Abstract
Background:
Bipolar disorder is a disabling illness characterized by recurrent episodes of mania, hypomania, and depression. The dialectical behaviour therapy (DBT) is basically designed to help regulate excitement, tolerance of discomfort, mindfulness and interpersonal relationships. This study aimed to determine the effectiveness of DBT on executive function, emotional control and symptom relief in patients with type 1 bipolar disorder.
Materials and Methods:
This clinical trial was conducted on 50 patients with type 1 bipolar disorder. These patients were divided into two 25 populated groups of controls and intervention. The control group did not receive any other alternative therapy apart from routine medications, but in the intervention group, in addition to routine medications, DBT treatment was also done as complementary therapy in 12 sessions based on Dick's protocol. Then, Mania severity, emotional control and their executive functions were evaluated before and after the intervention and compared in two groups.
Results:
After the intervention, the scores of mania and depression mood with the mean of 2.12 ± 3.09 and 31.08 ± 8.98 respectively in intervention group were significantly lower than control group with the mean of 4.24 ± 4.11 and 39.92 ± 9.05 respectively (P < 0.05). Depression and executive function of the patients had no significant difference between the two groups in the post-intervention period and had a modest and non-significant change.
Conclusion:
DBT has been effective in decreasing the intensity of mania, but, it cannot be used to reduce the emotional instability and impulsivity of these patients along with drug therapy although it has improved the executive functions and depression of the patients.
Keywords: Bipolar I disorder, dialectical behavioural therapy, emotional control, executive function
Introduction
Bipolar I disorder (BPD-I) is a chronic psychiatric disorder with recurrent episodes of depression, mania and hypomania. In addition to the mood instability, it is associated with significant dysfunction, low quality of life and the high rate of suicide compared to the general population.[1] The prevalence of this disorder is 0.4%–1.6%.[2] The mean age of the first mania episode, hypomania, or major depression in BPD-I is about 18 years. The recurrence rate of this disorder is more than 90% in the lifetime of these patients. The male to female ratio is approximately equal in BPD-I. In BPD, men refer to the physicians more with drug use disorders and women with simultaneous anxiety and eating disorders.[3] On the other hand, patients with BPD are also impaired in assignment tasks such as continuous performance task and digit span task, as well as in functional memory and performance such as Wisconsin Card Sorting Test (WCST), Trail Making Test, Verbal Fluency Test and Stroop Word Colour Test. These findings are also confirmed by nerve imaging studies that have shown the executive functions disorder is not specific to patients with schizophrenia and can also be found in BPD patients. In fact, from a biological point of view, there is considerable empirical evidence that bipolar disorder has major functional impairments in serotonergic and dopaminergic systems, as well as in the frontal lobes of the brain.[4,5] Many of the data suggest a defect in most of the frontal lobe executive functions in bipolar disorder and borderline personality.[5,6,7] In BPD patients, executive functional impairment is observed even in the periods of euthymia in the areas of sustained attention, response control, cognitive planning, and cognitive flexibility.[8]
Therefore, in addition to the injuries related to the emotional regulation in bipolar patients, evidence indicates injury to attention, memory and executive functions in such patients and it seems that a trait is associated with this disorder,[9,10] which increases the burden of disease, its time, and cumulative therapeutic effects.[11]
Today, special therapies are available for both manic and depression episodes. However, drug therapy is the main method of treatment for patients with bipolar disorder; Longitudinal retrospective studies show that less than half of the patients with bipolar disorder have had a long-term response to treatment even if the treatment continues, many patients have not achieved a complete recovery or have had lower acceptance for drug treatments,[12] that this medication refusal will result in at least one relapse episodes.[13] Therefore, adding psychosocial interventions such as cognitive-behavioral therapy (CBT), interpersonal social rhythm therapy (IPSRT) and family-focused therapy (FFT) as complementary therapies can increase the efficacy of treatment.
Previous studies have shown that CBT has been effective in treating depression episodes in bipolar disorder but its effectiveness in treating mania is unclear.[14] FFT also prevents symptoms of recurrence rather than individual treatments but this type of treatment is more suitable for patients who have family problems and conflicts, in addition to their bipolar disorder.[15] Therefore, complementary therapies seem to be more effective in helping patients with bipolar disorder to be more effective.
