Abstract
Objective
To examine the changing temporal association between caesarean birth and neonatal death within the context of Ethiopia from 2000 to 2016.
Design
Secondary analysis of Ethiopian Demographic and Health Surveys.
Setting
All administrative regions of Ethiopia with surveys conducted in 2000, 2005, 2011 and 2016.
Participants
Women aged 15–49 years with a live birth during the 5 years preceding the survey.
Main outcome measures
We analysed the association between caesarean birth and neonatal death using log-Poisson regression models for each survey adjusted for potential confounders. We then applied the ‘Three Delays Model’ to 2016 survey to provide an interpretation of the association between caesarean birth and neonatal death in Ethiopia.
Results
The adjusted prevalence ratios (aPR) for neonatal death among neonates born via caesarean section versus vaginal birth increased over time, from 0.95 (95% CI: 0.29 to 3.19) in 2000 to 2.81 (95% CI: 1.11 to 7.13) in 2016. The association between caesarean birth and neonatal death was stronger among rural women (aPR (95% CI) 3.43 (1.22 to 9.67)) and among women from the lowest quintile of household wealth (aPR (95% CI) 7.01 (0.92 to 53.36)) in 2016. Aggregate-level analysis revealed that an increased caesarean section rates were correlated with a decreased proportion of neonatal deaths.
Conclusions
A naïve interpretation of the changing temporal association between caesarean birth and neonatal death from 2000 to 2016 is that caesarean section is increasingly associated with neonatal death. However, the changing temporal association reflects improvements in health service coverage and secular shifts in the characteristics of Ethiopian women undergoing caesarean section after complicated labour or severe foetal compromise.
Keywords: epidemiology, paediatrics, public health, maternal medicine
Strengths and limitations of this study.
This was the first study to examine the temporal association between caesarean birth and neonatal death within the context of Ethiopia from 2000 to 2016.
A number of analyses conducted after adjustment for potential confounders helped develop the possible scenarios to better understand the interpretation of the changing associations.
We have used additional supporting evidence from the 2016 Ethiopian Demographic and Health Survey data which allowed us interpret the association between caesarean birth and neonatal death in view of contextual factors in Ethiopia using the ‘Three Delays Model’.
Given the very low base rates of caesarean delivery in Ethiopia, the interpretation of our findings may not reflect the context of other low-income and middle-income countries.
Introduction
Globally, 2.6 million neonatal deaths occurred within the first 28 days after birth, which accounted for 46% of all under-five deaths in 2016.1 The majority of these deaths were from low-income and middle-income countries. According to the United Nations Interagency Group for Child Mortality Estimation, Southern Asia (39%) and sub-Saharan Africa (38%) comprised the top two regions with the highest proportion of newborn deaths, while five countries (India, Pakistan, Nigeria, the Democratic Republic of the Congo and Ethiopia) accounted for 50% of all newborn deaths.1 Evidence shows that, compared with mortality among children aged 1–59 months, neonatal mortality is decreasing more slowly.1 If the current trend continues, more low-income and middle-income countries will fail to achieve the Sustainable Development Goal target for neonatal mortality at least as low as 12 deaths per 1 000 live births.1 2
In contemporary obstetric practice, caesarean section remains an important intervention in preventing neonatal mortality and other adverse birth outcomes.3 However, caesarean section may be prone to misuse because of unequal access, social and cultural factors.4–6 In developing country settings, due to limited medical provisions and/or lack of skilled birth attendants, some women may not benefit from caesarean birth though they are medically eligible, while ineligible women may sometimes have increased access. In the last decades, caesarean section rates have been increasing in low-income, middle-income and high-income countries.7–9 The World Health Organization (WHO) suggests that ‘every effort should be made to provide caesarean sections to women in need, rather than striving to achieve a specific rate’.10
Previous studies conducted using aggregate-level and individual-level data have yielded inconsistent results about the association between caesarean birth and neonatal mortality. For instance, two ecological studies11 12 conducted using worldwide country-level data have found that caesarean birth was associated with lower neonatal mortality, while another two ecological studies13 14 showed no association between caesarean birth and neonatal mortality, where caesarean section rates were higher than 10%. Inconsistent results for the association between caesarean birth and neonatal mortality were also reported by different studies based on individual-level data conducted in Africa, Latin America, Asia and USA.15–20 For example, a large study conducted by Villar et al in 410 health facilities in 24 areas in eight Latin American countries found that, with cephalic presentation, both intrapartum and elective caesarean were associated with 1.66 (95% CI: 1.26 to 2.20) and 1.99 (95% CI: 1.51 to 2.63) times higher odds of neonatal mortality up to hospital discharge, respectively.16 However, another study based on WHO global survey completed in nine countries in Asia found that both prelabour (adjusted odds ratio (aOR) 0.2 (95% CI: 0.1 to 0.3)) and intrapartum caesarean sections (aOR 0.3, 95% CI: 0.2 to 0.4) were associated with improved perinatal outcomes following breech presentation.15
On the other hand, using both country-level and individual-level data collected for nationally representative Demographic and Health Surveys (DHS), Kyu et al found an increased risk for neonatal death associated with caesarean versus vaginal births in countries with low (<5%) and medium (5%–15%) caesarean section rates.21 However, factors associated with caesarean section that increase risk for neonatal death in countries with low and moderate caesarean section rates remain ill-defined. Previous studies are limited by either inconsistent results or lack the interpretation of findings by considering the contextual factors.11–21 In addition to the underlying indications for caesarean interventions like ‘fetal distress’, ‘cord prolapse’, ‘prolonged and obstructed labour’, ‘fetal mal-presentation’, ‘major antepartum haemorrhage’ and ‘placenta praevia’,22 23 several contextual factors such as unequal access, infrastructural and health workforce constraints could play a role in the association between caesarean section and neonatal death.
In low-income and middle-income countries, the DHS are the most representative and widely available high-quality data sources for studies related to maternal and child health. We use Ethiopian DHS data from 2000, 2005, 2011 and 2016 to examine the changing temporal association between caesarean birth and neonatal death. We then apply the ‘Three Delays Model’ developed by Thaddeus and Maine24 to facilitate the interpretation of the association between caesarean birth and neonatal death in Ethiopia using the 2016 data.
Methods
Study design and data samples
We used data from the Ethiopian DHS completed in 2000, 2005, 2011 and 2016. The Ethiopian DHS are nationally representative cross-sectional surveys conducted in nine regional states (Tigray, Affar, Amhara, Oromia, Somali, Benishangul-Gumuz, SNNPR, Gambela and Harari) and two city administrations (Addis Ababa and Dire Dawa). Each of the surveys involved a two-stage, stratified, clustered sampling design. The survey datasets are deidentified and made freely available online. Permission to use these data was granted by the DHS Program. The details about the methodology and standards for protecting the privacy of study participants in all DHS can be accessed online (http://www.dhsprogram.com/What-We-Do/methodology.cfm).
Exposure
The DHS questionnaire asks women about pregnancy, antenatal and delivery care for live births they have reported in the past 5 years. The data on caesarean section and other variables in the DHS were collected based on mothers’ self-report. For example, the self-reported data on caesarean section were collected by asking mothers a question that reads, ‘Was (NAME) delivered by caesarean section, that is, did they cut your belly open to take the baby out?’ in the 2016 survey. Stanton and colleagues25 in their study demonstrated that the DHS caesarean section rates, compared with facility-based records of caesarean section rates, are reliable for national and global monitoring in developing countries. For this study, the exposure group were infants delivered by caesarean section and unexposed group comprised infants born vaginally.
Outcome
Neonatal death includes infants who were born alive in the 5 years before each survey, but died within the first 28 days of life. The outcome variable, neonatal death, was measured from two variables (whether the child is alive and age at death (in days)).
