Abstract
Objective
This study was conducted to evaluate the prevalence of significant coronary artery disease (CAD) in patients with severe valvular heart disease (VHD) and the association between these two cardiac entities. Our research aims to introduce the theory of a possible causal relationship.
Methods
A retrospective study was conducted on 1308 consecutive patients who underwent surgery for severe VHD in the cardiovascular department of Notre-Dame de Secours University Hospital (NDSUH) between December 2000 and December 2016. According to transthoracic echocardiography, patients were divided into 4 groups: patients with severe aortic stenosis (AS), patients with severe aortic regurgitation (AR), patients with severe mitral stenosis (MS), and patients with severe mitral regurgitation (MR). Preoperative coronary angiographies were reviewed for the presence or the absence of significant CAD (≥50% luminal stenosis). Chi-square test and 2 × 2 tables were used.
Results
Of the 1308 patients with severe VHD, 1002 patients had isolated aortic valve disease, 240 patients had isolated mitral valve disease, and 66 patients had combined aortomitral valve disease. CAD was detected in 27.75% of all patients with severe VHD, in 32% of patients with isolated aortic valve disease, and in 15% of patients with isolated mitral valve disease. Statistical analysis showed a higher prevalence in patients with severe aortic valve stenosis and a significant relationship between CAD and aortic valve disease, mainly severe AS (p < 0.0001).
Conclusion
The prevalence of CAD in patients with VHD is 27.75%, and it correlates significantly with aortic valve disease, in particular with severe AS. Future large studies are needed to evaluate the possible causal relationship.
Keywords: Coronary artery disease, Prevalence, Aortic valve disease, Aortic
Abbreviations: CVD, cardiovascular disease; CAD, coronary artery disease; VHD, valvular heart disease; AS, aortic stenosis; AR, aortic regurgitation; MS, mitral stenosis; MR, mitral regurgitation; NDSUH, Notre-Dame de Secours University Hospital
1. Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide. Coronary artery disease (CAD) and valvular heart disease (VHD) are responsible for major cardiovascular events.1, 2, 3 VHD is less often than heart failure, ischemic heart disease, and hypertension, but it is correlated to heart function deterioration with high fatal outcomes.4 Nonrheumatic degenerative aortic stenosis (AS) is the most frequent type of acquired VHD in Europe and North America.5 Investigators have postulated a conflicting relationship between CAD and VHD even though these two entities share in common the presence of atherosclerotic process and several risk factors such as aging, systemic hypertension, and cigarette smoking.6, 7, 8 VHD is a growing public health problem, so this study was conducted to evaluate the prevalence of angiographically significant CAD in patients with severe VHD and its association with different types of VHD. This study aims to identify the significant correlation between CAD and degenerative aortic valve disease, mainly severe AS. Furthermore, we introduce the idea of probable causal correlation and the corresponding possibility of reducing the increasing incidence of VHD by better management and control of CAD if this causal relationship has been demonstrated by future prospective studies.
2. Material and methods
A retrospective study was conducted on 1308 consecutive patients who underwent surgery for severe VHD in the cardiovascular department of Notre-Dame de Secours University Hospital (NDSUH) between December 2010 and December 2016. According to transthoracic echocardiography, patients were divided into 3 groups: patients with isolated aortic valve disease who were divided into 2 subgroups (AS and aortic regurgitation [AR]), patients with isolated mitral valve disease who were divided into 2 subgroups (mitral stenosis [MS] and mitral regurgitation [MR]), and patients with combined aortomitral valve disease. Severe AS was defined as a mean transaortic gradient > 40 mmHg or a calculated aortic valvular area of less than 1 cm2. Coronary angiography performed before operation was reviewed for the presence and the absence of significant CAD. Angiographically significant CAD was defined by the presence of ≥50% luminal narrowing on any major coronary artery or >50% narrowing of the left main coronary artery. Transthoracic echocardiography and coronary angiography were reviewed by the same reference doctors in the cardiovascular department of NDSUH. This study was approved by the ethics committees of NDSUH, and written consent was obtained from the hospital to allow data collection. Patients with incomplete clinical data, with prior Coronary artery bypass graft (CABG), with rheumatic heart disease, with prior angioplasty, or who aged <40 years were excluded from the study. The data were analyzed systematically using SPSS 20 statistical software. A chi-square test was used in the comparison of qualitative data. A P value < 0.05 was considered statistically significant.