In this regard, some studies have shown the effectiveness of dialectical behavior therapy (DBT) techniques in treating patients with BPD.[16] Although this treatment was developed for borderline personality disorder, its similarities with bipolar disorder with respect to the lack of adjustment of emotions, impulsivity and interpersonal problems, shows the logical use of DBT in treatment of bipolar disorder. DBT is an eclectic treatment and its related concepts have been extracted from supportive, cognitive, behavioural, and mindfulness-based therapies,[17] therefore, it seems to be more effective than other treatments. In DBT, as in other behavioural approaches, it is assumed that all behaviours (including emotions and thoughts) are learned and patients deal in a way that reinforces and even rewards their behaviour.[18] The goal of DBT is to create equilibrium between change and acceptance[19] and four main skills including distress tolerance, emotional regulation, mindfulness (shifting attention to activities and events of the present time) and effective interpersonal relationships are taught.[20] This behavioural therapy has been used in recent years for other types of mental illness such as drug abuse, eating disorders, schizophrenia and posttraumatic stress disorder[16] but few studies have been done about its effectiveness on bipolar disorder. Studies in this area have indicated the impact of DBT techniques on depression reduction and improvement of the excitement control of these patients in these 12-week, 6-month and 1 year investigations.[14,16,21]
Since DBT uses mindfulness techniques and many studies demonstrate the effectiveness of mindfulness-focused techniques on improving attention and executive function,[22,23,24] DBT seems to improve dipolar patients' performance in addition to adjusting their excitement.
Because of the areas that are related to the emotion regulation, it can be pointed out the anterior and frontal lobes. According to available information, executive functions are also related to these lobes. If DBT can affect emotional regulation, it can affect the brain's anterior and frontal lobes, as well as the executive functions. Therefore, considering the relationship between deep venous thrombosis, emotion regulation and the mentioned lobes it can be said that this treatment can improve the executive function of BPD patients.[24]
Therefore, considering the early use of DBT in the treatment of this disease, few studies have been conducted on the effectiveness of DBT, especially in the field of executive functions, and also due to the lack of evaluating its effectiveness in the Iranian population; more information is needed to support DBT as an effective treatment for bipolar disorder. For this purpose, in the present study, it has been evaluated the effectiveness of DBT on executive performance, emotional control and severity of its symptoms in patients with BPD-I.
Materials and Methods
The present study is a randomized controlled clinical trial. The study population included all patients with BPD-I referred to Noor and Ali Asghar Hospitals in Isfahan during 2018.
The sample size of 25 patients in each group to compare the mean between two groups was estimated based on a confidence level of 95%, a statistical power of test of 80%, By the standard deviation of the Beck Depression Scale score in a pilot study, the intervention and control groups equal to 12 and 10, respectively, and at least the mean difference between the two groups equal to 9.
So in a purposeful nonprobability way, 50 patients aged 20–45 years were included in the study in the maintenance phase of BPD-I and with the lack of personality disorders, using alcohol and drugs, or organic problems such as hypothyroidism, seizures or encephalopathies, receive no psychotherapy from 6 months ago, not using other psychotherapy simultaneously, not having psychotic symptoms, minimum level of guidance school education and satisfaction.
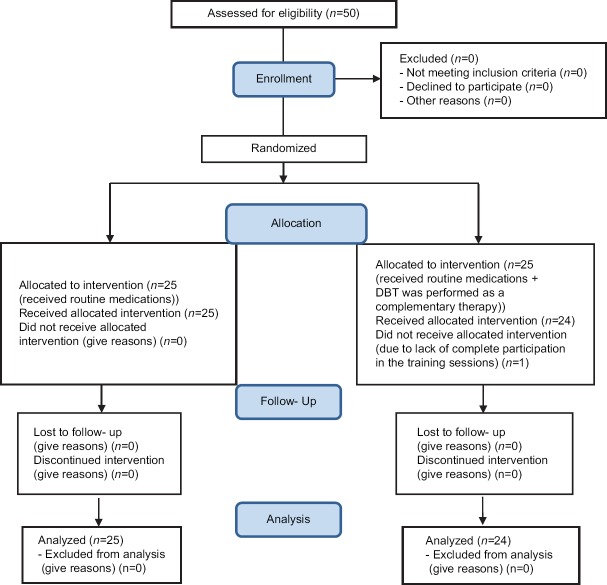
In the presence or creation of current episodes of mania in patients and absence in the two or more than two times of training sessions, they were omitted from the study. Consequently, only one case in intervention group was excluded from the study due to lack of complete participation in the training sessions [Figure 1]. This research project was approved scientifically by the Research Committee of Isfahan University of Medical Sciences and ethically by the ethic committee of the university (Ethic code: IR.MUI.MED.REC.1397.045). Also, it was registered in the Iranian registration system with IRCT20180909040974N1 before starting participant recruitment.
