“Nothing in this world is more dangerous than sincere ignorance and conscientious stupidity”
Dr. Martin Luther King
1. In search of a villain
After enjoying a 27-hole golf course before retiring, the US President Eisenhower felt some discomfort and interpreted it as indigestion. On the morning of September 24, 1955, he suffered a massive heart attack. His disease increased public awareness of the growing epidemic of disease (CVD) in the 1950s. The factors responsible and the diet involved for this increase was an enigma. People were looking for a scapegoat, and researchers provided them with one soon. Dietary fats, especially saturated fats, were implicated as a causal risk factor for atherosclerotic CVD owing to their role in formation of atheroma.
2. Keys was the key
The nutritional researcher, Ancel Keys, in his famous Seven Countries Study compared health and diet of 12,700 middle-aged men and concluded that populations that ate a large amount of saturated fats in the form of meat and dairy products faced more deaths from heart disease than those predominantly consuming grains, nuts, vegetables and fish.1 The “antisaturated fat” agenda became the agenda of the government and many private agencies in all parts of the world. In 1980, the first dietary guidelines for Americans were released, and saturated fats were the leading villain.2 The United Kingdom followed the same in 1984, and the overall fat consumption was limited to less than 30% of total calories and that of saturated fats to no more than 10% (values that have remained nearly the same over the decades).
3. In search of evidence
Various researchers have examined available evidence on saturated fatty acid (SFA) at different points of time. In an earlier analysis published, data on fats and CVD available with US and UK committees at that time (1980 and 1984) were examined.3 The analysis revealed that the six randomised trials available at that time did not provide sufficient evidence that cutting total fat or saturated fat intake reduces deaths from heart disease. Authors went on to say that “dietary advice not only needs a review but it should not have been introduced”. Later, another meta-analysis of 16 studies with more than 3.4 lakh patients concluded there is no significant evidence of dietary saturated fat being associated with an increased risk of coronary heart disease or CVD.4 In another meta-analysis of 32 observational studies on fatty acids and 27 randomised controlled trials of fatty acid supplementation, consumption of saturated fats was not associated with an increased risk of CVD.5 Authors concluded that the analysis did not support the current guidelines to lower consumption of saturated fats. Another recent study included up to 12 prospective cohort studies for saturated fats and up to 6 prospective cohort studies for trans saturated fatty acids (TFAs).6 After taking into account the methodological limitations, it was also found that saturated fats are not associated with all-cause mortality, CVD, coronary heart disease (CHD), ischaemic stroke or type 2 diabetes. Interestingly, it also showed that TFAs are associated with all-cause mortality, total CHD and CHD mortality, probably because of higher levels of intake of industrial trans fats than ruminant trans fats. A recent cohort study among 35,597 Dutch men and women reported that a higher intake of total SFAs was not associated with higher occurrence of ischaemic heart disease.7 Instead, its occurrence was less when certain types of SFAs were consumed. Thus, all the current evidence concluded that dietary guidelines must carefully consider the health effects of recommendations for alternative macronutrients to replace trans fats and saturated fats.
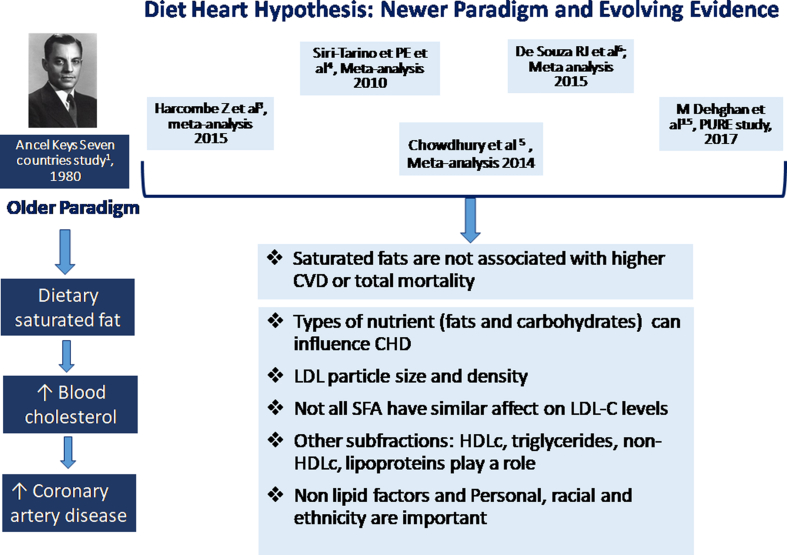
4. Demystifying “diet-heart hypothesis” (Fig. 1)
Fig. 1.
