Abstract
Background: Interpersonal violence continues to affect health long after violence has ended. This analysis investigated stress, support, and health behaviors as mediators potentially explaining persistent health impacts of violence.
Methods: Using a cross-sectional analysis of 12,594 women “Wellness, Health & You” (WHY) participants, authors measured violence as intimate partner violence (IPV), sexual assaults (SA), and childhood abuse (CA) by recency (current, past as an adult, or child) and number of violence forms. Current health-related quality of life (HR-QOL) was defined using the most recent survey as physical and mental health limiting usual activities for at least 4 days in the past 30 days. Adjusted prevalence rate ratios (aPRRs) for violence and HR-QOL were obtained using multiple variable log binomial regression where each mediator was included in separate models with demographic attributes.
Results: In this sample of middle-aged women, half (n = 6307) had ever experienced violence (38.3% IPV, 12.9% SA, and 24.6% CA) and 19.9% reported multiple forms. IPV, SA, and CA were each associated with poorer current HR-QOL, yet, WHY participants experiencing all three forms had a sixfold increased rate of poor mental HR-QOL (Model 1: aPRRs = 6.23 [95% confidence interval, 95% CI: 4.87–7.97]) versus no violence. Stress was the mediator associated with the greatest change in aPRRs (−34.7%; Model 2: aPRR = 4.07 [95% CI: 3.13–5.30]). When all mediators were included (Model 5: aPRR = 3.01 [95% CI: 2.29–3.96]), partial mediation was observed, evidenced by nonoverlapping CIs between Models 1 and 5.
Conclusions: Of relevance for interventions are findings that current health impacts of past violence may be mitigated through reducing current stress.
Keywords: intimate partner violence, childhood abuse, sexual assaults, mental health, physical health, intervention, health care, health-related quality of life
Introduction
Rates of intimate partner violence (IPV) remain high globally. More than a third of women (35.6%) in the United States have experienced rape, physical violence, and/or stalking by an intimate partner in their lifetime.1 Internationally IPV rates are equally high.2 The lifetime cost of IPV has been estimated at $3.6 trillion based on 43 million US adults with a history of IPV (2018 $US).3 Beyond the direct cost of treating IPV, this violence has long-term physical and mental health effects, including poorer current health.1,4
While IPV is the most common form of violence women experience, IPV frequently co-occurs with childhood abuse (CA) and sexual assaults (SA) by nonpartners.1 One in four adults has experienced sexual or physical abuse as a child.5,6 The total annual lifetime cost of CA was estimated at $124 billion (2008 $US).7 Recently, the cost of child sexual abuse (CSA) was estimated at $9.3 billion.8
SA also has significant negative impact on mental and physical health.9–11 The lifetime medical cost of rape was estimated at $1.2 trillion (US$ 2014)12 for >25 million adult men and women who have been raped (18.3% of US adult population).1
Despite the rates, health impacts, costs, and frequent co-occurrence of IPV, SA, and CA, little research has explored potentially mediating factors that may mitigate the cumulative health effects of polyvictimization of IPV, SA, and CA. This is a missed opportunity for intervention development directed at reducing the health impact of violence because health care systems can play a key role in needed multisectoral responses to these forms of violence disproportionally directed toward women.13 The current analysis seeks to fill this gap by exploring the extent to which hypothesized mediators (Fig. 1) reduce the effects of frequently co-occurring IPV, SA, and CA on current health-related mental and physical quality of life. If evidence of full or partial mediation is observed, these findings can inform the development or adaptation of existing or recommended interventions to reduce the continuing effect of violence on women's current health-related quality of life (HR-QOL).14–17
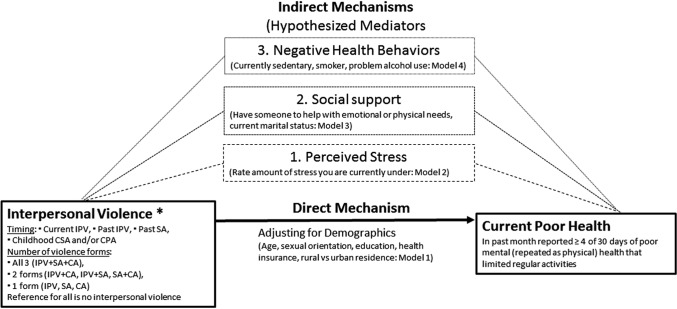
FIG. 1.
Hypothesized direct and indirect effects of current and past interpersonal violence* and measure of current poor mental and physical health among women. *Includes IPV (physical, sexual, and stalking), SA as an adult by someone other than a partner, and/or CSA or CPA. CPA, child physical abuse; CSA, child sexual abuse; IPV, intimate partner violence; SA, sexual assault.
In contrast to a growing literature, which has evaluated the potential utility of health care-based interventions,13–15,18 including advocacy19 and cognitive behavioral therapy (CBT),16 this current analysis focused on finding opportunities to reduce the impact of past violence on current HR-QOL. Interventions for past violence are different from those addressing current violence because the immediate threat of harm is not salient.
This current analysis adds to the literature with the use of a large nonclinical sample of Kentucky women volunteering to complete health surveys asking about experiences with IPV, SA, and CA. These comprehensive data on multiple violence forms provide the unique opportunity to investigate the HR-QOL impact of multiple forms of violence (polyvictimization) and violence recency from current and past adulthood to CA alone. This approach was encouraged by the recent federal report which urges researchers and other health professionals to “connect the dots” between multiple forms of violence, which frequently co-occur and have similar causes and consequences.20 “Connecting the dots” could lead to the identification of more efficient and effective intervention strategies across the lifespan.
Figure 1 provides a depiction of the direct and indirect pathways, by which hypothesized mediators may affect the associations between violence recency and number of forms and current mental and physical HR-QOL. Identifying mutable factors that may mediate the effect of violence on current HR-QOL can highlight avenues for interventions to reduce the impact of violence on women's health in both clinical and community settings.
The following provides a justification for the theoretical model of mediation to be tested. Violence is characterized by the number of forms experienced and its recency. HR-QOL was selected as a more comprehensive primary outcome measure because violence has been linked to a wide range of chronic conditions. Measuring HR-QOL has the unique advantage of rapidly measuring the self-perceived impact of chronic conditions on current daily functioning and activity limitations.21 The following three sets of mediators were examined: (1) self-perceived stress, (2) social support, and (3) health behaviors, including current smoking, problem alcohol use, and a sedentary life style.