Figure 1.
Consort flow diagram
Then patients were classified in a stratified way and they were divided into two groups of control and intervention, each one consisting 25 individuals. At the beginning of the study, their demographic data, such as age, sex, occupation, level of education and duration of their illness were recorded.
To assess the severity of mania, the Young Mania Rating Scale (YMRS) questionnaire was used while the affective control scale (ACS) questionnaire was utilized for the emotional control of them and The Beck Depression Index (BDI-II) questionnaire was applied to determine the level of depression in patients. Also, Color Trail Test (CTT) was used to evaluate their executive functions and the results of the evaluations were recorded before intervention.
YMRS was designed by Yang in 1978 in order to evaluate the severity of mania symptoms, and it has concurrent validity, reliability and Cronbach's alpha of more than 0.7–0.9[25] and it has been standardized in Iran in 2005 (Cronbach's alpha = 0.72).[26] This scale has eleven items; seven items from 0 to 4 and four items from 0 to 8 are scored based on a clinical interview with the patient. Total score is from 0 to 60 in which < 20 is considered as normal and more than 20 is taken into account as mania. ACS has 42 questions and its purpose is to assess the ability to control emotions and its sub-scales (anger, depressed mood, anxiety, and positive affection).
This scale is in form of self-evaluation and evaluates 4 aspects of anger (including questions: 1, 8, 11, 16, 28, 30, 34, 39), depressed mood (including questions: 3, 4, 13, 19, 25, 27, 29, 37), anxiety (including questions: 5, 7, 9, 15, 17, 20, 21, 24, 26, 33, 35, 38, 40) and positive affection (including questions: 2, 6, 10, 12, 14, 18, 22, 23, 31, 32, 36, 41, 42).
The answer to its questions is based on the 7 scores Likert scale (from “strongly disagree = 1” to “strongly agree” =7), and therefore, total score of this questionnaire varies from 42 to 294. The validity and reliability of this test in general and in each dimension have been reported and approved to be more than 0.7 in abroad as well as Iran (in 2009).[27] The BDI-II was also re-reviewed in 1996 to greater coordination with the new Diagnostic and Statistical Manual of Mental Disorder criteria. The correlation between the two previous and new forms of the questionnaire was reported between 0.89 and 0.97.[28] In the BDI-II, the subject is asked to consider their feelings in the last 2 weeks and answers the questions. This questionnaire has been designed to measure the severity of depression in adults and adolescents ranging from 13 years and older which has 21 questions. Validity and reliability have been evaluated and confirmed in the study of Beck et al. (1988) and the study of Taheri Tanjani et al. in Iran; respectively with Cronbach's alpha of 0.92 and 0.73.[28,29] The total score of this scale can range from 0 to 62.
Score (1–15) or (1–18) indicates lack of depression, score between (16–31) or (18–28) shows mild depression, (32–47) or (35–29) represents moderate depression and score between (62–48) or (63-–36) points to severe depression.[28]
The CTT assesses sustained attention, sequencing, and executive function and was designed to reduce reliance on language and diminish the effects of cultural bias. The CTT consists of two parts. For Part A, the examinee rapidly connects circles numbered 1–25 in sequence. In Part B, the examinee rapidly connects numbered circles in sequence but alternates between two colors (pink and yellow). The time to complete each part was recorded in seconds, together with performance variables, such as near-misses, prompts, number of sequence errors, and number of color sequence errors.[30] The administration time for the CTT is 3–8 min. The validity of the CTT has been documented for various clinical and neuropsychological populations. The test–retest reliability of the CTT has been reported to be. 64 for the CTT-A and 0.79 for the CTT-B after 2 weeks.[31] In Iran, Tavakoli et al. showed that correlation coefficients between the first performance and retest were 0.909 and 0.912 for the CCT-A and CTT-B, respectively.[5]
After recording the mentioned information before the study, all patients in both groups received their routine medications by a psychiatrist prescription. Prescribed medicine included Mood stabilizers and atypical antipsychotics. Moreover, the dosage and type of prescribed drugs were constant and identical over the last 3 months.
