Abstract
Introduction
A broad range of stakeholders have called for randomised evidence on the potential clinical benefits and harms of proton therapy, a type of radiation therapy, for patients with breast cancer. Radiation therapy is an important component of curative treatment, reducing cancer recurrence and extending survival. Compared with photon therapy, the international treatment standard, proton therapy reduces incidental radiation to the heart. Our overall objective is to evaluate whether the differences between proton and photon therapy cardiac radiation dose distributions lead to meaningful reductions in cardiac morbidity and mortality after treatment for breast cancer.
Methods
We are conducting a large scale, multicentre pragmatic randomised clinical trial for patients with breast cancer who will be followed longitudinally for cardiovascular morbidity and mortality, health-related quality of life and cancer control outcomes. A total of 1278 patients with non-metastatic breast cancer will be randomly allocated to receive either photon or proton therapy. The primary outcomes are major cardiovascular events, defined as myocardial infarction, coronary revascularisation, cardiovascular death or hospitalisation for unstable angina, heart failure, valvular disease, arrhythmia or pericardial disease. Secondary endpoints are urgent or unanticipated outpatient or emergency room visits for heart failure, arrhythmia, valvular disease or pericardial disease. The Radiotherapy Comparative Effectiveness (RadComp) Clinical Events Centre will conduct centralised, blinded adjudication of primary outcome events.
Ethics and dissemination
The RadComp trial has been approved by the institutional review boards of all participating sites. Recruitment began in February 2016. Current version of the protocol is A3, dated 08 November 2018. Dissemination plans include presentations at scientific conferences, scientific publications, stakeholder engagement efforts and presentation to the public via lay media outlets.
Trial registration number
Keywords: radiation oncology, clinical trials, protocols & guidelines, breast tumours
Strengths and limitations of this study.
The pragmatic and holistic approach reflects ‘real-world’ clinical practice, identifies subgroups of patients who might benefit more from proton therapy and helps patients and physicians understand and apply findings to their own lived experience.
Engagement of patients and other essential stakeholders in the design and conduct of large scale pragmatic randomised control trials of a promising, but expensive, medical technology will inform future efforts to conduct holistic, patient-centric and pragmatic comparative effectiveness research as part of a learning healthcare system.
Blinded, centralised adjudication of primary outcomes applies consistent, relevant definitions of fatal and non-fatal events comprising the major cardiovascular endpoint to detect possible events and avoids the influence of investigator or patient ascertainment bias.
The Radiotherapy Comparative Effectiveness Consortium may have the appearance of conflict of interest (COI) as it involves centres with proton therapy capabilities. COI concerns are addressed by randomised study design, blinded adjudication of primary outcome, accountability by the data safety monitoring board, and declaration, disclosure and management of COI.
Introduction
The Pragmatic Randomised Trial of Proton versus Photon Therapy for Patients with Non-Metastatic Breast Cancer: A Radiotherapy Comparative Effectiveness (RadComp) Consortium Trial is a large-scale, multicentre pragmatic randomised clinical trial following patients longitudinally for cardiovascular morbidity and mortality, health-related quality of life (HRQOL) and cancer control outcomes. We focus on radiotherapy for breast cancer requiring internal mammary nodal irradiation because: (1) regional node radiotherapy is an important component of curative treatment for high risk breast cancer; (2) the survival advantages of radiotherapy may be reduced by incidental radiation to the heart; (3) proton therapy, by reducing incidental radiation to the heart and other normal tissues, may lead to meaningful reductions in cardiac morbidity and mortality and improvements in HRQOL and (4) patients with breast cancer seek evidence on disease control, quality of life and cardiovascular outcomes after proton versus photon therapy to help make shared decisions with their physicians about treatment options.
