Abstract
Background:
Whether the time course of post-stroke depression (PSD) can be used to predict the quality of life (QoL) of patients with late-stage stroke remains unclear, this study investigated whether persistent depression at 1 year after stroke predicts QoL at 5 years following stroke.
Methods:
We analyzed the demographic and clinical data of patients with stroke in 56 hospitals across China that participated in the Prospective Cohort Study on the Incidence and Outcome of Patients with PSD in China Study. Follow-up assessments were performed at the following time points after stroke: in person, 2 weeks, 3 months, 6 months, and 1 year; by telephone, 5 years. National Institutes of Health Stroke Scale (NIHSS) score on admission, recurrence, disability, depression, QoL, and chronic complications were recorded. Depression was diagnosed using the Diagnostic and Statistical Manual of Mental Disorders. QoL was measured using short form-12 (SF-12). Multivariable ordinal logistic regression analysis was used to identify factors that independently affected the physical component summary (PCS) and mental component summary (MCS) scores of the SF-12.
Results:
Of the 801 patients evaluated in this study, 80 had persistent depression. The multivariable regression analysis of data obtained at 5 years showed that persistent depression at 1 year (odds ratio [OR]: 0.48; 95% confidence interval [CI]: 0.29–0.81) and disability at 5 years (OR: 0.34; 95% CI: 0.23–0.49) were associated with poor MCS scores at 5 years. Old age, a high NIHSS score on admission, disability at 5 years, and stroke recurrence within 5 years were associated with poor PCS scores at the 5-year follow-up.
Conclusions:
Persistent depression at the 1-year follow-up could predict poor MCS scores at the 5-year follow-up. The development of interventional strategies targeting post-stroke patients with persistent depression is warranted.
Keywords: Depression, Quality of Life, Stroke, Predictor
Introduction
Although the fatality rates in the acute phase of stroke have decreased owing to significant therapeutic advances,[1] stroke remains a leading health problem worldwide.[2] Moreover, maintaining or improving the quality of life (QoL) of stroke survivors in the chronic stage of the disease is becoming an increasingly important research area.
Various factors, such as age, sex, comorbidities, stroke severity, anxiety, and depression, have been identified as determinants of QoL in patients with chronic stroke.[3–5] In particular, some studies have indicated that depression is a major independent variable of the QoL of stroke survivors,[6] and several cross-sectional studies have shown that depression correlates with a low QoL at any time after stroke.[5–8] However, research on the longitudinal impact of depression on the QoL of stroke patients is rare.
Post-stroke depression (PSD) is a well-documented sequel of stroke,[9] and some authors have suggested that it exacerbates the severity of other stroke-induced disabilities.[10,11] However, only a few studies have focused on the time course of PSD; the limited amount of research on the topic has indicated the PSD can be transient, lasting only a few months, or maybe chronic.[12] Moreover, it remains unknown whether the time course of PSD can be used to predict patients’ QoL in the late stage of stroke. Thus, in the present report, we used data collected by a national, longitudinal study of a post-stroke cohort to determine whether the presence of PSD at 1 year following stroke predicts a poor QoL at 5 years after stroke.
Methods
Ethical approval
The study was approved by the medical ethics committee of Beijing Tian Tan Hospital, Capital Medical University. The study complied with the Declaration of Helsinki and its later amendments. Patients provided written informed consent and agreed to undergo follow-up at all scheduled times.
Participants
The data used in this 5-year follow-up study of stroke patients were collected from the Prospective Cohort Study on the Incidence and Outcome of Patients with PSD in China (PRIOD, project No. ISRCTN62169508: a large-scale, multi-center study with 56 participating hospitals nationwide).[10] Patients with stroke were recruited in the PRIOD study between April 2008 and April 2010 and were followed up in person four times following the stroke: 2 weeks, 3 months, 6 months, and 1 year (day 14 ± 2, day 84 ± 2, day 182 ± 2, day 360 ± 7, respectively). In addition, the patients were followed up by telephone at 5 years after stroke.