3. Results
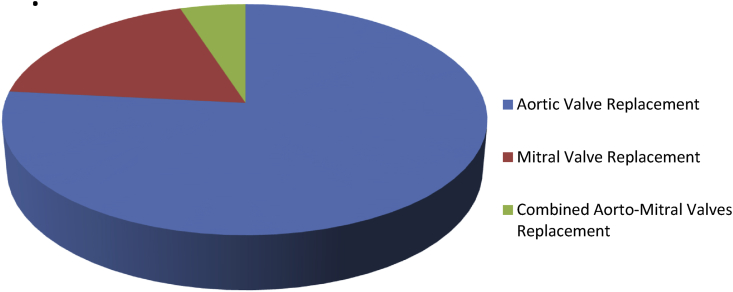
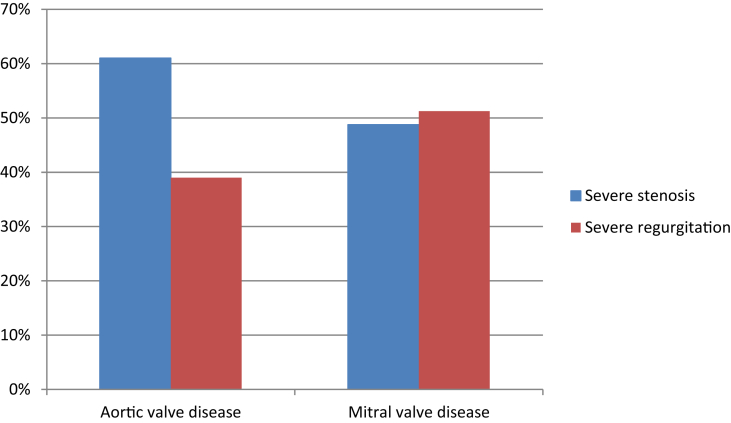
One thousand three hundred eight patients with a mean age of 67 years were studied. Of them, 759 (58%) were males with a mean age of 65 years, and 549 (42%) were females with mean age of 70 years. Of the 1308 patients included in the study, 1002 (76.6%) underwent surgery for aortic valve replacement because of severe aortic stenosis in 612 (61%) cases or severe aortic regurgitation in 390 (39%) cases; and 240 (18.35%) underwent surgery for mitral valve replacement because of severe mitral stenosis in 117 (48.75%) cases or severe mitral regurgitation in 123 (51.25%); and 66 (5%) underwent surgery for combined aortomitral valve replacement (Fig. 1, Fig. 2). Table 1 shows the demographic data of the population.
Fig. 1.
Types of valve replacement surgery.
Fig. 2.
Indications for valvular replacement surgery.
Table 1.
Patient demographic data.
