Abstract
While scientific evidence demonstrates conclusive associations between unhealthy lifestyle behaviors and increased morbidity and mortality related to noncommunicable chronic diseases (NCDs), most physicians are not formally taught the root causes of NCDs nor how to counsel patients regarding their lifestyle behaviors for disease prevention and treatment. Since its inception in 2012, the University of South Carolina School of Medicine Greenville has designed, developed, and implemented an innovative, formalized lifestyle medicine curriculum to provide required undergraduate medical student training with a graduating program-level goal to “Deliver total health care using lifestyle medicine to prevent and treat morbidity and mortality related to chronic diseases.” The process was guided by the Association of American Medical Colleges’ Core Entrustable Professional Activities (required for graduates entering residency) and aimed to satisfy the Quadruple Aim components of better outcomes, lower cost, improved patient experience, and improved physician experience. Four essential instructional design phases, Analysis, Design, Development, and Evaluation, were used as systematic steps to create and deploy the curriculum. This article describes the evidence-based approach used and offers guidance to other undergraduate medical schools that may wish to implement lifestyle medicine training to improve physicians’ medical knowledge and clinical skills for optimum health care.
Keywords: lifestyle medicine, curriculum, instructional design, undergraduate medical education, quadruple aim
‘AAMC [Association of American Medical Colleges] highlighted the need for lifestyle medicine–trained physicians due the staggering morbidity, morality, and costs of health care related to lifestyle behaviors.’
In July 2010, the Journal of American Medical Association (JAMA) published “Physician Competencies for Prescribing Lifestyle Medicine” to guide continuing medical education activities for primary care and preventive care physicians, and to urge physician educators at both the undergraduate and graduate medical education levels to incorporate lifestyle medicine competencies into education and training programs. Again, in July 2018, the American Association of American Medical Colleges (AAMC) recognized lifestyle medicine as 1 of 5 emerging medical specialties due to its significance in the prevention and treatment of chronic diseases, along with the rising demand for doctors trained in this field.1 AAMC highlighted the need for lifestyle medicine–trained physicians due the staggering morbidity, morality, and costs of health care related to lifestyle behaviors. Indeed, the United States spends more on health care than any other nation in the world ($9451 per capita, as compared to the #2 country, Switzerland, at $6934 per capita); yet the United States falls among the 30 developed nations that are ranked by the Organization for Economic Cooperation and Development with regard to suboptimal health outcomes.2 The Centers for Disease Control and Prevention estimates that approximately 90% of $3.3 trillion US health care dollars-are spent annually on the treatment of preventable, lifestyle-related, noncommunicable chronic diseases (NCDs), including obesity, cardiovascular disease, type 2 diabetes, and various forms of cancer.3
While scientific evidence demonstrates conclusive associations between unhealthy lifestyle behaviors and increased morbidity and mortality related to NCDs, most physicians are not formally educated in the root causes of these diseases nor how to counsel patients regarding their lifestyle behaviors. Indeed, practicing physicians cite having low confidence and lack of clinical knowledge and skills as major barriers to counseling patients about successful and sustainable lifestyle interventions, and only 10% of medical school deans feel their students could confidently write an exercise prescription.4,5 Restructuring undergraduate medical education (UME) to include training in the clinical discipline of lifestyle medicine6 (eg, education in the biomedical and clinically applied sciences of nutrition, exercise/physical activity, sleep health, tobacco cessation, stress management, healthy relationships, and behavior change) is essential to preventing and treating the NCDs currently affecting the population’s health.7 Furthermore, integrating a lifestyle medicine curriculum into UME addresses the Agency for Health Care Research and Quality’s (AHCRQ) Quadruple Aim8 that strives to improve (1) population health, (2) experience of care, and (3) per capita costs, as well as (4) the health status and resiliency of the physician themselves. However, to our knowledge, there is a dearth of required lifestyle medicine training in most undergraduate medical schools as a part of the core curriculum.
This article describes in detail the evidence-based, systematic approach used to design, develop, implement, and evaluate a lifestyle medicine curriculum at the University of South Carolina School of Medicine Greenville (USC SOM Greenville). We selected to integrate this curriculum across all 4 years of the students’ education as a required component of physician training in part due to an effort to achieve the AHCRQ’s Quadruple Aim, as well as to fill the demand of physicians needed in this emerging medical specialty.
Methods: Lifestyle Medicine Curriculum Design
Four essential instructional design phases (Analysis, Design, Development, and Evaluation) are required in systematic steps and are used by almost all instructional design models for designing and developing the learning experience.9 The goal of the systematic approach in designing instruction is to (1) provide clear goals and objectives, (2) provide careful linkage between each of the learning components, and (3) provide an empirical and replicable process.10 Therefore, we designed and developed the USC SOM Greenville Lifestyle Medicine curriculum by following a model driven by Dick and Carey,10 and based on Gagne’s domains of learning11 and Bloom’s taxonomy of learning outcomes.12 We then implemented the initial design through the 2012 to 2015 academic years. The following include details on how the 6 steps of this process were accomplished.
