Abstract
Angiomyolipoma is a benign neoplasm of the kidney, and is the most common renal tumour associated with haemorrhage. Risk of bleeding increases with the size of the angiomyolipoma. We report a case of spontaneous bleeding from an upper polar renal angiomyolipoma mimicking a spontaneous adrenal bleed from a pheochromocytoma.
Keywords: Angiomyolipoma, Embolization, Haemorrhage, Kidney, Nephrectomy
Introduction
Angiomyolipoma is a benign neoplasm of the kidney and in its classic form, consists of thick-walled poorly organized blood vessels, smooth muscle, and varying levels of mature adipose tissue.1 This tumor is predominantly found in females, is rare before puberty and strongly expresses β oestrogen, progesterone and androgen receptors, suggesting a potential hormonal influence.2 As of today most angiomyolipomas are diagnosed incidentally during workup of unrelated complaints and/or symptoms.3 Most angiomyolipomas were previously diagnosed following development of symptoms or massive retroperitoneal haemorrhage. Angiomyolipoma is the most common renal tumour associated with haemorrhage. Pregnancy is known to increase the risk of haemorrhage from angiomyolipoma. We report a case of spontaneous bleeding from an upper polar renal angiomyolipoma mimicking a spontaneous adrenal bleed from a pheochromocytoma.
Case report
A 50 year old male presented to a tertiary referral hospital elsewhere with symptoms of acute abdomen such as nausea, vomiting and severe pain. He was admitted and treated conservatively. He underwent an abdominal ultrasonography followed by computed tomography (CT) of the abdomen. He was referred to our hospital for further management. At our hospital his blood pressure (BP) at presentation was 210/100 mm of Hg. He was a known hypertensive on calcium channel blockers (Amlodipine) since the past few years.
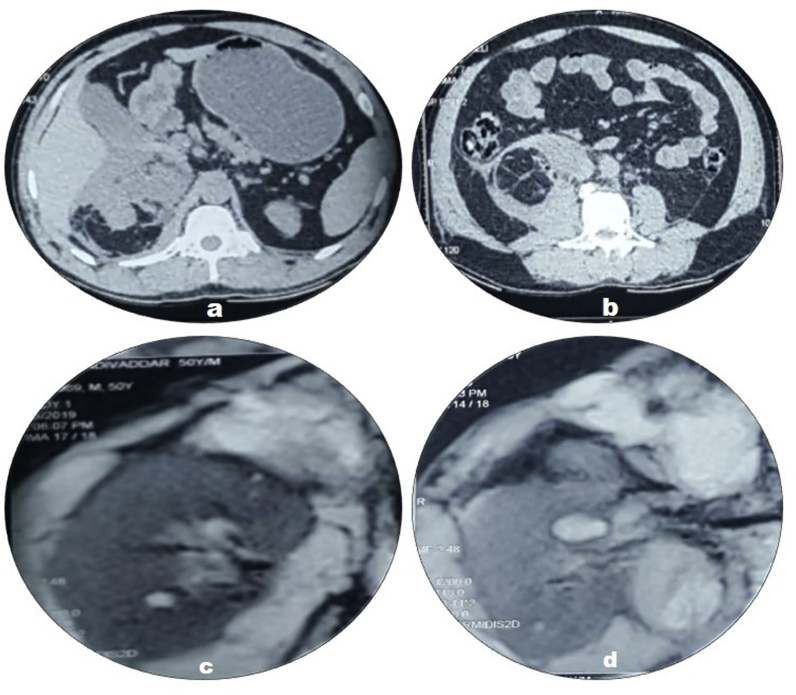
CT done at our hospital showed a peripherally enhancing hypodense area (Hounsfield Unit +50) in the right suprarenal area measuring 4 × 5.5 × 7.5cm (Fig. 1 a & b). The right adrenal gland could not be separately visualized. There was perinephric collection with a maximum thickness of 2.3 cm along the anterior and posterior aspects. This collection caused anteromedial displacement of the inferior vena cava and the 2nd part of the duodenum. A clinical diagnosis of a bleeding right adrenal adenoma was made. The patient was put on complete bed rest, started on antihypertensive therapy which included prazosin, metoprolol and amlodipine. Within three days the patient's BP came down to normal and the pain subsided. Urinary VMA (vanillyl mandelic acid) levels were 17.60 mg/24 hrs and metanephrines were 151.5 μg/24 hrs. Plasma adrenalin was 8.6 pg/ml, and plasma nor-adrenalin was 40.1 pg/ml.
Fig. 1.
a &b: CT shows a peripherally enhancing hypodense area (HU +50) in the right suprarenal area measuring 4 × 5.5 × 7.5cm. c: &d. MRI shows a peripherally enhancing T2 hyper-intense area in the region of right suprarenal gland measuring 3.5 × 5.0 × 6.0 cms.
