% |
| Umbilical | 4 | 11% |
| Right hypochondrium | 5 | 14% |
| Right iliac | 8 | 22% |
| Multiple areas | 4 | 11% |
| SD: Standard deviation, RTA: Road traffic accident. | ||
Evaluation of the Patients
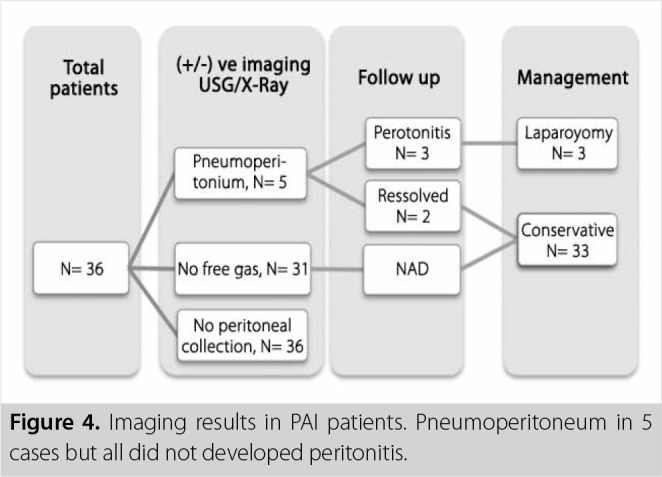
Following the incident of penetrating trauma, the patients were presented with various symptoms as active bleeding from wound site, abdominal pain, evisceration of the omentum and gut, respectively (Figure 2). Then we proceeded with our management algorithm (Figure 3). Routine imaging studies including FAST and abdominal X-Ray revealed 5 patients with peritoneal free gas (pneumoperitoneum) which could be due to entry of environmental air or leaked from hallow viscus, but no evidence of peritoneal collection or solid organ damage was suspected. Within 36 hours of follow-up, three patients developed features of peritonitis and explorative laparotomy were performed immediately and rest of the patients (33) were managed with conservative treatment (Figure 4).
Figure 2. Presentation of patients in our series.
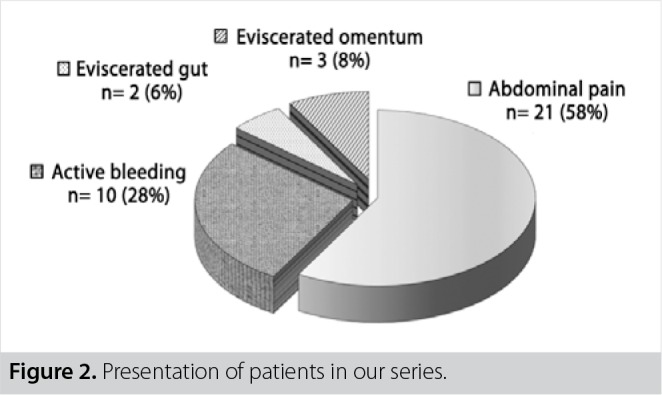
Figure 3. Algorithm for the management of penetrating abdominal trauma in our series.
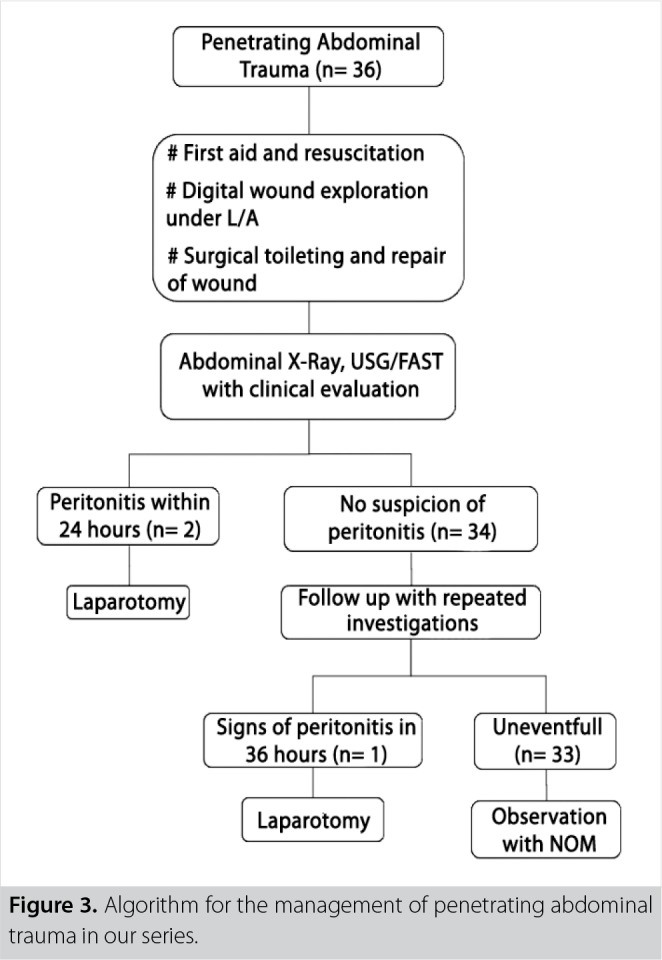
Figure 4. Imaging results in PAI patients. Pneumoperitoneum in 5 cases but all did not developed peritonitis.
