Summary box.
The human resource for health (HRH) in sub-Saharan Africa is neither fit for purpose, sufficient nor distributed equitably to meet the region’s universal health coverage (UHC) needs.
A regional strategy is required to replace the current inefficient, compartmentalised and ineffective approach that breeds inequity and extracontinental resource drain.
We propose a regional approach to HRH planning, needs mapping, production and distribution to meet the region’s requirement for UHC.
Introduction
The decline in child mortality by as much as 75% between 2000 and 2013 in Cape Verde, Equatorial Guinea, Eritrea and Rwanda,1 in the Africa region that is famous for its depressing health outcomes, is worthy of celebration. However, before we bring out the drums and dancers, let us deliberate over the sustainability of the gains, scale-up and expansion to the rest of sub-Saharan Africa (SSA) for implementing the Universal Health Coverage (UHC) agenda or for meeting the Sustainable Development Goal number three (SDG3). We did, but had no other choice than to suspend the euphoria. Until SSA countries crack the nut that keeps the region behind others in the prevention and containment of the issues which pose a major threat to UHC attainment in the region, all other ancillary efforts will continue to function at suboptimum level. The production, distribution and retention of the human resource for health (HRH) are at the heart of the region’s health system performance, which if addressed alongside the other health system elements such as infrastructure, medicines and financing will place the region on the right path towards UHC and SDG 3.
The shortage of skilled health workforce (HWF) and inequitable distribution of the available ones which is well acknowledged as the crux of the health inequity and the health outcomes in the region are major sources of apprehension.2–4 The pervasively inadequate human resource to meet the health needs of the population poses a great deal of anxiety about the region’s ability to realise SDG3.
Plenty yet scarce, too many yet not enough
More worrisome is the realisation that few country policy planners are paying attention to the World Health Assembly resolution 69.19 which urges the Member States to quantify and match supply with need. The World Health Report of 2006 motivated the development of a Regional Roadmap for scaling up health workforce interventions in SSA, despite which very little progress has been recorded towards meeting the region’s HRH needs.5 For example, using the minimum threshold of 2.3 doctors, nurses and midwives per 1000 population,2 3
Thirty-one SSA countries were projected to require an additional 800 000 health professionals at a cost of US$2.6 billion to meet that minimum threshold in 2015.6
The region has only filled 14.5% of its requirement for physicians and 36.7% for nurses and midwives.7
80% of SSA population are without a physician and 60% without a nurse or midwife.
Estimated demand for all cadres of health workers is escalated by 71% when one includes allied health professionals such as radiographers, laboratory technicians, psychologists and social workers, among others.8
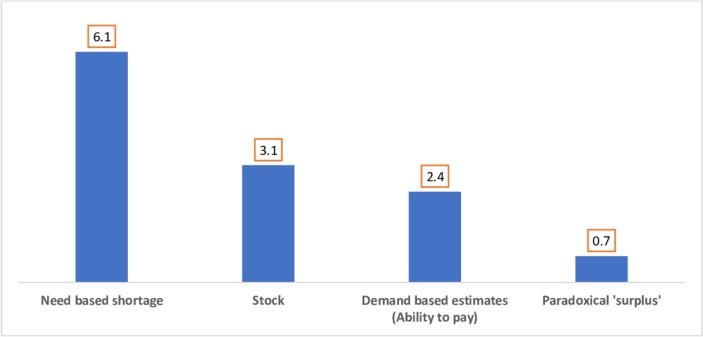
The primary employers of health professionals in SSA countries are the governments which also largely bear responsibility for HWF production. While the health personnel are grossly inadequate for the region’s health needs, the wage bill is, on the other hand, unbearably huge for most countries thus diminishing any hopes of effectively filling the HWF gaps to meet population health needs. Figure 1 indicates that although 3.1 million HWF will be available by the year 2030, financial capability for absorbing them into the workforce will be a major issue.5 9 As a result, an estimated 700 0000 skilled but paradoxically unemployed or underemployed health workers will be available in the region by 2030.