Diet heart hypothesis: newer paradigm and evolving evidence. CVD, cardiovascular disease.
first, researchers now widely accept the presence of range of low density lipoprotein (LDL) particles with different sizes and densities (not measured by standard LDL assays). Blood levels of smaller cholesterol-depleted LDL particles appear to be more strongly correlated with CVD risk than those of larger LDL particles.8 Studies show that SFA intake can raise plasma levels of larger LDL particles to much greater extent than those of smaller LDL particles. Hence, the effect of SFA consumption on serum LDL levels may not reflect its effect on CV risk.
Second, the relationship of dietary SFA and that of individual SFA to CVD risk have been reevaluated now. Not all SFAs have similar effects on low density lipoprotein -C (LDL-C) levels. Butter and dairy fats (containing myristic acid), beef fat (containing palmitic and stearic acid) and cocoa butter (containing largely stearic acid) all affect LDL levels differently.9
Third, studies have shown personal factors such as obesity may alter the effect of dietary fat on LDL cholesterol.10
Finally, there is clear possibility of differential effects of SFAs on racial and ethnic subgroups.10 One of the early surveys of the incidence of acute myocardial infarction and the dietary behaviour in railway populations in India showed that the disease was 7 times more common among South Indians as compared with the Punjabis in the North, although the fat intake by Punjabis was 8–19 times more than that by South Indians and was chiefly of animal origin.11
Thus, the analysis and evidence clearly suggests that understanding of relationship between SFA and CVD is not as it has been projected for decades.
5. Old is gold: really?
A look into traditional sources of saturated fats and oils brings out interesting facts. Ghee, a rich source of saturated fats, has been driven out of many kitchens because of negative understanding and fear of its cholesterol and saturated fat content. However, this view is not supported by scientific evidence. Ghee has 65% saturated fats (SF) and 35% unsaturated fats (predominantly monounsaturated fatty acids (MUFA) which reduces LDL). It has a near-ideal combination of linoleic/alpha-linoleic acid that is crucial for prevention of CHD. It is also rich in vitamins A and D and many minerals. The percentage of lauric acid and myristic acid that are atherogenic is low.12 Such properties are lost in refined oils that are prepared by heating.
The properties of coconut oil that is consumed by the South Indian population also need to be analysed. Most of the studies examining coconut oil and its cholesterol-raising effect have been conducted on hydrogenated coconut oil. Later, another study conducted on coconut oil that was not hydrogenated found that it is a neutral source fat in terms of atherogenicity.13 One of the studies demonstrated potential beneficial effect of virgin coconut oil in lowering lipid levels and LDL oxidation by physiologic oxidant polyphenols present in the oil.14
6. Prospective Urban Rural Epidemiology: new insights—not the final ones
The Prospective Urban Rural Epidemiology (PURE) study looked at dietary intake in 135,335 individuals aged 35–70 years from 18 countries worldwide and examined the balance of nutrients, specifically, carbohydrates and fats.15 On 7.4 years of follow-up, when carbohydrate intake was divided into quintiles, authors found that the highest carbohydrate intake (77.2% energy from carbohydrates) was associated with the greatest increased risk of mortality, when compared with the lowest intake. By contrast, the highest quintile of fat intake (35.3% of daily calories) was associated with a significantly reduced risk of mortality, as compared with the lowest intake. Surprisingly, the benefits of higher fat intake persisted regardless of the type of fat consumed. Although limited by the observational design, the findings further question the guidelines that only focus on limiting intake of total and saturated fats without considering the replacement nutrient.
7. Searching for the true culprit
In another subanalysis of PURE,16 it was found that as the percentage of energy from saturated fats increased, there was only a small increase in LDL cholesterol. This was accompanied by beneficial changes in high density lipoprotein (HDL) cholesterol, the ratio of total to HDL cholesterol and the ratio of apolipoprotein B to apolipoprotein A. It was carbohydrate intake that was most strongly associated with adverse changes in lipid measures.
In addition, TFAs have been shown to increase atherogenic lipoproteins (LDL and very low density lipoprotein (VLDL)) and also reduce the HDL and LDL particle size. Industrially produced TFAs include elaidic acid.17 They are byproducts of partial hydrogenation and that makes them really harmful. They are found in vanaspati, margarines and spreads. A 1% increase in TFA intake reduces HDL by 1% and increases LDL by 1%.
8. Where do we go from here?
-
-
The dietary guidelines advisory committee recommends the upper limit for SFA intake of 10%, reflecting concern that more restriction of SFA may accompany increased carbohydrate consumption.
-
-
It is prudent to distinguish between sources of saturated fats for cardiovascular health. Medium and possible short-chain saturated fats behave different from long-chain ones and have different metabolic and cardiac effects. Thus, not all SFAs in natural fats are atherogenic. Butter, desi ghee, coconut oil (virgin) and palm oil as a part of a healthy diet are not contraindicated when consumed appropriately.