Outcome Analysis
Among the 36 patients, thirty-three (91.7%) patients were managed with SNOM and 3 patients needed laparotomy. On laparotomy, jejunal perforation in two cases and ileal perforation in one case were noted (Table 3). Gut wounds were trimmed, and primary repair was done with placing abdominal drain tube. We didn’t find any negative laparotomy and no death in our study.
Table 3. Laparotomy incidence and findings.
| Management |
Patients (n= 36) | Percentages |
| Conservative | 33 | 91.7% |
| Laparotomy | 3 | 8.3% |
| Findings | Patients (n= 3) | Percentages |
| Hollow viscus injury | 3 | 100% |
| Solid organ injury | 0 | 0 |
| Negative | 0 | 0 |
In our study, among the conservatively treated patients, four developed wound infection, 3 developed fever, and two needed secondary wound closure. In the operative group, all three patients developed respiratory tract infection (RTI), anesthetic hazards, required more oxygen support, frequent nebulization and blood transfusion (Table 4). All conservatively managed 33 patients were discharged within 4-7 days.
Table 4. Complications and hospital stay in our study.
| Complications |
no of cases | Percentages |
|
| Conservative | laparotomy | ||
| Hypothermia | 0 | 2 | 5.5% |
| Fever | 3 | 2 | 14% |
| RTI | 0 | 3 | 8.3% |
| Wound infection | 4 | 2 | 16.7% |
| Secondary closure | 2 | 2 | 11% |
| Prolong hospital stay | 0 | 3 | 8.3 % |
| Delayed GEA recovery | 0 | 2 | 5.5 % |
| Blood transfusion | 0 | 3 | 8.3% |
| Duration of stay | |||
| 0-3 days | 14 | 0 | 39% |
| 4-7 days | 18 | 0 | 50% |
| 8-10 days | 1 | 0 | 2.7% |
| 11-14 days | 0 | 2 | 5.6% |
| > 14 days | 0 | 1 | 2.7% |
| RTI: Respiratory tract infection, GEA: General endo-tracheal anaesthesia. | |||
Discussion
The aim of this study was to observe the outcome of selective non-operative management (SNOM) of penetrating abdominal injuries by clinical evaluation and diagnostic methods and the effects of timing of the operation. Stab injury or other penetrating abdominal injury with minimal or no symptom always poses a management challenge for trauma surgeons in the casualty department. It always warrants immediate laparotomy in case of hemodynamic instability or any signs of peritonitis. However, the major challenge nowadays is to make the right decision with the help of diagnostic modalities available. Unfortunately, a single evaluation test will never provide adequate diagnosis in all cases of penetrating abdominal trauma.
Injury occurred most commonly among young persons (21-40 years) and the incidence declined rapidly with advancing age. In our study, all of the patients were males because of their mobile lifestyle, use of high-speed vehicles and involvement in civil violence and crime. In various large group studies, it has been reported that mean age ranges from 26-30 years for such trauma incidence (2,8,9).
Fifty eight percent of all PAI patients were rural dwellers in our study, which suggests that the injuries might have happened due to increased aggressiveness and arrogance among themselves for protecting their property and pride. Most of the patients (72.2%) were noted to come from lower class families. Probably due to active participation in high risk-taking activities, majority of the injuries was homicidal and occurred in rural areas with sharp metallic, locally-made, used in household affairs such as teta, ballam, kirich and knife etc. Most common site of external wound was noted over the epigastrium (42%) and then right iliac region. After laparotomy, jejunal perforation was most commonly noted. Lee WC at el. have reported the most common site of the external wound to be over the left upper quadrant and lower chest and small bowel (20%) followed by the liver (14%) (9). In another study, Gorge VC et al. have noticed that the most common injured organs include rectum then small bowel then liver by gunshot injury (10).
