Abstract
Background
Emotional and behavioural problems in children are common. Research suggests that parenting has an important role to play in helping children to become well‐adjusted, and that the first few months and years are especially important. Parenting programmes may have a role to play in improving the emotional and behavioural adjustment of infants and toddlers, and this review examined their effectiveness with parents and carers of young children.
Objectives
1. To establish whether group‐based parenting programmes are effective in improving the emotional and behavioural adjustment of young children (maximum mean age of three years and 11 months); and 2. To assess whether parenting programmes are effective in the primary prevention of emotional and behavioural problems.
Search methods
In July 2015 we searched CENTRAL (the Cochrane Library), Ovid MEDLINE, Embase (Ovid), and 10 other databases. We also searched two trial registers and handsearched reference lists of included studies and relevant systematic reviews.
Selection criteria
Two reviewers independently assessed the records retrieved by the search. We included randomised controlled trials (RCTs) and quasi‐RCTs of group‐based parenting programmes that had used at least one standardised instrument to measure emotional and behavioural adjustment in children.
Data collection and analysis
One reviewer extracted data and a second reviewer checked the extracted data. We presented the results for each outcome in each study as standardised mean differences (SMDs) with 95% confidence intervals (CIs). Where appropriate, we combined the results in a meta‐analysis using a random‐effects model. We used the GRADE (Grades of Recommendations, Assessment, Development, and Evaluation) approach to assess the overall quality of the body of evidence for each outcome.
Main results
We identified 22 RCTs and two quasi‐RCTs evaluating the effectiveness of group‐based parenting programmes in improving the emotional and behavioural adjustment of children aged up to three years and 11 months (maximum mean age three years 11 months).
The total number of participants in the studies were 3161 parents and their young children. Eight studies were conducted in the USA, five in the UK, four in Canada, five in Australia, one in Mexico, and one in Peru. All of the included studies were of behavioural, cognitive‐behavioural or videotape modelling parenting programmes.
We judged 50% (or more) of the included studies to be at low risk for selection bias, detection bias (observer‐reported outcomes), attrition bias, selective reporting bias, and other bias. As it is not possible to blind participants and personnel to the type of intervention in these trials, we judged all studies to have high risk of performance bias. Also, there was a high risk of detection bias in the 20 studies that included parent‐reported outcomes.
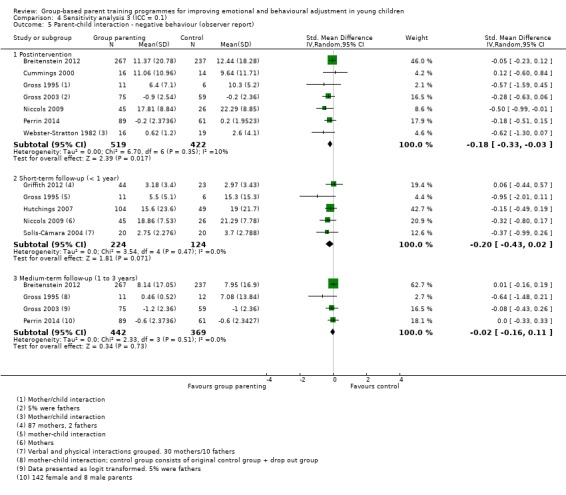
The results provide evidence that group‐based parenting programmes reduce overall emotional and behavioural problems (SMD ‐0.81, 95% CI ‐1.37 to ‐0.25; 5 studies, 280 participants, low quality evidence) based on total parent‐reported data assessed at postintervention. This result was not, however, maintained when two quasi‐RCTs were removed as part of a sensitivity analysis (SMD ‐0.67, 95% CI ‐1.43 to 0.09; 3 studies, 221 participants). The results of data from subscales show evidence of reduced total externalising problems (SMD ‐0.23, 95% CI ‐0.46 to ‐0.01; 8 studies, 989 participants, moderate quality evidence). Single study results show very low quality evidence of reductions in externalising problems hyperactivity‐inattention subscale (SMD ‐1.34; 95% CI ‐2.37 to ‐0.31; 19 participants), low quality evidence of no effect on total internalising problems (SMD 0.34; 95% CI ‐0.12 to 0.81; 73 participants), and very low quality evidence of an increase in social skills (SMD 3.59; 95% CI 2.42 to 4.76; 32 participants), based on parent‐reported data assessed at postintervention. Results for secondary outcomes, which were also measured using subscales, show an impact on parent‐child interaction in terms of reduced negative behaviour (SMD ‐0.22, 95% CI ‐0.39 to ‐0.06; 7 studies, 941 participants, moderate quality evidence), and improved positive behaviour (SMD 0.48, 95% CI 0.17 to 0.79; 4 studies, 173 participants, moderate quality evidence) as rated by independent observers postintervention. No further meta‐analyses were possible. Results of subgroup analyses show no evidence for treatment duration (seven weeks or less versus more than eight weeks) and inconclusive evidence for prevention versus treatment interventions.
Authors' conclusions
The findings of this review, which relate to the broad group of universal and at‐risk (targeted) children and parents, provide tentative support for the use of group‐based parenting programmes to improve the overall emotional and behavioural adjustment of children with a maximum mean age of three years and 11 months, in the short‐term. There is, however, a need for more research regarding the role that these programmes might play in the primary prevention of both emotional and behavioural problems, and their long‐term effectiveness.
Plain language summary
Group‐based parent training programmes for improving emotional and behavioural adjustment in young children
Review question
We wanted to know if group‐based parent training programmes are helpful in improving emotional and behavioural adjustment in young children.
Background
Emotional and behavioural problems are common among infants and toddlers and, for many children, these problems continue into their early school and teenage years as well. Parenting practices play an important role in how emotional and behavioural problems in children develop. Parent training programmes aimed at parents of infants and toddlers might help to prevent such problems before they start, as well as treat them after they are established.
Study characteristics
We searched the scientific literature for all randomised controlled trials (RCTs) and quasi‐RCTs published up to July 2015. RCTs are studies in which people are randomly allocated to treatment groups. Quasi‐RCTs are studies in which people receive treatment based on methods that are not strictly random such as date of birth, or their hospital record number, and the results of quasi‐RCTs are generally considered less trustworthy than those of RCTs.
We found 24 trials (22 RCTs and two quasi‐RCTs) to include in our review. These studies included, in total, information from 3161 parents and their young children. Eight studies had been carried out in the USA, five in the UK, four in Canada, five in Australia, one in Mexico, and one in Peru.
All of the studies looked at behavioural, cognitive‐behavioural or videotape modelling parenting programmes. Behavioural programmes are aimed at helping parents develop methods that will reduce bad behaviour, usually with the use of techniques such as praise or rewards. It also aims to help parents set limits that make sense. Cognitive‐behavioral skills allow parents think about behaviour patterns and focus on solutions. Programmes can use a variety of techniques; for example, videotape modelling programmes enable parents to learn by watching videotaped films of other parents implementing some of the techniques described above.
Key results and quality of the evidence
Some of the studies we found included people chosen specially because they were ‘at risk’ of behavioural problems, while others included parents and children without any specific risks. When we put all of the studies together, overall, we found that group‐based parenting programmes can improve the emotional and behavioural development of young children, although the quality of the evidence was, on the whole, low. Furthermore, our findings were not convincing when we removed two studies that used quasi‐randomised methods.
Our findings also showed evidence of an improvement in externalising problems (these might include negative behaviours in children or young people that are directed towards the external environment such as anger, aggression or conflict with the law). However, the evidence for this, once again, came from studies that we rated as being of only moderate quality, and was only found for some parts of the outcome measure (known as a subscale).
Results from single studies that could not be combined with other studies and that were of poor quality, on the whole, showed no impact on children’s internalising problems (e.g. depression and anxiety). However, there was some improvement on one subscale of a measure that focused on children’s hyperactivity‐inattention and another subscale that focused on social skills.
There was moderate‐quality evidence that group‐based parenting programmes also improve the way in which parents and children interact, as measured by fewer negative behaviours.
Our reasons for rating the quality of the evidence as low or moderate included: inconsistency in the findings from different studies (different studies yielded different results); unclear risk of bias (where it was not possible for us to assess the ways in which the included studies might be biased due to inadequate information); and small numbers of parents in the included studies.
We believe more research is needed to be able to reach a firm conclusion about whether the effects we have found are short term only or whether they continue over time and therefore may be able to prevent future behavioural problems.
Summary of findings
Summary of findings for the main comparison. Group‐based parent training programmes compared to control for improving emotional and behavioural adjustment in young children at postintervention.
| Group‐based parent training programmes for improving emotional and behavioural adjustment in young children at postintervention | |||||
|
Patient or population: young children
Settings: interventions were delivered in the community or at schools/preschools in Australia, Canada, Peru, the UK, and the USA
Intervention: group‐based parent training programmes Control: waiting list, no intervention, or treatment‐as‐usual | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI)** | Number of participants (studies) | Quality of the evidence (GRADE) | Comments |
|
Emotional and behavioural problems (parent report) Scales used: BSI‐II, BSQ, CAPES, CBCL, CBQ postintervention |
The mean child emotional and behavioural problems, as reported by parents, in the intervention groups was 0.81 standard deviations lower (1.37 to 0.25 lower) compared to the control group representing a large difference favouring group‐based parent training programmes | SMD ‐0.81 (‐1.37 to ‐0.25) | 280 (5 studies) | ⊕⊕⊝⊝ Low1,2 | ‐ |
|
Externalising problems (parent report) Scales used: CBCL, ECBI postintervention |
The mean child externalising problems, as reported by parents, in the intervention groups was 0.23 standard deviations lower (0.46 to 0.01 lower) compared to the control group representing a small difference favouring group‐based parent training programmes | SMD ‐0.23 (‐0.46 to ‐0.01) | 989 (8 studies) | ⊕⊕⊕⊝ Moderate2 | ‐ |
|
Externalising problems ‐ hyperactivity‐inattention (parent report) Scales used: HSQ postintervention |
The mean child hyperactivity‐inattention externalising problems, as reported by parents, in the intervention groups was 1.34 standard deviations lower (2.37 to 0.31 lower) compared to the control group representinga moderate difference favouring group‐based parent training programmes | SMD ‐1.34 (‐2.37 to ‐0.31) | 19 (1 study) | ⊕⊝⊝⊝ Very low1,3 | ‐ |
|
Internalising problems (parent report) Scale used: CAPES postintervention |
The mean child internalising problems, as reported by parents, in the intervention groups was 0.34 standard deviations higher (0.12 lower to 0.81 higher) compared to the control group representinglittle or no difference | SMD 0.34 (‐0.12 to 0.81) | 73 (1 study) | ⊕⊕⊝⊝ Low3 | ‐ |
|
Social skills (parent report) Scale used: VABS postintervention |
The mean child social skills, as reported by parents, in the intervention groups was 3.59 standard deviations higher (2.42 to 4.76 higher) compared to the control group representing a large difference favouring group‐based parent training programmes | SMD 3.59 (2.42 to 4.76) | 32 (1 study) | ⊕⊝⊝⊝ Very low1,3 | ‐ |
|
Parent‐child interaction ‐ negative behaviour (observer report) Scales used: DPICS, IBCS postintervention |
The mean child negative behaviour during parent‐child interaction, as reported by independent observers, in the intervention groups was 0.22 standard deviations lower (0.39 to 0.06 lower) compared to the control group representing a small difference favouring group‐based parent training programmes | SMD ‐0.22 (‐0.39 to ‐0.06) | 941 (7 studies) | ⊕⊕⊕⊝ Moderate1 | ‐ |
|
Parent‐child interaction ‐ positive behaviour (observer report) Scales used: Attachment Q‐set, DPICS postintervention |
The mean child positive behaviour during parent‐child interaction, as reported by independent observers, in the intervention groups was 0.48 standard deviations higher (0.17 to 0.79 higher) compared to the control group representing a small difference favouring group‐based parent training programmes | SMD 0.48 (0.17 to 0.79) | 173 (4 studies) | ⊕⊕⊕⊝ Moderate4 | ‐ |
| * The effect sizes are differences in standard deviations. To facilitate interpretation we have used rules of thumb in interpretation of effect size (section 12.6.2 in Higgins 2011), where a standard deviation of 0.2 represents a small difference between groups, 0.5 represents a moderate difference, and 0.8 represents a large difference. ** Several different scales were used to measure outcomes, therefore, the effect sizes were estimated by calculating SMDs. BSI‐II: Bayley Scale of Infant Development II;BSQ: Behaviour Screening Questionnaire;CAPES: Child Adjustment and Parent Efficacy Scale;CBCL: Child Behaviour Checklist;CBQ: Child Behaviour Questionnaire;CI: Confidence interval; DPICS: Dyadic Parent‐Child Interaction Coding System; ECBI: Eyberg Child Behaviour Inventory;GRADE: Grades of Recommendation, Assessment, Development and Evaluation; HSQ: Home Situations Questionnaire;IBCS: Interpersonal Behaviour Construct Scale; SMD: Standard mean difference; VABS: Vineland Adaptive Behaviour Scale. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1 Downgraded one level for risk of bias; inadequate allocation concealment and/or randomisation. Three out of the five included studies did not adequately conceal participant allocation and two studies did not adequately carry out randomisation, and were judged to be at high risk of bias. 2 Downgraded one level for inconsistency; heterogeneity was considerable (I² > 50%). 3 Downgraded two levels for imprecision; only one study with small number of participants was included. 4 Downgraded one level for imprecision; four studies with only 173 participants were included.
Background
Description of the condition
The epidemiology of child emotional and behavioural problems
The prevalence of emotional and behavioural problems in very young children (under three years of age) is high. The Copenhagen Child Cohort Study (6090 infants) found a population prevalence of regulatory problems (including emotional, behavioural, eating, and sleeping disorders) in children aged 1.5 years to be in the region of 18% (Skovgaard 2008; Skovgaard 2010). The rate of behavioural problems among older preschoolers is also high. One study found a six‐month prevalence of behavioural and emotional symptoms of 12.4% in a sample of 1887 German preschool children (Furniss 2006), and a study of a nationally representative sample of Turkish toddlers, aged two to three years, found 11.9% of children in the clinically significant range, and 18.6% of the children in the borderline range, using a measure of child behaviour (Erol 2005). Although some of these disturbances reflect developmental problems from which some children may recover, many such regulatory disturbances are stable over time with as many as 49.9% of infants and toddlers (aged 12 to 40 months) showing a continuity of emotional and behavioural problems one year after initial presentation (Briggs‐Gowan 2006).
Infant regulatory problems have a strong association with delays in motor, language, and cognitive development, and continuing parent‐child relational problems (DeGangi 2000a; DeGangi 2000b). Difficult temperament, non‐compliance, and aggression in infancy and toddlerhood (ages one to three years) are associated with internalising and externalising psychiatric disorders at five years of age (Keenan 1998), and emotional and behavioural problems in young children also predict an increased risk of a range of poor long‐term outcomes, including depression, alcohol and drug misuse, and psychosocial problems such as poor work and marital outcomes, delinquency, and criminal behaviour (Champion 1995; Farrington 1991; Farrington 1994; Kazdin 1990; Loeber 1997; Moffit 1996; Offord 1994; Robins 1990; Robins 1991; Rutter 1996). For example, the Dunedin study showed that antisocial behaviour at age 13 years was predicted by externalising behaviour at age three, and behavioural problems at age five (Robins 1991). A 22‐year, follow‐up study showed that peer‐rated aggression at age eight predicted the number of convictions by age 30, as well as the seriousness of the crimes (Eron 1990).
Description of the intervention
Parenting programmes
Parenting programmes are focused, short‐term interventions aimed at helping parents improve their relationship with their child, and preventing or treating a range of emotional and behavioural problems. The use of parents as modifiers of their children's behaviour began in the 1960s when it was shown that by using behavioural modification techniques, parents could successfully decrease tantrums, self destructive behaviours, verbal aggression, excessive crying, thumbsucking, soiling, school phobia, speech dysfunction, seizures, oppositional behaviour, and antisocial and immature behaviour (Johnson 1973; Rose 1974). This early work was conducted with individual families, and the use of groups did not begin until the 1970s. The expansion of group‐based parenting programmes has taken place in a number of countries over the past few decades (Pugh 1994).
Parenting programmes are underpinned by a range of theoretical approaches (including: Behavioural, Family Systems, Adlerian, Attachment and Psychodynamic), and can involve the use of a range of techniques in their delivery, including discussion, role play, watching video vignettes and homework. They are typically offered to parents over the course of eight to 12 weeks, for about one to two hours each week. They can be delivered on a one‐to‐one basis or to groups of parents, and are provided in a number of settings ranging from hospital/social work clinics to community‐based settings such as general practice (GP) surgeries, schools, and churches. They typically involve the use of a manualised and standardised programme or curriculum, and are aimed at increasing the knowledge, skills, and understanding of parents.
Parenting programmes are now being offered in a variety of settings, and guidance from the National Institute for Health and Clinical Excellence (NICE) supports their use with children aged three to 10 years with conduct/behavioural problems (Dretzke 2009; Furlong 2012; NICE 2006). Other reviews have demonstrated their effectiveness in improving maternal psychosocial health in the short‐term, including reducing anxiety and depression, and improving self esteem (Barlow 2014), and meta‐ethnographic evidence points to a range of benefits of taking part in a group with other parents (Kane 2007). It has also been suggested that group‐based parenting programmes may be a more effective method of supporting parents of children with sleep problems than individually‐tailored behavioural programmes (Szyndler 1992).
How the intervention might work
Parenting and child mental health
Recent research has suggested that infant regulatory problems can best be understood in a relational context, and that disturbances to the parent‐child relationship and parental psychosocial adversity are significant risk factors for infant emotional, behavioural, eating and sleeping disorders (Skovgaard 2008; Skovgaard 2010). There is a significant body of research underpinned by social learning theory, which addresses the relationship between early parenting practices and child emotional and behavioural problems. This shows that positive, proactive parenting (involving praise, encouragement, and affection) is strongly associated with high child self esteem and social and academic competence, and is protective against later disruptive behaviour and substance misuse (Kumpfer 2004). Parenting practices characterised by harsh and inconsistent discipline, little positive parental involvement with the child, and poor monitoring and supervision, however, have been shown to be associated with an increased risk of a range of poor outcomes, including delinquency and substance abuse (Patterson 1993), as a result of the coercive cycles of interaction that are established in early childhood (Patterson 1989).
While early research shows such parenting and family interaction variables to explain up to 30% to 40% of child antisocial behaviour (Patterson 1989), more recent research has suggested that many of the family correlates of aggressive child behaviour are present in infancy before the onset of such coercive cycles (Lyons‐Ruth 1996), and research has found that both insecure and disorganised infant attachment behaviours are precursors to a range of child behavioural problems, particularly for children living in high risk contexts such as poverty (Egeland 1979). Egeland 1993b, for example, found that intrusive parent‐infant interactions were associated with avoidant attachment at 12 months and with more negative, non‐compliant and hyperactive behaviour at 42 months. Infant attachment problems have been found to be associated with a range of later problems, including externalising disorders (Fearon 2010). Furthermore, this body of research has identified a range of parental behaviours as being important in terms of infant attachment security, including parental sensitivity (De Wolff 1997); the specific nature or quality of the attunement or contingency between parent and infant (Beebe 2010); the parent's capacity for what has been termed ‘maternal mind‐mindedness' (Meins 2001) or 'reflective function' (Slade 2001); and a range of atypical or anomalous parenting behaviours (Madigan 2006).
Why it is important to do this review
The above body of research suggests that early parenting is key to child emotional and behavioural functioning, and it has been suggested that the promotion of the mental health of infants and toddlers is key to the prevention of mental disorders throughout the lifespan (Fonagy 1998). In addition, there is consensus that early interventions designed to support parenting during the first two years of life are key to reducing later social and health inequalities (Marmot 2010). This reflects increased understanding about the way in which social adversity during this period is biologically embedded as a result of early parent‐child interactions (Shonkoff 2009). To date, however, there has been no attempt to synthesise the evidence concerning the effectiveness of parenting programmes that are directed at infants and toddlers, and that have a different focus from interventions that are directed at older children (those between three and eight years of age). In addition, although most current evidence from controlled trials address the use of parenting programmes as part of secondary, high risk approaches to prevention, it has been argued on theoretical grounds that they would be more effective if delivered as part of a population‐based approach (Barlow 2003a; Sanders 2008), in which they are offered to all parents with the aim of preventing problems before they occur and promoting child health. Although at least one parenting programme has been designed and delivered as part of a population‐based public health approach e.g. Triple P (Prinz 2009; Sanders 2002; Sanders 2008), parenting programmes have been typically used to date in a secondary/tertiary preventive role (i.e. the treatment of early mental health problems). It may be, however, that they have an important role to play in the primary prevention of mental health problems and the promotion of mental health. This review aims to address these issues.
Objectives
To establish whether group‐based parenting programmes are effective in improving the emotional and behavioural adjustment of young children (maximum mean age of three years and 11 months); and
To assess whether parenting programmes are effective in the primary prevention of emotional and behavioural problems.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and quasi‐RCTs.
Studies in which participants were randomly allocated to an experimental or a control group, the latter being a waiting list, no intervention (including treatment‐as‐usual or normal service provision), or a placebo control group.
We included quasi‐RCTs, defined as trials where allocation was conducted on the basis of a pseudo‐random sequence such as odd/even hospital number, date of birth, or alternation (Higgins 2011). We also included cluster‐RCTs and cross‐over trials (see Unit of analysis issues), which we labelled as such.
We did not include studies that compared two different therapeutic modality groups without a control group.
Types of participants
Studies were eligible for inclusion in the review if they targeted parents (or any adult defined as a primary carer, including mothers, fathers, foster parents, grandparents, or relatives) of children from birth to three years of age (including studies in which the maximum mean age of the children was three years and 11 months), with or without emotional or behavioural problems (i.e. the programme is aimed either at treating existing emotional or behavioural problems, or preventing the development of such problems). We included studies involving parents of a child older than three years of age providing that the maximum mean age of all the children in that study was three years and 11 months. This reflects the fact that whilst this review focuses on interventions that are developmentally appropriate for children from birth to three years of age, a number of studies evaluating relevant interventions may well have included children who are slightly older than this (i.e. up to five years) in addition to younger children.
We excluded studies which targeted parents of children over three years of age or in which the mean age of the sample was greater than three years and 11 months. We also excluded studies that focused on specific conditions other than emotional and behavioural problems (e.g. physical disabilities, autism, etc.), and studies that included parents of children born pre‐term or with complications.
Types of interventions
Studies evaluating the effectiveness of any group‐based parenting programme were eligible for inclusion irrespective of the theoretical basis underpinning the programme (i.e. behavioural, cognitive‐behavioural, humanistic, etc. were all eligible for inclusion). We excluded studies evaluating group‐based programmes that also included individual one‐to‐one sessions. Although we have not included studies that are provided on an individual basis, we have included group‐based programmes that provide one or two brief telephone sessions as an adjunct to the programme with the aim of reinforcing what has been learned or to trouble shoot, or both. We have excluded group‐based programmes that provide telephone sessions on a one‐to‐one basis to deliver aspects of the programme. In addition, we excluded programmes that began in the prenatal period.
Types of outcome measures
Previous versions of this review included one broad outcome: child emotional and behavioural adjustment. For this update, we have kept this as the primary outcome, but we have also included measures of externalising and internalising problems, where these are reported as subscales.
Primary outcomes
Total emotional and behavioural problems, as measured using a standardised instrument, such as the Behaviour Screening Questionnaire (BSQ, Richman 1971) or the Child Behaviour Questionnaire (CBQ, Rutter 1970).
Externalising problems, as measured using subscales from standardised instruments, such as the intensity subscale of the Eyberg Child Behaviour Inventory (ECBI, Eyberg 1978), or the externalising subscale of the Child Behaviour Checklist (CBCL, Achenbach 2000). Specific externalising problems, such as hyperactivity and inattention, as measured using subscales from standardised instruments, such as the inattentive subscale of the ECBI (Eyberg 1978), or the hyperactivity subscale of the Strengths and Difficulties Questionnaire (SDQ, Goodman 1997).
Internalising problems, as measured using a standardised instrument such as the Behavioural Inhibition Questionnaire (BIQ, Bishop 2003), or the internalising subscale of the CBCL (Achenbach 2000).
Secondary outcomes
Social skills, as measured using subscales from a standardised instrument, such as the Social Behaviour subscale from the ECBI (Eyberg 1978).
Parent‐child interaction, as measured using subscales from standardised instruments, such as the Negative and Positive Behaviour subscales of the Dyadic Parent‐Child Interaction Coding System (DPICS, Robinson 1981).
Timing of outcome assessments
We collected outcome measures for different time points and categorised them as:
post‐treatment;
short‐term follow‐up (less than one year);
medium‐term follow‐up (one to three years); and
long‐term follow‐up (more than three years).
Our primary time point is postintervention.
Outcomes of the 'Summary of findings' table
We used the Grades of Recommendations, Assessment, Development, and Evaluation (GRADE) approach to summarise and interpret findings (Schünemann 2008), and used GRADEprofiler Guideline Development Tool to import data from Review Manager 5 to create 'Summary of findings' tables (GRADEpro GDT 2015; RevMan 2014). These tables provide outcome‐specific information concerning within‐study risk of bias (methodological quality), heterogeneity, directness of evidence, precision of effect estimates, risk of publication bias, and the sum of available data on all outcomes rated as important to patient care and decision making. The GRADE approach specifies four levels of quality.
High quality: further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: we are very uncertain about the estimate.
Different scales were used in the included studies to measure the same outcomes, and we therefore combined them in the analyses using standardised mean differences (SMDs), see Data synthesis. To facilitate interpretation of SMDs in the 'Summary of findings' table, we used rules of thumb, where a standard deviation (SD) of 0.2 represents a small difference between groups, 0.5 represents a moderate difference, and 0.8 represents a large difference (section 12.6.2 in Higgins 2011). We included the following outcomes in the 'Summary of findings' table.
Emotional and behavioural problems.
Externalising problems, including hyperactivity and inattention.
Internalising problems.
Social skills.
Parent‐child interaction: negative and positive behaviour.
We included outcomes measured at the primary time point, post‐intervention, in the 'Summary of findings' table.
Search methods for identification of studies
Electronic searches
We originally ran searches for the first version of this review in 2000, and updated them in 2007/8 (Appendix 1). For this update, we initially ran searches in June 2014 using the original strategies (Appendix 2). We then revised the searches in order to increase their sensitivity, and added a filter to limit the records to RCTs (see Differences between protocol and review). In July 2014, we ran the revised strategies in Appendix 3 for all available years in each database. We did not apply any language or date restrictions. We ran the revised searches most recently in July 2015, to find any new studies published since 2014 (see Appendix 4 for a record of the searches for this update).
We searched the following databases.
Cochrane Central Register of Controlled Trials (CENTRAL; 2015, Issue 6; part of the Cochrane Library), and which includes the Cochrane Developmental, Psychosocial and Learning Problems Group Specialised Register.
Ovid MEDLINE (1946 to July week 3 2015).
Embase (1980 to 2015 week 30; Ovid).
CINAHL (1938 to 30 July 2015; EBSCOhost).
PsycINFO (1967 to 2015 July week 3; Ovid).
ERIC (1966 to 30 July 2015; EBSCOhost).
Sociological Abstracts (1952 to 23 July 2015; Proquest).
Social Sciences Citation Index (SSCI; 1970 to 29 July 2015; Web of Science).
Conference Proceedings Citation Index ‐ Social Science & Humanities (CPCI‐SS&H; 1990 to 29 July 2015; Web of Science).
Cochrane Database of Systematic Reviews (CDSR; 2015, Issue 7; part of the Cochrane Library).
Database of Abstracts of Reviews of Effects (DARE; 2015, Issue 2; part of the Cochrane Library).
BIOSIS Citation Index (1926 to 2 October 2015; Web of Science).
Dissertation Abstracts (all available years; Proquest), searched 2 October 2015.
World Health Oganisation International Clinical Trials Registry Platform (WHO ICTRP; all available years), searched 31 July 2015.
ClinicalTrials.gov (all available years), searched 31 July 2015.
Searching other resources
We searched reference lists of included studies and relevant systematic reviews for additional eligible studies.
Data collection and analysis
Selection of studies
We reviewed titles and abstracts of studies identified through searches of electronic databases to determine whether they met the inclusion criteria. For this updated review, two authors independently assessed titles and abstracts. They then obtained full copies of reports that appeared to meet the inclusion criteria, and again, independently assessed the reports for eligibility for inclusion in the review. Any uncertainties were resolved by JB. We did not exclude non‐English language publications. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram (Moher 2009), and 'Characteristics of excluded studies' table.
Data extraction and management
For this updated review, the Enhanced Reviews Team (Rosie Asher and Nicola Maayan) extracted data and this was cross‐checked by one of the review authors (HB) using web‐based data extraction forms, and entered into RevMan 2014. Any disagreements were resolved by discussion with JB. Where data were not available in the published trial reports, we contacted trial authors to supply missing information. Nine trial authors provided missing data (Hutchings 2007; Morawska 2011; Niccols 2008; Niccols 2009; Nicholson 2002; Perrin 2014; Sutton 1992; Tiedemann 1992; Webster‐Stratton 1982), and details are provided in the Characteristics of included studies tables.
We extracted the following data.
Study methods
Study design (e.g. RCT or quasi‐RCT).
Unit of allocation.
Follow‐up duration.
Participants
Inclusion/exclusion criteria.
Number (total/per group).
Age distribution of participants and children.
Gender.
Ethnicity.
Country.
Setting (number of sites, recruitment, intervention delivery).
Interventions
Intervention conditions.
Duration.
Type of prevention (primary/secondary/tertiary).
Details of intervention.
Outcomes
Prospectively stated.
Incomplete.
We have reported the scales and subscales used by each study in the Characteristics of included studies tables.
Data
Scale.
Timepoint.
Person reporting.
Methods of analysis (intention‐to‐treat/per‐protocol analysis).
Comparability of groups at baseline (yes/no).
Assessment of risk of bias in included studies
For this updated version of the review, two review authors independently assessed the risk of bias within each included study as 'low risk', 'high risk', and 'unclear risk' (unreported or uncertain risk of bias) across six domains (Higgins 2011); disagreements were resolved through discussion with JB (for more information please see the 'Characteristics of included studies' tables). Where information was not available in the published trial reports to make a judgement about the risk of bias, we contacted trial authors and asked them to supply missing information. Nine trial authors replied to our requests, see the Characteristics of included studies tables for full details.
We assessed risk of bias across the following six domains.
Sequence generation: we assessed the method used to generate the allocation sequence to determine if it produced comparable groups.
Allocation concealment: we assessed the method used to conceal allocation sequence to see whether it was adequate in terms of whether the intervention schedules could have been foreseen in advance of, or during, recruitment.
Blinding: we assessed whether any steps were taken to blind participants, personnel, and outcome assessors to which intervention a given participant might have received. This domain was split into (a) blinding of participants and personnel, (b) blinding of outcome assessors for independent observer outcomes, and (c) blinding of outcome assessors for parent‐rated outcomes.
Incomplete outcome data: we assessed whether incomplete data were dealt with adequately by the reviewers, and how data on attrition and exclusions were reported, compared with the total randomised.
Selective outcome reporting: we assessed whether any attempt had been made to reduce the possibility of selective outcome reporting by investigators.
Other sources of bias: we assessed whether the study was apparently free of other problems that could put it at a high risk of bias, such as baseline differences or insufficient consideration of clustering effects in cluster‐RCTs.
Measures of treatment effect
We analysed data from continuous outcomes that were measured with similar, but not identical instruments, using SMDs with 95% CIs. All analyses included all participants in the treatment groups to which they were allocated, whenever possible.
Unit of analysis issues
Cluster‐randomised trials
Including cluster‐randomised trials in a meta‐analysis with individually‐randomised trials can produce over‐precise results due to 'unit of analysis errors', and underestimations of effect due to 'herd effects' (Section 16.3.2 in Higgins 2011). We combined data from cluster‐randomised trials with individually‐randomised trials in the same meta‐analysis. If clustering was accounted for in a cluster trial, we used the study‐reported summary statistics in our meta‐analysis. Where clustering was not accounted for, we used the intracluster correlation coefficient (ICC) to calculate the inflated standard error (Higgins 2011). We replaced the originally‐reported standard error by the inflated standard error in our meta‐analysis. If the study did not report the ICC, we used the ICC from similar studies. We then conducted a sensitivity analysis assuming a set of different values for the ICC (see Sensitivity analysis).
Cross‐over trials
Two of the included studies were cross‐over trials (Cummings 2000; Webster‐Stratton 1982). A major problem with cross‐over trials is the carry‐over effect, which occurs if an effect of the treatment in the first phase is carried over to the second phase (Elbourne 2002). Therefore, we only used data from the first phase of these trials.
Dealing with missing data
We assessed missing data and dropouts/attrition for each included study and reported it in the 'Risk of bias' tables (Characteristics of included studies).
Assessment of heterogeneity
We assessed clinical and methodological heterogeneity by comparing the distribution of important participant factors between trials (e.g. age), and trial factors (randomisation concealment, blinding of outcome assessment, losses to follow‐up, treatment type, co‐interventions). We assessed statistical heterogeneity by examining the I² statistic (Higgins 2002), a quantity which describes approximately the proportion of variation in point estimates that is due to heterogeneity rather than sampling error. In addition, we used the Chi² test of heterogeneity to determine the strength of evidence for heterogeneity and Tau² to assess between‐study variability.
Assessment of reporting biases
Tests for publication bias can be conducted by inspecting funnel plots for asymmetry. However, these tests should only be carried out when there are at least 10 studies included in the meta‐analysis (see section 10.4.3.1 in Higgins 2011). Asymmetry can be due to publication bias, but can also be due to a real relationship between trial size and effect size. We did not include any meta‐analyses in this review with 10 or more studies, consequently we did not draw funnel plots nor carry out tests for publication bias.
Data synthesis
The studies included in this review used a range of scales to measure similar outcomes (e.g. the outcome of 'emotional and behavioural problems' was measured using scales such as the BSQ (Richman 1971) and the CBQ (Rutter 1970). Where studies reported both total and subscale results for the same scale, we did not include the total score because including both would introduce linear dependencies among the measures (Shadish 1992), and subscales provide more specific information than total scores (Shadish 1992).
We standardised the results from these different measures by dividing the mean difference in postintervention scores for the intervention and treatment group by the pooled SD, to obtain a SMD. Where appropriate, we combined the results in a meta‐analysis using a random‐effects model. We based our decision about whether to combine data in this way by the level of heterogeneity present in the population, intervention, and outcomes used in the primary studies. As expected, we did not find any dichotomous outcomes.
Subgroup analysis and investigation of heterogeneity
We conducted planned subgroup analyses for the primary outcome: to explore the effectiveness of longer (i.e. eight weeks or more) and shorter programmes, and to examine primary preventive programmes and secondary/tertiary programmes.
Sensitivity analysis
We conducted sensitivity analyses to test if the findings of the meta‐analyses were robust by examining the effect of including quasi‐RCTs and cluster‐RCTs (see Unit of analysis issues and Differences between protocol and review).
Results
Description of studies
Results of the search
We revised our original search strategies for this update and conducted a new search, which identified 18,431 records. After de‐duplication, we screened 12,052 records for inclusion in this update, see Figure 1.
1.
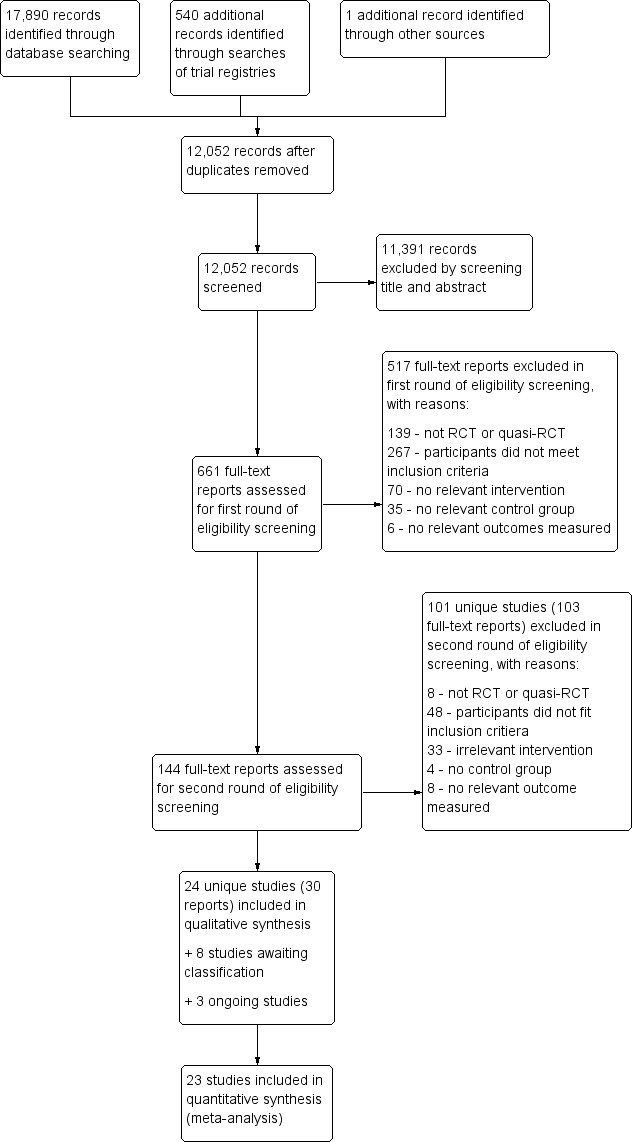
Study flow diagram.
Two reviewers independently examined the titles and abstracts. The majority of articles reviewed were written in English. All articles written in languages other than English had an abstract written in English, and we excluded most of these studies on the basis of information contained in the abstracts. We included two studies published in Spanish (Oré 2011; Solís‐Cámara 2004). Due to pending translation, one study published in Persian (Farzadfard 2008), and one study published in Chinese (Wang 2000), are currently awaiting classification (Characteristics of studies awaiting classification). We identified and obtained the full‐texts of 661 potentially eligible reports (i.e. by matching details in the abstract against the inclusion criteria), and subsequently excluded 620 reports (see Excluded studies). We identified 24 included studies (Bradley 2003; Breitenstein 2012; Cummings 2000; Dittman 2015; Griffith 2012; Gross 1995; Gross 2003; Hiscock 2008; Hutchings 2007; Kennedy 2009; Little 2012; Morawska 2011; Morawska 2014; Niccols 2008; Niccols 2009; Nicholson 1998; Nicholson 2002; Oré 2011; Perrin 2014; Simkiss 2013; Solís‐Cámara 2004; Sutton 1992; Tiedemann 1992; Webster‐Stratton 1982); eight studies awaiting classification (Farzadfard 2008; Herbert 2007; Sandy 1983; Schlarb 2012; Wang 2000; Zhu 2014;ISRCTN39288126; ISRCTN88988596), and three ongoing studies (ISRCTN16513449; ISRCTN11079129; ISRCTN17488830).
Included studies
An examination of the full‐texts of the 661 potentially relevant reports resulted in 24 studies (30 reports) being included. We included eight of these studies in the previous version of this review (Barlow 2010). We added 16 new studies as included studies in this review. In addition, we identified eight studies as awaiting classification (see Characteristics of studies awaiting classification), and three ongoing studies (see Ongoing studies).
All 24 included studies (22 RCTs and two quasi‐RCTs) in this review provided data on the effectiveness of group‐based parenting programmes in improving emotional and behavioural adjustment in young children.
The studies were published over a 35‐year period, the earliest being Webster‐Stratton 1982 and the most recent, Dittman 2015. There were some important differences between the studies, and we have summarised these alongside the main study characteristics below. An overview is provided in Table 2 and further details are in the Characteristics of included studies tables.