Stress was selected as the first hypothesized mediator because IPV, SA, and CA increase symptoms of stress, including posttraumatic stress disorder.22–24 Campbell et al.25 reported that physical health symptomatology associated with concurrent SA, CSA, and IPV was fully mediated by post-traumatic stress disorder (PTSD). These findings indicate that the number of violence forms may increase symptoms of stress; PTSD explained the noted physical health consequences associated with violence.25
Social support positively influences HR-QOL.26,27 Greater social support is buffer or moderator for the negative impact of violence.28 A recent literature review noted that positive reactions to IPV disclosure among one's support network were linked to psychological health benefits.29 A health care intervention targeting social support among pregnant women experiencing violence appeared to improve health outcomes.30
Health behaviors were selected as the third mediator because negative health behaviors such as alcohol abuse,31 cigarette smoking,32 and limited physical activity33,34 are correlates of common chronic conditions associated with poorer HR-QOL. Forms of violence have been associated with an increased risk of substance abuse,35 including alcohol and/or tobacco use.36 Childhood sexual abuse has been associated with adult obesity,37,38 which may result in or cause a sedentary lifestyle. Thus, violence may increase use of negative health behaviors potentially resulting in poorer current HR-QOL.
Two primary research questions were addressed: (1) Does violence (either recent or increasing number of violence forms) increase the rate of poorer current HR-QOL perceptions (direct mechanism in Fig. 1)? (2) Which potential mediators explain associations between violence and current HR-QOL (three indirect mechanisms in Fig. 1)?
Methods
The Kentucky Women's Health Registry was a longitudinal database that included health surveys from 16,645 women, participating from 2006 to 2014. No compensation was provided to respondents for their participation. This resource was recently renamed and relaunched as “Wellness, Health & You” (WHY). WHY is an all-comer, convenience sample database, where participants may self-select or be invited to WHY by health care providers, colleagues, friends, and/or family; current eligibility criterion requires that participants must be at least 18 years of age. WHY participation entails completing an annual survey (electronic and articles from 2006 to 2012; electronic only from 2013 to present). For the purposes of this article, longitudinal data are aggregated across survey years to identify any potential exposure to violence such that only one record per participant is used. This design is a secondary analysis using a cross section of the longitudinal registry data.
Measurement
Interpersonal violence: IPV, SA, and CA
Adult interpersonal violence exposure was measured using four items that solicited a yes or no response: physical IPV (has an intimate partner, hit, kicked, punched, or otherwise hurt you?), sexual IPV (has an intimate partner who used force [like hitting, holding down, or using a weapon] to make you have sex [any sex act, not just intercourse]?), adult stalking by an intimate partner (has an intimate partner, ever repeatedly followed you, spied on you, made unsolicited phone calls to your place of work or at home, damaged your property, or stalked you in any way?), and adult SA (has anyone other than an intimate partner or anyone else used force—such as hitting, holding down, or using a weapon to make you have sex, any sex act, not just intercourse?) These questions were based on items included in the Behavioral Risk Factor Surveillance System (BRFSS).39 A dichotomized variable was created to characterize any IPV, then IPV by form (physical, sexual, or stalking by an intimate partner) and by recency (current or past).
Childhood physical and sexual abuses were also measured, using the following BRFSS39 items: “Did a parent, stepparent, or guardian ever hit, kick, punch, or otherwise hurt you?” “Did any parent, stepparent, guardian, or any other person make you have sex [any sex act, not just intercourse] by using force or by threatening to harm you or someone close to you?).”
Six dichotomous variables were created for each specific violence form. We examined lifetime history of violence because the questionnaire did not contain information needed to construct a timeline of events. Women who gave a negative response to all six items were the “no violence” or unexposed group for all violence measures.
Two measures of violence recency were created. The first defined recency using a hierarchical strategy prioritizing current over past violence as follows: current IPV, past IPV (regardless of other violence forms and excluding current IPV), past SA (excluding IPV and regardless of CA), CA (excluding IPV/SV). This categorization was used because intervention options differ by violence recency (current vs. past as an adult or child). The second recency measure simplified the above such that either adult IPV or SA regardless of previous CA was grouped separately from those experiencing CA “alone” where the “no violence” group remained the referent exposure. This simplified recency measure was used to identify confounders for multivariable analyses. One measure counting the number of violence forms was created as follows: all three forms experienced by the same participant (IPV, SA, and CA) to two forms (IPV and SA, IPV and CA, or SA and CA), to one form (IPV alone, SA, alone or CA alone). Rates of poorer current HR-QOL were hypothesized to be greatest for those experiencing more recent violence and more violence (direct mechanism; Fig. 1).
Current HR-QOL
Two related measures of current HR-QOL were included in WHY and are based on the “Healthy Days” Core Module of the CDC's Health Related Quality of Life—4 Module40 which has been validated41 and used since 1993 in the state-based BRFSS telephone surveys. Items were “During the past 30 days, for about how many days did POOR MENTAL health prevent you from doing your usual daily activities, such as self-care, work, or recreation?” This same question was repeated where PHYSICAL replaced MENTAL health. Response options ranged from 0 to 30. To create a meaningful dichotomization, a response of >4 of the past 30 days was used as an indicator of poor current health; the comparison group was those reporting 0–3 days in the past month as poor health.
Demographic attributes
Demographic attributes included current age (based on the participant's most recently completed survey), race (self-reported and grouped as white and nonwhite), sexual orientation (responses were heterosexual, bisexual, lesbian, and transgender, yet were simplified as exclusively heterosexual and not), and current employment status, Kentucky region (grouped as rural or urban), highest education, and current health insurance coverage (based on the participant's most recently completed survey). See Table 2 for the demographic attribute categorizations, three hypothesized mediators, and two HR-QOL outcomes. (To request the survey questions e-mail WHY@uky.edu).
Table 2.