The following inclusion criteria were used to select patients eligible for inclusion in the present study: age >18 years, diagnosis of stroke informed by computed tomography or magnetic resonance imaging obtained within 14 days, and consistency between clinical presentations and the World Health Organization criteria for stroke.[13] Patients were excluded if they had dementia, obvious aphasia that could impede psychological assessments, other known neurological diseases that could affect cognitive function, psychiatric diagnosis, difficulty in communication, or death within the 5 years of follow-up.
Demographic and clinical variables
Demographic data (eg, age, sex, living condition [alone vs. with family], education, marital status, and personal characteristics), medical history, past psychiatric diagnoses, vascular risk factors (eg, history of hypertension, diabetes, or smoking), and clinical characteristics (eg, type of stroke, National Institutes of Health Stroke Scale [NIHSS] score at admission) were collected at the time of enrollment.
At the 5-year follow-up, data on stroke recurrence, disability, depression, QoL, and chronic complications (eg, hypertension, hyperlipidemia, diabetes, and coronary heart disease) were collected.
Measurements and evaluations
The clinical physiologists responsible for the follow-up of the patients at each center received systematic training in the use of the clinical assessment tools and application of the diagnostic criteria. The diagnosis of depression was based on the Diagnostic and Statistical Manual of Mental Disorders (fourth edition).[14]
The Composite International Diagnostic Interview was used to diagnose depression at day 14 ± 2.[15] The MINI International Neuropsychiatric Interview was used to diagnose depression at the 5-year follow-up.[16] The Hamilton Rating Scale for Depression-17 (17 items) was used to assess the severity of depression symptoms at 2 weeks, 3 and 6 months, and 1 year post-stroke.[17] Symptoms of depression at the 5-year follow-up were assessed using the patient health questionnaire-9.[18] Cognitive status was assessed using the mini-mental state examination (MMSE) at 3 months after stroke.[19] Patients with an MMSE score of <18 were considered to have serious cognitive impairment and were thus excluded from the study.[20] Disability was assessed using the modified Rankin score (mRS) at the 5-year follow-up and was defined as an mRS score ≥2.[21,22]
QoL was determined using the medical outcomes short form (SF)-12 (version 2) at the 5-year follow-up.[23] Derived from the SF-36, the SF-12 consists of eight domains and 12 items, which are grouped into two summary measures: the physical component summary (PCS) and the mental component summary (MCS). The SF-12 is scored on a scale of 0 to 100, where higher scores indicate better QoL.
Diagnosis and time course of PSD
Persistent depression was defined as the presentation of depression at each follow-up examination: 2 weeks, 3 months, 6 months, and 1 year. Transient depression was defined as confirmation of depression at one to three consecutive follow-up visits without any subsequent recurrence of depressive symptoms. Recurrent depression was defined as the reappearance of depressive symptoms after the documented recovery from a previous episode of depression.[24] Transient and recurrent depression was considered non-persistent forms of depression.
Statistical analysis
Statistical analyses were conducted using the Statistical Product and Service Solutions v24.0 (SPSS Inc., IBM Company, Chicago, IL, USA). Continuous data were expressed as median (interquartile range) or mean ± standard deviation. When comparing characteristics between the included patients and those who were lost to follow up, the categorical variables were analyzed with the chi-square test; the continuous variables, such as age, were analyzed with the independent t-test, and NIHSS scores were analyzed with the Mann-Whitney U test. In the multiple comparisons, the continuous variables, such as age, were analyzed with a one-way analysis of variance while the NIHSS, PCS, and MCS scores were analyzed with the Kruskal-Wallis test; the categorical variables, such as sex and level of education, were analyzed with the chi-square test. The association between persistent depression and QoL at the 5-year follow-up was analyzed using a multiple ordinal regression analysis with the group of patients without depression used as the reference. The PCS and MCS scores of the SF-12 were converted into categorical variables expressed as quartiles, which were then inputted into the ordinal regression analyses as dependent variables. Selected for inclusion into the models based on evidence from previous research and a high likelihood of influencing the MCS and PCS scores,[5] variables measured at admission were sequentially entered into the admission model as confounding variables, while those noted at the 5-year follow-up were entered into the 5-year follow-up model as confounding variables. For all analyses, a two-tailed probability value of P < 0.05 was considered to indicate statistical significance.