| Variable | N | % |
|---|---|---|
| Male | 759 | 58 |
| Gender | ||
| Female | 549 | 42 |
| Patient with diabetes | 620 | 47.4 |
| Patient with hypertension | 680 | 52 |
| Patient with dyslipidemia | 876 | 67 |
| Smokers | 745 | 56 |
| Mean age | 67 ± 10 years | |
| Isolated aortic valve | 1002 | 76.6 |
| Severe stenosis | 612 | 61 |
| Severe regurgitation | 390 | 39 |
| Isolated mitral valve | 240 | 18.34 |
| Severe stenosis | 117 | 48.75 |
| Severe regurgitation | 123 | 51.25 |
| Mixed aortomitral valve | 66 | 5 |
| Total | 1308 | 100 |
Significant CAD was detected in 360 (27.5%) patients of all groups, in 321 (32%) patients with isolated aortic valve disease, in 36 (15%) patients with isolated mitral valve disease, and in 3 (4.5%) patients with mixed aortomitral valve disease (Table 2). Statistical analysis shows a higher prevalence of CAD in the group of patients with isolated aortic valve disease than in other groups and a significant relationship between significant CAD and severe aortic valve disease, with a p value of 0.0001 and an odds ratio (OR) of 2.46, 95% confidence interval (CI) of (1.69–3.59) (Table 3). Of the 240 patients with isolated mitral valve disease, 117 (48.75%) patients presented severe mitral stenosis, of whom 12 (10.25%) had significant CAD, and 123 (51.25%) patients presented severe mitral regurgitation, of whom 24 (19.51%) had significant CAD. Of the 1002 patients with isolated aortic valve disease, 612 (61%) patients presented severe aortic stenosis, of whom 255 (41.66%) had significant CAD, and 390 (39%) patients presented severe aortic regurgitation, of whom 66 (16.92%) had significant CAD (Table 4).
Table 2.
Prevalence of CAD.
| Valvular heart disease | Significant CAD | Nonsignificant CAD | Total |
|---|---|---|---|
| Isolated aortic valve | 321 (32%) | 681 (68%) | 1002 (76.6%) |
| Isolated mitral valve | 36 (15%) | 204 (85%) | 240 (18.34%) |
| Mixed aortomitral valve | 3 (4.5%) | 63 (95.5%) | 66 (5%) |
| Total | 360 (27.5%) | 948 (72.5%) | 1308 |
CAD, coronary artery disease.
Table 3.
Relationship between CAD and aortic valve disease.
| CAD status | Aortic valve disease | Non–aortic valve disease | Total |
|---|---|---|---|
| Significant CAD | 324 | 36 | 360 |
| Nonsignificant CAD | 744 | 204 | 948 |
| Total | 1068 | 240 | 1308 |
OR: 2.46 (1.69–3.59); p < 0.0001; Se = 30.34%; Sp = 85%; PPV = 90%; NPV = 21.52%.
CAD, coronary artery disease; OR, odds ratio; Se, sensitivity; Sp, specificity; PPV, positive predictive value; NPV, negative predictive value.
Table 4.
Prevalence of CAD in different types of VHD.
| VHD | Prevalence of CAD |
|---|---|
| Severe MR | 19.51% |
| Severe MS | 10.25% |
| Severe AR | 19.62% |
| Severe AS | 41.66% |
CAD, coronary artery disease; MR, mitral regurgitation; MS, mitral stenosis; AR, aortic regurgitation; AS, aortic stenosis.
Statistical analysis shows the highest prevalence of CAD in the group of patients with severe AS and a higher significant relationship between CAD and severe AS with P values less than 0.0001 (Table 5). Concerning the gender, no significant difference was found between males and females, but the association between CAD and severe AS was more common in male gender (54% of patients were male, and 46% were females) and in patients with multiple risk factors (80% had hypertension, 63% had diabetes, 67% had dyslipidemia, and 56% were smokers).
Table 5.
Relationship between CAD and severe aortic stenosis.
| CAD status | Severe aortic stenosis | Nonaortic stenosis | Total |
|---|---|---|---|
| Significant CAD | 258 | 102 | 360 |
| Nonsignificant CAD | 390 | 558 | 948 |
| Total | 648 | 660 | 1308 |
OR: 3.62(2.78–4.70); p < 0.0001; Se = 39.81%; Sp = 84.54%; PPV = 71.67%; NPV = 58.8%.
CAD, coronary artery disease; OR, odds ratio; Se, sensitivity; Sp, specificity; PPV, positive predictive value; NPV, negative predictive value.