Distribution of Demographic and Mediational Factors Hypothesized to Correlate with Interpersonal Violence and Provide a Mechanism by Which the Effect of Violence on Current Mental May Be Mitigated
| Hierarchical combinations of violence (n, column %) | |||||||
|---|---|---|---|---|---|---|---|
| Attribute and measure inclusion in conceptual model | n in strata | IPV/SA as an adult | Chi square df p-value | Childhood abuse (no IPV/SA) | Chi square df p-value | No violence | |
| Direct mechanism (MODEL 1) | N = 5223 | N = 1084 | N = 6287 | ||||
| Potential demographic confounders | |||||||
| Age group | 76.62 2p < 0.0001 | 7.85 2p = 0.005 | |||||
| Age 18–39 | 3815 | 1670 (32.0) | 253 (23.4) | 1892 (30.1) | Ref. | ||
| Age 40–54 | 4309 | 2053 (39.3) | 384 (35.4) | 1872 (29.8) | |||
| Age 55+ | 4470 | 1500 (28.7) | 447 (41.2) | 2523 (40.1) | |||
| Race | 36.8 1p < 0.0001 | 12.41 1p = 0.0002 | Ref. | ||||
| White | 11,939 | 4886 (93.5) | 1015 (93.6) | 6039 (93.1) | |||
| Nonwhite | 655 | 337 (6.5) | 69 (6.4) | 248 (3.9) | |||
| Sexual orientation | 83.18 1p < 0.0001 | 13.64 1p = 0.0001 | Ref. | ||||
| Exclusively heterosexual | 12,141 | 4946 (94.7) | 1041 (96.0) | 6154 (97.9) | |||
| Not exclusively heterosexual | 453 | 277 (5.3) | 43 (4.0) | 133 (2.1) | |||
| Employment status | 45.79 3p < 0.0001 | 0.65 3p = NS | Ref. | ||||
| Employed | 8514 | 3697 (70.8) | 704 (65.0) | 4112 (65.4) | |||
| Unemployed | 232 | 140 (2.7) | 23 (2.1) | 69 (1.1) | |||
| Retired or disabled | 3683 | 1307 (25.0) | 342 (31.5) | 2034 (32.4) | |||
| Other | 165 | 78 (1.5) | 15 (1.4) | 72 (1.1) | |||
| Kentucky region | 3.69 1p = 0.02 | 5.21 1p = 0.01 | Ref. | ||||
| Rural | 4443 | 1909 (36.5) | 345 (31.8) | 2189 (34.8) | |||
| Urban | 8151 | 3314 (63.5) | 739 (68.2) | 4098 (65.2) | |||
| Education | 45.34 3p < 0.0001 | 46.96 3p < 0.0001 | |||||
| ≤High school graduate/GED) | 1042 | 445 (8.5) | 84 (7.7) | 513 (8.2) | |||
| Some college or Associates | 3761 | 1808 (34.6) | 309 (28.5) | 1644 (26.1) | |||
| College graduate or beyond | 7553 | 2851 (54.6) | 680 (62.8) | 4022 (64.0) | |||
| Other | 238 | 119 (2.3) | 11 (1.0) | 108 (1.7) | |||
| Insurance group | 146.41 4p < 0.0001 | 10.34 4p = 0.001 | Ref. | ||||
| Private insurance | 10,873 | 4360 (83.5) | 935 (86.3) | 5578 (88.7) | |||
| Medicare | 818 | 294 (5.6) | 77 (7.1) | 447 (7.1) | |||
| Medicaid | 167 | 120 (2.3) | 11 (1.0) | 36 (0.6) | |||
| VA | 161 | 74 (1.4) | 18 (1.7) | 69 (1.1) | |||
| Uninsured or unknown | 575 | 375 (7.2) | 43 (4.0) | 157 (2.5) | |||
| Proposed indirect mechanisms: mediators of the effects of violence on current health | |||||||
| (1) Self-perceived stress (MODEL 2) | 420.99 3p < 0.0001 | 33.21 4p < 0.0001 | Ref. | ||||
| Small | 3909 | 1243 (23.8) | 338 (31.2) | 2328 (37.0) | |||
| Moderate | 5553 | 2289 (43.9) | 465 (42.9) | 2799 (44.5) | |||
| Large | 2506 | 1276 (24.4) | 235 (21.7) | 995 (15.8) | |||
| Overwhelming | 626 | 415 (8.0) | 46 (4.2) | 165 (2.6) | |||
| (2) Support (MODEL 3) | |||||||
| Social Support | 226.10 1p < 0.0001 | 41.29 1p < 0.0001 | Ref. | ||||
| No | 1084 | 667 (12.8) | 107 (9.9) | 310 (4.9) | |||
| Yes | 11,510 | 4556 (87.2) | 977 (90.1) | 5977 (95.1) | |||
| Marital status | 461.93 4p < 0.0001 | 2.97 4p = NS | Ref. | ||||
| Married | 8345 | 3045 (58.3) | 772 (71.2) | 4528 (72.0) | |||
| Widowed | 710 | 240 (4.6) | 67 (6.2) | 403 (6.4) | |||
| Never married | 1507 | 617 (11.8) | 111 (10.2) | 779 (12.4) | |||
| Separated | 153 | 107 (2.0) | 13 (1.2) | 33 (0.5) | |||
| Divorced | 1879 | 1214 (23.2) | 121 (11.2) | 544 (8.7) | |||
| (3) Negative health behaviors (MODEL 4), n (% yes) | |||||||
| Current smoker | 1276 | 812 (15.5) | 255.3 1p < 0.0001 | 65 (6.0) | 0.258 1p = NS | 399 (6.3) | Ref. |
| Problem alcohol use | 865 | 582 (11.1) | 237.00 1p < 0.0001 | 47 (4.3) | 0.86 1p = NS | 236 (3.8) | Ref. |
| Sedentary lifestyle | 2799 | 1357 (26.0) | 78.33 1p < 0.0001 | 242 (22.3) | 5.99 1p = 0.008 | 1200 (19.1) | Ref. |
| Current health (outcomes) | |||||||
| (1) Poor mental health (≥4 days, past month) | 788 | 541 (10.4) | 237.00 1p < 0.0001 | 68 (6.3) | 31.94 1p < 0.0001 | 179 (2.8) | Ref. |
| (2) Poor physical health (≥4 days, past month) | 1625 | 931 (17.8) | 208.10 1p < 0.0001 | 146 (13.5) | 23.69 1p < 0.0001 | 548 (8.7) | Ref. |
Mediators
Stress, support, and health behaviors were selected as hypothesized mediators based on past research and the availability of relevant data in WHY (Figure 1). Stress was measured with the following item: “How would you rate the amount of stress you are currently under?” Response options included small, moderate, large, or overwhelming; higher scores indicated higher perceived stress (0–3). This single-item measure was based on a global measure of perceived stress developed and validated by Cohen et al.42 Social support was measured using the following question: “During difficult times in your life, do you feel you have close friends that you can turn to for support?” Response options were yes, no, and choose not to answer (coded as missing and excluded). This single item was adapted from questions in the BRFSS.39 Marital status was included with the single-item social support question because financial or emotional support may increase for those who are married.
Three items measured negative health behaviors: sedentary lifestyle, cigarette smoking, and problem alcohol use. All health behavior items were based on BRFSS questions.39 An item response of “sedentary” for the following was used to define sedentary lifestyle: “Think about a typical day of activities. Is your activity level usually Sedentary—little exercise, or active—you do a lot of moderate activities or very active—you spend a lot of time being very active?” All women were asked to describe their cigarette smoking history based on ever smoking (no or yes, at least 100 cigarettes in lifetime) and if a smoker, whether they currently smoked cigarettes (based on their most recent survey). A dichotomous variable was created to indicate current cigarette smoker (yes v. no) where “no” included never and former smokers. Survey questions differentiated current and past drinkers. Problem drinking was operationally defined for current drinkers as drinking four or more drinks per day (binge drinking) or daily drinkers. Among past drinkers, problem alcohol use was defined with the endorsement of one of the following reasons: the respondent stopped drinking “for health reasons”; “legal reasons”; a doctor, family, or friends said “you needed to stop drinking”; “alcohol was interfering with your work, family, or social life”; or “stopped drinking with help from AA, a therapist, detox, or other treatment center.”
