Abstract
BACKGROUND:
The patient handover process is in fact a valuable and essential part of the care processes in the hospitals. This can be a factor in increasing the quality and effectiveness of medical care. Incorrect and incomplete handover can increase the percentage of errors and cause serious problems for patients. The aim of this study was to identify the handover challenges concerning safety and quality of health services.
MATERIALS AND METHODS:
A systematic review was conducted according to the Preferred Reporting Item for Systematic Reviews and Meta-analyses guideline. The key words “challenges of patient handover” or “challenges of patient handoff” were used in combination with the Boolean operators OR and AND. The ProQuest, Ovid, Doaj, Magiran, SID, Scopus, Science Direct, PubMed, and ISI were searched.
RESULTS:
A total of 263 articles were extracted, and 20 articles were selected for final review. The results of selected articles indicated that there are various challenges such as communication, noncoordination, nonuse of checklist, poor management, time management, and other things. These studies reported that communication was the main challenge of handover process.
CONCLUSIONS:
Hospitals try to provide a lot of services to the patients and other customers in a safe and healthy environment. Lack of communication among the incoming and outgoing nurses in handover process is one of the main causes of reduced safety and quality of services and patient dissatisfaction.
Keywords: Challenges, hand off, hand over, nurses, safety
Introduction
Patient safety is an essential component of the health systems, and it is of a global concern.[1] Identification of services provided is the first step for the improvement of the quality of services.[2] Maintaining patient safety increases, the chances of success in gaining optimal results in treatments.[1] This is one of the biggest challenges of providers of healthcare services. Failure of effective handover is a major preventable cause of patient harm, which is also the most important step in ensuring the patient's safe handover. Patient handover is in fact a valuable affair and an essential part of processes and workflows in hospitals.[3,4,5] In other words, one of the most important steps in ensuring the continuity of care for patient is the transfer of professional responsibility and accountability for some or all aspects of patient care or a group of patients to an individual or a professional group temporarily or permanently. Safe handover of patients is a skill. Safe handover involves the transmission of patient information and also the transfer of responsibility for patient care to another shift or other person.[6] The purpose of each handover involves the effective communication of high-quality clinical information at any time or when the responsibility for caring of the patient is transferred to the person or another shift or hospital.[7] The accurate transmission of information at the end of the shifts is one of the main functions of delivering and evolving with secure and safe transfer of turns.[6] The terms used in describing these conditions include the handover and evolution of patient care, transfer of care responsibilities, clinical reports, and turnaround.[8]
In this article, we want to identify challenges of patient handover in delivering healthcare services to help improve quality and patient safety.
Materials and Methods
The present study was a systematic review of publications and literatures relating to challenges of patient handover or handoff which was conducted based on the Preferred Reporting Item for Systematic Reviews and Meta-analyses guideline.[9] The checklists were used for assessing the methodological quality and to improve the design and reporting of the study. This study was conducted during February 2018 to review all published articles about challenges of patient handover. For this purpose, we studied 10 electronic databases including ProQuest, Ovid, Doaj, Magiran, SID, Scopus, Science Direct, PubMed, and ISI. In addition, for gray literature, we searched articles in Cochrane. Articles were searched from 2010 through 2018. The search keywords included “challenges of patient handover” or “challenges of patient handoff.”
First, the reviewers screened titles based on the objectives of the study and in the field of healthcare system. After that, we reviewed the abstracts. When we understand these articles and selected the related abstracts to our study, then full copies of the articles were extracted from the literature and used for this study.
The inclusion criterion included related articles or literature published in English, from 2010 till 2018 and used our key words in their title and published in the area of healthcare and other articles written about improvement in handover challenges. We found 263 articles. The articles did not have abstract as well as the duplicated ones were excluded. The first and the second authors separately read and reviewed the full texts of the retrieved articles to identify the factors and criteria that had been used for evaluating challenges of handover process (20 articles). Figure 1 shows diagram of selection of articles reviewed.
