Introduction
Improving quality is about making health and social care safe, effective, person-centred, timely, efficient and equitable.1 Quality management is a key component of any high performing healthcare system.2 A well-known and popular quality management model is the Juran Trilogy: quality planning; quality control; quality improvement (QI).3 A recent 90-day process by Healthcare Improvement Scotland (HIS) on Quality Management Systems concluded that the current approach to quality management in Scotland is ‘out of balance’, with a ‘lack of effective quality planning’.4 This review aims to help both management and improvement teams to understand the specific components of quality planning, identified through improvement work in a Scottish context and supported by an appraisal of current literature.
Defining quality planning
Joseph Juran famously described quality planning within manufacturing as “a systematic process for developing services and processes that ensure customer needs are met”.5 He described a six-step process that has been adapted within healthcare over the last 30 years, leading to improved patient experience through a better understanding of the unmet needs of service-users.5 In addition to refinement of current processes to reduce duplication or waste, this concept has been expanded to include the development of novel services and delivery models.6 Quality planning can and does occur at a variety of levels within a healthcare system: macro or organisational level planning at senior management level; meso or group/service level planning for locality based improvement plans; and micro or clinical team level targeting specific services or patient groups.
Identifying key components
In order to identify the key components of successful quality planning, a structured, mixed methods process was undertaken. First, a series of interviews and focus groups were undertaken with individuals involved in successful local QI projects. In total, 16 people participated in eight interviews and one focus group: eight hospital-based clinicians, two primary care clinicians, two project managers, two quality directorate team members and two service managers. All interviews were conducted between 12 July and 31 August 2018 and lasted between 42 and 61 min. With appropriate consent, interviews were audio-recorded, transcribed verbatim and anonymised. Original recordings were retained on a password-protected computer for the period of analysis and subsequently deleted.
Inductive thematic analysis of the transcribed interviews and focus group led to the identification of five key themes: culture and leadership for improvement; engaging and empowering staff; forming collaborations and networks; building improvement capacity and capability; spreading and sustaining change. These factors then formed the basis of a subsequent narrative review of the literature. Using the five components identified from the interviews and focus group as Medical Subject Headings and/or key search terms, equivalent searches were carried out in three databases: MEDLINE, Embase (Exerpta Medica) and Google Scholar. Reference lists of pertinent articles or reports were hand searched for other relevant material. The five key components of quality planning are considered in detail below in relation to maximisation of impact, defined in this context as a marked effect or influence on quality of care in a meaningful and sustained way. The five components are each described in relation to current literature and illustrated by a practical example from our local context. Quotes within the examples are taken from the interview and focus group transcriptions, as described above.
Culture and leadership for improvement
QI leadership involves the creation of a shared vision (shared between frontline teams and managers/leaders), aligning improvement activities with that vision, and nurturing a culture that supports and sustains improvement.7 Culture or ‘the way we do things around here’ has a major influence on the function and outcomes of organisations.8 Culture is primarily the product of three main influences situated within a set of overarching values: the behaviour of leaders; the adopted systems and processes (such as hiring and rewarding); and the practices of groups and individuals.9 Different settings and services within a health and social care environment will have their own set of shared behaviours, values and beliefs. Understanding these at the quality planning stage can help identify barriers and enablers to the initiation and spread of improvement activity.
The promotion of innovative thinking and novel solutions requires specific cultural elements as described by the King’s Fund: inspiring vision and strategy; positive inclusion and participation; enthusiastic team and cross-boundary working; and support and autonomy.10 Each of these elements are promoted by collective and compassionate leadership that ensures staff are supported to deliver safe, effective and empathetic care. Furthermore, the increasing emphasis on co-production (collaboration between service providers and service users) of health and social care services requires leaders to develop the specific skills required to recruit and support service users to undertake such roles.
Practical example 1: Collective leadership.