In the control group, no other intervention was performed, but in the intervention group, DBT was performed as a complementary therapy by a trained PhD expert in Clinical Psychology in the field of third wave therapy along with a psychiatric resident.
The intervention consists of 12 sessions each of which lasts 1 h to one and a half hours.[16] Twenty-five subjects in intervention groups were divided into two groups of 12 and 13 cases. Both groups were simultaneously trained dialectically on days of the weeks [Table 1].
Table 1.
The content of dialectical behavioral therapy treatment sessions
| Week | DBT technique | Content of session |
|---|---|---|
| The 1st week | Introduction of mindfulness and completion of pretest | Teaching facts about bipolar disorder, depression, mania, hypomania and psychosis, and pretest completion |
| The 2nd week | Mind states | Mentioning the causes of bipolar disorder |
| The 3rd week | Introducing medications | Commenting on medication |
| The 4th week | Making balance | Training to reduce vulnerability to excitement, establishing balance for eating, sleeping and exercise |
| The 5th week | Not judging | Teaching solutions for not judging |
| The 6th week | Basic acceptance | Teaching on how to get basic acceptance |
| The 7th week | Individual management | Managing distraction and excitement and relaxing oneself |
| The 8th week | Self-confirmation | Teaching and introducing the realities about excitement |
| The 9th week | Coping with excitement | Learning to cope with excitements and control them |
| The 10th week | Take a look at relationships | Learning to close up pleasurable activities to responsibilities and establishing relationships |
| The 11th week | Decisiveness | Training decisiveness |
| The 12th week | Summary and completion of posttest | Review of medical provisions, consolidation of the materials learned and using them to prevent relapse, completion of posttest |
DBT: Dialectical behavioral therapy
All the patients in both groups received YMRS, ACS, BDI-II, and CTT tests immediately after the 12th session as well as 3 months later and the results were recorded. Finally, the collected data were entered into SPSS software (version 21; SPSS Inc., Chicago, Ill., USA) and analyzed by statistical tests of multivariate covariance analysis and paired t-test. In addition, a significance level was considered to be <0.05.
Results
In this study, the control group consisted of 9 males (36%) and 16 females (64%) with a mean age of 29.68 ± 5.12 years, and the intervention group consisted of 11 males (45.8%) and 13 females (54.2%) with a mean age of 32.25 ± 9.57 years and two group were matched in this regard (P > 0.05) [Table 2].
Table 2.
Demographic characteristics of patients in the two groups
| Characteristics | Intervention (n=24) | Control (n=25) | P |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 11 (45.8) | 9 (36.0) | 0.567 |
| Female | 13 (54.2) | 16 (64.0) | |
| Age (year) | 32.25±9.57 | 29.68±5.12 | 0.244 |
| Level of education (the success years) | 4.63±1.38 | 5.00±1.29 | 0.330 |
At the beginning of the study, the mean score of mania and depression in the two groups did not differ significantly, but after the intervention, the mania score in the intervention group with the mean of 3.09 ± 2.12 was lower than the control group with the mean of 4.11 ± 4.24 (P = 0.048). In fact, the score of mania in the intervention group decreased significantly after implementation of DBT sessions (P = 0.011). However, depression of patients after intervention was not significantly different between the two groups and no significant reduction was seen (P > 0.05) [Table 3].
Table 3.
Comparison of the mania and depression mean scores in patients before and after intervention in the two groups
| Variables | Intervention (n=24) | Control (n=25) | Pa |
|---|---|---|---|
| Mania | |||
| Before | 4.79±3.17 | 5.88±2.91 | 0.215 |
| After | 2.12±3.09 | 4.24±4.11 | 0.048 |
| Pb | 0.011 | 0.115 | |
| BDI | |||
| Before | 20.63±16.03 | 28.28±10.76 | 0.054 |
| After | 26.00±11.63 | 23.76±11.78 | 0.438 |
| Pb | 0.121 | 0.208 |
aThe significance level of multivariate covariance analysis was compared the mean of the variables between the two groups, bThe significance level of the paired t-test for comparing the mean of the variables after the intervention than before the intervention in each group. BDI: Beck Depression Index
In addition, affective control of patients in general and in regarding each dimensions (anger, depressed mood, anxiety and positive affection) was not significantly different between the two groups at the beginning of the study (P > 0.05). However, a significant difference was seen between the two groups only in the depressed mood dimension after the intervention (Intervention group = 31.08 ± 8.98 versus control group = 37.12 ± 10.10; P = 0.001) but no significant changes in other dimensions (P > 0.05) [Table 4].