Figure 1.
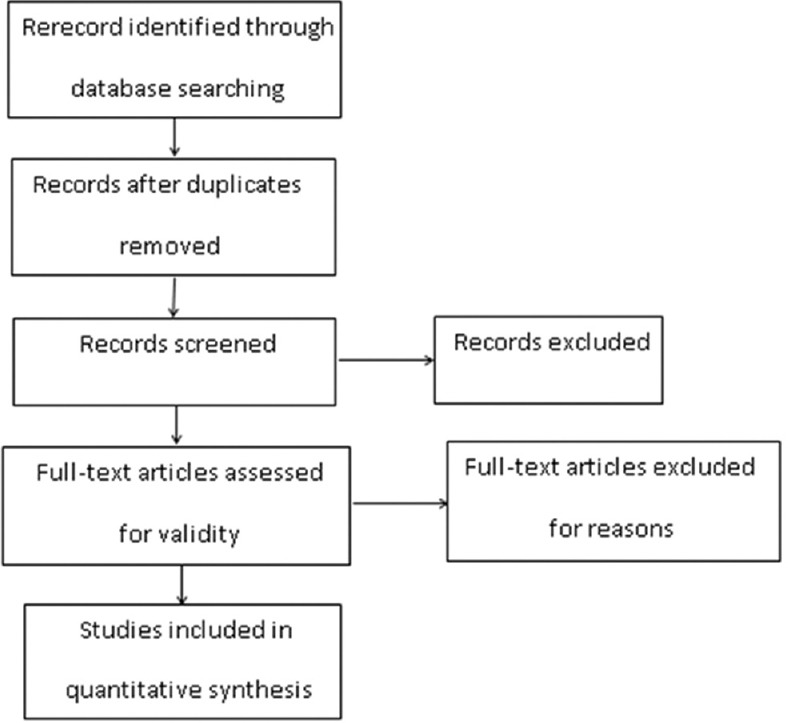
Diagram of selection of articles reviewed
Results
The initial 10 electronic databases search of the literature resulted in a total of 263 articles. Duplicate articles were eliminated, and the number of articles remaining was totaled to 254 articles. At the next step, we reviewed the titles to find those related to the purpose of our study and selected 41 articles. Using systematic screening, abstracts of the articles were studied and 28 articles were selected to be fully reviewed, eight of which were removed due to lack of access to article. All of the selected articles were completely read and thoroughly reviewed on the basis of the inclusion criteria.
We used the COSMIN's criteria to appraise the retrieved. The main psychometric properties of a challenge according to the COSMIN are content, criterion, and construct validity, stability, internal consistency, responsiveness, and interpretability. Details of each articles and their features regarding authors, year of publication, and their finding were more evaluated based on responsiveness and interpretability. The summaries of each article related to our purpose are shown in Table 1. The study results indicated that there are various challenges in handover processes. The most important challenge in handover process which leads to reduced patient safety is the lack of effective communication.
Table 1.