Results
Patient characteristics
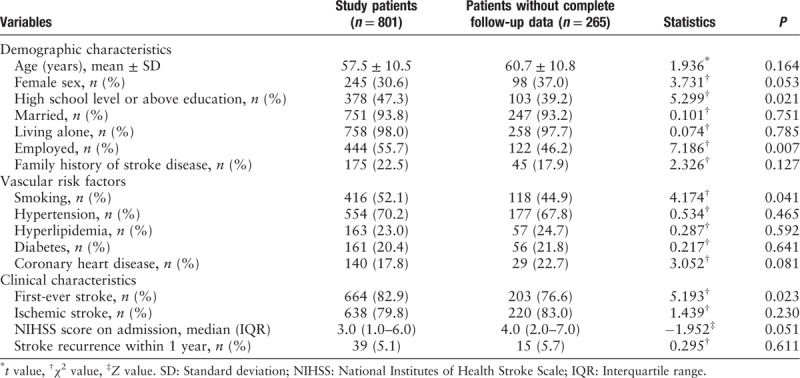
Excluding the patients who were ineligible for enrolment and those who did not complete follow-up, the present analysis included the data of 801 stroke patients (mean age, 57.5 ± 10.5 years) [Figure 1]. Compared with the 801 patients included in the final analysis, the 265 patients without complete follow-up data were associated with lower levels of education (39.2% vs. 47.3%, P = 0.021) and rates of employment (46.2% vs. 55.7%, P = 0.007), smoking (44.9% vs. 52.1%, P = 0.041), and first-ever stroke (76.6% vs. 82.9%, P = 0.023) [Table 1]. The other variables did not significantly differ between the two groups.
Figure 1.
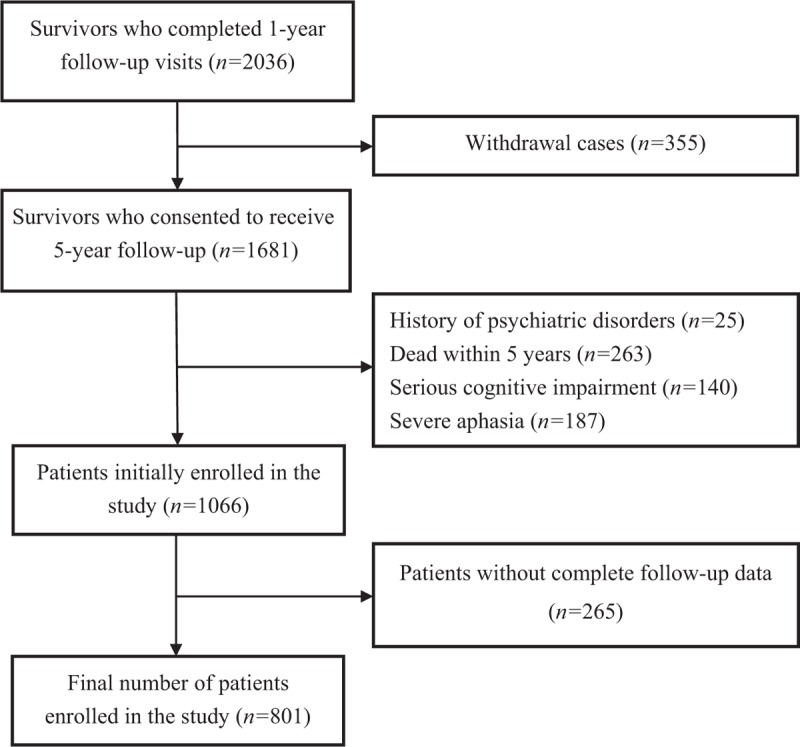
Flow chart of participant selection.
