Abstract
Objectives
Glaucoma filtering schemes such as the Manchester Glaucoma Enhanced Referral Scheme (GERS) aim to reduce the number of false positive cases referred to Hospital Eye Services. Such schemes can also have wider system benefits, as they may reduce waiting times for other patients. However, previous studies of the cost consequences and wider system benefits of glaucoma filtering schemes are inconclusive. We investigate the cost consequences of the Manchester GERS.
Design
Observational study.
Methods
A cost analysis from the perspective of the National Health Service (NHS) was conducted using audit data from the Manchester GERS.
Results
2405 patients passed through the Manchester GERS from April 2013 to November 2016. 53.3% were not referred on to Manchester Royal Eye Hospital (MREH). Assuming an average of 2.3 outpatient visits to MREH were avoided for each filtered patient, the scheme saved the NHS approximately £2.76 per patient passing through the scheme.
Conclusion
Our results indicate that glaucoma filtering schemes have the potential to reduce false positive referrals and costs to the NHS.
Keywords: glaucoma
Key messages.
What is already known about this subject?
Glaucoma referral filtering schemes aim to reduce false positive referrals to Hospital Eye Services (HES) and reduce costs to the National Health Service (NHS). However, there is mixed evidence concerning the costs of filtering schemes.
What are the new findings?
We use audit data to assess the costs associated with the Manchester Glaucoma Enhanced Referral Scheme (GERS). The Manchester GERS has not been costed since Henson et al.10 We find that the scheme is cost saving to the NHS if we assume that 2.2 outpatient visits to the HES are avoided.
How might these results change the focus of research or clinical practice?
The findings in this study highlight the need for consistent cost assessments of referral filtering schemes. The study finds that referral filtering schemes may not always be cost saving to the NHS.
Introduction
Glaucoma is the world’s leading cause of irreversible blindness.1 Up to 20% of new referrals to Hospital Eye Services (HES) (hospital outpatient eye services) in the UK are for suspected glaucoma, with the annual cost of monitoring patients with this chronic condition estimated to be £22.5 million.2 The National Health Service (NHS) is under tight budgetary restrictions3; it is therefore necessary that demand for outpatient ophthalmology services is managed effectively and efficiently.
Identifying the appropriate patients for outpatient hospital care remains an ongoing challenge for all UK glaucoma services. A concern for ophthalmology services in the UK is that a high proportion of referrals (between 20% and 65%) have been found to be false positives.4–6 Shah and Murdoch7 found both the percentage and the number of false positive referrals for suspected glaucoma had increased further since the introduction of the first National Institute for Clinical Excellence (NICE)glaucoma guideline in 2009. Not only do false positive referrals place unnecessary demands on overstretched resources, but false positive referrals also incur financial costs, both for the NHS and for the patient, as well as unnecessary anxiety potentially experienced by referred patients.8
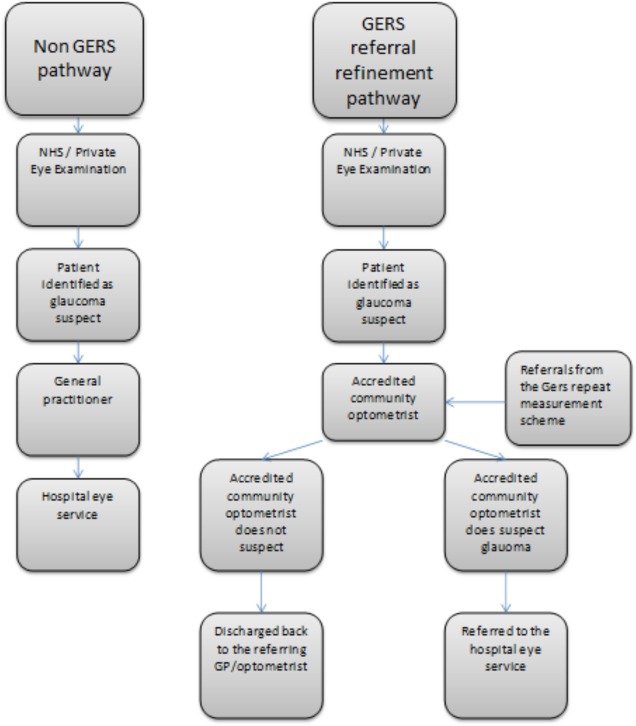
Concern regarding false positive referrals associated with glaucoma diagnosis has resulted in the introduction of glaucoma referral filtering schemes (including repeat measures (see figure 1), enhanced case finding, and referral refinement schemes9).9 An example is the Manchester Glaucoma Enhanced Referral Scheme (GERS), which was initially introduced in 2000 and updated in 2013. In this paper, we examine the cost consequences of the Manchester GERS by considering the total costs of the scheme.