When quality planning work began within NHS Lothian mental health services, there was a recognition that it needed to involve ‘harnessing people’s natural instincts to want to use their experience, their intellect and their desire to improve patients’ lives’ and somehow translate that enthusiasm into projects that ‘grow it into something that’s across the whole service’. There was a desire from those in leadership roles within mental health to ensure that they were ‘capturing the ideas of the people who are actually working with the patients about what is needed’. This inclusive, collaborative approach has permeated all stages of quality planning within mental health services. In the initial stages of the programme, the clinical lead and project manager spent time collating existing projects and discussing ideas with the individuals already involved in improvement work to ‘make sure they feel part of the programme’. The 1-year plan that evolved was the result of careful consideration of the needs of the service, the views of stakeholders and scrutiny of other organisations’ quality plans. But the team in mental health are the first to admit that it also involved a few ‘educated guesses’ and ‘an expectation that we weren’t going to get it right first time’. The subsequent 3-year quality plan built on the learning from the first year, and involved much more structured engagement with patients, carers and staff, to ensure that it reflected the views of all stakeholders.
While the importance of culture in quality planning is widely recognised, there is limited utilisation of the tools available for measuring ‘quality climate’ or readiness for QI activity. The literature includes a vast number of organisational culture survey tools that are used within the public and private sectors.11 Most of the tools measure dimensions such as leadership, teamwork, organisational structure, resources and communication networks. However, many of them are intensive, cumbersome and somewhat impractical in most healthcare settings. The Culture of Care Barometer, developed in 2014 following the report into the failings at Mid Staffordshire Hospital12 is a tool specifically designed to measure the culture of care and compassion within an organisation.13 The barometer gauges performance in four factors: Trust (or Board) level values and culture; team level support and management; support and respect between colleagues; constraints in undertaking the job. In the pilot studies, the Barometer was found to add depth and richness to the feedback received in staff surveys, allowing exploration of the feelings of staff at all levels to promote dialogue and change.13
Engaging and empowering staff
Staff engagement is an essential ingredient of sustainable QI.14 When staff are engaged it infuses everything they do with purpose, energy and enthusiasm. It is therefore vital that staff engagement is considered at the quality planning stage. As discussed earlier in this review, having an engaged, enthusiastic, compassionate, transparent and collaborative leadership team at senior management level is a necessary precondition to achieving staff engagement. Successful leaders are those who listen to truly understand what matters, adopt an inclusive grassroots approach to quality, give staff a voice, and empower them to try new and innovative ideas in a safe environment.15
A key component of empowerment in the quality planning stage is allowing people to find an ‘inner connection’, a link between what matters to them and what matters to the organisation.16 This approach parallels the well-known ‘What matters to you?’ campaign that encourages clinicians to explore the important issues in their patients’ lives, thereby driving deep personal engagement and genuine partnership. Storytelling can be a powerful tool to captivate interest as it enables articulation of emotional aspects alongside the factual content, allowing expression of tacit knowledge.16 Staff may be sceptical of QI initiatives, particularly in the planning stages.17 This may be because they confuse improvement with assurance, which is viewed as a punitive and judgmental process when externally imposed targets are not met. It is important to dispel this myth from the outset and to create an inspiring, bottom-up, shared vision that is truly meaningful to all staff. This involves exploring their intrinsic motivations, asking and listening to what matters, and encouraging innovative and creative change ideas.17 Effective questions can stimulate, guide and empower employees to think critically about the system and processes in which they work.18 Locally we have developed a series of thought-provoking questions to help stimulate conversations and ideas, outlined in box 1.
Box 1. What are your improvement opportunities? A nine-question approach.
Does the problem keep people awake at night?
Does this problem or issue occur commonly?
Does the problem arise from a chaotic system?
Can your problem be improved?
What has stopped you improving this problem or issue?
Is the service or process undergoing any change?
Does this problem upset people?
Does the problem lead to avoidable costs?
Can your problem be measured?
Practical example 2: Fostering engagement by aligning priorities.
The introduction of quality improvement (QI) into primary care in NHS Lothian has, at times, felt like ‘something that one GP was interested in, and tries to drag everybody else along’. Most general practitioners (GPs) felt that their workload prevented them from dedicating any time to quality planning and that it was an additional burden that should be shouldered by those with dedicated time in their job plans. In a canny move to align improvement work with the priorities of individuals, one of the first projects undertaken by the East Lothian Cluster Quality Lead centred on workload reduction. The aim of the project was to ‘make our systems more efficient and show ways of creating more time in the working day, then people’s creativity would open up a wee bit and perhaps feel able to then engage with changing things and making things better and feeling enthusiastic about it’. The dual effect has been to reduce the administrative burden on GPs, thereby releasing a small amount of time, as well as promote enthusiasm and buy-in to the concept of QI more generally.