Table 1.
Characteristics of the study patients and those without complete follow-up data.
Multiple comparisons of characteristics of patients with persistent depression, non-persistent depression, and patients without depression
At the 1-year follow-up, 330 of 801 stroke patients were diagnosed as having depression: 80 (24.3%) had persistent depression, 217 (65.7%) had transient depression, and 33 (10.0%) had recurrent depression.
Compared with the other two groups, stroke patients with persistent depression were significantly older, more likely to be a woman and have a family history of stroke, had significantly higher NIHSS scores, were significantly less likely to have had an ischemic stroke, and had a significantly higher frequency of hypertension. At the 5-year follow-up, stroke patients with persistent depression had significantly higher disability rates and significantly lower PCS and MCS scores than patients without depression. No other significant differences were found among the three groups [Table 2].
Table 2.
Multiple comparisons of the characteristics of patients according to the categories of PSD.
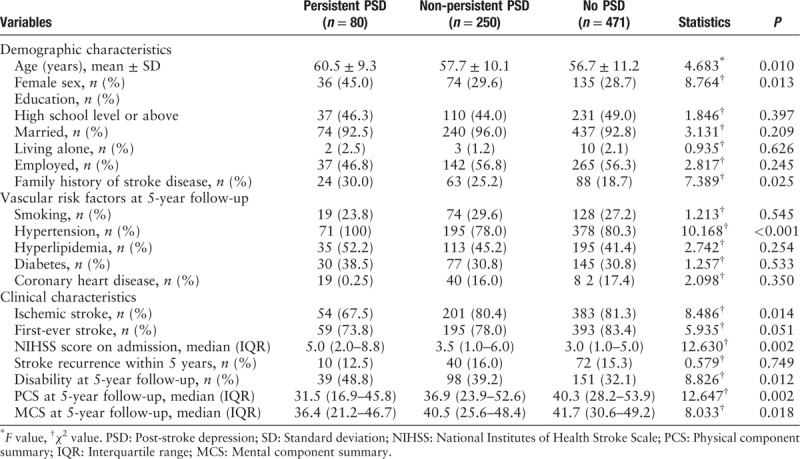
However, we found no significant differences between patients with non-persistent depression and those with no depression with respect to proportion of women (29.6% vs. 28.7%, P = 0.792), rate of ischemic stroke (80.4% vs. 81.3%, P = 0.802), age (57.7 ± 10.1 vs. 56.7 ± 11.2, P = 0.248), NIHSS scores (3.5 [1.0–6.0] vs. 3.0 [1.0–5.0], P = 0.183), PCS scores (36.9 [23.9–52.6] vs. 40.3 [28.2–53.9], P = 0.111), and MCS scores (40.5 [25.6–48.4] vs. 41.7 [30.6–49.2], P = 0.063).