Summaries of articles
| Article title | Authors | Source | Time | Method | Finding |
|---|---|---|---|---|---|
| The Ins and Outs of Change of Shift Handoffs Between Nurses: A Communication Challenge | Carroll et al. | ISI, Scopus, PubMed | 2012 | Multimethod | There is tremendous asymmetry between the roles of giving and receiving a report |
| Challenges of Nursing Handover: A Qualitative Study | Servestani et al. | ISI, Scopus | 2015 | Descriptive exploratory qualitative | The first theme was a no holistic approach and the second one was poor management. The subthemes were nontheistic/unstructured content, low nurses’ ethical and practical involvement and nonpatient-centered approach. Poor management have subthemes were poor task management and poor time and space management |
| The Unappreciated Challenges of Between-Unit Handoffs: Negotiating and Coordinating Across Boundaries | Hilligoss et al. | ISI, Scopus, Science Direct | 2013 | Review the literatures and observation | There are challenges by handoff type in aspect of negotiation and coordination |
| One size fits all? Challenges faced by physicians during shift handovers in a hospital with high sender/recipient ratio | Yang et al. | Scopus | 2015 | Multifaceted approach | This article revealed two major problems, namely poor implementation of nonmodifiable patient identifiers and inadequate transfer of critical information |
| Factors affecting quality of nurse shift handover in the emergency department | Thomson et al. | PubMed | 2017 | Quantitative and cross-sectional | Poor quality handover communication can result in negative consequences for patients, nurses and healthcare organizations. 4 factors were identified as significant explanatory variables (smooth flow of patient through triage, positive relationships between the incoming and outgoing nurse, positive safety climate and positive intrusions) in nurse-to-nurse shift handover quality in the ED |
| Patient Safety and Sociotechnical Considerations for Electronic Handover Tools in an Australian eHealth Landscape | Showell et al. | PubMed | 2010 | Case study | Effective and efficient handover of information, responsibility and accountability is now recognized as crucial for the delivery of safe high-quality health care. By use of electronic system to improve handover |
| Interhospital Transfer Handoff Practices among US Tertiary Care Centers: A Descriptive Survey | Herrigal et al. | PubMed | 2016 | Descriptive survey | Interhospital transfer practices vary widely amongst tertiary care centres. Practices that lead to improved patient handoffs and reduced medical errors need additional prospective evaluation. Standardizing intrahospital handoffs has been shown to decrease preventable medical errors and reduce possible near-miss events |
| Introduction of a Microsoft Excel-based unified electronic weekend handover document in Acute and General Medicine in a DGH: Aims, outcomes, and challenges | Kostelec et al. | PubMed | 2017 | Quasi-experimental before-after design | It showed the impact of having a standardized, electronic handover tool, on compliance with documentation. It helps to management |
| Strengthening surgical handover: Developing and evaluating the effectiveness of a handover tool to improve patient safety | Din et al. | PubMed | 2012 | Intervention | Clinical handover provides a platform to facilitate the continuity of patient information transfer and helps to identify and anticipate patient problems for the forthcoming shift |
| Development of a Nursing Handoff Tool: A Web-Based Application to Enhance Patient Safety | Goldsmith et al. | PubMed | 2010 | Spiral method (focus group interviews) | The single biggest problem in communication is the illusion that it has taken place. The handoff tool will serve to reduce: (1) in accuracy of data transfer, (2) missing critical information, (3) funneling, (4) data transcription error, and (5) time to prepare and give handoff report |
| Managing competing organizational priorities in clinical handover across organizational boundaries | Sujan et al. | PubMed | 2015 | Observation | The problem with handover are frequently linked to organizational factors such as the management of patient flows and time-related performance targets |
| Lost information during the handover of critically injured trauma patients: A mixed-method study | Zakrison et al. | PubMed | 2018 | Mixed-method | Patient handover from one unite to another represents a vulnerable time for communication errors that result in the loss of clinical information |
| Optimizing the patient handoff between emergency medical services and the emergency department | Meisel et al. | PubMed | 2015 | Focus group discussion | Ems providers viewed themselves as patient advocates but often encountered interpersonal, cultural and structural barriers to advocating effectively for their patients |
| Assessing clinical handover between paramedics and the trauma team | Evans et al. | PubMed | 2010 | Cross- sectional and comparative | Information handed over but not documented and information documented but not handed over were the challenges |
| Postoperative handover: characteristics and considerations on improvement: A systematic review | Meller et al. | PubMed | 2013 | Systematic review | Complex work process challenged by interruption, time pressure and a lack of supporting framework. And standardized handover tools in combination with environmental changes, resulting in better flow of information, better team work in two and less technical errors |
| Standardizing postoperative PICU handovers improves handover metrics and patient outcomes | Taicher et al. | PubMed | 2015 | Prospective cohort study | Postoperative communication and patient outcomes can be improved and sustained over time with implementation of a standardized handover protocol |
| A multicenter prospective cohort study of patient transfers from the ICU to the hospital ward | Stelfox et al. | Cochrane | 2017 | Prospective cohort study | ICU-to-ward transfer are characterized failures of patient flow and communication, experienced differently by patient, ICU/ward physicians and nurses, with distinct suggestions for improvement |