Step 1: Analysis and Planning Phase
As the integration of lifestyle medicine (or any curricular innovation) into the existing medical education structure can be challenging, it is essential to analyze all of the following components: the teaching and learning environment, the learners, the culture among biomedical and clinical faculty, and the institution’s attitude regarding adoption of new educational goals beyond the traditional medical curriculum. Unpublished survey results of outside institutions during a 2016 AAMC “Lead, Serve, Learn” session revealed that barriers to implementing a lifestyle medicine curriculum included competition for time in the existing curriculum, lack of availability of content experts, perceived importance at the faculty level, and competition with what students perceive as “essential” knowledge to pass the current United States Medical Licensing Examination examinations.13
Therefore, in the initial design to overcome the barriers of competition for time and faculty perception of lifestyle medicine importance, we first started by identifying faculty members within the school as change agents to assist in the integration and teaching of lifestyle medicine content within their disciplines. Examples include the first year (M1) Neuroscience module, in which exercise and nutrition components for enhancing neuronal development and repair was co-delivered by a lifestyle medicine content expert and a biomedical science/neuroscientist faculty content expert. In the M2 year, clinical faculty in family medicine and a lifestyle medicine content expert co-delivered nutritional components and exercise therapy in Lifestyle Medicine and Hypertension. In addition, buy-in at the deans’ level helped to bring importance of lifestyle medicine training across the curriculum for the majority of the school’s faculty. To address the barriers of students’ perception of lifestyle medicine importance for essential knowledge, students matriculating to their first biomedical science module were introduced to lifestyle medicine curriculum as a required component of UME for all students across the 4 years of our program. Then throughout their biomedical science modules, students were educated in detail and at the intracellular level in the biochemical and physiological mechanisms in which lifestyle either plays a role in the prevention of, or pathophysiology of disease. An example pathway taught in the M2 year demonstrates how saturated fat intake and obesity increase circulating leptin, which activates PI3K and MAPK signaling pathways as well as the JAK/STAT3 pathway, both associated with tumor cell formation and proliferation in cancer. Throughout these modules, students also were taught and supported to adapt Cura te ipsum, or, “heal thyself,” to foster a culture of students advocating for themselves “as their first and most important patient.”
Over time, faculty and students embraced the lifestyle medicine curriculum, and it became an integral part of the school’s culture because of its purposeful vertical and longitudinal integration. Therefore, in the spring of 2015, clinical and biomedical science faculty along with an instructional designer formed a Lifestyle Medicine Task Force (LMTF) to evaluate the initial design of the curriculum and to expand and implement lifestyle medicine as a longitudinal, required curriculum throughout the 4 UME years. The LMTF titled this the “Lifestyle Medicine Core Curriculum.” Next steps in analyzing and planning the Lifestyle Medicine Core Curriculum were to identify the overarching lifestyle medicine program-level goal, the graduating goals, and the learning objectives specific to each curricular year.
Step 2: Identification of the Lifestyle Medicine Core Overarching Program-Level Goal and 6 Graduating Goals
First, to determine the Lifestyle Medicine Core Curriculum overarching program-level goal for graduating medical students, the LMTF (1) performed goal analysis to determine the program goal and its components and (2) identified skills and knowledge a learner must achieve for the program-level goal. The LMTF determined the overarching program-level goal was to:
“Deliver total health care using lifestyle medicine to prevent and treat morbidity and mortality related to chronic diseases.”
This goal aligned with the medical school’s program-level goals, which were approved by the Liaison Committee on Medical Education 2011 Preliminary Accreditation of USC SOM Greenville program (Final Accrediation received in October 2016).
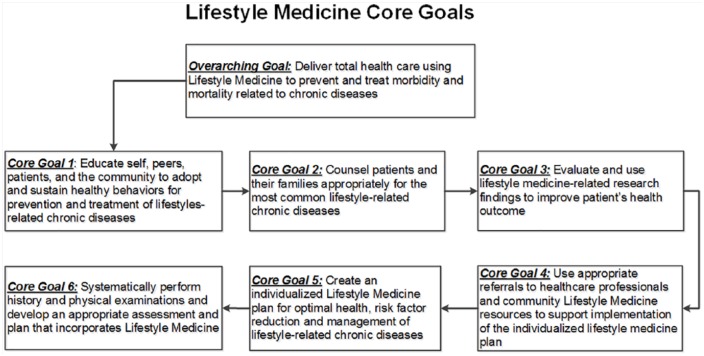
Next, the LMTF identified knowledge and skills needed by graduation to meet the goals of any residency program where lifestyle behaviors affect morbidity and mortality. These knowledge, skills, and goals were guided by the Core Entrustable Professional Activities required for graduates entering the residency program,14 and satisfied all 4 Quadruple Aim components.8 The product of this instructional analysis process is illustrated in Figure 1.
Figure 1.
USC SOM Greenville lifestyle medicine goal analysis output.
Step 3: Identification of the Lifestyle Medicine Core Curriculum Year-Specific Learning Objectives
The LMTF then developed a hierarchy of what the learners would specifically learn every year to demonstrate achievement of each of the 6 core graduating goals (Figure 1). To answer the aforementioned goal Analysis question, we used Bloom’s taxonomy to classify learning outcomes into their appropriate domains.12 We continued the Analysis process to include all critical knowledge and skills needed to reach the core goals. Moreover, we identified the prerequisite essential knowledge and skills needed to commence learning the Lifestyle Medicine Year 1 learning objectives (listed below the dotted line in Figure 2). As a result, we formalized year-specific lifestyle medicine learning objectives for the M1 to M4 years to achieve each core graduating goal. Figure 2 provides an example of year-specific learning objectives that lead to the graduating Core Goal #1.