1. Overview of key study characteristics.
|
Study ID Country |
Unit of randomisation | Who received the intervention? | How long was the intervention? | How long was the follow‐up? | What age was the child? | Did the child already have behavioural problems? | What was the group parent training intervention? | What was the control? | Which instruments were used to measure the effect? Completed by? | Was the therapist trained? |
|
Bradley 2003 Canada |
Individual caregiver (parallel) | Parents (N = 198) |
3 (2 hours) sessions in 3 weeks + 1 booster | 3 months | 3 to 4 years | Difficult behaviour | 1‐2‐3 Magic | Waiting list | PBQ (hyper): parents report; PCQ: parents | Facilitators trained in problem solving |
|
Breitenstein 2012 USA |
Day care centres (cluster) | Parent or caregiver (N = 253) |
11 sessions in 11 weeks (+ 1 booster) | 1 year | 2 to 4 years | No (low SES) | Chicago Parenting Program | Waiting list | C‐TRF: teachers; ECBI: parents; DPICS‐R: observers | Facilitators trained and supervised |
|
Cummings 2000 USA |
Individual parents (cross‐over) | Parents and other caregivers (N = 37) |
6 (1.5 hours) sessions in 3 weeks | 4 weeks | 2 to 3 years | Negative behaviour | Not specified | Waiting list | DPICS: clinical staff | Researcher |
|
Dittman 2015 Australia/New Zealand |
Individual caregiver (parallel) | Parents (N = 45) |
1 (2 hours) session | 4 weeks | 3 to 5 years | Disobedient or non‐compliant behaviour | Dealing with Disobedience | Waiting list | ECBI (intensity): parents | Registered psychologist |
|
Griffith 2012 UK |
Parent/child dyads (parallel, 2:1) | Parents (Flying Start initiative) (N = 89) |
12 (2.5 hours) sessions in 12 weeks | 6 months | 12 to 36 months | No (low SES) | Incredible Years Toddler Parenting Program (IYTPP) | Waiting list | SGS‐II: healthy visitors; DPICS: researcher | Trained group leaders with mentor’s supervision |
|
Gross 1995 USA |
Individual family (parallel) | Parents (N = 23) |
10 (2 hours) sessions in 10 weeks | 1 year | 24 to 36 months | Difficult behaviour | Parenting Training Intervention | No intervention | ECBI (intensity and problem scales); DPICS: observer | Master degree in psychiatric nursing and experience |
|
Gross 2003 USA |
Day care centres (cluster) | Parents and teachers (N = 264) |
12 (2 hours) sessions in 12 weeks | 1 year | 2 to 3 years | No (low SES) | Incredible Years BASIC Program | Waiting list | ECBI: parents; KPC: teachers; DPICS‐R: observers | Trained group leaders |
|
Hiscock 2008 Australia |
Primary care health centres (cluster) | Mothers (N = 733) |
1 individual session + 2 (2 hours) sessions in 7 months | 3 years | 8 months | No | Toddlers Without Tears | Usual primary care | CBCL: mother | Nurses trained by a paediatrician and child psychologist |
|
Hutchings 2007 UK |
Parent/child dyads (parallel, 2:1) | Caregiver (N = 153) |
12 (2 to 2.5 hours) sessions in 12 weeks | 6 months | 36 to 59 months | At risk of conduct disorders (low SES) | Incredible Years BASIC Program | Waiting list | ECBI; SDQ; CAPTRS; KSCRS: parents | Trained leaders with supervision |
|
Kennedy 2009 Australia |
Individual children (parallel) | Parents with DSM anxiety disorder (N = 71) |
8 sessions in 8 weeks (+ 1 follow‐up call) | 6 months | 36 to 58 months | Behaviour inhibition | Parenting Intervention Program | Waiting list | BIQ; PAS‐R; CALIS‐PV: mothers and fathers; CBIS; GBIR; SSR | Experienced researchers |
|
Little 2012 UK |
Individual family (parallel, 2:1) | Parents (≈ 50% of low SES) (N = 161) |
12 sessions in 12 weeks | 6 months | 3 to 4 years | At risk of social, emotional or behaviour disorders | Incredible Years BASIC Program | Waiting list | SDQ; ECBI: parents | Trained centre staff, educational psychologists and practitioners |
|
Morawska 2011 Australia |
Individual parent (Parallel) | Mothers (1 father only) (N = 67) |
1 (2 hours) session in 1 week + 2 follow‐up calls | 6 months | 2 to 5 years | No | Positive Parenting Program – Triple P | Waiting list | ECBI: parent; PRQ‐P: parent | Psychologists (after training and accreditation) |
|
Morawska 2014 Australia |
Individual parent (parallel) | Parents (N = 86) |
1 (2 hours) session in 1 week | 6 months | 2 to 5 years | Eating and mealtime difficulties | Hassle Free Mealtime – Triple P | Waiting list | PTFA: parent; CAPES: parent | Psychologists (after training and accreditation) |
|
Niccols 2008 Canada |
Individual participant (parallel) | Mothers (N = 76) |
8 (2 hours) sessions in 8 weeks | 6 months | 1 to 24 months | No | Right from the Start Parenting Program | Usual primary care (home visit) | AQS: mothers | Psychologists and social workers with additional training |
|
Niccols 2009 Canada |
Individual participant (parallel) | Mothers (N = 79) |
8 sessions in 8 weeks | 1 month | 12 to 36 months | No | COPEing with Toddler Behaviour | Waiting list | ECBI: mothers; parent‐child interaction: observer | After 20 hours workshop training |
|
Nicholson 1998 USA |
Individual parent (parallel) | Parent (N = 40) |
4 (2.5 hours) sessions in 4 weeks | Postintervention (6 weeks for those receiving intervention) | 1 to 5 years | No | STAR cognitive strategy | Waiting list | BSQ: parents | Master degree parent educators |
|
Nicholson 2002 USA |
Individual parent or caregiver (parallel) | At‐risk parents (violent) (N = 26) |
10 (1.5 hours) sessions in 10 weeks | 1 month | 1 to 5 years | No (low SES) | STAR Parenting Program | Waiting list | BSQ; ECBI: parents; PSC: teachers; | 1 PhD and 4 Master trained professionals |
|
Oré 2011 Peru |
Mother/child dyads (parallel) | Mothers (N = 163) |
4 sessions in 4 weeks | Postintervention | 8 to 11 months | No | Group parenting training (not specified) | No information | BSID‐II: mother | Psychologist and nurse |
|
Perrin 2014 USA |
Individual parents (parallel) | Parents (N = 150) |
10 (2 hours) sessions in 10 weeks | 12 months | 2 to 4 years | Disruptive behaviour | Incredible Years ‐ abbreviated | Waiting list | ECBI: parents; DPICS‐R: clinical observers | Research clinician and a paediatrician |
|
Simkiss 2013 UK |
Individual family (parallel) | Parents (Flying Start early years) (N = 286) |
10 (2 hours) sessions in 10 weeks | 9 months | 2 to 4 years | No | Family Links Nurturing Programme | Waiting list | PrePACS: researchers; PedsQL: parents | Facilitators trained over a 4‐day programme and supervision |
|
Solís‐Cámara 2004 Mexico |
Mother/child dyads (parallel) | Parent (N = 40) |
8 (1.5 hours) sessions in 8 weeks | 6 months | 3 to 5 years | Behaviour difficulties | Research‐based standardised parenting programme | Waiting list | ECBI: parents | Not reported |
|
Sutton 1992 UK |
Individual family (quasi‐RCT) | Parents (N = 37) |
8 (1 to 2 hours) sessions in 22 weeks (+ 2 boosters) | 12 to 18 months | 1 to 4.9 years | Difficult preschool children | Group parenting training (booklets from researcher) | Waiting list | HSQ; CBQ: parents | Researcher |
|
Tiedemann 1992 Canada |
Individual parent (parallel) | Mothers (only married ones) (N = 49) |
5 sessions | 6 weeks | 2.5 to 6.9 years | Difficulties in sibling interactions | Group sharing programme | Waiting list | VABS: mother, father and out‐of‐home; CBCL: mother | Not reported |
|
Webster‐Stratton 1982 USA |
Individual mothers (cross‐over) | Mothers (N = 35) |
4 (2 hour) sessions in 4 weeks | Postintervention | 3 to 5 years | No | Videotape modelling group discussion programme | Waiting list | ECBI: parents IBCS: observers | Graduate student therapist with extensive group work training |
AQS: Attention Questionnaire Scale; BIQ: Behavioural Inhibition Questionnaire; BITSEA: Brief Infant Toddler Social‐Emotional Asessment; BSID‐II: Bayley Scales of Infant Development ‐ Second Edition; BSQ: Behavioural Style Questionnaire; CALIS‐PV: Child Anxiety Life Interference Scale; CAPES: Children's Assessment of Participation and Enjoyment; CAPTRS: Conners Abbreviated Parent/Teacher Rating Scale; CBQ: Children's Behaviour Questionnaire; CBCL: Child Behaviour Checklist; CBIS: Composite Behavioural Inhibition score; C‐TRF: Caregiver ‐ Teacher Report Form; DPICS: Dyadic Parent‐Child Interaction Coding System; DPICS‐R: Dyadic Parent‐Child Interaction Coding System‐Revised; DSM: Diagnostic and Statistical Manual of Mental Disorders; ECBI: Eyberg Child Behaviour Inventory; GBIR: Global Behavioural Inhibition rating; HSQ: Home Situations Questionnaire; IBCS: Interpersonal Behaviour Construct Scale; KPC: Kohn's Problem Checklist; KSCRS: Kendall Self Control Rating Scale; PAS‐R: Preschool Anxiety Scale ‐ Revised; PBQ: Preschool Behaviour Questionnaire; PCQ: Parental Concerns Questionnaire; PedsQL:Pediatric Quality of Life Inventory; PrePACS: Parent Account of Child Symptoms; PSC: Pediatric Symptom Checklist; PTFA: Parent and Toddler Feeding Assessment; PRQ‐P: Parenting Relationships Questionnaire ‐ Preschool; RCT: randomised controlled trials; SDQ: Strengths and Difficulties Questionnaire; SES: socioeconomic status; SGS‐II: Schedule of Growing Skills ‐ Second Edition; SSR: Social Skills Rating System; VABS: Vineland Adaptive Behaviour Scales.
Design
Sixteen studies were RCTs that randomly allocated individuals, families or parent‐child dyads to intervention and control conditions utilising a parallel design. Three studies were cluster‐randomised trials: Breitenstein 2012 and Gross 2003 used day care centre as the unit of allocation, Hiscock 2008 randomised by primary care health centre. Two studies were quasi‐RCTs (Nicholson 1998; Sutton 1992). Nicholson 1998 allocated some parents on the basis of the night that they were able to attend the programme (e.g. one night included the parent‐education group, and the second night included the wait‐list control group). Only participants with no preferences were randomised to the two study conditions; remaining families were allocated on the basis of preference. Sutton 1992 comprised a quasi‐randomised design in which participants were sequentially allocated to one of four study conditions. Eleven families who were initially randomised to the wait‐list control group were reallocated to the intervention group. Two studies were cross‐over trials (Cummings 2000; Webster‐Stratton 1982). Cummings 2000 reported that 37 parents participated in the study, but only 31 participants were randomised to the intervention (n = 15) or the control (n = 16) condition. Six of the parents who first participated in the wait‐list control group, participated later in the intervention group and therefore were double‐counted. Data for Webster‐Stratton 1982 were reported separately for each of the two cross‐over stages; due to potential carry‐over effects we only used data from the first stage.
Of the three cluster trials, Hiscock 2008 accounted for clustering in their analysis by using multilevel models. The remaining two cluster trials reported means and SDs based on descriptive statistics (Breitenstein 2012; Gross 2003), so we set out to calculate the inflated standard errors in order to account for clustering and obtain approximate correct analysis (Higgins 2011). However, the intracluster correlation coefficients (ICCs) were not reported in these two studies (Breitenstein 2012; Gross 2003). Hiscock 2008 reported an ICC of 0.03. We used this value (ICC = 0.03) to compute the inflated standard errors in the Breitenstein 2012 and Gross 2003 studies, which were included in one or more of the following meta‐analyses (Analysis 1.3; Analysis 1.4; Analysis 1.6; Analysis 1.9; Analysis 1.13). In order to assess the impact of this chosen ICC value, we conducted sensitivity analyses by assuming a set of different ICC values (0, 0.02, and 0.1). We assumed an ICC of 0 in sensitivity analysis one (see Analysis 2.1, Analysis 2.2, Analysis 2.3, Analysis 2.4, Analysis 2.5); we set the ICC at 0.02 in sensitivity analysis two (see Analysis 3.1, Analysis 3.2, Analysis 3.3, Analysis 3.4, Analysis 3.5); lastly, we used a larger ICC value of 0.1 in sensitivity analysis three (Analysis 4.1, Analysis 4.2, Analysis 4.3, Analysis 4.4, Analysis 4.5).
1.3. Analysis.
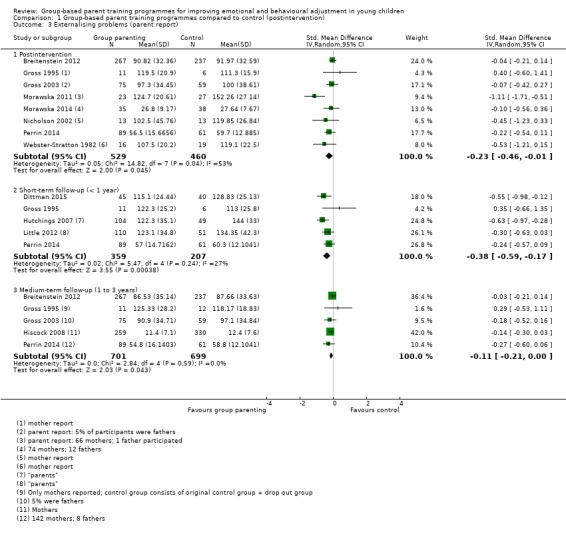
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 3 Externalising problems (parent report).
1.4. Analysis.
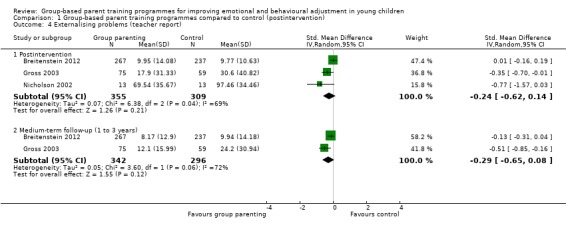
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 4 Externalising problems (teacher report).
1.6. Analysis.
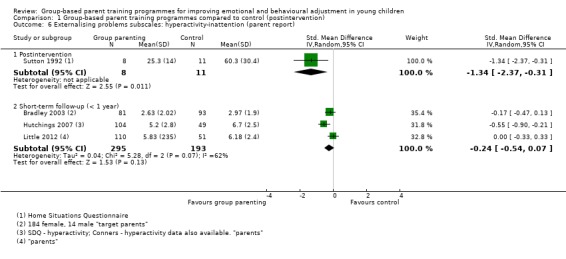
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 6 Externalising problems subscales: hyperactivity‐inattention (parent report).
1.9. Analysis.
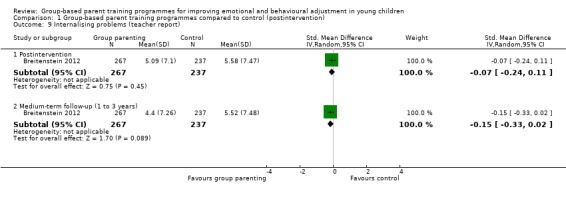
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 9 Internalising problems (teacher report).
1.13. Analysis.
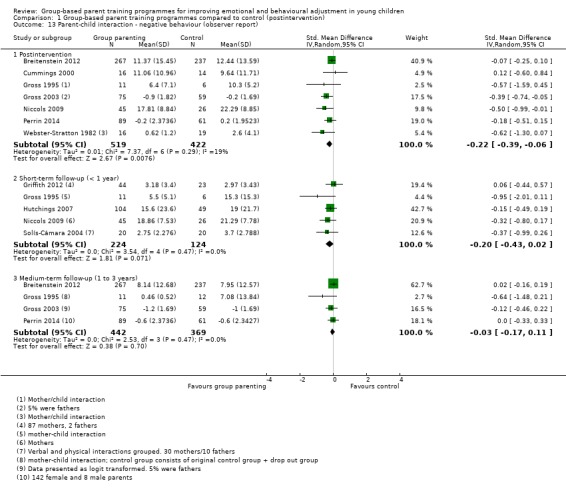
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 13 Parent‐child interaction ‐ negative behaviour (observer report).
2.1. Analysis.
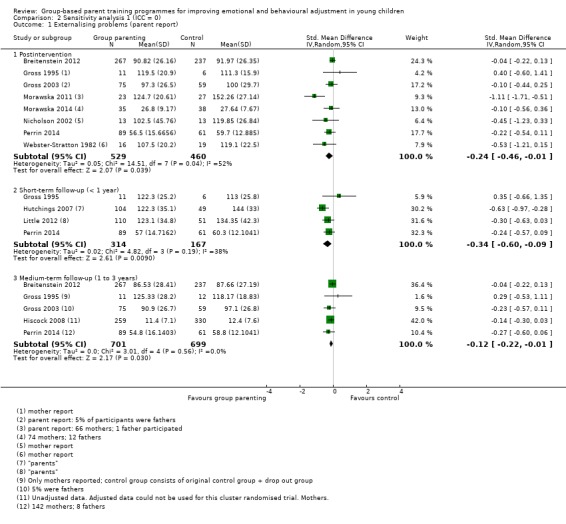
Comparison 2 Sensitivity analysis 1 (ICC = 0), Outcome 1 Externalising problems (parent report).
2.2. Analysis.
Comparison 2 Sensitivity analysis 1 (ICC = 0), Outcome 2 Externalising problems (teacher report).
2.3. Analysis.
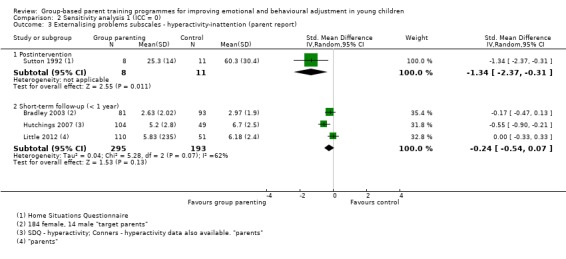
Comparison 2 Sensitivity analysis 1 (ICC = 0), Outcome 3 Externalising problems subscales ‐ hyperactivity‐inattention (parent report).
2.4. Analysis.
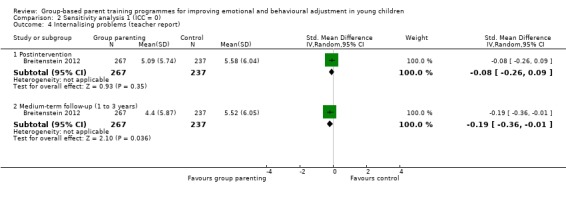
Comparison 2 Sensitivity analysis 1 (ICC = 0), Outcome 4 Internalising problems (teacher report).
2.5. Analysis.
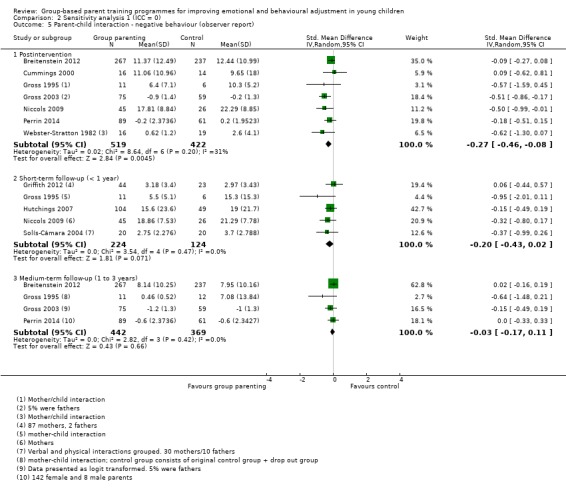
Comparison 2 Sensitivity analysis 1 (ICC = 0), Outcome 5 Parent‐child interaction ‐ negative behaviour (observer report).
3.1. Analysis.
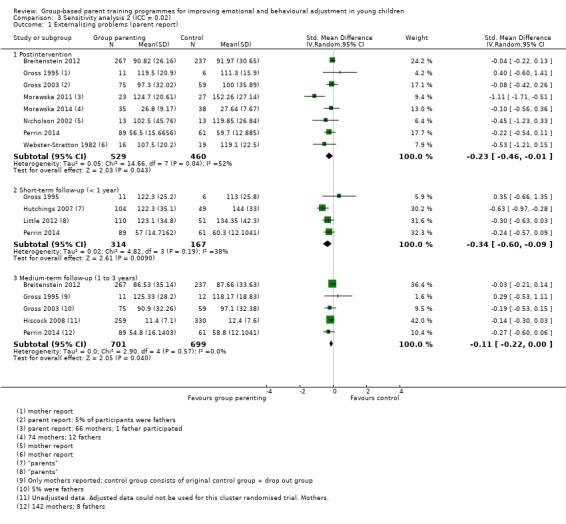
Comparison 3 Sensitivity analysis 2 (ICC = 0.02), Outcome 1 Externalising problems (parent report).
3.2. Analysis.
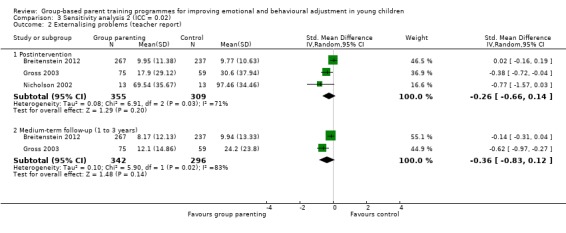
Comparison 3 Sensitivity analysis 2 (ICC = 0.02), Outcome 2 Externalising problems (teacher report).
3.3. Analysis.
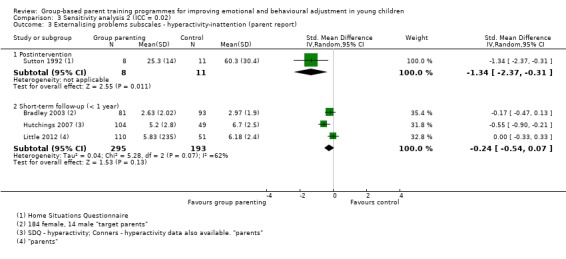
Comparison 3 Sensitivity analysis 2 (ICC = 0.02), Outcome 3 Externalising problems subscales ‐ hyperactivity‐inattention (parent report).
3.4. Analysis.
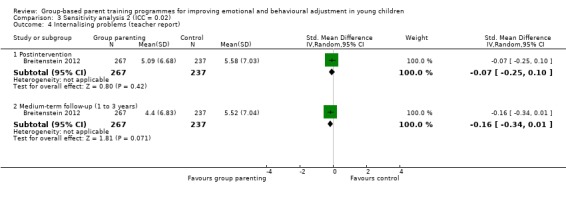
Comparison 3 Sensitivity analysis 2 (ICC = 0.02), Outcome 4 Internalising problems (teacher report).
3.5. Analysis.
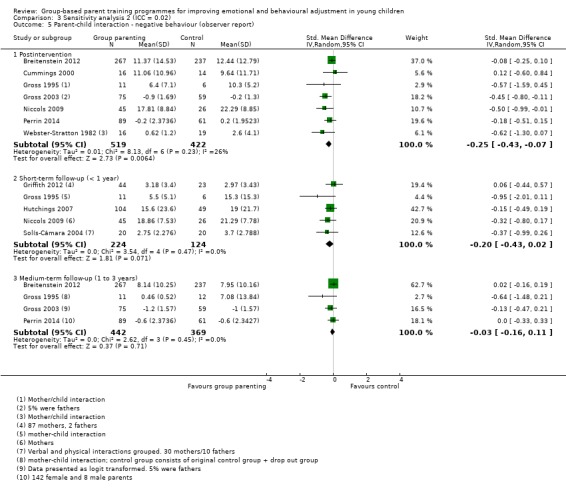
Comparison 3 Sensitivity analysis 2 (ICC = 0.02), Outcome 5 Parent‐child interaction ‐ negative behaviour (observer report).
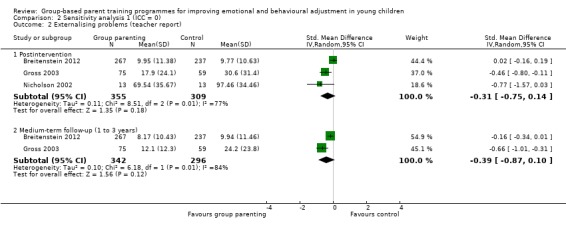
4.1. Analysis.
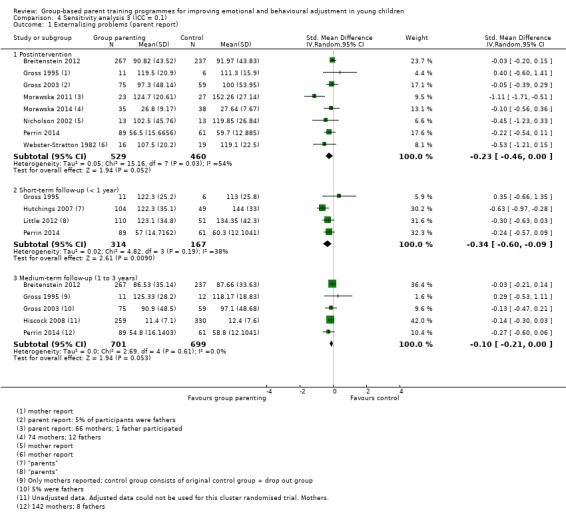
Comparison 4 Sensitivity analysis 3 (ICC = 0.1), Outcome 1 Externalising problems (parent report).
4.2. Analysis.
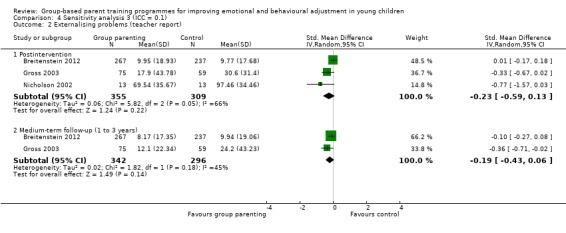
Comparison 4 Sensitivity analysis 3 (ICC = 0.1), Outcome 2 Externalising problems (teacher report).
4.3. Analysis.
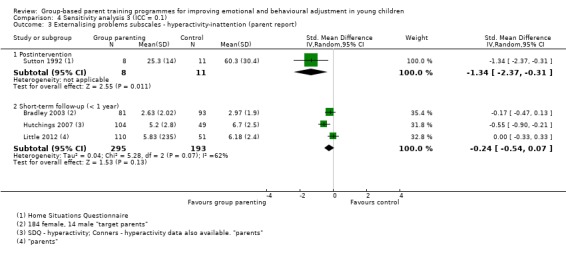
Comparison 4 Sensitivity analysis 3 (ICC = 0.1), Outcome 3 Externalising problems subscales ‐ hyperactivity‐inattention (parent report).
4.4. Analysis.
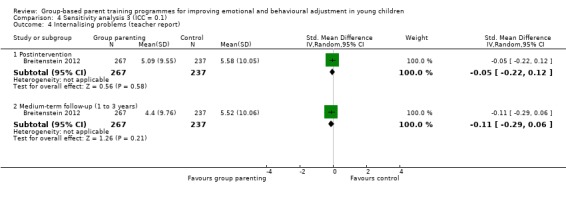
Comparison 4 Sensitivity analysis 3 (ICC = 0.1), Outcome 4 Internalising problems (teacher report).
4.5. Analysis.
Comparison 4 Sensitivity analysis 3 (ICC = 0.1), Outcome 5 Parent‐child interaction ‐ negative behaviour (observer report).
Sample sizes
There was considerable variation in sample size between studies. Overall, the number of participants (primary carer and index child pair) initially randomised per study ranged from 23 in Gross 1995 to 733 in Hiscock 2008. In two studies some participants were included in the analysis twice (i.e. once as a control case and again as an intervention case; Cummings 2000; Sutton 1992).
Setting
Eight studies were conducted in the USA (Breitenstein 2012; Cummings 2000; Gross 1995; Gross 2003; Nicholson 1998; Nicholson 2002; Perrin 2014; Webster‐Stratton 1982), five in the UK (Griffith 2012; Hutchings 2007; Little 2012; Simkiss 2013; Sutton 1992), four in Canada (Bradley 2003; Niccols 2008; Niccols 2009; Tiedemann 1992), five in Australia (Dittman 2015; Hiscock 2008; Kennedy 2009; Morawska 2011; Morawska 2014), and one each in Mexico (Solís‐Cámara 2004) and Peru (Oré 2011).
Twelve studies were multicentre trials (Breitenstein 2012; Dittman 2015; Griffith 2012; Gross 2003; Hiscock 2008; Hutchings 2007; Little 2012; Morawska 2011; Morawska 2014; Perrin 2014; Simkiss 2013; Sutton 1992), 10 were single‐centre trials (Bradley 2003; Cummings 2000; Gross 1995; Kennedy 2009; Niccols 2008; Niccols 2009; Nicholson 1998; Nicholson 2002; Tiedemann 1992; Webster‐Stratton 1982), and two did not provide sufficient information to be classified (Oré 2011; Solís‐Cámara 2004).
The trials were mostly conducted in community settings such as community‐based agencies, medical centres and day care centres. Six studies did not report details of where the study was set or where the intervention was delivered (Griffith 2012; Gross 1995; Niccols 2008; Niccols 2009; Nicholson 2002; Simkiss 2013).
Participants
Participants comprised primary carer‐index child pairs. The target primary carers were predominantly mothers or fathers, or both. Two studies involved foster parents, grandparents or other relatives as the primary carer (Gross 2003; Nicholson 2002). Fourteen studies recruited children without emotional and behavioural problems, one of which recruited parents who were deemed to be 'at‐risk' on the basis of their frequent use of verbal and corporal punishment (Nicholson 2002). Of these 14 studies, four recruited from low‐income samples (Breitenstein 2012; Griffith 2012; Gross 2003; Nicholson 2002).
Twelve studies recruited children experiencing emotional or behavioural difficulties such as conduct problems, hostile/aggressive behaviour, self destructive behaviour, or hyperactivity. Bradley 2003 recruited preschoolers with behavioural problems. Dittman 2015 included children whose parents were concerned with disobedient or non‐compliant behaviour. Gross 1995 included parents of children meeting the criteria for behavioural difficulty as measured by the intensity scale of the Eyberg Child Behaviour Inventory (ECBI, Eyberg 1978). Hutchings 2007 also recruited children scoring above the clinical cut‐off on either the problem or intensity subscales of the ECBI (Eyberg 1978). Kennedy 2009 included parents of children scoring high on behavioural inhibition. Little 2012 included parents of children at risk of social‐emotional or behavioural disorders reaching the “high need” threshold of the “total difficulties” score of the Strengths and Difficulties Questionnaire (SDQ). Morawska 2014 included parents who were concerned about and seeking assistance for their child's eating or mealtime difficulties. Perrin 2014 included parents of children who had disruptive behaviours on the Infant‐Toddler Social‐Emotional Assessment (ITSEA) scale (Carter 2003). Solís‐Cámara 2004 included parents of children described as fulfilling criteria for behavioural difficulties, but no further details were provided. Sutton 1992 recruited children described as exhibiting 'difficult' behaviour, but provided no further criteria. Tiedemann 1992 included married mothers of siblings with parent‐reported difficulties in sibling interaction. Cummings 2000 did not provide details about the use of eligibility criteria to select participants, but described the programme as being aimed at addressing children's negative behaviours, including sleep problems and toileting.
There was considerable variation across studies in terms of the inclusion of mothers and fathers. Six studies recruited only mothers (Hiscock 2008; Niccols 2008; Niccols 2009; Oré 2011; Tiedemann 1992; Webster‐Stratton 1982). Twelve studies recruited parents, but predominantly mothers participated (Breitenstein 2012; Cummings 2000; Dittman 2015; Griffith 2012; Gross 2003; Morawska 2011; Morawska 2014; Nicholson 1998; Nicholson 2002; Perrin 2014; Simkiss 2013; Solís‐Cámara 2004); one study recruited couples (Gross 1995); and five studies recruited parents, but did not provide details on participant gender (Bradley 2003; Hutchings 2007; Kennedy 2009; Little 2012; Sutton 1992). The age range of target parents was between mid‐20s and mid‐30s.
Thirteen studies included some older children (up to five years of age), but still met our criterion that the maximum mean age of children in the study was no greater than three years and 11 months. In addition, Tiedemann 1992 included mothers of at least two children aged between two years and six months and six years and 11 months. Data for the younger children (mean age 38.0 months) were analysed and reported separately, which allowed the study to be included in this review. Further details of the participant ages are given in the Characteristics of included studies tables.
Interventions
Fourteen studies examined the effectiveness of programmes aimed at the primary prevention of emotional and behavioural problems, whereas 12 studies evaluated the effectiveness of parenting programmes targeted at children with early problems, 'difficult' children, or children with existing problems (secondary or tertiary prevention) (Bradley 2003; Cummings 2000; Dittman 2015; Gross 1995; Hutchings 2007; Kennedy 2009; Little 2012; Morawska 2014; Perrin 2014; Solís‐Cámara 2004; Sutton 1992; Tiedemann 1992).
Six of the included studies involved an evaluation of the Incredible Years Basic Parenting Programme (Incredible Years 2009; Griffith 2012; Gross 1995; Gross 2003; Hutchings 2007; Little 2012; Perrin 2014). The programme consists of a series of brief, videotaped vignettes of parents and children engaging in a variety of typical family situations. Two studies evaluated the Triple P‐Positive Parenting Program adapted to eating and mealtime behaviour (Morawska 2011; Morawska 2014). The programme targeted parenting practices and parental cognitions, which constitute the direct and indirect pathways of parenting impact on child mealtime behaviours. Two studies evaluated the cognitive‐behavioural STAR (Stop Think Ask Respond) programme, which was delivered over three‐weekly, two‐hour sessions followed by a booster session one month later (Nicholson 1998; Nicholson 2002). The remaining 15 programmes were evaluated in individual studies. Nine studies included videotape modelling as an element of the studied interventions (Bradley 2003; Breitenstein 2012; Cummings 2000; Gross 1995; Gross 2003; Hutchings 2007; Niccols 2009; Perrin 2014; Webster‐Stratton 1982). Specific details of the content of each programme are provided in Table 3.
2. Content of the parenting programmes.
| Study | Content |
| Bradley 2003 | A video group‐based training. There were seven to eight parents in each group. Participants watched the video 1‐2‐3 Magic during the first three sessions. This video provides simple clear strategies, such as timeout and rewards to reduce coercive and conflicting patterns of parent‐child interaction, and stresses importance of reducing nagging, yelling, hitting, and critical and hostile comments. Handouts were also provided. The facilitators encouraged the group to explore strategies and support one another. The group intervention consisted of a two‐hour group meeting, once a week for three weeks, followed by a booster session four weeks after the third session |
| Breitenstein 2012 | The Chicago Parent Program employs videotaped vignettes, a group discussion format that corresponds to principles being addressed in each of the vignettes. Parents receive weekly homework assignments and handouts summarising important points from each session. The topics covered in the 11‐weekly Chicago Parent Program sessions include: the concept of child‐centred time; the importance of family routines and traditions; the value of praise and encouragement; the role of rewards for reducing challenging behaviour; the importance of setting clear limits and of following through on limit‐setting; the need to establish consequences in response to misbehaviour parents want stopped; and the use of specific parenting strategies such as ignore, distract, and time‐out; stress management; and problem‐solving skills. Two months after the 11ͭ ͪ session, a booster session is offered to help parents continue using the programme principles without the ongoing support of the parent group |
| Cummings 2000 | Group‐based behavioural programme using video and other educational material. Topics covered in the six sessions included positive attention and reinforcement; decreasing and eliminating problem behaviours; reading to children; sleep management; and toilet training. Each of the following topics were covered in a one and a half hour session. A 65‐minute video, leader's guide, handouts, and a book were used in the positive attention and reinforcement session |
| Dittman 2015 | Discussion group facilitated by registered psychologist. Participants shared experiences and took part in exercises. Topics covered by the facilitators' presentations were the role of parent behaviour in moderating child negative and positive behaviours. Participants also received a workbook |
| Griffith 2012 | Incredible Years Toddler Parenting Program is a 12‐week parenting programme, see Gross 2003 below |
| Gross 1995 | Group‐based parenting programme delivered over the course of 10 weeks and developed by Webster‐Stratton using self efficacy theory. Parents learn through mastery experiences, viewing and discussing videotaped vignettes of parent and child models, and mutual support and reinforcement among group participants. The programme includes information on (a) how to play with your child, (b) helping your child learn, (c) using praise and rewards effectively, (d) strategies for setting limits effectively, and (e) managing misbehaviour. Groups were led by psychiatric nurses |
| Gross 2003 | Group‐based parenting programme (The Incredible Years BASIC Programme) delivered to groups of 8 to 12 parents in two‐hour sessions over the course of 12 weeks. Topics covered included child‐directed play, helping young children learn, using praise and rewards, effective limit setting, handling misbehaviour and problem solving. Home work assignments were also used. The course was taught using video vignettes which were appropriate for toddlers |
| Hiscock 2008 | The intervention consisted of three sessions targeting key modifiable parenting risk factors for childhood behavioural problems: unreasonable expectations, harsh parenting, and lack of nurturing parenting. At eight months, mothers received handouts discussing normal child behavioural, motor, and social development. At 12 months, two‐hour group session discussing ways to develop a warm and sensitive relationship and encourage desirable behaviour. At 15 months, two‐hour group session discussing ways to manage unwanted behaviour in children. Draws on attachment theory and social learning theory |
| Hutchings 2007 | The Webster‐Stratton Incredible Years Basic Parenting Program is a programme promoting positive parenting and improving parenting skills, including establishing a positive relationship with the child through play and child‐centred activities; encouraging, rewarding and praising the child for appropriate behaviour; giving guidance in effective limit setting and strategies for managing noncompliance. A group‐based intervention was provided once a week over a 12‐week period. Each group consists of a maximum of 12 parents, and each session lasted for 2 to 2.5 hours. Two trained leaders from different backgrounds (social workers, family support workers, health visitors, psychologists, etc.) held the sessions. The programme aims to promote positive parenting through: increasing positive child behaviour through praise and incentives; improving parent‐child interaction; setting clear expectations and applying consistent gentle consequences for problem behaviour. The programme uses a number of methods including: role play; helping parents to identify social learning principles; modelling; discussion; skills practice and analysis of video material. The programme promotes positive parenting and uses a collaborative approach (e.g. role play, modelling, discussion, etc.) |
| Kennedy 2009 | Group‐based parenting programme. The content of the sessions is (a) psychoeducation about the development, maintenance, and treatment of excessive anxiety in young children; (b) parent management strategies for anxious children, including positive parenting skills and reduction of overprotection; (c) introduction to exposure with development of graded hierarchies; (d) revision of exposure hierarchies and development/enhancement of social skills; (e) cognitive restructuring for anxious/negative thinking styles for parents and children; (f) exposure for parents’ fears; (g) coping plans (summary of anxiety management skills) for anxious children; (h) maintenance and relapse prevention |
| Little 2012 | The Incredible Years BASIC Parenting Program for parents of three and four‐year‐olds showing the symptoms of a conduct disorder. The 12‐week version was delivered in children’s centres. The programme was delivered by a mixture of children’s centre staff, family support workers, educational psychologists, and parenting practitioners |
| Morawska 2011 | The intervention consisted of one two‐hour discussion group on children’s problem eating and mealtime behaviour. The programme was designed to target parenting practices and parental cognitions, which constitute the direct and indirect pathways of parenting impact on child mealtime behaviours |
| Morawska 2014 | Hassle Free Mealtime Triple P consisted of one two‐hour discussion group on children’s problem eating and mealtime behaviour. The programme was designed to target parenting practices and parental cognitions, which constitute the direct and indirect pathways of parenting impact on child mealtime behaviours |
| Niccols 2008 | Right from the Start is intended to enhance parental sensitivity, parent‐child interaction, the impact of parent and child temperament on interactions, and building a healthy relationship. Large groups of parents (12 to 40) sit at tables of 4 to 6 parents each and watch video clips of confederate parents making exaggerated errors in common parent‐child interaction situations. They discuss in their small groups (i.e. at their tables) the errors and the impact of the errors, as well as alternatives and the benefits of the alternatives. Large group discussion follows each small group discussion. Parents practice skills in structured homework assignments |
| Niccols 2009 | Parent training programme with session topics focus on preventing challenging behaviours in children |
| Nicholson 1998 | A 10‐hour group‐based educational parenting programme specifically designed for parents of children aged one to five years, based on well‐established knowledge and practices of parenting drawn from the literature on child development, cognitive psychology, and social learning theory. The programme comprises four major components, represented by the STAR acronym. The first encouraged parents to stop and think (S and T in the acronym) before responding to their child's behaviours. The second focused on parents questioning their expectations of their child (A for ask in the acronym). The third dealt with nurturing strategies for encourage development, and the fourth dealt with discipline and setting limits on children's behaviour (R for respond in the acronym). The programme was delivered by parent educators |
| Nicholson 2002 | A psychoeducational programme using the STAR Parenting Program (as described in Nicholson 1998). Training delivered by facilitators trained in the STAR Program |
| Oré 2011 | Group‐based behavioural programme for mothers and children using educational material. Topics covered in the four sessions included positive attention and reinforcement; interaction and games between mothers and children. The four sessions were co‐ordinated by the same psychologist with the support of a nurse that dealt with the logistics |
| Perrin 2014 | Researchers abbreviated the Incredible Years curriculum to create a 10‐week manualised protocol. The programme encourages proactive, nurturing parenting, while discouraging harsh, punitive approaches using videotaped modelling, group discussion, role plays, and home practice tasks arranged across four modules |
| Simkiss 2013 | Family Links Nurturing Programme (FLNP) is a structured, manualised course comprising of an introductory "coffee morning", followed by 10 weekly 2‐hour sessions for groups of 6 to 10 parents. It aims to help parents understand and manage feelings and behaviour, improve relationships at home and in school, improve emotional health and wellbeing, and develop confidence and self esteem, which are essential for effective parenting and learning. It offers support to help parents build on pre‐existing parenting skills, use positive behaviour management, communication and relationship strategies, and look after their own emotional needs so they can parent more effectively |
| Solís‐Cámara 2004 | Group‐based parenting programme delivered over the course of eight weeks, based on the principles of behaviour and therapy cognitive learning. The programme was developed by the author and focused on parents learning about themselves, and child‐management skills. The training was delivered by the authors. |
| Sutton 1992 | Group‐based parenting programme delivered over the course of eight weeks, based on the principles of social learning theory. The programme was developed by the author and focused on parents learning child‐management skills. The parents aimed to obtain their child's compliance with an instruction within one minute of receiving it. The training was delivered by the author |
| Tiedemann 1992 | The sharing programme was adapted from Barton 1979 and Bryant 1984, which provided children with specific training in component skills of sharing, detailed rationales, and instructions regarding sharing, and information about inappropriate sharing‐related behaviour. Mothers received basic developmental and behaviour management information in the first two sessions through lecture, discussion, reading material and instructor modelling, which were followed by three sessions with the instructor presenting training in the sharing programme by means of lecture, group discussion, reading material, and modelling |
| Webster‐Stratton 1982 | A videotape modelling group discussion programme was designed to provide parents with a broad base of knowledge and skills in ways of interacting and communicating with their children and in handling their children's behavioural problems. For example, videotape vignettes were shown of non‐study parent models who were nurturing, playful, and sensitive to the individuality of their children in contrast to other vignettes of parent models who were rigid, controlling, and concrete with their children. The programme was delivered over four weekly two‐hour videotape modelling discussion sessions, which were conducted over four consecutive weeks |
Twenty of the included studies compared group‐based parenting programmes with a wait‐list control group as part of the evaluation of their effectiveness in improving the emotional and behavioural adjustment of infants and toddlers. However, one study compared a parenting programme with no intervention (Gross 1995). Hiscock 2008 compared a parenting programme with usual primary care and Niccols 2008 with treatment‐as‐usual, consisting of home visits. Oré 2011 did not report what the control condition consisted of; we requested this information from the study authors but did not receive an answer at the time of preparing this review.