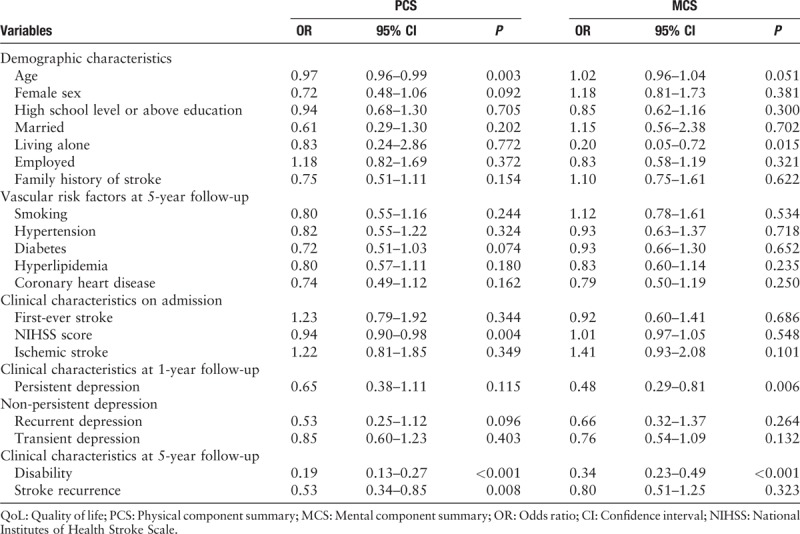
Risk factors associated with QoL
The risk factors associated with QoL assessed at the 5-year follow-up model are shown in Table 3. Even after adjusting for age, sex, marital status, education level, diagnosis, NIHSS score on admission, comorbidities, disability at 5 years, and stroke recurrence within 5 years, multivariable ordinal logistic regression revealed that persistent depression at the 1-year follow-up (odds ratio [OR]: 0.48; 95% confidence interval [CI]: 0.29–0.81) and disability at the 5-year follow-up (OR: 0.34; 95% CI: 0.23–0.49) were both independently associated with poor MCS scores at the 5-year follow-up. The variables associated with low PCS scores at the 5-year follow-up were as follows: age (OR: 0.97; 95% CI: 0.96–0.99), high NIHSS score at admission (OR: 0.94; 95% CI: 0.90–0.98), disability at the 5-year follow-up (OR: 0.19; 95% CI: 0.13–0.27), and stroke recurrence at the 5-year follow-up (OR: 0.53; 95% CI: 0.34–0.85).
Table 3.
Risk factors associated with QoL among the patients included in the multivariable ordinal logistic regression.
Discussion
This longitudinal study of a post-stroke cohort highlighted persistent depression as a predictor of poor QoL in stroke patients at 5 years following the stroke event regardless of stroke sub-type. However, we found that the adverse effects of persistent depression manifested as lower MCS scores and remained significant after adjustments for relevant covariates. Furthermore, this study also showed that old age, high NIHSS score on admission, stroke recurrence within 5 years, and disability at the 5-year follow-up could predict poor PCS scores at the 5-year follow-up. These results are consistent with those of previous studies.[5,11,25–27]
Previous studies have observed that the baseline characteristics of patients with stroke are associated with the subsequent development of depression symptoms[28]: for example, female stroke survivors are reportedly more likely to be dead or dependent at 12 months following stroke onset,[29] and high baseline NIHSS scores are associated with an increased risk of neurological and medical complications.[30] Some authors have postulated that such characteristics at baseline might, therefore, predict poor outcomes of patients following stroke.
To the best of our knowledge, this study is the first nationwide longitudinal multi-center prospective cohort study to study the effect of the time course of PSD on the QoL of stroke survivors. PSD is a long-term problem that can occur in the sub-acute and acute hospitalization phases as well as in later stages.[31] While previous research has indicated a link between persistent depression and a high risk of poor prognosis and that recovery from depression after stroke might reduce the negative impact of the disease on QoL,[10,32–34] only three longitudinal studies have thus far reported that depression in the acute and sub-acute phases independently predicts poor QoL among stroke patients. Of these investigations, two have reported that PSD was independently associated with poor QoL at 1 year,[32,35] while one reported that PSD at 3 months could predict poor QoL at 5 years after stroke.[36]
While some investigations have reported that most cases of PSD recover spontaneously within a few months without any treatment,[17,37] others have reported that PSD might remain persistent in some cases.[11,33,38] In the present study, 10.0% (80/801) of stroke survivors exhibited persistent depression, and this result is consistent with a previous study,[39] which reported 9.2% of stroke survivors had persistent depression in the 1-year follow-up.
In agreement with our study, a previous investigation found that psychiatric symptoms affected MCS scores, while neurological conditions influenced PCS scores[40]; specifically, the investigators found that persistent depression could predict low MCS scores but could not predict long-term PCS scores. However, several cross-sectional studies have reported that PSD adversely affects both the physical and psychological dimensions of QoL.[5,8] This discrepancy in findings may indicate that patterns of MCS and PCS differ among various stroke conditions: for example, in cross-sectional studies, depression symptoms coexisted with neurological impairment, which may have impeded the rehabilitation of physical function in stroke patients; and while depression may limit gait recovery after stroke, poor physical health may negatively affect the mental dimensions of QoL in stroke patients.