Statistical analysis
The frequency of IPV, SA, and CA was provided by specific items, violence recency, and number of forms (Table 1). To assess potential confounding, violence recency was correlated with demographic attributes, hypothesized mediators, and HR-QOL outcomes (Table 2) using chi-square tests and associated p-values (Table 2). Demographic attributes associated with violence recency (p ≤ 0.01) were considered potential confounders for subsequent modeling to test direct and indirect mechanisms (Fig. 1). Multiple variable log-binomial regression was used to estimate associations between violence and current HR-QOL. Adjusted prevalence rate ratios (aPRRs) and 95% confidence intervals (95% CI) were calculated using PROC GENMOD (link = log, dist = bin). This measure of association was used because incidence of HR-QOL cannot be estimated, yet, prevalence can be based on the most recently completed survey.43
Table 1.
Frequency of Interpersonal Violence by Form, Timing, and Number of Lifetime Co-Occurring Experiences
| n (%) of 12,594 Women in WHY | Overlapping forms of life-time interpersonal violence, n (%) among those experiencing violence forma | ||||
|---|---|---|---|---|---|
| Violence formb | No other form | IPVc | SA | CA | |
| Any lifetime IPV | 4822 (38.3) | 2548 (52.8) | NA | 1224 (25.4) | 1790 (37.1) |
| IPV—physicalc | 3490 (27.7) | 682 (19.5) | 2396 (68.7) | 961 (27.5) | 1380 (39.5) |
| IPV—sexualc | 1674 (13.3) | 77 (4.6) | 1515 (90.5) | 742 (44.3) | 1493 (89.2) |
| IPV—stalkingc | 3227 (25.6) | 680 (21.1) | 2124 (65.8) | 891 (27.6) | 1248 (38.7) |
| All three forms of IPV | 1056 (8.4) | 356 (33.7) | NA | 537 (50.9) | 525 (49.7) |
| Nonpartner sexual (SA) assault | 1625 (12.9) | 179 (11.0) | 1224 (75.3) | NA | 962 (59.2) |
| Any childhood abuse (CSA or CPA) | 3096 (24.6) | 1084 (35.0) | 1790 (57.8) | 962 (31.1) | NA |
| CSA | 1295 (10.3) | 227 (17.5) | 764 (59.0) | 660 (51.0) | NA |
| CPA | 2463 (19.6) | 732 (29.7) | 1725 (70.0) | 876 (35.6) | NA |
| Both CSA and CPA (independent of other forms) | 662 (5.3) | 125 (18.9) | 445 (67.2) | 398 (60.1) | NA |
| Violence combinations (polyvictimization) | |||||
| All three forms: IPV and SA and CA | 744 (5.9) | ||||
| Two forms | 1756 (14.0) | ||||
| IPV and CA | 1046 (8.3) | ||||
| IPV and SA | 484 (3.9) | ||||
| SA and CA | 222 (1.8) | ||||
| One form | 3811 (30.3) | ||||
| SA alone | 179 (1.4) | ||||
| IPV alone | 2548 (20.3) | ||||
| CA alone | 1084 (8.6) | ||||
| Violence timingd | |||||
| Current IPV | 174 (1.4) | ||||
| Past IPV (no current IPV) | 4648 (36.9) | ||||
| Past SA (no IPV) | 401 (3.2) | ||||
| Past CSA (no IPV/SA) | 352 (2.8) | ||||
| Past CPA (no CSA, nor IPV/SA) | 732 (5.8) | ||||
| Hierarchical combinations of violencee | |||||
| Adult IPV or SA | 5223 (41.5) | ||||
| Childhood abuse (no IPV or SA) | 1084 (8.6) | ||||
| No IPV/SA nor CA | 6287 (49.9) | ||||
Denotes overlap within three violence forms; % within row could sum to >100%.
n, independent of overlapping violence forms (% reporting violence among 12,594 participants).
Within IPV forms, overlap indicates presence of either of the two other forms of IPV.
Prioritizes current IPV over past IPV; past IPV over SA by nonpartner; past SA over CA; and childhood sexual over physical abuse.
Simplified timing categories where adult IPV or SA is prioritized over CA (alone) relative to no violence.
CA, childhood abuse; CPA, child physical abuse; CSA, child sexual abuse; IPV, intimate partner violence; NA, not applicable; SA, sexual assault; WHY, Wellness, Health & You.
Measures of association (aPRR and 95% CI) between violence recency and number of forms and current mental and physical HR-QOL, adjusted for demographic attributes, are presented in Table 3 as Model 1 (direct mechanism). Two sets of logistic regression models were run for mental and physical HR-QOL outcomes. Three additional models were run for each mediator, and demographic attributes were included in each model. Given the large sample size and multiple comparisons, p < 0.001 was used to establish statistical significance.
Table 3.