Three studies used more than one intervention group. In addition to group‐based parent training and control groups, Gross 2003 included a group with teacher training and a group with teacher and parent training; Sutton 1992 included a group receiving home visits and a group receiving telephone consultation; and Tiedemann 1992 included a group that received individual support. None of the data for any of the additional groups have been reported in the review.
The duration of the interventions ranged between one week and seven months (mean 9.7 weeks; median 10 weeks).
Outcomes
Outcomes were reported by parents, teachers, or independent observers and involved the use of a variety of standardised instruments. We assessed outcomes at four time points: postintervention (less than one month after the end of the programme), at short‐term follow‐up (less than one year after the end of the programme), at medium‐term follow‐up (one to three years after the end of the programme), and at long‐term follow‐up (more than three years after the end of the programme).
Primary outcome
Emotional and behavioural problems
Nine studies measured child emotional and behavioural problems, mostly reported by parents. Oré 2011 used the Bayley Scale of Infant Development II (BSID‐II, Bayley 1993); Nicholson 1998 and Nicholson 2002 both used the Behaviour Screening Questionnaire (BSQ, Richman 1971); Tiedemann 1992 used the total behaviour scale of the Child Behaviour Checklist (CBCL, Achenbach 2000); and Sutton 1992 used the Child Behaviour Questionnaire (CBQ, Rutter 1970). One study reported on the Pediatric Symptom Checklist (PSC, Murphy 1988) teacher‐reported scale (Nicholson 2002).
Externalising problems
Thirteen studies measured child externalising problems, mostly reported by parents. Most ‐ Breitenstein 2012; Dittman 2015; Gross 1995; Gross 2003; Hutchings 2007; Little 2012; Morawska 2011; Nicholson 2002; Perrin 2014; Webster‐Stratton 1982 ‐ used the intensity subscale of the ECBI (Eyberg 1978). Hiscock 2008 used the CBCL ‐ externalising scale (Achenbach 2000), and Morawska 2014 and Dittman 2015 used the Child Adjustment and Parent Efficacy Scale (CAPES, Morawska 2010). A number of studies used scales reported by teachers: Breitenstein 2012 used the externalising behaviour subscale of the Caregiver‐Teacher Report Form (C‐TRF, Achenbach 2000); Gross 2003 used Kohn's Problem Checklist (KPC, Kohn 1977); and Nicholson 2002 used the Sutter‐Eyberg Student Behaviour Inventory (SESBI, Sutter 1984) ‐ intensity. Simkiss 2013 used the Parent Account of Child Symptoms (PrePACS, Taylor 1986) ‐ C‐scale, independent, observer‐reported scale.
Internalising problems
Seven studies measured child internalising problems. Parent‐reported scales included the Behavioural Inhibition Questionnaire (BIQ, Bishop 2003) used in Kennedy 2009, the emotional subscale of the CAPES (Morawska 2010 used in Morawska 2014), the internalising subscale of the CBCL (Achenbach 2000 used in Hiscock 2008), and the negative adaptation and affect subscale of the Preschool Characteristics Questionnaire (PCQ, Finegan 1989 used in Bradley 2003). The internalising behaviour subscale of the C‐TRF was the only teacher‐reported scale used (Achenbach 2000; Breitenstein 2012). Independent, observer‐reported scales included a composite behaviour inhibition score based on the criteria used in Kennedy 2009, and the PrePACS ‐ internalising scale (Taylor 1986 used in Simkiss 2013).
Externalising problems: inattention‐hyperactivity
Six studies measured inattention‐hyperactivity, mainly on various externalising behaviour subscales, and mostly reported by parents. Sutton 1992 used the Home Situations Questionnaire (HSQ, Barkley 1981); Bradley 2003 used the hyper/distractible subscale of the Preschool Behaviour Questionnaire (PBQ) (Behar 1974), and Hutchings 2007 and Little 2012 both used the hyperactivity subscale of the Strengths and Difficulties Questionnaire (SDQ, Goodman 1997). Simkiss 2013 reported on the H‐scale, independent observer‐reported subscale of the PrePACS (Taylor 1986).
Secondary outcomes
Social skills
Three studies measured child social skills, mostly reported by parents. Solís‐Cámara 2004 used the social behaviour subscale of the ECBI (Eyberg 1978); Little 2012 used the prosocial subscale of the SDQ (Goodman 1997); and Tiedemann 1992 used the socialisation domain of the Vineland Adaptive Behaviour Scale (VABS, Sparrow 1984).
Parent‐child interaction
Eleven studies measured child behaviour of parent‐child interaction, mostly reported by independent observers. Seven studies used the Dyadic Parent‐Child Interaction Coding System (DPICS, Robinson 1981) (Breitenstein 2012; Cummings 2000; Griffith 2012; Gross 1995; Gross 2003; Hutchings 2007; Perrin 2014); Niccols 2008 used the Attachment Q‐set (Waters 1995); Solís‐Cámara 2004 used a version of the DPICS, developed specifically for the study: the Informe de Observation de la Interaction (IOI); Webster‐Stratton 1982 used the Interpersonal Behaviour Construct Scale (IBCS, Kogan 1975 ); and Niccols 2009 used an observation of parent‐child interaction previously described in Cunningham 1995. One study used the Parenting Relationship Questionnaire (PRQ, Kamphaus 2006) reported by parents (Morawska 2011).
The follow‐up period ranged from four weeks to seven years. In six studies the follow‐up period was 12 months or longer (Breitenstein 2012; Gross 1995; Gross 2003; Hiscock 2008; Perrin 2014; Sutton 1992).
Studies awaiting classification
Eight studies are currently awaiting classification. Farzadfard 2008 (published in Persian), Zhu 2014 (published in Chinese), and Wang 2000 (published in Chinese) are currently awaiting translation so they may be assessed. The full‐text of Sandy 1983 is not available; it has been requested from the author who is trying to locate a copy. In Herbert 2007, the age of the children is unclear, and Schlarb 2012 is an abstract with insufficient detail to assess eligibility; we are trying to locate contact details of the authors to request more information for these two studies. ISRCTN39288126 and ISRCTN88988596 are completed studies, but study results have not yet been published, and are not available in any other fashion. See the Characteristics of studies awaiting classification tables for further details.
Ongoing studies
We identified three ongoing studies. ISRCTN11079129 is being conducted in the UK and is comparing the effects of Incredible Years versus service as usual. Child outcomes include social and emotional wellbeing, behaviour, attachment, cognitive development, and health. Children are included at less than eight weeks of age, and followed up at two, nine, and 18 months. ISRCTN16513449 is being conducted in Sweden and is evaluating child behavioural problems in the Triple‐P group‐parenting intervention versus treatment‐as‐usual for parents of children aged three, four, and five years. ISRCTN17488830 is being conducted in Ireland and is comparing the effects of the Parent and Infant (PIN) programme versus 'services as usual' (SAU). See the Characteristics of ongoing studies tables for further details.
Excluded studies
After assessing 12,052 titles and abstracts retrieved by the updated search in 2015, we assessed 661 full‐text reports for eligibility. We excluded 517 of these in the first round of full‐text screening, for the following reasons: 139 were not RCTs or quasi‐RCTs, 267 did not include participants who met the inclusion criteria, 70 did not include a relevant intervention, 35 did not include a relevant control group, and six did not measure any relevant outcomes. We excluded a further 101 unique studies (103 reports) in a second round of full‐text screening, for the following reasons: eight were not RCTs or quasi‐RCTs, 48 did not include participants who fitted the inclusion criteria, 33 did not include a relevant intervention, four studies did not include any control group, and eight studies did not measure any relevant outcome.
Of the 69 reports we had excluded in the previous version of this review, we excluded 67 and included two in the current version: Tiedemann 1992 and Webster‐Stratton 1982. The reason for exclusion of these studies in the previous version was that they failed to meet the age criterion. We included Tiedemann 1992 because the authors reported outcomes on a younger group of children who did meet the age criterion, separately, and we included Webster‐Stratton 1982 because the children's overall mean age met our age criterion (see Included studies).
One previously excluded report was a secondary publication arising from the EHSRC 2001 trial, which we had also excluded in the previous version of the review (Love 2005). We chose to remove Love 2005 from the list of excluded studies, but kept the reference together with the major publication (EHSRC 2001).
Sixty‐six (of the 69) previously excluded studies are presented in the Characteristics of excluded studies tables, along with 35 (out of the 101) studies that were excluded from this version of the review's second round of full‐text screening (see Differences between protocol and review).
In this version of the review, we corrected the study identifiers for three of the previously excluded studies: Bierman 2000 (CPPRG 2000), Caughy 2000 (O'Brien Caughy 2004), and James‐Roberts 2001 (St James‐Roberts 2001).
Risk of bias in included studies
The 'Risk of bias' tables provide details of our 'Risk of bias' assessments within the 24 included studies (see Characteristics of included studies). Figure 2 and Figure 3 are summarised overviews of the included studies' risks of bias.
2.
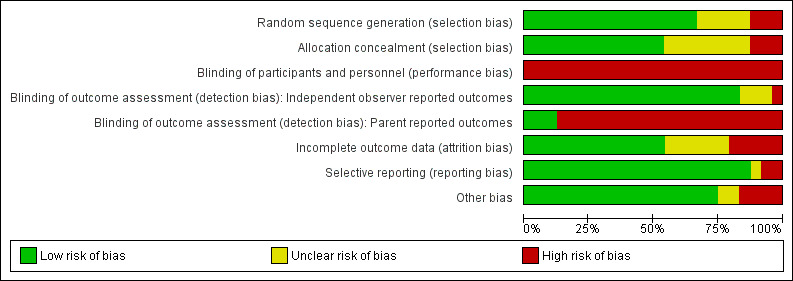
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
3.
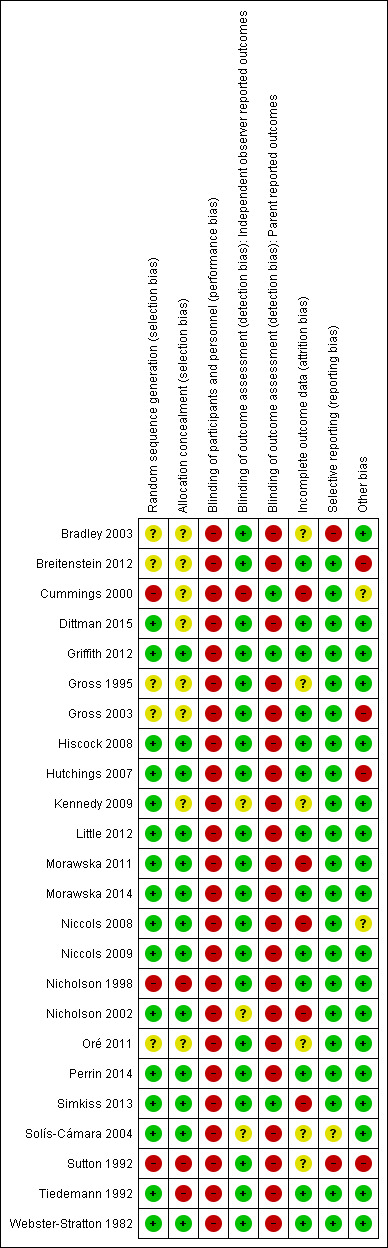
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
The method of sequence generation was described adequately in 16 studies and we rated these studies at low risk of bias. Five studies described their studies as randomised but did not provide further details about the generation of randomisation sequence and we subsequently rated these studies at unclear risk of bias. We rated the remaining three studies at high risk of bias: the randomisation process was compromised for Cummings 2000, as participants were allowed to cross‐over into the intervention arm by choice; two studies used unreliable methods of allocating participants to groups: Nicholson 1998 used parent preference and availability and Sutton 1992 used sequential and not random assignment with some assignments "out of order". Consequently, we conducted sensitivity analyses to assess the impact of these studies.
We judged the allocation concealment method to have been carried out adequately for 13 studies, and rated these studies at low risk of bias. Eight studies did not describe any method of allocation concealment and were not otherwise thought to have compromised concealment of allocation, and we subsequently rated these studies at unclear risk of bias. We rated three studies at high risk of bias: Nicholson 1998 and Sutton 1992 were quasi‐randomised, so it would have been possible to predict the allocation for participants in these studies. Allocation of participants for Tiedemann 1992 was carried out by the same investigator who delivered the intervention programme and carried out the assessments.
Blinding
In trials of parenting programmes, it is not possible to blind either facilitators or parents to the type of treatment being implemented or received, therefore we rated all included studies at high risk of bias for blinding of participants and personnel.
One of the methods of minimising bias arising from failure to blind participants and study personnel is to blind assessors of clinical outcomes. We judged most studies reporting independent observer‐reported outcomes to be adequately blinded, except for Cummings 2000 who we rated at high risk of bias (all observational assessments were coded by the researcher, who was not blinded to group allocation), and Kennedy 2009, Nicholson 2002 and Solís‐Cámara 2004 who we rated at unclear risk of bias (information was reported insufficiently for a judgement to be made).
We rated all studies that included parent‐reported outcomes at high risk of bias for blinding of parent‐reported outcome assessments as parents participated and were aware of the intervention condition. Three studies did not include parent‐reported outcomes (Cummings 2000; Griffith 2012; Simkiss 2013), and we rated these studies at low risk of bias.
Incomplete outcome data
There were no missing outcome data in one study (Nicholson 1998). None of the participating families dropped out of the study and it would appear that all participants remained in the group to which they were allocated. Twelve other studies adequately addressed incomplete data.
Outcome data were not adequately addressed in five studies that we rated at high risk of bias. The results reported in Cummings 2000 suggest that analyses were performed on completers only, and no information was given about attrition and missing outcomes. Reasons for leaving the Morawska 2011 study early were not reported and five participants were not accounted for as only 50 participants were included in the analysis. Only a subset of participants were evaluated in Niccols 2008; the Attachment Q‐set test was only used to evaluate babies over nine months, excluding more than half of the randomised participants. The Nicholson 2002 study reported a 10% dropout rate, but did not describe whether these parents were included in the analyses or from which group they dropped out. For Simkiss 2013, the number of analysed participants does not match the numbers reported lost to follow‐up or the numbers excluded from analyses.
The remaining six studies did not report sufficient information about incomplete data and we rated these studies at unclear risk of bias (Bradley 2003; Gross 1995; Kennedy 2009; Oré 2011; Solís‐Cámara 2004; Sutton 1992). Although Bradley 2003 reports that data were analysed using an intention‐to‐treat analysis, it appears that the post‐test sample comprised completers only (174 participants). No further information was given about missing data for 24 participants. In the Sutton 1992 study, only two families dropped out, but it was not clear whether the data from these families were included in the analyses.
Selective reporting
We rated two studies at high risk of bias: Bradley 2003 reported only the results that were statistically significant (i.e. only two out of four scales of the Preschool Behaviour Questionnaire (PBQ, Behar 1974) are reported ‐ total score and hyperactive/distractible subscale score); and Sutton 1992 reported one outcome (negative child behaviour) insufficiently. We rated Solís‐Cámara 2004 at unclear risk of bias because there was insufficient information reported to make a judgement of high or low risk. No indications of reporting bias were apparent in the remaining 20 studies, and they were rated at low risk of bias.
Other potential sources of bias
Distribution of confounders
While the use of randomisation should, in theory, ensure that any possible confounders are equally distributed between the arms of the trial, the randomisation of small numbers of parents may result in an unequal distribution of confounding factors. It is therefore important that the distribution of known potential confounders is: (a) compared between the different study groups at the outset; or (b) adjusted at the analysis stage. Niccols 2008 reported an imbalance between intervention and control participants for baseline educational level and it is unclear whether this has influenced the results.
Cluster trials
Out of the three included cluster‐randomised trials, only Hiscock 2008 had adjusted for clustering adequately in the reporting of data. Consequently, we rated the remaining two cluster‐randomised studies at high risk of other bias (Breitenstein 2012; Gross 2003).
Additional other sources of bias
Hutchings 2007 reported a conflict of interest in terms of the principal investigator and we rated this study at high risk of bias. Sutton 1992 did not report the number of participants randomised into each group, and we also rated this study at high risk of other bias. We rated Cummings 2000 at unclear risk of other bias as it provided inadequate information to make an assessment about the reliability of many aspects of the study, and as such, may include additional sources of bias.
The remaining 17 studies appeared to be free of any other sources of bias and we rated them at low risk of bias.
Effects of interventions
See: Table 1
The findings of the included studies, reported in the Data and analyses tables, are presented as effect sizes with 95% confidence intervals (CIs), combined using standard mean differences (SMDs). We have used the postintervention scores and follow‐up scores to calculate effect sizes rather than change scores (i.e. pre‐to‐post scores for each group). This reflects the fact that a change SD is required to calculate change scores, and these data were not available for any of the included studies.
For parent‐reported measures, some were reported by mothers only and the remainder by parents, although these consisted mainly of mothers. Mother‐reported measures and parent‐reported measures were pooled, with a footnote in the analysis indicating the type of report.
Three studies also reported on father‐reported measures (Gross 1995; Kennedy 2009; Tiedemann 1992), but we prioritised mother‐reported measures for these studies due to the fact that this is a more common way of assessing children's behaviour. For the same reason, we prioritised observation of mother‐child interaction over father‐child interaction in the one study that reported on both (Gross 1995).
Group‐based parent training programmes compared to control
Primary outcomes
1. Total emotional and behavioural problems
Meta‐analysis results
Included studies used a range of scales to measure total emotional and behavioural problems, including the Bayley Scale of Infant Development II (BSID‐II,Bayley 1993), Behaviour Screening Questionnaire (BSQ, Richman 1971), Child Behaviour Checklist (CBCL, Achenbach 2000), Child Behaviour Questionnaire (CBQ, Rutter 1970), and Pediatric Symptom Checklist (PSC, Murphy 1988). Nicholson 1998 used two scales to measure emotional and behavioural problems; we prioritised the BSQ over the Problem‐Behaviour Rating Scale (PBRS, Fox 1991) because one other study also used the BSQ for this outcome, and because the two scales measure similar concepts.
For parent‐reported scales (Analysis 1.1), there was low quality evidence that group‐based parent training was more effective than control at postintervention (SMD ‐0.81, 95% CI ‐1.37 to ‐0.25; 5 studies, 280 participants; Table 1). The quality of the evidence was downgraded one level for high risk of bias in the included studies (three out of the five included studies did not adequately conceal participant allocation and two studies did not adequately carry out randomisation), and one level for considerable heterogeneity (Tau² = 0.28, I² = 72%). At short‐term follow‐up, one study found that group‐based parent training was more effective than control (SMD ‐1.88, 95% CI ‐2.73 to ‐1.03; 32 participants).
1.1. Analysis.
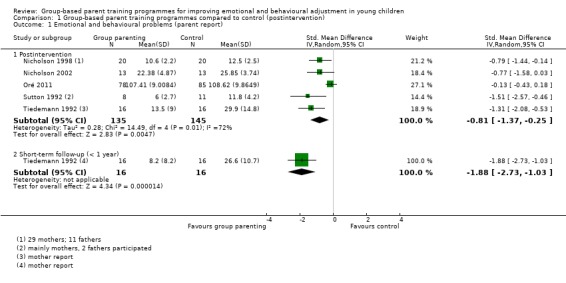
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 1 Emotional and behavioural problems (parent report).
One study measured emotional and behavioural problems at postintervention as reported by teachers, and found no statistically significant difference (SMD ‐0.63, 95% CI ‐1.42 to 0.16; 26 participants, Analysis 1.2).
1.2. Analysis.
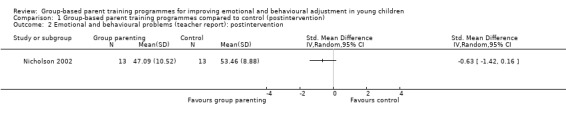
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 2 Emotional and behavioural problems (teacher report): postintervention.
2. Externalising problems
Externalising problems (subscale)
Meta‐analysis results
Included studies used a range of scales to measure externalising problems, including the intensity subscale of the ECBI (Eyberg 1978), externalising subscale of the CBCL (Achenbach 2000), Child Adjustment and Parent Efficacy (CAPES, Morawska 2010), conduct problems subscale of the Preschool Behaviour Questionnaire (SDQ, Goodman 1997), externalising behaviour subscale of the C‐TRF (Achenbach 2000), KPC (Kohn 1977), intensity subscale of the SESBI (Sutter 1984), and PrePACS (Taylor 1986).
For parent‐reported scales (Analysis 1.3), there was moderate quality evidence that group‐based parent training was more effective than control at postintervention (SMD ‐0.23, 95% CI ‐0.46 to ‐0.01; 8 studies, 989 participants; Table 1). The quality of evidence was downgraded one level for inconsistency; heterogeneity was considerable (Tau² = 0.05, I² = 53%). An effect favouring group‐based parent training was maintained at short‐term follow‐up (SMD ‐0.38, 95% CI ‐0.59 to ‐0.17, 5 studies, 566 participants, Tau² = 0.02, I² = 27%), and at medium‐term follow‐up (SMD ‐0.11, 95% CI ‐0.21 to ‐0.00, 5 studies, 1400 participants, Tau² = 0.00, I² = 0%).
For teacher‐reported scales (Analysis 1.4), we found no statistically significant difference between group‐based parent training and control at post‐treatment (SMD ‐0.24, 95% CI ‐0.62 to 0.14; 3 studies, 664 participants, Tau² = 0.07, I² = 69%) or at medium‐term follow‐up (SMD ‐0.29, 95% CI ‐0.65 to 0.08; 2 studies, 638 participants, Tau² = 0.05, I² = 72%).
Single study results
For independent, observer‐reported scales (Analysis 1.5), one study reported no statistically significant difference at short‐term follow‐up (SMD ‐0.14, 95% CI ‐0.39 to 0.11; 243 participants).
1.5. Analysis.
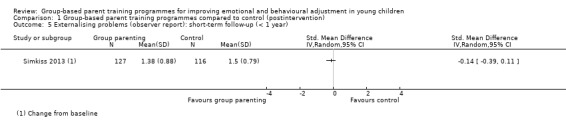
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 5 Externalising problems (observer report): short‐term follow‐up (< 1 year).
Externalising problems: hyperactivity‐inattention (subscale)
Meta‐analysis
It was not possible to combine data in a meta‐analysis for this outcome.
Single study results
A range of scales were used to measure hyperactivity‐inattention, including the attention/hyperactivity subscale of the CBCL (Achenbach 2000), HSQ (Barkley 1981), hyper/distractible subscale of the Preschool Behaviour Questionnaire (PBQ, Behar 1974), hyperactivity subscale of the SDQ (Goodman 1997), and Hscale of the PrePACS (Taylor 1986). Hutchings 2007 used two scales to measure hyperactivity‐inattention; we prioritised the hyperactivity subscale of the SDQ over Conners Abbreviated Parent/Teacher Rating Scale ‐ Hyperactivity subscale because one other study also used the SDQ for this outcome (Conners 1994; Goodman 1997).
For parent‐reported scales (Analysis 1.6), there was very low quality evidence that group‐based parent training was more effective than control at postintervention (SMD ‐1.34, 95% CI ‐2.37 to ‐0.31; 1 study, 19 participants; Table 1). The quality of evidence was downgraded one level for risk of bias (the included study did not adequately carry out randomisation or conceal participant allocation), and two levels for imprecision due to the small number of participants in the included study. We found no statistically significant difference at short‐term follow‐up (SMD ‐0.24, 95% CI ‐0.54 to 0.07; 3 studies, 488 participants, Tau² = 0.04, I² = 62%).
For scales reported by independent observers (Analysis 1.7), one study found no statistically significant difference between group‐based parent training and control at short‐term follow‐up (SMD ‐0.05, 95% CI ‐0.30 to 0.20; 244 participants).
1.7. Analysis.
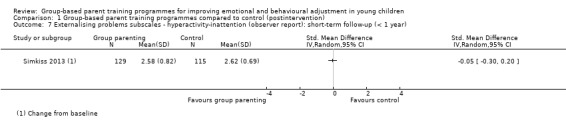
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 7 Externalising problems subscales ‐ hyperactivity‐inattention (observer report): short‐term follow‐up (< 1 year).
3. Internalising problems
Meta‐analyses
It was not possible to combine data in a meta‐analysis for this outcome.
Single study results
Included studies used a range of scales to measure internalising problems, including the BIQ (Bishop 2003), emotional subscale of the CAPES (Morawska 2010), internalising subscale of the CBCL (Achenbach 2000), negative adaptation and affect subscale of the PCQ (Finegan 1989), emotional problems subscale of the SDQ (Goodman 1997), internalising behaviour subscale of the C‐TRF (Achenbach 2000), a composite behavioural inhibition score (Kennedy 2009), and internalising subscale of the PrePACS (Taylor 1986). Kennedy 2009 used three scales to measure Internalising problems; we prioritised the internalising subscale of the BIQ (Bishop 2003) over the Child Anxiety Life Interference Scale (CALIS, Lyneham 2013) and the Preschool Anxiety Scale (PAS, Spence 2001), because the latter two are narrower subscales of internalising problems.
For parent‐reported scales (Analysis 1.8), there was low quality evidence of no statistically significant difference between group‐based parent training and control at postintervention (SMD 0.34, 95% CI ‐0.12 to 0.81; 1 study, 73 participants; Table 1). The quality of evidence was downgraded two levels for imprecision due to the small number of participants in the included study. We found no statistically significant difference at short‐term follow‐up (SMD ‐0.31, 95% CI ‐0.96 to 0.34; 2 studies, 242 participants, Tau² = 0.18, I² = 80%) or at medium‐term follow‐up (SMD ‐0.13, 95% CI ‐0.29 to 0.03; 1 study, 589 participants).
1.8. Analysis.
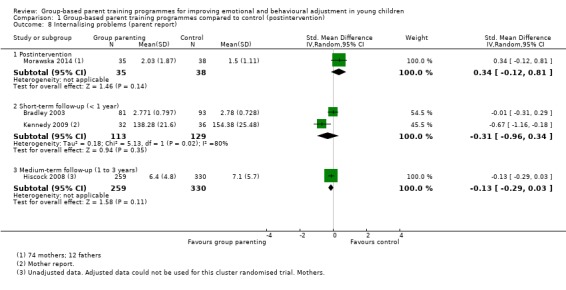
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 8 Internalising problems (parent report).
For teacher‐reported scales (Analysis 1.9), there was no statistically significant difference between group‐based parent training and control at postintervention (SMD ‐0.07, 95% CI ‐0.24 to 0.11; 1 study, 504 participants) or at medium‐term follow‐up (SMD ‐0.15, 95% CI ‐0.33 to 0.02; 1 study, 504 participants).
For scales reported by independent observers (Analysis 1.10), at short‐term follow‐up, we found no statistically significant difference between group‐based parent training and control (SMD ‐0.05, 95% CI ‐1.00 to 0.91; Tau² = 0.43, 2 studies, 295 participants). There was substantial heterogeneity in study results (I² = 91%).
1.10. Analysis.
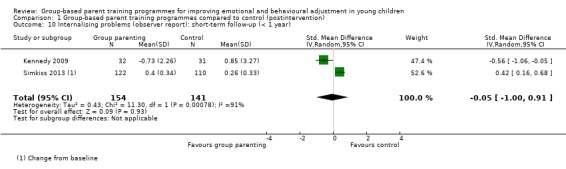
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 10 Internalising problems (observer report): short‐term follow‐up (< 1 year).
Secondary outcomes
1. Social skills
Meta‐analysis results
It was not possible to combine any data in a meta‐analysis for this outcome.
Single study results
Included studies used a range of scales to measure social skills, including the social behaviour subscale of the ECBI (Eyberg 1978), prosocial subscale of the SDQ (Goodman 1997), and socialisation domain of the VABS (Sparrow 1984).
For parent‐reported scales (Analysis 1.11), there was very low quality evidence from one study that group‐based parent training was more effective than control (SMD 3.59, 95% CI 2.42 to 4.76; 1 study, 32 participants; Table 1). The quality of evidence was downgraded one level for risk of bias (the included study did not adequately conceal participant allocation), and two levels for imprecision due to the small number of participants in the included study. At short‐term follow‐up, we found no statistically significant difference between group‐based parent training and control (SMD 1.33, 95% CI ‐0.15 to 2.81; 3 studies, 233 participants). There was substantial heterogeneity in study results (Tau² = 1.55, I² = 94%).
1.11. Analysis.
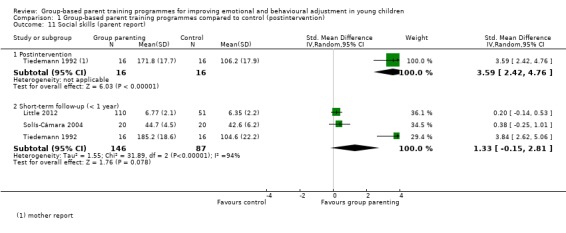
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 11 Social skills (parent report).
For scales reported by independent observers (Analysis 1.12), one study found that there was no statistically significant difference between group‐based parent training and control at postintervention (SMD 0.64, 95% CI ‐0.07 to 1.35; 1 study, 32 participants), but at short‐term follow‐up, there was an effect favouring group‐based parent training (SMD 0.98, 95% CI 0.24 to 1.71; 1 study, 32 participants).
1.12. Analysis.
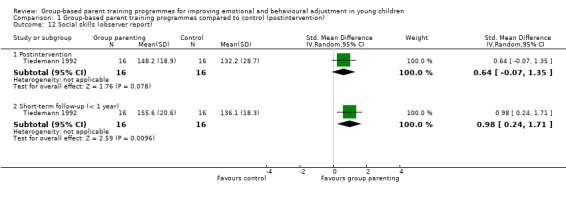
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 12 Social skills (observer report).
2. Parent‐child interaction
2.1 Parent‐child interaction: negative child behaviour (subscale)
Meta‐analyses
Included studies used a range of scales to measure positive and negative child behaviour within the context of parent‐child interaction, including the Dyadic Parent‐Child Interaction Coding System (DPICS, Robinson 1981), Attachment Q‐set (Waters 1995), Interpersonal Behaviour Construct Scale (IBCS, Kogan 1975), and Parenting Relationship Questionnaire (PRQ, Kamphaus 2006).
For scales reported by independent observers (Analysis 1.13), there was moderate quality evidence that group‐based parent training was more effective than control at postintervention (SMD ‐0.22, 95% CI ‐0.39 to ‐0.06; 7 studies, 941 participants, Tau² = 0.01, I² = 19%; Table 1). The quality of evidence was downgraded one level for risk of bias (three out of the six included studies did not adequately describe how randomisation was carried out or allocation concealed, and one study was at high risk of selection bias due to compromised randomisation). We found no statistically significant difference at short‐term follow‐up (SMD ‐0.20, 95% CI ‐0.43 to 0.02; 5 studies, 348 participants, Tau² = 0.00, I² = 0%), or at medium‐term follow‐up (SMD ‐0.03, 95% CI ‐0.17 to 0.11; 4 studies, 811 participants; Tau² = 0.00, I² = 0%).
Single study results
For parent‐reported scales (Analysis 1.14), there was no statistically significant difference between group‐based parent training and control at postintervention (SMD 0.49, 95% CI ‐0.08 to 1.05; 1 study, 50 participants).
1.14. Analysis.
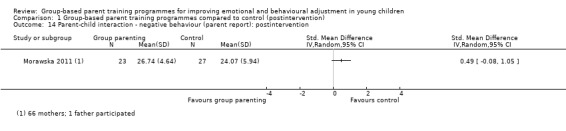
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 14 Parent‐child interaction ‐ negative behaviour (parent report): postintervention.
2.2 Parent‐child interaction: positive child behaviour (subscale)
For scales reported by independent observers (Analysis 1.15), there was moderate quality evidence that group‐based parent training was more effective than control at post‐treatment (SMD 0.48, 95% CI 0.17 to 0.79; 4 studies, 173 participants, Tau² = 0.00, I² = 0%; Table 1). The quality of evidence was downgraded one level for imprecision due to the low number of participants in the included studies. At short‐term follow‐up, we found no statistically significant difference (SMD 0.32, 95% CI ‐0.07 to 0.72; Tau² = 0.04, I² = 34%, 3 studies, 167 participants).
1.15. Analysis.
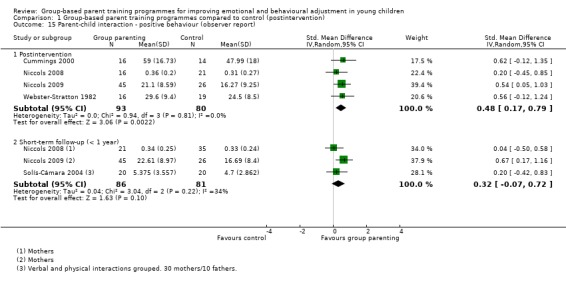
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 15 Parent‐child interaction ‐ positive behaviour (observer report).
Subgroup analyses
We conducted subgroup analyses to assess the impact of intervention duration and type of prevention on the results for the primary outcome reported by parents at postintervention.
Duration of intervention
For the five studies that reported on the primary outcome of emotional and behavioural problems, interventions lasted for more than eight weeks in two of the studies and less than eight weeks in two of the studies. As Tiedemann 1992 did not report on duration of intervention, we excluded this study from the analysis. The results show that group‐based parenting training programmes lasting more than eight weeks are more effective than controls (SMD ‐1.06, 95% CI ‐1.77 to ‐0.35; 2 studies, 45 participants, Tau² = 0.04, I² = 16%, Analysis 1.16 ), while there is no statistically significant difference between intervention and control groups in studies lasting less than eight weeks (SMD ‐0.40, 95% CI ‐1.03 to 0.24; 2 studies, 203 participants, Tau² = 0.15, I² = 70%). A test for between‐subgroup differences gave a test statistic Chi² = 1.87 with an associated P = 0.17, which suggests that there is no evidence for different intervention effects between the subgroups. We also conducted a meta‐regression to check if there is any difference between subgroups. The meta‐regression coefficient for the duration of intervention is estimated as ‐0.69 (95% CI from ‐2.92 to 1.53; P = 0.31), which confirms the results from testing the subgroup difference by using the Chi² test.
1.16. Analysis.
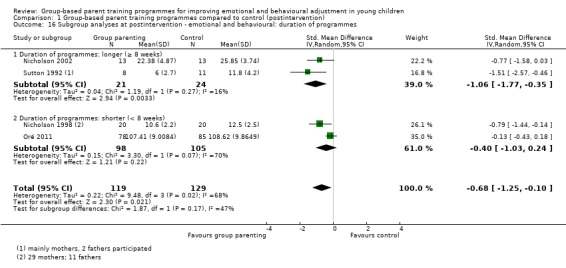
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 16 Subgroup analyses at postintervention ‐ emotional and behavioural: duration of programmes.
Type of prevention
Three of the five studies that reported on emotional and behavioural problems included primary prevention interventions, and two of the studies evaluated the effectiveness of secondary or tertiary interventions. The results show no statistically significant difference between group‐based parent training and controls for the primary preventive interventions (SMD ‐0.47, 95% CI ‐0.98 to 0.03; 229 participants, Tau² = 0.12, I² = 58%, Analysis 1.17 ), but do show that secondary/tertiary group‐based parent training was more effective than controls (SMD ‐1.38, 95% CI ‐2.00 to ‐0.75; 51 participants, Tau² = 0.00, I² = 0%). A test for between‐subgroup differences gave a test statistic Chi² = 4.89 with an associated P = 0.03. We also conducted a meta‐regression to check if there were any differences between subgroups. The coefficient for type of prevention is estimated as 0.94 (95% CI from ‐0.47 to 2.34; P = 0.125). Here we observed conflicting results from the Chi² test and the meta‐regression as to whether there is evidence for the subgroup differences. Since there are a low number of studies in each subgroup, both of these two methods may have low power and may potentially produce unreliable results. Therefore, we are not able to conclude whether there is a difference between subgroups, but report the SMD and its 95% CI for each subgroup in the above.
1.17. Analysis.
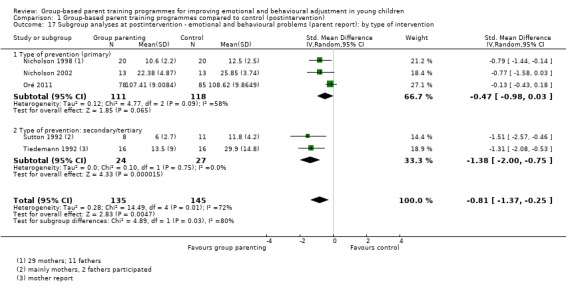
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 17 Subgroup analyses at postintervention ‐ emotional and behavioural problems (parent report): by type of intervention.
Sensitivity analyses
We conducted sensitivity analyses to assess the impact of study quality on the results for the primary outcome reported by parents at postintervention, measured by excluding quasi‐RCTs from the analyses. These findings were not maintained when the two quasi‐RCTs were excluded from the emotional and behavioural problems meta‐analysis (SMD ‐0.67, 95% CI ‐1.43 to 0.09; 3 studies, 221 participants, Tau² = 0.34, I² = 78%, see Analysis 1.18) compared to when quasi‐RCTs were included (SMD ‐0.81, 95% CI ‐1.37 to ‐0.25; 5 studies, 280 participants, Tau² = 0.28, I² = 72%, see Analysis 1.1).
1.18. Analysis.
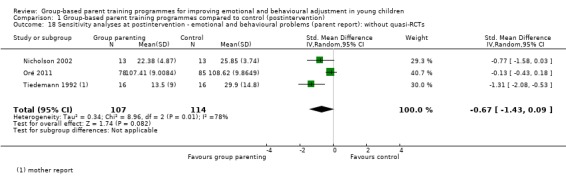
Comparison 1 Group‐based parent training programmes compared to control (postintervention), Outcome 18 Sensitivity analyses at postintervention ‐ emotional and behavioural problems (parent report): without quasi‐RCTs.
We assessed the impact of the assumed ICC value 0.03 for cluster‐randomised trials in further sensitivity analyses. We assumed a set of different ICC values (0, 0.02, 0.1).
There were no significant differences in internalising problems as rated by teachers between group‐based parent training and control at medium‐term follow‐up when we assumed ICC = 0.03 (SMD ‐0.15, 95% CI ‐0.33 to 0.02; 1 study, 504 participants, Analysis 1.9); ICC = 0.02 (SMD ‐0.16, 95% CI ‐0.34 to 0.01; 1 study, 504 participants, Analysis 3.4); or ICC 0.1 (SMD ‐0.11, 95% CI ‐0.29 to 0.06; 1 study, 504 participants, Analysis 4.4). However, when we assumed ICC = 0, we found significant differences in internalising problems as reported by teachers between group‐based parent training and control at medium‐term follow‐up (SMD ‐0.19, 95% CI ‐0.36 to ‐0.01, Analysis 2.4), indicating that, failing to control for the clustering effect provided an overly liberal estimate.
The results for the other comparisons involving cluster trials remain largely unchanged, with slightly narrower 95% CIs with a larger ICC value of 0.1 (Analysis 4.1; Analysis 4.2; Analysis 4.3; Analysis 4.5), and slightly wider 95% CIs with a smaller ICC value of 0 (Analysis 2.1; Analysis 2.2; Analysis 2.3; Analysis 2.5) and ICC value of 0.02 (Analysis 3.1; Analysis 3.2; Analysis 3.3; Analysis 3.5).
Discussion
Summary of main results
We identified 22 RCTs and two quasi‐RCTs evaluating the effectiveness of group‐based parenting programmes for improving the emotional and behavioural adjustment of children aged up to three years and 11 months (maximum mean age three years and 11 months).
For group‐based parenting programmes compared to control at postintervention, we found a significant reduction in total emotional and behavioural problems (standardised mean difference (SMD) ‐0.81, 95% confidence interval (CI) ‐1.37 to ‐0.25; 5 studies, 280 participants, low quality evidence) based on parent‐reported data, although the effect size was smaller (‐0.67) and the significance level was lost (95% CI ‐1.43 to 0.09) when two quasi‐RCTs were removed as part of a sensitivity analysis. Subscale scores for externalising problems showed a difference favouring the intervention group based on parent reports (SMD ‐0.23, 95% CI ‐0.46 to ‐0.01; 8 studies, 989 participants, moderate quality evidence). See Summary of findings table 1 for further details.