| Sociotechnical issues and challenges in implementing safe patient handovers: insights from ethnographic case studies | Balka et al. | Science Direct | 2013 | Ethnographic case study | The contextual nature of information, ethical and medico-legal issued arising in relation to information handover, and issues related to data standard and system interoperability must be addressed if computerized health information systems are to achieve improvements in patient safety related to handovers in care |
| The condition of neonatal transport to NICU in Mazandaran | Nakhshab et al. | SID | 2010 | Descriptive study | The process of current neonatal transport needs to be improved in terms of a regionalized program, communication system, optimal equipment, skilled personnel, etc. |
| Effect of applying checklist on quality of intrahospital transport of intensive care patient | Habibzadeh et al. | SID | 2014 | Quasi-experimental | The checklist will reduce medical mistakes, standardize processes, improve the quality of safety, reduce the cost of health care and facilitate careful and systematic care and improve performance. It is also conducted using a checklist of nursing interventions according to an appropriate framework and can be considered as an effective clinical observation for clinical activities |
ED=Emergency department, ICU=Intensive care unit, PICU=Pediatric intensive care unit, NICU=Neonatal intensive care unit
Poor-quality handover communication has some negative consequences for the patients such as lack of follow-ups on treatments and medication, poor task management, and poor time and space management. The incoming and outgoing nurse have the responsibility to pay close attention to their patient’ needs and conditions to exchange all the necessary and appropriate present and future information about them. So that the patient in safe hands and could avoid consequent patient injury, death, and increased costs of healthcare. In communication the exchange of information such as patient's condition, doctor's order, diagnostic tests, medicines, follow ups and other steps to be taken in the next shift. Also, when new incoming nurse got in charge of the patient, he/she has to introduce himself/herself to the patient. This causes the patient to be relaxed and be sure of his/her nurse and improve his/her recovery process more extensively.
Discussion
Different results and classifications of handover challenges were given in various studies. Most studies have focused on handover communication challenges;[10,11,12,13,14,15,16,17,18,19,20,21,22] other studies have also stated the importance of coordination between the incoming and outgoing nurses.[23,24,25] Another research showed the importance of using a checklist in handover process and suggested that applying checklist could improve intrahospital transport of intensive care patient to other floors. It is recommended to use this checklist for intrahospital transport of intensive care patients to increase patient safety and reduce the complications of intrahospital transport.[26] Another study expressed that poor management can cause some challenges for patient handover process.[27] Time management was also reported as a challenge of handover process.[28,29]
Shift report handover requires technical communication, that is, the transmission of information about the patients, relevant to their conditions and needed care during the next shift. The quality of communication is not only simply equivalent to transmission of technical facts but also includes all interpersonal behaviors that help create an effective conversation and productive relationships among coworkers.[23] There was also information that was written but not transmitted by the outgoing nurse to the incoming nurse, as well as the information transmitted but not recorded and often some information removed or not completed during transfer which could lead to the patient injury or damage the care process.[10,17,18,22] It is suggested that a standard protocol or policy and procedure should be used to ensure that both handover process management and communication are improved.[20] Carroll et al. in their research found that incoming nurse wanted eye contact and opportunity for question, but these same features are experienced as interruptions and problems for the outgoing nurse who wants to transfer care and get to go home.[23] Furthermore, positive relationship between the incoming and outgoing nurses has led to higher ratings of handover quality.[11] In some studies, relationship between coworkers and teamwork attitude was identified as influencing communication in handover process.[30,31,32] Stelfox et al. reported that we have to avoid transfer delays to minimize challenges of the transfer of patient information and responsibility of care.[21]
On the other hand, there are barriers in electronic tools that prevent proper communication in term of comprehensiveness and completeness of information, standardization of data and professional norms, especially in health information exchange during interhospital transfers.[12,13,22]
Hilligoss and Cohen stated the challenges of handoff types in two groups: challenges of negotiation, within-unit handoffs understanding the patient interpersonal responsibility for clinical tasks and in-between-unit handoff, understanding of patient interunit responsibility for clinical tasks, diagnosis and disposition plans. Furthermore, challenges of coordination, within-unit handoff, portfolio problem that is allocating time and attention across multiple patients and in between-unit handoff are additional actions required to initiate and complete patient transfer.[24]
We conclude that the biggest problem is in communication and relationship between the incoming and outgoing nurses. When this problem is solved, other reasons could be least important and could be improved easily.