Test of Mediation Models for Interpersonal Violence Recency, Number of Forms, and Self-Reported Days of Poorer Mental and Physical Health (Health-Related Quality Of Life) in the Past Month
| Prevalence rate ratios (95% CI) for violence and current health: models adjusting for demographics (Model 1) and mediators (Models 2–5) | |||||||
|---|---|---|---|---|---|---|---|
| N = 12,594 | n Within violence strata | Poorer current mental HR-QOL,a n (%), n = 788 | Model 1, demographics | Model 2, +stress | Model 3, +support | Model 4, +health behaviors | Model 5, all 1–4 |
| Violence recency | |||||||
| Current IPV | 174 | 46 (26.4) | 6.85 (4.62–10.16) | 3.88 (2.53–5.95) | 5.01 (3.32–7.55) | 5.57 (3.68–8.41) | 2.70 (1.72–4.22) |
| Past IPV, no current | 4648 | 464 (10.0) | 3.19 (2.66–3.83) | 2.37 (1.97–2.87) | 2.72 (2.26–3.27) | 2.71 (2.25–3.26) | 1.88 (1.55–2.29) |
| Past SA (no IPV) | 401 | 31 (7.7) | 2.55 (1.70–3.81) | 1.75 (1.15–2.66) | 2.17 (1.44–3.27) | 2.11 (1.40–3.18) | 1.34 (0.87–2.07) |
| Past CA | 1084 | 68 (6.3) | 2.22 (1.66–2.98) | 1.85 (1.37–2.51) | 2.03 (1.51–2.73) | 2.17 (1.61–2.91) | 1.76 (1.29–2.39) |
| No. of violence forms (polyvictimization) | |||||||
| Three forms: IPV and SA and CA | 740 | 150 (20.3) | 6.23 (4.87–7.97) | 4.07 (3.13–5.30) | 4.86 (3.78–6.27) | 4.90 (3.80–6.32) | 3.01 (2.29–3.96) |
| Two formsb | 1756 | 210 (12.0) | 3.85 (3.11–4.77) | 2.69 (2.15–3.37) | 3.22 (2.59–4.00) | 3.17 (2.54–3.94) | 2.06 (1.64–2.60) |
| One form | 3811 | 249 (6.5) | 2.19 (1.80–2.68) | 1.75 (1.42–2.15) | 1.96 (1.60–2.40) | 2.00 (1.63–2.44) | 1.50 (1.22–1.86) |
| None | 6287 | 179 (2.8) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Poorer current physical HR-QOL,a n (%), n = 1625 | |||||||
|---|---|---|---|---|---|---|---|
| Violence recency | |||||||
| Current IPV | 174 | 47 (27.0) | 3.34 (2.33–4.81) | 2.33 (1.60–3.40) | 2.90 (2.00–4.20) | 3.05 (2.09–4.45) | 2.12 (1.43–3.14) |
| Past IPV, no current | 4648 | 814 (17.5) | 2.14 (1.90–2.41) | 1.83 (1.62–2.07) | 1.99 (1.76–2.25) | 1.95 (1.72–2.21) | 1.67 (1.47–1.89) |
| Past SA (no IPV) | 401 | 70 (17.5) | 2.17 (1.64–2.87) | 1.80 (1.36–2.40) | 2.01 (1.52–2.66) | 1.93 (1.46–2.57) | 1.59 (1.19–2.12) |
| Past CA (no IPV/SA) | 1084 | 68 (6.3) | 2.22 (1.66–2.98) | 1.85 (1.37–2.51) | 2.03 (1.51–2.73) | 2.17 (1.61–2.91) | 1.76 (1.29–2.39) |
| No. of violence forms (polyvictimization) | |||||||
| Three forms: IPV and SA and CA | 740 | 215 (29.1) | 3.75 (3.12–4.53) | 2.96 (2.43–3.60) | 3.33 (2.74–4.05) | 3.24 (2.66–3.94) | 2.56 (2.09–3.11) |
| Two formsb | 1756 | 352 (20.0) | 2.51 (2.15–2.91) | 2.07 (1.77–2.41) | 2.31 (1.98–2.69) | 2.23 (1.91–2.61) | 1.84 (1.57–2.16) |
| One form | 3811 | 510 (13.4) | 1.62 (1.42–1.84) | 1.45 (1.27–1.65) | 1.54 (1.35–1.76) | 1.54 (1.35–1.76) | 1.37 (1.20–1.57) |
| No violence | 6287 | 548 (8.7) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
Model 1: adjusted for demographic variables age (grouped as 18–39, 40–54, and 55+), not exclusively heterosexual (yes or no), education (≤high school graduate, some college or associates degree, college graduate, or beyond, other), health insurance coverage (private, Medicare, Medicaid, VA, or other governmental, uninsured or unknown), Kentucky region (rural vs. urban). Adjustments are based on the most recent survey with the exception of not exclusively heterosexual. Model 2: additionally adjusted for self-perceived stress (small, moderate, large, and overwhelming amount). Model 3: additionally adjusted for current social support (yes or no) and marital status (currently married or not). Model 4: additionally adjusted for sedentary lifestyle (yes or no), current smoker (yes or no) and substance abuse (yes or no). Model 5: adjusted for all variables in Models 1–4.
Poorer health defined as ≥4 of the past 30 days when poor mental health (repeated as physical) prevented usual daily activities, such as self-care, work, or recreation.
Categories include IPV and SA or SA alone.
95% CI, 95% confidence interval; HR-QOL, health-related quality of life; Ref., Referent Group; SA, sexual assault as an adult (>18) by someone other than an intimate partner.
Evidence of mediation arose through comparisons of aPRR and 95% CI resulting from Model 1 with Models 2–4, including each mediator and Model 5 with all mediators. Mediation evidence was defined by changes in the aPRR and 95% CI for violence (recency or forms) and HR-QOL no longer being statistically significantly associated (aPRR and 95% CI for addition of mediator included 1.0). Percent change in the estimated PRR resulting from Models 1 and 5, where Model 1 was used as the denominator change estimation, provided a qualitative descriptor of the degree of mediated effect.
Results
Of 16,645 WHY participants, 4051 participants were excluded due to missing violence exposures or HR-QOL outcomes (n = 633) or demographics attributes (n = 3418). Of the final analytical sample (n = 12,594), the number of participants increased from 2008 to 2014 as follows: (2008: 1221; 2009: 775; 2010: 1154; 2011: 1794; 2012: 2029; 2013: 2737; and 2014: 2884). In the decade of data collection, 3439 of 12,594 women (27.3%) completed one survey, 2156 (17.1%) completed two, 1700 (13.5%) completed three, 2818 (22.4%) completed four or five, and 2481 (19.7%) completed six or more surveys.
Overall sample and violence experienced
In this relatively well-educated population, 50.1% reported ever experiencing one of the three violence forms (IPV, SA, or CA) (Table 1): IPV (38.3%), adult SA (12.9%), or CA (24.6%). A minority (1.4%) were currently experiencing IPV.
Polyvictimization was identified by 19.9% of women (Table 1). Among women experiencing IPV (n = 4822), 52.8% reported IPV “alone,” while 25.4% and 37.1% additionally experienced SA and/or CA. Women experiencing SA by a nonpartner (n = 1625) were most likely to have experienced other forms of violence.
Correlates of violence
The following demographic attributes were associated with violence recency (p ≤ 0.01) and were considered as confounders: age, sexual orientation, Kentucky region, education, and insurance coverage (Table 2). Although race was correlated with violence (Table 2), it was not included as a confounder because models did not converge due to high correlations between race and education, region, and insurance coverage. Mediators were selected based on past research correlating these factors with violence and health; as anticipated, each was correlated with violence (p < 0.001).
Among 12,594 participants, 6.3% had ≥4 days of poor mental health and 12.9% had ≥4 days of poor physical health (Table 2). As hypothesized, IPV or SA and CA “alone” were associated with poorer current mental and physical HR-QOL outcomes (p < 0.0001).
Violence and HR-QOL (direct mechanism)
There was evidence that both violence recency and number of forms were associated with poorer HR-QOL (see Table 3, Model 1, research question 1). When compared with women experiencing no violence, those currently disclosing IPV (aPRR = 6.85) had significantly higher rate of poorer mental HR-QOL. This pattern held for past IPV (aPRR = 3.19), SA (aPRR = 2.55), and CA (aPRR = 2.22). A similar pattern was observed for recency and poorer physical HR-QOL, yet 95% CIs overlapped.