In terms of secondary outcomes, the results show a reduction in negative behaviour during parent‐child interaction as reported by observers (SMD ‐0.22, 95% CI ‐0.39 to ‐0.06; 7 studies, 941 participants, moderate quality evidence); and an increase in positive behaviour (SMD 0.48, 95% CI 0.17 to 0.79; 4 studies, 173 participants, moderate quality evidence).
Overall, these findings, which relate to the broad group of universal and at‐risk (targeted) children and parents, provide tentative support, based on parent‐reported data, that group‐based parenting programmes can improve the overall emotional and behavioural adjustment of children aged up to three years and 11 months immediately postintervention. However, the limited evidence available, suggests that these results diminish over time. Although this finding is consistent with that for older children, infancy and toddlerhood is a period of rapid development, and may highlight the need for top‐up sessions to enable parents to maintain the gains made.
The results of subgroup analyses suggest that there is no difference in terms of the effectiveness of longer (i.e. more than eight weeks) compared with briefer (i.e. seven weeks or less) programmes, and that they may not be effective when they are provided on a preventive basis (i.e. on a universal basis prior to the onset of problems). These results should, however, be treated with caution due to the small number of somewhat atypical programmes, in terms of length, that were included in these analyses. Furthermore, duration of intervention may be a proxy for approach or theoretical underpinning of the intervention, making it difficult to reach any firm conclusions about these results.
The included studies provide no evidence of harm in terms of deterioration in any of the key outcome measures. However, one qualitative study of parents’ experiences of the Webster‐Stratton programmes found that participants sometimes found it challenging to gain the support of partners in implementing the new techniques at home; to change their established habits and those of their partners; or to find the time to parent together, and incorporate the techniques into their already busy lives. The results of this study also suggest that a change in one parent’s approach to parenting may result in increased discrepancies in parenting techniques between the parent who attended the programme and the parent who did not, which may result in parental conflict (Mockford 2004).
Overall completeness and applicability of evidence
This review includes 22 RCTs and two quasi‐RCTs, and we obtained additional data from nine study authors (Hutchings 2007; Morawska 2011; Niccols 2008; Niccols 2009; Nicholson 2002; Perrin 2014; Sutton 1992; Tiedemann 1992; Webster‐Stratton 1982), which increased the completeness of the evidence substantially.
The parenting programmes included in this review were all behavioural or cognitive‐behavioural, and are, as such, similar in terms of content and methods (e.g. they all involve the use of modelling and behaviour rehearsal). Around half of the included interventions used videotape modelling but it was not possible to conduct subgroup analysis for this moderator variable due to lack of data. As was suggested above, there is also currently insufficient evidence regarding the moderating impact of programme duration or use prior to the onset of problems.
Some of the new studies included children with a mean age of three years and 11 months (i.e. 11 months longer than in the original review), but few included children under two years of age, and indeed, it seems likely that most of the cognitive‐behavioural therapy‐based parenting programmes included in this review, are not suitable for children less than 18 months of age.
Most of the included studies were conducted in developed countries (please see Description of studies for further details), and therefore these results should not be generalised more widely than this. Of the 12 studies reporting parents' ethnicity, a majority included predominantly Caucasian samples (please see Description of studies for further details). Although both mothers and fathers participated in the parenting programmes being evaluated in the included studies, mothers predominated in most studies. It is, therefore, unclear whether the results of this review are generalisable to non‐Caucasian samples or to fathers.
Quality of the evidence
Using the Grades of Recommendations, Assessment, Development, and Evaluation (GRADE) approach, we rated the overall quality of the body evidence from very low to moderate (please see Table 1). There were three main reasons for downgrading the quality of the evidence: inadequate randomisation or allocation procedures, statistical heterogeneity, and scarcity of data. Our sensitivity analyses removing quasi‐RCTs and cluster‐randomised trials had little or no impact on the results for the primary outcomes, thus providing some additional confidence in the robustness of the findings of the review.
Based on subgroup analyses, statistical heterogeneity appears to be explained in terms of heterogeneity in the interventions. Interventions of more than eight weeks' duration were more effective than control conditions, while those that lasted for eight weeks or less were not. Similarly, secondary or tertiary preventive interventions were effective, while primary prevention was not.
In two studies the dropout rate was in the region of 30% (Gross 1995; Hutchings 2007). In one of these studies, the parents who dropped out had significantly lower over‐reactive discipline scores than the parents who remained, indicating that they were less likely to use harsh and coercive discipline strategies. They were also more likely to be Latino. As this study did not report the attrition rate of participants by the group to which they were randomised, we used the initial participant numbers for each group at each time point in our analyses (Gross 2003), which may slightly decrease the treatment effect. In the second study, parents who dropped out all rated their children's behaviour as being less problematic than the parents who continued with the intervention.
While the Nicholson 2002 study reported a 10% dropout rate, it is not clear whether the parents who dropped out were included in the analyses or indeed from which of the groups they dropped out. Dropout rates, and the method by which they were dealt with, were unclear in the remaining included studies. Premature termination from parenting programmes among families with children referred for antisocial behaviour is associated with more severe conduct disorder symptoms and more delinquent behaviours; mothers reporting greater stress from their relations with the child, their own role functioning, and life events; and families being at greater socioeconomic disadvantage (Kazdin 1990).
Other studies have also identified individuals more likely to drop out as including those from a lower social class or a minority ethnic group (Farrington 1991; Holden 1990; Strain 1981), and those children with a greater number of presenting problems (Holden 1990). There are a number of points at which a parent may drop out of a parenting programme. Research has shown that failure to persist through the initial intake is associated with parental feelings of helplessness and negativity, and that failure to persist through the programme itself is associated with therapist inexperience (Frankel 1992). These problems surrounding the issue of attrition and dropout point to the importance of evaluating the results of trials on an intention‐to‐treat basis, which would limit bias arising from this source.
Potential biases in the review process
We are confident that our literature searches and screening process enabled us to identify all published RCTs and quasi‐RCTs on the effectiveness of group‐based parenting programmes for young children, as defined by our review, and published up to our most recent search date (July 2015). We performed systematic searches in 13 databases, including two trial registries, to identify both completed and ongoing trials. Two review authors independently screened potentially eligible studies for inclusion and assessed risk of bias in included studies. None of the review authors had any conflicts of interest.
Agreements and disagreements with other studies or reviews
There are a number of systematic reviews evaluating the effectiveness of parenting programmes, but this is the first to assess their effectiveness within this particular age group, and in terms of their level of prevention (e.g. primary versus secondary or tertiary).
The findings of this review are consistent with recent systematic reviews of the effectiveness of parenting programmes with older children. For instance, Dretzke 2009 found short‐term reductions in behavioural problems in children up to 18 years of age amongst those whose parents had participated in parenting programmes, and more recently, Furlong 2012 found that behavioural and cognitive‐behavioural, group‐based parenting interventions are effective and cost‐effective in improving child conduct problems in children aged three to 12 years, in addition to improved parental mental health and parenting skills in the short‐term.
Authors' conclusions
Implications for practice.
The results from this review provide tentative evidence of the short‐term effectiveness of group‐based parenting programmes, as assessed by parent reports of children's emotional and behavioural adjustment. These results apply to the broad group of universal and at‐risk (targeted) children and parents (Bradley 2003; Gross 1995; Little 2012; Tiedemann 1992).
There was a paucity of follow‐up data available regarding the extent to which the effects of these programmes are maintained over time and, in a number of cases, only data for the intervention group were available. The six studies that provided 12‐month or longer follow‐up data for both intervention and control groups had mixed results (Breitenstein 2012; Gross 1995; Gross 2003; Hiscock 2008; Perrin 2014; Sutton 1992), pointing to the need for further evaluation before it will be possible to reach any firm conclusions concerning the long‐term effectiveness of early parenting programmes for this age group.
The findings of this review provide some support for the use of group‐based parenting and, in particular, behavioural or cognitive‐behavioural programmes (i.e. six of the included studies evaluated the Incredible Years programme), to improve the emotional and behavioural adjustment of young children. The extent to which these results are maintained over time, however, is both limited and equivocal; it may be that during this period of rapid change in infant/toddler development, further input at a later date is required. More research to address this issue, as such, is needed.
There is currently insufficient evidence to reach any firm conclusions regarding the role of parenting programmes in the primary prevention of mental health problems.
Implications for research.
The current review suggests that parenting programmes may be effective in improving the emotional and behavioural adjustment of infants and toddlers. However, it has not been possible with the limited data available to provide conclusive evidence regarding the specific aspects of emotional and behavioural problems that are improved, or the extent to which the positive effects identified are maintained over time. Neither has it been possible to assess the role of parenting programmes in the primary prevention of mental health problems. The period between birth and three years of age is a more optimal time to be delivering and evaluating universal preventive interventions, and there is, as such, a need for large‐scale trials of the effectiveness of parenting programmes that are provided on a primary‐preventive population basis during the early years of a child's life. Such studies should evaluate interventions that combine the use of a universal setting and approach, with the ability to respond appropriately, in terms of intensity and content, to presenting need. Larger numbers of participants should be included to increase the external validity of the research, and measurement of a wider range of outcomes should be undertaken, including an assessment of aspects of parent‐child interaction in addition to aspects of the child's social and emotional functioning, for which there was limited evidence of effectiveness in the current review (e.g. internalising problems). Such studies would provide the basis for further long‐term follow‐up through childhood. Future research should also examine whether factors, such as temperament, influence the effectiveness of these programmes.
Future research should also address the comparative effectiveness of different models of working during the early years. For example, cognitive and behavioural parenting programmes, such as Incredible Years and Triple P Babies, should be compared to the use of more attachment‐based interventions such as Video‐Feedback to Promote Positive Parenting (VIPP) and Video Interaction Guidance (VIG).
The limited follow‐up data available point to the need for further research to assess to what extent the results of such programmes are maintained over time, and whether parents require further input at a later date. Evidence concerning the longer‐term effectiveness of such programmes (i.e. at school entry and later), is also required. None of the included studies provided data on cost or cost‐effectiveness and economic analyses should be included in all future studies.
Feedback
Comments about the review's Plain Language Summary, 23 May 2018
Summary
Comment
I think the plain language summary is pitched at far too high a reading level. Among the phrases that need rewording are "behavioural, cognitive‐behavioural or videotape modelling parenting programmes", "quasi‐methods of randomisation", and "Data from subscales showed moderate quality evidence of an improvement in externalising problems".
Also some of the sentences would be better if they were split into two, particularly this complex sentence: "We searched the scientific literature for all randomised controlled trials (RCTs, in which participants are randomly allocated to one of two or more treatment groups) and quasi‐RCTs (where participants are allocated to a treatment group using methods that are not strictly random e.g. date of birth), published up to July 2015; we found 24 trials (22 RCTs and two quasi‐RCTs) to include in the review."
Do you have any affiliation with or involvement in any organisation with a financial interest in the subject matter of your comment? I do not have any affiliation with or involvement in any organisation with a financial interest in the subject matter of my comment.
Melissa Raven (University of Adelaide)
Reply
We thank Dr Raven for her comments and have made changes in response. The Plain Language Summary has now been expanded and reads as follows.
Group‐based parent training programmes for improving emotional and behavioural adjustment in young children
Review question
We wanted to know if group‐based parent training programmes are helpful in improving emotional and behavioural adjustment in young children.
Background
Emotional and behavioural problems are common among infants and toddlers and, for many children, these problems continue into their early school and teenage years as well. Parenting practices play an important role in how emotional and behavioural problems in children develop. Parent training programmes aimed at parents of infants and toddlers might help to prevent such problems before they start, as well as treat them after they are established.
Study characteristics
We searched the scientific literature for all randomised controlled trials (RCTs) and quasi‐RCTs published up to July 2015. RCTs are studies in which people are randomly allocated to treatment groups. Quasi‐RCTs are studies in which people receive treatment based on methods that are not strictly random such as date of birth, or their hospital record number, and the results of quasi‐RCTs are generally considered less trustworthy than those of RCTs.
We found 24 trials (22 RCTs and two quasi‐RCTs) to include in our review. These studies included, in total, information from 3161 parents and their young children. Eight studies had been carried out in the USA, five in the UK, four in Canada, five in Australia, one in Mexico, and one in Peru.
All of the studies looked at behavioural, cognitive‐behavioural or videotape modelling parenting programmes. Behavioural programmes are aimed at helping parents develop methods that will reduce bad behaviour, usually with the use of techniques such as praise or rewards. It also aims to help parents set limits that make sense. Cognitive‐behavioral skills allow parents think about behaviour patterns and focus on solutions. Programmes can use a variety of techniques; for example, videotape modelling programmes enable parents to learn by watching videotaped films of other parents implementing some of the techniques described above.
Key results and quality of the evidence
Some of the studies we found included people chosen specially because they were ‘at risk’ of behavioural problems, while others included parents and children without any specific risks. When we put all of the studies together, overall, we found that group‐based parenting programmes can improve the emotional and behavioural development of young children, although the quality of the evidence was, on the whole, low. Furthermore, our findings were not convincing when we removed two studies that used quasi‐randomised methods.
Our findings also showed evidence of an improvement in externalising problems (these might include negative behaviours in children or young people that are directed towards the external environment such as anger, aggression or conflict with the law). However, the evidence for this, once again, came from studies that we rated as being of only moderate quality, and was only found for some parts of the outcome measure (known as a subscale).
Results from single studies that could not be combined with other studies and that were of poor quality, on the whole, showed no impact on children’s internalising problems (e.g. depression and anxiety). However, there was some improvement on one subscale of a measure that focused on children’s hyperactivity‐inattention and another subscale that focused on social skills.
There was moderate‐quality evidence that group‐based parenting programmes also improve the way in which parents and children interact, as measured by fewer negative behaviours.
Our reasons for rating the quality of the evidence as low or moderate included: inconsistency in the findings from different studies (different studies yielded different results); unclear risk of bias (where it was not possible for us to assess the ways in which the included studies might be biased due to inadequate information); and small numbers of parents in the included studies.
We believe more research is needed to be able to reach a firm conclusion about whether the effects we have found are short term only or whether they continue over time and therefore may be able to prevent future behavioural problems.
Contributors
Melissa Raven (email: melissa.raven@adelaide.edu.au), University of Adelaide Jane Barlow (email: jane.barlow@spi.ox.ac.uk), University of Oxford, on behalf of review co‐authors Hanna Bergman, Hege Kornør, Yinghui Wei and Cathy Bennett Jane Dennis (Feedback Editor); Joanne Duffield (Managing Editor) (Cochrane Developmental, Psychosocial and Learning Problems)
What's new
| Date | Event | Description |
|---|---|---|
| 16 October 2019 | Feedback has been incorporated | In this version of the review, we addressed comments recommending improvements to the Plain Language Summary. |
History
Protocol first published: Issue 4, 2001 Review first published: Issue 2, 2002
| Date | Event | Description |
|---|---|---|
| 11 November 2015 | New citation required and conclusions have changed | 16 new included studies |
| 7 July 2015 | New search has been performed | This review was updated following a new search in July 2014 and a top up search in July 2015 |
| 9 May 2012 | Amended | Line added to Acknowledgements section on behalf of CB |
| 24 September 2009 | New search has been performed | Updated with new included studies |
| 24 September 2009 | New citation required but conclusions have not changed | Updated, new authors |
| 25 June 2008 | Amended | Converted to new review format |
| 1 November 2003 | Amended | Also, in Issue 4, 2003, the result of the parent‐report meta‐analysis has been corrected from the previously published text from a non‐significant improvement of intervention to control of ‐0.29 (‐3.31 to ‐1.10) to a non‐significant improvement of intervention to control of ‐0.29 (‐0.55 to ‐0.02) |
| 31 July 2003 | Amended | Small errors in a previous version of this review were changed in Issue 3, 2003, to reflect incorrect setting of the WMD instead of the SMD statistic in the meta‐analyses and to align correct results in the meta‐view with incorrect ones in the text |
| 22 November 2002 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
This review is supported by Warwick Medical School, the Nottinghamshire National Health Service (NHS) Trust, the NHS Cochrane Collaboration Programme Grant, and the Regional Centre for Child and Adolescent Mental Health, Eastern and Southern Norway (RBUP). The views expressed in this review are those of the authors and not necessarily those of our sources of support.
We thank the Cochrane Developmental, Psychosocial and Learning Problems (CDPLP) Group for their support and encouragement in updating this review, and Margaret Anderson, Information Specialist at the CDPLP Group, for organising the search for this update.
We also thank the authors of the earlier version of this review who were not involved in this update ‐ Michael Ferriter, Hannah Jones, and Verena Roloff (PhD student, MRC Cambridge, Cambridge, UK) for her advice in the earlier version of the review on adjusting for the effects of cluster‐randomised trials; she provided advice, some explanatory text used in the review and sample calculations.
Cathy Bennett thanks the University of Bristol and Queen’s University Belfast for awarding visiting fellowships to support her in the academic activities of writing this review between 2008 and 2012.
We thank Karla Soares‐Weiser, Rosie Asher, Molly Grimes and Nicola Maayan at Enhance Reviews, Simon‐Peter Neumer and Karianne Thune Hammerstrøm at RBUP, and Philip Lobmaier at Oslo University Hospital for help with screening and data extraction.
Appendices
Appendix 1. Search strategies of previous versions of review
Search strategies used in 2000 version of this review
The following search terms were adapted for use in each of the databases listed below:
(parent* training or parent* program* or parent* education;
(toddler or infant or preschool or pre‐school or pre school or baby or babies); and
#1 and #2
List of databases
The Cochrane Library (including Cochrane Database of Systematic Reviews (CDSR), Cochrane Central Register of Controlled Trials (CENTRAL), and Database of Abstracts of Reviews of Effectiveness (DARE)).
Ovid MEDLINE (limited to journal articles);
Embase;
ASSIA ;
Biological Abstracts;
British Nursing Index;
CINAHL: Cumulative Index to Nursing and Allied Health Literature;
Dissertation Abstracts (International A, 1980 to 2001; Only theses available in the UK were retrieved in full text, due to the cost of accessing international dissertations);
ERIC;
National Research Register;
PsycINFO (limited to journal articles and books/chapters);
Sociological Abstracts;
Social Science Citation Index; and
Social Science Citation Index.
In addtion, the reference lists of relevant papers were examined to identify further relevant studies
Search strategies used in 2007/2008 update of this review
Cochrane Central Register of Controlled Trials (CENTRAL), part of the Cochrane Library and National Research Register (NRR)
#1 (parent* next training or parent* next program* or parent* next education or parent* next promotion) #2 (toddler* or infant* or preschool* or pre‐school* or baby or babies) #3 (#1 AND #2)
Ovid MEDLINE
1 (parent$ training or parent$ program or parent$ education or parent$ promotion).mp. [mp=title, original title, abstract, name of substance word, subject heading word] 2 (parent$ training or parent$ program or parent$ education or parent$ promotion).tw. 3 exp Infant/ 4 (baby or babies or toddler$ or infant$ or preschool$ or pre‐school$).tw. 5 3 or 4 6 2 and 5
Embase (OVID)
1 (parent$ training or parent$ program or parent$ education or parent$ promotion).mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name] 2 (parent$ training or parent$ program or parent$ education or parent$ promotion).tw. 3 exp Infant/ 4 (baby or babies or toddler$ or infant$ or preschool$ or pre‐school$).tw. 5 3 or 4 6 2 and 5
CINAHL: Cumulative Index to Nursing and Allied Health Literature (OVID)
1 (parent$ training or parent$ program or parent$ education or parent$ promotion).mp. [mp=title, subject heading word, abstract, instrumentation] 2 (parent$ training or parent$ program or parent$ education or parent$ promotion).tw. 3 exp Infant/ 4 (baby or babies or toddler$ or infant$ or preschool$ or pre‐school$).tw. 5 3 or 4 6 2 and 5
PsycINFO (SilverPlatter)
#5 (("Parent‐Training" in MJ,MN) or ((parent* training) or (parent* program*) or (parent* education) or (parent* promotion))) and (toddler* or infant* or preschool* or pre‐school* or baby or babies) #4 ("Parent‐Training" in MJ,MN) or ((parent* training) or (parent* program*) or (parent* education) or (parent* promotion)) #3 toddler* or infant* or preschool* or pre‐school* or baby or babies #2 "Parent‐Training" in MJ,MN #1 (parent* training) or (parent* program*) or (parent* education) or (parent* promotion)
Sociological Abstracts (CSA Illumina)
(toddler* or infant* or preschool* or pre‐school* or baby or babies) and (((parent* training) or (parent* program*) or (parent* education)) or (parent* promotion))
BIOSIS (Biological Abstracts) and Social Science Citation Index (SSCI) (Web of Knowledge)
#7 #6 AND #5 #6 TS=(toddler* or infant* or preschool* or pre‐school or baby or babies) #5 #4 OR #3 OR #2 OR #1 #4 TS=(parent* SAME promotion) #3 TS=(parent* SAME education) #2 TS=(parent* SAME program*) #1 TS=(parent* SAME training)
Dissertation Abstracts (Proquest Dissertations & Theses)
(parent* PRE/1 promotion) OR (parent* PRE/1 training) OR (parent* PRE/1 education) OR (parent* PRE/1 program*) AND (infant* OR baby OR babies OR toddler* OR pre‐school* OR preschool*)
ASSIA (CSA Illumina)
(toddler* or infant* or preschool* or pre‐school* or baby or babies) and (((parent* training) or (parent* program*) or (parent* education)) or (parent* promotion))
British Nursing Index
((parent* promotion OR parent* training OR parent* education OR parent* program*) AND (infant* OR baby OR babies OR toddler* OR pre‐school* OR preschool*))
Appendix 2. Initial search strategies for review update
Search dates for each database are reported in Appendix 4.
Cochrane Central Register of Controlled Trials (CENTRAL, part of the Cochrane Library)
#1 parent* next training #2 parent* next program* #3 parent* next education #4 parent* next promotion #5 infant*:TI,AB,KY #6 toddler*:TI,AB,KY #7 preschool*:TI,AB,KY #8 pre‐school*:TI,AB,KY #9 baby:TI,AB,KY #10 babies:TI,AB,KY #11 #1 OR #2 OR #3 OR #4 #12 #5 OR #6 OR #7 OR #8 OR #9 OR #10 #13 #11 AND #12 #14 2008 TO 2014:YR
Ovid MEDLINE
1. (parent$ training or parent$ program or parent$ education or parent$ promotion).mp. 2. (parent$ training or parent$ program or parent$ education or parent$ promotion).tw. 3. exp Infant/ 4. (baby or babies or toddler$ or infant$ or preschool$ or pre‐school$).tw. 5. 3 or 4 6. 2 and 5 7. (200710* or 200711* or 200712*).ed. 8. (2008* or 2009* or 2010* or 2011* or 2012* or 2013* or 2014*).ed. 9. 7 or 8 10. 6 and 9
Embase (OVID)
1. (parent$ training or parent$ program or parent$ education or parent$ promotion).mp. 2. (parent$ training or parent$ program or parent$ education or parent$ promotion).tw. 3. exp infant/ 4. (baby or babies or toddler$ or infant$ or preschool$ or pre‐school$).tw. 5. 3 or 4 6. 2 and 5 7. (2007* or 2008* or 2009* or 2010* or 2011* or 2012* or 2013* or 2014*).em. 8. 6 and 7
CINAHL: Cumulative Index to Nursing and Allied Health Literature (EBSCOhost)
S1 TX "parent* program*" S2 TX "parent* training" S3 TX "parent* education" S4 TX "parent* promotion*" S5 S1 OR S2 OR S3 OR S4 S6 (MH "Infant+") S7 TX baby S8 TX babies S9 TX toddler* S10 TX infant* S11 TX preschool* S12 TX pre‐school* S13 S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 S14 S5 AND S13 S15 EM 2007 S16 EM 2008 S17 EM 2009 S18 2010 S19 2011 S20 2012 S21 2013 S22 2014 S23 S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 S24 S14 AND S23
PsycINFO (OVID)
1. ("parent* training" or "parent* program*" or "parent* education" or "parent* promotion").tw. 2. exp Parent Training/ 3. (toddler* or infant* or preschool* or pre‐school* or baby or babies).tw. 4. 1 and 3 5. 2 and 3 6. 4 or 5 7. (200710* or 200711* or 200712*).up. 8. (2008* or 2009* or 2010* or 2011* or 2012* or 2013* or 2014*).up. 9. 7 or 8 10. 6 and 9
ERIC (Proquest)
("parent train*" OR "parent promot*" OR "parent educat*" OR "parent program*" OR "parent program*" OR "parent train*" OR "parent educat*" OR "parent promot*") AND (toddler* OR infant* OR preschool* OR preschool OR baby OR babies) [after 01 Nov 2007]
Sociological Abstracts (Proquest)
("parent train*" OR "parent promot*" OR "parent educat*" OR "parent program*" OR "parent program*" OR "parent train*" OR "parent educat*") AND (toddler* OR infant* OR preschool* OR preschool OR baby OR babies) [after 01 Nov 2007]
BIOSIS Citation Index (ISI Web of Knowledge)
TOPIC: ("parent* program*" OR "parent* training" OR "parent* education" OR "parent* promotion") AND TOPIC: (toddler* OR infant* OR preschool* OR pre‐school OR baby OR babies)
Timespan: 2008 to 2014. Indexes: BCI.
Dissertation Abstracts (ProQuest)
("parent train*" OR "parent promot*" OR "parent educat*" OR "parent program*" OR "parent program*" OR "parent train*" OR "parent educat*") AND (toddler* OR infant* OR preschool* OR preschool OR baby OR babies) [after 01 Nov 2007]
ClinicalTrials.gov
Search terms: (baby OR infant OR toddler OR preschool OR "pre‐school" OR babies OR infants) AND Intervention: ("parent training" OR "parent education" OR "parent program" OR "parental training" OR "parental education")
All dates; Intervention Studies; Recruitment status: all
Appendix 3. Revised search strategies for review update
Search dates for each database are reported in Appendix 4.
Cochrane Central Register of Controlled Trials (CENTRAL; part of the Cochrane Library)
#1(parent* near/1 component*) #2(parent* near/1 course*) #3(parent* near/1 education*) #4(parent* near/1 intervention*) #5(parent* near/1 group*) #6(parent* near/1 positive) #7(parent* near/1 program*) #8(parent* near/1 promotion) #9(parent* near/1 support*) #10(parent* near/1 training) #11"Incredible Years" #12"Early Head Start" #13"Sure Start" #14"Flying Start" #15"Webster Stratton" #16"Triple P" #17#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 #18(baby or babies or child* or toddler* or infant* or preschool* or pre‐school*) #19#17 and #18
Ovid MEDLINE
1 exp Infant/ 2 Child, Preschool/ 3 (baby or babies or child$ or toddler$ or infant$ or preschool$ or pre‐school$).tw. (1182507) 4 or/1‐3 5 (parent$ adj1 component$).tw. 6 (parent$ adj1 course$).tw. 7 (parent$ adj1 education$).tw. 8 (parent$ adj1 group$).tw. 9 (parent$ adj1 intervention$).tw. 10 (parent$ adj1 positive).tw. 11 (parent$ adj1 program$).tw. 12 (parent$ adj1 promotion).tw. 13 (parent$ adj1 support$).tw. 14 (parent$ adj1 training).tw. 15 Incredible Years.tw. 16 Early Head Start.tw. 17 Sure Start.tw. 18 Flying Start.tw. 19 Webster Stratton.tw. 20 Triple P.tw. 21 or/5‐20 22 randomized controlled trial.pt. 23 controlled clinical trial.pt. 24 randomi#ed.ab. 25 placebo$.ab. 26 drug therapy.fs. 27 randomly.ab. 28 trial.ab. 29 groups.ab. 30 or/22‐29 31 Program Evaluation/ 32 Treatment Outcome/ 33 30 or 31 or 32 34 exp animals/ not humans.sh. 35 33 not 34 36 4 and 21 and 35
Embase (OVID)
1 (parent$ adj1 component$).tw. 2 (parent$ adj1 course$).tw. 3 (parent$ adj1 education$).tw. 4 (parent$ adj1 group$).tw. 5 (parent$ adj1 intervention$).tw. 6 (parent$ adj1 positive).tw. 7 (parent$ adj1 program$).tw. 8 (parent$ adj1 promotion).tw. 9 (parent$ adj1 support$).tw. 10 (parent$ adj1 training).tw. 11 Incredible Years.tw. 12 Early Head Start.tw. 13 Sure Start.tw. 14 Flying Start.tw. 15 Webster Stratton.tw. 16 Triple P.tw. 17 or/1‐16 18 exp infant/ 19 toddler/ 20 pre‐school child/ 21 (baby or babies or child$ or toddler$ or infant$ or preschool$ or pre‐school$).tw. 22 or/18‐21 23 17 and 22 24 Randomized controlled trial/ 25 controlled clinical trial/ 26 Single blind procedure/ 27 Double blind procedure/ 28 triple blind procedure/ 29 Crossover procedure/ 30 (crossover or cross‐over).tw. 31 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 32 prospective.tw. 33 factorial$.tw. 34 random$.tw. 35 assign$.ab. 36 allocat$.tw. 37 volunteer$.ab. 38 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 39 treatment outcome/ 40 program evaluation/ or program efficacy/ or program impact/ or program sustainability/ 41 38 or 39 or 40 42 23 and 41
CINAHL: Cumulative Index to Nursing and Allied Health Literature (EBSCOhost)
S76 S60 AND S75 S75 S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 S74 (MH "Treatment Outcomes") S73 (MH "Program Evaluation") S72 TI ("prospective study" or "prospective research") or AB("prospective study" or "prospective research") S71 TI ("follow‐up study" or "follow‐up research") or AB ("follow‐upstudy" or "follow‐up research") S70 AB("cross over") S69 (MH "Crossover Design") S68 AB((tripl* N1 mask*) or (tripl* N1 blind*)) S67 AB((trebl* N1 mask*) or (trebl* N1 blind*)) S66 AB ((doubl* N1 mask*) or (doubl* N1 blind*)) S65 AB ((singl* N1 mask*) or(singl* N1 blind*)) S64 AB(trial) S63 AB(random*) S62 (MH "Random Assignment") S61 (MH "Clinical Trials+") S60 S55 AND S59 S59 S56 OR S57 OR S58 S58 (baby or babies or child* or toddler* or infant* or preschool* or pre‐school*) S57 AG preschool S56 AG infant S55 S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 S54 Triple P S53 Webster Stratton S52 Flying Start S51 Sure Start S50 Early Head Start S49 Incredible Years S48 (parent* N1 training) S47 (parent* N1 support*) S46 (parent* N1 promotion) S45 (parent* N1 program*) S44 (parent* N1 positive) S43 (parent* N1 intervention*) S42 (parent* N1 group*) S41 (parent* N1 education*) S40 (parent* N1 course*) S39 (parent* N1 component*) S38 S22 AND S37 S37 S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 S36 (MH "Treatment Outcomes") S35 (MH "Program Evaluation") S34 TI ("prospective study" ) or AB("prospective study") S33 TI ("follow‐up study" or "follow‐up research") or AB ("follow‐up study" or "follow‐up research") S32 AB("cross over" or "cross‐over" or crossover) S31 (MH "Crossover Design") S30 AB((tripl* N1 mask*) or (tripl* N1 blind*)) S29 AB((trebl* N1 mask*) or (trebl* N1 S28 AB ((doubl* N1 mask*) or (doubl* N1 blind*)) S27 AB ((singl* N1 mask*) or(singl* N1 blind*)) S26 AB(clinic N1 trial or control* N1 trial*) S25 AB(random* N1 allocat* or random* N1 assign*) S24 MH random assignment S23 (MH "Clinical Trials+") S22 S17 AND S21 S21 S18 OR S19 OR S20 S20 (baby or babies or child* or toddler* or infant* or preschool* or pre‐school*) S19 AG preschool S18 AG infant S17 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 S16 Triple P S15 Webster Stratton S14 Flying Start S13 Sure Start S12 Early Head Start S11 Incredible Years S10 (parent* N1 training) S9 (parent* N1 support*) S8 (parent* N1 promotion) S7 (parent* N1 program*) S6 (parent* N1 positive) S5 (parent* N1 intervention*) S4 (parent* N1 group*) S3 (parent* N1 education*) S2 (parent* N1 course*) S1 (parent* N1 component*)
PsycINFO (Ovid)
1 parent training/ 2 (parent$ adj1 component$).tw. 3 (parent$ adj1 course$).tw. 4 (parent$ adj1 education$).tw. 5 (parent$ adj1 group$).tw. 6 (parent$ adj1 intervention$).tw. 7 (parent$ adj1 positive).tw. 8 (parent$ adj1 program$).tw. 9 (parent$ adj1 promotion).tw. 10 (parent$ adj1 support$).tw. 11 (parent$ adj1 training).tw. 12 Incredible Years.tw. 13 Early Head Start.tw. 14 Sure Start.tw. 15 Flying Start.tw. 16 Webster Stratton.tw. 17 Triple P.tw. 18 or/1‐17 19 (infancy 2 23 mo or neonatal birth 1 mo or preschool age 2 5 yrs).ag. (134493) 20 (baby or babies or child$ or toddler$ or infant$ or preschool$ or pre‐school$).tw. (558507) 21 19 or 20 22 18 and 21 23 clinical trials/ 24 random$.tw. 25 ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$ or mask$)).tw. 26 (crossover$ or "cross over$").tw. 27 trial$.tw. 28 group$.ab. 29 exp program evaluation/ 30 treatment effectiveness evaluation/ 31 treatment outcome clinical trial.md. 32 ((effectiveness or evaluat$) adj2 (stud$ or research$)).tw. 33 (allocat$ or assign$).tw. 34 placebo.ab. 35 23 or 24 or 25 or 26 or 27 or 29 or 30 or 31 or 32 or 33 or 34 36 22 and 35 37 remove duplicates from 36
ERIC
ERIC (Proquest), searched in July 2014
((SU.EXACT("Toddlers") OR SU.EXACT("Infants") OR SU.EXACT("Preschool Children") OR (baby OR babies OR infant* OR toddler* OR child* OR preschool* OR pre‐school*)) AND ("parent* training" OR "parent* intervention*" OR "parent* program*" OR "parent* support" OR "positive parenting" OR "parent* component*" OR "parent* course*" OR "parent* group*" OR "parent* education" OR ("Early Head Start" OR "Incredible Years" OR "Sure Start" OR "Flying Start" OR "Webster Stratton" OR "Triple P"))) AND (SU.EXACT("Randomised Experiments") OR random* OR control* OR SU.EXACT("Control Groups") OR SU.EXACT("Experimental Groups") OR SU.EXACT("Programme Effectiveness") OR SU.EXACT("Programme Evaluation") OR SU.EXACT("Programme Validation") OR SU.EXACT("Outcomes of Treatment"))
ERIC (EBSCOhost), searched in July 2015
S11 S3 AND S6 AND S10 S10 S8 OR S9 36 S9 random* OR control* or group* S8 (DE "Control Groups" OR DE "Experimental Groups" OR DE "Program Effectiveness" OR DE "Evaluation Research" OR DE "Program Evaluation" OR DE "Program Validation" OR DE "Outcomes of Treatment" S7 S3 AND S6 S6 S4 OR S5 S5 ("Early Head Start" OR "Incredible Years" OR "Sure Start" OR "Flying Start" OR "Webster Stratton" OR "Triple P") S4 "parent* training" OR "parent* intervention*" OR "parent* program*" OR "parent* support" OR "positive parenting" OR "parent* component*" OR "parent* course*" OR "parent* group*" OR "parent* promotion" S3 S1 OR S2 S2 (baby or babies or infant* or toddler* or child* or preschool* or pre‐school*) S1 DE "Toddlers" OR DE "Infants" OR DE "Preschool Children"
Sociological Abstracts (Proquest)
Searched for: (SU.EXACT("Infants") OR SU.EXACT("Preschool Children") OR (baby OR babies OR infant* OR toddler* OR child* OR preschool* OR pre‐school*)) AND (SU.EXACT("Parent Training") OR (parent* NEAR/1 component*) OR (parent* NEAR/1 course*) OR (parent* NEAR/1 intervention*) OR (parent* NEAR/1 train*) OR (parent* NEAR/1 program*) OR (parent* NEAR/1 support*) OR (positive NEAR/1 parent*) OR (parent* NEAR/1 education*) OR ("Early Head Start" OR "Incredible Years" OR "Sure Start" OR "Flying Start" OR "Webster Stratton" OR "Triple P")) AND (SU.EXACT("Treatment Outcomes") OR SU.EXACT("Program Evaluation") OR random* OR control* OR trial*)
Social Sciences Citation Index (SSCI; Web of Science)
#5 #4 AND #3 DocType=All document types; Language=All languages; #4 TS=(random* ) DocType=All document types; Language=All languages; #3 #2 AND #1 DocType=All document types; Language=All languages; #2 TS=(infant* or child* or baby or babies or toddler* or preschool* or pre‐school*) DocType=All document types; Language=All languages; #1 ts= ("parent* education*" or "parent* training" OR "parent* intervention*" OR "parent* program*" ) DocType=All document types; Language=All languages;
Conference Proceedings Citation Index ‐ Social Science & Humanities (CPCI ‐ SS&H; Web of Science)
#5 #4 AND #3 DocType=All document types; Language=All languages; #4 TS=(random* ) DocType=All document types; Language=All languages; #3 #2 AND #1 DocType=All document types; Language=All languages; #2 TS=(infant* or child* or baby or babies or toddler* or preschool* or pre‐school*) DocType=All document types; Language=All languages; #1 ts= ("parent* education*" or "parent* training" OR "parent* intervention*" OR "parent* program*" ) DocType=All document types; Language=All languages;
Cochrane Database of Systematic Reviews (CDSR; part of the Cochrane Library)
#1(parent* near/1 component*):ti,ab #2(parent* near/1 course*):ti,ab #3(parent* near/1 education*):ti,ab #4(parent* near/1 intervention*):ti,ab #5(parent* near/1 group*):ti,ab #6(parent* near/1 positive):ti,ab #7(parent* near/1 program*):ti,ab #8(parent* near/1 promotion):ti,ab #9(parent* near/1 support*):ti,ab #10(parent* near/1 training):ti,ab #11"Incredible Years":ti,ab #12"Early Head Start":ti,ab #13"Sure Start":ti,ab #14"Flying Start":ti,ab #15"Webster Stratton":ti,ab #16"Triple P":ti,ab #17#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 #18(baby or babies or child* or toddler* or infant* or preschool* or pre‐school*):ti,ab #19#17 and #18
Database of Abstracts of Reviews of Effects (DARE; part of the Cochrane Library)
#1(parent* near/1 component*):ti,ab #2(parent* near/1 course*):ti,ab #3(parent* near/1 education*):ti,ab #4(parent* near/1 intervention*):ti,ab #5(parent* near/1 group*):ti,ab #6(parent* near/1 positive):ti,ab #7(parent* near/1 program*):ti,ab #8(parent* near/1 promotion):ti,ab #9(parent* near/1 support*):ti,ab #10(parent* near/1 training):ti,ab #11"Incredible Years":ti,ab #12"Early Head Start":ti,ab #13"Sure Start":ti,ab #14"Flying Start":ti,ab #15"Webster Stratton":ti,ab #16"Triple P":ti,ab #17#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 #18(baby or babies or child* or toddler* or infant* or preschool* or pre‐school*):ti,ab #19#17 and #18
BIOSIS Previews (ISI Web of Knowledge)
TOPIC: ("parent* program*" OR "parent* training" OR "parent* education" OR "parent* promotion") AND TOPIC: (toddler* OR infant* OR preschool* OR pre‐school OR baby OR babies)
Timespan: 2014 to 2015. Indexes: BIOSIS Previews.