Figure 1.
Manchester GERS pathway. GERS, Glaucoma Enhanced Referral Scheme; GP, general practitioner; NHS, National Health Service.
Glaucoma referral filtering schemes
In the UK, most referrals for suspected glaucoma are generated through opportunistic surveillance during sight tests or private eye examinations by community optometrists. These community optometrists will refer patients onto HES if they suspect glaucoma. The number of patients being referred to HES ophthalmology outpatient departments is rapidly increasing due to: an ageing population; advances in diagnostic and screening tools; until the updated NICE guideline of 2017, changes in national and professional guidance regarding glaucoma care.9
Glaucoma referral filtering services allow trained practitioners to repeat, enhance or refine their findings for patients who have suspected glaucoma in community settings, before onward referral to the HES, therefore reducing/avoiding unnecessary referrals. Not only does the reduction in false positive referrals relieve excess demand on overstretched ophthalmology departments, but it also has the potential to reduce waiting times for other patients. There are different types of filtering services: repeat measures schemes include those where measures such as intraocular pressure and/or visual fields are repeated prior to referral, enhanced case finding schemes sees the optometrist undertake a higher level of assessment to offer testing, adding value beyond repeat measures and finally, glaucoma referral refinement offers a level of testing sufficient for diagnosis of glaucoma.
The Manchester GERS is an example of an enhanced case finding scheme with a repeat measures filter also feeding into the enhanced case finding pathway. Figure 1 shows the different aspects of the Manchester GERS. In the Manchester GERS patients with suspected glaucoma are referred to a group of trained and accredited community optometrists who have undergone specialist training in glaucoma, rather than being referred through their general practitioner (GP) onto ophthalmology outpatient departments. These community optometrists work to an agreed assessment protocol and set of referral criteria, and, depending on whether or not the patient meets these criteria, either refer the patient directly to the HES or discharge them back to the care of to their referring optometrist or GP (see figure 1). Not only does the GERS pathway aim to reduce false positive referrals, but it also allows patients with suspected glaucoma to be seen by a trained specialist optometrist within 20 working days of referral. Furthermore, the additional clinical information collected by the accredited community optometrist means that triage at the hospital ophthalmology department can prioritise patients with higher clinical need.
In 2003 Henson et al10 analysed the Manchester scheme (then known as a glaucoma referral refinement scheme) and found that 42% of patients passing through the scheme were not referred onto the Manchester Royal Eye Hospital (MREH). This reduction in false positive referrals meant that the scheme reduced costs to the NHS by approximately £17 per patient.
Similar glaucoma referral filtering schemes throughout the UK have also been found to reduce false positive referrals to HES and to be cost saving to the NHS.11 12 Devarajan et al11 assessed a variation of the Manchester GERS with an additional form of refinement for patients not referred 12 months later. Devarajan et al11 found the Carmarthenshire Glaucoma Referral Refinement Scheme to be cost saving at £117 per patient passing through the scheme. Parkins and Edgar12 also analysed two glaucoma referral filtering schemes within the Bexley Care Trust; a glaucoma repeat measurements scheme and a refinement pathway scheme. The authors found the repeat measurement scheme demonstrated a substantial cost benefit to the NHS, whereas, the onward referral refinement scheme was found to be cost neutral.
Henson et al10 based their analysis on the assumption that false positive referrals attending the HES before the introduction of the glaucoma referral filtering scheme would have had on average 2.3 clinic visits before being discharged. Previous cost consequence studies have either used values of 2.3 or 2.1 visits to the HES prior to discharge (Devarajan et al,11 Parkins and Edgar12 and Ratnarajan et al2). All of these studies found glaucoma referral filtering schemes to be cost saving. However, these studies assume that false positive patients would make more than two visits to an eye hospital prior to discharge. This figure comes from an audit of new referrals to the MREH in 1997. Due to advances in technology, the introduction of payment by results, and amended clinical guidelines, it could be possible that the number of follow-up visits prior to discharge may have changed from Henson et al’s audit in 1997 (Henson et al10).