Our study included all PAI patients with peritoneal violation presented with severe abdominal pain, active bleeding from wound, eviscerated gut and omentum respectively. All of those features are not absolute indications for laparotomy and proceed with SNOM. In a study by Ertekin C et al. among 117 patients with stab wounds, 92 (79%) patients have been discharged without surgery (11). Different large group studies have also not supported the view that omental or bowel evisceration is an absolute indication for an emergency operation (8,12).
In our study, after resuscitation, FAST, chest and abdominal X-Ray were done in all patients. Throughout our study, these imaging tests were repeated as needed. We did not include CT scan routinely due to lack of availability and affordability rather than the role of CT scan being debatable in PAI. Exadaktylos et al. have described that CT may not be necessary for patients with SW. At their center in South Africa, out of 496 patients of abdominal SWs, 298 patients have been selected for SNOM. None of the patients underwent CT, and management was based on clinical examination alone (13). In a meta-analysis, CT has not been independently associated with failure or success of SNOM (14).
This study included 36 PAI patients with peritoneal violation, hemodynamically stable and arrived within 6 hours of injury. Thirty-three patients (around 92%) were successfully managed conservatively avoiding unexpected complication rates of negative laparotomy. Taviloglu K et al. have reported that when laparotomy is routine in PAI, negative and nontherapeutic laparotomy rates rise to 12% and 23%, respectively but in later periods with SNOM, these rates decline to 7% and 4% (15). Three patients in our study underwent therapeutic laparotomy based on clinical evaluation and repeated imaging studies, all of them became the victim of anesthetic hazard but there was no negative laparotomy.
Most common complication noted in our study was trauma site wound infection (16.7%) and 11% required secondary closure and 8.3% needed blood transfusion in the post-operative period. Delay of laparotomy in our study was 24 to 36 hours. Velmahos GC et al. have stated that the greatest concern related to a policy of SNOM is the complication produced by the delay of operation with unnoticed features of peritonitis. Among 80 patients with delayed laparotomy, five developed complications potentially related to delaying operation, and they believe that 24 hours’ time of observation is adequate for majority of the patients (10).
Regarding hospital stay and other complications, fourteen patients (39%) were managed by SNOM, discharged within 3 days with advice to stitch off later. Eighteen (50%) patients were discharged within 7 days due to wound infection and pyrexia. Three patients underwent laparotomy and had increased morbidity not due to gut injury but for anesthetic hazard, severe wound infection, post-operative pneumonitis, fever and prolonged hospital stay, which demanded extra costly investigations and higher total treatment expense. Unnecessary laparotomies for trauma are associated with a significant complication rate, ranging from 22% to 41%, and a significantly prolonged hospital stay (12,16,17).
The ongoing dilemma for hemodynamically stable patients almost concluded with the introduction of ‘‘selective conservatism’’ by Shaftan (4). In a study in 1960, he suggested that clinical examination could reliably and safely predict the need for laparotomy in PAI.
Conclusion
Continuous clinical evaluation together with different and repeated diagnostic tools could minimize the number of nontherapeutic laparotomies and limit possible unexpected complications of negative laparotomy in penetrating abdominal injuries. Trauma surgeons who used to manage PAI may feel more comfortable dealing with a selective non-operative approach. In a developing country like Bangladesh, by adopting selective non-operative management, we could manage some of those patients with less complication and expanse safely.
Footnotes
Conflict of Interest: No conflict of interest was declared by the authors.
Peer Review: Externally peer-reviewed.
Ethics Committee Approval: This study was approved by the BCPS (Bangladesh College of Physicians and Surgeons), Bangladesh ethical review committee.
Informed Consent: Informed consent was obtained from all individual patients included in our study.