Dissertations & Theses (ProQuest)
("parent train*" OR "parent promot*" OR "parent educat*" OR "parent program*" OR "parent program*" OR "parent train*" OR "parent educat*") AND (toddler* OR infant* OR preschool* OR preschool OR baby OR babies) [after 01 Jan 2014]
World Health Organisation International Clinical Trials Registry Platform (WHO ICTRP)
Intervention: parent training OR parenting training OR parental training OR parent intervention OR parenting intervention OR parental intervention OR parent program* OR parental program* OR parenting program* OR parent education OR parenting education OR parental education
Clinical Trials in Children selected Recruitment status = all
No date limits
ClinicalTrials.gov
Advanced search: Interventional Studies | parent training | Child (278 records) No date limits
Appendix 4. Record of searches for review update
| Database | Search date | Date range | Number of records |
| CENTRAL (part of the Cochrane Library), which includes the Cochrane Developmental, Psychosocial and Learning Problems Group Specialised Register | 8 June 2014 | Issue 6 of 12 June 2014 | 240 |
| 24 July 2014 | Issue 6 of 12 June 2014 | 1178 | |
| 29 July 2015 | Issue 6 of 12 June 2015 | 143 | |
| Ovid MEDLINE | 8 June 2014 | 1946 to Week 1 2014 | 595 |
| 23 July 2014 | 1946 to July Week 2 2014 | 2668 | |
| 29 July 2015 | 1946 to July Week 3 2015 | 246 | |
| Embase (OVID) | 8 June 2014 | 1974 to Week 1 2014 | 735 |
| 23 July 2014 | 1980 to Week 29 2014 | 2214 | |
| 29 July 2015 | 1946 to July Week 3 2015 | 281 | |
| CINAHL Plus (EBSCOhost) | 8 June 2014 | 1938 to current | 1352 |
| 24 July 2014 | 1938 to current | 1778 | |
| 30 July 2015 | 1938 to current | 156 | |
| PsycINFO (OVID) | 8 June 2014 | 1806 to Week 1 2014 | 558 |
| 24 July 2014 | 1967 to July Week 3 2014 | 2354 | |
| 30 July 2015 | 1967 to July Week 3 2015 | 305 | |
| ERIC (Proquest) | 8 June 2014 | 1966 to current | 180 |
| 24 July 2014 | 1966 to current | 636 | |
| ERIC (EBSCOhost) | 30 July 2015 | 1966‐current | 58 |
| Sociological Abstracts and ASSIA (Proquest) | 8 June 2014 | 1952 to current | 87 |
| Sociological Abstracts ( Proquest) | 24 July 2014 | 1952 to current | 588 |
| 30 July 2015 | 1952 to current | 58 | |
| Social Sciences Citation Index/Conference Paper Citation Index ‐ Social Science & Humanities (Web of Science) | 24 July 2014 | 1970 to current / 1990 to current | 929 |
| 30 July 2015 | 1970 to 29 July 2015 / 1990 to 29 July 2015 | 172 | |
| Cochrane Database of Systematic Reviews (CDSR, part of the Cochrane Library) | 24 July 2014 | Issue 7 of 12 July 2014 | 16 |
| 29 July 2015 | Issue 7 of 12 July 2015 | 1 | |
| Database of Abstracts of Reviews of Effects (DARE, part of The Cochrane Libaray) | 24 July 2014 | Issue 2 of 4 April 2014 | 19 |
| 29 July 2015 | Issue 2 of 4 April 2015 | 4 | |
| BIOSIS Citation Index (Web of Knowledge) | 8 June 2014 | 1926 to current | 253 |
| BIOSIS Previews (Web of Knowledge) | 2 October 2015 | 1926 to current | 58 |
| Dissertation Abstracts (Proquest) | 8 June 2014 | all available years | 2 |
| Dissertations & Theses (Proquest) | 2 October 2015 | all available years | 26 |
| WHO ICTRP | 25 July 2014 | all available years | 123 |
| 31 July 2015 | all available years de‐duplicated against previous records | 27 | |
| ClinicalTrials.gov | 8 June 2014 | all available years | 38 |
| 25 July 2014 | all available years | 278 | |
| 31 July 2015 | Trials added 1 July 2014 to 31 July 2015 | 74 | |
| Total | 18,430 | ||
| Total after removal of duplicates | 12,051 | ||
Footnotes
ASSIA: Applied Social Sciences Index and Abstracts. CENTRAL: The Cochrane Central Register of Controlled Trials. CINAHL: Cumulative Index to Nursing and Allied Health Literature. ERIC: Education Resources Information Center. WHO ICTRP: World Health Organisation International Clinical Trials Registry.
Appendix 5. Eligibility form
Study eligibility form
Group‐based parent training programmes for improving emotional and behavioural adjustment in young children (D0026)
Study ID: Reviewer: Final decision:
Answer all questions
| Type of study | ||
| Q1. Is the study described as randomised or quasi‐randomised? | Yes Unclear No |
Go to next question Go to next question Exclude |
| Participants in the study | ||
| Q2. Were the participants parents of 0 to 3 year‐old children? OR Were the participants parents of children who were slightly older than birth to 3 years (up to 5 years) of age, providing that the mean age of all children was under 3 years and 11 months? |
Yes Unclear No |
Go to next question Go to next question Exclude |
| Q3. Were the participants parents of children with specific condition other than emotional and behavioural problems (e.g. physical disabilities; autism, etc.)? | Yes Unclear No |
Exclude Go to next question Go to next question |
| Design of the study | ||
| Q4. Did the study contain a control group which was either: a waiting list control, or a no‐treatment control, or a placebo control, or a TAU (or a normal service provision) control |
Yes Unclear No |
Go to next question Go to next question Exclude |
| Interventions in the study | ||
| Q5. Was the intervention group‐based? N.B. Any theoretical framework including Behavioural, Family System, Psychodynamic, etc. is acceptable |
Yes Unclear No |
Go to next question Go to next question Exclude |
| Q6. Did the intervention focus on the improvement, or prevention of emotional and behavioural problems? | Yes Unclear No |
Go to next question Go to next question Exclude |
| Outcomes | ||
| Q7. Are the following outcomes reported? Emotional and behavioural adjustment (such as successfully decreased: tantrums, self destructive behaviours, verbal aggression, excessive crying, thumb‐sucking, sleep problems, etc.) |
Yes Unclear No |
Go to next question Go to next question Exclude |
| Q8. Did study include at least one standardised instrument measuring the above outcomes? | Yes Unclear No |
Go to next question Go to next question Exclude |
| Comments/other reasons for exclusion | ||
TAU: treatment‐as‐usual
Data and analyses
Comparison 1. Group‐based parent training programmes compared to control (postintervention).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Emotional and behavioural problems (parent report) | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Postintervention | 5 | 280 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.37, ‐0.25] |
| 1.2 Short‐term follow‐up (< 1 year) | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.88 [‐2.73, ‐1.03] |
| 2 Emotional and behavioural problems (teacher report): postintervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3 Externalising problems (parent report) | 12 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Postintervention | 8 | 989 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.46, ‐0.01] |
| 3.2 Short‐term follow‐up (< 1 year) | 5 | 566 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.59, ‐0.17] |
| 3.3 Medium‐term follow‐up (1 to 3 years) | 5 | 1400 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.21, ‐0.00] |
| 4 Externalising problems (teacher report) | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Postintervention | 3 | 664 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.62, 0.14] |
| 4.2 Medium‐term follow‐up (1 to 3 years) | 2 | 638 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.65, 0.08] |
| 5 Externalising problems (observer report): short‐term follow‐up (< 1 year) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Externalising problems subscales: hyperactivity‐inattention (parent report) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 6.1 Postintervention | 1 | 19 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.34 [‐2.37, ‐0.31] |
| 6.2 Short‐term follow‐up (< 1 year) | 3 | 488 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.54, 0.07] |
| 7 Externalising problems subscales ‐ hyperactivity‐inattention (observer report): short‐term follow‐up (< 1 year) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8 Internalising problems (parent report) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 Postintervention | 1 | 73 | Std. Mean Difference (IV, Random, 95% CI) | 0.34 [‐0.12, 0.81] |
| 8.2 Short‐term follow‐up (< 1 year) | 2 | 242 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.96, 0.34] |
| 8.3 Medium‐term follow‐up (1 to 3 years) | 1 | 589 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.29, 0.03] |
| 9 Internalising problems (teacher report) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 Postintervention | 1 | 504 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.24, 0.11] |
| 9.2 Medium‐term follow‐up (1 to 3 years) | 1 | 504 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.33, 0.02] |
| 10 Internalising problems (observer report): short‐term follow‐up (< 1 year) | 2 | 295 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [1.00, 0.91] |
| 11 Social skills (parent report) | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 11.1 Postintervention | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | 3.59 [2.42, 4.76] |
| 11.2 Short‐term follow‐up (< 1 year) | 3 | 233 | Std. Mean Difference (IV, Random, 95% CI) | 1.33 [‐0.15, 2.81] |
| 12 Social skills (observer report) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Postintervention | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | 0.64 [‐0.07, 1.35] |
| 12.2 Short‐term follow‐up (< 1 year) | 1 | 32 | Std. Mean Difference (IV, Random, 95% CI) | 0.98 [0.24, 1.71] |
| 13 Parent‐child interaction ‐ negative behaviour (observer report) | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 13.1 Postintervention | 7 | 941 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.39, ‐0.06] |
| 13.2 Short‐term follow‐up (< 1 year) | 5 | 348 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.43, 0.02] |
| 13.3 Medium‐term follow‐up (1 to 3 years) | 4 | 811 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.17, 0.11] |
| 14 Parent‐child interaction ‐ negative behaviour (parent report): postintervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 15 Parent‐child interaction ‐ positive behaviour (observer report) | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 15.1 Postintervention | 4 | 173 | Std. Mean Difference (IV, Random, 95% CI) | 0.48 [0.17, 0.79] |
| 15.2 Short‐term follow‐up (< 1 year) | 3 | 167 | Std. Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.07, 0.72] |
| 16 Subgroup analyses at postintervention ‐ emotional and behavioural: duration of programmes | 4 | 248 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐1.25, ‐0.10] |
| 16.1 Duration of programmes: longer (≥ 8 weeks) | 2 | 45 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.06 [‐1.77, ‐0.35] |
| 16.2 Duration of programmes: shorter (< 8 weeks) | 2 | 203 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐1.03, 0.24] |
| 17 Subgroup analyses at postintervention ‐ emotional and behavioural problems (parent report): by type of intervention | 5 | 280 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.37, ‐0.25] |
| 17.1 Type of prevention (primary) | 3 | 229 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.98, 0.03] |
| 17.2 Type of prevention: secondary/tertiary | 2 | 51 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.38 [‐2.00, ‐0.75] |
| 18 Sensitivity analyses at postintervention ‐ emotional and behavioural problems (parent report): without quasi‐RCTs | 3 | 221 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.43, 0.09] |
Comparison 2. Sensitivity analysis 1 (ICC = 0).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Externalising problems (parent report) | 11 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Postintervention | 8 | 989 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.46, ‐0.01] |
| 1.2 Short‐term follow‐up (< 1 year) | 4 | 481 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.60, ‐0.09] |
| 1.3 Medium‐term follow‐up (1 to 3 years) | 5 | 1400 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.22, ‐0.01] |
| 2 Externalising problems (teacher report) | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Postintervention | 3 | 664 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.75, 0.14] |
| 2.2 Medium‐term follow‐up (1 to 3 years) | 2 | 638 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐0.87, 0.10] |
| 3 Externalising problems subscales ‐ hyperactivity‐inattention (parent report) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Postintervention | 1 | 19 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.34 [‐2.37, ‐0.31] |
| 3.2 Short‐term follow‐up (< 1 year) | 3 | 488 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.54, 0.07] |
| 4 Internalising problems (teacher report) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Postintervention | 1 | 504 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.26, 0.09] |
| 4.2 Medium‐term follow‐up (1 to 3 years) | 1 | 504 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.36, ‐0.01] |
| 5 Parent‐child interaction ‐ negative behaviour (observer report) | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Postintervention | 7 | 941 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.46, ‐0.08] |
| 5.2 Short‐term follow‐up (< 1 year) | 5 | 348 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.43, 0.02] |
| 5.3 Medium‐term follow‐up (1 to 3 years) | 4 | 811 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.17, 0.11] |
Comparison 3. Sensitivity analysis 2 (ICC = 0.02).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Externalising problems (parent report) | 11 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Postintervention | 8 | 989 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.46, ‐0.01] |
| 1.2 Short‐term follow‐up (< 1 year) | 4 | 481 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.60, ‐0.09] |
| 1.3 Medium‐term follow‐up (1 to 3 years) | 5 | 1400 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.22, ‐0.00] |
| 2 Externalising problems (teacher report) | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Postintervention | 3 | 664 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.66, 0.14] |
| 2.2 Medium‐term follow‐up (1 to 3 years) | 2 | 638 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.83, 0.12] |
| 3 Externalising problems subscales ‐ hyperactivity‐inattention (parent report) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Postintervention | 1 | 19 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.34 [‐2.37, ‐0.31] |
| 3.2 Short‐term follow‐up (< 1 year) | 3 | 488 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.54, 0.07] |
| 4 Internalising problems (teacher report) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Postintervention | 1 | 504 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.25, 0.10] |
| 4.2 Medium‐term follow‐up (1 to 3 years) | 1 | 504 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.34, 0.01] |
| 5 Parent‐child interaction ‐ negative behaviour (observer report) | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Postintervention | 7 | 941 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.43, ‐0.07] |
| 5.2 Short‐term follow‐up (< 1 year) | 5 | 348 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.43, 0.02] |
| 5.3 Medium‐term follow‐up (1 to 3 years) | 4 | 811 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.16, 0.11] |
Comparison 4. Sensitivity analysis 3 (ICC = 0.1).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Externalising problems (parent report) | 11 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Postintervention | 8 | 989 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.46, 0.00] |
| 1.2 Short‐term follow‐up (< 1 year) | 4 | 481 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.60, ‐0.09] |
| 1.3 Medium‐term follow‐up (1 to 3 years) | 5 | 1400 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.21, 0.00] |
| 2 Externalising problems (teacher report) | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Postintervention | 3 | 664 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.59, 0.13] |
| 2.2 Medium‐term follow‐up (1 to 3 years) | 2 | 638 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.43, 0.06] |
| 3 Externalising problems subscales ‐ hyperactivity‐inattention (parent report) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Postintervention | 1 | 19 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.34 [‐2.37, ‐0.31] |
| 3.2 Short‐term follow‐up (< 1 year) | 3 | 488 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.54, 0.07] |
| 4 Internalising problems (teacher report) | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Postintervention | 1 | 504 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.22, 0.12] |
| 4.2 Medium‐term follow‐up (1 to 3 years) | 1 | 504 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.29, 0.06] |
| 5 Parent‐child interaction ‐ negative behaviour (observer report) | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Postintervention | 7 | 941 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.33, ‐0.03] |
| 5.2 Short‐term follow‐up (< 1 year) | 5 | 348 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.43, 0.02] |
| 5.3 Medium‐term follow‐up (1 to 3 years) | 4 | 811 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.16, 0.11] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bradley 2003.
| Methods |
Design: Randomised controlled trial
Unit of randomisation: Individual caregiver
Follow‐up: 3 months Study dates: 1998 to 1999 |
|
| Participants |
Participants: Parents (gender not reported) who were experiencing problems managing the behaviour of their children Mean age of child: Intervention 3.76 (SD 0.66), control 3.84 (SD 0.57) Mean age of parent: Intervention 35.20 (SD 5.51), control 35.88 (SD 5.73) Ethnicity: Not reported Number randomised: 198 (intervention 89, control 109) Country & setting: Canada; single‐site; recruited from community settings; intervention delivered in community agencies Eligibility criteria: Not specified |
|
| Interventions |
2 conditions: Group‐based parent training (1‐2‐3 Magic); wait‐list control
Duration of intervention: 3 (2 hours) sessions in 3 weeks + 1 booster 4 weeks after completion of the intervention Therapist training: Facilitators trained in problem solving |
|
| Outcomes |
Externalising problems subscale ‐ hyperactivity/inattention: Preschool Behaviour Questionnaire ‐ hyper/distractible, as completed by parents (total score and persistent/unstoppable subscale data not added) Internalising problems: Preschool Characteristics Questionnaire ‐ negative adaptation and affect, as completed by parents (difficulties subscale data not added) Timing of outcomes: Outcomes reported for 3 months follow‐up Secondary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes |
Level of prevention: Secondary/tertiary Funding: The Counselling Foundation of Canada |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The study reported that participants were randomly assigned, but no further details were reported for a judgement to be made. We requested clarification from study investigators, but no further information was available at the time this review was prepared |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficiently for a judgement to be made. We requested clarification from study investigators, but no further information was available at the time this review was prepared |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study meant personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | There were no independent observer‐rated outcomes |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 8/89 (9%) of intervention group members and 16/109 (15%) of control group members did not complete post‐test assessments. Reasons for dropping out were not reported. The study reports that intention‐to‐treat analysis was planned, but it seems only completers were analysed |
| Selective reporting (reporting bias) | High risk | The published report included all expected outcomes, including those that were prespecified. However, only statistically significant results were fully reported for the Preschool Behaviour Questionnaire scales (hostile/aggressive and anxious subscales were not reported) |
| Other bias | Low risk | The study appeared to be free of other sources of bias |
Breitenstein 2012.
| Methods |
Design: 2 cluster‐randomised controlled trials
Unit of randomisation: Childcare centre
Follow‐up: 1 year Study dates: 2002 to 2011 |
|
| Participants |
Participants: Parent or legal guardian (452 mothers, 33 fathers, 17 legal guardians for those analysed and self reporting as African American or Latino (93%)) of children, enrolled in 1 of 7 participating Chicago day care centres serving low‐income families Mean age of parents: Not reported for full sample; 30.9 (SD 7.53; range: NR) years for those analysed and self reporting as African American or Latino (93%) Mean age of child: 2.81 (SD 0.73; range 2 to 4) years; 230 (46%) girls and 274 (54%) boys Ethnicity: Not reported for full sample; 291 African American, 213 Latino for those analysed Number randomised: 15 centres (2185 families; 1155 intervention; 1031 control) Country & setting: USA; multi‐site; recruited from community settings; intervention delivered in preschool/day care centre Eligibility criteria: The centre (a) had > 90% of its families eligible to receive low‐income childcare subsidies, (b) was licensed by the state, (c) enrolled ≥ 60 children aged between 2 and 4, (d) had on‐site space to run Chicago Parent Program groups, and (e) had approval from the director to have centre randomised |
|
| Interventions | 2 conditions: Group‐based parent training (Chicago Parent Program); wait‐list control Duration of intervention: 11 sessions over 11 weeks plus a booster 2 months after the sessions Therapist training: Facilitators trained and supervised | |
| Outcomes |
Externalising problems: Eyberg Child Behaviour Inventory ‐ intensity, parent‐reported; Caregiver‐Teacher Rating Form ‐ externalising, as reported by teacher Internalising problems: Caregiver‐Teacher Rating Form ‐ internalising, as reported by teacher Secondary outcomes: Parent‐child interaction as measured by the Dyadic Parent‐Child Coding System Revised, observer‐rated Timing of outcomes: Outcomes reported for postintervention and 1‐year follow‐up Adverse events: None specified |
|
| Notes | Only participants self reporting as African American or Latino (93% of participants with data) were included in the analyses Level of prevention: Primary prevention Funding: National Institute for Nursing Research, Grant No. R01 NR004085 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The study reported that day centres "were randomly assigned", but no further details were reported for a judgement to be made. We requested clarification from study investigators, but no further information was available at the time this review was prepared |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficiently for a judgement to be made. We requested clarification from study investigators, but no further information was available at the time this review was prepared |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | Observers were blinded to intervention condition |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 44/330 (13%) participants enrolled in the intervention group and 31/283 (11%) enrolled in the control group left the study early. Reasons for leaving early were reported |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | High risk | Data for two trials were merged and only African American and Latino participants were included in the analyses. In addition, this was a cluster‐randomised trial and the study authors reported their means and SDs based on descriptive statistics, but did not report ICC |
Cummings 2000.
| Methods |
Design: Cross‐over randomised controlled trial
Unit of randomisation: Individual family
Follow‐up: 4 weeks Study dates: 1999 |
|
| Participants |
Participants: Parents (32 mothers; 5 fathers) and other caregivers of children with negative behaviour Mean age of parents: Not reported Age of child: 2 and 3 years (mean, SD, range: NR); 17 boys and 11 girls Ethnicity: 54% Black, 46% White Number randomised: 37 (intervention 21; control 16)* Country & setting: USA; single‐site; recruited from community settings; intervention delivered in health centre or at drug treatment centre Eligibility criteria: Not specified |
|
| Interventions |
Two conditions: Group‐based parent training (not specified); wait‐list control
Duration of intervention: 6 (1.5 hours) sessions over 3 weeks Therapist training: Researcher |
|
| Outcomes |
Secondary outcomes: Parent‐child interaction as measured by the Dyadic Parent‐Child Coding System, reported by observing clinical staff Timing of outcome: postintervention and at four‐week follow‐up Primary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes | *Six participants who were initially in the wait‐list control group were admitted in subsequent cohorts and were included in the analysis twice over: “21 parents were assigned to the treatment group (six also had been in the wait list control group), and 16 were assigned to the Wait List Control group” (p 41) Level of prevention: Secondary or tertiary Funding: no information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | A random sequence was generated by flipping a coin. Participants who were initially assigned to the wait‐list control group were offered the opportunity to participate in the intervention group after the first training series. Those who wanted to participate were placed in the intervention group in the next training series, while the new participants were randomly placed in either the intervention or wait‐list control group (see p 41 and Table 4, p 43). Participants who were initially randomly assigned to the wait‐list control group (n = 6) were not randomly assigned to the further intervention groups; the process of randomisation was compromised |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficiently for a judgement to be made |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and being placed on a waiting list). Participants were made aware of their group allocation Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | High risk | All observational assessments were coded by the researcher, who was not blinded to group allocation |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | Low risk | There were no parent‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The study permitted control group members to cross‐over into the intervention arm; 6 out of 16 chose to do so. However, data is not clearly broken down (i.e. it is not clear where the final numbers for intervention outcomes came from and how many of original intervention arm dropped out) |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | Unclear risk | Study investigators reported "The six parents who first participated in the Wait List Control group, then in the treatment group were counted twice for demographic purposes." (p 29). There is insufficient information to assess whether these items could introduce bias |
Dittman 2015.
| Methods |
Design: Parallel randomised controlled trial
Unit of randomisation: Individual participant
Follow‐up: 6 months Study dates: No information provided |
|
| Participants |
Participants: Parents (94% mothers) who were concerned about disobedient or non‐compliant behaviour of their child
Mean age of parents: 37.33 (SD 5.08; range 20 to 47) years; 94% mothers; intervention group: 36.8 (SD 5.5; range: NR) years, wait‐list: 38.0 (SD 4.5; range: NR) years Mean age of child: 3.62 (SD 0.68) years, range 3 to 5 years; 30 girls and 55 boys Ethnicity: 79% Australian or New Zealand European, 13% other, 8% unknown Number randomised: 85 (45 intervention; 40 control) Country & setting: New Zealand and Australia; two sites; recruited from community settings; intervention delivered in the community Eligibility criteria: Child aged between 3 and 5 years; parent report of concerns about that child’s disobedient behaviour (assessed by the question ‘‘are you concerned about dealing with the disobedience of your child?’’); parent was not receiving services for their child’s behavioural problems or for their own psychological difficulties; and the child did not have a developmental disability |
|
| Interventions |
Two conditions: Group parent training (Dealing with Disobedience discussion group); no intervention control: wait‐list
Duration of intervention: 1 session (2 hours) Therapist training: Registered psychologist trained and accredited through competency‐based assessment to deliver Triple P discussion groups |
|
| Outcomes |
Behavioural problems: Eyberg Child Behaviour Inventory ‐ intensity scale (parent report) Timing of outcome: Outcome reported 4 weeks after discussion group Secondary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes |
Level of prevention: Secondary Funding: No information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was conducted after completion of T1 assessment using a list of computer‐generated random numbers |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficiently for a judgement to be made |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not be possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study means personnel delivering the intervention would be aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | There were no independent observer‐rated outcomes |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | The outcome assessment by parents was not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4/45 of the intervention group did not receive the intervention, and 12/45 (27%) of intervention group members and 2/40 (5%) of control group members did not complete the post‐test assessment. Intent‐to‐treat analysis was carried out with the expectation–maximisation method used to estimate missing data |
| Selective reporting (reporting bias) | Low risk | The published report includes all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Griffith 2012.
| Methods |
Design: Randomised controlled trial
Unit of randomisation: Parent/child dyads
Follow‐up: 6 months Study dates: October 2007 to September 2010 |
|
| Participants |
Participants: Parents (87 mothers, 2 fathers) living in a designated Flying Start area (low socioeconomic area) Mean age of parents: 28.97 (SD 6.72; range: NR) years; intervention group: 28.6 (SD 7.0; range: NR) years, control group: 29.8 (SD 6.1; range: NR) years Age of child: 21.2 (SD 6.3, range 12 to 36) months; 37 girls and 52 boys Ethnicity: Not reported Number randomised: 89 (intervention 60; control 29) Country & setting: UK (Wales); multi‐site; recruited from Flying Start centres; delivery of intervention not reported Eligibility criteria: Child aged 12 to 36 months; parent and child must live within a designated Flying Start area in Wales; and families not to have been on an Incredible Years parenting programme in the past |
|
| Interventions |
Two conditions: Group parent training (Incredible Years Toddler parenting programme); wait‐list control
Duration of intervention: 12 (2.5 hours) sessions over 12 weeks Therapist training: Trained group leaders with mentor’s supervision |
|
| Outcomes |
Secondary outcomes: Parent‐child interaction as measured by the Dyadic Parent‐Child Interaction Scale, reported by observing researcher Timing of outcomes: Outcomes reported for 6 months follow‐up Primary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes |
Level of prevention: Primary Funding: the Welsh Assembly Government, Welsh Language Board, and Incredible Years Cymru |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study reported that participants were randomised using a "remote dynamic randomisation service provided by an independent trials unit" |
| Allocation concealment (selection bias) | Low risk | The study reported that participants were randomised using a "remote dynamic randomisation service provided by an independent trials unit" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and being placed on a waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | The investigators reported that observers were blinded to the participants' experimental condition at baseline and follow‐up |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | Low risk | There were no parent‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 100% of participants completed the Schedule of Growing Skills assessment at follow‐up. 44/60 (73%) of the intervention group and 23/29 (79%) of the control group completed the Dyadic Parent‐Child Interaction Scale at follow‐up |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appeared to be free of other sources of bias |
Gross 1995.
| Methods |
Design: Randomised controlled trial
Unit of randomisation: Individual family
Follow‐up: 1 year Study dates: 1989 to 1994 |
|
| Participants |
Participants: Both parents (23 mothers; 23 fathers) of children who met criteria for behavioural difficulty, as defined by a score of > 125 on the Eyberg Child Behaviour Inventory Mean age of parents: Mothers 32 (SD 4.8) years, fathers 33 (SD 4.9) years; mean, SD, range for entire sample, intervention and control groups: NR Child age: 24 to 36 months (mean, SD: NR); 20 (83%) boys and 3 girls Ethnicity: Not reported Number randomised: 23 families (10 intervention (10 mothers + 10 fathers + 11 toddlers); 13 control (13 mothers + 13 fathers + 13 toddlers)) Country & setting: USA; single‐site; recruited from urban medical centre and community; delivery of intervention not reported Eligibility criteria: Child aged between 24 and 36 months; both parents willing to participate, complete series of questionnaires and observation sessions at preintervention, postintervention, and 3 months postintervention; and child meets criteria for behavioural difficulty |
|
| Interventions |
Two conditions: Group‐based parent training (Parenting Training Intervention); no intervention
Duration of intervention: 10 (2 hours) sessions over 10 weeks Therapist training: Master degree in psychiatric nursing and experience |
|
| Outcomes |
Externalising problems: Eyberg Child Behaviour Inventory ‐ intensity, as completed by mother (father report data not added) Secondary outcomes: Parent‐child interaction as measured by the Dyadic Parent‐Child Interaction Coding System, observer‐rated observation of mother and child (data for father‐child observation were not added) Timing of outcomes: Outcomes reported for postintervention, 3‐month and 1‐year follow‐up Adverse events: None specified |
|
| Notes |
Level of prevention: Secondary or tertiary Funding: the National Institute for Nursing Research (grant no. R29 NR02013) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The study reported that participants were randomly assigned, but no further details were reported for a judgement to be made. We requested clarification from study investigators, but no further information was available at the time this review was prepared |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficiently for a judgement to be made. We requested clarification from study investigators, but no further information was available at the time this review was prepared |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and receiving no intervention). Participants were notified of their group assignment once randomisation was completed Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | Dyadic Parent‐Child Interaction Coding System was assessed by observers that were unaware of child group assignments |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Eyberg Child Behaviour Inventory and Toddle Temperament Scale were assessed by parents who were not blinded to intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Study investigators reported that 12 children of intervention group participants completed the 1‐year follow‐up assessment. In their initial study, investigators reported a total of 11 child participants; at 1‐year follow‐up, they reported a total of 12 child participants |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appeared to be free of other sources of bias |
Gross 2003.
| Methods |
Design: Cluster‐randomised controlled trial
Unit of randomisation: Day care centres
Follow‐up: 1 year Study dates: No information provided |
|
| Participants |
Participants: Parents ("approximately 90% mothers", 4.9% fathers) and teachers of child enrolled in a participating day care centre in low socioeconomic areas Mean age of parents: 27.9 (SD 6.8; range: NR) years; Mean, SD, range for mothers, fathers and intervention and control groups: NR Age of child: 2 or 3 years (mean, SD: NR); number of boys and girls: NR Ethnicity: 57.2% African American; 29.3% Latino; 3.4% White; 4.3% Multi‐ethnic; 5.8% other Number randomised: 264 (intervention one: 78; intervention two: 75; intervention three: 52; control: 59) Country & setting: USA; multi‐site; recruited from preschools in community; intervention delivered in preschools Eligibility criteria: Parent was the legal guardian of a 2‐ or 3‐year‐old child enrolled in participating day care centre and completed all baseline assessments |
|
| Interventions |
Four conditions: Incredible Years BASIC with parents and teachers; Incredible Years BASIC with parents only; Incredible Years BASIC with teachers only; wait‐list control
Duration of intervention: 12 (2 hours) sessions over 12 weeks Therapist training: Trained group leaders |
|
| Outcomes |
Externalising problems: Eyberg Child Behaviour Inventory ‐ intensity, as completed by parent (total score, conduct, inattentive and oppositional factor data not added); Kohn's Problem Checklist, as completed by teachers Secondary outcomes: Parent‐child interaction as measured by the Dyadic Parent‐Child Interaction Coding System ‐ Revised ‐ negative behaviour scale, completed by observers Timing of outcomes: Outcomes reported for postintervention and 1‐year follow‐up Adverse events: None specified |
|
| Notes |
Level of prevention: Primary Funding: Grant R01 NRO4085 from the National Institute for Nursing Research and Grant K02 MH00988 from the National Institute for Mental Health |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The study reported that participants were randomly assigned, but no further details were reported for a judgement to be made. We requested clarification from study investigators, but no further information was available at the time this review was prepared |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficiently for a judgement to be made. We requested clarification from study investigators, but no further information was available at the time this review was prepared |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and being placed on a waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | Study investigators reported that for the observational outcome (Dyadic Parent‐Child Interaction Coding System ‐ Revised), assessors were blind to study hypotheses and group assignments |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Parent (Eyberg Child Behaviour Inventory) and teacher (Kohns Problem Checklist) reported outcomes could not have been blinded as they participated in the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Researchers reported initial numbers of families randomised to each group. They reported that 21.2% of parents and 31.2% of teachers dropped out of the study, but did not report which groups the parents and teachers dropped out from. Further, study investigators reported: "The growth care models presented in this article are based on 208 participants who remained in the study. To assess the effects of dropouts on the results on these analyses, we also run the final growth curve on the initial sample of 246 participants. The pattern of significant parameters remained unchanged as a result of using the larger sample. This indicate that participants attrition did not modify the interpretation of results" (pp 266 ‐ 77) |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | High risk | This was a cluster‐randomised trial and the study authors reported their means and SDs based on descriptive statistics, but did not report ICC |
Hiscock 2008.
| Methods |
Design: Parallel, cluster‐randomised controlled trial
Unit of randomisation: Mother and child heath centre
Follow‐up: 21 months Study dates: 2004 to 2006 |
|
| Participants |
Participants: 733 mothers Mean age of parents: Intervention 33.0 (SD 4.8; range: NR) years; control 33.3 (SD 4.7; range: NR) years; mean, SD, range for entire sample: NR Age of child: 8 months (mean, SD, range: NR); number of boys and girls: NR Ethnicity: Not reported Number randomised: 733 (intervention 329; control 404) Country & setting: Australia; multi‐site; recruited from community settings; intervention delivered in the community Eligibility criteria: Parents of children aged 6 months attending community well‐child clinics |
|
| Interventions |
Two conditions: Group‐based parent training (Toddlers Without Tears); usual primary care
Duration of intervention: 7 months Therapist training: Nurses trained by a paediatrician and child psychologist |
|
| Outcomes |
Externalising problems: Child Behaviour Checklist 1.5 to 5 years ‐ externalising, mother‐reported Internalising problems: Child Behaviour Checklist 1.5 to 5 years ‐ internalising, mother‐reported Timing of outcomes: Outcomes reported for 3 years follow‐up (12 and 18 months data also reported in the study but not entered in the review) Secondary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes |
Level of prevention: Primary Funding: Philanthropic Organisation, William Buckland Foundation, Telstra Community Development Fund |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Maternal and child health centres were cluster‐randomised using a computer‐generated allocation sequence |
| Allocation concealment (selection bias) | Low risk | Study investigators reported that "an independent statistician randomly allocated maternal and child health centres" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: Study investigators reported "masking occurred at randomisation, with group allocation concealed from researchers and participants until allocation was complete", however, no specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found after allocation was complete Personnel: The design of the study means personnel delivering the intervention would be aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | There were no independent observer‐rated outcomes |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcomes were mother‐reported, study investigators reported "masking occurred at randomisation, with group allocation concealed from researchers and participants until allocation was complete", however, no specific additional measures were reported after allocation was complete |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 37 out of 329 families in the intervention group and 40 out of 404 families in the control group left the study early. Reasons for leaving early were not reported. Intention‐to‐treat analysis was done |
| Selective reporting (reporting bias) | Low risk | The published report includes all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appears to be free of other sources of bias. This was a cluster‐randomised trial, the study authors reported ICC and accounted for clustering in their analysis by using multilevel models |
Hutchings 2007.
| Methods |
Design: Parallel randomised controlled trial
Unit of randomisation: Parent‐child dyads
Follow‐up: 6 months Study dates: 2002 to 2006 |
|
| Participants |
Participants: Socially disadvantaged parents (gender not reported) with children scoring above the clinical cut‐off on either the Eyberg Child Behaviour Inventory ‐ problem or intensity scale Mean age of parents: Not reported Mean age of child: Entire sample range 3 to 4 years (mean, SD: NR), intervention mean 46.2 (SD 4.2; range: NR) months, control 46.4 (SD 6.6; range: NR) months; 70 boys and 63 girls Ethnicity: Not reported Number randomised: 153 (intervention 104; control 49) Country & setting: UK (Wales); multi‐site; recruited from community settings; intervention delivered in the community Eligibility criteria: Families living within a designated Sure Start (socially disadvantaged, predominantly low‐income) area with a child aged three or four years scoring above the clinical cut‐off on either the problem or intensity scale of the Eyberg Child Behaviour Inventory |
|
| Interventions |
Two conditions: Group‐based parent training (Incredible Years BASIC parenting programme); wait‐list control
Duration of intervention: 12 weeks Therapist training: Trained leaders with supervision |
|
| Outcomes |
Externalising problems: Eyberg Child Behaviour Inventory ‐ intensity, parent‐reported (problem and conduct subscale data not added) Externalising problems subscale ‐ hyperactivity/inattention: Strengths and Difficulties Questionnaire ‐ hyperactivity, parent‐reported (total child deviance and conduct subscale data not added) Secondary outcomes: Parent‐child interaction as measured by Dyadic Parent‐Child Interaction Coding System ‐ child deviance, observer‐reported Data for Conners Abbreviated Parent/Teacher Rating Scale, parent‐report and Kendall Self Control Rating Scale, parent‐rated were not added to the meta‐analyses Timing of outcomes: Outcomes reported for 6 months follow‐up Adverse events: None specified |
|
| Notes | We are grateful to the study authors for replying to our request for additional data Level of prevention: Secondary or tertiary Funding: The Health Foundation (UK) (ref: 1583/1566) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were block randomised by area using a random number generator, after stratification by gender and age |
| Allocation concealment (selection bias) | Low risk | One of the authors blindly allocated participants, further information from the study investigators confirmed this and states "...researchers kept blind as to allocation" (Hutchings 2007) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not be possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and waiting list. No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study means personnel delivering the intervention would be aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | Study investigators reported "researchers blind to allocation carried out the interviews and observations" |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 18 out of 104 participants in the intervention group and 2 out of 49 left the study early; reasons for leaving early were reported. An intention‐to‐treat analysis was used |
| Selective reporting (reporting bias) | Low risk | The published report includes all expected outcomes, including those that were prespecified |
| Other bias | High risk | The principal investigator reports a conflict of interest which could potentially lead to pro‐intervention bias in the language of the paper: “Competing interests: JH is paid by Incredible Years for running occasional training courses in the delivery of the parent programme . . ." (p 7600) |
Kennedy 2009.
| Methods |
Design: Parallel randomised controlled trial
Unit of randomisation: Individual children
Follow‐up: 6 months Study dates: Started January 2005 |
|
| Participants |
Participants: Parents (gender not reported) of children with a high score on behavioural inhibition. At least one parent had a DSM‐IV diagnosis of an anxiety disorder Mean age of parents: Not reported Mean age of child: 47.07 (SD 7.05, range 36 to 58) months; intervention group 48.4 (SD 7.1; range: NR) months, 58% girls; wait‐list 45.8 (SD 6.9; range: NR) months, 51% girls Ethnicity: Not reported (majority of Anglo‐Catholic background) Number randomised: 71 (intervention 35; control 36) Country & setting: Australia; single‐site; recruited from community settings; intervention delivered in the community Eligibility criteria: Children were required to score high on a laboratory measure of behavioural inhibition, and at least one parent was required to meet DSM‐IV criteria for diagnosis of an anxiety disorder |
|
| Interventions | Two conditions: Group‐based parent training (Parent Intervention Program); wait‐list control Duration of intervention: 8 sessions over 8 weeks + one telephone follow‐up call a month after completion Therapist training: Experienced researchers | |
| Outcomes |
Internalising problems: Behavioural Inhibition Questionnaire, mother‐reported (father‐reported data not added); Composite Behavioural Inhibition score, clinician report Data for Child Anxiety Life Interference Scale‐Preschool Version, mother‐ and father‐reported; Preschool Anxiety Scale, mother‐ and father‐reported; Global Behavioural Inhibition rating, clinician report; Clinician Severity rating, clinician report were not added to the meta‐analyses Timing of outcomes: Outcomes reported for 6 months follow‐up Secondary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes |
Level of prevention: Secondary or tertiary Funding: self funded |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done using a coin toss for each individual |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficiently for a judgement to be made. We requested clarification from study investigators, but no further information was available at the time this review was prepared |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not be possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study means personnel delivering the intervention would be aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Unclear risk | Information reported insufficiently for a judgement to be made |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 91.4% of the intervention and 86.1% of the control group completed the 6‐month follow‐up. Reasons for losses to follow‐up not reported. Information reported insufficiently for a judgement to be made |
| Selective reporting (reporting bias) | Low risk | The published report includes all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Little 2012.
| Methods |
Design: Parallel randomised controlled trial (2:1)
Unit of randomisation: Individual parent
Follow‐up: 6 months Study dates: No information provided |
|
| Participants |
Participants: Parents (gender not reported; ≈ 50% of low socioeconomic status) of children at risk of social‐emotional or behavioural disorder, reaching the “high need” threshold (17 or above out of 40) of the “total difficulties” score of the parent‐completed Strengths and Difficulties Questionnaire Mean age of parents: Not reported Mean age of child: 44 (SD 6) months, range 3 to 4 years; mean, SD, range for intervention and control: NR Ethnicity: Not reported Number randomised: 161 (intervention 110; control 51) Country & setting: UK; multi‐site; recruited from community settings; intervention delivered in the community Eligibility criteria: Children needed to be at risk of a social‐emotional or behavioural disorder |
|
| Interventions | Two conditions: Group‐based parent training (Incredible Years BASIC parenting programme); wait‐list control Duration of intervention: 12 sessions over 12 weeks Therapist training: Trained centre staff, educational psychologists, and practitioners | |
| Outcomes |
Externalising problems: Eyberg Child Behaviour Inventory ‐ intensity, parent‐reported Externalising problems subscale ‐ hyperactivity/inattention: Strengths and Difficulties Questionnaire ‐ hyperactivity, parent‐reported Secondary outcomes: Social skills as measured by the Strengths and Difficulties Questionnaire ‐ pro‐social, parent‐reported (conduct, impact, emotion problems, and peer problems subscales data and total score data were not added) Timing of outcomes: Outcomes reported for 6 months follow‐up Adverse events: None specified |
|
| Notes |
Level of prevention: Secondary or tertiary Funding: no information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Central randomisation service. The randomisation sequence was created by the North Wales Organisation for Randomised Trials in Health (& Social Care) (NWORTH) |
| Allocation concealment (selection bias) | Low risk | Central randomisation service. The randomisation sequence was created by the North Wales Organisation for Randomised Trials in Health (& Social Care) (NWORTH) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not be possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study means personnel delivering the intervention would be aware which groups had been assigned to the different study condition |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | There were no independent observer‐rated outcomes |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10/110 (9%) in the intervention group and 4/51 (8%) in the control group left the study early. Reasons for leaving early were reported |
| Selective reporting (reporting bias) | Low risk | The published report includes all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Morawska 2011.