Table 4.
Comparison of affective control and its dimensions in patients before and after intervention in two groups
| Variables | Intervention (n=24) | Control (n=25) | Pa |
|---|---|---|---|
| Emotional control | |||
| Before | 172.27±40.02 | 180.61±25.44 | 0.386 |
| After | 162.27±48.49 | 188.91±37.42 | 0.054 |
| Pb | 0.413 | 0.472 | |
| Anger | |||
| Before | 34.13±10.40 | 34.80±10.39 | 0.627 |
| After | 33.00±11.11 | 37.12±10.10 | 0.273 |
| Pb | 0.707 | 0.499 | |
| Depressed mood | |||
| Before | 36.17±10.12 | 36.12±8.31 | 0.949 |
| After | 31.08±8.98 | 39.92±9.05 | 0.001 |
| Pb | 0.039 | 0.151 | |
| Anxiety | |||
| Before | 51.78±14.47 | 54.67±11.62 | 0.340 |
| After | 51.30±16.23 | 56.96±13.31 | 0.202 |
| Pb | 0.903 | 0.551 | |
| Positive affection | |||
| Before | 49.68±11.78 | 54.76±12.65 | 0.110 |
| After | 47.05±15.38 | 55.56±11.88 | 0.121 |
| Pb | 0.488 | 0.812 |
aThe significance level of multivariate covariance analysis was compared the mean of the variables between the two groups, bThe significance level of the paired t-test for comparing the mean of the variables after the intervention than before the intervention in each group
Finally, evaluating the performance of patients in the two groups indicated that there was no significant difference between two groups in terms of mean of executive performance based on the CTT test before and after intervention (P > 0.05) [Table 5].
Table 5.
Comparison the mean of patients’ executive performance before and after intervention in the two groups
| Variables | Intervention (n=24) | Control (n=25) | Pa |
|---|---|---|---|
| CTT-A | |||
| Before | 78.00±54.7 | 56.00±12.79 | 0.056 |
| After | 77.27±45.49 | 58.64±12.7 | 0.054 |
| Pb | 0.960 | 0.467 | |
| CTT-B | |||
| Before | 166.50±79.8 | 128.83±63.16 | 0.072 |
| After | 165.01±56.32 | 127.30±81.06 | 0.066 |
| Pb | 0.941 | 0.934 |
aThe significance level of multivariate covariance analysis was compared the mean of the variables between the two groups, bThe significance level of the paired t-test for comparing the mean of the variables after the intervention than before the intervention in each group. CTT: Color Trail Test
Discussion
With regard to the effect of DBT on the severity of mania and depression in patients with BPD-I, the results of this study showed that although the two groups were similar in terms of these two variables at the beginning of the study, the mania score in the DBT-receiving group was significantly reduced after the intervention, and this group showed significant difference in comparing with control group (without DBT treatment) after intervention. However, the depression score of these patients, despite a slight decrease, did not differ significantly between the two groups after the intervention.
In contrast to the results of this study, Van Dijk et al.[14] in a work on the effect of DBT on bipolar disorder symptoms showed that DBT techniques reduced depressive symptoms but did not reduce the severity of mania symptoms.[14] Many other previous studies have also found inconsistent results in this regard. As in the study of Goldstein et al., the estimated average rate of euthymic weeks over follow-up among DBT receiving adolescents was more than twice of those receiving psychological treatment as usual (TAU). Furthermore, DBT received adolescents showed less severe depressive symptoms during follow-up and displayed significant improvement of manic symptoms with treatment, whereas adolescents receiving TAU did not.[32]
Similarly Fristad et al. documented improvement in mood symptom severity on a composite scale of depression and mania among school-age mood-disordered youth with a 12 weeks multifamily psychoeducational psychotherapy.[33] Among adolescents with blood pressure (BP), Miklowitz et al. demonstrated improvement in depression symptoms, but not about mania, with FFT-A.[34] documented improvement was shown by Hlastala et al. in both depression and mania symptoms among adolescents with BP in an open trial of IPSRT.[35]
In addition, affective control of patients with DBT treatment was not significantly different between the two groups before and after intervention, but more detailed examination showed that this intervention can play a significant role in controlling and reducing the patients' depressed mood. However, it has not been able to have significant effect on other dimensions of affective control in the factors including patients' anger, anxiety and positive affection.