Forming collaborations and networks
A key component of quality planning is the development of collaborations and networks to foster and support QI activity.19 The Health Foundation defines a network as “a cooperative structure where interconnected groups or individuals coalesce around a shared purpose and where members act as peers on the basis of reciprocity and exchange, based on trust, respect and mutuality”.20 It delineates the five core features of effective QI networks as: critical mass; common purpose; collective intelligence; cooperative structure; community building.20 The features are interdependent, collectively enabling a network to support service delivery while encouraging learning and change.
QI collaboratives exist within many networks, whereby select members of the network work together to rapidly achieve improvement in a topic of interest, with the aim of spreading the learning to others through the network.21 The Institute of Healthcare Improvement introduced the concept of the ‘Breakthrough Series Collaborative’ in 1995, a way of helping healthcare organisations to close the gap between improvement science and practical implementation, through learning from each other and recognised experts.22 Such collaborations can promote dynamic improvement strategies that translate into dramatic results, with rapid dissemination of successful change ideas. Similarly, communities of practice, classically defined as groups of people who share the same concern or passion, are growing in popularity in the National Health Service, with local partner organisations working together to plan, design and deliver more integrated services that better meet the needs of the population. Such communities can exist online, with the Health Foundation’s Q community consisting of dozens of online groups that interested individuals can join to share and collaborate, all motivated by the desire to improve health and care quality across the UK.
Networks can also be a valuable resource for benchmarking performance against internal and external departments or organisations.23 They provide a platform to learn from organisations achieving excellence, and motivation to continually improve performance. Juran introduced the concept of benchmarking in his 1964 book ‘Managerial Breakthrough’ when he asked the question “What is that organisation doing that gets results so much better than ours?”24 Asking such questions can motivate teams to reflect on their performance, learn from others and consider adopting external solutions.16
Practical example 3: The Newborn Care Collaborative.
The Newborn Care Collaborative (NCC) was conceived in 2013 and is a locally developed network consisting of 10 teams, each involving between six and 20 staff members from a variety of professional groups. Each team focuses on a particular topic and asks questions, extracts and analyses data, implements tests of change, and assesses improvement related to their area of interest. The growing number of individuals trained in quality improvement (QI) within the unit are spread between the groups to provide informal ‘just in time’ coaching to the rest of the group. Each month the groups take turns to present their run charts and achievements on a board within the unit and at departmental meetings to allow ideas to spread and achievements to be celebrated. Temporary staff members, such as junior doctors on 4-month or 6-month rotations, are asked to select a group to join and are expected to either involve themselves with an ongoing project or, if desired, initiate a new QI project. Parents of ex-patients, pharmacists, social workers, domestic staff and microbiology are all involved, ensuring that the NCC is a truly collaborative network of individuals dedicated to improving care within the unit. Everyone within the collaborative is involved in discussing unit priorities and creating the 2-year strategic plan.
Building improvement capacity and capability
A key part of quality planning, improvement capability has two dimensions: individual staff member capability and organisational capability.25 The totality of this review covers the specific capabilities required in the wider organisational context for improvement that is, culture, leadership, strategy, stakeholder and staff engagement, collaboration and spread. This section deals specifically with individual capability—the extent to which individuals are able to develop and deploy the skills, tools and knowledge necessary to improve the quality and safety of the care they provide. Research suggests that a lack of these skills among individual clinicians and managers is a barrier to improving quality in health and social care.26
At the quality planning stage, improvement teams should consider the skills that already exist within the service, so that they can make full use of the clinicians and teams with existing QI and patient safety experience. Departments with little improvement expertise or experience need to consider use of external resources to help them up-skill their staff and teams. While this sounds costly, local work has shown that it is possible to set up an effective programme for relatively modest costs. Delivery of in-house training or making use of free or low-cost external resources can help to achieve this. One of the main challenges, however, is time for staff to attend training sessions; time for trainers who lack dedicated improvement activity in their job plans to be released from their day-to-day clinical responsibilities; and time for those with dedicated activity to keep up with training demands.27 28
Regular evaluation of capability is necessary to ensure it is continuing to meet the needs of the workforce, the department and the organisation. It will evolve over time as the capabilities of teams grow and a common language around improvement begins to emerge.