Conclusions
Hospitals try to provide a lot of clinical and nonclinical services to the patients and other customers in a safe and healthy environment. In-between services such as patient handover also requires a safe environment. It is necessary to identify the challenges of this process in clinical services. Communication between nurses during the handover process has the highest important among reported challenges. In this study, lack of communication among incoming shift nurse and outgoing shift nurse in handover process is one of the main causes of reduced safety and quality of services and patient dissatisfaction.
Financial support and sponsorship
This study was financially supported by School of Management and Medical Information Sciences, Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We appreciate all the help received from faculty of management and medical science of medical university of Isfahan.
References
- 1.Hemmati MP, Sheikh B, Mehri B. The relationship between nurse-patient communication skills and patients' safety status in special sectors. [Last accessed on 2018 Feb 2];Clin Nurs Midwifery J. 2014 3:77–84. URL: http://jcnm.skums.ac.ir/article-1-72-fa.html . [Google Scholar]
- 2.Mohseni M, Raeisi AR, Azami-Aghdash S, Moosavi A, Mousavi SM. Hospital services quality from patients' perspective in Iran: A systematic review and meta-analysis. [Last accessed 2018 Feb 2];Evid Based Health Policy Manage Econ. 2017 1:261–9. URL: http://jebhpme.ssu.ac.ir/article-1-116-en.html . [Google Scholar]
- 3.Hemmati MP, Sheikh B, Mehri B. The relationship between nurse-patient communication skills and patients' safety status in special sectors. [Last accessed on 2018 Feb 2];Clin Nurs Midwifery J. 2014 3:77–84. URL: http://jcnm.skums.ac.ir/article-1-72-fa.html . [Google Scholar]
- 4.Till A, Sall H, Wilkinson J. Safe handover: Safe patients – The electronic handover system. BMJ Qual Improv Rep. 2014;2 doi: 10.1136/bmjquality.u202926.w1359. pii: u202926.w1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Etezadi Gam Tectam Malekzadeh Javad, Mazlum Reza, Taseiri Alireza . Nursing shift counseling guide: A way to ensure the safe operation of nurses in intensive care units. [Last accessed on 2018 Feb 2];Evid Based Q J. 2012 2:7–18. http://osub.mums.ac.ir/osub/nilfr/nmjournal/index.php . [Google Scholar]
- 6.Allen DE, Vitale-Nolen RA. Patient care delivery model improves nurse job satisfaction. J Contin Educ Nurs. 2005;36:277–82. doi: 10.3928/0022-0124-20051101-08. [DOI] [PubMed] [Google Scholar]
- 7.Gier, Kathleen, “The Effects of a Care Delivery Model Change on Nursing Staff and Patient Satisfaction” (2013) Nursing Theses and Capstone Projects. 61. [Last accessed on 2018 Feb 2]. https://digitalcommons.gardner-webb.edu/nursing_etd/61 .