While only depressed mood decreased in this research and other dimensions of affective control did not improve significantly, in contrast to the results of this study, some studies suggest the effectiveness of DBT and its group skill learning in reducing impulsivity, self-harm, emotion regulation and improving a number of mood and emotional disorders such as depression, anxiety, anger, emotional instability and irritability.[16,36,37]
In fact, the main focus of DBT is on the learning, application, and generalization of specific adaptive skills trained in this therapeutic approach and its final goal is helping a patient with BPD to overcome this defective cycle and affective instability.[38] Moreover, brain images showed that performing mindfulness exercises of the components of DBT can reduce bio-vulnerability to negative emotional stimuli and can be effective in affective control of the individual by increasing the activity of frontal part of the brain (associated with positive affections) and reducing brain base activity (associated with involuntary behavior caused by emotions).[14,39]
Therefore, it seems that this therapeutic approach can have an effective therapeutic role on improving the emotional control of patients. The reason for the lack of significance difference in all dimensions might be due to low sample size, limited number of sessions (8 sessions) or lack of completion affective control questionnaire accurately by patients in our study. Further studies seem to be required in this regard. Finally, the executive performance of the patients showed slight and nonsignificant difference before and after the intervention.
Only one study has been conducted with regard to evaluation the executive performance of these patients, which its results are inconsistent with those of present study. In this study, Afshari et al. evaluated the effect of this therapeutic approach in 12 sessions on the executive performance of BPD patients and concluded that the combination of DBT therapy and drug therapy could improve the performance of these patients in effective planning and problem solving. Thus, DBT can have an impact on the executive performance.[40]
A few studies have conducted on the effect of this therapeutic approach on executive performance which is significantly associated with psychological function in the area such as job performance, family relationship and life satisfaction.[41] Executive performance is considered as an umbrella, which includes a variety of cognitive functions as working memory planning, attention, inhibition, self-regulation and many of the functions of the frontal lobe.[42]
It should be noted that the mentioned studies have measured and evaluated the executive performance of patients by using other methods such as Wisconsin Card Sorting Task (WCST) and Tower of London. Therefore, their measurement tools were different from those of our study that might justify the inconsistent results of present study.
In general, one of the strengths of this study was the combination of psychotherapy and drug therapy to achieve effective results for patients with BPD-I. Although significance was found in only two items of mania severity and depressed mood, but it seems that this approach in combination with drug therapy can keep the patient in a stable condition. Short-term psychotherapy such as DBT can be helpful in regulation of emotions, mindfulness, relationships, and emotional control. These four skills are the core of all psychotherapies and psychological disorders. Therefore, DBT skills can be used for other psychological disorders.
Some limitations of this study included difficulty in follow up to continue the sessions, as well as performing the exercises and tasks by patient and commuting problems of patients to the training center.
Conclusion
Based on the results of this study, DBT skills can significantly reduce the severity of mania and patients' depressed mood, but had slight and non-significant impact in improving depression, emotional control, anger, anxiety, positive affection and executive performance.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I am extremely thankful to Professor Majid Barekatain for his valuable suggestions have helped me in planning, executing, and completing my research.
