Abstract
Renal schwannoma is a very infrequent tumor. It is usually benign and it does not have any specific symptoms or imaging characteristics. Its final diagnosis is usually made after surgery. We present a 66 year-old-man that was referred to our center after the casual finding of a renal mass. With a suspected diagnosis of a renal cell carcinoma, a partial nephrectomy was performed. The histological study revealed the final diagnosis of a benign renal schwannoma.
Keywords: Kidney, Kidney tumor, Renal cancer, Schwannoma
Introduction
The schwannoma is a tumor that arises from the Schwann cells of the nerve sheaths. It is usually sporadic, although sometimes it can be related with some syndromes as neurofibromatosis.1 This tumor is most usually located at the head, neck and limbs,2 and its location at the urinary tract is extremely uncommon, with only a few cases described.
Case report
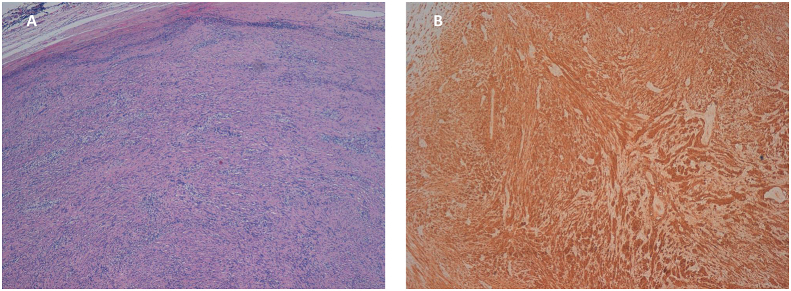
We present a 66-year-old male that was referred to us after a casual finding on a sonography study of a focal solid lesion on the right kidney. A CT was performed and it informed of a 35 mm long solid mass on the superior pole of the right kidney, medially extending over the renal vein, compatible with a renal tumor (see Fig. 1). No abnormal lymph nodes or metastasis were found. A laparoscopic partial nephrectomy was performed of a solid tumor on the superior pole of the right kidney, close to the renal vein, but with no inflitration of it. Histologic findings of the tumor can be seen on Fig. 2. It was informed as a benign neoplastic proliferation made up of spindle cells forming irregular bundles, constituting a solid encapsulated neoplasm, formed by compact areas with other loose areas and, occasionally, areas with fence disposing nucleii. The tumor cells were positive for S-100 protein. All these findings were compatible with a schwannoma. After the exeresis, the patient has remained stable and there have been no relapse signs after a 5-years follow-up.
Fig. 1.

Axial CT showing a renal mass on the superior pole of the right kidney.
Fig. 2.
Histologic findings of the tumor resected. A: H&E staining. Detail of an encapsulated proliferation, surrounded by lymphoid tissue. It is made up of spindle cells forming irregular bundles and, focally, fence disposing nucleii mixed together with hipo or acellular collagen tissue. B: Inmunohistochemical findings. Inmunostainig showed intense positivity for S-100 (schwann cells).
Discussion
Renal schwannoma is a very rare entity, with only 34 cases reported in medical literature.1, 2, 3, 4, 5 Being such an infrequent disease, it is commonly misdiagnosed as a renal carcinoma. It is usually a benign tumor, although some malignancy cases have been described.3
The first case was reported on 1956. After that, 33 more cases have been described, all of them as sporadic tumors. Only three cases has been reported as malignant. Two of them had metastasis at the time of the diagnosis, causing the patients’ death at 3 and 15 months after the finding. The other malignant case was still alive 24 months after the treatment, with no signs of recidiva.3 The rest of the cases were reported as benign schwannomas.
The most frequent symptom reported at the diagnostic was mild abdominal or flank pain, followed by hematuria. Other symptoms described were fever, palpable mass and nausea and vomits. Some other cases were asymptomatic at the time of the diagnosis and were found by chance when taking an image study for other reasons. The age at diagnosis ranged between 18 and 89 years. The median age was 55 years. It appears to be more frequent among women, with 62% of the cases described.1, 2, 3, 4, 5
The image study performed is usually a CT or MRI.1,2 The median size of the tumors was 6 cm (2,7cm4 to 14 cm 3) The lesion was located on the hilium (44% of patients), on the renal parenchyma in (31%), both the hilium and the parenchyma, or the tumor arose from the capsule. The most frequent location on the hilium may result from the fact that the parasympathetic nerve cells enter the kidney through the renal artery.4 In any case, this does not exclude its presentation inside the renal parenchyma.
Although there are no specific findings on imaging,2 some MR characteristics could be more specific to this disease. It has been described to be isointese in T1-weighted images, and hiperintense in T2-weighted images. Using Gadolinium contrast there is an important homogeneous enhance of the solid part of the tumor on T1-weighted images. It seems that the higher or lower intensity seen on T2-weighted images can be related with the different microscopic areas.1
Histologically, these tumors are formed by two different types of cell patterns, which are usually combined representing greater or lesser tumor parts. A hipercellular pattern of spindle cell arranged in palisading, with Verocay bodies, is known as Antoni A. This pattern is combined with Antoni B areas, a less cellular pattern with a bigger component of mixoid tissue. All cases are strongly positive for S100 protein inmunostating.3
Definitive treatment is surgery excision. Given the low frequency of this diagnosis, a parcial or radical nephrectomy is usually performed with no clinical suspicion of a schwannoma. MR could help to suspect the real diagnosis, as it can show more specific findings. However, it is not usually performed as a routine study. For those cases where MR is done due to any other reason, the results cannot distinguish between a benign or a malignant tumor. For this reason, surgery remains the elected treatment.4,5. After intervention, all benign cases described are still alive with no signs of relapse during the follow-up, as in our case.
Conclusions
Renal located schwannoma is an extremely rare tumor. It is usually presented with no specific symptoms or found by chance in an asymptomatic patient. Its diagnose with conventional image studies is difficult. MR may be of help if performed. It is generally mixed up with a renal cell carcinoma, and the diagnosis is done after the histologic results. Most of the times there is no previous suspicion, as both symptomatology and image studies are unspecific. Even when a MR is performed and the suspicion of a schwannoma exists, it is impossible to dismiss its malignancy, although most of the cases are benign. Given that, the final treatment remains the surgical excision.
References
- 1.Tsurusaki M., Mimura F., Yasui N. Neurilemoma of the renal capsule: MR imaging and pathologic correlation. Eur Radiol. 2001;11:1834–1837. doi: 10.1007/s003300000767. [DOI] [PubMed] [Google Scholar]
- 2.Hung S.F., Chung S.D., Lai M.K. Renal schwannoma: case report and literature review. Urology. 2008;72:716.e3–716.e6. doi: 10.1016/j.urology.2007.12.056. [DOI] [PubMed] [Google Scholar]
- 3.Gobbo S., Eble J.N., Huang J. Schwannoma of the kidney. Mod Pathol. 2008;21:779–783. doi: 10.1038/modpathol.2008.52. [DOI] [PubMed] [Google Scholar]
- 4.Yang H.J., Lee M.H., Kim D.S. A case of renal schwannoma. Korean J Urol. 2012;53:875–878. doi: 10.4111/kju.2012.53.12.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelley J., Collins R., Allam C. Robot-assisted laparoscopic renal schwannoma excision. J. Endourol. Case Rep. 2016;2:221–223. doi: 10.1089/cren.2016.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]