This study is subject to several limitations. First, due to the absence of certain assessment scales, patients with aphasia who were unable to complete the self-rating scales were excluded; reliably measuring depression in these patients was thought to have been overly challenging.[41] Second, mood was continuously assessed only in the first year but not thereafter. Third, although we performed a comparison between the baseline characteristics of the included patients and those who did not complete the 5-year follow-up, and did not find significant difference, however, no comparison has been made between the baseline characteristics of the patients lost at 1-year follow-up and those of the included patients.
In conclusion, this longitudinal study showed that persistent depression at the 1-year follow-up could independently predict poor MCS scores at the 5-year follow-up. Other variables, such as old age, NIHSS score at admission, and recurrence of PSD during the 5-year follow-up predicted poor PCS scores at the 5-year follow-up. Disability at the 5-year follow-up was associated with low MCS and PCS scores.
Funding
This work was supported by grants from the National Key Research & Development Program of China (No. 2016YFC1307200), Beijing Brain Research (No. Z161100000216131), and Beijing Municipal Science & Technology Commission (No. Z151100004015127).
Conflicts of interest
None.
Footnotes
How to cite this article: Li LJ, Yao XM, Guan BY, Chen Q, Zhang N, Wang CX. Persistent depression is a predictor of quality of life in stroke survivors: results from a 5-year follow-up study of a Chinese cohort. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000400
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics–2012 update: a report from the American Heart Association. Circulation 2012; 125:e2–e220. doi: 10.1161/CIR.0b013e31825e74db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feigin VL, Krishnamurthi RV, Parmar P, Norrving B, Mensah GA, Bennett DA, et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990-2013: the GBD 2013 study. Neuroepidemiology 2015; 45:161–176. doi: 10.1159/000441085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kouwenhoven SE, Kirkevold M, Engedal K, Kim HS. Depression in acute stroke: prevalence, dominant symptoms and associated factors. A systematic literature review. Disabil Rehabil 2011; 33:539–556. doi: 10.3109/09638288.2010.505997. [DOI] [PubMed] [Google Scholar]
- 4.Choi-Kwon S, Choi JM, Kwon SU, Kang DW, Kim JS. Factors that affect the quality of life at 3 years post-stroke. J Clin Neurol (Seoul, Korea) 2006; 2:34–41. doi: 10.3988/jcn.2006.2.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ellis C, Grubaugh AL, Egede LE. Factors associated with SF-12 physical and mental health quality of life scores in adults with stroke. J Stroke Cerebrovasc Dis 2013; 22:309–317. doi: 10.1016/j.jstrokecerebrovasdis.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Christensen MC, Mayer SA, Ferran JM, Kissela B. Depressed mood after intracerebral hemorrhage: the FAST trial. Cerebrovasc Dis (Basel, Switzerland) 2009; 27:353–360. doi: 10.1159/000202012. [DOI] [PubMed] [Google Scholar]
- 7.Paolucci S, Gandolfo C, Provinciali L, Torta R, Toso V. The Italian multicenter observational study on post-stroke depression (DESTRO). J Neurol 2006; 253:556–562. doi: 10.1007/s00415-006-0058-6. [DOI] [PubMed] [Google Scholar]
- 8.Pan JH, Song XY, Lee SY, Kwok T. Longitudinal analysis of quality of life for stroke survivors using latent curve models. Stroke 2008; 39:2795–2802. doi: 10.1161/STROKEAHA.108.515460. [DOI] [PubMed] [Google Scholar]