Figure 1.
Health workforce availability estimates for Africa, 2030 (million). Source: WHO Global Health Workforce Strategy—2030.
This surplus in the midst of scarcity is likely to seek employment opportunities elsewhere, most probably in North America and Europe and so further depleting the region of an already scarce resource. This provides an opportunity for developing a binding regional strategy for diffusing the ‘surplus’ across and within the region to prevent the impending extra-Africa resource flight. The strategy would build on the Africa Regional Road Map that provided policy options for countries to follow.2 We advocate a mechanism that will address the composite level of production (viz-a-viz needs), provide a standardised training curriculum, accreditation and licensing, as well as regulate the conditions of work across countries within the region. This will limit the extra-Africa drain of health workers, provide opportunity for equitable distribution of skilled personnel and enhance mobility of the HWF within the region. A regional team of experts could review the economic, political and health factors associated with the HWF flow, identify the interest groups and initiate broad partnership around the concept.
The proposed expert committee will develop an operational pathway for taking this recommendation forward. Such a multicountry partnership would develop a ground-up policy initiative where subregional health communities coalesce to make bold intervention decisions that could be implemented at country and subnational levels. At the country level, implementation would be enhanced through a peer-to-peer accountability mechanism that is monitored by regional HRH groups. To make it more binding, we propose that countries would be urged to submit the proposed strategy to their respective legislatures for ratification thereby giving it a firm legal status for implementation across countries.
Filial inequity
The strategy should address the inequitable distribution of available HWF that must be removed from the wheel of SSA’s health systems. For example, about 29% to 53% of health workers are inequitably distributed in the region where 90% of pharmacists, 86% of medical specialists, 63% of general physicians and 51% of nurses-midwives are employed in urban areas,8 leaving the remaining to be shared between small towns and the rural areas. This is an obvious threat to the UHC agenda.
Although well acknowledged as critical to planning, few attempts have yet been made to measure the extent of inequity in the health workforce distribution in SSA.4 10 The intercountry comparison that is required for planning the HWF that will deliver UHC in SSA will require regionally appropriate indicators that a regional expert committee could develop. A primary requirement is to resolve the controversy about what constitutes equity in the HRH distribution.11 The region needs an explicit definition of the criteria on which the HRH distribution would be deemed to have been fairly made.12
The region must address the traditional utilitarian population-based approach to HWF distribution,13 where majority get the most,14 in favour of leaving no one behind. In order to achieve equality, the equity and social justice component of UHC in the region must not be sacrificed.4 Planners cannot avoid differentiation in order to achieve equity and ensure horizontal and vertical distribution where similar is similarly treated and unequals are unequally treated in order to achieve UHC.15
At the heart of the equity discourse is the determination of ‘need’,11 16 which has been variously described synonymously with the degree of ill-health, in which case the most severely ill are deemed to have the greatest need. A regional mapping of needs of the communities, districts and countries with poorest health outcomes will be valuable for HRH planning. However, caution is required to avoid a subjective definition of needs by local interests which could be inimical to the UHC agenda.
In the United Republic of Tanzania and Cameroon, the HWF distributional inequities were considered as either low or high depending on how ‘need’ was defined.4 10 A set of priority indicators that serve a political interest rather than a health need will harm the equity issue. A regional consensus of experts on need definition: disease burden, child mortality, maternal mortality, immunisation coverage and others that they may decide will side-step this dilemma.
The proposed strategy should address these matters and will require the development of regional regulations regarding the production, accreditation of the various health professionals and their mobility within the region.
Conclusion
A pan-African strategy for resolving the gap in the production and equitable distribution of the HWF that will meet the needs of the UHC is required in place of an isolated and uncoordinated country-specific planning approach. The regional strategy will provide a holistic definition of health needs and mapping of needs for HWF production to deliver service that will meet those needs. It will also ensure the mobility of HWF and distribution at the various levels of need to solve the equity issue in HRH in the region. A regulatory council will be required to adopt uniform standards for the production and accreditation of various health professionals within and across countries. The existing subregional bodies are best placed to commence the pan-regional strategy for production, distribution and retention of the required HWF needs for UHC in the region.