Our primary hypothesis is that proton therapy, as part of multimodality curative treatment for patients with non-metastatic breast cancer who have indications for regional nodal irradiation, reduces major cardiovascular events (MCEs) compared with photon therapy. MCEs are defined as myocardial infarction, coronary revascularisation, cardiovascular death or hospitalisation for unstable angina, heart failure, valvular disease, arrhythmia or pericardial disease. Photon therapy, delivered as either intensity-modulated radiotherapy or three-dimensional (3D) conformal radiotherapy, uses multiple X-ray beams to irradiate a tumour target but unavoidably deposits radiation in normal tissues beyond the target volume. In contrast, proton therapy directs a beam of protons (positively charged subatomic particles) at the target volume, where they deposit the bulk of their energy in the last few millimetres of their range.1 Proton radiation dose distributions may appear superior to photon therapy, particularly in the reduction of low and intermediate radiation dose to normal tissues like the heart and lungs.
However, both photon and proton therapy have physical and biological uncertainties that could impact important clinical outcomes. For example, investigators have noted uncertainties about the exact range of the proton therapy in tissue and its biological effects at the end of the range.2 In addition, due to their distinct physical properties, there may be differences in the biological effect of proton therapy and photon therapy on normal tissues.
Thus, a broad range of stakeholders (patients, providers, manufacturers, researchers and policy-makers) have called for randomised evidence on the clinical benefits and harms of proton therapy for patients with breast cancer.3–9
Methods
Study design
This study is a superiority pragmatic randomised clinical trial in breast cancer to compare two external beam radiation therapies: proton versus photon therapy. Treatment techniques represent current care standards and are easy to replicate. Study endpoints are assessed via self-report, medical record review, vital records database search and centralised adjudication. The primary outcome is assessed by an adjudication team of cardiologists who are blinded to treatment assignment.
Informed by the work of Sedrakyan, Luce, Ellenberg and Treweek,10–14 the conceptual framework for the trial (figure 1) addresses sources of variability that are unique to radiation devices, including facility and device characteristics.
Figure 1.
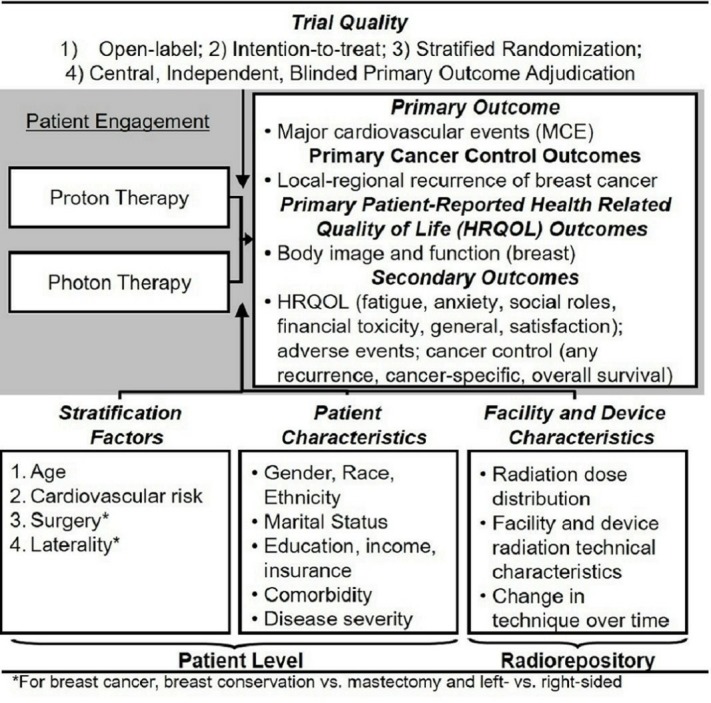
Conceptual framework for randomised pragmatic clinical trial of proton versus photon therapy for locally advanced breast: generating patient centric, real-word evidence.
The RadComp trial has in common a highly pragmatic approach in most Pragmatic Explanatory Continuum Indicator Summary domains15 (table 1). We highlight three choices essential to maintaining internal and external validity: first, the trial is open label (both the researchers and participants know which treatment is administered); however, we conduct independent, centralised primary outcome adjudication of MCEs to protect against differential misclassification between treatment groups. Second, participant eligibility is minimally restricted, without exclusions for pre-existing comorbidities, and treatment is flexible in dosing and technique; however, we provide the best practice guidelines for radiotherapy delivery, consistent with prior pragmatic clinical trials of technologically complex treatments (based on consensus among RadComp centres).16 Third, treatment decisions are at the discretion of the local treating providers and patients; however, we will store radiotherapy treatment plans within the RadComp Radiorepository for retrospective research review.