Figure 2.
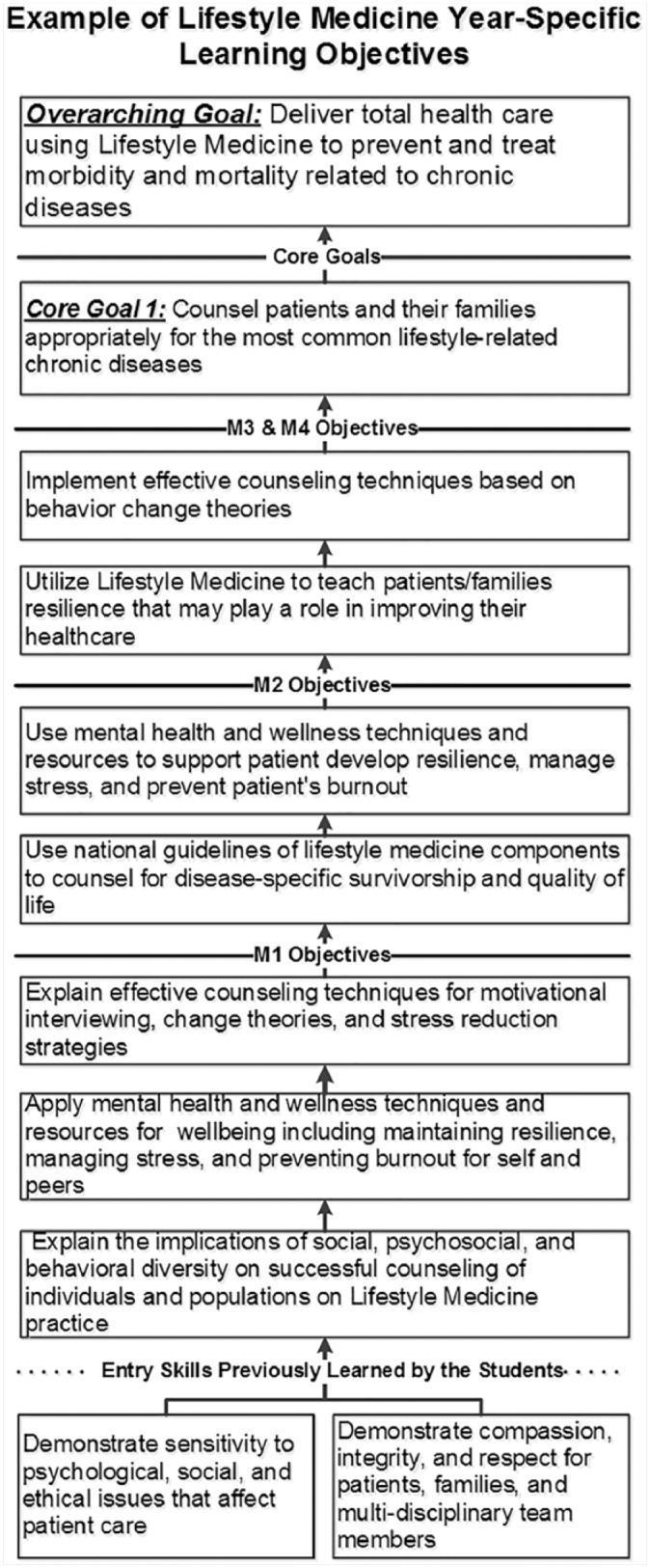
Example of lifestyle medicine year-specific learning objectives leading to Core Goal #1.
Using this systematic approach, we created a structured and verified method for analyzing the learning objectives and parsing each into 6 separate but complimentary learning components. Using this approach, we also were able to:
Identify subordinate skills within the learning map in an instructional and sequencing manner
Identify prerequisites skills needed to perform the learning objectives
Eliminate any knowledge or skill not essential or especially supportive to attain the lifestyle medicine–specific graduating goals
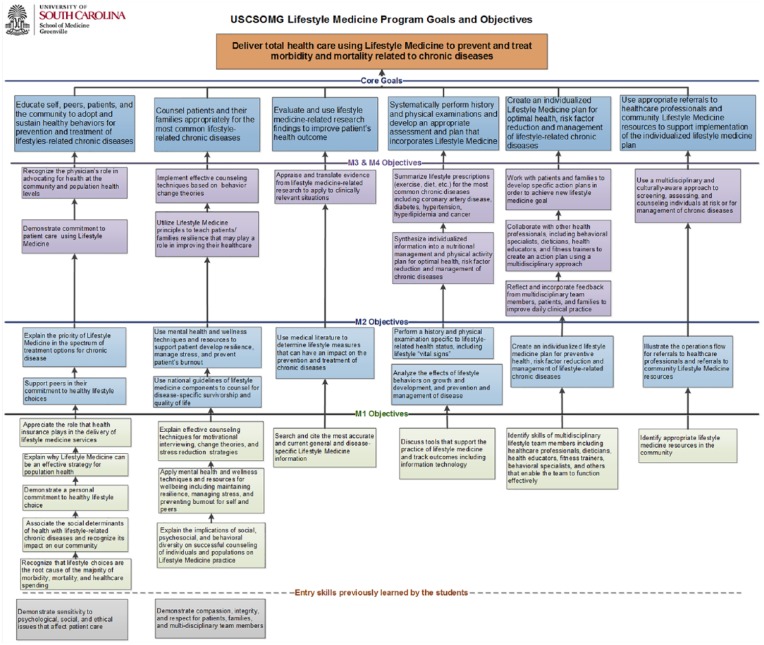
The LMTF took an additional step to approve the Analysis process by submitting the Overarching Program-Level Goal, the 6 Graduating Goals, and the Year-specific Learning Objectives (Figure 3) for review, revisions, confirmation, and approval by the M1 to M4 year subcommittees before being vetted and approved by the USC SOM Greenville’s Curriculum Committee.