Confounding
The following potential confounders were identified based on a priori subject-matter and expert knowledge. They included place of delivery (public, private, non-governmental organisation and home), type of residence (urban/rural), sex of child (male/female), size of baby at birth (very large, larger than average, average, smaller than average, very small and do not know), mother’s age at birth (in years), mother’s education (no education, primary, secondary and higher), birth order (1, 2–3 and 4+) and household wealth quintile (poorest, poorer, middle, richer and richest). The size of baby at birth was assessed based on mother’s perception (estimate) of baby size at birth. It has previously been shown that, in the absence of complete enumeration of birth weight, mother’s perception of baby size at birth can be used as a proxy to birth weight in nationally representative surveys.26 Mother’s age at birth was calculated as a difference (in years) between infant’s date of birth and mother’s date of birth. The DHS computes the wealth index for each survey based on household assets using principal components analyses27 and categorises households into wealth quintiles. These asset-based measures represent the wealth distribution relative to other households within the country. They are widely used and are consistent with comparisons to household expenditures and the measurement of inequalities in child mortality, education and healthcare use in low-income and middle-income countries.28
Statistical analysis
Missing information is uncommon in DHS because the data are collected by a trained interviewers at a face-to-face interview. All analyses (ie, Ethiopian DHS 2000, 2005, 2011 and 2016) were weighted to be nationally representative. As women may have had more than one births within the 5-year survey periods, we also accounted for both clustering of caesarean deliveries within women as well as the complex survey design during the data analyses using the unit of analysis (ie, children) study number and sample weights. We then conducted both individual-level and aggregate-level analyses. Our 2016 data analysis was also supplemented by an application of the ‘Three Delays Model’ to interpret the association between caesarean birth and neonatal death both empirically and theoretically. All analyses were conducted using STATA/SE V.15.1 (Stata Corporation).
Individual-level analysis
Associations between caesarean birth and neonatal death at individual-level were analysed using log-Poisson regression models using data from Ethiopian DHS conducted in 2000, 2005, 2011 and 2016. We calculated unadjusted and adjusted prevalence ratios (aPR) and their 95% CIs for each survey. We have then compared the strength of association between caesarean birth and neonatal death across all surveys analysed.
After noting the increasing association between caesarean birth and neonatal death over time, we conducted a series of analyses to explore what was during the change. We used the 2016 data because the association was more pronounced. We first restricted the analysis to participants living in regions with the highest caesarean section rates to examine whether the increased access to caesarean section affected the proportion of neonatal deaths. We then estimated the effect of caesarean birth on neonatal death in regions with low caesarean section rate (ranged: 0.4%–5.3%) or where access to caesarean section is limited, by excluding births in relatively high caesarean section rate regions—Addis Ababa (21.4%) and Harari (9.0%).29 Both low-level and high-level of caesarean use has risks exceeding the risks of spontaneous vaginal deliveries.15 30 It was demonstrated that low levels of caesarean are related to lack of access and can contribute to maternal and newborn deaths.21 31
Given the very large rural–urban differences in caesarean section rates in Ethiopia,29 32 we also conducted similar analyses separately for rural women. In addition, we evaluated the association by restricting the analyses to births from the lowest quintile of household wealth, births from the highest quintile of household wealth, and births in public health facilities separately. These alternative analyses were exploratory in nature and helped us understand contextual factors leading to inequalities in caesarean use that may occur not only due to inadequate access among the poorest women, but also due to overuse among the richest population subgroups.33 34 The subgroup analyses allowed us to explain how contextual factors such as unequal access, infrastructural and workforce constraints could play role in the association between caesarean section and neonatal death because these factors will result in delay in accessing emergency caesarean section, which is usually accessible at specialised health facilities.
The 2016 DHS included an additional question regarding ‘timing of decision to conduct caesarean section (ie, whether it was before or after the onset of labour pains)’. We used this variable as a proxy to the types of caesarean birth (indicative of intrapartum or prelabour caesarean section) and conducted analysis to examine the association between types of caesarean section and neonatal death. As this was confined only to 2016 data, we have provided the results in online supplementary table A1.
bmjopen-2018-027235supp001.pdf (476.6KB, pdf)
Aggregate-level analysis
Data on the caesarean section rates and proportion of neonatal deaths were disaggregated by urban–rural areas for each of the nine regional states and two city administrations in Ethiopia for each of the surveys completed in 2000, 2005, 2011 and 2016. However, the urban–rural stratification for Addis Ababa is only available for the 2005 survey. These results in a total of 85 data points (observations). In order to assess the correlation between caesarean section and neonatal death at the aggregate level, we conducted simple linear regression for overall surveys together and for individual surveys separately.
Application of the ‘Three Delays Model’
The ‘Three Delays Model’ is a conceptual framework developed by Thaddeus and Maine to examine factors contributing to maternal mortality with specific focus on those that affect the ‘interval between the onset of obstetric complication and its outcome’.24 The ‘Three Delays Model’ summarises the various factors that affect this interval into three phases of delay—delay in deciding to seek care (phase I delay); delay in identifying and reaching medical facility (phase II delay); and delay in receiving adequate and appropriate treatment (phase III delay). Some of the key factors that shape the model include status of women; distance from health facility; availability and cost of transportation; condition of roads; distribution of health facilities; shortage of supplies, equipment and skilled birth attendants and adequacy of referral system.24 The pictorial presentation of the ‘Three Delays Model’ is provided in online supplementary figures A1–A4.
As maternal and neonatal mortality share many risk factors, we adopted the ‘Three Delays Model’ as a framework to help interpret the association between caesarean birth and neonatal mortality within the context of Ethiopia using the 2016 survey because factors contributing to the ‘three delays’ aggravate the underlying medical indications for caesarean intervention that make neonatal death difficult to prevent. The 2016 survey was selected for interpretation of the association between caesarean birth and neonatal death using the ‘Three Delays Model’ because the association was more pronounced in the 2016 data. Previous studies conducted in India,35 Tanzania36 and Uganda37 have applied the ‘Three Delays Model’ to their analyses of perinatal deaths.
We have identified some contributing factors underlying the ‘Three Delays Model’ from the 2016 survey. For example, information regarding problems faced by women of reproductive age (15–49 years) in accessing healthcare to obtain medical advice or treatment for themselves when they are sick were gathered. It consisted of four questions: distance to health facility (big problem/not big problem); getting money for treatment (big problem/not big problem); getting permission to go for treatment (big problem/not big problem) and not wanting to go alone (big problem/not big problem). Furthermore, data on skilled assistance during delivery, and women’s socioeconomic and demographic status are also available in the DHS. This information can particularly be important to understand and address the barriers that women face in seeking care during pregnancy and delivery.32 We have, therefore, analysed the 2016 data to describe these factors empirically in the context of Ethiopia.
Patient and public involvement
This research was done without patient involvement in setting the research question or the outcome measures, and in the design and implementation of the study. No patients were asked to advise on interpretation or writing up of results. There are no plans to disseminate the results of this research to study participants or the relevant patient community.