In 2016 the Royal College of Ophthalmologists and College of Optometrists issued Joint College Guidance recommending the implementation of glaucoma referral filtering schemes across the UK, where possible, to reduce the false positive referral rate to ophthalmology services.13 However, the cost consequences of such glaucoma referral schemes are unclear and previous studies indicate that more than one visit to the HES needs to be avoided to make the scheme cost saving.10–12
We aim to calculate the costs savings of the Manchester GERS from the perspective of the NHS.
Data
Cost analysis
The Manchester GERS was revised in 2013. Data were collected on patients passing through the scheme from April 2013 to November 2016. The main change from the earlier Manchester glaucoma referral refinement scheme was the inclusion of pachymetry (the measurement of central corneal thickness) and a related revision of referral criteria based on age, intraocular pressure and central corneal thickness, to better reflect the then NICE guideline’s treatment algorithm CG8514 and deal with concerns about an increase in false positive referrals following the introduction of the guideline.7 All patients registered with a GP in Manchester who present at a community optometrist or GP with any suspect signs of glaucoma were eligible to participate in the scheme.
Waiting times and referrals
We also use data from national Hospital Episodes Statistics to examine the impact of the number of referrals on waiting times. Hospital Episode Statistics provide information on all outpatient hospital appointments across all hospital trusts in England. This data allow us to examine whether a reduction in the number of people referred to HES reduces waiting times for patients at a national level. We focused on first referral appointments to ophthalmology departments. Using Hospital Episode Statistics, we have information on: waiting times; number of referrals; age of patients; and, identifiers for the hospital Trust attended for all ophthalmology outpatient appointments between April 2008 and March 2012.
Methods
Cost analysis
We calculated the cost of a first outpatient visit to ophthalmology by taking the average of the tariffs from the national tariff workbook for years 2013–2017 which specifies national prices for specific healthcare services paid by the NHS. Patients from the participating practices attended Manchester University NHS Foundation Trust (MFT). Therefore, we applied the Market Forces Factor of 1.0568 for MFT. This calculation resulted in a cost of £114 for a first attendance and £65 for a follow-up appointment. Costs of training optometrists, optometrists’ fees and the cost of equipment were collected through an audit of the scheme. Savings were calculated by multiplying the cost of an outpatient appointment by the number of visits avoided through the Manchester GERS.
An internal audit of the Manchester scheme found that approximately 8% of patients seen through the repeat measurements pathway were referred onto the Manchester GERS per year. We calculate the average cost per patient passing through the repeat measurement scheme per year using internal audit data and include this cost in our analysis.
We go onto calculate a threshold value of follow-up visits to the MREH that would make the scheme cost neutral.
Patient and public involvement
No patients were involved in the development of the research question and outcomes measures, nor were they involved in the design of the study. No patients were asked to advise on the interpretation of the results.
Results
Cost analysis
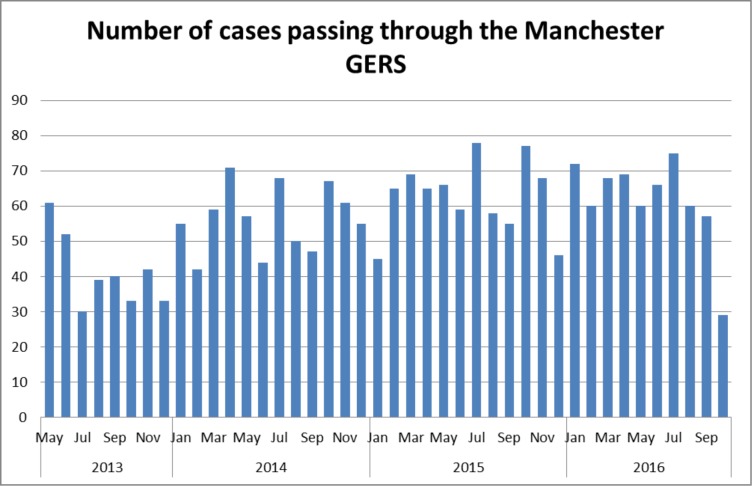
18 community optometric practices across Greater Manchester participated in the Manchester GERS and 2405 patients passed through the scheme between April 2013 and November 2016. Figure 2 shows the distribution of cases passing through the scheme. The average number of patients per month throughout the scheme was 53. The distribution of patients is fairly evenly distributed across months with a reduction in the number of cases in December each year.
Figure 2.
Number of patients passing through the GERS each month. GERS, Glaucoma Enhanced Referral Scheme.