- 9.Das J, Rajanikant GK. Post stroke depression: the sequelae of cerebral stroke. Neurosci Biobehav Rev 2018; 90:104–114. doi: 10.1016/j.neubiorev.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 10.Zhang N, Wang CX, Wang AX, Bai Y, Zhou Y, Wang YL, et al. Time course of depression and one-year prognosis of patients with stroke in mainland China. CNS Neurosci Ther 2012; 18:475–841. doi: 10.1111/j.1755-5949.2012.00312.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oni OD, Olagunju AT, Olisah VO, Aina OF, Ojini FI. Post-stroke depression: prevalence, associated factors and impact on quality of life among outpatients in a Nigerian hospital. S Afr J Psychiatr 2018; 24:1058.doi: 10.4102/sajpsychiatry.v24i0.1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Whyte EM, Mulsant BH, Vanderbilt J, Dodge HH, Ganguli M. Depression after stroke: a prospective epidemiological study. J Am Geriatr Soc 2004; 52:774–778. doi: 10.1111/j.1532-5415.2004.52217.x. [DOI] [PubMed] [Google Scholar]
- 13.Kunitz SC, Gross CR, Heyman A, Kase CS, Mohr JP, Price TR, et al. The pilot stroke data bank: definition, design, and data. Stroke 1984; 15:740–746. doi: 10.1161/01.STR.15.4.740Stroke. [DOI] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th ed., Text Revision). 2000; Washington, DC:American Psychiatric Association, doi: 10.1016/B978-1-4377-2242-0.00016-X. [Google Scholar]
- 15.Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, et al. The composite international diagnostic interview. An epidemiologic Instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Arch Gen Psychiatry 1988; 45:1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- 16.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998; 59 (Suppl 20):22–33. doi: 10.1016/s0924-9338(97)83297-x. [PubMed] [Google Scholar]
- 17.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960; 23:56–62. doi: 10.1007/978-3-642-70486-4_14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Folstein MF, Maiberger R, McHugh PR. Mood disorder as a specific complication of stroke. J Neurol Neurosurg Psychiatry 1977; 40:1018–1020. doi: 10.1136/jnnp.40.10.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12:189–198. doi: 10.1002/(SICI)1099-1166(199805)13:53.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 21.Bloch RF. Interobserver agreement for the assessment of handicap in stroke patients. Stroke 1988; 19:1448.doi: 10.1161/01.STR.19.5.604. [DOI] [PubMed] [Google Scholar]
- 22.Uyttenboogaart M, Stewart RE, Vroomen PC, De Keyser J, Luijckx GJ. Optimizing cutoff scores for the Barthel index and the modified Rankin scale for defining outcome in acute stroke trials. Stroke 2005; 36:1984–1987. doi: 10.1161/01.STR.0000177872.87960.61. [DOI] [PubMed] [Google Scholar]
- 23.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Bour A, Rasquin S, Aben I, Boreas A, Limburg M, Verhey F. A one-year follow-up study into the course of depression after stroke. J Nutr Health Aging 2010; 14:488–493. doi: 10.1007/s12603-010-0033-x. [DOI] [PubMed] [Google Scholar]
- 25.Niemi ML, Laaksonen R, Kotila M, Waltimo O. Quality of life 4 years after stroke. Stroke 1988; 19:1101–1107. doi: 10.1161/01.STR.19.9.1101. [DOI] [PubMed] [Google Scholar]
- 26.Rudberg AS, Berge E, Gustavsson A, Nasman P, Lundstrom E. Long-term health-related quality of life, survival and costs by different levels of functional outcome six months after stroke. Eur Stroke J 2018; 3:157–164. doi: 10.1177/2396987317753444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Delcourt C, Hackett M, Wu Y, Huang Y, Wang J, Heeley E, et al. Determinants of quality of life after stroke in China: the China QUEST (quality evaluation of stroke care and treatment) study. Stroke 2011; 42:433–438. doi: 10.1161/STROKEAHA.110.596627. [DOI] [PubMed] [Google Scholar]