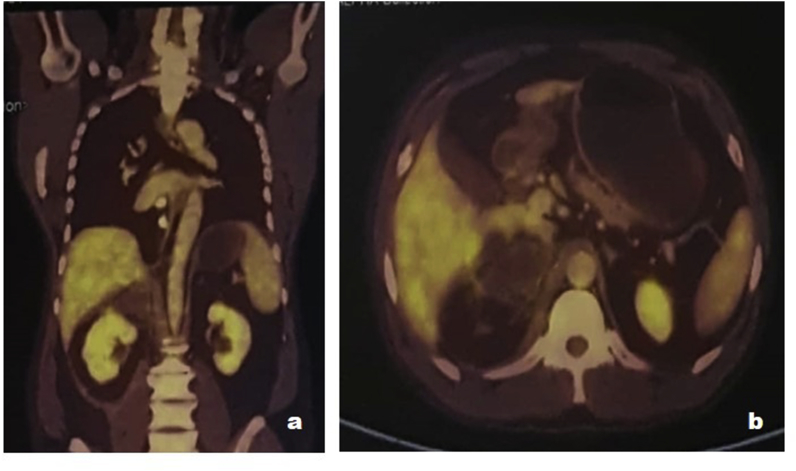
With a suspicion of rupture of pheochromocytoma, MRI (magnetic resonance imaging) was done, which showed a peripherally enhancing T2 hyper-intense area in the region of right suprarenal gland measuring 3.5 × 5.0 × 6.0 cms (Fig. 1 c &d). The right adrenal gland could not be separately visualized. There was perinephric collection both anteriorly as well as posteriorly with a maximum thickness of 2.8 cms. PET-CT (Positron emission tomography -CT) revealed a non FDG avid hypodense collection with minimal peripheral enhancement measuring 3.8 × 4.9 × 5.3 cms (Fig. 2a and b) in the right adrenal area. Right adrenal gland was not separately visualized.
Fig. 2.
a & b. PET-CT revealed a non FDG avid hypodense collection with minimal peripheral enhancement measuring 3.8 × 4.9 × 5.3 cms in the right adrenal area.
A clinical diagnosis of rupture of pheochromocytoma was made and the patient explored surgically using a right flank incision. The right kidney and the right adrenal gland were plastered to the surrounding fat and fascia. The right suprarenal gland was dissected and removed along with the tumour. The excision was not possible in one piece and the gland being friable was removed in three pieces. A good haemostasis was achieved and abdomen closed in layers. Post-operative period was uneventful. Histopathological examination of the resected specimen showed adipose tissue, bundles of spindle cells resembling smooth muscle haphazardly arranged and prominent vessels. Large areas of haemorrhage was also noticed accompanied by giant cell reaction. The pathological diagnosis was Angiomyolipoma (Fig. 3a and b). The blood pressure was stable and well controlled. Urinary VMA level was 12.60 mg/24 hours, six weeks following surgery.
Fig. 3.
a &b. Histopathological examination shows adipose tissue, bundles of spindle cells resembling smooth muscle haphazardly arranged and prominent vessels. Large areas of haemorrhage was also noticed accompanied by giant cell reaction. A diagnosis of Angiomyolipoma.
Discussion
Most small angiomyolipomas are asymptomatic and usually found incidentally on imaging studies performed for unrelated clinical indications.4 The images generally show a highly or mixed echogenic renal tumour without calcification that is difficult to distinguish from renal cell carcinoma on Ultrasonography and thus require further imaging with CT. On CT, angiomyolipomas appear to have well defined margins, with a variable proportion of fat and soft tissue. The minority of patients who are symptomatic classically present with flank pain (53%), a palpable tender mass (47%) and gross haematuria (23%); this is known as 'Lenk's triad'.5
Risk of bleeding increases with the size of the angiomyolipoma. There is a 13% risk of bleeding if the lesion is < 4 cm and a 51% risk if > 4 cm.5 Our case is interesting that the initial CT showed the lesion to be having 50 HU. The 24 hours urinary excretion of VMA was elevated raising a suspicion of Pheochromocytoma although urinary metanephrines, plasma adrenaline and nor-adrenaline were within normal limits. The patient was explored on suspicion of pheochromocytoma and the lesion excised along with the removal of surrounding haematoma. Patients with bleeding angiomyolipoma are an indication for angiography and selective transarterial embolization as a first line management. Nephrectomy, partial or radical, is indicated if there is persistent haemorrhage, suspicion of malignancy, or failed embolization.
Acknowledgement
The authors highly acknowledge the contribution of Mr. Neeraj Dixit during the preparation of manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eucr.2019.101031.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Bissler J.J., Kingswood J.C. Renal angiomyolipomata. Kidney Int. 2004;66:924–934. doi: 10.1111/j.1523-1755.2004.00838.x. [DOI] [PubMed] [Google Scholar]
- 2.Boorjian S.A., Sheinin Y., Crispen P.L. Hormone receptor expression in renal angiomyolipoma: clinicopathologic correlation. Urology. 2008;72:927–932. doi: 10.1016/j.urology.2008.01.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seyam R.M., Bissada N.K., Kattan S.A. Changing trends in presentation, diagnosis and management of renal angiomyolipoma: comparison of sporadic and tuberous sclerosis complex–associated forms. Urology. 2008;72:1077–1082. doi: 10.1016/j.urology.2008.07.049. [DOI] [PubMed] [Google Scholar]
- 4.Wright T., Sooriakumaran P. Renal angiomyolipoma presenting with massive retroperitoneal haemorrhage due to deranged clotting factors: a case report. Cases J. 2008;1:213. doi: 10.1186/1757-1626-1-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simmons J.L., Hussain S.A., Riley P., Wallace D.M. Management of renal angiomyolipoma in patients with tuberous sclerosis complex. Oncol Rep. 2003;10:237–241. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.