Figure 3.
USC SOM Greenville lifestyle medicine goal overarching program-level goal, the 6 graduating goals, and the year-specific learning objectives.
In summary, the instructional Analysis, specification, and categorization of the lifestyle medicine learning objectives for each medical year assisted participating faculty in next selecting educational strategies, learning activities, teaching methods, cognitive levels, and assessment instruments for the Lifestyle Medicine Core Curriculum in UME. This information and the curriculum mapping of the topics related to lifestyle medicine helped in designing the structure and flow of the lifestyle medicine content into every module across the 4 years.
Step 4: Design and Development of the Lifestyle Medicine Core Curriculum Educational Strategies
Different domains of learning require appropriate teaching methods and assessment instruments.9 Thus, we planned multiple teaching methods to deliver the curriculum, including the following:
Instructor-led primary lifestyle medicine teaching sessions within the organ systems
Problem-based learning where lifestyle medicine mechanisms are integrated within biomedical science cases
Case-based learning where lifestyle medicine discussion is embedded into the clinical reasoning cases
Simulation of lifestyle medicine behavior change with standardized patients and fellow students within clinical skills practice
Clinical experience where lifestyle medicine is embedded in relevant clinical clerkship areas
Relevant to the above-mentioned teaching methods, interprofessional education (IPE) is essential for impacting how physicians are trained to comprehensively provide healthy lifestyle interventions for patients,15,16 as well as striving to meet the Quadruple Aim of decreasing physician burnout and improving satisfaction in practice.8 To achieve the curriculum goals, in particular Core Goal #4, to “Use appropriate referrals to healthcare professionals and community lifestyle medicine resources to support implementation of the individualized lifestyle medicine plan,” as well as Core Goal #1, to “Educate self, peers, patients, and the community to adapt and sustain healthy behaviors for prevention and treatment of lifestyle-related chronic diseases,” we also designed IPE-based learning activities to provide students opportunities to:
Interact with allied health providers in the field who have face-to-face contact with both patients and students
Become aware of non-medical community resources available to students when they are ready to practice
Learn the importance of creating a team for optimal continuity of patient care
Furthermore, the American College of Lifestyle Medicine recognizes that physicians alone cannot provide all lifestyle medicine clinical and education services for patients and families; thus, team-based care is one of the core competencies required for prescribing lifestyle medicine.17 Teams are not meant to replace the physician-patient relationship but rather provide value for patients, contribute to successful health outcomes,7,16 and improve the well-being of the physician.8 USC SOM Greenville emphasizes student health and wellness as an essential part of the lifestyle medicine curriculum, and therefore chose to provide activities that foster a culture of student value in maintaining self-care behaviors to boost resilience and avoid burnout.18,19 Additionally, as demonstrated in “Healthy Doc = Healthy Patient” survey studies, physicians who maintain healthy lifestyles tend to encourage healthy lifestyle behaviors in their patients.20,21
Step 5: Implementation and Examples of the Lifestyle Medicine Core Curriculum
The implementation stage is the actual delivery of the lifestyle medicine curriculum. To address some of the issues encountered in the initial implementation such as availability of time in the curriculum and faculty buy-in, successful lifestyle medicine implementation occurred through working with module/course directors and willing biomedical/clinical science faculty to plan, integrate, and deliver content within their module, disciplines, and sessions. Table 1 summarizes all contact hours of distribution of lifestyle medicine content across the 4 years by module. Table 2 shows an example of the lifestyle medicine session plan for the second year Hematology/Oncology module.
Table 1.
Lifestyle Medicine Content Outline and Contact Hours Across the 4 Years.