4. Discussion
According to literature review, the overall prevalence of CAD in patients undergoing valve replacement has been shown to vary widely from 9% to 41%.9 For example, Marchant et al10 evaluated the prevalence of CAD to be 14% by analyzing the electrocardiogram (ECG) of 100 patients. Shaikh et al11 reviewed medical records of 144 patients and found a prevalence of CAD to be 25%. Manjunath et al9 showed a prevalence of CAD of 8.7% by studying 300 patients referred for cardiac surgery for noncoronary lesions. According to Cazelli et al,12 the prevalence of obstructive CAD in patients with VHD in the preoperative period was 20%.
The importance of our study is that it was conducted on a larger population than the other studies mentioned previously and those found in the literature. The prevalence of CAD, defined by ≥ 50% luminal narrowing, is 27.75% in patients undergoing valvular replacement.
This prevalence is higher in the group of patients with aortic valve disease than in other groups, and this group has the highest prevalence among patients with severe AS. Statistical analysis shows a significant relationship between CAD and VHD with significant p value (p < 0.0001, OR = 2.46, 95% CI [1.69–3.59]) as shown in Table 3. When patients with severe AR were excluded from the group of patients with aortic valve disease and patients with isolated AS were maintained to study the correlation between CAD and AS, statistical analysis shows more significant relationship with P value < 0.0001 and OR of 3.62 and 95% CI of 2.78–4.70 as shown in Table 5.
In contrast to the study by Morrison et al13 who evaluated 239 patients and found the highest prevalence of CAD defined by >50% luminal stenosis to be in patients with isolated mitral valve disease, our study conducted on 1308 patients shows the highest prevalence of CAD to be in patients with severe AS, a finding similar to that reported by Sonmez et al.14 The high prevalence of CAD in patients with AS can be explained by the role of atherosclerotic process played in the etiology of AS and CAD. In addition, the risk factors for the development of a calcified aortic valve are similar to those involved in the development of vascular atherosclerosis. These risk factors include increased low-density lipoprotein cholesterol, diabetes mellitus, smoking history, and hypertension.15, 16, 17
This study finds that CAD is significantly correlated with aortic valve stenosis (p < 0.0001). This study conducted on a large population of patients with VHD helps resolve some of the conflicting data present in the literature as a result of smaller studies. In addition to this significant association proven by the present study, we will be the first by this research to ask if there might be a causal relationship explained by the presence of concomitant risk factors between these two cardiac diseases, the similar pathophysiology of evolution, the fact that myocardial ischemia caused by the repetitive phenomenon of sclerosis, abnormal vasomotricity, stenosis, or narrowing of coronary arteries with age leads to decrease the myocardial compliance, to induce heart failure by altering systolic and diastolic heart function. These abnormalities contribute to heart valve calcification and to promote the progression of cardiac valves damage which may direct to aggravate coronary artery ischemia. This sets up a vicious circle.
Further prospective studies are requested to investigate the probable causal relationship between CAD and AS and the possibility of decreasing the impact of growing incidence of AS by improving the prevention and management strategies of CAD, when a causal correlation has been established.
5. Conclusion
CAD is frequently associated with VHD. This study estimates the prevalence of significant CAD in patients undergoing valvular heart surgery to be 27.5%, and it is highest in patients with AS. This study identifies that CAD correlates significantly with aortic valve disease, in particular with AS. Therefore, future studies are needed to evaluate a possible causal relationship and to prove if strengthening the prevention of CAD in the clinical setting might have a positive significance for reducing or delaying the incidence of VHD, mainly AS.
Conflict of interest
All authors have none to declare.
Funding sources
None.