Practical example 4: Building capability.
The large number of general practitioners (GPs) within NHS Lothian, along with the pressures of clinical work, means that attendance at Quality Academy courses is unrealistic for the vast majority. To build capability and foster a ‘whole-team’ approach, certain clusters of primary care practices within NHS Lothian have therefore utilised the expertise of the quality team based at NHS Lothian’s headquarters, Waverley Gate. The team has been able to provide training in quality improvement methodology and support to plan and develop new projects. The training sessions have included receptionists, administrative staff, practice managers, nurses and GPs in a staggered format to allow normal service to continue within the practices. The NHS Lothian practices have also utilised external resources, many of which are freely available, such as the NHS School for Change Agents (http://horizonsnhs.com/school/).
Spreading and sustaining change
Spreading and sustaining change is an oft-neglected aspect of quality planning.29 Consequently, across the UK, a third of healthcare improvement projects never spread beyond their original unit, a further third are embedded within their own unit and spread across an organisation, and a final third are spread across their own and other similar organisations.30 This statistic emphasises the importance of considering a strategy for spread and sustainability at an early stage.
Spread has been defined as “when best practice is disseminated consistently and reliably across a whole system and involves the implementation of proven interventions in each applicable care setting”.31 Likewise sustainability is “when new ways of working and improved outcomes become the norm”.30 In other words, it is when an improvement has become an integrated and the mainstream way of working withstanding challenge and variation over time, through a process of continuous improvement.32
The two widely recognised approaches to spread are dissemination and diffusion. Dissemination is the planned, formalised spread that occurs through rigid, vertical hierarchies. Diffusion is informal, peer-mediated organic flow often through word of mouth or social networks. In reality, a combination of these approaches is necessary to support spread throughout and beyond a large health or social care organisation.33 34 Planning for spread involves defining target audiences, agreeing on key messages for each audience, defining methods or strategies to reach each target audience, and a measurement plan to monitor and evaluate success. The concept of social diffusion helps to define the target audience: Once a new idea or behaviour has been adopted by 15%–20% of a particular population, it has the critical mass to spread without much additional scaffolding.35
Sustainability, or holding the gains, relies heavily on a supportive management structure and the development of structures to ‘foolproof’ change, including technology to support sustained implementation of the intervention.36 Robust and transparent feedback systems must generate performance data that is appropriately pitched for differing audiences, mapped using tools that allow shared analysis of systems. All staff should be aware of, and take pride in, the QI work being undertaken and the gains secured.36
Practical example 5: Spreading change.
Planning for sustainability and spread is often the aspect of quality planning that receives least attention. The neonatal service in NHS Lothian is working hard to embed the changes that they have made to their service by allowing nursing staff recognised ‘quality improvement (QI)’ time during their working day. This has required improving communication with the senior nurses who coordinate the staffing for each shift, and encouraging more dialogue between the senior medical and nursing teams. Innovative ideas and improvements are spread to other similar units via the Vermont Oxford Network, non-profit collaboration of healthcare professionals working within neonatal care with the aim of improving the quality and safety of medical care for newborn infants and their families through a coordinated program of research, education and QI projects.
Conclusion
Quality planning is an important pre-requisite of impactful QI. This review summarises key literature relating to the five important aspects of quality planning (as shown in figure 1), accompanied by practical examples to aid understanding. The quality planning process should involve defining priorities and utilising data-driven decision-making to clarify and understand the issues that are important to patients, service users and staff. In order for QI activity to have the best chance of improving care in a meaningful and sustained way, each of the five aspects discussed above must be considered at the planning stage.
Figure 1.