- 8.Australian Medical Association. Safe Handover: safe Patients. Guidance on Clinical Handover for Clinicians and Managers. Australian Medical Association. 2006. [Last accessed on 2018 Feb 2]. Available from: https://www.ama.com.au/sites/default/files/documents/Clinical_Handover_0.pdf .
- 9.Meyer RM, Wang S, Li X, Thomson D, O’Brien-Pallas L. Evaluation of a patient care delivery model: Patient outcomes in acute cardiac care. J Nurs Scholarsh. 2009;41:399–410. doi: 10.1111/j.1547-5069.2009.01308.x. [DOI] [PubMed] [Google Scholar]
- 10.Sheikhbardsiri H, Yarmohammadian MH, Khankeh HR, Nekoei-Moghadam M, Raeisi AR. Meta-evaluation of published studies on evaluation of health disaster preparedness exercises through a systematic review. J Educ Health Promot. 2018;7:15. doi: 10.4103/jehp.jehp_159_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang XJ, Park T, Siah TH, Ang BL, Donchin Y. One size fits all? Challenges faced by physicians during shift handovers in a hospital with high sender/recipient ratio. Singapore Med J. 2015;56:109–15. doi: 10.11622/smedj.2014198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thomson H, Tourangeau A, Jeffs L, Puts M. Factors affecting quality of nurse shift handover in the emergency department. J Adv Nurs. 2018;74:876–86. doi: 10.1111/jan.13499. [DOI] [PubMed] [Google Scholar]
- 13.Showell C, Thomas M, Wong MC, Yee KC, Miller S, Pirone C, et al. Patient safety and sociotechnical considerations for electronic handover tools in an Australian eHealth landscape. Stud Health Technol Inform. 2010;157:193–8. [PubMed] [Google Scholar]
- 14.Herrigel DJ, Carroll M, Fanning C, Steinberg MB, Parikh A, Usher M, et al. Interhospital transfer handoff practices among US tertiary care centers: A descriptive survey. J Hosp Med. 2016;11:413–7. doi: 10.1002/jhm.2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Din N, Ghaderi S, O’Connell R, Johnson T. Strengthening surgical handover: Developing and evaluating the effectiveness of a handover tool to improve patient safety. BMJ Qual Improv Rep. 2012;1 doi: 10.1136/bmjquality.u492.w164. pii: u492.w164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goldsmith D, Boomhower M, Lancaster DR, Antonelli M, Kenyon MA, Benoit A, et al. Development of a nursing handoff tool: A web-based application to enhance patient safety. AMIA Annu Symp Proc. 2010;2010:256–60. [PMC free article] [PubMed] [Google Scholar]
- 17.Sujan MA, Chessum P, Rudd M, Fitton L, Inada-Kim M, Cooke MW, et al. Managing competing organizational priorities in clinical handover across organizational boundaries. J Health Serv Res Policy. 2015;20:17–25. doi: 10.1177/1355819614560449. [DOI] [PubMed] [Google Scholar]
- 18.Zakrison TL, Rosenbloom B, McFarlan A, Jovicic A, Soklaridis S, Allen C, et al. Lost information during the handover of critically injured trauma patients: A mixed-methods study. BMJ Qual Saf. 2016;25:929–36. doi: 10.1136/bmjqs-2014-003903. [DOI] [PubMed] [Google Scholar]
- 19.Meisel ZF, Shea JA, Peacock NJ, Dickinson ET, Paciotti B, Bhatia R, et al. Optimizing the patient handoff between emergency medical services and the emergency department. Ann Emerg Med. 2015;65:310–70. doi: 10.1016/j.annemergmed.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Evans SM, Murray A, Patrick I, Fitzgerald M, Smith S, Andrianopoulos N, et al. Assessing clinical handover between paramedics and the trauma team. Injury. 2010;41:460–4. doi: 10.1016/j.injury.2009.07.065. https://doi.org/10.1016/j.injury. 2009.07.065. [DOI] [PubMed] [Google Scholar]