-
-
Studies clearly suggest a relook into the current guidelines regarding SFA recommendation. Simple and direct conclusions drawn on an existing hypothesis can be dangerous and harmful.
-
-
There is unity in diversity: the same holds true for cooking practice in this part of the world. Thus, no one cooking medium is ideal, and the best strategy is to rotate and blend oils with desi ghee and butter.
Conflict of interest
There is no conflict of interest
References
- 1.Keys A. Harvard Univ Press; 1980. Seven Countries: A Multivariate Analysis of Death and Coronary Heart Disease. [Google Scholar]
- 2.Dietary Guidelines for Americans. 1980. https://health.gov/dietaryguidelines/history.htm#6 [Google Scholar]
- 3.Harcombe Z., Baker J.S., Cooper S.M. Evidence from randomised controlled trials did not support the introduction of dietary fat guidelines in 1977 and 1983: a systematic review and meta-analysis. Open Heart. 2015 Jan 29;2(1) doi: 10.1136/openhrt-2014-000196. e000196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.SiriTarino P.W., Sun Q., Hu F.B., Krauss R.M. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. Am J ClinNutr. 2010;91:535–546. doi: 10.3945/ajcn.2009.27725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chowdhury R., Warnakula S., Kunutsor S. Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med. 2014;160:398–406. doi: 10.7326/M13-1788. [DOI] [PubMed] [Google Scholar]
- 6.de Souza R.J., Mente A., Maroleanu A. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease,and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ. 2015;351:h3978. doi: 10.1136/bmj.h3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Praagman J., Beulens J.W., Alssema M. The association between dietary saturated fatty acids and ischemic heart disease depends on the type and source of fatty acid in the European Prospective Investigation into Cancer and Nutrition-Netherlands cohort. Am J ClinNutr. 2016;103:356–365. doi: 10.3945/ajcn.115.122671. [DOI] [PubMed] [Google Scholar]
- 8.Krauss R.M., Blanche P.J., Rawlings R.S., Fernstrom H.S., Williams P.T. Separate effects of reduced carbohydrate intake and weight loss on atherogenicdyslipidemia. Am J ClinNutr. 2006;83:1025–1031. doi: 10.1093/ajcn/83.5.1025. [DOI] [PubMed] [Google Scholar]
- 9.Willett W.C. Dietary fats and coronary heart disease. J Intern Med. 2012;272:13–24. doi: 10.1111/j.1365-2796.2012.02553.x. [DOI] [PubMed] [Google Scholar]
- 10.Hannon B.A., Thompson S.V., An R., Teran-Garcia M. Clinical outcomes of dietary replacement of saturated fatty acids with unsaturated fat sources in adults with overweightand obesity: a systematic review and meta-analysis of randomized control trials. Ann Nutr Metab. 2017;71:107–117. doi: 10.1159/000477216. [DOI] [PubMed] [Google Scholar]
- 11.Malhotra S.L. Geographical aspects of acute myocardial infarction in India with special reference to patterns of diet and eating. Br Heart J. 1967 May;29(3):337–344. doi: 10.1136/hrt.29.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bier D.M. Saturated fats and cardiovascular disease:Interpretations not as simple as they once were. Crit Rev Food SciNutr. 2016;56:1943–1946. doi: 10.1080/10408398.2014.998332. [DOI] [PubMed] [Google Scholar]
- 13.Blackburn G.L., Kater G., Mascioli E.A., Kowalchuk M., Babayan V.K., kBistrian B.R. A reevaluation of coconut oil's effect on serum cholesterol and atherogenesis. J Philipp Med Assoc. 1989;65:144–152. [Google Scholar]
- 14.Nevin K.G., Rajamohan T. Beneficial effects of virgin coconut oil on lipid parameters and in vitro LDL oxidation. ClinBiochem. 2004;37:830–835. doi: 10.1016/j.clinbiochem.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 15.Dehghan M., Mente A., Zhang X., etal Prospective Urban Rural Epidemiology (PURE) study investigators. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017;390:2050–2062. doi: 10.1016/S0140-6736(17)32252-3. [DOI] [PubMed] [Google Scholar]
- 16.Mente A., Dehghan M., Rangarajan S. Association of dietarynutrients with bloodlipids and bloodpressure in 18countries: a cross-sectionalanalysis from the PUREstudy. Lancet Diabetes Endocrinol. 2017 Oct;5(10):774–787. doi: 10.1016/S2213-8587(17)30283-8. [DOI] [PubMed] [Google Scholar]
- 17.WHO, Food and Agriculture Organization of the United Nations . WHO; Geneva: 2002. Diet, Nutrition and the Prevention of Chronic Diseases. Report of a Joint WHO/FAO Expert Consultation. WHO Technical. Report Series, No. 916. [Google Scholar]