| Medical Year | Module | Session Name (Preclinical and Clinical) | Teaching Hours |
|---|---|---|---|
| First year | Molecular and Cellular Foundations of Medicine | The Foundational Components of Lifestyle Medicine | 2 |
| Structure and Function of the Human Body 1 |
Muscle Energetics, Strength, and Power (1
hour)
Musculoskeletal Health Through the Lifespan (1 hour) • Bone Health • Aging and Detraining Lifestyle Medicine and Hematopoiesis (1 hour) Lifestyle Medicine, Lipoprotein Metabolism, and Cardiovascular Health (1 hour) Lifestyle Medicine and Respiratory Health (1 hour) |
5 | |
| Structure and Function of the Human Body 2 |
Lifestyle Medicine and Gastrointestinal Health (1
hour)
Lifestyle Medicine and Renal Health (1 hour) BMI, Obesity, and Body Composition (1 hour) |
3 | |
| Neuroscience | Nutrition, Exercise, Brain Functions, and Neuronal Repair | 1.5 | |
| Defenses and Responses | Lifestyle Medicine and the Immune System | 2 | |
| Integrated Practice of Medicine 1 |
Introduction to Lifestyle Medicine (1 hour)
The Art and Science of Nutrition (1.5 hours) Medical Student Stress, Burnout and Resiliency M1 (1.5 hours) Motivational Interviewing (1.5 hours) Prochaska’s Stages of Behavior Change for Nutrition and Exercise (1 hour) |
6.5 | |
| Second year | Cardiovascular, Pulmonary, and Renal |
Hypertension and Lifestyle Medicine (1
hour)
Lifestyle Medicine and Chronic Kidney Disease • How to Eat for your Kidneys (1 hour) |
2 |
| Endocrine and Reproductive Systems |
Lifestyle Medicine and Reproductive Health (2
hours)
Multisystem Function: Step 1 Prep (2 hours) • Concept linkage of biochemical, endocrine, reproductive, oncological, and lifestyle factors |
4 | |
| Gastrointestinal and Hepatic Systems |
Alcoholic Fatty Liver Disease, Non–Alcoholic Fatty
Liver Disease, and Metabolic Syndrome (2 hours)
Lifestyle Medicine and the Pancreas (1 hour) Nutrition for the Bariatric Surgery Patient (1 hour) Nutrition for Type 2 Diabetes (1 hour) Nutrition for Inflammatory Bowel Disease (1 hour) |
6 | |
| Hematology and Oncology |
Lifestyle Medicine for the Prevention and Treatment
of Cancer
• Includes Lifestyle Medicine for Cancer Cachexia |
2 | |
| Mind, Brain, and Behavior |
Lifestyle Medicine and Brain Health
• Includes Sleep Hygiene |
1 | |
| Musculoskeletal, Dermatology, and Rheumatology |
Lifestyle Medicine and Musculoskeletal Disorders (2
hours)
• Low Back Pain Osteoporosis (1.5 hours) |
3.5 | |
| Integrated Practice of Medicine 2 |
Medical Student Stress, Burnout, and Resiliency M2
(1.5 hours)
Lifestyle Medicine for Movement Disorders (1.5 hours) • Parkinson’s and Huntington’s Disease Lifestyle Medicine in Cancer Care: Teachable Moments for Behavior Change (1.5 hours) • Cancer Survivor Panel Behavior Change and Shared Decision Making (1.5 hours) Lifestyle Medicine and Autoimmune Diseases (1.5 hours) Patients with Obesity Panel (1.5 hours) |
9 | |
| Third year (lifestyle medicine integration required) | Family Medicine Clerkship |
Introduction to Preventive Care (1 hour)
Hypertensive disorders (1 hour) Cardiology Pearls for the Family Physician (1 hour) Ob/GYN for the Family Physician (1 hour) Diabetes Management Primer (1 hour) Glycemic Management (1 hour) Continuity of Care Project (2 hours) |
8 |
| Internal Medicine Clerkship |
Liver (1 hour)
Lipids (1 hour) The Art of Medicine (1 hour) Diabetes (1 hour) Anemia (1 hour) |
5 | |
| Neuropsychiatry Clerkship |
Mood Disorders (1 hour)
Epilepsy (1 hour) Psychotherapy (1 hour) Neuromuscular Diseases (1 hour) Geriatric Psych (1 hour) Sleep (1 hour) |
6 | |
| Obstetrics and Gynecology Clerkship |
Clinical-Teaches Lifestyle Medicine Concepts (1
hour)
Preconception and Antepartum Care (1 hour) Preventative Care and Health Management (1 hour) Diabetic/Thyroid (1 hour) Puberty (1 hour) Anxiety and Depression (1 hour) |
6 | |
| Pediatrics Clerkship |
Pediatric Obesity (1.5 hours)
Wellness plans for children and adolescents (1 hour) |
2.5 | |
| Surgery Clerkship | Multidisciplinary Cancer Conference (1 hour) | 1 | |
| Exercise is Medicine (Required self-directed learning) | Exercise is Medicine Workflow Education Guide Using Epic | 0.5 | |
| Integrated Practice of Medicine 3 |
Health Policy and Advocacy (1 hour)
Faces and Voices of Recovery (FAVOR; 1 hour) Populations and Disease: Patient Panel (1 hour) Stress, Burnout, and Mental Health (1 hour) Integrative Health/Lifestyle Medicine (1 hour) Communication (1 hour) |
6 | |
| Fourth year (lifestyle medicine integration required) | Integrated Practice of Medicine 4 |
Medical Management GI (1 hour)
Antihypertension (1 hour) Medical Management Diabetes (1 hour) Anticoagulation (1 hour) |
4 |
| Total | 86.5 |
Table 2.