Author Contributions: Consept - M.S.R.; Design - M.S.R.; Supervision - A.M.R., H.U.B.; Data Collection and/or Processing - M.S.R., K.H., T.H.; Analysis and Interpretation - M.S.R., A.M.R., H.U.B., K.H., T.H.; Literature Search - T.H., H.U.B.; Writing Manuscript - H.U.B., K.H.; Critical Reviews - M.S.R., A.M.R.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Welch CE. War wounds of the abdomen. N Engl J Med. 1947;237:187–194. doi: 10.1056/NEJM194708072370605. [DOI] [PubMed] [Google Scholar]
- 2.Zafar SN, Rushing A, Haut ER, Kisat MT, Villegas CV, Chi A, et al. Outcome of selective non-operative management of penetrating abdominal injuries from the North American National Trauma Database. Br J Surg. 2012;99:155–164. doi: 10.1002/bjs.7735. [DOI] [PubMed] [Google Scholar]
- 3.Butt MU, Zacharias N, Velmahos GC. Penetrating abdominal injuries: management controversies. Scand J Trauma Resusc Emerg Med. 2009;17:19–19. doi: 10.1186/1757-7241-17-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaftan GW. Indications for operation in abdominal trauma. Am J Surg. 1960;99:657–664. doi: 10.1016/0002-9610(60)90010-6. [DOI] [PubMed] [Google Scholar]
- 5.Como JJ, Bokhari F, Chiu WC, Duane TM, Holevar MR, Tandoh MA, et al. Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma. 2010;68:721–733. doi: 10.1097/TA.0b013e3181cf7d07. [DOI] [PubMed] [Google Scholar]
- 6.Biffl WL, Moore EE. Management guidelines for penetrating abdominal trauma. Curr Opin Crit Care. 2010;16:609–617. doi: 10.1097/MCC.0b013e32833f52d2. [DOI] [PubMed] [Google Scholar]
- 7.Navsaria PH, Berli JU, Edu S, Nicol AJ. Non-operative management of abdominal Stab wounds – an analysis of 186 patients. S Afr J Surg. 2007;45:128–132. [PubMed] [Google Scholar]
- 8.Demetriades D, Rabinowitz B. Indications for operation in abdominal stab wounds. A prospective study of 651 patients. An Surg. 1987;205:129–132. doi: 10.1097/00000658-198702000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee WC, Uddo JF Jr, Nance FC. Surgical judgment in the management of abdominal stab wounds. utilizing clinical criteria from a 10-year experience. Ann Surg. 1984;199:549–554. doi: 10.1097/00000658-198405000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Velmahos GC, Demetriades D, Toutouzas KG, Sarkisyan G, Chan LS, Ishak R, et at. Selective nonoperative management in 1,856 patients with abdominal gunshot wounds: should routine laparotomy still be the standard of care. Ann Surg. 2001;234:395–402. doi: 10.1097/00000658-200109000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ertekin C, Yanar H, Taviloglu K, Gluloglu R, Alimoglu O. Unnecessary laparotomy by using physical examination and different diagnostic modalities for penetrating abdominal stab wounds. Emerg Med J. 2005;22:790–794. doi: 10.1136/emj.2004.020834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arikan S, Kocakusak A, Yucel AF, Adas G. A prospective comparison of the selective observation and routine exploration methods for penetrating abdominal stab wounds with organ or omentum evisceration. J Trauma. 2005;58:526–532. doi: 10.1097/01.ta.0000152498.71380.3e. [DOI] [PubMed] [Google Scholar]
- 13.Exadaktylos A, Stettbacher A, Edul S, Nichols A, Bautz P. Successful management of abdominal stab wounds with clinical evaluation: experiences of a South-African trauma unit with 496 consecutive patients. Der Unfallchirurg. 2003;106:215–219. doi: 10.1007/s00113-002-0543-z. [DOI] [PubMed] [Google Scholar]
- 14.Goodman CS, Hur JY, Adajar MA, Coulam CH. How well does CT predict the need for laparotomy in hemodynamically stable patients with penetrating abdominal injury. A review and meta-analysis. AJR Am J Roentgenol. 2009;193:432–437. doi: 10.2214/AJR.08.1927. [DOI] [PubMed] [Google Scholar]
- 15.Taviloglu K, Gunay K, Ertekin C, Calis A, Türel O. Abdominal stab wounds: the role of selective management. Eur J Surgery. 1998;164:17–21. doi: 10.1080/110241598750004904. [DOI] [PubMed] [Google Scholar]
- 16.Renz BM, Feliciano DV. Unnecessary laparotomies for trauma: a prospective review of morbidity. J Trauma. 1995;38:350–356. doi: 10.1097/00005373-199503000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Ross SE, Dragon GM, O’Malley KF, Rehm CG. Morbidity of negative coeliotomy in trauma. Injury. 1995;26:393–394. doi: 10.1016/0020-1383(95)00058-h. [DOI] [PubMed] [Google Scholar]