Results
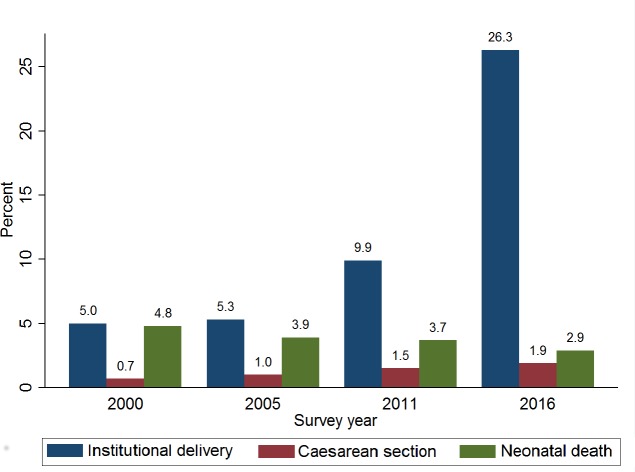
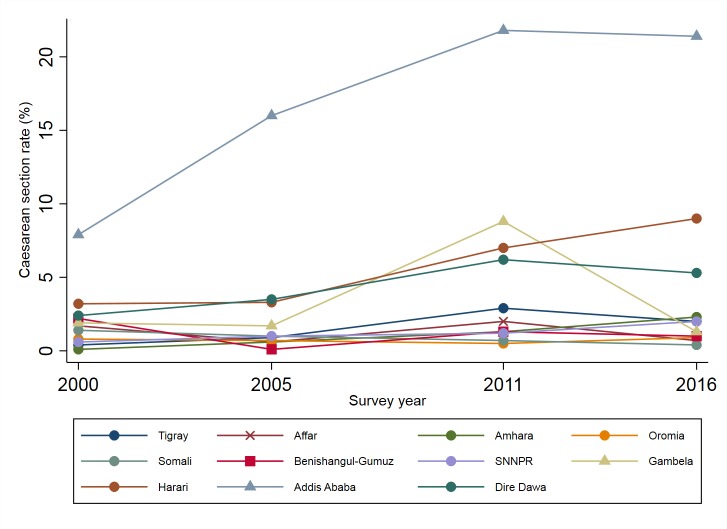
Table 1 shows the characteristics of mothers and children according to mode of delivery for each of the surveys conducted in 2000, 2005, 2011 and 2016. Across the four DHS waves, women who underwent caesarean delivery were more likely to live in urban areas, had a higher level of education and were from the richest quintile of household wealth. They were also more likely to have male children. Caesarean deliveries were more frequent in women in the age category of 20–29 years, and among infants who had either very large or larger than average size of baby at birth. Figure 1 shows that the proportion of institutional deliveries increased from 5.0% in 2000 to 26.3% in 2016, whereas the national caesarean section rate increased from 0.7% in 2000 to 1.9% in 2016. However, the rate of caesarean delivery in Ethiopia varied widely across administrative regions (figure 2). For instance, Addis Ababa had the highest (21.4%) rate, while Somali had the lowest (0.4%) in 2016. The national proportion of neonatal deaths decreased from 4.8% in 2000 to 2.9% in 2016 (figure 1), but the proportion varies among administrative regions of Ethiopia (online supplementary table A2).
Table 1.
Characteristics of the study participants according to the mode of delivery, Ethiopia DHS 2000, 2005, 2011 and 2016
| Mode of delivery | ||||||||
| DHS 2000 | DHS 2005 | DHS 2011 | DHS 2016 | |||||
| Caesarean (n=86) % |
Vaginal (n=12 174) % |
Caesarean (n=111) % |
Vaginal (n=11 052) % |
Caesarean (n=175) % |
Vaginal (n=11 697) % |
Caesarean (n=213) % |
Vaginal (n=10 810) % |
|
| Neonatal death | ||||||||
| Yes | 4.5 | 4.8 | 6.7 | 3.9 | 5.5 | 3.7 | 8.3 | 2.7 |
| No | 95.5 | 95.2 | 93.3 | 96.1 | 94.5 | 96.3 | 91.7 | 97.3 |
| Types of residence | ||||||||
| Urban | 76.2 | 9.9 | 68.8 | 6.7 | 70.9 | 12.0 | 60.4 | 10.1 |
| Rural | 23.8 | 90.1 | 31.2 | 93.3 | 29.1 | 88.0 | 39.6 | 89.9 |
| Region | ||||||||
| Tigray | 4.0 | 6.4 | 5.4 | 6.3 | 12.5 | 6.2 | 6.8 | 6.5 |
| Affar | 2.5 | 1.0 | 0.6 | 1.0 | 1.4 | 1.0 | 0.4 | 1.0 |
| Amhara | 3.7 | 26.3 | 15.2 | 23.6 | 19.4 | 22.4 | 22.1 | 18.7 |
| Oromia | 46.3 | 40.7 | 28.5 | 39.6 | 14.6 | 42.6 | 21.2 | 44.5 |
| Somali | 2.3 | 1.2 | 4.2 | 4.3 | 1.4 | 3.1 | 1.0 | 4.7 |
| Benishangul-Gumuz | 3.1 | 1.0 | 0.1 | 0.9 | 1.0 | 1.2 | 0.6 | 1.1 |
| SNNPR | 18.5 | 21.2 | 21.6 | 22.4 | 17.4 | 21.1 | 21.0 | 20.8 |
| Gambela | 0.6 | 0.2 | 0.5 | 0.3 | 2.0 | 0.3 | 0.2 | 0.2 |
| Harari | 0.9 | 0.2 | 0.7 | 0.2 | 1.2 | 0.2 | 1.1 | 0.2 |
| Addis Ababa | 16.9 | 1.4 | 22.1 | 1.2 | 27.6 | 1.5 | 24.5 | 1.8 |
| Dire Dawa | 1.1 | 0.3 | 1.2 | 0.3 | 1.4 | 0.3 | 1.2 | 0.4 |
| Mother’s age at birth | ||||||||
| <20 | 19.4 | 12.0 | 13.3 | 13.4 | 10.5 | 10.9 | 6.4 | 10.0 |
| 20–29 | 70.8 | 51.3 | 59.8 | 51.2 | 62.8 | 55.7 | 58.4 | 54.6 |
| 30–39 | 9.8 | 30.0 | 24.1 | 29.3 | 23.7 | 28.7 | 31.7 | 30.9 |
| 40–49 | 0.0 | 6.7 | 2.9 | 6.2 | 3.3 | 4.7 | 3.4 | 4.5 |
| Mother’s education | ||||||||
| No education | 15.7 | 82.5 | 30.1 | 79.7 | 19.9 | 70.0 | 22.8 | 66.9 |
| Primary | 21.8 | 13.0 | 14.5 | 16.6 | 44.7 | 26.8 | 35.1 | 26.6 |
| Secondary | 56.4 | 4.3 | 46.5 | 3.4 | 22.2 | 1.9 | 15.3 | 4.5 |
| Higher | 6.2 | 0.2 | 8.9 | 0.3 | 13.2 | 1.2 | 26.8 | 2.0 |
| Place of delivery* | ||||||||
| Public | 96.3 | 4.0 | 90.2 | 3.9 | 83.5 | 7.6 | 84.0 | 23.6 |
| Private | 1.3 | 0.1 | 5.9 | 0.3 | 13.6 | 0.8 | 13.7 | 0.9 |
| NGO | 2.4 | 0.2 | 3.8 | 0.1 | 3.0 | 0.2 | 2.4 | 0.2 |
| Home | 0.0 | 95.6 | 0.0 | 95.7 | 0.0 | 91.4 | 0.0 | 75.2 |
| Birth order | ||||||||
| 1 | 75.5 | 18.6 | 53.2 | 17.0 | 53.5 | 18.5 | 41.4 | 18.2 |
| 2 | 17.5 | 16.5 | 26.0 | 15.5 | 17.0 | 17.0 | 25.6 | 16.0 |
| 3 | 2.2 | 13.7 | 5.7 | 14.5 | 10.3 | 14.2 | 18.2 | 14.2 |
| 4 | 1.0 | 11.3 | 1.5 | 12.9 | 6.0 | 12.6 | 3.3 | 12.5 |
| 5 | 0.6 | 10.4 | 2.2 | 10.8 | 8.4 | 10.5 | 5.3 | 11.4 |
| 6+ | 3.2 | 29.5 | 11.4 | 29.4 | 4.7 | 27.2 | 6.3 | 27.6 |
| Sex of child | ||||||||
| Male | 61.8 | 51.2 | 51.3 | 51.3 | 57.2 | 51.9 | 54.0 | 51.9 |
| Female | 38.2 | 48.8 | 48.7 | 48.7 | 42.8 | 48.1 | 46.0 | 48.1 |
| Size of baby at birth† | ||||||||
| Very large | 9.8 | 5.3 | 30.7 | 22.3 | 25.8 | 19.2 | 26.5 | 17.6 |
| Larger than average | 32.0 | 25.4 | 11.4 | 9.5 | 11.7 | 12.7 | 16.0 | 13.8 |
| Average | 34.6 | 35.7 | 37.4 | 40.0 | 42.3 | 38.2 | 36.1 | 41.7 |
| Smaller than average | 19.7 | 27.5 | 9.4 | 7.3 | 4.9 | 8.7 | 7.0 | 10.1 |
| Very small | 3.7 | 5.9 | 9.5 | 20.6 | 14.8 | 20.6 | 12.7 | 16.0 |
| Do not know | 0.2 | 0.2 | 1.1 | 0.4 | 0.6 | 0.4 | 1.7 | 0.8 |
| Wealth quantile | ||||||||
| Poorest | 1.9 | 21.1 | 0.6 | 22.1 | 2.0 | 23.1 | 7.2 | 24.2 |
| Poorer | 4.9 | 21.0 | 5.9 | 21.3 | 8.4 | 22.6 | 12.2 | 23.1 |
| Middle | 4.1 | 22.0 | 3.9 | 22.5 | 9.0 | 20.7 | 10.8 | 20.9 |
| Richer | 6.1 | 20.5 | 9.7 | 20.0 | 6.5 | 19.3 | 9.3 | 18.3 |
| Richest | 83.0 | 15.5 | 79.9 | 14.2 | 74.1 | 14.2 | 60.4 | 13.5 |
n=weighted.