References
- 1.Matta A., Moussallem N. Evolution of the prevalence of angiographically significant coronary artery disease in Lebanese population referred to cardiac catheterization. Leban Med J. 2017;65(4):205–207. [Google Scholar]
- 2.Sanchis-Gomar Fabian, Perez-Quilis Carme, Leishik Roman, Lucie Abjandro. Epidemiology of coronary heart disease and acute coronary syndrome. Transl Med. 2016 jul;4(13):256. doi: 10.21037/atm.2016.06.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heart disease and stroke statistics 2017 update A report from the American heart association. Circulation. 2017:135. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang S., Si C., Tingting Q. Prevalence and correlates of valvular heart diseases in the elderly population in Hubei, China. Sci Rep. 2016;6:27253. doi: 10.1038/srep27253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bobrowska B., Zasada W., Surdacki A. Predictors of coronary and carotid atherosclerosis in patients with severe degenerative aortic stenosis. Int J Med Sci. 2013;10(10):1361–1366. doi: 10.7150/ijms.6389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Opolski M.P., Staruch A.D., Jakubczyk M. Ct angiography for the detection of coronary artery stenosis in patients referred for cardiac valve surgery: systematic review and meta-analysis. JACC Cardiovasc Imaging. 2016 Sep;9(9):1059–1070. doi: 10.1016/j.jcmg.2015.09.028. [DOI] [PubMed] [Google Scholar]
- 7.El Sabbagh A., Nishimura R. Clinical conundrum of coronary artery disease and aortic valve stenosis. J Am Heart Assoc. 2017 Feb;6(2) doi: 10.1161/JAHA.117.005593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fukumoto R., Kawai M., Minai K. Conflicting relationship between age-dependent disorders, valvular heart disease and coronary artery disease by covariance structural analysis: possible contribution of natriuretic peptide. PLoS One. 2017;12(7) doi: 10.1371/journal.pone.0181206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manjunath C.N., Agarwal A., Bhat P. Coronary artery disease in patients undergoing cardiac surgery for non-coronary lesions in a tertiary care centre. Indian Heart J. 2014 Jan-Feb;66(1):52–56. doi: 10.1016/j.ihj.2013.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marchant E., Pichard A., Casanegra P. Association of coronary artery disease and valvular disease in Chile. Clin Cardiol. 1983;6:352–356. doi: 10.1002/clc.4960060709. [DOI] [PubMed] [Google Scholar]
- 11.Hussain Shaikh Ayaz, Bashir Hanif, Khursheed Hasan. Coronary artery disease in patients undergoing valve replacement at a tertiary care cardiac centre. JPMA. 2011;61:340. [PubMed] [Google Scholar]
- 12.Cazelli J., Camargo G., Kruczan D., Weksler C., Felipe A., Gottlieb I. Prevalence and prediction of obstructive coronary artery disease in patients undergoing primary heart valve surgery. Arq Bras Cardiol. 2017 Oct;109(4):348–356. doi: 10.5935/abc.20170135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morrison G.>W., Thomas R.D., Grimmer S.F., Siherton P.N., Smith D.R. Incidence of coronary artery disease in patients with valvular heart disease. Br Heart J. 1980;44:630–637. doi: 10.1136/hrt.44.6.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sönmez K., Gencbay M., Akçay A. Prevalence and predictors of significant artery disease in patients who undergo heart valve surgery. J Heart Valve Dis. 2002;11(3):431–437. [PubMed] [Google Scholar]
- 15.Rajamannan N.M., Gersh B., Bonow R.O. Calcific aortic stenosis: from bench to the bedside-emerging clinical and cellular concepts. Heart. 2003;89(7):801–805. doi: 10.1136/heart.89.7.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Freeman R.V., Otto C.M. Spectrum of calcific aortic valve disease: pathogenesis, disease progression, and treatment strategies. Circulation. 2005;111(24):3316–3326. doi: 10.1161/CIRCULATIONAHA.104.486738. [DOI] [PubMed] [Google Scholar]
- 17.Fukumoto R., Kawai M., Inoue Y., Yoshimura M. A paradoxical association between valvular heart disease and coronary artery disease: a study by covariance structure analysis. J Card Fail. 2017 Oct;23(10) [Google Scholar]