Henson et al’s10 method of cost analysis is replicated in table 1. In total 2405 patients passed through the Manchester GERS from April 2013 to November 2016. Of these 2405 patients, 1282 (53.3%) were not referred on to the MREH. When following the assumptions of Henson et al10 that 2.3 outpatient visits to MREH are avoided, the scheme is cost saving to the NHS of £6635, equating to approximately £ 2.76 per patient (£6635/2405) passing through the scheme.
Table 1.
Costs/savings of the Manchester referral refinement GERS from April 2013 to November 2016 based on 2.3 visits before discharge
| Savings (£) | Costs (£) | Notes | |
| Cost of patients entering from the repeat measurement scheme | 4938.05 | Approximately 8% of patients were referred to GERS per year from the repeat measures pathway. The average cost of the repeat measurement scheme is £27.82 per patient, calculated by the number of patients who were seen for an initial assessment (359*£29) and the number of patients who were seen for a second examination (124*£25).* The total cost is then divided by the number of patients who were assessed in the repeat measures scheme per year (£13 436/483). 71 patients seen by the repeat measurements scheme are referred onto GERS creating an annual cost of £1975.22 (£27.82*71). As we only have data for one financial year for the repeat measurements scheme, we then calculated the total average cost across the time scale of the trial (two and a half years) | |
| Training of optometrists | 2500 | The training for the revised Manchester GERS took place in 2013 and cost £2500 | |
| Fees to optometrists | 192 400 | £80 per assessment for the 2405 patients seen by accredited community optometrists | |
| Equipment costs | 48 000 | ||
| MREH non-referred cases | 254 477 | 1282 patients not referred, one first visit avoided at £114 and 1.3 follow-up visits avoided at £65 | |
| Total | 254 477 | 247 838 | |
| Savings | 6638.95 | ||
| Savings per patient | 2.76 | £6635.95/2405 patients |
*This additional GERS pathway cost is not applied in the current operation of GERS. The repeat measures pathway no longer feeds into GERS so this cost does not apply as of 2018.
GERS, Glaucoma Enhanced Referral Scheme; MREH, Manchester Royal Eye Hospital.
With advances in technology and additional guidance for clinicians it could be possible that only one outpatient visit to MREH is avoided through the Manchester GERS. Therefore, in table 2 we assume that only one outpatient visit is avoided. With this assumption the GERS is no longer cost saving and incurs a cost to the NHS of £101 690 which is approximately £42.28 per patient within the scheme.
Table 2.
Costs/savings of the Manchester GERS from April 2013 to November 2016 based on one visit before discharge
| Savings (£) | Costs (£) | Notes | |
| Cost of patients entering from the repeat measurements scheme | 4938.05 | See table 1 | |
| Training of optometrists | 2500 | The training for the relaunched Manchester GERS took place in 2013 and cost £2500 | |
| Fees to optometrists | 192 400 | £80 per assessment 2405 patients seen by community optometrists | |
| Equipment cost | 48 000 | ||
| MREH non referred cases | 146 148 | 1282 patients not referred, one visit avoided at £114 per first visit avoided | |
| Totals | 146 148 | 247 838 | |
| Savings | −101 690 | ||
| Savings per patient | −42.28 | 101 690/2405 patients |
GERS, Glaucoma Enhanced Referral Scheme; MREH, Manchester Royal Eye Hospital.
Table 3 shows the threshold value of visits before discharge to make the Manchester GERS cost neutral. Patients need to have an average of 2.22 visits to MREH prior to discharge to make the GERS scheme cost neutral.
Table 3.
Threshold value of visits before discharge to make the Manchester GERS cost neutral
| Threshold value | Patients not referred | Costs (£) | Notes |
| 101 690 | Based on one visit to MREH avoided | ||
| 65 | Cost of follow-up visit | ||
| 1282 | 1282 patients not referred to MREH due to GERS scheme | ||
| 1.22 follow-ups | £101 690/ (1282*£65) | ||
| 2.22 visits in total |
GERS, Glaucoma Enhanced Referral Scheme; MREH, Manchester Royal Eye Hospital.
Discussion
Previous research investigating the cost implications of glaucoma referral filtering schemes has found these schemes to be cost saving to the NHS. However, the previous study by Henson et al10 which analysed data from the MFT scheme based the cost analysis on a review of new referrals made to MREH in 1997. The discrepancy between the cost savings in tables 1 and 2 highlights the importance of considering the number of visits made to HES prior to discharge for false positive patients.