*Missing for 2000 (n = 9).
†Mother’s estimate of baby’s size at birth.
DHS, Demographic and Health Survey; NGO, Non-governmental Organisation.
Figure 1.
Trends in proportion of institutional deliveries, caesarean section and neonatal death in the 5 years before each of the surveys, Ethiopia DHS 2000, 2005, 2011 and 2016.
Figure 2.
Trends in caesarean section rates in the 5 years before each of the surveys according to the nine regional states and two city administrations, Ethiopia DHS 2000, 2005, 2011 and 2016.
Table 2 shows that the aPR for neonatal death associated with caesarean versus vaginal births in 2000 survey was 0.95 (95% CI: 0.29 to 3.19) while in 2005, it was 1.53 (95% CI: 0.52 to 4.50). In 2011, the aPR for neonatal death associated with caesarean versus vaginal births was 1.15 (95% CI: 0.45 to 2.93), while it was 2.81-fold higher risk of neonatal death (aPR, 2.81; 95% CI: 1.11 to 7.13) in 2016.
Table 2.
Crude and multivariable-adjusted prevalence ratios for neonatal death associated with caesarean versus vaginal delivery, Ethiopia DHS 2000, 2005, 2011 and 2016
| Prevalence ratio (95% CI) for neonatal death | |
| Ethiopia DHS 2000 | |
| Vaginal delivery | 1 (Ref.) |
| Caesarean delivery, crude (n=10 873) | 0.93 (0.38 to 2.30) |
| Caesarean delivery, model 1* (n=10 853) | 0.95 (0.29 to 3.19) |
| Ethiopia DHS 2005 | |
| Vaginal delivery | 1 (Ref.) |
| Caesarean delivery, crude (n=9 861) | 1.74 (0.67 to 4.51) |
| Caesarean delivery, model 1* (n=9 861) | 1.53 (0.52 to 4.50) |
| Ethiopia DHS 2011 | |
| Vaginal delivery | 1 (Ref.) |
| Caesarean delivery, crude (n=11 654) | 1.49 (0.62 to 3.61) |
| Caesarean delivery, model 1* (n=11 654) | 1.15 (0.45 to 2.93) |
| Ethiopia DHS 2016 | |
| Vaginal delivery | 1 (Ref.) |
| Caesarean delivery, crude (n=10 641) | 3.02 (1.37 to 6.66) |
| Caesarean delivery, model 1* (n=10 641) | 2.81 (1.11 to 7.13) |
*Adjusted for place of delivery, type of residence (urban/rural), sex of child, size of baby at birth, mother’s age at birth, mother’s education, birth order and household wealth.
DHS, Demographic and Health Surveys.
Table 3 summarises the findings of the subgroup analyses based on the 2016 data. When women living in urban settings—Addis Ababa (caesarean section rate (21.4%)) and Harari (9.0%)—were excluded from the analyses, the corresponding aPR for neonatal death was increased to 3.55 (95% CI: 1.31 to 8.56). Similarly, when we restricted the analyses to include only rural women, the prevalence ratio for neonatal death associated with caesarean versus vaginal births was found to be 3.43 (95% CI: 1.22 to 9.67). The respective risk of neonatal death increased to 7.01 (95% CI: 0.92 to 53.36) when the analysis was limited to women from the lowest quintile of household wealth.
Table 3.
Crude and multivariable-adjusted prevalence ratios for neonatal death associated with caesarean versus vaginal delivery, Ethiopia DHS 2016
| Prevalence ratio (95% CI) for neonatal death | |
| Main analysis | |
| Vaginal delivery | 1 (Ref.) |
| Caesarean delivery, crude (n=10 641) | 3.02 (1.37 to 6.66) |
| Caesarean delivery, model 1* (n=10 641) | 2.81 (1.11 to 7.13) |
| Subgroup analyses | |
| Restricted to Addis Ababa† (n=461) | 1.07 (0.20 to 5.73) |
| Excluded Addis Ababa and Harari* (n=9 575) | 3.35 (1.31 to 8.56) |
| Restricted to births in public facility* (n=3 023) | 2.78 (1.16 to 6.63) |
| Restricted to rural mothers† (n=8 636) | 3.43 (1.22 to 9.67) |
| Restricted to women from lowest quintile of household wealth‡ (n=3 958) | 7.01 (0.92 to 53.36) |
| Restricted to women from highest quintile of household wealth‡ (n=2 092) | 2.72 (0.55 to 13.38) |
*Adjusted for place of delivery, type of residence (urban/rural), sex of child, size of baby at birth, mother’s age at birth, mother’s education, birth order and household wealth.
†Adjusted for place of delivery, sex of child, size of baby at birth, mother’s age at birth, mother’s education, birth order and household wealth.
‡Adjusted for place of delivery, sex of child, size of baby at birth, mother’s age at birth, mother’s education and birth order.
When we restricted the analyses to Addis Ababa, the capital of Ethiopia, the relative risk for neonatal death associated with caesarean versus vaginal births was 1.07 (95% CI: 0.20 to 5.73). Moreover, when the analysis was confined to women from the highest quintile of the household wealth, the risk of neonatal death was 2.72 (95% CI: 0.55 to 13.38).
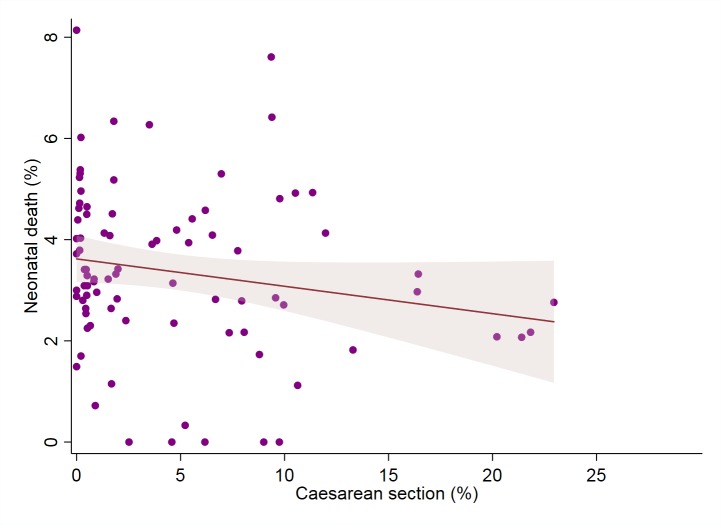
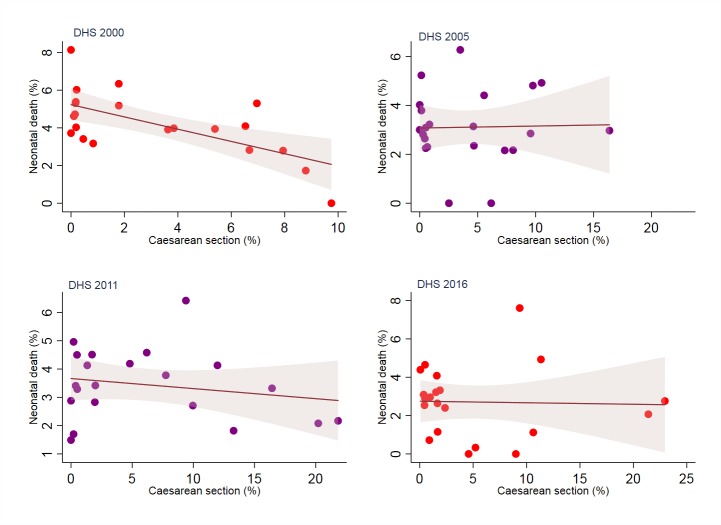
Finally, figure 3 shows that an increase in caesarean section rate is weakly correlated with a decrease in the proportion of neonatal deaths (correlation coefficient (r)=−0.1839) when aggregate-level data for all surveys together were analysed. However, the relationship between caesarean birth and neonatal death is variable when the analysis is restricted to each survey year separately (figure 4).