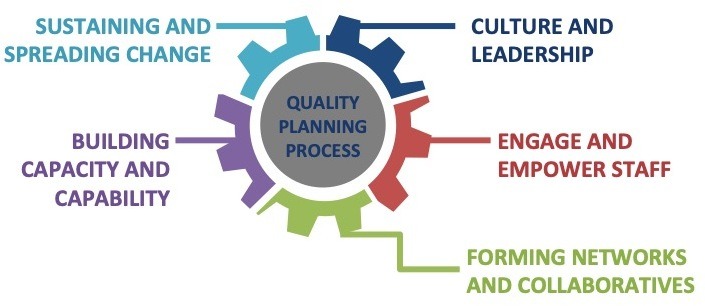
The five key aspects of quality planning.
Acknowledgments
The authors would like to acknowledge all those who were interviewed for this work who, as agreed, will remain anonymous.
Footnotes
Contributors: VRT, CAH and SW all contributed equally to the conception and formatting of this review. CAH collected the raw interview data included in the practical examples. VRT drafted the manuscript and CAH and SW contributed to editorial changes and reviewed the final manuscript prior to submission. All authors are responsible for the overall content of the manuscript as guarantors.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Committee on Quality of Health Care in America, Institute of Medicine Crossing the quality chasm: a new health system for the 21st century. Washington, DC, USA: National Academies Press, 2001: 360. [Google Scholar]
- 2.Healthcare Improvement Scotland Quality Management System: A 90-day innovation cycle - Second literature review, 2018. Available: http://www.healthcareimprovementscotland.org/idoc.ashx?docid=727c6c1b-71e7-4a7f-980d-d737722643ae&version=-1
- 3.Juran JM. Quality-control handbook. New York: McGraw-Hill, 1951. [Google Scholar]
- 4.Healthcare Improvement Scotland Quality management system: a 90-day innovation cycle, 2018. Available: http://www.healthcareimprovementscotland.org/previous_resources/policy_and_strategy/quality_management_system.aspx
- 5.Defeo JA. Juran’s quality handbook. 7th edn McGraw-Hill Education, 2016: 992. [Google Scholar]
- 6.Bhattacharyya O, Blumenthal D, Stoddard R, et al. . Redesigning care: adapting new improvement methods to achieve person-centred care. BMJ Qual Saf 2019;28:242–8. 10.1136/bmjqs-2018-008208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Swensen S, Pugh M. High-Impact leadership: improve care, improve the health of populations, and reduce costs, 2013. Available: http://www.ihi.org/resources/Pages/IHIWhitePapers/HighImpactLeadership.aspx
- 8.NHS Improvement Culture and leadership programme: concepts and evidence, 2016. Available: https://improvement.nhs.uk/documents/1546/01-NHS101-Evidence_030417.pdf
- 9.Daimler M. Why great employees leave “great cultures”. Harvard Business Review, 2018. [Google Scholar]
- 10.West M, Collins B. Caring to change: how compassionate leadership can stimulate innovation in health care, 2017. Available: https://www.kingsfund.org.uk/publications/caring-change
- 11.Jung T, Scott T, Davies HTO, et al. . Instruments for exploring organizational culture: a review of the literature. Public Adm Rev 2009;69:1087–96. 10.1111/j.1540-6210.2009.02066.x [DOI] [Google Scholar]
- 12.Report of the mid Staffordshire NHS Foundation trust public inquiry, 2013. Available: https://webarchive.nationalarchives.gov.uk/20150407084231/http://www.midstaffspublicinquiry.com/report
- 13.Rafferty AM, Philippou J, Fitzpatrick JM, et al. . Development and testing of the ‘Culture of Care Barometer’ (CoCB) in healthcare organisations: a mixed methods study. BMJ Open 2017;7:e016677 10.1136/bmjopen-2017-016677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The King’s Fund Leadership and engagement for improvement in the NHS: together we can, 2012. Available: https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/leadership-for-engagement-improvement-nhs-final-review2012.pdf
- 15.West M, West T. Leadership in healthcare: a review of the evidence. Health Management 2015;15:123–5. [Google Scholar]
- 16.Healthcare Improvement Scotland Ready to lead? developing the skills that drive change, 2014. Available: http://www.healthcareimprovementscotland.org/previous_resources/implementation_support/ready_to_lead.aspx