With increasing number of violence forms, an increased effect on poorer mental and physical HR-QOL was observed; relative to “no violence” those experiencing a greater number of violence forms had greater prevalence of poorer HR-QOL outcomes. For mental HR-QOL, the aPRR estimates for experiencing all three forms (aPRR = 6.23), two forms (aPRR = 3.85), or one form (aPRR = 2.19) were all significantly different evidenced by nonoverlapping 95% CIs (Table 3). A similar pattern was observed for physical HR-QOL, although aPRR estimates were smaller than for mental HR-QOL.
Violence, mediators, and HR-QOL (indirect mechanisms)
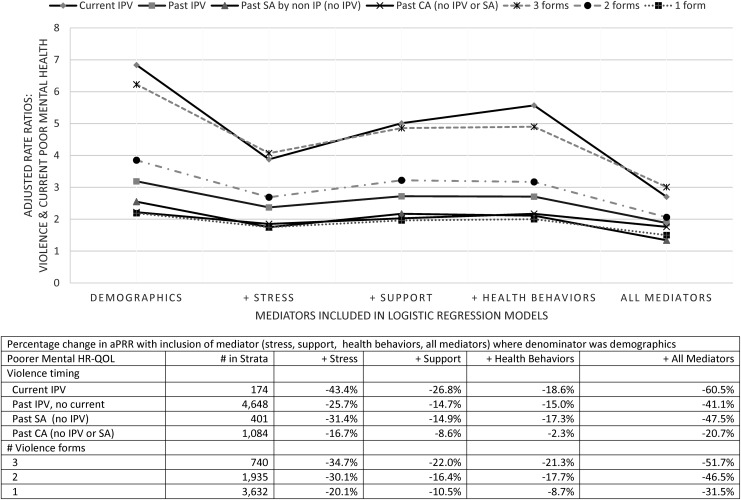
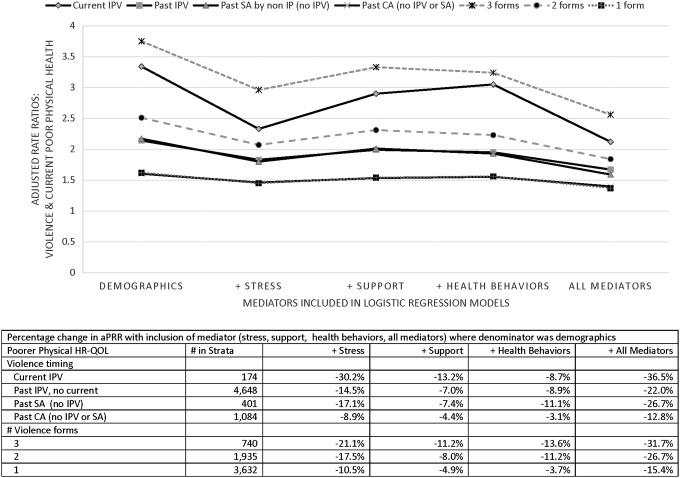
Models 2–5 provide the data needed to examine research question 2. The addition of each mediator resulted in a reduction of aPRR estimate relative to Model 1 (demographics only) for violence recency and number of forms and both HR-QOL outcomes (Table 3). However, across all three mediators for both HR-QOL outcomes, the greatest qualitative change in aPRRs was consistently observed in models with the addition of stress (comparison of Models 1 and 2). This observation was most clearly illustrated in Figures 2 and 3 for mental and physical HR-QOL, respectively, where the aPRR estimates across Models 1–5 for violence recency, and number of forms were presented with percent change from Model 1 (adjusting for only demographics).
FIG. 2.
Violence recency, number of forms, and current poor mental HR-QOL. HR-QOL, health-related quality of life.
FIG. 3.
Violence recency, number of forms, and current poor physical HR-QOL.
When all mediators were included (Model 5), the aPRR estimates, as observed, were consistently lowest when compared across all models. Only the aPRR estimate for poorer mental HR-QOL and past SA (and no IPV; n = 401) was no longer statistically significant (Model 5: aPRR = 1.34 [95% CI: 0.87–2.07]). However, when comparing results from Models 1 and 5 (poorer mental HR-QOL outcome) for violence recency and number of forms, significant differences with nonoverlapping aPRRs CIs with the addition of mediator variables were apparent. Similar trends were noted for physical HR-QOL, but only for past IPV and experiencing all violence forms. Considering the percent change in aPRR estimates provided a qualitative measure of the extent that mediators indirectly may affect outcomes. The inclusion of stress resulted in the greatest observed percent change in aPRR estimates (see Figs. 2 and 3 legend tables for mental and physical HR-QOL, respectively). For example, adding stress to Model 1 resulted in a 34.7%, 30.1%, and 20.1% reduction in the aPRR estimates for poorer mental HR-QOL for three, two, and one violence forms, respectively. The inclusion of all mediators (Model 5 vs. Model 1) resulted in an overall reduction of 51.7%, 46.5%, and 31.5% in aPRR estimates for number of violence forms (three, two, and one) and poorer mental HR-QOL.
Discussion
IPV, SA, and CA were each associated with at least a twofold increase of poorer current mental and physical HR-QOL; experiencing multiple violence forms increased this risk in a dose-dependent pattern. While full mediation by stress, support, and health behaviors was not observed, evidence of partial mediation was noted for current stress as the more important mediator. This finding fits with the existing literature indicating that violence resulted in symptoms of posttraumatic stress disorders linked to long-term health impacts.5,44–46 If the impact of violence on current health can be partially mitigated through reducing perceived stress, the effects of IPV, SA, and CA may be significantly reduced. Improvements in current HR-QOL may impact economic evaluation driven by changes in the quality-adjusted life-year measuring disease burden, including both the quality and the quantity of life lived.40
From a clinical perspective, the contribution of this research is our finding that current perceived stress is the strongest of the three tested mediators and that including stress in models with violence recency and number of violence forms resulted in the largest reductions in the effect of violence on current health. Given the high frequency of adult and childhood violence (>40%), even in this more highly educated population, screening all patients for a history of violence is not feasible in a busy clinical setting. However, asking about current stress at clinical visits is feasible. Clinical approaches to reduce the impact of past violence on current HR-QOL may be more efficient and acceptable to patients if providers have information on past violence and ask patients about their current stress levels. From a health perspective, the salient issue for patients may well be their distress and concurrent poorer health status. Previous research, described in the following paragraph, indicates that clinical and community-based interventions have been developed and evaluated. These approaches may be useful to improve HR-QOL among women who have experienced violence and are currently distressed. While past violence may be a source of the distress, using group or individual behavioral therapy to address stress may more acceptable and efficacious in improving health.
Previous interventions addressing current violence are relevant for this discussion if the outcomes are mental or physical health. Findings from a reanalysis47 of a large randomized controlled trial of an intervention to improve health and safety outcomes for abused women (Women's Evaluation of Abuse and Violence) illustrate this point.48 The reanalysis documented that self-efficacy was the construct most predictive of abused women creating or maintaining change; depression predicted no changes.47 Findings from this reanalysis and our current findings highlight the need for interventionists to assess depression/anxiety and target self-efficacy as a route to change.