Figure 3.
The relationship between caesarean section rate and neonatal death in Ethiopia (2000 to 2016).
Figure 4.
The relationship between caesarean section rate and neonatal death by survey years.
Interpretation
The primary individual-level analyses showed that the aPR for neonatal death associated with caesarean versus vaginal births increased from 0.95 (95% CI: 0.29 to 3.19) in 2000 to 2.81 (95% CI: 1.11 to 7.13) in 2016. These findings suggest that the circumstances for foetuses born in 2000 survey were different from the foetuses in 2016. Our subgroup analyses using 2016 data suggest that the association between caesarean birth and neonatal death was stronger among rural women (aPR (95% CI) 3.43 (1.22 to 9.67)) and among women from the lowest quintile of household wealth (aPR (95% CI) 7.01 (0.92 to 53.36)), but not for births in areas with wider availability of caesarean such as Addis Ababa (aPR (95% CI) 1.07 (0.20 to 5.73)). The changing association between caesarean birth and neonatal death over time, and the stronger association observed among different subgroup analyses may be attributable to changes in the pattern of confounding by indication due to contextual factors such as unequal access, structural health-system deficiencies (insufficient equipment, supplies and drugs), infrastructural and health workforce constraints.
The national caesarean section and institutional delivery rates in Ethiopia are still low though increases in the past decade are notable. There is also substantial disparity in caesarean section rates, with very low rates in rural areas and among the poorest women,29 suggesting unequal access which may be as a consequence of a range of geographic, social and economic barriers. The low caesarean rates may also be due to lack of skilled birth attendants, and poor health infrastructure (eg, shortage of medical care institutions, deficiencies in surgical facilities, surgical and anaesthesia personnel and equipment, and blood transfusion capacity).38–40 For instance, in Ethiopia, there are only 820 obstetricians, 10 846 general practitioners, 996 emergency obstetric surgeons, 6 345 health officers, 41 009 nurses, 8 635 midwives, 233 anaesthesiologists and 33 320 health extension workers for the population of over 90 million in 2015.41 Similarly, there are only 3 547 functional health centres, 16 447 functional health posts and 189 functional hospitals in 2015.42
We know from previous research that inadequate access to timely caesarean section may result in perinatal asphyxia, uterine rupture, obstructed labour, and these can contribute to maternal and newborn deaths.43 Conversely, it was demonstrated that maternal and neonatal mortality due to obstetric complications can be prevented with timely access to caesarean section.43 44 Delay, therefore, emerges as relevant factor in worsening the underlying obstetric indications for caesarean intervention thereby contributing to neonatal death. Context-specific factors that delay access to caesarean section may have the capacity to make women with labour problems undergo caesarean section after severe complication of labour or severe foetal compromise. Therefore, our interpretation is that caesarean section conducted after severe foetal compromise may not prevent neonatal deaths because they have already experienced such severity of complications that although live born, neonatal death is difficult to prevent.
There are two possible scenarios leading to caesarean section in Ethiopia. First, when women who have previously had a caesarean section, with breech presentation, or other risk factors such as eclampsia attend specialised health facilities, they are usually allowed to undergo caesarean section. Their caesarean section is commonly classified as ‘elective or scheduled caesarean section’. Second, when caesarean section is performed for ‘emergency reasons’. Full-term mothers with or without signs of labour will be admitted to health facilities where their progress is monitored and labour-augmenting or inducing medications may be administered. Decisions to perform caesarean section in these facilities or decision to refer the mother to nearby hospitals for caesarean delivery or other action depends on the condition of the mother and fetus during the progress of labour. In primary health facilities (ie, health posts and health centres), obstetric care providers usually use a ‘Partograph’,45 46 a routine labour monitoring instrument (chart) which helps the healthcare providers to identify slow progress in labour and take appropriate action. In hospitals, the decision to perform a caesarean section is reached when the labour is prolonged and/or the second stage of labour is complicated risking the life of mother and fetus.
Given these pathways to caesarean delivery in mind, our interpretation of the association between caesarean birth and neonatal death in Ethiopia using the 2016 survey may be shaped by examining factors contributing to delays in the ‘Three Delays Model’. This is because delays to caesarean section aggravate the underlying medical indications for caesarean intervention. Table 4 shows factors affecting the length of delays in the ‘Three Delays Model’ according to sociodemographic characteristics in the 2016 survey.
Table 4.
Factors contributing to the ‘Three Delays Model’, according to sociodemographic characteristics, Ethiopia DHS 2016
| Delivery by skilled provider* | Number of births | Problems in accessing healthcare by women aged 15–49 years† | ||||||
| Distance to health facility | Getting money for treatment | Getting permission to go for treatment | Not wanting to go alone | At least one problem accessing healthcare | Number of women | |||
| Types of residence | ||||||||
| Urban | 80.1 | 1 216 | 17.0 | 34.7 | 15.1 | 21.4 | 45.6 | 3 476 |
| Rural | 21.2 | 9 807 | 59.8 | 60.5 | 37.0 | 47.9 | 76.9 | 12 207 |
| Region | ||||||||
| Tigray | 59.3 | 716 | 37.4 | 46.1 | 15.3 | 24.6 | 60.7 | 1 129 |
| Affar | 16.4 | 114 | 54.3 | 51.7 | 28.2 | 41.8 | 66.6 | 128 |
| Amhara | 27.7 | 2 072 | 33.7 | 35.3 | 15.4 | 34.6 | 55.7 | 3 714 |
| Oromia | 19.7 | 4 851 | 68.9 | 70.1 | 58.3 | 57.0 | 82.9 | 5 701 |
| Somali | 20.0 | 508 | 47.3 | 63.0 | 25.7 | 32.2 | 72.6 | 459 |
| Benishangul-Gumuz | 28.6 | 122 | 57.4 | 62.4 | 36.5 | 43.8 | 76.8 | 160 |
| SNNPR | 28.6 | 2 296 | 52.7 | 59.1 | 18.4 | 39.5 | 75.4 | 3 288 |
| Gambela | 46.9 | 27 | 41.0 | 44.3 | 24.3 | 33.7 | 61.2 | 44 |
| Harari | 51.2 | 26 | 18.1 | 28.2 | 16.3 | 13.8 | 30.8 | 38 |
| Addis Ababa | 96.8 | 244 | 10.8 | 29.2 | 8.7 | 14.5 | 40.0 | 930 |
| Dire Dawa | 56.7 | 47 | 57.4 | 64.5 | 58.7 | 55.2 | 71.4 | 90 |
| Mother’s education | ||||||||
| No education | 17.2 | 7 284 | 59.2 | 62.9 | 37.6 | 47.1 | 78.0 | 7 498 |
| Primary | 38.6 | 2 951 | 50.3 | 55.7 | 31.9 | 43.2 | 71.1 | 5 490 |
| Secondary | 78.4 | 514 | 27.8 | 33.2 | 18.2 | 27.8 | 48.1 | 1 817 |
| More than secondary | 93.2 | 274 | 20.6 | 23.8 | 15.9 | 20.4 | 39.8 | 877 |
| Wealth quintile | ||||||||
| Poorest | 11.0 | 2 636 | 67.7 | 70.9 | 40.0 | 54.5 | 85.3 | 2 633 |
| Poorer | 20.8 | 2 520 | 66.8 | 67.0 | 42.1 | 52.7 | 82.9 | 2 809 |
| Middle | 24.2 | 2 280 | 59.4 | 61.0 | 35.2 | 47.6 | 77.3 | 2 978 |
| Richer | 28.5 | 1 999 | 49.8 | 50.2 | 33.8 | 41.2 | 68.2 | 3 100 |
| Richest | 70.3 | 1 588 | 22.1 | 35.2 | 17.0 | 23.4 | 47.7 | 4 163 |
| Total | 27.7 | 11 023 | 50.3 | 54.8 | 32.1 | 42.0 | 70.0 | 15 683 |
*Percentage delivered by a skilled provider (ie, doctor, nurse, midwife, health officer and health extension worker).