- 21.Breuer KR, Taicher B, Turner DA. Standardizing postoperative PICU handovers improves handover metrics and patient outcomes. [Last accessed on 2018 Feb 2];Qual Saf. 2015 16:256–62. doi: 10.1097/PCC.0000000000000343. https://doi.org/10.1097/PCC.0000000000000343. [DOI] [PubMed] [Google Scholar]
- 22.Stelfox HT, Leigh JP, Dodek PM, Turgeon AF, Forster AJ, Lamontagne F, et al. A multi-center prospective cohort study of patient transfers from the intensive care unit to the hospital ward. Intensive Care Med. 2017;43:1485–94. doi: 10.1007/s00134-017-4910-1. [DOI] [PubMed] [Google Scholar]
- 23.Balka E, Tolar M, Coates S, Whitehouse S. Socio-technical issues and challenges in implementing safe patient handovers: Insights from ethnographic case studies. Int J Med Inform. 2013;82:e345–57. doi: 10.1016/j.ijmedinf.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Carroll JS, Williams M, Gallivan TM. The ins and outs of change of shift handoffs between nurses: A communication challenge. BMJ Qual Saf. 2012;21:586–93. doi: 10.1136/bmjqs-2011-000614. [DOI] [PubMed] [Google Scholar]
- 25.Hilligoss B, Cohen MD. The unappreciated challenges of between-unit handoffs: Negotiating and coordinating across boundaries. Ann Emerg Med. 2013;61:155–60. doi: 10.1016/j.annemergmed.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 26.Nakhshab M, Vosughi E. The Condition of Neonatal Transport to NICU in Mazandaran. [Last accessed on 2018 Feb 2];J Mazandaran Univ Med Sci. 2010 20(78):50–57. URL: http://jmums.mazums.ac.ir/article-1-623-en.html . [Google Scholar]
- 27.Habibzadeh F, Imanipour M, Mohammad Aliha J, Mehran A. Effect of applying checklist on quality of intra-hospital transport of intensive care patients. [Last accessed on 2018 Feb 2];2014 3(3):30–37. URL: http://journal.icns.org.ir/article-1-257-en.html . [Google Scholar]
- 28.Sabet Sarvestani R, Moattari M, Nasrabadi AN, Momennasab M, Yektatalab S. Challenges of nursing handover: A qualitative study. Clin Nurs Res. 2015;24:234–52. doi: 10.1177/1054773813508134. [DOI] [PubMed] [Google Scholar]
- 29.Kostelec P, Emanuele Garbelli P, Emanuele Garbelli P. Introduction of a Microsoft excel-based unified electronic weekend handover document in acute and general medicine in a DGH: Aims, outcomes and challenges. BMJ Qual Improv Rep. 2017;6 doi: 10.1136/bmjquality.u212152.w5721. pii: u212152.w5721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Møller TP, Madsen MD, Fuhrmann L, Østergaard D. Postoperative handover: Characteristics and considerations on improvement: A systematic review. Eur J Anaesthesiol. 2013;30:229–42. doi: 10.1097/EJA.0b013e32835d8520. [DOI] [PubMed] [Google Scholar]
- 31.Anthony MK, Preuss G. Models of care: The influence of nurse communication on patient safety. Nurs Econ. 2002;20:209–15, 248. [PubMed] [Google Scholar]
- 32.Cheung DS, Kelly JJ, Beach C, Berkeley RP, Bitterman RA, Broida RI, et al. Improving handoffs in the emergency department. Ann Emerg Med. 2010;55:171–80. doi: 10.1016/j.annemergmed.2009.07.016. doi: 10.1016/j.annemergmed.2009.07.016. Epub 2009 Oct 2. [DOI] [PubMed] [Google Scholar]