- 17.Gollop R, Whitby E, Buchanan D. Influencing sceptical staff to become supporters of service improvement: a qualitative study of doctors' and managers' views. Qual Saf Health Care 2004;13:108–14. 10.1136/qshc.2003.007450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coffey RJ, Jones L, Kowalkowski A, et al. . Asking effective questions: an important leadership role to support quality improvement. Jt Comm J Qual Improv 1993;19:454–64. 10.1016/S1070-3241(16)30026-8 [DOI] [PubMed] [Google Scholar]
- 19.The Health Foundation Leading networks in healthcare: Learning about what works - the theory and the practice, 2013. Available: https://www.health.org.uk/sites/default/files/LeadingNetworksInHealthcare.pdf
- 20.The Health Foundation Effective networks for improvement: developing and managing effective networks to support quality improvement in healthcare, 2014. Available: https://www.health.org.uk/sites/default/files/EffectiveNetworksForImprovement.pdf
- 21.The Health Foundation Improvement collaboratives in health care: evidence scan, 2014. Available: https://www.health.org.uk/publications/improvement-collaboratives-in-health-care
- 22.Institute for Healthcare Improvement The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. IHI Innovation Series white paper, 2003. Available: www.IHI.org
- 23.NHS Benchmarking Network East London NHS Foundation Trust, 2019. Available: https://www.nhsbenchmarking.nhs.uk
- 24.Juran JM. Managerial Breakthough. McGraw-Hill, 1964: 492. [Google Scholar]
- 25.The Health Foundation Building the foundations for improvement: how five UK trusts built quality improvement capability at scale within their organisations, 2015. Available: https://www.health.org.uk/publications/building-the-foundations-for-improvement
- 26.The Health Foundation Quality improvement training for healthcare professionals: evidence scan, 2012. Available: https://www.health.org.uk/publications/quality-improvement-training-for-healthcare-professionals
- 27.Zoutman DE, Ford BD. Quality improvement in hospitals: barriers and facilitators. Int J Health Care Qual Assur 2017;30:16–24. 10.1108/IJHCQA-12-2015-0144 [DOI] [PubMed] [Google Scholar]
- 28.The Health Foundation What’s getting in the way? Barriers to improvement in the NHS., 2015. Available: https://www.health.org.uk/sites/default/files/WhatsGettingInTheWayBarriersToImprovementInTheNHS.pdf
- 29.Scoville R, Little K. Sustaining improvement. IHI white paper. Available: www.ihi.org
- 30.Maher L, Gustafson D, Evans A. NHS sustainability: model and guide, 2010. Available: https://improvement.nhs.uk/resources/Sustainability-model-and-guide/
- 31.Counte MA, Meurer S. Issues in the assessment of continuous quality improvement implementation in health care organizations. Int J Qual Heallth 2001;13:197–207. 10.1093/intqhc/13.3.197 [DOI] [PubMed] [Google Scholar]
- 32.NHSScotland Quality Improvement Hub, Healthcare Improvement Scotland The spread and sustainability of quality improvement in healthcare, 2014. Available: http://www.qihub.scot.nhs.uk/media/596811/the%20spread%20and%20sustainability%20ofquality%20improvement%20in%20healthcare%20pdf%20.pdf
- 33.Healthcare Improvement Scotland Guide on spread and sustainability, 2013. Available: http://www.healthcareimprovementscotland.org/about_us/what_we_do/knowledge_management/knowledge_management_resources/spread_and_sustainability.aspx
- 34.Greenhalgh T, Robert G. How to spread good ideas: a systematic review of the literature on diffusion, dissemination and sustainability of innovations in health service delivery and organisation, 2004. Available: http://www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1201-038_V01.pdf
- 35.Rogers E. Diffusion of innovations. New York: Free Press, 2003. [Google Scholar]
- 36.Institute for Healthcare Improvement Protecting 5 million lives from harm. getting started kit: sustainability and spread. How-to guide, 2008. Available: https://qi.elft.nhs.uk/wp-content/uploads/2016/10/13_SpreadSustainabilityHowToGuidev141.pdf