†Percentage of women aged 15–49 who reported that they have serious problems in accessing healthcare for themselves when they are sick, by type of problem, according to sociodemographic characteristics, Ethiopia DHS 2016.
Phase I delay: deciding to seek care
In Ethiopia, poorer and less-educated women are more likely to select a nearby health facility, especially in rural areas, where there is limited access to caesarean section and the possibility of benefiting from caesarean section is mainly through referral to higher levels of care. Women are more likely to undergo a caesarean section if they present to specialised health facilities. However, the outcome of delivery depends on how quick/competent the healthcare provider is in referring the mother or on intervening, and the severity of the underlying obstetric complications for caesarean intervention which may be affected by the delay in women’s or family’s decision to seek care. Poor health decision-making depends on numerous factors such as educational status, distance to health facility, economic status, sociocultural factors (eg, unsupportive spouse and lack of autonomy) and quality of care.24 47 48
Table 4 shows that ‘distance to health facility’ was a big problem in accessing healthcare for about 60% of rural and 17% of urban women in Ethiopia. Similarly, ‘getting money for treatment’ is a big problem to access healthcare and was reported by 61% of rural and 35% of urban women in 2016. On the other hand, the status of women in a given society affects the decision to seek care. For instance, efforts to seek timely care are influenced by women’s limited mobility because they need permission to travel from spouse and/or mother-in-law.24 In Ethiopia, about 37% of rural and 15% of urban women reported ‘getting permission to go for treatment’ was a big problem to access healthcare.
Phase II delay: identifying and reaching a medical facility
Delay in reaching healthcare may occur when women who encounter obstetric complication live farther from health facilities, where the availability and cost of transportation is problematic. In one study conducted in rural India, Kumar et al 47 found that health facility births occur less likely among women living farther away from the health facilities, suggesting distance as an important barrier to in-facility births for rural women. In addition to the travel distance, the scarcity of transportation which may be accompanied by poor roads is also another obstacle for women with labour complications to timely reach even the closest health facility. As a result of this, women who arrive at the nearby facility following obstetric complications probably will travel further to specialised hospital due to emergency referral. It is clear that the obstetric complications encountered by mothers reaching nearby primary health facilities will be compounded by additional delays when they are referred for caesarean section. These scenarios highlight the likelihood of adverse delivery outcome followed by aggravated obstetric complications due to delays in reaching medical facility as high.
In Ethiopia, about 50% of women of reproductive age (15–49 years) reported ‘distance to health facility’ as a big problem to access healthcare (table 4). Moreover, access to caesarean situation in Ethiopia is worse than in most other settings.
Phase III delay: receiving adequate and appropriate treatment
Phase III delays occur within any health facilities and are indicators of inadequate care due to lack of facilities; inadequately trained obstetric care givers (skilled birth attendants) and deficiencies in surgical facilities, surgical and anaesthesia personnel and equipment, and blood transfusion as well as inadequate and inappropriate referral systems. These deficiencies will limit women’s access to lifesaving procedures such as caesarean section. In Ethiopia, only 28.0% of all births were delivered by ‘skilled providers’ (ie, doctor, nurse, midwife, health officer and health extension worker) in the 2016 survey. Table 4 also shows that there are disparities in the proportion of births attended by skilled birth attendants by urban–rural place of residence, region, level of mother’s education and household wealth. It is quite clear that insufficient number of skilled birth attendants at any health facility will lead to delay in receiving appropriate treatment among women with obstetric complications. Although health posts and health centres (primary healthcare unit) are the most accessible to the general population in Ethiopia, they are not fully equipped to deal with obstetric complications.41 42 As a result of this, women with obstetrics complications will have to travel on to better equipped institutions (secondary and tertiary levels of healthcare) with caesarean section capacity (eg, general hospitals and specialised hospitals) through referral. By the time women reach these well-equipped health facilities, the delays will have further aggravated the obstetric complications on the way. A schematic representation of the Ethiopian health system structure is provided in online supplementary figure A5.
On the other hand, delay in caesarean intervention may even happen if mothers with less severe obstetric complications were referred and presented to specialised health facilities in a timely manner. This is because a trial of labour is usually attempted before a decision to have caesarean section. For instance, some women who are referred from primary health facilities undergo induction and augmentation of labour because these interventions are only provided in health facilities with the capacity to provide caesarean section in Ethiopia. These practices, in turn, will result in delay in receiving caesarean section leading to worsening of the already existing obstetric complications. Thus, any delays to caesarean intervention have a higher chance of aggravating the already existing complications and increase the risk of neonatal death.
Discussion
Our study examined the changing temporal association between caesarean birth and neonatal death within the context of Ethiopia from 2000 to 2016. The association between caesarean section and neonatal death increased over time and was variable among population subgroups. These changes over time, and variation across population subgroups may be attributable to changes in the pattern of confounding by indication due to contextual factors such as improvement in health service coverage, unequal access (eg, due to a range of geographic, social and economic barriers) and structural and health workforce constraints.
In Ethiopia, the proportion of women aged 15–49 years who received any antenatal care from a skilled provider has increased from 27% in 2000 to 62% in 2016.32 Health facility-based deliveries have increased from 5% in 2000 to 26% in 2016 (increased from 2% in 2000 to 20% in 2016 for rural women, and increased from 32% in 2000 to 79% in 2016 for urban women).32 The proportion of births in health facilities assisted by skilled birth attendants increased from 6% in 2000 to 28% in 2016.32 These figures reflect improvement in health service coverage in Ethiopia.
Moreover, since 2003, with the implementation of the Health Extension Program—a community-based primary healthcare program—the Ethiopian government has increased the number of health posts from 4 211 in 2005 to 16 447 in 2015.42 49 Likewise, the number of health centres was increased from 600 in 2005 to 3 586 in 2015.42 49 However, due to limitations in proper monitoring of labour for making timely decisions, especially on whether or not to initiate a referral from primary health facilities to higher level facilities, and due to poor transport and road networks which are still the common problems in low-income countries,50 the underlying medical indications for caesarean intervention will be worsened by factors contributing to ‘delays’. Delay in receiving adequate and appropriate care is still a common problem in low-income countries due to deficiencies in surgical facilities, surgical and anaesthesia personnel and equipment, blood transfusion capacity and shortage of skilled birth attendants.51–53 There is also an inequitable distribution of the health workforce across urban and rural areas. For example, the majority of specialist doctors in Ethiopia serve in urban areas, where the total population distribution is only 19.4%.41 42 These situations often result in poor quality care to rural women, and the caesarean section conducted after a complicated labour may be associated with increased neonatal mortality due to confounding by indication.
Unlike previous studies, the present study takes into account the interpretation of the association between caesarean birth and neonatal death within the context of Ethiopia using DHS data. The change in the strength of effect estimates across DHS waves, and the different subgroup analyses suggest that neonatal mortality can be reduced by increasing timely access to caesarean section and timely decision for caesarean delivery via increasing health service coverage, improving infrastructure (eg, increasing number of health facilities), increasing the number of skilled birth attendants, improving quality of care and increasing awareness about antenatal care and health facility delivery among women. Moreover, provision of training to skilled birth attendants on close monitoring of labour and early detection of complications, equipping the primary health facilities (eg, health centres) to the level of caesarean capacity, and continuous financial investment in primary health facilities will be an important strategy to reduce neonatal mortality.