References
- 1.Rowland TA, Marwaha S. Epidemiology and risk factors for bipolar disorder. Ther Adv Psychopharmacol. 2018;8:251–69. doi: 10.1177/2045125318769235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68:241–51. doi: 10.1001/archgenpsychiatry.2011.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Philadelphia: American Psychiatric Association; 2013. p. 2. [Google Scholar]
- 4.Paris J, Gunderson J, Weinberg I. The interface between borderline personality disorder and bipolar spectrum disorders. Compr Psychiatry. 2007;48:145–54. doi: 10.1016/j.comppsych.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Tavakoli M, Barekatain M, Emsaki G. An Iranian normative sample of the color trails test. Psychol Neurosci. 2015;8:75. [Google Scholar]
- 6.Gvirts HZ, Harari H, Braw Y, Shefet D, Shamay-Tsoory SG, Levkovitz Y. Executive functioning among patients with borderline personality disorder (BPD) and their relatives. J Affect Disord. 2012;143:261–4. doi: 10.1016/j.jad.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 7.Gvirts HZ, Braw Y, Harari H, Lozin M, Bloch Y, Fefer K, et al. Executive dysfunction in bipolar disorder and borderline personality disorder. Eur Psychiatry. 2015;30:959–64. doi: 10.1016/j.eurpsy.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 8.Mann-Wrobel MC, Carreno JT, Dickinson D. Meta-analysis of neuropsychological functioning in euthymic bipolar disorder: An update and investigation of moderator variables. Bipolar Disord. 2011;13:334–42. doi: 10.1111/j.1399-5618.2011.00935.x. [DOI] [PubMed] [Google Scholar]
- 9.Clark L, Goodwin GM. State- and trait-related deficits in sustained attention in bipolar disorder. Eur Arch Psychiatry Clin Neurosci. 2004;254:61–8. doi: 10.1007/s00406-004-0460-y. [DOI] [PubMed] [Google Scholar]
- 10.Malhi GS, Ivanovski B, Szekeres V, Olley A. Bipolar disorder: It's all in your mind? The neuropsychological profile of a biological disorder. Can J Psychiatry. 2004;49:813–9. doi: 10.1177/070674370404901204. [DOI] [PubMed] [Google Scholar]
- 11.Torres IJ, DeFreitas VG, DeFreitas CM, Kauer-Sant'Anna M, Bond DJ, Honer WG, et al. Neurocognitive functioning in patients with bipolar I disorder recently recovered from a first manic episode. J Clin Psychiatry. 2010;71:1234–42. doi: 10.4088/JCP.08m04997yel. [DOI] [PubMed] [Google Scholar]
- 12.Akiskal SH. Mood disorders. In: Sadock BJ, Sadock VA, Ruiz P, editors. Kaplan and Sadock's Comprehensive Textbook of Psychiatry. 9th ed. Vol. 121. Philadelphia: Lippincott Williams and Wilkins; 2009. pp. 1629–45. [Google Scholar]
- 13.Sadock BJ, Sadock VA. Kaplan and Sadock's Synopsis of Psychiatry: Behavioral Sciences/Clinical Psychiatry. Philadelphia: Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 14.Van Dijk S, Jeffrey J, Katz MR. A randomized, controlled, pilot study of dialectical behavior therapy skills in a psychoeducational group for individuals with bipolar disorder. J Affect Disord. 2013;145:386–93. doi: 10.1016/j.jad.2012.05.054. [DOI] [PubMed] [Google Scholar]
- 15.McMahon K, Herr NR, Zerubavel N, Hoertel N, Neacsiu AD. Psychotherapeutic treatment of bipolar depression. Psychiatr Clin North Am. 2016;39:35–56. doi: 10.1016/j.psc.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Miller AL, Rathus JH, Linehan MM. Dialectical Behavior Therapy with Suicidal Adolescents. New York: Guilford Press; 2006. [Google Scholar]
- 17.McKay M, Wood JC, Brantley J. The Dialectical Behavior Therapy Skills Workbook: Practical DBT Exercises for Learning Mindfulness, Interpersonal Effectiveness, Emotion Regulation and Distress Tolerance. Australia: 2010. ReadHowYouWant. com. [Google Scholar]
- 18.Pederson LD. Dialectical Behavior Therapy: A Contemporary Guide for Practitioners. The Atrium Southern Gate: John Wiley & Sons, Ltd; 2015. [Google Scholar]
- 19.Barlow DH, editor. Clinical Handbook of Psychological Disorders: A Step-By-Step Treatment Manual. New York: Guilford Publications; 2014. [Google Scholar]
- 20.Gross JJ, editor. Handbook of Emotion Regulation. New York: Guilford Publications; 2013. [Google Scholar]