Because many women and men do not disclose SA until long after the incident,49 the efficacy of interventions to address past violence are relevant to this discussion. The WHO guidelines16 recommend Eye Movement Desensitization and Reprocessing (EMDR) and CBT.50 Lieberman et al.51 found evidence of Child-Parent Psychotherapy (CPP) effectiveness to reduce mothers' PTSD symptoms and general distress. Importantly for the current analysis, CPP was effective and results were sustained for 6 months among those exposed to multiple traumatic life events.52 Similarly, in Project Support,53 mothers showed improvements in parenting behaviors and reductions in psychiatric symptoms.
It is not coincidental that most treatments for traumatic stress conditions involve self-regulation and stress-reduction strategies. Cognitive behavioral strategies to reduce stress levels by cognitive restructuring and self-regulation have been shown to interrupt the progression of stress response into damaging and persistent internalizing and externalizing behaviors that can lead to adverse health outcomes.12,13 The optimal timing for delivery of this type of intervention is paramount, as more proximal therapeutic responses have been shown to be preferable and capable of stemming the long-term impact associated with an unmitigated stress response.14
Interestingly, negative health behaviors were not strong mediators of the IPV and current health associations. Efforts to reduce negative health behaviors (physical inactivity, smoking, and alcohol abuse16) are important, but these efforts in combination with those to increase support and reduce stress might be more effective.
Limitations
The present analysis exclusively used self-reported data for all measures, including violence experienced, current mental and physical HR-QOL, hypothesized mediators, and demographic attributes. Reliance on self-reported data may result in misclassification of measures. For several measures, self-report was the only source of data because perceptions of HR-QOL, stress, support were hypothesized. In this cross-sectional analysis using self-selected WHY participants, we cannot determine the correct temporal sequence between violence and current poorer HR-QOL. However, by using the most recent WHY survey data to measure all variables, we were able to address the appropriate temporal sequence. Admittedly, those experiencing violence may have poorer HR-QOL before violence. The list of childhood or adult violent exposures used in this study was not exhaustive; our focus was on IPV, adult SA, and CA because these are the more commonly occurring forms of interpersonal violence among women. Poorer HR-QOL is not a diagnosis yet. As operationally defined, HR-QOL measures the current and sustained impact of health conditions on daily activities or functions. Stress, social support, and health behaviors were the mediators investigated in this analysis, yet, these are by no means the only mediators or intervention targets to reduce the impact of past violence on current HR-QOL.
Conclusion
Women's current and past IPV, SA, and CA experiences alone or in combination continue to be associated with poorer current mental and physical HR-QOL relative to those with no violence experience, even after adjusting for current stress, social support, and health behaviors. Finding evidence of partial mediation of the effect of violence on poorer HR-QOL by current perceived stress supports the WHO recommendation for trauma-focused CBT and related interventions among women not currently experiencing violence. Further intervention development and adaptation to reduce (dis)stress and ultimately mitigate the impact of past violence on women's current perceptions of health are encouraged.
Acknowledgments
The project described was supported by the NIH National Center for Advancing Translational Sciences through grant number UL1TR001998. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The study protocols were approved by the appropriate Institutional Review Board.
Author Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1. Black MC, Basile KC, Breiding MJ, et al. The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 Summary report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, 2011 [Google Scholar]
- 2. World Health Organization. Global and regional estimates of violence against women: Prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva: World Health Organization, 2013 [Google Scholar]
- 3. Peterson C, Kearns M, McIntosh WI, et al. Lifetime economic burden of intimate partner violence among USA adults. Am J Prev Med 2018;55:433–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sugg N. Intimate partner violence: Prevalence, health consequences, and intervention. Med Clin North Am 2015;99:629–649 [DOI] [PubMed] [Google Scholar]
- 5. Fellitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) study. Am J Prev Med 1998;14:245–258 [DOI] [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System survey ACE module data, 2010. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2015. Available at: www.cdc.gov/violenceprevention/acestudy/index.html Accessed August8, 2018 [Google Scholar]
- 7. Fang X, Brown DS, Florence C, Mercy J. The economic burden of child maltreatment in the United States and implications for prevention. Child Abuse Negl 2012;36:156–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Letourneau EJ, Brown DS, Fang X, Hassan A, Mercy JA. The economics burden of child sexual abuse in the United States. Child Abuse Negl 2018;79:413–422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Basile KC, Breiding MJ, Smith SG. The association of disability status and recent sexual violence victimization among a national sample of women and men. Am J Public Health 2016;106:928–933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Abrahams N, Devries K, Watts C, et al. Worldwide prevalence of non-partner sexual violence: A systematic review. Lancet 2014;383:1648–1654 [DOI] [PubMed] [Google Scholar]
- 11. Paras ML, Murad MH, Chen LP, et al. Sexual abuse and lifetime diagnosis of somatic disorders: A systematic review and meta-analysis. J Am Med Assoc 2009;302:550–561 [DOI] [PubMed] [Google Scholar]
- 12. Peterson C, DeGue S, Florence C, Lokey CN. Lifetime economic burden of rape among U.S. adults. Am J Prev Med 2017;52:691–701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. García-Moreno C, Hegarty K, d'Oliveira AFL, Koziol-McLain J, Colombini M, Feder G. The health-systems response to violence against women. Lancet 2015;385:1567–1579 [DOI] [PubMed] [Google Scholar]
- 14. Cork C, White R, Noel P, Bergin N. Randomized controlled trials of interventions addressing intimate partner violence in Sub-Saharan Africa: A systematic review. Trauma Violence Abuse 2018;1–17. DOI: 10.1177/1524838018784585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Signorelli MC, Hillel S, de Oliveira DC, Quintanilla BPA, Hegarty K, Taft A. Voices from low-income and middle income countries: A systematic review protocol of primary healthcare interventions within public health systems addressing intimate partner violence against women. BMJ Open 2018;8:e019266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. World Health Organization. Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. Geneva: WHO, 2013. Available at: http://apps.who.int/iris/bitstream/10665/85240/1/9789241548595_eng.pdf?ua=1 Accessed March17, 2016 [PubMed] [Google Scholar]