It is difficult to define a false positive patient. If a trained and accredited community optometrist is willing to discharge a patient to ongoing community care then it seems logical that a clinician at the MREH would also discharge that patient to community care after just one visit (based on the assumption that visual fields are performed at the first visit). However, it might be the case that once patients are within HES care clinicians may be more open to observing the patient over time to check that they are true false positives. Based on the costs presented in tables 1 and 2, the HES visits before discharge would need to be approximately 2.2 or greater to make the scheme cost saving. Using Health Episodes Statistics data on outpatient ophthalmology visits from 2010 to 2012, we found the average number of visits prior to discharge for all ophthalmology outpatient patients to be 1.57 across all trusts and 1.49 at MFT. This figure is not specific to glaucoma referrals but is lower than the threshold value calculated to make the GERS scheme cost neutral.
The cost analysis does not take into account potential capacity constraints of specialist ophthalmology services. If hospitals are unable to expand their specialist eye services due to a skill shortage it could be that the optimal way to spend NHS resources is to provide a referral filtering scheme. The filtering scheme can improve referral accuracy and provide a community service that could otherwise develop a longer hospital waiting list, even if this scheme is not cost saving.
One potential limitation with the Manchester GERS is that the patients in the scheme who are the true positives wait longer to be seen in the HES. If a patient was not participating in the scheme, they would be referred directly to the HES and seen within their time constraint (currently 14 weeks). However, through participating in the scheme, patients are instead referred to a trained and accredited community optometrist who is required to see the patient within 20 working days. The GERS optometrist will then refer the patient to MREH if they suspect glaucoma. This pathway means that patients who need to be seen by the HES could potentially be waiting an additional 20 working days prior to referral. We do not know how long patients within the scheme actually wait to be seen by a trained community optometrist. It is unlikely that the increase in capacity for MREH through not seeing false positives offsets this additional wait. To overcome this shortfall and to ensure that GERS is clinically safe, the true positives identified within the scheme are risk profiled with criteria for more urgent assessment being in place. Furthermore, a false negative evaluation of the Manchester GERS has been conducted.15 The authors followed a proportion of patients who were not referred to the HES. Of 131 patients not referred to HES by the Manchester GERS only one patient in this sample was found to be a true false negative (met the GERS referral criteria but was not referred).
Long waiting times that might rise from a high number of false positive referrals can cause disutility to patients due to: their time preference, deterioration of health while on the waiting list, and anxiety associated with waiting for treatment.16 The importance of reducing waiting times for treatment has also been highlighted by Propper,16 who used contingent valuation to estimate the disutility of time spent on a waiting list, which per week is equivalent to £19 in 2013 prices. Nikolova et al17 found that waiting time for a treatment can have a significant impact on the health outcome of that treatment. After controlling for health, the authors found that a longer waiting time has a negative and statistically significant impact on the health gain from hip and knee replacement surgery. The monetary value of the loss in the health-related quality of life for each additional week of waiting was found to be £153 per hip replacement and £149 for a knee replacement. The findings of Propper16 and Nikolova et al17 highlight the intrinsic utility that can be attached to waiting time for treatment. Therefore, a reduction in waiting times through schemes such as the Manchester GERS has the potential to improve health outcomes for patients, potentially saving the NHS money in the long term.
Conclusion
Glaucoma referral filtering schemes have the potential to alleviate the pressure facing the HES and reduce waiting times for patients. The Manchester GERS resulted in a 53% reduction in the number of false positive referrals to the MREH between April 2013 and November 2016. Reducing false positive referrals has associated benefits for both the hospital and the patient. However, introducing additional services also have a cost. Our study shows that the Manchester GERS only results in a cost saving if more than the threshold value of 2.22 visits to MREH is, on average, avoided through the scheme. This finding highlights the need for a clear and consistent cost analysis of glaucoma referral filtering schemes. A full cost and benefit analysis needs to take these wider system consequences into account.