Footnotes
Handling editor: Seye Abimbola
Contributors: JAA: conceptualised the idea, conducted the literature search and drafted the initial version of the manuscript. OBA: conceptualised the idea, conducted the literature search and drafted the initial version of the manuscript. JN: supported literature search, contributed to drafting the initial manuscript and approved the final version of the manuscript. AA: conceptualised the idea, contributed to drafting the initial manuscript and approved the final version of the manuscript. JN-O: conceptualised the idea, contributed to drafting the initial manuscript and approved the final version of the manuscript. PT: conceptualised the idea, reviewed the draft manuscript and approved the final version.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.African Union Commission, others MDG report 2012: assessing progress in Africa toward the Millennium Development Goals. Addis Adaba, 2015. [Google Scholar]
- 2.WHO Road map for scaling up the human resources for health for improved health service delivery in the African region 2012–2025. Afr Reg Off 2013. [Google Scholar]
- 3.WHO The World Health Report: 2006: working together for health, 2006. Available: http://apps.who.int/iris/handle/10665/43432 [Accessed 10 Oct 2016].
- 4.Munga MA, Maestad O. Measuring inequalities in the distribution of health workers: the case of Tanzania. Hum Resour Health 2009;7 10.1186/1478-4491-7-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu JX, Goryakin Y, Maeda A, et al. . Global health workforce labor market projections for 2030, 2016. Available: http://documents.worldbank.org/curated/en/546161470834083341/pdf/WPS7790.pdf [Accessed 29 Aug 2016].
- 6.Scheffler RM, Mahoney CB, Fulton BD, et al. . Estimates of health care professional shortages in sub-Saharan Africa by 2015. Health Aff 2009;28:w849–62. 10.1377/hlthaff.28.5.w849 [DOI] [PubMed] [Google Scholar]
- 7.WHO Equitable access to functional health workforce and community health workers in the Africa region, 2016. Available: http://www.afro.who.int/index
- 8.8 WHO/AFRO WHO Regional Office for Africa Survey on HRH Profiles, Inputs World Health Report—2006. World Health Organ Afr Reg Off, 2006. [Google Scholar]
- 9.Global strategy on human resources for health: workforce 2030 2016.
- 10.Tandi TE, Cho Y, Akam AJ-C, et al. . Cameroon public health sector: shortage and inequalities in geographic distribution of health personnel. Int J Equity Health 2015;14http://equityhealthj.biomedcentral.com/articles/ 10.1186/s12939-015-0172-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Culyer A. Equity of what in healthcare? Why the traditional answers don’t help policy—and what to do in the future. Hcpap 2007;8:12–26. 10.12927/hcpap.2007.19216 [DOI] [PubMed] [Google Scholar]
- 12.Culyer AJ, Wagstaff A. Equity and equality in health and health care. J Health Econ 1993;12:431–57http://www.sciencedirect.com/science/article/pii/016762969390004X 10.1016/0167-6296(93)90004-X [DOI] [PubMed] [Google Scholar]
- 13.Hongoro C, McPake B. How to bridge the gap in human resources for health. Lancet 2004;364:1451–6. 10.1016/S0140-6736(04)17229-2 [DOI] [PubMed] [Google Scholar]
- 14.Whitehead M. The concepts and principles of equity and health. Int J Health Serv 1992;22:429–45http://joh.sagepub.com/content/22/3/429.short 10.2190/986L-LHQ6-2VTE-YRRN [DOI] [PubMed] [Google Scholar]
- 15.Culyer AJ, Bombard Y. An equity framework for health technology assessments. Med Decis Making 2012;32:428–41. 10.1177/0272989X11426484 [DOI] [PubMed] [Google Scholar]
- 16.Culyer AJ. Need: an instrumental view : Principles of health care ethics. John Wiley & Sons, Ltd, 2006: 231–8. (accessed 19 Apr 2016). [Google Scholar]