Table 1.
Key elements of the RadComp pragmatic approach to study design
| Domain | Typical explanatory RCT | RadComp Pragmatic RCT |
| Blinding | Open label | Open label |
| Participant eligibility | Highly selected (avoid diluting effect) | Little selection beyond the clinical indication for RT |
| Intervention flexibility | Standardised, inflexible treatment guidelines | Flexible treatment guidelines, promote local care standards |
| Practitioner expertise | Expert subspecialists at elite academic settings | Academic and community settings, real-world care |
| Follow-up | Frequent research visits, more extensive than routine care | Annual research visits, tied to routine care; engage patients |
| Primary outcome | Clinically meaningful, often surrogate | Clinically meaningful, patient-centric MCE and HRQOL |
| Event adjudication | Variable | Independent, blinded, centralised primary outcome adjudication |
| Adherence | Stringent for both patient and provider | Relaxed, usual care, best practice recommendations |
| Analysis | Intention to treat | Intention to treat |
| Relevance to practice | Indirect: trial design ≠ needs of stakeholders | Direct: trial design = needs of patients and stakeholders |
HRQOL, health-related quality of life; MCE, major cardiovascular event; RadComp, Radiotherapy Comparative Effectiveness; RCT, randomised controlled trial; RT, radiation therapy.
Overall aims
Aim 1 addresses the effectiveness of proton versus photon therapy in reducing MCEs. Aim 2 assesses the non-inferiority of proton versus photon therapy in reducing risk of breast cancer local-regional recurrence and in reducing risk of any recurrence, defined as the first reported breast cancer recurrence of any type (local-regional or distant recurrence or cancer-specific mortality). Aim 3 considers the effectiveness of proton versus photon therapy in improving physical, mental and social HRQOL; specifically, body image and function in breast cancer, and fatigue, anxiety, social roles, general HRQOL, side effects burden and satisfaction. Aim 4 focuses on development of predictive models to examine the associations of radiation dose distributions and MCE and HRQOL to identify subgroups of patients most likely to benefit from proton or photon therapy.
Eligibility
Eligibility criteria are defined broadly to maximise generalisability of results, striking a balance between pragmatism and treatment appropriateness (table 2). Rarely, patients will be ineligible if proton or photon therapy cannot be administered safely.
Table 2.
Summary of inclusion and exclusion criteria for the RadComp trial
| Inclusion criteria |
|
| Exclusion criteria |
|
RadComp, Radiotherapy Comparative Effectiveness.
Baseline assessments
Prior to randomisation, enrolled patients complete initial assessments that include a patient interview and medical record review to assess relevant prerandomisation covariates. Additional data regarding patient contact and alternate contacts information and baseline HRQOL are collected.
Interventions
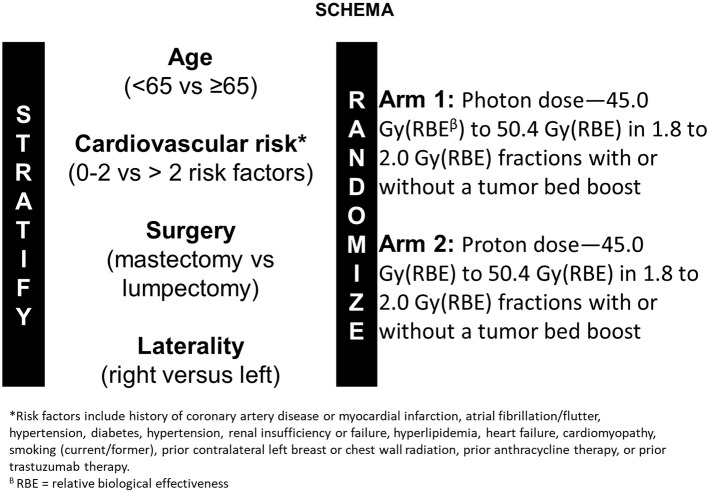
Patients are randomly assigned to receive either photon or proton therapy. Participants are stratified by age (<65 vs ≥65), cardiovascular risk (0–2 vs >2 risk factors), surgery (mastectomy vs lumpectomy) and laterality (left sided vs right sided) (figure 2). Bilateral patients are classified as left sided.