It appears that previous studies which used individual-level data are more likely to report an increased risk of neonatal death among infants born by caesarean section than the ecological studies. This may be due to the indications for the caesarean delivery (eg, the severity of the underlying causes) was involved in causing both caesarean delivery and neonatal death in studies which used individual-level data, suggesting the role of confounding by indication in the association between caesarean birth and neonatal death because an intended effect of caesarean birth is prevention of neonatal death. Therefore, the increased risk for neonatal death associated with caesarean birth, compared with vaginal birth, would appear to be intuitive given the fact that neonatal death rates after emergency caesarean section is strongly dependent on the underlying medical indication (eg, antenatally diagnosed foetal malformation or foetal growth restriction) for caesarean intervention.
In Ethiopia, the national rate of caesarean section increased from 0.7% in 2000 to 1.9% in 2016. On the other hand, neonatal mortality rate declined from 49 deaths per 1 000 live births in 2000 to 29 deaths per 1 000 births in 2016.32 Similarly, the pregnancy-related mortality ratio decreased from 871 pregnancy-related deaths per 100 000 live births in 2000 to 412 pregnancy-related deaths per 100 000 live births in 2016.32 Our analyses based on aggregate-level data from Ethiopian DHS showed that an increase in caesarean section rate is correlated with a decrease in the proportion of neonatal deaths. Even though similar context-specific interpretation is applicable to ecological studies, additional explanation may also be necessary to interpret the association. For example, a change in neonatal mortality rate may be attributable to changes acting on the population as a whole—that is, changes in health coverage indicators, such as an increase in births attended by skilled birth attendants (increased from 6% in 2000 to 28% in 2016)32 and immunisation coverage (was 86.4% in 2015).42
We acknowledge the following limitations of this study. First, as both the proportion of institutional deliveries and caesarean section rate is low in Ethiopia, especially in rural areas, the number of neonatal deaths following caesarean section may be low. However, since our analyses are weighted, we believe that the weight improves the representativeness of the data in terms of size, distribution and characteristics of the Ethiopian population. The weight may also ensure that our estimates are unbiased though the CI for some subgroup analyses are somewhat wide. Second, the interpretation of our study is specific to the context of Ethiopia and may not be generalisable to other developing countries in Africa or elsewhere. Another limitation is the mother’s recall of the child’s size at birth was used as a substitute for the child’s birth weight in this study because the data for birth weight were not collected for more than 50% of the neonates in DHS.
Conclusions
A naïve interpretation of the changing temporal association between caesarean birth and neonatal death from 2000 to 2016 is that caesarean section is increasingly associated with neonatal death. However, the changing temporal association likely reflects improvements in health service coverage and secular shifts in the characteristics of Ethiopian women undergoing caesarean section after complicated labour or severe foetal compromise.
Supplementary Material
Acknowledgments
The authors are grateful to The DHS Program for providing the data sets used for this analysis. BWM is supported by an NHMRC Practitioner Fellowship (GNT1082548) and also reports consultancy for ObsEva, Merck Merck KGaA, and Guerbet. JWL is supported by an NHMRC Centre of Research Excellence (GNT1099422).
Footnotes
Twitter: @@Engida_Yisma
Contributors: All authors (EY, BWM, JWL and LGS) contributed to the design of the study and the interpretation of data. EY performed the data analysis and drafted the manuscript. All other authors critically revised the draft manuscript. All authors read and approved the final manuscript. EY is the guarantor of the paper.
Funding: The first author is fully supported by an Australian Government Research Training Programme Scholarship (RTPS).
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository.
References
- 1. United Nations Inter-agency Group for Child Mortality Estimation (UN IGME) Levels and trends in child mortality: report 2017, estimates developed by the UN Inter-agency Group for Child Mortality Estimation. New York: United Nations Children’s Fund, 2017. [Google Scholar]
- 2. UN General Assembly Transforming our world: the 2030 agenda for sustainable development, 21 October 2015, A/RES/70/1. Available: https://www.refworld.org/docid/57b6e3e44.html [Accessed 28 Jun 2019].
- 3. Costello A, Osrin D. Epidemiological transition, medicalisation of childbirth, and neonatal mortality: three Brazilian birth-cohorts. Lancet 2005;365:825–6. 10.1016/S0140-6736(05)71017-5 [DOI] [PubMed] [Google Scholar]
- 4. Gibbons L, Belizan JM, Lauer JA, et al. Inequities in the use of cesarean section deliveries in the world. Am J Obstet Gynecol 2012;206:331.e1–19. 10.1016/j.ajog.2012.02.026 [DOI] [PubMed] [Google Scholar]
- 5. Leone T, Padmadas SS, Matthews Z. Community factors affecting rising caesarean section rates in developing countries: an analysis of six countries. Soc Sci Med 2008;67:1236–46. 10.1016/j.socscimed.2008.06.032 [DOI] [PubMed] [Google Scholar]
- 6. de Mello e Souza C. C-sections as ideal births: the cultural constructions of beneficence and patients' rights in Brazil. Camb Q Healthc Ethics 1994;3:358–66. [DOI] [PubMed] [Google Scholar]
- 7. Dumont A, de Bernis L, Bouvier-Colle MH, et al. Caesarean section rate for maternal indication in sub-Saharan Africa: a systematic review. Lancet 2001;358:1328–33. 10.1016/S0140-6736(01)06414-5 [DOI] [PubMed] [Google Scholar]
- 8. Vogel JP, Betrán AP, Vindevoghel N, et al. Use of the Robson classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. Lancet Glob Health 2015;3:e260–70. 10.1016/S2214-109X(15)70094-X [DOI] [PubMed] [Google Scholar]
- 9. Ye J, Betrán AP, Guerrero Vela M, et al. Searching for the optimal rate of medically necessary cesarean delivery. Birth 2014;41:237–44. 10.1111/birt.12104 [DOI] [PubMed] [Google Scholar]
- 10. World Health Organization WHO statement on caesarean section rates. Geneva: World Health Organization, 2015. [Google Scholar]
- 11. Betrán AP, Merialdi M, Lauer JA, et al. Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol 2007;21:98–113. 10.1111/j.1365-3016.2007.00786.x [DOI] [PubMed] [Google Scholar]
- 12. Molina G, Weiser TG, Lipsitz SR, et al. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA 2015;314:2263–70. 10.1001/jama.2015.15553 [DOI] [PubMed] [Google Scholar]
- 13. Ye J, Zhang J, Mikolajczyk R, et al. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: a worldwide population-based ecological study with longitudinal data. BJOG 2016;123:745–53. 10.1111/1471-0528.13592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Althabe F, Sosa C, Belizán JM, et al. Cesarean section rates and maternal and neonatal mortality in low-, medium-, and high-income countries: an ecological study. Birth 2006;33:270–7. 10.1111/j.1523-536X.2006.00118.x [DOI] [PubMed] [Google Scholar]
- 15. Lumbiganon P, Laopaiboon M, Gülmezoglu AM, et al. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007-08. Lancet 2010;375:490–9. 10.1016/S0140-6736(09)61870-5 [DOI] [PubMed] [Google Scholar]
- 16. Villar J, Carroli G, Zavaleta N, et al. Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicentre prospective study. BMJ 2007;335 10.1136/bmj.39363.706956.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. MacDorman MF, Declercq E, Menacker F, et al. Infant and neonatal mortality for primary cesarean and vaginal births to women with ‘no indicated risk,’ United States, 1998-2001 birth cohorts. Birth 2006;33:175–82. 10.1111/j.1523-536X.2006.00102.x [DOI] [PubMed] [Google Scholar]