Footnotes
Contributors: HF is the first author, who completed the analysis and prepared this paper. MS reviewed the analysis and contributed towards the content of paper. DFE planned the study, reviewed and contributed to the content of this paper. JL planned the study, reviewed and contributed to the content of this paper. AFS planned the study and contributed to the content of this paper. CF planned the study and contributed to the content of this paper. RH planned the study, collected the data, reviewed and contributed to the content of this paper.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Tham Y-C, Li X, Wong TY, et al. . Global prevalence of glaucoma and projections of glaucoma burden through 2040. Ophthalmology 2014;121:2081–90. 10.1016/j.ophtha.2014.05.013 [DOI] [PubMed] [Google Scholar]
- 2.Ratnarajan G, Newsom W, Vernon SA, et al. . The effectiveness of schemes that refine referrals between primary and secondary care--the UK experience with glaucoma referrals: the Health Innovation & Education Cluster (HIEC) Glaucoma Pathways Project. BMJ Open 2013;3:e002715 10.1136/bmjopen-2013-002715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelsey IJ, HSJ . NHS faces £30bn funding gap by 2020. Available: https://www.hsj.co.uk/news/kelsey-nhs-faces-30bn-funding-gap-by-2020/5060745.article [Accessed 2 Aug 2018].
- 4.Burr JM, Mowatt G, Hernández R, et al. . The clinical effectiveness and cost-effectiveness of screening for open angle glaucoma: a systematic review and economic evaluation. Health Technol Assess 2007;11:iii-iv, ix-x, 1-190 10.3310/hta11410 [DOI] [PubMed] [Google Scholar]
- 5.Bowling B, Chen SDM, Salmon JF. Outcomes of referrals by community optometrists to a hospital glaucoma service. Br J Ophthalmol 2005;89:1102–4. 10.1136/bjo.2004.064378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vincent SJ, Vincent RA, Shields D, et al. . Comparison of intraocular pressure measurement between rebound, non-contact and Goldmann applanation tonometry in treated glaucoma patients. Clin Exp Ophthalmol 2012;40:e163–70. 10.1111/j.1442-9071.2011.02670.x [DOI] [PubMed] [Google Scholar]
- 7.Shah S, Murdoch IE. NICE—impact on glaucoma case detection: ophthalmic and physiological optics; 2011. [DOI] [PubMed]
- 8.Davey CJ, Green C, Elliott DB. Assessment of referrals to the hospital eye service by optometrists and GPs in Bradford and Airedale. Ophthalmic Physiol Opt 2011;31:23–8. 10.1111/j.1475-1313.2010.00797.x [DOI] [PubMed] [Google Scholar]
- 9.Ratnarajan G, Newsom W, French K, et al. . The impact of glaucoma referral refinement criteria on referral to, and first-visit discharge rates from, the hospital eye service: the Health Innovation & Education Cluster (HIEC) Glaucoma Pathways project. Ophthalmic Physiol Opt 2013;33:183–9. 10.1111/opo.12029 [DOI] [PubMed] [Google Scholar]
- 10.Henson DB, Spencer AF, Harper R, et al. . Community refinement of glaucoma referrals. Eye 2003;17:21–6. 10.1038/sj.eye.6700261 [DOI] [PubMed] [Google Scholar]
- 11.Devarajan N, Williams GS, Hopes M, et al. . The Carmarthenshire glaucoma referral refinement scheme, a safe and efficient screening service. Eye 2011;25:43–9. 10.1038/eye.2010.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parkins DJ, Edgar DF. Comparison of the effectiveness of two enhanced glaucoma referral schemes. Ophthalmic Physiol Opt 2011;31:343–52. 10.1111/j.1475-1313.2011.00853.x [DOI] [PubMed] [Google Scholar]
- 13.The Royal College of Ophthalmologists Commissioning guide: glaucoma, 2016. Available: https://www.rcophth.ac.uk/wp-content/uploads/2016/06/Glaucoma-Commissioning-Guide-Long-June-2016-Final.pdf
- 14.NICE Glaucoma: diagnosis and management, 2017. Available: https://www.nice.org.uk/guidance/ng81/chapter/recommendations
- 15.Gunn PJG, Marks JR, Konstantakopoulou E, et al. . Clinical effectiveness of the Manchester glaucoma enhanced referral scheme. Br J Ophthalmol 2019;103:1066–71. 10.1136/bjophthalmol-2018-312385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Propper C. The Disutility of time spent on the United Kingdom's National health service waiting Lists. J Hum Resour 1995;30:677 10.2307/146227 [DOI] [Google Scholar]
- 17.Nikolova S, Harrison M, Sutton M. The impact of waiting time on health gains from surgery: evidence from a national patient-reported outcome dataset. Health Econ 2016;25:955–68. 10.1002/hec.3195 [DOI] [PubMed] [Google Scholar]