Figure 2.
Study stratification schema.
Proton therapy techniques may include passively scattered or scanning technology. All patients receive breast/chest wall and comprehensive nodal radiation therapy including internal mammary node treatment. Treatment planning guidelines are described in the protocol, available on request. A contouring atlas has been developed for guidance and is available at https://www.rtog.org/CoreLab/ContouringAtlases/RADCOMPBreastAtlas.aspx. A novel aspect of this atlas is that it can be viewed in coronal, axial and sagittal planes by treating physicians.
RadComp Radiorepository
In a technology-based medical discipline like radiation oncology, significant centre-to-centre variations exist in implementation of technologies.11 We draw a balance between allowing for local practice variation while promoting the best practice radiotherapy delivery across centres; this effort is crucial to conduct a valid, credible study, as well as to minimise the number of patients required and maximise the protection of participants.17 18 The RadComp Radiorepository collects and stores three-dimensional radiation treatment plans for all patients through the data collection infrastructure provided by The Cancer Imaging Archive (TCIA)19 20 to ensure efficiency of these processes for participating centres. Data are stored in TCIA with the approval of the National Cancer Institute (NCI), as a private collection and can be made publicly available at an appropriate time following the completion of the trial.
Centralised adjudication of primary outcomes
The RadComp Clinical Events Centre (CEC) will conduct centralised adjudication of clinical events related to the primary outcomes of MCEs. The objectives of the CEC are: (1) to apply consistent, simple, relevant definitions of the fatal and non-fatal cardiovascular events comprising the MCE endpoint to detect possible events and to avoid the influence of investigator or patient ascertainment bias and (2) to conduct adjudication blinded to treatment assignment to protect against differential misclassification events. The goal of centralised adjudication of primary outcomes is to increase confidence in the validity of our findings.21–23 Leveraging the best practice adjudication procedures from the National Lung Screening Trial24 and prior work at the University of Pennsylvania in managing large, complex clinical event adjudication programmes,25 26 the CEC employs key processes to define, identify, track, investigate and determine whether a primary event has occurred. The RadComp adjudication manual is available on request.
Outcomes, patient characteristics, and facility and device characteristics
As shown in the conceptual framework, study measures include primary outcomes (MCE), secondary outcomes, baseline stratification factors, patient characteristics and facility characteristics.
Major cardiovascular events
The primary outcome is MCE, defined as myocardial infarction, coronary revascularisation, cardiovascular death or hospitalisation for unstable angina, heart failure, valvular disease, arrhythmia, or pericardial disease.
Local-regional recurrence and any recurrence
The primary cancer control outcome is local-regional recurrence, defined as the local recurrence as a first event.27–29 We will also evaluate any recurrence, defined as the first reported breast cancer recurrence of any type (local-regional or distant recurrence or cancer-specific mortality).
Baseline cardiovascular disease
Assessed at baseline, elevated risk of cardiovascular disease is defined by a history of coronary artery disease or myocardial infarction, atrial fibrillation/flutter, hypertension, diabetes, renal failure, hyperlipidaemia, heart failure, cardiomyopathy, smoking (current/former), prior contralateral left breast or chest wall radiation, prior anthracycline therapy or prior trastuzumab therapy. We choose this approach as both valid (based on the Framingham risk score) and consistent with our pragmatic framework, acknowledging that some cardiovascular risk stratification schemes include laboratory or echocardiographic assessment.30 Other cardiovascular risk factors (including family history) will be assessed but will not contribute to the definition of cardiovascular risk factors for the purposes of stratification.