Example Lifestyle Medicine Session Plan.
| Hematology and Oncology Module: Lesson Plan | |||
|---|---|---|---|
| Instructor: Trilk/Motley | Time: 2 hours | Date: 8/23/18 | Location: Lecture Hall |
| Session Topic: Lifestyle Medicine for the Prevention and Treatment of Cancer | |||
| Lifestyle Medicine Longitudinal Objectives for
M2 • Explain the priority of lifestyle medicine in the spectrum of treatment options for chronic diseases • Use national guidelines of lifestyle medicine components to counsel for disease-specific survivorship and quality of life • Use medical literature to determine lifestyle measures that can have an impact on the prevention and treatment of chronic diseases | |||
| Module-level Objective: • Discuss wellness, preventive measures and treatment side effects related to cancer with understanding of the underlying pathophysiologic mechanisms and biochemical alterations | |||
| Session Objectives (Include high level and low
level): • Recognize the contribution of obesity, insulin resistance, nutritional insufficiencies, and a sedentary lifestyle to the tumor environment. • Explain the etiology of cancer prevention through nutrition and diet, calorie restriction, and exercise, including effects on inflammatory markers, DNA repair, and improved insulin sensitivity. • Describe the mechanisms of chemotherapy/radiation-induced mitochondrial damage, and how exercise protects from mitochondrial damage during chemotherapy/radiation. • Summarize the proposed mechanisms by which antioxidants protect against cancers. Identify the four antioxidants for which the evidence of efficacy is strongest. • Summarize the proposed mechanisms by which folate, fiber, and excess dietary fat increase or decrease the risk of specific cancers. • Summarize the American Cancer Society’s dietary recommendations. | |||
| Out of Class | In Class | ||
| Clear Expectations • Learning objectives • Participation • Assignments due dates • Grades |
|||
| Instructional Method | Case-based Instruction/Learning | ||
| Guided Prework/SLM/YouTube • Covers low cognitive level objectives • Guided learning • Time on task • Practice and feedback Learning Activities • In class activities encourage retrieve, apply, and extend of knowledge |
Required Pre-class: Watch the video: How Not to Die from Cancer (https://nutritionfacts.org/video/how-not-to-die-from-cancer/) Read the article: Anand et al. 2008, Cancer Is a Preventable Disease that Requires Major Lifestyle Changes. |
Facilitated Large Group Discussion | |
| Assessments • Assessment clearly assess learning outcomes • Formative/Summative |
Exam—Institutionally Developed, Written/Computer-based | ||
| Resource List Summary of the ACS Guidelines on Nutrition and Physical Activity: http://www.cancer.org/healthy/eathealthygetactive/; https://www.cancer.org/healthy/eat-healthy-get-active/acs-guidelines-nutrition-physical-activity-cancer-prevention.html |
|||
The Integrated Curriculum: M1 to M4
In the M1 year, the primary focus of student learning is the normal anatomy and physiology of the human body, which are taught through didactic and case-based lectures. Lifestyle medicine content was integrated into these lectures by supplementing the biochemical, molecular, and cellular basis of human function, physiology, endocrinology, neurologic control and homeostasis, and immunology. Again a lifestyle medicine expert taught individually or with a biomedical science faculty member. An example of a session delivered in the Defenses and Responses module was a case-based session titled, “Lifestyle Medicine and Immune Function.” This session discusses how an increase in caloric consumption beyond what is needed for homeostasis increases adiposity and subsequently creates an inflammatory state and reduces immune function over time. Accordingly, improved lifestyle using physical activity and plant-based, calorie-mindful diets reduce adipose tissue and improve immune function.
During the M2 year, students continue learning the scientific basis of medicine in an organ-system based approach, focused more on pathophysiological disease processes, diagnostic testing and imaging, and principles of treatment and management. As described above, a M2 session in the Hematology and Oncology module example titled, “Lifestyle Medicine for the Prevention and Treatment of Cancer,” educates students how obesity, sedentary behavior, and dietary saturated and trans-fat intake-based mechanisms are related to increases in reactive oxygen species, DNA damage, mutagenesis, tumorigenesis, and cancer.
During the M3 year, all students who rotate through the Family Medicine Clerkship are educated in lifestyle medicine components for patient encounters. Lifestyle factors are entered in the Clinical Skills Checklist and Patient Encounter Information, as students are required to:
Complete an exercise prescription for at least one patient
Provide dietary counseling to at least one patient
Provide behavioral change counseling using principles of the transtheoretical model and motivational interviewing
In the Internal Medicine Clerkship, students practice application of nutrition therapy as part of their clinical practice.
During the M4 year, regardless of their specialty selection, all students are required to take an Intensification module that consolidates the topics, skills, and competencies addressed throughout the entire program in preparation for residency training. This module includes clinical cases and scenarios that bring back lifestyle medicine learning topics from M1 to M3 years to assure competency in lifestyle prescription such as treatment of pneumonia or a hypertension case. Additional topics include well-being, for example, “Sleep Hygiene during Residency.”
Additionally in their clerkship years, students are able to rotate in the lifestyle medicine elective created through the Department of Family Medicine during M3 and M4 years for 2 or 4 weeks, respectively, to expose students to applying the core pillars of lifestyle medicine in the clinical setting and community. Students participate in a number of experiences during the rotation: examples include an Intensive Therapeutic Lifestyle Change program such as cardiac rehabilitation where they interview patients who have sustained a significant cardiac event, a live cooking session where they must demonstrate basic cooking techniques using plant-based foods, observe a grocery store class to better counsel their patients on how to shop for food, and counsel patients in a dedicated lifestyle medicine clinic. Students also are allotted at least 10 hours per week of separate student wellness time. Each experience aligns with the goals and objectives laid out by the American Board of Lifestyle Medicine.