- 17. Feder G, Wathen CN, MacMillian HL. An evidence-based response to intimate partner violence: WHO Guidelines. JAMA 2013;310:479–480 [DOI] [PubMed] [Google Scholar]
- 18. Taft A, Colombini M. Healthcare system responses to intimate partner violence in low and middle-income countries: Evidence is growing and the challenges become clearer. Commentary. BMC Med 2017;15:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rivas C, Ramsay J, Sadowski L, et al. Advocacy interventions to reduce or eliminate violence and promote the physical and psychosocial well-being of women who experience intimate partner abuse. Cochrane Database Syst Rev 2015;3:CD005043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Preventing multiple forms of violence: A strategic vision for connecting the dots. Atlanta, GA: Division of Violence Prevention, National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, 2016 [Google Scholar]
- 21. Centers for Disease Control and Prevention. Measuring healthy days. Atlanta, GA: CDC, 2000 [Google Scholar]
- 22. Campbell JC. Health consequences of intimate partner violence. Lancet 2002;359:1331–1336 [DOI] [PubMed] [Google Scholar]
- 23. Golding JM. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. J Fam Violence 1999;14:99–132 [Google Scholar]
- 24. Polusny MA, Follette VM. Long-term correlates of child sexual abuse: Theory and review of empirical literature. Appl Prev Psychol 1995;4:143–166 [Google Scholar]
- 25. Campbell R, Greeson MR, Bybee D, Raja S. The co-occurrence of childhood sexual abuse, adult sexual assault, intimate partner violence, and sexual harassment: A mediational model. J Consult Clin Psychol 2008;76:194–207 [DOI] [PubMed] [Google Scholar]
- 26. CDC. Social support and health-related quality of life among older adults—Missouri, 2000. MMWR Morb Mortal Wkly Rep 2005;54:433–437 [PubMed] [Google Scholar]
- 27. Ozbay F, Johnson DC, Dimoulas E, Morgan III CA, Charney D, Southwick S. Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry 2007;4:35–40 [PMC free article] [PubMed] [Google Scholar]
- 28. Coker AL, Smith PH, Thompson MP, McKEown RE, Bethea L. Social support protects against the negative effects of partner violence on mental health. J Women's Health 2002;11:465–476 [DOI] [PubMed] [Google Scholar]
- 29. Sylaska KM, Edward KM. Disclosure of intimate partner violence to informal social support network members: A review of the literature. Trauma Violence Abuse 2014;15:3–21 [DOI] [PubMed] [Google Scholar]
- 30. Sigalla GN, Rasch V, Gammeltoft T, et al. Social support and intimate partner violence during pregnancy among women attending antenatal care in Moshi municipality, Northern Tanzania. BMC Public Health 2017;17:240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rehm J, Baliunas D, Borges GL, et al. The relation between different dimensions of alcohol consumption and burden of disease: An overview. Addiction 2010;105:817–843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. U.S. Department of Health and Human Services. The health consequences of smoking: A report of the surgeon general. Rockville, MD: Centers for Disease Control and Prevention, 2004. Available at: www.cdc.gov/tobacco/data_statistics/sgr/sgr_2004 Accessed August18, 2016 [Google Scholar]
- 33. Penedo FJ, Dahn JR. Exercise and well-being: A review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry 2005;18:189–193 [DOI] [PubMed] [Google Scholar]
- 34. Bize R, Johnson JA, Plotnikoff RC. Physical activity level and health-related quality of life in the general adult population: A systematic review. Prev Med 2007;45:401–415 [DOI] [PubMed] [Google Scholar]
- 35. Boles SM, Miotto K. Substance abuse and violence: A review of the literature. Aggress Violent Behav 2003;8:155–174 [Google Scholar]
- 36. Crane CA, Hawes SW, Weinberger AH. Intimate partner violence victimization and cigarette smoking: A meta analytic review. Trauma Violence Abuse 2013;14:305–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Smith A, Markovic N, Danielson ME, et al. Sexual abuse, sexual orientation and obesity in women. J Womens Health 2010;19:1525–1532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Gunstad J, Paul RH, Spitznagel MB, et al. Exposure to early life trauma is associated with adult obesity. Psychiatry Res 2006;142:31–37 [DOI] [PubMed] [Google Scholar]
- 39. Behavioral Risk Factor Surveillance System Survey Questionnaire. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, 2007 [Google Scholar]
- 40. Moriatry DG, Zack MM, Kobau R. The Centers for Disease Control and Prevention's healthy days measures—Population tracking of perceived physical and mental health over time. Health Qual Life Outcomes 2013;1:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hennessy CH, Moriarty DG, Zack MM, Scherr PA, Brackbill R. Measuring health-related quality of life for public health surveillance. Public Health Rep 1994;109:665–672 [PMC free article] [PubMed] [Google Scholar]
- 42. Cohen S, Kamarck T, Mercelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385–396 [PubMed] [Google Scholar]
- 43. Tamhane AR, Westfall AO, Burkholder GA, Cuter GR. Prevalence odds ratio versus prevalence ratio: Choice comes with consequences. Stat Med 2016;25:5730–5735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci 2009;10:434. [DOI] [PubMed] [Google Scholar]
- 45. Mechanic MB, Weaver TL, Patricia A. Resick PA. Mental health consequences of intimate partner abuse. A multidimensional assessment of four different forms of abuse. Violence Against Women 2008;14:634–654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jaquier V, Hellmuth JC, Sullivan TP. Posttraumatic stress and depression symptoms as correlates of deliberate self-harm among community women experiencing intimate partner violence. Psychiatry Res 2013;206:37–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Reisenhofer SA, Hegarty K, Valpied J, Watson LF, Davey MA, Taft A. Longitudinal changes in self-efficacy, mental health, abuse, and stages of change, for women fearful of a partner: Findings from a primary care trial (WEAVE). J Interpers Violence 2019;34:337–365 [DOI] [PubMed] [Google Scholar]
- 48. Hegarty KL, Gunn JM, O'Doherty LJ, et al. Women's evaluation of abuse and violence care in general practice: A cluster randomised controlled trial (WEAVE). BMC Public Health 2010;10:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lanthier S, DuMont J, Mason R. Responding to delayed disclosure of sexual assault in health settings: A systematic review. Trauma Violence Abuse 2018;19:251–265 [DOI] [PubMed] [Google Scholar]
- 50. O'Callaghan P, McMullen J, Shannon C, Rafferty H, Black A. A randomized controlled trial of trauma-focused cognitive behavioral therapy for sexually exploited, war-affected Congolese girls. J Am Acad Child Adolesc Psychiatry 2013;52:359–369 [DOI] [PubMed] [Google Scholar]
- 51. Lieberman AF, Van Horn P, Ippen CG. Toward evidence-based treatment: Child-parent psychotherapy with preschoolers exposed to marital violence. J Am Acad Child Adolesc Psychiatry 2005;44:1241–1248 [DOI] [PubMed] [Google Scholar]
- 52. Ippen CG, Harris WW, Van Horn P, Lieberman AF. Traumatic and stressful events in early childhood: Can treatment help those at highest risk? Child Abuse Negl 2011;35:504–513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Jouriles EN, McDonald R, Rosenfield D, Stephens N, Corbitt-Shindler D, Miller PC. Reducing conduct problems among children exposed to intimate partner violence: A randomized clinical trial examining effects of Project Support. J Consult Clin Psychol 2009;77:705–717 [DOI] [PubMed] [Google Scholar]