Patient characteristics
We will collect demographic information including gender, race, ethnicity, marital status, educational attainment, insurance, household income, comorbidity assessment and disease severity, leveraging the Patient-Reported Outcomes Measurement Information System (PROMIS) sociodemographic and comorbidity questionnaire.31
Facility/device characteristics and radiation dose distribution
We will investigate the relationship between proton and photon dose distribution metrics and differences in MCE and HRQOL in order to identify subgroups of patients that might benefit from proton or photon therapy. To facilitate this analysis, we will record patient-level radiation dose distributions and treatment delivery parameters, facility and device radiation technical characteristics, and any evolution of radiation techniques over time through the RadComp Radiorepository. We also will conduct centralised contouring of organs at risk, including the heart and its substructures (left anterior descending artery, left and right atria, left and right ventricles, left main, left circumflex and the right coronary artery, lungs, oesophagus and thyroid). Centralised contouring is important in any radiotherapy trial but is particularly pertinent to a pragmatic trial in which the local norms of anatomic delineation for radiation treatment planning vary widely.32 33 While patients will be treated according to anatomic delineation of local providers, centralised contouring will be conducted by trained staff at the RadComp Coordinating Centre and the results stored in the Radiorepository. Participating sites must submit a facility questionnaire, complete a physics plan review and demonstrate successful digital data submission to the Radiorepository prior to study initiation.
HRQOL instruments
The HRQOL instruments and outcomes chosen for the proposed trials are hypothesis driven, validated, reliable and have been shown to be meaningful to patients.34–37 Each instrument is described below. The estimated patient response burden to complete these instruments is approximately 30 min.
Functional Assessment of Cancer Therapy-Breast
The Functional Assessment of Cancer Therapy-Breast (FACT-B) measures general and breast cancer-specific HRQOL.38 It has multiple subscales, three of which are combined to form a Trial Outcome Index that is useful for clinical trials. It also has a four-item arm mobility subscale39 40 and two items to measure pain and swelling.
BREAST-Q
The BREAST-Q was designed to evaluate outcomes among women undergoing different types of breast surgery.41 A five-item subscale to assess adverse effects of radiotherapy will be used in this trial.
Satisfaction with breast cosmetic outcomes
This six-item scale was developed to provide a brief assessment of patient-reported cosmetic outcomes after breast cancer treatment.42
PROMIS fatigue
The four-item fatigue short form combines items on fatigue experience and interference derived from the Functional Assessment of Chronic Illness Therapy (FACIT) system and PROMIS.31 43–45 It has been used extensively in oncology trials and is responsive to change after radiation therapy.
PROMIS anxiety
Anxiety is a common concern among patients with cancer34 and is especially relevant for the RadComp trials. The PROMIS 4-item short form for Anxiety was developed based on content and psychometric measurement precision.46
PROMIS social roles
Social function has historically been a relatively neglected domain due to the lack of measures for clinical populations. A four-item PROMIS short form will be used in this trial, derived from the validated a 35-item measure of ability to participate in social roles and activities.47
This side effects short form will solicit experience, shortness of breath and chest pain. Items were selected from the NCI’s Patient-Reported Outcomes version of the Common Terminology Criteria for Adverse Events (PRO-CTCAE) system, which was developed to collect patient reports of symptoms they are experiencing while undergoing treatment, for the purpose of enhancing adverse event (AE) reporting (http://healthcaredelivery.cancer.gov/pro-ctcae/) or were written for this trial using the PRO-CTCAE format. A single item from the FACT-B will also be used to measure the overall burden of side effects (‘I am bothered by side effects of treatment: not at all, a little bit, somewhat, quite a bit, very much’), as used in prior cancer studies.48–50
Functional Assessment of Chronic Illness Therapy-Treatment Satisfaction-General
The FACIT system includes an eight-item measure of general satisfaction with treatment, developed and validated with patients with cancer and HIV/AIDS.51 Six of the eight items will be used in this trial.