- 28.Park EY, Kim JH. An analysis of depressive symptoms in stroke survivors: verification of a moderating effect of demographic characteristics. BMC Psychiatry 2017; 17:132.doi: 10.1186/s12888-017-1292-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boone M, Chillon JM, Garcia PY, Canaple S, Lamy C, Godefroy O, et al. NIHSS and acute complications after anterior and posterior circulation strokes. Ther Clin Risk Manag 2012; 8:87–93. doi: 10.2147/TCRM.S28569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Geng C, Lin Y, Tang Q, Tang Y, Wang X, Zhou JS, et al. Sex differences in clinical characteristics and 1-year outcomes of young ischemic stroke patients in East China. Ther Clin Risk Manag 2019; 15:33–38. doi: 10.2147/TCRM.S182232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arwert HJ, Meesters JJL, Boiten J, Balk F, Wolterbeek R, Vliet Vlieland TPM. Post stroke depression, a long term problem for stroke survivors. Am J Phys Med Rehabil 2018; 97:565–571. doi: 10.1097/PHM.0000000000000918. [DOI] [PubMed] [Google Scholar]
- 32.Shi YZ, Xiang YT, Yang Y, Zhang N, Wang S, Ungvari GS, et al. Depression after minor stroke: the association with disability and quality of life–a 1-year follow-up study. Int J Geriatr Psychiatry 2016; 31:421–427. doi: 10.1002/gps.4353. [DOI] [PubMed] [Google Scholar]
- 33.Berg A, Palomaki H, Lehtihalmes M, Lonnqvist J, Kaste M. Poststroke depression: an 18-month follow-up. Stroke 2003; 34:138–143. doi: 10.1161/01.STR.0000048149.84268.07. [DOI] [PubMed] [Google Scholar]
- 34.Dabrowska-Bender M, Milewska M, Golabek A, Duda-Zalewska A, Staniszewska A. The impact of ischemic cerebral stroke on the quality of life of patients based on clinical, social, and psychoemotional factors. J Stroke Cerebrovasc Dis 2017; 26:101–107. doi: 10.1016/j.jstrokecerebrovasdis.2016.08.036. [DOI] [PubMed] [Google Scholar]
- 35.Kim ES, Kim JW, Kang HJ, Bae KY, Kim SW, Kim JT, et al. Longitudinal impact of depression on quality of life in stroke patients. Psychiatry Investig 2018; 15:141–146. doi: 10.30773/pi.2017.10.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ayerbe L, Ayis S, Crichton S, Wolfe CD, Rudd AG. The long-term outcomes of depression up to 10 years after stroke; the South London Stroke Register. J Neurol Neurosurg Psychiatry 2014; 85:514–521. doi: 10.1136/jnnp-2013-306448. [DOI] [PubMed] [Google Scholar]
- 37.Hackett ML, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke 2005; 36:1330–1340. doi: 10.1161/01.STR.0000165928.19135.35. [DOI] [PubMed] [Google Scholar]
- 38.Astrom M, Adolfsson R, Asplund K. Major depression in stroke patients. A 3-year longitudinal study. Stroke 1993; 24:976–982. doi: 10.1161/01.STR.24.7.976. [DOI] [PubMed] [Google Scholar]
- 39.El Husseini N, Goldstein LB, Peterson ED, Zhao X, Olson DM, Williams JW, et al. Depression status is associated with functional decline over 1-year following acute stroke. J Stroke Cerebrovasc Dis 2017; 26:1393–1399. doi: 10.1016/j.jstrokecerebrovasdis.2017.03.026. [DOI] [PubMed] [Google Scholar]
- 40.Prisnie JC, Sajobi TT, Wang M, Patten SB, Fiest KM, Bulloch AGM, et al. Effects of depression and anxiety on quality of life in five common neurological disorders. Gen Hosp Psychiatry 2018; 52:58–63. doi: 10.1016/j.genhosppsych.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 41.Kauhanen ML, Korpelainen JT, Hiltunen P, Maatta R, Mononen H, Brusin E, et al. Aphasia, depression, and non-verbal cognitive impairment in ischaemic stroke. Cerebrovascis (Basel, Switzerland) 2000; 10:455–461. doi: 10.1159/000016107. [DOI] [PubMed] [Google Scholar]