| Methods |
Design: Parallel randomised controlled trial
Unit of randomisation: Individual parent
Follow‐up: 6 months Study dates: No information provided |
|
| Participants |
Participants: 66 mothers (1 father only) Age of parents: Mother 36.30 (SD 4.51; range: NR) years, father 39.67 (SD 6.73; range: NR) years; intervention group mean 35.9 (SD 5.26; range: NR) years, control group 36.7 (SD 3.7; range: NR) years; mean, SD, range for entire sample: NR Mean age of child: 3.63 (SD 0.92, range 2 to 5) years; intervention group mean 3.8 (SD 0.9; range: NR) years, control group mean 3.5 (SD 1.0; range: NR) years; 37 (55%) boys and 30 (45%) girls Ethnicity: 95.5% White, 4.5% Asian Number randomised: 67 (intervention 33; control 34) Country & setting: Australia; single‐site; recruited from community settings; intervention delivered in the community Eligibility criteria: Not specified |
|
| Interventions | Two conditions: Group‐based parent training (Triple P‐Positive Parenting Program); wait‐list control Duration of intervention: 1 (2 hours) session in 1 week + 2 follow‐up calls Therapist training: Psychologists (after training and accreditation) | |
| Outcomes |
Externalising problems: Eyberg Child Behaviour Inventory ‐ intensity, parent‐reported Secondary outcomes: Parent‐child interaction as measured by the Parenting Relationship Questionnaire attachment subscale, parent‐reported Timing of outcomes: Outcomes reported for postintervention. 6 months follow‐up data were only reported for intervention group and not added to the review Adverse events: None specified |
|
| Notes | We are grateful to the study authors for replying to our request for additional data Level of prevention: Primary Funding: No information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study reported that participants were "randomly allocated", further information from the study investigators states "The randomisation sequence was generated from an online random number generator" (Morawska 2011) |
| Allocation concealment (selection bias) | Low risk | Further information from the study investigators indicates that allocation was concealed: "The randomisation sequence was generated from an online random number generator. One of the authors was responsible for allocation of participants based on this sequence. This author had no contact with the participants and allocated to condition based on the participant number provided by the author who screened and collected data from parents, once the participant had completed all t1 assessment" (Morawska 2011) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not be possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study means personnel delivering the intervention would be aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | There were no independent observer‐rated outcomes |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 6/33 (18%) of participants in the intervention group and 6/34 (18%) in the control group left the study early. Reasons for leaving early were not reported. A further 5 participants were not accounted for, as only 50 participants were included in the analysis |
| Selective reporting (reporting bias) | Low risk | The published report includes all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Morawska 2014.
| Methods |
Design: Parallel randomised controlled trial
Unit of randomisation: Individual parent
Follow‐up: 6 months Study dates: No information provided |
|
| Participants |
Participants: Parents (74 mothers; 12 fathers) who were concerned about and seeking assistance for their child's eating and/or mealtime difficulties
Mean age of parents: Intervention (mother) 35.88 (SD 3.92; range: NR) years, (father) 38.06 (SD 4.22; range: NR) years; control (mother) 37.0 (SD 3.55) years, (father) 39.97 (SD 4.81); mean, SD, range for entire sample: NR Mean age of child: Entire sample 3.72 (SD 1.13, range 2 to 5) years; intervention group mean 45.9 (SD 13.0; range: NR) months, control group mean 43.4 (SD 14.2; range: NR) months; 41 boys and 45 girls Ethnicity: Intervention: 95.3% Caucasian, 4.7% Asian; Control: 85.7% Caucasian, 14.3% Asian Number randomised: 86 (intervention 44; control 42) Country & setting: Australia; multi‐site; recruited from community settings; intervention delivered in centres Eligibility criteria: Parents with a 2‐ to 5‐year‐old child currently experiencing feeding and/or mealtime difficulties, and parents wanted assistance for these difficulties. Parents were excluded if currently receiving professional help for child behavioural or emotional problems, or psychological help or counselling for personal or marital problems; if child had been diagnosed with a disability or developmental disorder; or if parents were intellectually disabled and/or hearing impaired |
|
| Interventions | Two conditions: Group‐based parent training (Hassle Free Mealtime Triple P); wait‐list control Duration of intervention: 1 (2 hours) session in 1 week Therapist training: Psychologists (after training and accreditation) | |
| Outcomes |
Externalising problems: Child Adjustment and Parent Efficacy Scales ‐ behavioural subscale, as completed by parents Internalising problems: Child Adjustment and Parent Efficacy Scales ‐ emotional subscale, as completed by parents; data for Parent and Toddler Feeding Assessment ‐ child frequency and child problem, as completed by parents were not added to the meta‐analyses Timing of outcomes: Outcomes reported for postintervention. Six‐month follow‐up data were only reported for intervention group and not added to the review Secondary outcomes/adverse events: no other outcomes relevant to this review specified |
|
| Notes |
Level of prevention: Secondary or tertiary Funding: no information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random sequence was computer‐generated |
| Allocation concealment (selection bias) | Low risk | Study investigators reported that a person outside the research group generated and concealed the allocation sequence in sealed, numbered envelopes and that allocation to group was implemented by the third author, by sequentially drawing and opening the sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not be possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and in being placed on a waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study means personnel delivering the intervention would be aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | There were no independent observer‐rated outcomes |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 8/44 (18%) of the intervention group and 4/42 (10%) of the control group withdrew from the study prior to follow‐up assessment. The study investigators reported that one parent withdrew from the intervention group due to inability to attend a group session, and seven intervention parents attended a group but did not complete time 2 assessment. Study investigators reported that the proportion of participants who withdrew before follow‐up assessment did not differ significantly between groups |
| Selective reporting (reporting bias) | Low risk | The published report includes all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Niccols 2008.
| Methods |
Design: Parallel randomised controlled trial
Unit of randomisation: Individual participant
Follow‐up: 6 months Study dates: No information provided |
|
| Participants |
Participants: 76 mothers registering for Right from the Start Parenting Program Mean age of parents: 28.8 (SD 6.2, range 18 to 40) years; mean, SD, range for intervention and control groups: NR Mean age of child age: 8.4 (SD 5.4, range 1 to 24) months; 50% boys; mean, SD, range for intervention and control groups: NR Ethnicity: Not reported Number randomised: 76 (intervention 48; control 28) Country & setting: Canada; single‐site; recruited from mothers interested registering for parent training programme; delivery of intervention not reported Eligibility criteria: Mothers were eligible for the study if they were able to complete questionnaires in English and had not attended any portion of Right from the Start previously |
|
| Interventions | Two conditions: Group‐based parent training (Right from the Start); usual primary care (home visit) Duration of intervention: 8 (2 hour) sessions over 8 weeks Therapist training: Psychologists and social workers with additional training | |
| Outcomes |
Secondary outcomes: Parent‐child interaction as measured by the Attachment Q‐set, reported by mother. Only a subset of children were evaluated as the test is for babies over 9 months only. The data reported in the study paper could not be used in our review. We requested clarification from study investigators, and received data that could be used in meta‐analysis (Niccols 2008) Timing of outcomes: Outcomes reported for postintervention and 6 months follow‐up Primary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes | We are grateful to the study authors for replying to our request of additional data Level of prevention: Primary prevention Funding: Grants from the Hamilton Health Sciences Foundation and the Ontario Mental Health Foundation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random sequence was generated using a random number table |
| Allocation concealment (selection bias) | Low risk | Further information from the study investigators indicates that allocation was concealed: "After the pre‐test assessments were completed, the Principle Investigator (me) randomised the participants to one of the two interventions. I did not reveal group allocation information to the research assistants and I instructed the group facilitators, home visitors, and participants not to reveal this information to the research assistants. I maintained group allocation data on a secure computer (mine) and research assistants did not have access to this data until after the study data collection period was completed" (Niccols 2008) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not be possible to fully blind participants in this type of study (there is an obvious difference between receiving group training plus home visitation and receiving only home visitation). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study means personnel delivering the intervention would be aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | There were no independent observer‐rated outcomes |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only a subset of participants were evaluated; the Attachment Q‐set test was only used to evaluate babies over 9 months, excluding more than half of the randomised participants |
| Selective reporting (reporting bias) | Low risk | We received information from study authors to enable inclusion of data for the relevant outcome measure |
| Other bias | Unclear risk | Study investigators reported that completers had higher level of education than did non‐completers |
Niccols 2009.
| Methods |
Design: Parallel randomised controlled trial
Unit of randomisation: Individual participant
Follow‐up: 1 month Study dates: 2002 to 2005 |
|
| Participants |
Participants: 79 mothers Mean age of parents: 31.0 (SD 5.7, range 18 to 45) years; mean, SD, range for intervention and control groups: NR Mean age of child: 24.0 (SD 6.8, range 12 to 36) months; 59,5% boys; mean, SD, range for intervention and control groups: NR Ethnicity: Not reported Number randomised: 79 (intervention 49; control 30) Country & setting: Canada; single‐site; recruited from community; delivery of intervention not reported Eligibility criteria: Mothers able to complete questionnaires in English and had not attended any portion of COPEing with Toddler Behaviour previously |
|
| Interventions | Two conditions: Group‐based parent training (COPEing with Toddler Behaviour); wait‐list control Duration of intervention: 8 sessions over 8 weeks Therapist training: 20 hours workshop training | |
| Outcomes |
Externalising problems: Data for Eyberg Child Behaviour Inventory ‐ problem were not added to the meta‐analyses Secondary outcomes: Parent‐child interaction as measured by structured observation by 2 observers Timing of outcomes: Outcomes reported for postintervention and 1‐month follow‐up Adverse events: None specified |
|
| Notes | We are grateful to the study authors for replying to our request for additional data Level of prevention: Primary Funding: Grant from the Canadian Psychiatric Research Foundation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The principle investigator used the random number table for random assignment (i.e. assigned those with numbers 0, 1, 2, 3, 4, or 5 to COPEing with Toddler Behaviour, and assigned those with numbers 6, 7, 8, or 9 to no intervention) |
| Allocation concealment (selection bias) | Low risk | Further information from the study investigators indicates that allocation was concealed: "Group allocation was concealed from the research assistants. The participants and group facilitators were instructed not to tell them and I did not tell them. I kept the group assignment information on a separate computer file on a secure private computer" (Niccols 2009) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not be possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study means personnel delivering the intervention would be aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | Study investigators reported that research assistants conducting all research assessments were blinded to group assignment and the method of randomisation |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4/49 (8%) of the intervention group and 1/30 (3%) of the control group could not be reached for the postintervention assessment. 4/49 (8%) of the intervention group and 4/30 (13%) of the control group could not be reached for the 1‐month follow‐up. Researchers reported that non‐completers did not differ from completers in terms of child behavioural problems or demographic characteristics. Similar reasons for missing data, that is, "unable to reach" |
| Selective reporting (reporting bias) | Low risk | The published report includes all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Nicholson 1998.
| Methods |
Design: Parallel, quasi‐randomised controlled trial
Unit of randomisation: Individual parent
Follow‐up: 6 weeks Study dates: No information provided |
|
| Participants |
Participants: Parents (29 mothers; 11 fathers) Mean age of parents: Mid‐30s (Mean, SD, range for entire sample, for mothers and numbers, for intervention and control: NR) Mean age of child: entire sample range 1 to 5 years (mean, SD: NR); intervention group mean 3.1 (SD 1.4; range: NR) years, 16 boys and 4 girls; control mean 2.8 (SD 1.1; range: NR) years, 12 boys and 8 girlsEthnicity: 95% White, 5% Hispanic Number randomised: 40 (intervention 20; control 20) Country & setting: USA; single‐site; recruited from community settings; intervention delivered in elementary schools Eligibility criteria: Not specified |
|
| Interventions | Two conditions: Group‐based parent training (STAR parenting programme); wait‐list control Duration of intervention: 4 (2.5 hour) sessions in 4 weeks Therapist training: Parents with a master degree in education or psychology | |
| Outcomes |
Emotional and behavioural problems: Behaviour Screening Questionnaire (BSQ), parent‐reported. Data for Child Problem Behaviour Rating Scale, parent‐reported were not included in the meta‐analyses because they did not add information to the already included BSQ data Timing of outcomes: Outcomes reported for postintervention Secondary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes |
Level of prevention: Primary Funding: No information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The study reported that "Two different week nights were offered to parents for attending classes; parents' choices for class nights were honored whenever possible. Those who indicated no preference were randomly assigned" |
| Allocation concealment (selection bias) | High risk | The allocations sequence could not have been adequately concealed due to the method of randomisation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | There were no independent observer‐rated outcomes |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | At follow‐up assessment 2/20 (10%) of the intervention group had dropped out |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appeared to be free of other sources of bias |
Nicholson 2002.
| Methods |
Design: Parallel quasi‐randomised controlled trial
Unit of randomisation: Individual parent or caregiver
Follow‐up: 1 month Study dates: No information provided |
|
| Participants |
Participants: At‐risk parents (23 mothers; 2 grandmothers; 1 father) of young children, whereby "at‐risk" is determined by excessive use of verbal and corporal punishment combined with low‐income status Mean age of parents: 30.79 (SD 11.97; range: NR) years; Mean, SD, range for intervention and control: NR Age of child: 1 to 5 years (mean, SD: NR); 14 (54%) boys and 12 (46%) girls; Mean, SD, range for intervention and control groups: NR Ethnicity: 54% African‐American; 23% Hispanic; 15% White; 8% other Number randomised: 26 (intervention 13; control 13) Country & setting: USA; single‐site, recruited from community settings; delivery of intervention not reported Eligibility criteria: One child between ages 1 and 5 years and frequent use of verbal or corporal punishment |
|
| Interventions | Two conditions: Group‐based parent training (STAR Parenting Program); wait‐list control Duration of intervention: 10 (1.5 hour) sessions in 10 weeks Therapist training: 1 PhD and 4 Master trained professionals | |
| Outcomes |
Emotional and behavioural problems: Behaviour Screening Questionnaire, parent‐reported; Pediatric Symptom Checklist, as reported by teachers Externalising problems: Eyberg Child Behaviour Inventory ‐ intensity, as reported by parents; Sutter‐Eyberg Behaviour Inventory ‐ intensity, as reported by teachers (problems scale data were not added) Timing of outcomes: Outcomes reported for postintervention. 1‐month follow‐up data were reported for intervention group only and not added to the review Secondary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes | We are grateful to the study authors for replying to our request for additional data Level of prevention: Primary Funding: Grants from the Child Abuse Prevention Fund, the Todd Wehr Foundation, and Robert T. Foote |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study reported that participants were randomly assigned. Further information from the study investigators states "We have the computer generate a random numbers table of 0s and 1s with identified and eligible participants assigned the next unused number in the table as they are consecutively recruited into the sample" (Nicholson 2002) |
| Allocation concealment (selection bias) | Low risk | Information from the study investigators (see quote above) indicates that allocation was concealed (Nicholson 2002) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and being placed on a waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Unclear risk | Information was reported insufficiently for a judgement to be made |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome measures rated by parent (Behaviour Screening Questionnaire and Eyberg Child Behaviour Inventory) could not have been blinded as parents were aware of intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The study reported a 10% dropout rate, but did not describe whether these parents were included in the analyses or from which group they dropped out |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appeared to be free of other sources of bias |
Oré 2011.
| Methods |
Design: Parallel randomised controlled trial
Unit of randomisation: Mother/child dyads
Follow‐up: postintervention Study dates: No information provided |
|
| Participants |
Participants: Mother‐child dyad of children previously participating in a nutrition study. All mothers Mean age of parents: Intervention 24.5 years (SD, range: NR), control 24.6 years (SD, range: NR); Mean, SD, range for entire sample: NR Age of child: 8 to 11 months (mean, SD: NR); 59% boys; Mean, SD, range for intervention and control: NR Ethnicity: Not reported Number randomised: 182 participated (number randomised was not reported, we have requested more information from the study investigators on numbers randomised, but no further information was available at the time this review was prepared). Number analysed: 163 (intervention 78; control 85) Country & setting: Peru; recruited from community settings ‐ children participating in a previous study on nutrition Eligibility criteria: Mothers of healthy children aged 8 to 11 months |
|
| Interventions | Two conditions: Group‐based parent training (not specified); control group (no information, we have requested more information from the study investigators on the control condition, but no further information was available at the time this review was prepared) Duration of intervention: 4 sessions over 4 weeks Therapist training: Psychologist and nurse | |
| Outcomes |
Emotional and behavioural problems: Bayley Scale of Infant Development ‐ II Edition, mother‐reported Timing of outcomes: Outcomes reported for postintervention Secondary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes |
Level of prevention: Primary Funding: No information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The study reported that participants were randomly allocated, but no further details were reported for a judgement to be made. In addition, study researchers reported that some children were assigned to groups "according to time of arrival" and that children assigned to the treatment group had to wait until a group of 10 participants were ready to start the intervention. In all cases the waiting time was not more than two months. We requested clarification from study investigators, but no further information was available at the time this review was prepared |
| Allocation concealment (selection bias) | Unclear risk | Information reported insufficiently for a judgement to be made. We requested clarification from study investigators, but no further information was available at the time this review was prepared |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not be possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study means personnel delivering the intervention would be aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | There were no independent observer‐rated outcomes |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome measure rated by mothers could not have been blinded as they were aware of intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | ±10% (19/182) children entered study and were not analysed because of problems with the questionnaires ‐ no information about which group they belonged to |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appeared to be free of other sources of bias |
Perrin 2014.
| Methods |
Design: Parallel randomised controlled trial
Unit of randomisation: Individual parents
Follow‐up: 12 months Study dates: November 2006 to December 2011 |
|
| Participants |
Participants: Parents (142 mothers, 8 fathers) of children who had disruptive behaviours on the Infant‐Toddler Social‐Emotional Assessment Scale. Age of parents: 30 '< 27 years old'; 42 '28 to 33 years old'; 43 '34 to 37 years old'; 35 '> 38 years old' (mean, SD, range: NR) Age of child age: 2 to 4 years (mean, SD for entire sample: NR); intervention mean 2.7 (SD 0.6; range: NR) years, control mean 2.8 (SD 0.7; range: NR); 94 boys and 56 boys Ethnicity: 9 % Hispanic, 91% Not Hispanic Number randomised: 150 (intervention 89; control 61) Country & setting: USA; multi‐site; recruited from health centres in the community; intervention delivered at health centre and occasionally at local library Eligibility criteria: Parents were eligible if their child scored at the 80th percentile or greater on the screener. Parents were excluded if they (1) could not speak English or Spanish well enough to participate in a parenting group or (2) reported that the child had a diagnosis of pervasive developmental disorder or global developmental delay |
|
| Interventions | Two conditions: Group‐based parent training (Incredible Years ‐ abbreviated); wait‐list control Duration of intervention: 10 weeks Therapist training: Research clinician and a paediatrician | |
| Outcomes |
Externalising problems: Early Childhood Behaviour Inventory ‐ intensity, as reported by parents Secondary outcomes: Parent‐child interaction as measured by the Dyadic Parent‐Child Interactive Coding System‐Revised, reported by clinical observers Timing of outcomes: Outcomes reported for postintervention, 6‐month, and 1‐year follow‐up Adverse events: None specified |
|
| Notes | We are grateful to the study authors for replying to our request for additional data Level of prevention: Secondary or tertiary prevention Funding: National Institute of Mental Health R01 grant MH076244‐01 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random number generator was used to conduct randomisation |
| Allocation concealment (selection bias) | Low risk | Further information from the study investigators states "Intervention assignment was communicated directly to clinicians, who then informed parents of their intervention status" (Perrin 2014) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | It would not have been possible to fully blind participants or personnel delivering the intervention in this type of study (there is an obvious difference between receiving group training and wait‐list). Further information from the study investigators states "Participants (i.e. parents) knew whether they were receiving intervention (group parent training) or not. Likewise, the clinicians who ran the parent training groups also knew about assignment to intervention" (Perrin 2014) |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | The observational assessment videotapes were scored by independent coders who were unaware of intervention condition and assessment period |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 17/89 (19%) participants in the intervention group and 11/50 (22%) participants in the control group dropped out of the study. Researchers hypothesised that the data were missing "at random," as supported by the fact that several baseline, but not outcome, variables predicted missingness |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appeared to be free of other sources of bias |
Simkiss 2013.
| Methods |
Design: Parallel randomised controlled trial
Unit of randomisation: Individual family
Follow‐up: 9 months Study dates: December 2008 to January 2011 |
|
| Participants |
Participants: Parents (275 mothers; 11 father) living in the catchment area of "Flying Start" early years centres who had not previously attended the Family Links Nurturing Programme Mean age of parents: Not reported Age of child: 2 to 4 years (mean, SD, range, number of boys and girls: NR) Ethnicity: 71% White British; 16% White Other; 1% Black African; 0.3% Black Caribbean; 5% Asian Indian/Pakistani/Bangladeshi; 0.7% Asian Chinese; 6% other Number randomised: 286 (intervention 143; control 143) Country & setting: UK; multi‐site; recruited from early years' centres; delivery of intervention not reported Eligibility criteria: Parents with children aged 2 to 4 years living in the catchment area of ‘Flying Start’ early years centres who had not previously attended a Family Links Nuturing Programme |
|
| Interventions | Two conditions: Group‐based parent training (Family Links Nurturing Programme); wait‐list control Duration of intervention: 10 (2 hour) sessions over 10 weeks Therapist training: Facilitators trained over a 4‐day programme and had supervision | |
| Outcomes |
Externalising problems: Parent Account of Child Symptoms ‐ Cscale, as reported by researchers observing child behaviour Externalising problems subscales ‐ hyperactivity/inattention: Parent Account of Child Symptoms ‐ Hscale, as reported by researchers observing child behaviour Internalising problems: Parent Account of Child Symptoms ‐ internalising, as reported by researchers observing child behaviour. We included data from the Hscale and Cscales, but have requested confirmation from the study investigators that these scales represent hyperactivity and conduct. No further information was available at the time this review was prepared Timing of outcomes: Outcomes reported for 9‐month follow‐up Secondary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes |
Level of prevention: Primary Funding: Trial was funded by a consortium of four local authorities in South Wales: Cardiff, Torfaen, Newport and Caerphilly and the Welsh Assembly Government. Additional funding was provided by the Esme Fairburn Foundation and the Waterloo Foundation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A random sequence was computer‐generated |
| Allocation concealment (selection bias) | Low risk | Study investigators reported that the allocation sequence was held by a service not involved with recruitment, therapy, or evaluation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and wait list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | Study investigators reported that assessors conducting coding and data analysis were blind to group allocation, "except on rare occasions when families disclosed their assignment status during postcourse interviews" |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | Low risk | There were no parent‐reported outcome measures |
| Incomplete outcome data (attrition bias) All outcomes | High risk | The study reported that 48/143 families (34%) allocated to the intervention group did not attend any sessions; a further 27/143 (19%) discontinued the programme in the first 3 sessions. Reasons for dropout not given. 15/143 (10%) control group families attended a Family Links Nurturing Programme before 9‐month follow‐up and a further 13/143 (9%) control group parents attended other parenting support programmes during the trial. Number of analysed participants does not match with these numbers |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appeared to be free of other sources of bias |
Solís‐Cámara 2004.
| Methods |
Design: Parallel randomised controlled trial
Unit of randomisation: Mother/child dyads
Follow‐up: 6 months Study dates: No information provided |
|
| Participants |
Participants: Parents (30 mothers, 10 fathers) of children fulfilling criteria for behavioural difficulties Mean age of parents: 35.3 (SD 6.9; range: NR) years; Mean, SD, range for intervention and control and for mothers and fathers: NR Mean age of child: 3.7 (SD 0.8, range 3 to 5) years; 24 boys and 16 girls; Mean, SD, range for intervention and control: NR Ethnicity: Not reported Number randomised: 40 (intervention 20; control 20) Country & setting: Mexico; recruited from preschool settings Eligibility criteria: Not specified |
|
| Interventions | Two conditions: Group‐based parent training (research‐based standardised parenting programme); wait‐list control Duration of intervention: 8 (1.5 hour) sessions over 8 weeks Therapist training: Not reported | |
| Outcomes |
Secondary outcomes: Social skills as measured by the Eyberg Child Behaviour Inventory ‐ social behaviour, parent‐reported (negative behaviour not added); parent‐child interaction as measured by a checklist of observations of interactions (IOI ‐ Informe de Observation de la Interaction, back‐translated and validated), observer‐rated Timing of outcomes: Outcomes reported for 6‐month follow‐up Primary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes |
Level of prevention: Secondary or tertiary Funding: No information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study investigators reported "people were randomly assigned to two groups using a table of random numbers; subsequently with a toss of a coin it was decided which group was to receive the intervention or control (waiting list)" (p 203) |
| Allocation concealment (selection bias) | Low risk | The study investigators reported "people were randomly assigned to two groups using a table of random numbers; subsequently with a toss of a coin it was decided which group was to receive the intervention or control (waiting list)" (p 203) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and wait list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Unclear risk | Information reported insufficiently for a judgement to be made |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | There was no mention of incomplete outcome data. They stated that 50 children and parents were chosen and 10 were excluded before entering the study |
| Selective reporting (reporting bias) | Unclear risk | It seems that all outcomes were reported, but not with sufficient information |
| Other bias | Low risk | The study appeared to be free of other sources of bias |
Sutton 1992.
| Methods |
Design: Quasi‐randomised controlled trial
Unit of randomisation: Individual family
Follow‐up: 12 to 18 months Study dates: 1984 |
|
| Participants |
Participants: Parents (gender not reported) of difficult preschool children Mean age of parents: Not reported Mean age of child: 2.8 (range 1 to 4.3; SD: NR) years; 25 boys and 5 girls; Mean, SD, range for intervention and control: NR Ethnicity: All children, except for 1, was White, and all parents except for 1 father was White Number randomised: 37 (allocation numbers not reported) Country & setting: UK; multi‐site; recruited from community settings; group‐based parenting training likely took place in treatment centre, though not reported Eligibility criteria: Not specified |
|
| Interventions | Four conditions: Group‐based parent training (with booklets from researcher); home visit parent training; telephone consultation parent training; wait‐list control Duration of intervention: 8 (1 to 2 hour) sessions over 8 weeks + boosters 2 weeks and 3 months later Therapist training: Researcher | |
| Outcomes |
Emotional and behavioural problems: Child Behaviour Questionnaire, as reported by parent Externalising problems subscale ‐ hyperactivity/inattention: Home Situations Questionnaire, as reported by parent Timing of outcomes: Outcomes reported for postintervention. Follow‐up data were only reported for intervention group and not entered in the review Secondary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes |
Level of prevention: Secondary or tertiary Funding: No information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The study investigators reported that participants were sequentially (not randomly) assigned to their intervention group, and that 3 applications were allocated "out of order" due to "difficulty of access or similar reasons" |
| Allocation concealment (selection bias) | High risk | Participants were aware of their group allocation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training, home visits or telephone consulting and being assigned to a waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | There were no independent observer‐rated outcomes |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Study investigators reported that 37 participants were assigned to the 4 intervention arms. 2 participants in the parent training group and 5 participants in the wait‐list group dropped out of the study; reasons for dropout were not provided. Participants placed on the waiting list were subsequently allocated to home, or telephone intervention groups and their outcome data were analysed for both intervention condition and wait‐list condition |
| Selective reporting (reporting bias) | High risk | Endpoint data for wait list condition were not supplied for negative child behaviours |
| Other bias | High risk | The study investigators did not report numbers of participants allocated to each intervention arm |
Tiedemann 1992.
| Methods | Design: Parallel randomised controlled trial Unit of randomisation: Individual parent Follow‐up: 6 weeks | |
| Participants |
Participants: 49 married mothers of siblings with parent‐reported difficulties in sibling interaction (younger children 20 girls, 28 boys; older children 27 girls, 21 boys) Mean age of parents: 36 years (SD/range not reported). No details per intervention group Mean age of child: Younger children 38.0 (SD not reported) months, range not reported; older children 64.1 (SD not reported) months, range not reported. No details per intervention group Ethnicity: Not reported Number randomised: 49 (group intervention 17; individual intervention 16; waiting list 16) Country & setting: Canada; single‐site; recruited from community settings; intervention delivered in the community Eligibility criteria: Married women with at least a Grade 10 education, a family socioeconomic status of semiskilled worker or above, and two children between the ages of 2 years and 6 months and 6 years and 11 months, but no older children |
|
| Interventions | Three conditions: Group‐based parent training (Group Sharing Program); Individual Sharing Program; wait‐list control Duration of intervention: 5 sessions, no further information reported Therapist training: Not reported | |
| Outcomes |
Emotional and behavioural problems: Child Behaviour Checklist ‐ total, mother report Secondary outcomes: Social skills as measured by the Vineland Adaptive Behaviour Scales ‐ socialisation domain, mother and out‐of‐home informant reported (father report not added) Timing of outcomes: Outcomes reported for postintervention and 6‐week follow‐up Secondary outcomes/adverse events: No other outcomes relevant to this review specified |
|
| Notes | Data reported for younger and older children separately We are grateful to the study authors for replying to our request of additional data Level of prevention: Secondary or tertiary Funding: Grant from the Laidlaw Foundation to the second author, and a SSHRC doctoral fellowship and APA Dissertation Award |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study reported that "families were randomly assigned". Further information from the study investigators states "there was a list of randomly‐generated numbers, from which I randomly selected a starting point and then used the list to create a random sequence of 1’s, 2’s, and 3’s. This sequence would then have been used to assign subjects to one of the three conditions after they agreed to participate" (Tiedemann 1992) |
| Allocation concealment (selection bias) | High risk | Information from the study investigators states "As for concealment of group allocation, that certainly wouldn’t have been possible for me, as I had to both deliver the programme and run the assessment sessions" (Tiedemann 1992) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training, individual training and waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | Information from the study investigators states "The research assistants scoring the video data, though, would have been blind to group assignment" (Tiedemann 1992) |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 participant in the intervention group left the study early |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appeared to be free of other sources of bias |
Webster‐Stratton 1982.
| Methods |
Design: Cross‐over, randomised controlled trial
Unit of randomisation: Individual mothers
Follow‐up: postintervention Study dates: No information provided |
|
| Participants |
Participants: 35 mothers; (23 boys, 12 girls) Mean age of parents: 33 years (SD/range not reported); intervention 32.3 (SD 3.3) years, range not reported; control 33.8 (SD 3.5) years, range not reported Child age: 3 years and 11 months (SD not reported), range 3 to 5 years; intervention 48.0 (SD 8.2) months, range not reported; control 46.3 (SD 10.0) months, range not reported Ethnicity: Not reported Number randomised: 35 (intervention 16; control 19) Country & setting: USA; single‐site; recruited from community settings; intervention delivered in the community Eligibility criteria: Not specified |
|
| Interventions | Two conditions: Group‐based parent training (videotape modelling group discussion programme); wait‐list control Duration of intervention: 4 weeks Therapist training: Graduate student therapist with extensive group work training | |
| Outcomes |
Externalising problems: Eyberg Child Behaviour Inventory ‐ intensity, parent‐reported
Secondary outcomes: Parent‐child interaction as measured by the Interpersonal Behaviour Construct Scale ‐ child negative effect, observer‐rated (child nonacceptance, child dominance, and child submissiveness subscales were not added) Timing of outcomes: Outcomes reported for postintervention. Adverse events: None specified |
|
| Notes | Data was only used from the first stage of the trial We are grateful to the study authors for replying to our request of additional data Level of prevention: Primary Funding: No information provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The study reported that participants were randomly assigned. Further information from the study investigators states "for random assignment we put the subject numbers (folded to keep them blinded) in a basket and then picked each one in process assigning one to control and one to treatment. This process was observed by 3 people to make sure it was done correctly. Once numbers were assigned to their condition we then checked the numbers against the names of the families and let families know of their assignment. Everyone stuck to this random assignment process" (Webster‐Stratton 1982) |
| Allocation concealment (selection bias) | Low risk | Information from the study investigators states "for random assignment we put the subject numbers (folded to keep them blinded) in a basket and then picked each one in process assigning one to control and one to treatment. This process was observed by 3 people to make sure it was done correctly. Once numbers were assigned to their condition we then checked the numbers against the names of the families and let families know of their assignment. Everyone stuck to this random assignment process" (Webster‐Stratton 1982) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk |
Participants: It would not have been possible to fully blind participants in this type of study (there is an obvious difference between receiving group training and waiting list). No indication of any specific additional measures taken to reduce the risk of bias that might result from differential behaviours by participants were found Personnel: The design of the study meant that personnel delivering the intervention were aware which groups had been assigned to the different study conditions |
| Blinding of outcome assessment (detection bias) Independent observer reported outcomes | Low risk | Study investigators reported that "coders, blind to the hypotheses and group membership of the subjects, analyzed the videotapes" |
| Blinding of outcome assessment (detection bias) Parent reported outcomes | High risk | Outcome assessments by parents were not blinded as parents were aware of the intervention condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no reported losses to follow‐up |
| Selective reporting (reporting bias) | Low risk | The published report included all expected outcomes, including those that were prespecified |
| Other bias | Low risk | The study appeared to be free of other sources of bias |
APA: American Psychological Association DSM‐IV: Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition ICC: intracluster correlation coefficient NR: not reported SD: standard deviation SSHRC: Social Sciences and Humanities Research Council STAR: stop, think, ask, respond
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTRN12615000166572 | Randomised; parent intervention includes an individual component as well as group‐based intervention |
| Adamson 2013 | Randomised; parent training includes an individual component as well as group‐based training |
| Adesso 1981 | Randomised; child age not birth to 3 years; control group meets inclusion criteria; group‐based parent training |
| Bamba 2000 | Randomised; child age not birth to 3 years |
| Barber 1992 | Control group meets inclusion criteria; child age not birth to 3 years |
| Baydar 2003 | Randomised; children did not meet the age criterion (mean age greater than 3 years and 11 months for all children: "The mean age of the group was 55.8 months (4.65 years) at the time of pre‐intervention assessment" (Baydar 2008 [pers comm]); TAU control group ("Regular Head Star curriculum"); intervention was group‐based |
| Benjamin 2010 | Randomised; child age not birth to 3 years |
| Bergan 1983 | No standardised child outcome measures |
| Billingham 1994 | Quasi‐randomised; child age not birth to 3 years; details of control group not reported |
| Bor 2002 | Randomised; children did meet age criterion (mean age 3 years and 11 months for all children); wait‐list group; interventions were not group‐based (10 or 12 sessions were delivered on an individual basis) |
| Brody 1985 | Child age not birth to 3 years; no additional information |
| Brotman 2003 | Randomised report of a pilot study; mean age under 3 years and 11 months for all children; no‐treatment control group; preventive intervention programme consisted not only of group sessions (n = 50) but also of individualised home visits (n = 10) |
| Brotman 2005a | Randomised; children did not meet age criterion (range 2 years and 9 months to 5 years and 3 months); no‐intervention control group; intervention consisted not only of group sessions (n = 22) but also of individualised home visits (n = 10) |
| Brunk 1987 | Randomised to either of 2 treatment conditions; child age not birth to 3 years |
| Cerezo 1999 | Randomised; group‐based parent training; no child outcomes reported |
| Conner 2011 | Intervention includes a child programme together with the parenting programme |
| Constantino 2001 | Intervention includes an individual component ‐ home visitation |
| Cook 2012 | Randomised; intervention includes an individual component |
| CPPRG 2000 | Child age not birth to 3 years; multimodal; not solely group‐based |
| Cunningham 1995 | Block randomised; child age not birth to 3 years (mean age 54.2 months for community Intervention group, 52.3 months for clinic Intervention group, and 54.1 months for wait‐list control group); group‐based training; community intervention compared with clinic‐based intervention and wait‐list control |
| Dadds 1992 | No control group; child age not birth to 3 years |
| Drummond 2005 | Randomised; dual treatment cross‐over design; children did not meet age criterion (mean age 49.22 months); type of control group not specified; intervention was not group‐based |
| Dubey 1977 | Randomised; child age not birth to 3 years |
| EHSRC 2001 | Randomised; children did meet age criterion; intervention was not solely group‐based ("Participation in group parenting activities was lower than participation in other key services. Overall, slightly more than half of the families reported that they had attended an Early Head Start group parenting activities by the time of the second follow‐up" p 90) |
| Esdaile 1996 | Child age 2 to 3.5 years; further data not available from author |
| Fanning 2007 | Randomised; children did not meet age criterion (3 to 5 years old, mean age 56 months for treatment group and 55 months for control group); wait‐list control group; intervention was group‐based |
| Farrar 2005 | Randomised; children meet age criterion; control group meets inclusion criteria (placebo control group); intervention was group‐based; no relevant outcome measures (all outcomes were related to parent or parent's perception; not specific ratings of child's emotional and behavioural adjustment) |
| Farris 2013 | Randomised; outcomes in mothers only |
| Feinberg 2010 | Randomised; group‐based intervention began during the prenatal period |
| Fleming 2002 | Randomised; children did not meet age criterion (3 to 4 years old, mean age 50 months); normal service provision control group; no group‐based intervention (intervention delivered individually in participants' homes) |
| Forgatch 1979 | Randomised; children aged 3 to 5; parent training materials evaluated |
| Formiga 2004 | Randomised; children did meet age criterion (mean age 3 months and 6 days); normal service provision control group; it is not clear whether intervention was group‐based |
| Fujiwara 2011 | Not randomised or quasi‐randomised; cohort study |
| Glazebrook 2007 | Randomised; pre‐term infants in NICU; not measuring child emotional and behavioural adjustment |
| Gross 2014 | Randomised; Comparison of 2 active group‐based parent training programmes (Parent‐Child Interaction Therapy and Chicago Parent Program); No no‐intervention control group |
| Hanisch 2006 | Unclear from abstract whether study was a RCT or a quasi‐RCT; children did not meet age criterion (range 3 to 6 years); no‐treatment control group; group‐based intervention; full paper was in German |
| Harris 1989 | Child age not birth to 3 years |
| Hawkins‐Walsh 2007 | Not randomised or quasi‐randomised; commentary |
| Hayes 2008 | Randomised; intervention includes individual component |
| Helfenbaum‐Kun 2007 | Randomised; children did not meet age criterion (range 3 to 5 years, mean age 4 years); no‐treatment control group; intervention was group‐based |
| Hutchings 2008 | Not randomised or quasi‐randomised; commentary |
| Joachim 2010 | Randomised; children did not meet age criterion (range 2 to 6 years) |
| Johnson 1981 | Randomised; does not report on child emotional and behavioural adjustment outcomes |
| Kalymon 2009 | Randomised; no control group; same intervention administered a few weeks apart |
| Kern 2007 | Randomised; child age 3 to 5 years (mean age 53.2 months for MCI group and 54.1 months for PE group); control group did not meet the inclusion criteria; parent education and individualised assessment‐based intervention versus parent education |
| Lambermon 1989 | Randomised; child age birth to 3 years; not group‐based parent training |
| Letourneau 2001 | Randomised; first study: children meet age criterion (infants); second study: range (3 to 4 years) was within the age criterion, but mean age of all children was not reported; treatment‐as‐usual control group; intervention was not group‐based (the intervention was individually delivered in participants' homes) |
| Leung 2014 | Randomised; group‐based intervention (Grandparent Triple P) targeted grandparents who were not primary caregivers |
| Markie‐Dadds 2006 | Randomised; children meet age criterion (range 2 to 5 years, mean age 42.91 months for intervention group and 43.26 months for control group); wait‐list control group; intervention was not group‐based (self administered behavioural family intervention programme) |
| Mazza 2002 | Randomised; children meet age criterion (mean age 9 months for all children); treatment‐as‐usual control group; intervention not solely group‐based (intervention consisted of individual and group counselling, educational/vocational referrals, medical care and referrals, and housing and legal advocacy) |
| McBride 1991a | Randomised, child too old (range 25 to 64 months); wait‐list control group; group‐based parent training; no child outcome measures |
| McDade 1998 | Inappropriate outcome measures (not behavioural) |
| McGoey 2005 | Randomised; children did not meet age criterion (range 3 to 5 years, mean age 4 years); treatment‐as‐usual control group; intervention was group‐based |
| Melhuish 2007 | Not randomised or quasi‐randomised; commentary |
| Mendelsohn 2007 | Randomised; children did meet age criterion (new born babies, assessment took place at 33 months of age); treatment‐as‐usual control group; intervention was delivered on an individual basis during paediatrician visits (30‐ to 45‐minute sessions) |
| Minkovitz 2003 | Randomised and quasi‐randomised (6 randomisation and 9 quasi‐randomisation sites); children did meet age criterion (newborns up to 4 weeks of age were enrolled at birth and followed up to age 3 years); normal service provision control group; intervention was not group‐based (intervention consisted mainly of visits with physician, home visits etc.; parents were also offered support and learning opportunities in groups, as part of the intervention) |
| Moxley‐Haegert 1983 | Randomised; child age birth to 3 years; not group‐based parent training |
| Neef 1995 | Child age not birth to 3 years |
| Nixon 2004 | Randomised to 2 treatment conditions or control group; children did not meet age criterion (mean age 47.36 months for STD group and 48.30 months for ABB group); no‐treatment control group; intervention was not group‐based |
| Nurcombe 1984 | Randomised; child age birth to 3 years; not group‐based parent training |
| O'Brien Caughy 2004 | Randomised; children meet age criterion; control group meets inclusion criteria (placebo control group); type of control group not specified; intervention was not group‐based (intervention consisted of 9 standard paediatric office visits and 6 home visits) |
| Ostergren 2003 | Quasi‐randomised; children meet age criterion; no‐treatment control group; intervention was not group‐based (participants received individualised or generic guidance) |
| Oswalt 2013 | Randomised; pre‐term infants in NICU |
| Owen 2007 | Not randomised or quasi‐randomised; children meet age criterion (range 27 to 64 months); type of control group not specified; intervention was group‐based |
| Perez‐Nieves 2001 | Not truly randomised or quasi‐randomised: 2 intervention arms of the study were randomised but control group was partially a convenience sample of those who could not attend the intervention groups; children meet age criterion; control group meets the inclusion criteria; intervention was group‐based |
| Perou 2012 | Randomised; intervention included an individual component |
| Pisterman 1989 | Randomised; child age not birth to 3 years; wait‐list control; group‐based |
| Pitts 2001 | Randomised, children aged 3 to 12 years |
| Plant 2007 | Randomised; children did not meet age criterion; wait‐list control group; focus of the study were children with developmental disabilities |
| Puckering 1994 | No child outcome measures; no control group |
| Quinn 2007 | Randomised; children did not meet age criterion (mean age 4.95 years for intervention group and 4.83 years for control group); wait‐list control group, intervention was group‐based |
| Rapee 2005 | Randomised; children did not meet age criterion (some children were older than 5 years of age, range 36 to 62 months, mean age 47.3 months for intervention group and 46.1 months for control group); no‐treatment control group; intervention was group‐based |
| Reedtz 2011 | Children were above age for inclusion ‐ range 2 to 8 years, mean age 47.4 months for boys and 45.7 months for girls |
| Roosa 1983 | Not group‐based parent training |
| Routh 1995 | Child age not birth to 3 years |
| Sanders 2000 | Randomised; not group‐based parent training |
| Sanders 2004 | Randomised; children did not meet age criterion (mean age 53.71 months for SBFI control group and 52.84 months for EBFI group); normal service provision control group; intervention was group‐based (intervention consisted of 4 additional group sessions targeting risk factors; normal service provision intervention consisted of 4 group sessions and 4 individual telephone sessions; both the intervention and the control group received normal service provision treatment) |
| Sanders 2007 | Randomised to 1 of 3 intervention conditions or to a wait‐list control condition; range 36 to 48 months at baseline (mean age not reported); wait‐list control group; interventions were not group‐based (interventions were self directed behavioural family therapy or interventions delivered on an individual basis) |
| Schachman 2001 | Randomised; participants were primiparous, expectant mothers, who were between 22 and 32 weeks gestation; normal service provision control group; intervention was group‐based Baby Boot Camp (BBC) education programme; study did not include any outcomes measuring infant mental health |
| Schappin 2013 | Randomised; parents of pre‐term infants and of term infants born with perinatal asphyxia |
| Shaw 2006 | Randomised; children did meet age criterion (range 17 to 26 months, mean age 24.1 months for all children); no‐treatment control group; intervention was not group‐based (intervention was delivered on an individual basis at participants' homes) |
| Sheeber 1994 | Randomised; mean age 4 years; wait‐list control; group‐based parent training |
| Shelton 2000 | Follow‐up study |
| Shrewsberry 1978 | Randomised; mean age 10.14 years |
| Siegert 1980 | Randomised; child age not birth to 3 years; no treatment control group; group‐based |
| Sonuga‐Barke 2001 | Randomised; children did meet age criterion (3‐year‐old children, mean age not reported); wait‐list control group; intervention was not group‐based (intervention was delivered on an individual basis in participants' homes) |
| Sonuga‐Barke 2004 | Randomised; children did meet age criterion (3‐year‐old children, mean age not reported); wait‐list control group; intervention was not group‐based (intervention was delivered on an individual basis in participants' homes) |
| St James‐Roberts 2001 | Randomised; children meet age criterion; treatment‐as‐usual control group; intervention was not group‐based (2 interventions were delivered on an individual basis in participants' homes) |
| Strayhorn 1989 | Childrens' ages ranged from 2 to 5 years; control group does not fit inclusion criteria |
| Taylor 1997 | Randomised; compares group well child care with individual well child care |
| Taylor 2011 | Randomised; mean age 5.3 years |
| Thomas 1977 | Randomised; severely emotionally disturbed children identified by Chatham‐Effingham Psychoeducational Center |
| Trillingsgaard 2015 | Randomised; group‐based intervention (Family Startup Program) started during pregnancy; Child socioemotional development (classified as tertiary outcome) assessed at ages 9 and 18 months |
| Truss 1977 | In addition to the group‐based intervention, booklets were mailed to parents in the experimental group on a monthly basis until the infant was 48 months of age |
| Tuerk 2008 | Randomised; mean age 10.6 years |
| Turner 1994 | Not group‐based parent training |
| Turner 2006 | Randomised; children did not meet age criterion (range 2 to 6 years); wait‐list control group; intervention was not group‐based (intervention was delivered on an individual basis at a primary care setting) |
| US Health Department 2001 | Randomised; children did meet age criteria (12 months of age or younger at baseline); type of control group was not reported; intervention was not group‐based |
| Vogel 2000 | Age of children not reported, correlational reanalysis of a RCT |
| Webster‐Stratton 2001 | Randomised; children did not meet age criterion (4 years old); 2 interventions were compared; group‐based intervention was combined with some individually‐delivered sessions |
| Wint 1987 | Not group‐based parent training |
ABB: an abbreviated form of parent‐child interaction therapy EBFI: enhanced group behavioural family intervention MCI: multi‐component intervention NICU: neonatal intensive care unit PE: parent education RCT: randomised controlled trial SBFI: standard behavioural family intervention STD: standard Parent‐Child Interaction Therapy
Characteristics of studies awaiting assessment [ordered by study ID]
Farzadfard 2008.