Financial burden
In discussion with the stakeholder advisory committee, we included an item to assess overall financial burden. This item is part of the European Organization for Research and Treatment of Cancer QLQ-C30 instrument: ‘Has your physical condition or medical treatment caused you financial difficulties?’ (not at all, a little bit, quite a bit, very much).52
Productivity
This single item has been developed to assess the extent that a patient was able to resume normal activities. It is rated on a 0%–100% scale.53
EuroQOL-5D
The EuroQOL-5D is a standardised two-part, self-administered instrument for direct and indirect assessment of health state utilities; it is cognitively simple, takes only a few minutes to complete and yields a utilities index value for health status.54
Recruitment
All patients will be recruited in clinic settings between the time of presentation with breast cancer and prior to start of radiation therapy. Radiation oncologists at each recruiting site will assess willingness for their patients to be enrolled.
RadComp recruiting sites have been selected to represent a broad range of geographic locations and practice settings in the USA, including large teaching and non-teaching treatment centres and smaller community facilities. The site selection process for RadComp included consideration of volume of patients with breast cancer, treatment practices and presence of buy-in from clinical leaders. Over 95% of existing proton therapy treatment centres in the USA are participating in the trial.
AE monitoring
At each contact with the subject, including the pretreatment assessment, the investigator seeks information on AEs by specific questioning and, as appropriate, by examination. AEs will be recorded by clinicians using the National Cancer Institute Common Toxicity Criteria for Adverse Events (CTCAE) V.4.0, a comprehensive, multimodality grading system for reporting the acute and late effects of cancer treatment.55
Data analysis and management
Analyses for all endpoints will follow the intention-to-treat principle. As-treated analyses will be conducted for MCEs and other safety endpoints secondarily. The primary analysis will be a comparison of time to MCE between treatment arms. Log-rank tests will be used to compare the time to MCE between treatment arms; Kaplan-Meier plots will be used to graphically depict time to MCE by treatment arm. The main subgroups assessed for heterogeneity of treatment effects (HTE) within Cox models will be the stratification factors as defined in the schema. In secondary analyses, we will assess the influence of patient characteristics (gender, race, ethnicity, marital status, education, health literacy, income, insurance status, comorbidities and disease severity) and device and facility characteristics (radiation dose distribution, facility and device radiation technical characteristics, change in technique over time). To account for the presence of competing risks, we also will conduct secondary analyses of the cumulative incidence of MCE using non-parametric cumulative incidence functions. We will use the Fine-Gray semiparametric model for subdistribution hazards to estimate the effects of stratification factors and other covariates.
Initial evaluation of HTE will be made by analysis of interactions between treatment and patient-level and facility/device covariates using a Cox regression model with the primary outcome (MCE) as the dependent variable. Treatment effects within subgroups, such as ethnicity and race, will be conducted if any treatment–covariate interactions are at least suggestive (p<0.20) and sample sizes and numbers of events within these subgroups are sufficient for analysis. Due to the exploratory nature of these analyses and the expected limited sample size in each subgroup, no adjustments for multiple comparisons will be made. These analyses will follow the primary comparisons as specified for MCE.
Power and sample size
Our primary hypothesis is that treatment with proton therapy as compared with photon therapy will reduce the rate of MCEs.
The study will randomise 1278 patients to photon therapy versus proton therapy for treatment of breast cancer. The 10-year estimate of the proportion of patients with breast cancer with MCEs in the photon arm is estimated to be 6.3% based on study team analyses of data from the Surveillance Epidemiological End Results database (available on request from the authors). Assuming a 45% relative reduction of MCEs using proton therapy, resulting in an MCE rate of 3.5% for the proton arm, this sample will provide 80% power to detect this difference between the two arms using a log-rank test with a one-sided alpha of 0.05. A sample size of 1278 will allow sufficient power with a loss to follow-up rate of 13%.
The planned sample size will also provide sufficient power for testing hypotheses related to our secondary outcomes. An underlying assumption is that proton therapy will not negatively impact cancer control outcomes. This assumption is biologically plausible given similar radiation doses and biological effects of protons and photons on tumour bed targets; yet, clinical evidence is scarce. We plan to evaluate local-regional relapse, the primary cancer control outcome of interest for radiation, using a non-inferiority approach. Non-inferiority margins were evaluated based on prior studies showing improvements in local-regional relapse rates with photon therapy, relative to no radiation.28 29 With a sample size of 1278 patients, there is 80% power for a 5-year non-inferiority margin not higher than 3.8% for local-regional recurrence assuming local-regional recurrence in the photon arm of 5% at 5 years using a log-rank test with a one-sided alpha of 0.025. We will examine cancer-specific and overall survival according to methods described above for time-to-event analyses.