Finally, reinforcement of the clinical relevancy of lifestyle medicine is integrated across all years into the M1 to M4 in the longitudinal module Integrated Practice of Medicine (IPM) via clinical cases and skills. IPM provides teaching in lifestyle behavior skills practice including theories such as Prochaska Stages of Change Model and the “5 As”22 as well as tools such as motivational interviewing and shared decision making.
Implementation of Interprofessional Education
To deliver the aforementioned IPE learning activities and opportunities, medical students in the M2 year receive IPE by registered dieticians and board-certified lifestyle medicine clinical faculty on how to use lifestyle medicine to treat patients with type 2 diabetes, hypertension, chronic kidney disease, low back pain, and others. Medical students in the M3 and M4 years are educated about the innovative “Exercise is Medicine Greenville” (EIMG) program.23 Through partnership with the USC SOM Greenville, Prisma Health-Upstate, YMCA of Greenville, and American College of Sports Medicine, EIMG delivers a community-based, clinical exercise and lifestyle behavioral intervention for prevention and treatment of NCDs including obesity, dyslipidemia, hypertension, and type 2 diabetes. Patients in the Departments of Family Medicine and Internal Medicine are counseled and referred through the EPIC electronic health record to the program. In detail, M2 students are first introduced to and educated in the Exercise Vital Sign programmed into the electronic health records and the EIMG exercise therapy for chronic disease referral program. Subsequently, M3 and M4 medical students are then prompted to facilitate physician referrals and patient transition to the EIMG Program. This learning and experience allows for students to transition their knowledge and skills from the classroom to a patient clinical-community setting resource in lifestyle medicine.
Experiential Education
Students throughout all years are faculty-supported in their efforts to create a lifestyle medicine culture in the medical school environment through actual experience, as well as are encouraged to put their knowledge into action in the community. For example, students lead the Lifestyle Medicine Special Interest Group, the Student Wellness Committee, and the student-proposed organic garden, “Harvesting Health and Hope,” along with multiple physical activity–related charity events such as the Susan G. Komen Breast Cancer Race for the Cure, Lungs4Life, and GHS Dragonboat day24 for cancer research. Medical students also offer healthy meals, coaching, and cooking demonstrations at the Greenville Free Clinic.25 These provide an interprofessional service opportunity to work in teams on a common goal and to lead lifestyle medicine–based programs in the communities they serve.
Step 6: Evaluation of the Lifestyle Medicine Core Curriculum
We evaluated the Lifestyle Medicine Core Program through each year and module’s End of Year Report to determine if the learning objectives were achieved, along with the faculty evaluation of the session-level content delivery methods. Learning is assessed through the performance statistics of the end-of-module summative exam items mapped to lifestyle medicine. Yearly module student evaluations of faculty delivering the Lifestyle Medicine Core Curriculum are also evaluated for strengths and weaknesses and are used to continue to refine the curriculum.
For medical programs that are interested in designing and implementing a lifestyle medicine curriculum, Table 3 shows a checklist for practical implementation of lifestyle medicine.
Table 3.
Road Map for Practical Implementation of Lifestyle Medicine Curriculum.
| Analysis and Planning Phase • Ensure that the medical educational context at your institute is appropriate for lifestyle medicine curriculum • Consider the region and local community health needs • Check if the teaching and learning culture support the adoption of new educational goals • Involve the curriculum stakeholders • Include lifestyle medicine content expert Design and Development Phase • Align the lifestyle medicine goals with the overall medical program goals • Use validated standards to determine the lifestyle medicine goals and objectives (For example, “Physician Competencies for Prescribing Lifestyle Medicine” (JAMA, 2010)17) • Develop the lifestyle medicine curriculum with the appropriate model for the main curriculum (discipline-based, system-based, blocks, etc) • Use educational strategy that is appropriate for your institute mission and vision Implementation Phase • Clearly communicate lifestyle medicine required graduation goals and objectives • Encourage collaboration between lifestyle medicine content expert and biomedical/clinical science faculty to plan, integrate, and deliver content within their module, disciplines, or sessions • Provide opportunities for Interprofessional education and community based activities within the lifestyle medicine training • Apply multiple assessment strategies to monitor and evaluate students’ performance throughout the curriculum, for example, formative and summative assessments Evaluation Phase • Use students’ feedback to evaluate and improve the curriculum • Systematically collect and review assessment data to improve student learning outcomes • Conduct curriculum mapping to ensure that lifestyle medicine curriculum support the program-level goals and objectives |
Conclusion
By establishing a clear mission and plan for implementation, and by starting with small, incremental steps, this collaborative teaching model has so far demonstrated that a lifestyle medicine curriculum can be complementary (not competitive) to traditional medical teaching and is indeed a natural component of total health care. Success of the Lifestyle Medicine Core Curriculum, including faculty buy-in, increased student candidate interest, and greater recognition in the academic medical community, has subsequently led to strategic planning by the dean to offer a Lifestyle Medicine Distinction Track that began in May 2018.26 The Lifestyle Medicine Distinction Track will further prepare honor students to become board certified in lifestyle medicine. In conclusion, as AAMC states, demand for lifestyle medicine physicians is already high1; therefore, more medical schools are encouraged to implement lifestyle medicine into their students’ education to become frontline advocates in this emerging field of medicine to reduce the staggering morbidity, mortality, and health care costs related to NCDs.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
ORCID iDs: Jennifer L. Trilk  https://orcid.org/0000-0001-5565-8895
https://orcid.org/0000-0001-5565-8895
Ann Blair Kennedy  https://orcid.org/0000-0002-3518-6314
https://orcid.org/0000-0002-3518-6314
References
- 1. Howard B. Five emerging medical specialties you’ve never heard of—until now. https://news.aamc.org/medical-education/article/five-emerging-medical-specialties/. Accessed July 24, 2018.