- 18. MacDorman MF, Declercq E, Menacker F, et al. Neonatal mortality for primary cesarean and vaginal births to low-risk women: application of an ‘intention-to-treat’ model. Birth 2008;35:3–8. 10.1111/j.1523-536X.2007.00205.x [DOI] [PubMed] [Google Scholar]
- 19. Källén K, Olausson PO. Neonatal mortality for low-risk women by method of delivery. Birth 2007;34:99–100. author reply 1-2 10.1111/j.1523-536X.2006.00155_1.x [DOI] [PubMed] [Google Scholar]
- 20. Shah A, Fawole B, M'imunya JM, et al. Cesarean delivery outcomes from the WHO global survey on maternal and perinatal health in Africa. Int J Gynaecol Obstet 2009;107:191–7. 10.1016/j.ijgo.2009.08.013 [DOI] [PubMed] [Google Scholar]
- 21. Kyu HH, Shannon HS, Georgiades K, et al. Caesarean delivery and neonatal mortality rates in 46 low- and middle-income countries: a propensity-score matching and meta-analysis of Demographic and Health Survey data. Int J Epidemiol 2013;42:781–91. 10.1093/ije/dyt081 [DOI] [PubMed] [Google Scholar]
- 22. Begum T, Rahman A, Nababan H, et al. Indications and determinants of caesarean section delivery: evidence from a population-based study in Matlab, Bangladesh. PLoS One 2017;12:e0188074 10.1371/journal.pone.0188074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Belizán JM, Minckas N, McClure EM, et al. An approach to identify a minimum and rational proportion of caesarean sections in resource-poor settings: a global network study. Lancet Glob Health 2018;6:e894–901. 10.1016/S2214-109X(18)30241-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med 1994;38:1091–110. 10.1016/0277-9536(94)90226-7 [DOI] [PubMed] [Google Scholar]
- 25. Stanton CK, Dubourg D, De Brouwere V, et al. Reliability of data on caesarean sections in developing countries. Bull World Health Organ 2005;83:449–55. doi:/S0042-96862005000600013 [PMC free article] [PubMed] [Google Scholar]
- 26. Channon AAR. Can mothers judge the size of their newborn? assessing the determinants of a mother's perception of a baby's size at birth. J Biosoc Sci 2011;43:555–73. 10.1017/S0021932011000198 [DOI] [PubMed] [Google Scholar]
- 27. Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography 2001;38:115–32. 10.1353/dem.2001.0003 [DOI] [PubMed] [Google Scholar]
- 28. Filmer D, Scott K. Assessing asset indices. Demography 2012;49:359–92. 10.1007/s13524-011-0077-5 [DOI] [PubMed] [Google Scholar]
- 29. Yisma E, Smithers LG, Lynch JW, et al. Cesarean section in Ethiopia: prevalence and sociodemographic characteristics. J Matern Fetal Neonatal Med 2019;32:1130–5. 10.1080/14767058.2017.1401606 [DOI] [PubMed] [Google Scholar]
- 30. Souza JP, Gülmezoglu A, Lumbiganon P, et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004-2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med 2010;8:71 10.1186/1741-7015-8-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ronsmans C, Etard JF, Walraven G, et al. Maternal mortality and access to obstetric services in West Africa. Trop Med Int Health 2003;8:940–8. 10.1046/j.1365-3156.2003.01111.x [DOI] [PubMed] [Google Scholar]
- 32. Central Statistical Agency - CSA/Ethiopia, ICF . Ethiopia Demographic and Health Sruvey 2016. Addis Ababa, Ethiopia: CSA and ICF, 2017. [Google Scholar]
- 33. Boerma T, Ronsmans C, Melesse DY, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet 2018;392:1341–8. 10.1016/S0140-6736(18)31928-7 [DOI] [PubMed] [Google Scholar]
- 34. Boatin AA, Schlotheuber A, Betran AP, et al. Within country inequalities in caesarean section rates: observational study of 72 low and middle income countries. BMJ 2018;360 10.1136/bmj.k55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Upadhyay RP, Rai SK, Krishnan A. Using three delays model to understand the social factors responsible for neonatal deaths in rural Haryana, India. J Trop Pediatr 2013;59:100–5. 10.1093/tropej/fms060 [DOI] [PubMed] [Google Scholar]
- 36. Mbaruku G, van Roosmalen J, Kimondo I, et al. Perinatal audit using the 3-delays model in Western Tanzania. Int J Gynaecol Obstet 2009;106:85–8. 10.1016/j.ijgo.2009.04.008 [DOI] [PubMed] [Google Scholar]
- 37. Waiswa P, Kallander K, Peterson S, et al. Using the three delays model to understand why newborn babies die in eastern Uganda. Trop Med Int Health 2010;15:964–72. 10.1111/j.1365-3156.2010.02557.x [DOI] [PubMed] [Google Scholar]
- 38. Holmer H, Lantz A, Kunjumen T, et al. Global distribution of surgeons, anaesthesiologists, and obstetricians. Lancet Glob Health 2015;3(Suppl 2):S9–11. 10.1016/S2214-109X(14)70349-3 [DOI] [PubMed] [Google Scholar]
- 39. Ologunde R, Vogel JP, Cherian MN, et al. Assessment of cesarean delivery availability in 26 low- and middle-income countries: a cross-sectional study. Am J Obstet Gynecol 2014;211:504.e1–12. 10.1016/j.ajog.2014.05.022 [DOI] [PubMed] [Google Scholar]
- 40. Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ 2007;85:812–9. 10.2471/BLT.06.035659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. WHO Primary health care systems (PRIMASYS): case study from Ethiopia, abridged version. Geneva: World Health Organization, 2017. Licence: CC BY-NC-SA 3.0 IGO. [Google Scholar]
- 42. Federal Ministry of Health Health and health related indicators 2007 E.C. (2014/15 G.C). Addis Ababa, Ethiopia: Federal Ministry of Health, 2015. [Google Scholar]
- 43. Betran AP, Torloni MR, Zhang JJ, et al. WHO statement on caesarean section rates. BJOG 2016;123:667–70. 10.1111/1471-0528.13526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Thomas S, Meadows J, McQueen KAK. Access to cesarean section will reduce maternal mortality in low-income countries: a mathematical model. World J Surg 2016;40:1537–41. 10.1007/s00268-016-3479-0 [DOI] [PubMed] [Google Scholar]
- 45. Yisma E, Dessalegn B, Astatkie A, et al. Knowledge and utilization of partograph among obstetric care givers in public health institutions of Addis Ababa, Ethiopia. BMC Pregnancy Childbirth 2013;13:17 10.1186/1471-2393-13-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yisma E, Dessalegn B, Astatkie A, et al. Completion of the modified World Health Organization (WHO) partograph during labour in public health institutions of Addis Ababa, Ethiopia. Reprod Health 2013;10:23 10.1186/1742-4755-10-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kumar S, Dansereau EA, Murray CJL. Does distance matter for institutional delivery in rural India? Appl Econ 2014;46:4091–103. 10.1080/00036846.2014.950836 [DOI] [Google Scholar]
- 48. Anselmi L, Lagarde M, Hanson K. Health service availability and health seeking behaviour in resource poor settings: evidence from Mozambique. Health Econ Rev 2015;5:62 10.1186/s13561-015-0062-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Federal Ministry of Health Health and health related indicators 1997 E.C. (2004/05 G.C). Addis Ababa, Ethiopia: Federal Ministry of Health, 2005. [Google Scholar]
- 50. Atuoye KN, Dixon J, Rishworth A, et al. Can she make it? transportation barriers to accessing maternal and child health care services in rural Ghana. BMC Health Serv Res 2015;15:333 10.1186/s12913-015-1005-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Bergström S. Training non-physician mid-level providers of care (associate clinicians) to perform caesarean sections in low-income countries. Best Pract Res Clin Obstet Gynaecol 2015;29:1092–101. 10.1016/j.bpobgyn.2015.03.016 [DOI] [PubMed] [Google Scholar]
- 52. Orji EO, Ojofeitimi EO, Esimai AO, et al. Assessment of delays in receiving delivery care at a tertiary healthcare delivery centre in Nigeria. J Obstet Gynaecol 2006;26:643–4. 10.1080/01443610600903628 [DOI] [PubMed] [Google Scholar]
- 53. Miller S, Abalos E, Chamillard M, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet 2016;388:2176–92. 10.1016/S0140-6736(16)31472-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-027235supp001.pdf (476.6KB, pdf)