| Methods | RCT |
| Participants | 51 mothers |
| Interventions | Child‐rearing training skills versus control |
| Outcomes | Mothers' stress Child behavioural problems |
| Notes | Article in Farsi; awaiting translation/review by a Farsi speaking reviewer |
Herbert 2007.
| Methods | RCT |
| Participants | Foster parents |
| Interventions | Child Wise Programme (CWP) versus waiting list control |
| Outcomes | Child Behavioural Checklist (CBCL) |
| Notes | Age of children unclear; we are trying to locate contact details of the authors to request this information |
ISRCTN39288126.
| Methods | RCT |
| Participants | Parents of children aged between 2 years and 9 months and 4 years and 6 months with positive screening for ADHD symptoms |
| Interventions | New Forest Parenting Programme (NFPP) versus Incredible Years (IY) versus treatment as usual |
| Outcomes | Change in parent‐reported ADHD symptoms as measured by the Swanson, Nolan and Pelham Questionnaire Fourth Version (SNAP‐IV) |
| Notes |
Trial registration: ISRCTN39288126 The study was completed in 2014. As yet, there are no published results. We contacted the authors for more information but they could not provide additional information about the study |
ISRCTN88988596.
| Methods | RCT |
| Participants | Mother‐infant dyads in which the infant is 4 to 9 months of age and the mother is a fluent speaker of German |
| Interventions | Circle of Security versus treatment‐as‐usual |
| Outcomes | Child Behaviour Checklist (CBCL) (parent‐reported) |
| Notes |
Trial registration: ISRCTN88988596 The study was completed in 2011. As yet, there are no published results. We contacted the authors for more information and are still awaiting their response |
Sandy 1983.
| Methods | RCT |
| Participants | 22 parents |
| Interventions | Child development information and parent/child conflict training versus control |
| Outcomes | Parental awareness Child perceptions of parental behaviour |
| Notes | PDF not available. It has been requested from the author who is trying to locate a copy |
Schlarb 2012.
| Methods | RCT |
| Participants | Parents of children aged 6 months to 4 years |
| Interventions | Multimodal short‐term group intervention program (Mini‐KiSS) versus waiting list control |
| Outcomes | Child sleep problems |
| Notes | Conference proceedings; we are trying to locate contact details of the authors to request more information |
Wang 2000.
| Methods | Controlled trial, unclear if randomised |
| Participants | Parents of 562 kindergarten children |
| Interventions | Lectures on child psychological development, child mental health, teaching attitudes and methods, and parents' rearing attitudes and discipline methods versus control |
| Outcomes | Child mental health status |
| Notes | Article in Chinese; awaiting translation |
Zhu 2014.
| Methods | RCT |
| Participants | Parents of children aged 3 to 4 years with anxiety symptoms |
| Interventions | Short‐term educational intervention with "collective curriculum" versus follow‐up only |
| Outcomes | Child anxiety symptoms |
| Notes | Article in Chinese; awaiting translation |
ADHD: attention deficit hyperactivity disorder RCT: randomised controlled trial PDF: portable document format
Characteristics of ongoing studies [ordered by study ID]
ISRCTN11079129.
| Trial name or title | Enhancing social and emotional health in the early years |
| Methods | RCT |
| Participants | Parents of children aged < 8 weeks at initial engagement |
| Interventions | Incredible Years versus service as usual |
| Outcomes | Behaviour – measured at 18‐month follow‐up using parent report Eyberg Child Behaviour Inventory (ECBI) |
| Starting date | February 2015 |
| Contact information | sarah.blower@york.ac.uk |
| Notes | Trial registration: ISRCTN11079129 |
ISRCTN16513449.
| Trial name or title | The Children and Parents in Focus project: a population‐based cluster‐randomised controlled trial to prevent behavioural and emotional problems in children |
| Methods | RCT |
| Participants | Parents of 3, 4, and 5 year‐old children who attend annual check‐up |
| Interventions | Triple‐P (level 2) versus Triple P (level 2, 3, & 4) versus treatment‐as‐usual |
| Outcomes | Strengths and Difficulties Questionnaire (SDQ) (reported by mothers, fathers, and teachers) |
| Starting date | August 2013 |
| Contact information | anna.sarkadi@kbh.uu.se |
| Notes | Trial registration: ISRCTN16513449 |
ISRCTN17488830.
| Trial name or title | Evaluation of a group‐based, early parenting intervention |
| Methods | Multicentre non‐randomised study |
| Participants | Parents aged 16 years or older, willing and able to participate in the programme and/or are willing and able to participate in the research, living in the target research areas. Must have a very good working knowledge of English |
| Interventions | The Parent and Infant (PIN) programme versus "services as usual" (SAU) |
| Outcomes | Parent and infant relationships, child development and socioemotional adjustment, infant temperament |
| Starting date | 1 Aug 2014 |
| Contact information | grainne.nimhaille@gmail.com |
| Notes |
ADHD: attention deficit hyperactivity disorder RCT: randomised controlled trial
Differences between protocol and review
Methods
Criteria for considering studies for this review
Types of participants
In this updated review we clarified the criteria for inclusion in terms of the age of the participants. The previously published version stated that children with a mean age between birth and three years were included. We clarified this to state that the review includes children with a maximum mean age of three years and 11 months.
Studies were excluded where they targeted parents of children under three years of age with specific conditions other than emotional and behavioural problems (e.g. physical disabilities, autism, etc.). When the protocol for this review was first published in 2001 (Parsons 2001), the inclusion criteria did not state this explicitly. The first published versions of the review (Barlow 2002a; Barlow 2002b; Barlow 2003b), and a subsequent update (Barlow 2010), included studies that did not have participants who were disabled, and parent training programmes for children with disabilities, such as attention deficit hyperactivity disorder (ADHD), were covered by other Cochrane systematic reviews.
Our intention was always to evaluate studies on parent training with child participants who had no disabilities other than emotional and behavioural problems, as we felt that children with disabilities might be the focus of more targeted, parent training programmes and therefore different in concept and delivery. Also, we did not envisage that young children would be diagnosed with, for example, autism or ADHD, although children are now being diagnosed earlier with these conditions. For this update, we carefully considered the implications of including studies with disabled children and decided to continue to only include trials of parent training programs for children without disabilities. However, no studies that had disabled child participants were, in fact, excluded.
In the previous versions of this review there was only one primary outcome covering child emotional and behavioural problems in general, and no secondary outcomes (Barlow 2002a; Barlow 2002b; Barlow 2003b; Barlow 2010). For this update, we decided to add secondary outcomes to include more specific problem areas. Child emotional and behavioural problems can be structured hierarchically, with one broad category that can be divided into two narrower categories: internalising and externalising problems. Internalising and externalising problems are quite different, both in nature and in their manifestations, and different interventions might be necessary for the different categories. Each of the two narrower categories can be further categorised, providing even more specific outcomes that may be important for the choice of intervention. Social skills and child‐parent interaction are other, clinically important, aspects of emotional and behavioural adjustment.
Data synthesis
When carrying out the update we discovered that studies often reported both the total and subscale scores for the same measure. As such, where both the total score of the scale and a subscale were reported, we report on the subscale (i.e. not the total score as well) because to report both would introduce linear dependencies among the measures (Shadish 1992). Although it is not clear whether total scores or subscales are more reliable, subscales provide more specific information (Shadish 1992).
'Summary of findings' table
The updated review includes a 'Summary of findings' table in line with updated Cochrane guidelines.
Search methods for identification of studies
Electronic searches
We increased the sensitivity of the search for this update by expanding the section on parent training to include phrases such as 'positive parenting' and 'parenting support', and by adding 'children' to our search terms for participants. In order to refine the large number of records produced by the revised search, we also added a filter to limit the records to RCTs.
Data collection and analyses
Assessment of heterogeneity
For this updated review, we also report tau (Tau²), to assess between‐study variability.
Sensitivity analyses
For this updated review, we planned to carry out sensitivity analyses to test if the findings of the meta‐analyses were robust, by examining the effect of variables between the studies, such as older participants, RCTs, quasi‐RCTs, and cluster‐RCTs. This was not explicitly described in earlier versions of the published review (Barlow 2002a; Barlow 2002b; Barlow 2003b; Barlow 2010), and is a departure from protocol (Parsons 2001).
Results
Description of studies
Excluded studies
In the amended 2009 review, we revised the excluded studies list so that it listed only those studies that appeared initially to fit the inclusion criteria but after examination of the abstract or full‐text, the studies were excluded. In practice, this meant that some previously excluded studies no longer appear as they did not meet any of the inclusion criteria, for example, studies that were review articles and non‐randomised studies. For some of the previously excluded studies we only reviewed the abstracts, and where no further information was available from the abstracts, we have stated this in the Characteristics of excluded studies table.
Changes in authors teams and review titles
In the fourth version of the review (Barlow 2010), one of the authors of the first review version (Barlow 2002a), J Parsons, did not contribute. Four new authors were included the fourth review version: N Smailagic, M Ferriter, C Bennett and H Jones (Barlow 2010). In this updated version, N Smailagic, M Ferriter and H Jones did not contribute, and H Bergman, H Kornør and Y Wei have been added as new authors.
The updated review title, 'Group‐based parent training programmes for improving emotional and behavioural adjustment in young children', has been changed from 'Group‐based parent‐training programmes for improving emotional and behavioural adjustment in children from birth to three years old' (Barlow 2010), which was changed from 'Group‐based parent‐training programmes for improving emotional and behavioural adjustment in 0‐3 year old children' (Barlow 2002a).
Contributions of authors
JB: Updated and wrote the background and discussion sections, edited the methods, wrote up the results, and gave advice about the set up of the analyses. She has overall responsibility for ensuring data in the review are correct.
HB: Contributed to the 2015 update by screening studies, extracting data, analysing the data, updating the text in the methods and results sections, performing GRADE, and constructing the 'Summary of findings' table.
HK: Contributed to the 2015 update by screening studies, extracting data, updating the text in the results sections, providing methodological support, and helping to update the text in the methods section of the review.
YW: Contributed to the 2015 update by providing statistical support.
CB: Worked with all review authors to ensure that the review met publication deadlines. CB contributed to the methods section, analyses, recorded outcomes for drafts of the 'Additional tables' and 'Characteristics of excluded studies' tables. She also provided general review and publication support.
Sources of support
Internal sources
-
Health Services Research Unit at the University of Warwick, UK.
Staff time and other resources for the review.
-
Institute of Mental Health, Nottinghamshire Healthcare National Health Service (NHS) Trust, UK.
Staff time and other resources for the review. The views expressed are those of the authors and not necessarily those of the Institute of Mental Health or the NHS.
-
Regional Centre for Child and Adolescent Mental Health, Eastern and Southern Norway (RBUP), Norway.
Staff time and other resources for the review.
External sources
-
NHS National Institute of Health Research (NIHR) Cochrane Collaboration Programme Grant Scheme, UK.
Staff time and other resources for the review. The views expressed are those of the authors and not necessarily those of the NIHR or the NHS.
Declarations of interest
Jane Barlow: Receives royalties for a book entitled 'Keeping the Baby in Mind'. Jane is an Editor for the Cochrane Developmental, Psychosocial and Learning Problems Group (CDPLPG).
Hanna Bergman: Works for Enhance Reviews Ltd. and was paid for her contribution to this review. Enhanced Reviews Ltd. is a private company that performs systematic reviews of literature and currently does not work with the pharmaceutical industry.
Hege Kornør: Associate Editor for CDPLPG.
Yinghui Wei: Statistical Editor for CDPLPG.
Cathy Bennett: Proprietor of Systematic Research Ltd, a company providing research services, and is also an employee of that company. Cathy receives a consultancy fee for her contribution to other Cochrane reviews and work in evidence‐based medicine, which includes screening search results, extracting data, co‐ordinating research and drafting text and reports, etc., and travel expenses are paid by clients. However, for this review, she did not receive any payment or fee. Travel expenses are paid to Cathy for travel related to the review. She has worked as Review Group Co‐ordinator (Managing Editor) for the Cochrane Upper Gastrointestinal and Pancreatic Diseases Review Group in the past. Cathy does not perceive a conflict of interest but makes this statement in the interest of full disclosure. Cathy is a member of the data monitoring committee for Barrett's Oesophagus Surveillance Study (BOSS), a clinical trial of surveillance intervals for Barrett's oesophagus. This work is not related to review writing.
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Bradley 2003 {published data only}
- Bradley SJ, Jadaa DA, Brody J, Landy S, Tallet S, Watson W, et al. Brief psychoeducational parenting program: an evaluation and 1‐year follow‐up. Journal of the American Academy of Child and Adolescent Psychiatry 2003;42(10):1171‐8. [PUBMED: 14560166] [DOI] [PubMed] [Google Scholar]
Breitenstein 2012 {published data only}
- Breitenstein SM, Gross D, Fogg L, Ridge A, Garvey C, Julion W, et al. The Chicago Parent Program: comparing 1‐year outcomes for African American and Latino parents of young children. Research in Nursing & Health 2012;35(5):475‐89. [PUBMED: 22622598] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross D, Garvey C, Julion W, Fogg L, Tucker S, Mokros H. Efficacy of the Chicago parent program with low‐income African American and Latino parents of young children. Prevention Science 2009;10(1):54‐65. [PUBMED: 19067166] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross D, Garvey C, Julion WA, Fogg L. Preventive parent training with low‐income, ethnic minority families of preschoolers. In: Briesmeister JM, Schaefer CE editor(s). Handbook of Parent Training: Helping Parents Prevent and Solve Problem Behaviours. 3rd Edition. New York: John Wiley & Sons, 2007:5‐24. [Google Scholar]
Cummings 2000 {unpublished data only}
- Cummings LL. Parent Training: A Program for Parents of Two‐ and Three‐Year‐Olds [PhD thesis]. Michigan, USA: Central Michigan University, 2000. [Google Scholar]
Dittman 2015 {published data only}
- Dittman CK, Farruggia SP, Keown LJ, Sanders MR. Dealing with disobedience: an evaluation of a brief parenting intervention for young children showing noncompliant behavior problems. Child Psychiatry and Human Development 2015 April 12 [Epub ahead of print]. [DOI: 10.1007/s10578-015-0548-9] [DOI] [PubMed]
Griffith 2012 {published data only}
- Griffith N. Evaluating the Incredible Years Toddler Programme in Disadvantaged Areas of Wales [PhD thesis]. Bangor, Wales: Bangor University, 2012. [Google Scholar]
Gross 1995 {published data only}
- Gross D, Fogg L, Tucker S. The efficacy of parent training for promoting positive parent‐toddler relationships. Research in Nursing & Health 1995;18(6):489‐99. [PUBMED: 7480850] [DOI] [PubMed] [Google Scholar]
Gross 2003 {published data only}
- Gross D, Fogg L, Webster‐Stratton C, Garvey C, Julion W, Grady J. Parent training of toddlers in day care in low‐income urban communities. Journal of Consulting and Clinical Psychology 2003;71(2):261‐78. [PUBMED: 12699021] [DOI] [PubMed] [Google Scholar]
Hiscock 2008 {published data only}
- Hiscock H, Bayer JK, Price A, Ukoumunne OC, Rogers S, Wake M. Universal parenting programme to prevent early childhood behavioural problems: cluster randomised trial. BMJ 2008;336(7639):318‐21. [PUBMED: 18244958 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hutchings 2007 {published data only}
- Edwards RT, Céilleachair A, Bywater T, Hughes DA, Hutchings J. Parenting programme for parents of children at risk of developing conduct disorder: cost effectiveness analysis. BMJ 2007;334(7595):682‐5. [PUBMED: 17350965] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchings J [pers comm]. Parenting intervention in Sure Start services for children at risk of developing conduct disorder: pragmatic randomised controlled trial [personal communication]. Email to: H Kornør 14 January 2015. [DOI] [PMC free article] [PubMed]
- Hutchings J, Bywater T, Daley D, Gardner F, Whitaker C, Jones K, et al. Parenting intervention in Sure Start services for children at risk of developing conduct disorder: pragmatic randomised controlled trial. BMJ 2007;334(7595):678‐82. [PUBMED: 17350966] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones K, Daley D, Hutchings J, Bywater T, Eames C. Efficacy of the Incredible Years Basic parent training programme as an early intervention for children with conduct problems and ADHD. Child: Care, Health and Development 2007;33(6):749‐56. [PUBMED: 17944785] [DOI] [PubMed] [Google Scholar]
Kennedy 2009 {published data only}
- Kennedy SJ, Rapee RM, Edwards SL. A selective intervention program for inhibited preschool‐aged children of parents with an anxiety disorder: effects on current anxiety disorders and temperament. Journal of the American Academy of Child and Adolescent Psychiatry 2009;48(6):602‐9. [PUBMED: 19454916] [DOI] [PubMed] [Google Scholar]
Little 2012 {published data only}
- Little M, Berry V, Morpeth L, Blower S, Axford N, Taylor R, et al. The impact of three evidence‐based programmes delivered in public systems in Birmingham, UK. International Journal of Conflict and Violence 2012;6(2):260‐72. [Google Scholar]
Morawska 2011 {published data only}
- Morawska A [pers comm]. Evaluation of a brief parenting discussion group for parents of young children [personal communication]. Email to: H Kornør 19 January 2015.
- Morawska A, Haslam D, Milne D, Sanders MR. Evaluation of a brief parenting discussion group for parents of young children. Journal of Developmental and Behavioral Pediatrics 2011;32(2):136‐45. [PUBMED: 20814338] [DOI] [PubMed] [Google Scholar]
Morawska 2014 {published data only}
- Morawska A, Adamson M, Hinchliffe K, Adams T. Hassle Free Mealtimes Triple P: a randomised controlled trial of a brief parenting group for childhood mealtime difficulties. Behaviour Research and Therapy 2014;53:1‐9. [PUBMED: 24362359] [DOI] [PubMed] [Google Scholar]
Niccols 2008 {published data only}
- Niccols A. 'Right from the Start': randomized trial comparing an attachment group intervention to supportive home visiting. Journal of Child Psychology and Psychiatry, and Allied Disciplines 2008;49(7):754‐64. [PUBMED: 18355218] [DOI] [PubMed] [Google Scholar]
- Niccols A [pers comm]. 'Right from the Start': Randomized trial comparing an attachment group intervention to supportive home visiting [personal communication]. Email to: H Kornør 28 January 2015. [DOI] [PubMed]
Niccols 2009 {published data only}
- Niccols A. Immediate and short‐term outcomes of the 'COPEing with Toddler Behaviour' parent group. Journal of Child Psychology and Psychiatry, and Allied Disciplines 2009;50(5):617‐26. [PUBMED: 19076262] [DOI] [PubMed] [Google Scholar]
- Niccols A [pers comm]. Immediate and short‐term outcomes of the 'COPEing with Toddler Behaviour' parent group [personal communication]. Email to: H Kornør 19 January 2015. [DOI] [PubMed]
Nicholson 1998 {published data only}
- Janz PC. The effectiveness of an education program for parents of young children. Dissertation Abstracts International Section A: Humanities and Social Sciences 1997;58:0058. [Google Scholar]
- Nicholson B, Janz P, Fox R. Evaluating a brief parental‐education program for parents of young children. Psychological Reports 1998;82(3 Pt 2):1107‐13. [PUBMED: 9709516] [DOI] [PubMed] [Google Scholar]
Nicholson 2002 {published data only}
- Fox R [pers comm]. One family at a time: a prevention program for at‐risk parents [personal communication]. Email to: H Kornør 15 January 2015.
- Nicholson B, Anderson M, Fox R, Brenner V. One family at a time: a prevention program for at‐risk parents. Journal of Counseling & Development 2002;80(3):362‐71. [DOI: 10.1002/j.1556-6678.2002.tb00201.x] [DOI] [Google Scholar]
Oré 2011 {published data only}
- Oré B, Díaz JJ, Penny M. Impact of a group intervention with mothers and babies on child development [Impacto de una intervención con grupos de mamás y bebes en el desarrollo infantil]. Revista de Psicología 2011;29(1):37‐66. [Google Scholar]
Perrin 2014 {published data only}
- NCT00402857. Advanced Parenting Education in Pediatrics: The APEP Project. 1.usa.gov/1Cshfes (accessed 23 June 2015).
- Perrin E [pers comm]. Improving parenting skills for families of young children in pediatric settings: a randomized clinical trial [personal communication]. Email to: H Kornør 15 January 2015. [DOI] [PubMed]
- Perrin EC, Sheldrick RC, McMenamy JM, Henson BS, Carter AS. Improving parenting skills for families of young children in pediatric settings: a randomized clinical trial. JAMA Pediatrics 2014;168(1):16‐24. [PUBMED: 24190691] [DOI] [PubMed] [Google Scholar]
Simkiss 2013 {published data only}
- Simkiss DE, Snooks HA, Stallard N, Kimani PK, Sewell B, Fitzsimmons D, et al. Effectiveness and cost‐effectiveness of a universal parenting skills programme in deprived communities: multicentre randomised controlled trial. BMJ Open 2013;3(8):e002851. [DOI] [PMC free article] [PubMed] [Google Scholar]
Solís‐Cámara 2004 {published data only}
- Solís‐Cámara PR, Covarrubias Salcido P, Díaz Romero M, Rivera Aguirre BI. Multidimensional effects of a parenting program on the reciprocal interaction between parents and their young children with behavior problems [Efectos multidimensionales de un programa de crianza en la interacción recíproca entre padres y sus niños pequeńos con problemas de comportamiento]. Behavioural Psychology 2004;12(2):197‐214. [Google Scholar]
Sutton 1992 {published data only}
- Sutton C. Training parents to manage difficult children ‐ a comparison of methods. Behavioural Psychotherapy 1992;20(2):115‐39. [DOI: 10.1017/S0141347300016906] [DOI] [Google Scholar]
Tiedemann 1992 {published data only}
- Johnston C [pers comm]. Parent training article details [personal communication]. Email to: H Kornør 20 January 2015.
- Tiedemann GL, Johnston C. Evaluation of a parent training program to promote sharing between young siblings. Behavior Therapy 1992;23(2):299‐318. [DOI: 10.1016/S0005-7894(05)80387-9] [DOI] [Google Scholar]
Webster‐Stratton 1982 {published data only}
- Webster‐Stratton C. Teaching mothers through videotape modeling to change their children's behavior. Journal of Pediatric Psychology 1982;7(3):279‐94. [DOI: 10.1093/jpepsy/7.3.279] [DOI] [PubMed] [Google Scholar]
- Webster‐Stratton C [pers comm]. Teaching mothers through videotape modeling to change their children's behavior [personal communication]. Email to: H Kornør 27 January 2015. [DOI] [PubMed]
References to studies excluded from this review
ACTRN12615000166572 {published and unpublished data}
- Tully L, Hunt C. A randomised controlled trial comparing a brief and standard parenting intervention for toddler externalising and aggressive behaviours [trial protocol]. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=367843 2015.
- Tully L, Hunt C [pers comm]. A randomized controlled trial of a brief versus standard group parenting program for toddler aggression [personal communication]. Email to: H Kornør 18 August 2015. [DOI] [PubMed]
Adamson 2013 {published data only}
- Adamson M, Morawska A, Sanders MR. Childhood feeding difficulties: a randomized controlled trial of a group‐based parenting intervention. Journal of Developmental and Behavioral Pediatrics 2013;34(5):293‐302. [PUBMED: 23751884] [DOI] [PubMed] [Google Scholar]
Adesso 1981 {published data only}
- Adesso VJ, Lipson JW. Group training of parents as therapists for the children. Behavior Therapy 1981;12(5):625‐33. [Google Scholar]
Bamba 2000 {published data only}
- Bamba ML. Evaluating the Impact of Parent Education for Parents of Young Children. Oregon: University of Oregon, 2000. [Google Scholar]
Barber 1992 {published data only}
- Barber JG. Evaluating parent education groups: effects on sense of competence and social isolation. Research on Social Work Practice 1992;2(1):28‐38. [DOI: 10.1177/104973159200200103] [DOI] [Google Scholar]
Baydar 2003 {published data only}
- Author team [pers comm]. Email correspondence clarifying the age of the trial participants [personal communication]. Email to: N Baydar 5 May 2008.
- Baydar NRM, Reid MJ, Webster‐Stratton C. The role of mental health factors and program engagement in the effectiveness of a preventive parenting program for Head Start mothers. Child Development 2003; Vol. 74, issue 5:1433‐53. [PUBMED: 14552407] [DOI] [PubMed]
Benjamin 2010 {published data only}
- Benjamin JL. Biopsychosocial‐based versus behavioral‐based parenting model: a clinical trial for adoptive parents with attachment‐challenged children. Dissertation Abstracts International: Section B: The Sciences and Engineering 2010;71:3379. [Google Scholar]
Bergan 1983 {published data only}
- Bergan JR, Neumann AJ, Karp CL. Effects of parent training on parent instruction and child learning of intellectual skills. Journal of School Psychology 1983;21(1):31‐9. [DOI: 10.1016/0022-4405(83)90064-X] [DOI] [Google Scholar]
Billingham 1994 {published data only}
- Billingham SC. Evaluation research design for the family and schools together program (FAST). Dissertation Abstracts International: Section B: The Sciences and Engineering 1994;54:4908. [Google Scholar]
Bor 2002 {published data only}
Brody 1985 {published data only}
- Brody GH, Forehand R. The efficacy of parent training with maritally distressed and nondistressed mothers: a multimethod assessment. Behaviour Research and Therapy 1985;23(3):291‐6. [DOI: 10.1016/0005-7967(85)90007-5] [DOI] [PubMed] [Google Scholar]
Brotman 2003 {published data only}
- Brotman LM, Klein RG, Kamboukos D, Brown EJ, Coard SI, Sosinsky LS. Preventive intervention for urban, low‐income preschoolers at familial risk for conduct problems: a randomised pilot study. Journal of Clinical Child and Adolescent Psychology 2003;32(2):246‐57. [PUBMED: 12679283] [DOI] [PubMed] [Google Scholar]
Brotman 2005a {published data only}
- Brotman L, Gouley K, Chesir‐Teran D, Dennis T, Klein R, Shrout P. Prevention for preschoolers at high risk for conduct problems: immediate outcomes on parenting practices and child social competence. Journal of Clinical Child and Adolescent Psychology 2005; Vol. 34, issue 4:724‐34. [PUBMED: 16232069] [DOI] [PubMed]
Brunk 1987 {published data only}
- Brunk MA, Henggeler SW, Whelan JP. Comparison of multisystemic therapy and parent training in the brief treatment of child abuse and neglect. Journal of Consulting and Clinical Psychology 1987;55(2):171‐8. [DOI] [PubMed] [Google Scholar]
Cerezo 1999 {published data only}
- Cerezo MA, Dolz L Pons‐Salvador G, Cantero MJ. Infancy maltreatment prevention: a program impact on child development. Anales de Psicología 1999;15(2):239‐50. [Google Scholar]
Conner 2011 {published data only}
- Conner NW, Fraser MW. Preschool social‐emotional skills training: a controlled pilot test of the making choices and strong families programs. Research on Social Work Practice 2011;21(6):699‐711. [DOI: 10.1177/1049731511408115] [DOI] [Google Scholar]
Constantino 2001 {published data only}
- Constantino JN, Hashemi N, Solis E, Alon T, Haley S, McClure S, et al. Supplementation of urban home visitation with a series of group meetings for parents and infants: results of a "real‐world" randomized, controlled trial. Child Abuse & Neglect 2001;25(12):1571‐81. [DOI] [PubMed] [Google Scholar]
Cook 2012 {published data only}
- Cook F, Bayer J, Le HND, Mensah F, Cann W, Hiscock H. Study protocol: Baby Business: a randomised controlled trial of a universal parenting program that aims to prevent early infant sleep and cry problems and associated parental depression. BMC Pediatrics 2012;12:13. [DOI: 10.1186/1471-2431-12-13] [DOI] [PMC free article] [PubMed] [Google Scholar]
CPPRG 2000 {published data only}
- Conduct Problems Prevention Research Group. Merging universal and indicated prevention programs: the Fast Track model. Addictive Behaviors 2000;25(6):913‐27. [DOI: 10.1016/S0306-4603(00)00120-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cunningham 1995 {published data only}
- Cunningham CE, Bremner R, Boyle M. Large group community‐based parenting programs for families of preschoolers at risk for disruptive behavior disorders: utilization, cost‐effectiveness, and outcome. Journal of Child Psychology and Psychiatry, and Allied Disciplines 1995;36(7):1141‐59. [DOI] [PubMed] [Google Scholar]
Dadds 1992 {published data only}
- Dadds MR, McHugh TA. Social support and treatment outcome in behavioral family therapy for child conduct problems. Journal of Consulting and Clinical Psychology 1992;60(2):252‐9. [PUBMED: 1592955] [DOI] [PubMed] [Google Scholar]
Drummond 2005 {published data only}
Dubey 1977 {published data only}
- Dubey DR. Training parents of hyperactive children in child management: a comparative outcome study. Dissertation Abstracts International 1977;37:5828. [DOI] [PubMed] [Google Scholar]
EHSRC 2001 {published data only}
- Love J, Kisker E, Ross C, Raikes H, Constantine J, Boller K, et al. The effectiveness of Early Head Start for 3‐year‐old children and their parents: lessons for policy and programs. Developmental Psychology 2005; Vol. 41, issue 6:885‐901. [PUBMED: 16351335] [DOI] [PubMed]
- The Early Head Start Research Consortium. Building their Futures: How Early Head Start Programmes are Enhancing the Lives of Infants and Toddlers in Low‐Income Families. Summary report. New York: The Commissioner’s Office of Research and Evaluation and the Head Start Bureau, Administration on Children, Youth and Families, Department of Health and Human Services, 2001. [Google Scholar]
Esdaile 1996 {published data only (unpublished sought but not used)}
- Esdaile SE. A play‐focused intervention involving mothers of preschoolers. American Journal of Occupational Therapy 1996;50(2):113‐213. [DOI: 10.5014/ajot.50.2.113] [DOI] [PubMed] [Google Scholar]
Fanning 2007 {published data only}
- Fanning JL. Parent Training for Caregivers of Typically Developing, Economically Disadvantaged Preschoolers: An Initial Study in Enhancing Language Development, Avoiding Behavior Problems, and Regulating Family Stress [PhD thesis]. Oregon, USA: University of Oregon, 2007. [UMI: 3276047] [Google Scholar]
Farrar 2005 {published data only}
- Farrar RLE. The Effect of a Cognitively Based Parent Training Intervention on Parental Stress. Oklahoma, USA: The University of Tulsa, 2005. [UMI: 3161353] [Google Scholar]
Farris 2013 {published data only}
- Farris JR, Bert SSC, Nicholson JS, Glass K, Borkowski JG. Effective intervention programming: improving maternal adjustment through parent education. Administration and Policy in Mental Health 2013;40(3):211‐23. [PUBMED: 22246615] [DOI] [PubMed] [Google Scholar]
Feinberg 2010 {published data only}
- Feinberg ME, Jones D, Roettger ME, Hostettler M, Solmeyer A. Long‐term follow‐up of a randomized trial of family foundations: effects on children’s emotional, behavioral, and school adjustment. Journal of Family Psychology in press. [DOI] [PubMed]
- Feinberg ME, Jones DE, Kan ML, Goslin MC. Effects of family foundations on parents and children: 3.5 years after baseline. Journal of Family Psychology 2010;24(5):532‐42. [PUBMED: 20954763] [DOI] [PubMed] [Google Scholar]
Fleming 2002 {published data only}
- Fleming DS. Promoting Healthy Child Development: A Population Health Approach [PhD thesis]. Alberta, Canada: University of Alberta, 2002. [Google Scholar]
Forgatch 1979 {published data only}
- Forgatch MS, Toobert DJ. A cost‐effective parent training program for use with normal preschool children. Journal of Pediatric Psychology 1979;4(2):129‐45. [Google Scholar]
Formiga 2004 {published data only}
- Formiga CK, Pedrazzani ES, Silva FPDS, Lima CD. Effectiveness of the early intervention program with preterm infants [Eficácia de um programa de intervenção precoce com bebês pré‐termo]. Cadernos de Psicologia e Educação Paidéia 2004; Vol. 14, issue 29:301‐11. [DOI: 10.1590/S0103-863X2004000300006] [DOI]
Fujiwara 2011 {published data only}
- Fujiwara T, Kato N, Sanders MR. Effectiveness of Group Positive Parenting Program (Triple P) in changing child behavior, parenting style, and parental adjustment: an intervention study in Japan. Journal of Child and Family Studies 2011;20(6):804‐13. [DOI: 10.1007/s10826-011-9448-1] [DOI] [Google Scholar]
Glazebrook 2007 {published data only}
- Glazebrook C, Marlow N, Israel C, Croudace T, Johnson S, White IR, et al. Randomised trial of a parenting intervention during neonatal intensive care. Archives of Disease in Childhood ‐ Fetal & Neonatal Edition 2007;92:438‐43. [DOI: 10.1136/adc.2006.103135] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gross 2014 {published data only}
- Gross DA, Belcher HME, Ofonedu ME, Breitenstein S, Frick KD, Chakra B. Study protocol for a comparative effectiveness trial of two parent training programs in a fee‐for‐service mental health clinic: can we improve mental health services to low‐income families?. Trials 2014;15:70. [DOI: 10.1186/1745-6215-15-70] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hanisch 2006 {published data only}
- Hanisch C, Pluck J, Meyer N, Brix G, Freund‐Braier I, Hautmann C, et al. Short‐term effects of the indicated prevention programme for externalizing problem behaviour (Pep). Zeitschrift Fur Klinische Psychologie und Psychotherapie 2006; Vol. 35, issue 2:117‐26. [MEDLINE: ]
Harris 1989 {published data only}
- Harris JD, Larsen JM. Parent education as a mandatory component of preschool: effects on middle‐class, educationally advantaged parents and children. Early Childhood Research Quarterly 1989;4(3):275‐87. [DOI: 10.1016/0885-2006(89)90014-8] [DOI] [Google Scholar]
Hawkins‐Walsh 2007 {published data only}
- Hawkins‐Walsh E. A cognitive‐behavioural parenting intervention reduced problem behaviours in at‐risk preschool children and improved parenting skills in socially disadvantaged families. Evidence‐Based Nursing 2007;10(4):105. [PUBMED: 17905757] [DOI] [PubMed] [Google Scholar]
Hayes 2008 {published data only}
- Hayes L, Matthews J, Copley A, Welsh D. A randomized controlled trial of a mother‐infant or toddler parenting program: demonstrating effectiveness in practice. Journal of Pediatric Psychology 2008;33(5):473‐86. [PUBMED: 17938146] [DOI] [PubMed] [Google Scholar]
Helfenbaum‐Kun 2007 {published data only}
- Helfenbaum‐Kun E, Ortiz C. Parent‐training groups for fathers of Head Start children: a pilot study of their feasibility and impact on child behavior and intra‐familial relationships. Child & Family Behavior Therapy 2007; Vol. 29, issue 2:47‐64. [DOI: 10.1300/J019v29n02_04] [DOI]
Hutchings 2008 {published data only}
- Hutchings J. A parenting programme does not affect behavioural problems in toddlers. Evidence‐Based Mental Health 2008;11(4):119. [DOI: 10.1136/ebmh.11.4.119] [DOI] [PubMed] [Google Scholar]
Joachim 2010 {published data only}
- Joachim S, Sanders MR, Turner KM. Reducing preschoolers' disruptive behavior in public with a brief parent discussion group. Child Psychiatry and Human Development 2010;41(1):47‐60. [PUBMED: 19633952] [DOI] [PubMed] [Google Scholar]
Johnson 1981 {published data only}
- Johnson DL. The influence of an intensive parent education program on behavioral continuity of mothers and children. Child Study Journal 1981;11(4):187‐99. [Google Scholar]
Kalymon 2009 {published data only}
- Kalymon KM. Combining positive behavior support and functional assessment in a parent‐training program: an evaluation of effectiveness and outcomes. Dissertation Abstracts International: Section B: The Sciences and Engineering 2009;69:5765. [Google Scholar]
Kern 2007 {published data only}
- Kern L, DuPaul G, Volpe RJ, Sokol NG, Lutz JG, Arbolino LA, et al. Multisetting assessment‐based intervention for young children at risk for attention deficit hyperactivity disorder: initial effects on academic and behavioral functioning. School Psychology Review 2007; Vol. 36, issue 2:237‐55.