- 2. Organization for Economic Co-operation and Development. Health spending (indicator). https://data.oecd.org/healthres/health-spending.htm. Accessed June 2, 2017.
- 3. National Center for Chronic Disease Prevention and Health Promotion. Health and Economic Costs of Chronic Disease. https://www.cdc.gov/chronicdisease/about/costs/index.htm. Accessed June 2, 2017.
- 4. Stoutenberg M, Stasi S, Stamatakis E, et al. Physical activity training in US medical schools: preparing future physicians to engage in primary prevention. Phys Sportsmed. 2015;43:388-394. [DOI] [PubMed] [Google Scholar]
- 5. Huang J, Yu H, Marin E, Brock S, Carden D, Davis T. Physicians’ weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79:156-161. [DOI] [PubMed] [Google Scholar]
- 6. American College of Lifestyle Medicine. Lifestyle medicine in its clinical application. https://www.lifestylemedicine.org/Clinical-Discipline. Accessed June 2, 2017.
- 7. Kushner RF, Van Horn L. Teaching nutrition in the context for lifestyle medicine. Med Sci Educ. 2018;28(suppl 1):9-12. [Google Scholar]
- 8. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12:573-576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khalil MK, Elkhider IA. Applying learning theories and instructional design models for effective instruction. Adv Physiol Educ. 2016;40:147-156. [DOI] [PubMed] [Google Scholar]
- 10. Dick W, Carey L, Carey JO. The Systematic Design of Instruction. 6th ed. Boston, MA: Pearson/Allyn & Bacon; 2005. [Google Scholar]
- 11. Gagne RM. The Conditions of Learning and Theory of Instruction. 4th ed. New York, NY: Holt, Rinehart & Winston; 1985. [Google Scholar]
- 12. Bloom BS, Engelhart MD, Furst EJ, Hill WH, Krathwohl DR. Taxonomy of Educational Objectives: Handbook 1: Cognitive Domain. Harlow, England: Longman; 1984. [Google Scholar]
- 13. AAMC medical education: Lifestyle factors, disease burden, and medical school education—connecting the dots. Paper presented at: 2015 Association for American Medical Colleges; 2015. [Google Scholar]
- 14. Association of American Medical College. Core entrustable professional activities for entering residency: Curriculum Developers’ Guide. https://members.aamc.org/eweb/upload/core%20EPA%20Curriculum%20Dev%20Guide.pdf. Accessed September 30, 2016. [DOI] [PubMed]
- 15. Arena R, Lavie CJ. The healthy lifestyle team is central to the success of accountable care organizations. Mayo Clin Proc. 2015;90:572-576. [DOI] [PubMed] [Google Scholar]
- 16. Nester J. The importance of interprofessional practice and education in the era of accountable care. N C Med J. 2016;77:128-132. [DOI] [PubMed] [Google Scholar]
- 17. Lianov L, Johnson M. Physician competencies for prescribing lifestyle medicine. JAMA. 2010;304:202-203. [DOI] [PubMed] [Google Scholar]
- 18. Cecil J, McHale C, Hart J, Laidlaw A. Behaviour and burnout in medical students. Med Educ Online. 2014;19:25209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mustafa OM. Health behaviors and personality in burnout: a third dimension. Med Educ Online. 2015;20:28187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lobelo F, Duperly J, Frank E. Physical activity habits of doctors and medical students influence their counselling practices. Br J Sports Med. 2009;43:89-92. [DOI] [PubMed] [Google Scholar]
- 21. Duperly J, Lobelo F, Segura C, et al. The association between Colombian medical students’ healthy personal habits and a positive attitude toward preventive counseling: cross-sectional analyses. BMC Public Health. 2009;9:218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38-48. [DOI] [PubMed] [Google Scholar]
- 23. Exercise is Medicine Greenville. www.eimgreenville.org. Accessed June 2, 2017.
- 24. Dragon Boat Upstate. Dragon boat upstate festival (2019). http://donate.ghsgiving.org/site/TR/DragonBoat/General?team_id=1981&pg=team&fr_id=1170. Accessed March 8, 2019.
- 25. University of South Carolina. Medical students offer heathy meals and coaching via Greenville Free Clinic. https://www.sc.edu/study/colleges_schools/medicine_greenville/news/2018/garden.php. Published December 18, 2018. Accessed March 8, 2019.
- 26. University of South Carolina School of Medicine Greenville. The lifestyle medicine distinction track. https://sc.edu/study/colleges_schools/medicine_greenville/curriculum/distinctiontracks/lifestylemedicine.php. Accessed September 5, 2018.