- 21.Goldstein TR, Axelson DA, Birmaher B, Brent DA. Dialectical behavior therapy for adolescents with bipolar disorder: A 1-year open trial. J Am Acad Child Adolesc Psychiatry. 2007;46:820–30. doi: 10.1097/chi.0b013e31805c1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang YY, Yang L, Leve LD, Harold GT. Improving executive function and its neurobiological mechanisms through a mindfulness-based intervention: Advances within the field of developmental neuroscience. Child Dev Perspect. 2012;6:361–6. doi: 10.1111/j.1750-8606.2012.00250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moore A, Malinowski P. Meditation, mindfulness and cognitive flexibility. Conscious Cogn. 2009;18:176–86. doi: 10.1016/j.concog.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 24.Gallant SN. Mindfulness meditation practice and executive functioning: Breaking down the benefit. Conscious Cogn. 2016;40:116–30. doi: 10.1016/j.concog.2016.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 26.Barakatain M, Tavakkoli M, Molavi H, Maroofi M, Salehi M. Standardization, validity and reliability of young mania rating scale in Iran. J Psychol. 2007;2:150–66. [Google Scholar]
- 27.Swart M, Kortekaas R, Aleman A. Dealing with feelings: Characterization of trait alexithymia on emotion regulation strategies and cognitive-emotional processing. PLoS One. 2009;4:e5751. doi: 10.1371/journal.pone.0005751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Beck AT, Steer RA, Carbin MG. Psychometric properties of the beck depression inventory: Twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 29.Taheri Tanjani P, Garmaroudi GH, Azadbakht M, Fekrizadeh Z, Hamidi R, Fathizadeh SH, et al. Validity and reliability beck depression inventory-II among the Iranian elderly population. Q J Sabzevar Univ Med Sci. 2015;22:189–98. [Google Scholar]
- 30.Strauss E, Sherman EM, Spreen O. A Compendium of Neuropsychological Tests: Administration, Norms, and Commentary. Washington: American Chemical Society; 2006. [Google Scholar]
- 31.Vogel A, Stokholm J, Jørgensen K. Performances on symbol digit modalities test, color trails test, and modified stroop test in a healthy, elderly Danish sample. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2013;20:370–82. doi: 10.1080/13825585.2012.725126. [DOI] [PubMed] [Google Scholar]
- 32.Goldstein TR, Fersch-Podrat RK, Rivera M, Axelson DA, Merranko J, Yu H, et al. Dialectical behavior therapy for adolescents with bipolar disorder: Results from a pilot randomized trial. J Child Adolesc Psychopharmacol. 2015;25:140–9. doi: 10.1089/cap.2013.0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fristad MA, Verducci JS, Walters K, Young ME. Impact of multifamily psychoeducational psychotherapy in treating children aged 8 to 12 years with mood disorders. Arch Gen Psychiatry. 2009;66:1013–21. doi: 10.1001/archgenpsychiatry.2009.112. [DOI] [PubMed] [Google Scholar]
- 34.Miklowitz DJ, Axelson DA, Birmaher B, George EL, Taylor DO, Schneck CD, et al. Family-focused treatment for adolescents with bipolar disorder: Results of a 2-year randomized trial. Arch Gen Psychiatry. 2008;65:1053–61. doi: 10.1001/archpsyc.65.9.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hlastala SA, Kotler JS, McClellan JM, McCauley EA. Interpersonal and social rhythm therapy for adolescents with bipolar disorder: Treatment development and results from an open trial. Depress Anxiety. 2010;27:457–64. doi: 10.1002/da.20668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van den Bosch LM, Verheul R, Schippers GM, van den Brink W. Dialectical behavior therapy of borderline patients with and without substance use problems. Implementation and long-term effects. Addict Behav. 2002;27:911–23. doi: 10.1016/s0306-4603(02)00293-9. [DOI] [PubMed] [Google Scholar]
- 37.Kröger C, Schweiger U, Sipos V, Arnold R, Kahl KG, Schunert T, et al. Effectiveness of dialectical behaviour therapy for borderline personality disorder in an inpatient setting. Behav Res Ther. 2006;44:1211–7. doi: 10.1016/j.brat.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 38.Bornovalova MA, Daughters SB. How does dialectical behavior therapy facilitate treatment retention among individuals with comorbid borderline personality disorder and substance use disorders? Clin Psychol Rev. 2007;27:923–43. doi: 10.1016/j.cpr.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 39.Aftanas L, Golosheykin S. Impact of regular meditation practice on EEG activity at rest and during evoked negative emotions. Int J Neurosci. 2005;115:893–909. doi: 10.1080/00207450590897969. [DOI] [PubMed] [Google Scholar]
- 40.Afshari B, Omidi A, Sehat M. The effect of dialectical behavior therapy on executive function in patients with a bipolar disorder. Feyz J Kashan Univ Med Sci. 2018;22:404–10. [Google Scholar]
- 41.Cotrena C, Branco LD, Shansis FM, Fonseca RP. Executive function impairments in depression and bipolar disorder: Association with functional impairment and quality of life. J Affect Disord. 2016;190:744–53. doi: 10.1016/j.jad.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 42.Goldstein S, Naglieri JA, editors. Handbook of Executive Functioning. Berlin: Springer Science & Business Media; 2013. [Google Scholar]