Lambermon 1989 {published data only}
- Lambermon MWE, IJzendoorn MH. Influencing mother‐infant interaction through videotaped or written instruction: evaluation of a parent education program. Early Childhood Research Quarterly 1989;4(4):449‐58. [Google Scholar]
Letourneau 2001 {published data only}
- Letourneau N, Drummond J, Fleming D, Kysela G, McDonald L, Stewart M. Supporting parents: can intervention improve parent‐child relationships?. Journal of Family Nursing 2001;7(2):159‐87. [DOI: 10.1177/107484070100700203] [DOI] [Google Scholar]
Leung 2014 {published data only}
- Leung C, Sanders M, Fung B, Kirby J. The effectiveness of the Grandparent Triple P program with Hong Kong Chinese families: a randomized controlled trial. Journal of Family Studies 2014;20(2):104‐17. [Google Scholar]
Markie‐Dadds 2006 {published data only}
- Markie‐Dadds C, Sanders MR. Self‐directed Triple P (Positive Parenting Program) for mothers with children at‐risk of developing conduct problems. Behavioural and Cognitive Psychotherapy 2006; Vol. 34, issue 3:259‐75. [DOI: 10.1017/S1352465806002797] [DOI]
Mazza 2002 {published data only}
- Mazza C. Young dads: the effects of a parenting program on urban African‐American adolescent fathers. Adolescence 2002; Vol. 37, issue 148:681‐93. [PUBMED: 12564822] [PubMed]
McBride 1991a {published data only}
- McBride BA. Parent education and support programs for fathers: outcome effects on paternal involvement. Early Child Development and Care 1991;67(1):73‐85. [DOI: 10.1080/0300443910670107] [DOI] [Google Scholar]
McDade 1998 {published data only}
- McDade A, McCartan P. 'Partnership with parents' a pilot project. International Journal of Language & Communication Disorders 1998;33 Suppl:556‐61. [PUBMED: 10343754] [DOI] [PubMed] [Google Scholar]
McGoey 2005 {published data only}
- McGoey KE, DuPaul GJ, Eckert TL, Volpe RJ, Brakle J. Outcomes of a multi‐component intervention for preschool children at‐risk for attention‐deficit/hyperactivity disorder. Child & Family Behavior Therapy 2005; Vol. 27, issue 1:34‐56. [DOI: 10.1300/J019v27n01_03] [DOI]
Melhuish 2007 {published data only}
- Melhuish EC. Parenting training improves problem behaviour in children at risk of conduct disorder. Evidence‐Based Mental Health 2007;10(4):125. [DOI: 10.1136/ebmh.10.4.125] [DOI] [PubMed] [Google Scholar]
Mendelsohn 2007 {published data only}
- Mendelsohn A, Valdez P, Flynn V, Foley G, Berkule S, Tomopoulos S, et al. Use of videotaped interactions during pediatric well‐child care: impact at 33 months on parenting and on child development. Journal of Developmental and Behavioral Pediatrics 2007; Vol. 28, issue 3:206‐12. [PUBMED: 17565287] [DOI] [PMC free article] [PubMed]
Minkovitz 2003 {published data only}
Moxley‐Haegert 1983 {published data only}
- Moxley‐Haegert L, Serbin LA. Developmental education for parents of delayed infants: effects on parental motivation and children's development. Child Development 1983;54(5):1324‐31. [PUBMED: 6194944] [PubMed] [Google Scholar]
Neef 1995 {published data only}
- Neef NA. Pyramidal parent training by peers. Journal of Applied Behavior Analysis 1995;28(3):333‐7. [DOI: 10.1901/jaba.1995.28-333] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nixon 2004 {published data only}
Nurcombe 1984 {published data only}
- Nurcombe B, Howell DC, Rauh VA, Teti DM, Ruoff P, Brennan J. An intervention program for mothers of low‐birthweight infants: preliminary results. Journal of the American Academy of Child Psychiatry 1984;23(3):319‐25. [DOI: 10.1016/S0002-7138(09)60511-2] [DOI] [PubMed] [Google Scholar]
O'Brien Caughy 2004 {published data only}
- O'Brien Caughy M, Huang K‐Y, Miller T, Genevro JL. The effects of the Healthy Steps for Young Children Program: results from observations of parenting and child development. Early Childhood Research Quarterly 2004;19(4):611‐30. [DOI: 10.1016/j.ecresq.2004.10.004] [DOI] [Google Scholar]
Ostergren 2003 {published data only}
- Ostergren C. Evaluation of a Temperament‐Based Parenting Program: Factors Affecting Program Usefulness, Ease of Understanding, Preferred Amount of Materials and Parental Attitudes [PhD thesis]. Vol. 64, Madison: University of Wisconsin, 2003. [Google Scholar]
Oswalt 2013 {published data only}
- Oswalt KL, McClain DB, Melnyk B. Reducing anxiety among children born preterm and their young mothers. American Journal of Maternal Child Nursing 2013;38(3):144‐9. [PUBMED: 23625101] [DOI] [PMC free article] [PubMed] [Google Scholar]
Owen 2007 {published data only}
- Owen PL. Fostering Preschooler Attachment and Development through a Relationship‐Based Group Parent‐Training Program [PhD thesis]. Fresno, California: Alliant International University, 2007. [Google Scholar]
Perez‐Nieves 2001 {published data only}
- Perez‐Nieves L. A Comparative Study of REBT/Parent Training Versus Parent Training with Hispanic Parents of Exceptional Preschoolers [PhD thesis]. New York: St. John's Univeristy, 2001. [Google Scholar]
Perou 2012 {published data only}
- Perou R, Elliott MN, Visser SN, Claussen AH, Scott KG, Beckwith LH, et al. Legacy for Children TM: a pair of randomized controlled trials of a public health model to improve developmental outcomes among children in poverty. BMC Public Health 2012;12:691. [DOI: 10.1186/1471-2458-12-691] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pisterman 1989 {published data only}
- Pisterman S, McGrath P, Firestone P, Goodman JT, Webster I, Mallory R. Outcome of parent‐mediated treatment of preschoolers with attention deficit disorder with hyperactivity. Journal of Consulting and Clinical Psychology 1989;57(5):628‐35. [PUBMED: 2794183] [DOI] [PubMed] [Google Scholar]
Pitts 2001 {published data only}
- Pitts RP. The effectiveness and acceptability of the modified effective Black parenting program with children exhibiting severe conduct problems. Dissertation Abstracts International: Section B: The Sciences and Engineering 2001;62:2115. [Google Scholar]
Plant 2007 {published data only}
Puckering 1994 {published data only}
- Puckering C, Rogers J, Mills M, Cox AD, Raff MM‐G. Process and evaluation of a group intervention for mothers with parenting difficulties. Child Abuse Review 1994;3(4):299‐310. [DOI: 10.1002/car.2380030409] [DOI] [Google Scholar]
Quinn 2007 {published data only}
- Quinn M, Carr A, Carroll L, O'Sullivan D. Parents Plus Programme 1: evaluation of its effectiveness for pre‐school children with developmental disabilities and behavioural problems. Journal of Applied Research in Intellectual Disabilities 2007; Vol. 20, issue 4:345‐59. [DOI: 10.1111/j.1468-3148.2006.00352.x] [DOI]
Rapee 2005 {published data only}
Reedtz 2011 {published data only}
- Reedtz C, Handegård BH, Mørch WT. Promoting positive parenting practices in primary pare: outcomes and mechanisms of change in a randomized controlled risk reduction trial. Scandinavian Journal of Psychology 2011;52(2):131‐7. [PUBMED: 21121925 ] [DOI] [PubMed] [Google Scholar]
Roosa 1983 {published data only}
- Roosa M, Vaughn L. Teen mothers enrolled in an alternative parenting program: a comparison with their peers. Urban Education 1983;18(3):348‐60. [DOI: 10.1177/004208598301800306] [DOI] [Google Scholar]
Routh 1995 {published data only}
- Routh CP, Hill JW, Steele H, Elliot CE, Dewey ME. Maternal attachment status, psychosocial stressors and problem behaviour: follow‐up after parent training courses for conduct disorder. Journal of Child Psychology and Psychiatry, and Allied Disciplines 1995;36(7):1179‐98. [PUBMED: 8847379 ] [DOI] [PubMed] [Google Scholar]
Sanders 2000 {published data only}
- Sanders MR, Markie‐Dadds C, Tully LA, Bor W. The Triple P‐positive parenting program: a comparison of enhanced, standard, and self‐directed behavioral family intervention for parents of children with early onset conduct problems. Journal of Consulting and Clinical Psychology 2000;68(4):624‐40. [PUBMED: 10965638] [PubMed] [Google Scholar]
Sanders 2004 {published data only}
- Sanders MR, Pidgeon A, Gravestock F, Connors M, Brown S, Young R. Does parental attributional retraining and anger management enhance the effects of the triple P‐positive parenting program with parents at risk of child maltreatment?. Behavior Therapy 2004; Vol. 35, issue 3:513‐35. [DOI: 10.1016/S0005-7894(04)80030-3] [DOI]
Sanders 2007 {published data only}
Schachman 2001 {published data only}
- Schachman KA. Baby Boot Camp: Facilitating Maternal Role Adaptation in Military Wives [PhD thesis]. St Louise, Missouri: University of Missouri, 2001. [Google Scholar]
- Schachman KA, Lee RK, Lederma RR. Baby Boot Camp: facilitating maternal role adaptation among military wives. Nursing Research 2004;53(2):107‐15. [PUBMED: 15084995] [DOI] [PubMed] [Google Scholar]
Schappin 2013 {published data only}
- Schappin R, Wijnroks L, Venema MU, Wijnberg‐Williams B, Veenstra R, Koopman‐Esseboom C, et al. Brief parenting intervention for parents of NICU graduates: a randomized, clinical trial of Primary Care Triple P. BMC Pediatrics 2013;13:69. [DOI: 10.1186/1471-2431-13-69] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shaw 2006 {published data only}
- Shaw D, Dishion T, Supplee L, Gardner F, Arnds K. Randomized trial of a family‐centered approach to the prevention of early conduct problems: 2‐year effects of the family check‐up in early childhood. Journal of Consulting and Clinical Psychology 2006; Vol. 74, issue 1:1‐9. [PUBMED: 16551138] [DOI] [PubMed]
Sheeber 1994 {published data only}
- Sheeber LB, Johnson JH. Evaluation of a temperament‐focused, parent‐training program. Journal of Clinical Child Psychology 1994;23(3):249‐59. [DOI: 10.1207/s15374424jccp2303_3] [DOI] [Google Scholar]
Shelton 2000 {published data only}
- Shelton TL, Barkley RA, Crosswait C, Moorehouse M, Fletcher K, Barrett S, et al. Multimethod psychoeducational intervention for preschool children with disruptive behavior: two‐year post‐treatment follow‐up. Journal of Abnormal Child Psychology 2000;28(3):253‐66. [PUBMED: 10885683] [DOI] [PubMed] [Google Scholar]
Shrewsberry 1978 {published data only}
- Shrewsberry RD. Assignment completion in group parent training. Dissertation Abstracts International 1978;38:4739. [Google Scholar]
Siegert 1980 {published data only}
- Siegert FE, Yates BT. Behavioral child‐management cost‐effectiveness: a comparison of individual in‐office, individual in‐home, and group delivery systems. Evaluation & the Health Professions 1980;3(2):123‐52. [DOI: 10.1177/016327878000300201] [DOI] [Google Scholar]
Sonuga‐Barke 2001 {published data only}
- Sonuga‐Barke E, Daley D, Thompson M, Laver‐Bradbury C, Weeks A. Parent‐based therapies for preschool attention‐deficit/hyperactivity disorder: a randomized, controlled trial with a community sample. Journal of the American Academy of Child and Adolescent Psychiatry 2001; Vol. 40, issue 4:402‐8. [PUBMED: 11314565] [DOI] [PubMed]
Sonuga‐Barke 2004 {published data only}
- Sonuga‐Barke E, Thompson M, Daley D, Laver‐Bradbury C. Parent training for Attention Deficit/Hyperactivity Disorder: is it as effective when delivered as routine rather than as specialist care?. British Journal of Clinical Psychology 2004; Vol. 43, issue Pt 4:449‐57. [PUBMED: 15530214] [DOI] [PubMed]
St James‐Roberts 2001 {published data only}
Strayhorn 1989 {published data only}
- Strayhorn JM, Weidman CS. Reduction of attention deficit and internalizing symptoms in preschoolers through parent‐child interaction training. Journal of the American Academy of Child and Adolescent Psychiatry 1989;28(6):888‐96. Erratum in: Journal of the American Academy of Child and Adolescent Psychiatry 1990 29(2):314. [PUBMED: 2808259] [DOI] [PubMed] [Google Scholar]
Taylor 1997 {published data only}
- Taylor JA, Davis RL, Kemper KJ. A randomized controlled trial of group versus individual well child care for high‐risk children: maternal‐child interaction and developmental outcomes. Pediatrics 1997;99(6):E9. [PUBMED: 9164805] [DOI] [PubMed] [Google Scholar]
Taylor 2011 {published data only}
- Taylor HL. A school‐based parent intervention program to improve student behavior problems and the school‐family relationship during the transition to kindergarten. Dissertation Abstracts International: Section B: The Sciences and Engineering 2011;72:3742. [Google Scholar]
Thomas 1977 {published data only}
- Thomas CA. The effectiveness of two child management training procedures for high and low educational level parents of emotionally disturbed children. Dissertation Abstracts International 1977;37:7652‐3. [Google Scholar]
Trillingsgaard 2015 {published data only}
- Trillingsgaard T, Maimburg RD, Simonsen M. The Family Startup Program: study protocol for a randomized controlled trial of a universal group‐based parenting support program. BMC Public Health 2015;15:409. [DOI: 10.1186/s12889-015-1732-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Truss 1977 {published data only}
- Truss C. Parent training in preprimary competence. Paper Presented at the 85th Annual Convention of the American Psychological Association; 1977 August 26‐30; San Francisco, CA. 1977.
Tuerk 2008 {published data only}
- Tuerk EH. Parenting from the inside: assessing a curriculum for incarcerated mothers. Dissertation Abstracts International: Section B: The Sciences and Engineering 2008;68:7680. [Google Scholar]
Turner 1994 {published data only}
- Turner KMT, Sanders MR, Wall CR. Behavioural parent training versus dietary education in the treatment of children with persistent feeding difficulties. Behaviour Change 1994;11(4):242‐58. [DOI: 10.1017/S0813483900004514] [DOI] [Google Scholar]
Turner 2006 {published data only}
US Health Department 2001 {published data only}
- US Department of Health & Human Services. Building their futures: how Early Head Start Programs are enhancing the lives of Infants and toddlers in low‐income families: summary report, January 2001. bit.ly/1Gyxibs (accessed 20 October 2014).
Vogel 2000 {published data only}
- Vogel CA. Improving the odds for children of teen mothers: what matters most? (parenting programs). Dissertation Abstracts International Section A: Humanities and Social Sciences 2000;60:2391. [Google Scholar]
Webster‐Stratton 2001 {published data only}
Wint 1987 {published data only}
- Wint EBJ. Promoting effective parenting: a study of two methods in Kingston, Jamaica. Child Welfare 1987;66(6):507‐16. [Google Scholar]
References to studies awaiting assessment
Farzadfard 2008 {published data only}
- Farzadfard SZ, Hooman HA. The role of child rearing training skills in reducing mothers' stress and children's behavioral problems. Journal of Iranian Psychologists 2008;4(15):1‐16. [Google Scholar]
Herbert 2007 {published data only}
- Herbert M, Wookey J. The Child Wise Programme: a course to enhance the self‐confidence and behaviour management skills of foster carers with challenging children. Adoption & Fostering 2007;31(4):27‐37. [DOI: 10.1177/030857590703100405] [DOI] [Google Scholar]
ISRCTN39288126 {published data only}
- McCann DC, Thompson M, Daley D, Barton J, Laver‐Bradbury C, Hutchings J, et al. Study protocol for a randomized controlled trial comparing the efficacy of a specialist and a generic parenting programme for the treatment of preschool ADHD. Trials 2014;15:142. [DOI: 10.1186/1745-6215-15-142] [DOI] [PMC free article] [PubMed] [Google Scholar]
ISRCTN88988596 {published data only}
- Ramsauer B, Lotzin A, Mühlhan C, Romer G, Nolte T, Fonagy P, et al. A randomized controlled trial comparing Circle of Security Intervention and treatment as usual as interventions to increase attachment security in infants of mentally ill mothers: study protocol. BMC Psychiatry 2014; Vol. 14:24. [DOI: 10.1186/1471-244X-14-24] [DOI] [PMC free article] [PubMed]
Sandy 1983 {published data only}
- Sandy LR. Parent intervention and the development of parental awareness. Proceedings of the Biennial Meeting of the Society for Research in Child Development; 1983 April 21‐24; Detroit (MI). Detroit, 1983:15.
Schlarb 2012 {published data only}
- Schlarb AA, Brandhorst I. Mini‐KiSS ‐ Effectiveness of a parent sleep training for toddlers and young children. Journal of Sleep Research. Proceedings of the 21st Congress of the European Sleep Research Society; 2012 September 4‐8; Paris, France 2012;21(Suppl s1):302. [Google Scholar]
Wang 2000 {published data only}
- Wang F, Ye G, Wang Y. Intervention study on the mental health of kindergarten children. Chinese Mental Health Journal 2000;14:45‐7. [Google Scholar]
Zhu 2014 {published data only}
- Zhu MZ, Zhu XJ, Du JE, Zhang XL. Efficacy of short‐term educational intervention for parents of preschool children with anxiety [父母短期教育干预对学龄前儿童焦虑的影响]. Chinese Journal of Contemporary Pediatrics 2014;16(9):901‐4. [PUBMED: 25229956] [PubMed] [Google Scholar]
References to ongoing studies
ISRCTN11079129 {published data only}
- ISRCTN11079129. Enhancing social and emotional health in the early years. http://www.isrctn.com/ISRCTN11079129 (accessed 14 March 2016).
ISRCTN16513449 {published data only}
- Salari R, Fabian H, Prinz R, Lucas S, Feldman I, Fairchild A, et al. The Children and Parents in Focus project: a population‐based cluster‐randomised controlled trial to prevent behavioural and emotional problems in children. BMC Public Health 2013; Vol. 13:961. [PUBMED: 24131587] [DOI] [PMC free article] [PubMed]
ISRCTN17488830 {published data only}
- McGilloway S. A controlled trial, cost‐effectiveness and process evaluation of a group‐based early parenting intervention to improve parental competence and infant wellbeing for parents and infants (aged 0‐2). ICTRP 2015.
Additional references
Achenbach 2000
- Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms & Profiles. Burlington, VT: University of Vermont Department of Psychiatry, 2000. [Google Scholar]
Barkley 1981
- Barkley RA. Hyperactive Children: A Handbook for Diagnosis and Treatment. New York: Guilford Press, 1981. [Google Scholar]
Barlow 2003a
- Barlow J, Stewart‐Brown S. Letter to the editor: why a universal population‐level approach to the prevention of child abuse is essential. Child Abuse Review 2003;12(5):279‐81. [DOI: 10.1002/car.819] [DOI] [Google Scholar]
Barlow 2014
- Barlow J, Smailagic N, Huband N, Roloff V, Bennett C. Group‐based parent training programmes for improving parental psychosocial health. Cochrane Database of Systematic Reviews 2014, Issue 5. [DOI: 10.1002/14651858.CD002020.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barton 1979
- Barton EJ, Ascione ER. Sharing in preschool children: facilitation, stimulus generalization, response generalization, and maintenance. Journal of Applied Behavior Analysis 1979;12(3):417‐30. [DOI: 10.1901/jaba.1979.12-417] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bayley 1993
- Bayley N. Bayley Scales of Infant Development. Antonio, TX: Psychological Corporation, 1993. [Google Scholar]
Beebe 2010
- Beebe B, Jaffe J, Markese S, Buck K, Chen H, Cohen P, et al. The origins of 12‐month attachment: a microanalysis of 4‐month mother‐infant interaction. Attachment & Human Development 2010;12(1‐2):3‐141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Behar 1974
- Behar L, Stringfield S. A behavior rating scale for the preschool child. Developmental Psychology 1974;10(5):601‐10. [Google Scholar]
Bishop 2003
- Bishop G, Spence SH, McDonald C. Can parents and teachers provide a reliable and valid report of behavioral inhibition?. Child Development 2003;74(6):1899‐917. [PUBMED: 14669903] [DOI] [PubMed] [Google Scholar]
Briggs‐Gowan 2006
- Briggs‐Gowan MJ, Carter AS, Bosson‐Heenan J, Guyer AE, Horwitz SM. Are infant‐toddler social‐emotional and behavioral problems transient?. Journal of the American Academy of Child and Adolescent Psychiatry 2006;45(7):849‐58. [PUBMED: 16832322] [DOI] [PubMed] [Google Scholar]
Bryant 1984
- Bryant LE, Budd KS. Teaching behaviorally‐handicapped preschool children to share. Journal of Applied Behavior Analysis 1984;17(1):45‐56. [DOI: 10.1901/jaba.1984.17‐45.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carter 2003
- Carter AS, Briggs‐Gowan MJ, Jones SM, Little TD. The Infant‐Toddler Social and Emotional Assessment (ITSEA): factor structure, reliability, and validity. Journal of Abnormal Child Psychology 2003;31(5):495‐514. [DOI] [PubMed] [Google Scholar]
Champion 1995
- Champion LA, Goodall G, Rutter M. Behaviour problems in childhood and stressors in early adult life: 1. A 20 year follow‐up of London school children. Psychiatric Medicine 1995;25(2):231‐46. [PUBMED: 7675912] [DOI] [PubMed] [Google Scholar]
Conners 1994
- Conners CK. The Conners rating scales: use in clinical assessment, treatment planning and research. In: Maruish M editor(s). Use of Psychological Testing for Treatment Planning and Outcome Assessment. Hillsdale, New Jersey: Erlbaum Associates, 1994. [Google Scholar]
De Wolff 1997
- Wolff MS, Ijzendoorn MH. Sensitivity and attachment: a meta‐analysis on parental antecedents of infant attachment. Child Development 1997;68(4):571‐91. [PUBMED: 9306636] [PubMed] [Google Scholar]
DeGangi 2000a
- DeGangi GA. Pediatric Disorders of Regulation in Affect and Behavior: A Therapist’s Guide to Assessment and Treatment. New York: Academic Press, 2000. [Google Scholar]
DeGangi 2000b
- DeGangi GA, Breinbauer C, Roosevelt JD, Porges S, Greenspan S. Prediction of childhood problems at three years in children experiencing disorders of regulation during infancy. Infant Mental Health Journal 2000;21(3):156‐75. [Google Scholar]
Dretzke 2009
- Dretzke J, Davenport C, Frew E, Barlow J, Stewart‐Brown S, Bayliss S, et al. The clinical effectiveness of different parenting programmes for children with conduct problems: a systematic review of randomised controlled trials. Child and Adolescent Psychiatry and Mental Health 2009;3:7. [DOI: 10.1186/1753-2000-3-7] [DOI] [PMC free article] [PubMed] [Google Scholar]
Egeland 1979
- Egeland B, Deinard A, Brunnquell D, Phipps‐Yonas S, Crichton L. Final report: a prospective study of the antecedents of child abuse. National Center on Child Abuse and Neglect, Administration for Children, Youth and Families. Washington, DC: Office of Child Development, HEW, 1979. [Google Scholar]
Egeland 1993b
- Egeland B, Pianta R, O’Brien MA. Maternal intrusiveness in infancy and child maladaptation in early school years. Development and Psychopathology 1993;5(3):359‐370. [DOI: 10.1017/S0954579400004466] [DOI] [Google Scholar]
Elbourne 2002
- Elbourne D, Altman DG, Higgins JPT, Curtina F, Worthington HV, Vaile A. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140‐9. [DOI: 10.1093/ije/31.1.140] [DOI] [PubMed] [Google Scholar]
Erol 2005
- Erol N, Simsek Z, Oner O, Munir K. Behavioral and emotional problems among Turkish children at ages 2 to 3 years. Journal of the American Academy of Child and Adolescent Psychiatry 2005;44(1):80‐7. [PUBMED: 15608547] [DOI] [PMC free article] [PubMed] [Google Scholar]
Eron 1990
- Eron LD, Huesmann LR. The stability of aggressive behavior ‐ even into the third generation. In: Lewis M, Miller SM editor(s). Handbook of Developmental Psychopathology. New York: Plenum Press, 1990:147‐56. [Google Scholar]
Eyberg 1978
- Eyberg SM, Ross AW. Assessment of child behavior problems: the validation of a new inventory. Journal of Clinical Child Psychology 1978;7(2):113‐6. [DOI: 10.1080/15374417809532835] [DOI] [Google Scholar]
Farrington 1991
- Farrington DP. Childhood aggression and adult violence: early precursors and later life outcomes. The Development and Treatment of Adult Aggression. Hillsdale, NJ: Lawrence Erlbaum, 1991:5‐29. [Google Scholar]
Farrington 1994
- Farrington DP. Early developmental prevention of juvenile delinquency. Criminal Behaviour and Mental Health 1994;4:209‐27. [Google Scholar]
Fearon 2010
- Fearon RP, Bakermans‐Kranenburg MJ, Ijzendoorn MH, Lapsley AM, Roisman GI. The significance of insecure attachment and disorganization in the development of children's externalizing behavior: a meta‐analytic study. Child Development 2010;81(2):435‐56. [PUBMED: 20438450] [DOI] [PubMed] [Google Scholar]
Finegan 1989
- Finegan J‐A, Niccols A, Zacher J, Hood J. Factor structure of the preschool characteristics questionnaire. Infant Behavior and Development 1989;12(2):221‐7. [DOI: 10.1016/0163-6383(89)90008-8] [DOI] [Google Scholar]
Fonagy 1998
- Fonagy P. Prevention, the appropriate target of infant psychotherapy. Infant Mental Health Journal 1998;19(2):124‐50. [Google Scholar]
Fox 1991
- Fox RA, Fox TA, Anderson RC. Measuring the effectiveness of the Star Parenting Program with parents of young children. Psychological Reports 1991;68(1):35‐40. [PUBMED: 2034775] [DOI] [PubMed] [Google Scholar]
Frankel 1992
- Frankel, Simmons JQ. Parent behavioral training: why and when some parents drop out. Journal of Clinical Psychology 1992;21(4):322‐30. [DOI: 10.1207/s15374424jccp2104_1] [DOI] [Google Scholar]
Furlong 2012
- Furlong M, McGilloway S, Bywater T, Hutchings J, Smith SM, Donnelly M. Behavioural and cognitive‐behavioural group‐based parenting programmes for early‐onset conduct problems in children aged 3 to 12 years. Cochrane Database of Systematic Reviews 2012, Issue 2. [DOI: 10.1002/14651858.CD008225.pub2] [DOI] [PubMed] [Google Scholar]
Furniss 2006
- Furniss T, Beyer T, Guggenmos J. Prevalence of behavioural and emotional problems among six year old preschool children: baseline results of a prospective longitudinal study. Social Psychiatry and Psychiatric Epidemiology 2006;41(5):394‐9. [PUBMED: 16565920 ] [DOI] [PubMed] [Google Scholar]
Goodman 1997
- Goodman R. The Strengths and Difficulties Questionnaire: a research note. Journal of Child Psychology and Psychiatry 1997;38(5):581‐6. [PUBMED: 9255702] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- McMaster University. GRADEpro GDT: GRADEpro Guideline Development Tool. McMaster University, 2015 (developed by Evidence Prime, Inc.) Available from www.gradepro.org.
Higgins 2002
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21(11):1539‐58. [PUBMED: 12111919] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of InterventionsVersion 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Holden 1990
- Holden GW, Lavigne VV, Cameron AM. Probing the continuum of effectiveness in parent training: characteristics of parents and preschoolers. Journal of Clinical Child Psychology 1990;19(1):2‐8. [DOI: 10.1207/s15374424jccp1901_1] [DOI] [Google Scholar]
Incredible Years 2009
- Webster‐Stratton C. Incredible Years Program. bit.ly/1NaI5NM (accessed 30 September 2009).
Johnson 1973
- Johnson CA, Katz RC. Using parents as change agents for their children: a review. Journal of Child Psychology and Psychiatry, and Allied Disciplines 1973;14(3):181‐200. [PUBMED: 4584401] [DOI] [PubMed] [Google Scholar]
Kamphaus 2006
- Kamphaus RW, Reynolds CR. Parenting Relationship Questionnaire Manual. Minneapolis: Pearson, 2006. [Google Scholar]
Kane 2007
- Kane GA, Wood VA, Barlow J. Parenting programmes: a systematic review and synthesis of qualitative research. Child: Care, Health and Development 2007;33(6):784‐93. [PUBMED: 17944788] [DOI] [PubMed] [Google Scholar]
Kazdin 1990
- Kazdin AE. Premature termination from treatment among children referred for antisocial behavior. Journal of Child Psychology and Psychiatry, and Allied Disciplines 1990;31(3):415‐25. [PUBMED: 2318922] [DOI] [PubMed] [Google Scholar]
Keenan 1998
- Keenan K, Shaw D, Delliquadri E, Giovannelli J, Walsh B. Evidence for the continuity of early problem behaviors: application of a developmental model. Journal of Abnormal Child Psychology 1998;26(6):441‐54. [DOI] [PubMed] [Google Scholar]
Kogan 1975
- Kogan KL, Gordon BN. A mother‐instruction program: documenting change in mother‐child interactions. Child Psychiatry and Human Development 1975;5(3):189‐200. [PUBMED: 1139977] [DOI] [PubMed] [Google Scholar]
Kohn 1977
- Kohn M. The Kohn Social Competence Scale and Kohn Symptom Checklist for the preschool child: a follow‐up report. Journal of Abnormal Child Psychology 1977;5(3):249‐63. [DOI] [PubMed] [Google Scholar]
Kumpfer 2004
- Kumpfer KL, Bluth B. Parent/child transactional processes predictive of resilience or vulnerability to "substance abuse disorders". Substance Use & Misue 2004;39(5):671‐98. [PUBMED: 15202804] [DOI] [PubMed] [Google Scholar]
Loeber 1997
- Loeber R, Hay D. Key issues in the development of aggression and violence from childhood to early adulthood. Annual Review of Psychology 1997;48:371‐410. [DOI: 10.1146/annurev.psych.48.1.371] [DOI] [PubMed] [Google Scholar]
Love 2005
- Love J, Kisker E, Ross C, Raikes H, Constantine J, Boller K, et al. The effectiveness of Early Head Start for 3‐year‐old children and their parents: lessons for policy and programs. Developmental Psychology 2005;41(6):885‐901. [PUBMED: 16351335] [DOI] [PubMed] [Google Scholar]
Lyneham 2013
- Lyneham HJ, Sburlati ES, Abbott MJ, Rapee RM, Hudson JL, Tolin DF, et al. Psychometric properties of the Child Anxiety Life Interference Scale (CALIS). Journal of Anxiety Disorders 2013;27(7):711‐9. [DOI: 10.1016/j.janxdis.2013.09.008] [DOI] [PubMed] [Google Scholar]
Lyons‐Ruth 1996
- Lyons‐Ruth K. Attachment relationships among children with aggressive behavior problems: the role of disorganized early attachment patterns. Journal of Consulting and Clinical Psychology 1996;64(1):64‐73. [DOI: 10.1037/0022-006X.64.1.64] [DOI] [PubMed] [Google Scholar]
Madigan 2006
- Madigan M, Bakermans‐Kranenburg MJ, Ijzendoorn G, Moran DR, Pederson DR, Benoit D. Unresolved states of mind, anomalous parental behaviour and disorganized attachment: a review and meta‐analysis of a transmission gap. Attachment & Human Behavior 2006;8(2):89‐111. [PUBMED: 16818417] [DOI] [PubMed] [Google Scholar]
Marmot 2010
- Marmot M. The Marmot Review. Fair society, healthy lives: strategic review of health inequalities in England post‐2010. bit.ly/1hs5CeE (accessed 11 March 2015).
Meins 2001
- Meins E, Fernyhough C, Fradley E, Tuckey M. Rethinking maternal sensitivity: mothers’ comments on infants’ mental processes predict security of attachment at 12 months. Journal of Child Psychology and Psychiatry 2001;42(5):637‐48. [PubMed] [Google Scholar]
Mockford 2004
- Mockford C, Barlow J. Parenting programmes: some unintended consequences. Primary Health Care Research and Development 2004;5(3):219‐27. [Google Scholar]
Moffit 1996
- Moffit TE, Caspi A, Dickson N, Silva P, Stanton W. Childhood‐onset versus adolescent‐onset antisocial conduct problems in males: natural history from ages 3 to 18 years. Development and Psychopathology 1996;8(2):399‐424. [DOI: 10.1017/S0954579400007161] [DOI] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG for the PRISMA Group. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morawska 2010
- Morawska A, Sanders MR. The Child Adjustment and Parent Efficacy Scale. Brisbane: Parenting and Family Support Centre, 2010. [Google Scholar]
Murphy 1988
- Murphy JM, Jellinek M. Screening for psychosocial dysfunction in economically disadvantaged and minority group children: further validation of the Pediatric Symptom Checklist. American Journal of Orthopsychiatry 1988;58(3):450‐6. [PUBMED: 3407735] [DOI] [PubMed] [Google Scholar]
NICE 2006
- National Institute for Health and Clinical Excellence. Parent Training/Education Programmes in the Management of Children with Conduct Disorders. London: NICE, 2006. [Google Scholar]
Offord 1994
- Offord MD, Bennett KJ. Conduct disorder: long‐term outcomes and intervention effectiveness. Journal of the American Academy of Child and Adolescent Psychiatry 1994;33(8):1069‐78. [DOI: 10.1097/00004583-199410000-00001] [DOI] [PubMed] [Google Scholar]
Patterson 1989
- Patterson GR, DeBaryshe D, Ramsey E. A developmental perspective on antisocial behavior. American Psychiatry 1989;44(2):329‐35. [PUBMED: 2653143] [DOI] [PubMed] [Google Scholar]
Patterson 1993
- Patterson GR, Dishion TJ, Chamberlain P. Outcomes and methodological issues relating to treatment of antisocial children. In: Giles TR editor(s). Handbook of Effective Psychotherapy. New York: Plenum Press, 1993. [Google Scholar]
Prinz 2009
- Prinz RJ, Sanders MR, Shapiro CJ, Whitaker DJ, Lutzker JR. Population‐based prevention of child maltreatment: the U.S. Triple P system population trial. Prevention Science 2009;10(1):1‐12. [DOI: 10.1007/s11121-009-0123-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pugh 1994
- Pugh G, De'Ath E, Smith C. Confident Parents, Confident Children: Policy and Practice in Parent Education and Support. London: National Children's Bureau, 1994. [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Richman 1971
- Richman N, Graham PJ. A behavioural screening questionnaire for use with three‐year‐old children. Preliminary findings. Journal of Child Psychology and Psychiatry, and Allied Disciplines 1971;12(1):5‐33. [DOI: 10.1111/j.1469-7610.1971.tb01047.x] [DOI] [PubMed] [Google Scholar]
Robins 1990
- Robins LN, Rutter M, (editors). Straight and Devious Pathways from Childhood to Adulthood. Cambridge: Cambridge University Press, 1990. [Google Scholar]
Robins 1991
- Robins LN. Conduct disorder. Journal of Child Psychology and Psychiatry 1991;32(1):193‐212. [DOI: 10.1111/j.1469-7610.1991.tb00008.x] [DOI] [PubMed] [Google Scholar]
Robinson 1981
- Robinson EA, Eyberg SM. The dyadic parent–child interaction coding system: standardization and validation. Journal of Consulting and Clinical Psychology 1981;49(2):245‐50. [PUBMED: 7217491] [DOI] [PubMed] [Google Scholar]
Rose 1974
- Rose SD. Group training of parents as behaviour modifiers. Social Work 1974;19(2):156‐62. [Google Scholar]
Rutter 1970
- Rutter M, Tizard J, Whitmore K. Education, Health and Behaviour. London: Longman, 1970. [Google Scholar]
Rutter 1996
- Rutter M. Connections between child and adult psychopathology. European Child & Adolescent Psychiatry 1996;5(1 Suppl):4‐7. [DOI] [PubMed] [Google Scholar]
Sanders 2002
- Sanders MR, Turner KM, Markie‐Dadds C. The development and dissemination of theTriple P—Positive Parenting Program: a multilevel, evidence‐based system of parenting and family support. Prevention Science 2002;3(3):173‐89. [DOI: 10.1023/A:1019942516231] [DOI] [PubMed] [Google Scholar]
Sanders 2008
- Sanders MR. Triple P‐Positive Parenting Program as a public health approach to strengthening parenting. Journal of Family Psychology 2008;22(4):505‐17. [PUBMED: 18729665] [DOI] [PubMed] [Google Scholar]
Schünemann 2008
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons, 2008:359‐83. [Google Scholar]
Shadish 1992
- Shadish WR. Do family and marital psychotherapies change what people do? A meta‐analysis of behavioral outcomes. In: Cook TD, Cooper H, Corday DS editor(s). Meta‐Analysis for Explanation. A Casebook. New York: Russell Sage Foundation, 1992. [Google Scholar]
Shonkoff 2009
- Shonkoff JP, Boyce T, McEwen BS. Neruoscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA 2009;301(21):2252‐9. [PUBMED: 19491187] [DOI] [PubMed] [Google Scholar]
Skovgaard 2008
- Skovgaard AM, Olsen EM, Christiansen E, Houmann T, Landorph S, Jørgensen T. Predictors (0‐10 months) of psychopathology at age 1½ years ‐ a general population study in The Copenhagen Child Cohort CCC 2000. Journal of Child Psychology and Psychiatry, and Allied Disciplines 2008;49(5):553‐62. [PUBMED: 18341552] [DOI] [PubMed] [Google Scholar]
Skovgaard 2010
- Skovgaard AM. Mental health problems and psychopathology in infancy and early childhood. An epidemiological study. Danish Medical Bulletin 2010;57(10):B4193. [PUBMED: 21040689] [PubMed] [Google Scholar]
Slade 2001
- Slade A, Grienenberger J, Bernbach E, Levy D, Locker A. Maternal reflective functioning and attachment: considering the transmission gap. Proceedings of the Biennial Meeting of the Society for Research in Child Development; 2001 April 19‐22; Minneapolis (MN). Minneapolis: Society for Research on Child Development, 2001.
Sparrow 1984
- Sparrow SS, Balla DA, Ciccettti DV. Vineland Adaptive Behavior Scales. Circle Pines, MN: American Guidance Service, 1984. [Google Scholar]
Spence 2001
- Spence SH, Rapee R, McDonald C, Ingram M. The structure of anxiety symptoms among preschoolers. Behaviour Research and Therapy 2001;39(11):1293‐316. [PUBMED: 11686265] [DOI] [PubMed] [Google Scholar]
Strain 1981
- Strain PS, Young CC, Horowitz J. Generalised behavior change during oppositional child training: an examination of child and family demographic variables. Behavior Modification 1981;5(1):15‐26. [DOI: 10.1177/014544558151002] [DOI] [Google Scholar]
Sutter 1984
Szyndler 1992
- Szyndler J, Bell G. Are groups for parents of children with sleep problems effective?. Health Visitor 1992;65(8):277‐9. [PUBMED: 1468951] [PubMed] [Google Scholar]
Taylor 1986
- Taylor E, Schachar R, Thorley G, Wieselberg M. Conduct disorder and hyperactivity: I. Separation of hyperactivity and antisocial conduct in British child psychiatric patients. British Journal of Psychiatry 1986;149:760‐7. [PUBMED: 3790875] [DOI] [PubMed] [Google Scholar]
Waters 1995
- Waters E. Appendix A: the Attachment Q‐Set (version 3.0). Monographs of the Society for Research in Child Development 1995;60(2‐3):234‐46. [DOI: 10.1111/j.1540-5834.1995.tb00214.x] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Barlow 2002a
- Barlow J, Parson, J. Group‐based parent‐training programmes for improving emotional and behavioural adjustment in 0‐3 year old children (Cochrane Review). The Cochrane Library, Issue 2. Oxford: Update Software, 2002. [DOI] [PubMed] [Google Scholar]
Barlow 2002b
- Barlow J, Parsons J. Group‐based parent‐training programmes for improving emotional and behavioural adjustment in 0‐3 year old children (Cochrane Review). The Cochrane Library, Issue 4. Oxford: Update Software, 2002. [Google Scholar]
Barlow 2003b
- Barlow J, Parsons J. Group‐based parent‐training programmes for improving emotional and behavioural adjustment in 0‐3 year old children. Cochrane Database of Systematic Reviews 2003, Issue 2. [DOI: 10.1002/14651858.CD003680; Art. No.: CD003680] [DOI] [PubMed] [Google Scholar]
Barlow 2010
- Barlow J, Smailagic N, Ferriter M, Bennett C, Jones H. Group‐based parent‐training programmes for improving emotional and behavioural adjustment in children from birth to three years old. Cochrane Database of Systematic Reviews 2010, Issue 3. [DOI: 10.1002/14651858.CD003680.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parsons 2001
- Parsons J, Barlow J. Group‐based parenting programmes for improving the mental health of 0‐3 year old children (Cochrane Protocol). The Cochrane Library, Issue 4. Oxford: Update Software, 2001. [Google Scholar]