For HRQOL outcomes, effect sizes were estimated as the expected difference between groups at the 6-month assessment. A correlation of 0.40–0.60 between repeated measures was assumed, based on data from previous longitudinal studies of HRQOL and satisfaction in patients with cancer.56–58 An effect size of 0.33 corresponds to a clinically important difference in HRQOL outcomes.59 60 The proposed sample sizes in each treatment arm (n=650) will be sufficient to detect an effect size of 0.33 under various scenarios. For example, even with a correlation as low as 0.40, 174 patients per treatment arm will provide power of 80% at a two-sided significance level of 0.05. Adjusting for multiple primary endpoints in the breast cancer trial, 330 patients per treatment arm will provide power of 90% at a two-sided significance level of 0.01. There will be adequate statistical power even with assuming 15% drop-out.
Study monitoring
The Radiation Therapy Oncology Group Foundation data monitoring committee (DMC) will review the study twice a year with respect to patient accrual and morbidity, and at any other times on an ‘as needed’ basis. The review of the study will include, but not be limited to, the following items: accrual, baseline demographic characteristics, withdrawal rates, toxicity data, protocol compliance, treatment arm-specific data including radiation dose, toxicity and compliance, HRQOL questionnaire compliance, interim analyses of AEs and safety results and outcome analyses results. Data by treatment arm will be seen only by the DMC, which will assess the integrity of the accruing data and compare selected measures between treatment arms that may affect study validity or raise potential ethical concerns regarding safety.
Patient and public involvement
Since 2009, leaders of the RadComp Consortium have convened or participated in workgroups of patients, clinicians, methodologists, cancer researchers, payers, product developers, vendors and government representatives to explore the feasibility of alternative efficacy and effectiveness study designs and to build momentum for comparative studies of proton and photon therapy (These efforts resulted in the currently accruing NCI-sponsored efficacy PARTIQoL trial).61–63 In 2014, RadComp investigators called for randomised trial evidence generation for proton therapy in breast and lung cancer64 and the current multi-institutional RadComp Consortium of 22 proton/photon centres agreed to seek Patient-Centered Outcomes Research Institute funding for a pragmatic randomised clinical trial. In June 2014, in partnership with the NCI’s Radiation Research Branch, the Consortium hosted a stakeholder engagement meeting on the NCI campus, in which we gained important insights on the formulation of the research questions, study designs, study implementation plans and other key characteristics of comparative effectiveness research.3
We learnt from stakeholders that one essential challenge in conducting randomised trials of proton therapy is restrictive insurance coverage for proton therapy, particularly for breast cancer.65 While Medicare typically covers proton therapy for breast cancer indications, commercial insurers are more restrictive; however, reasonable clinical rationale supports coverage of radiation modalities such as intensity-modulated photon therapy or proton therapy for patients with breast cancer who require internal mammary node treatment (that is, patients with breast cancer clinically eligible for RadComp). Restrictive commercial coverage policies for proton therapy may impact the pace of enrolment to RadComp and the generalizability of the results. Therefore, RadComp engages with stakeholders to develop potential solutions to support for trial participation for eligible and interested patients.
The Stakeholder Advisory Committee and the larger stakeholder group have and will continue to participate in stakeholder deliberations. The Stakeholder Advisory Committee provides their insight on: (1) the creation of strategies to recruit and retain all patient populations, (2) developing study talking points in plain language to overcome patient confusion or fear of the concept of equipoise/uncertainty among treatment options, (3) translating study findings and (4) mechanisms for the broad dissemination and implementation of the best practices.
Ethics and dissemination
Of currently approved sites, nine have designated the University of Pennsylvania IRB as the IRB of record. Recruitment began in February 2016 and will continue through the end of 2021. Changes to the protocol will be communicated via teleconferences and memos to all sites with an expected date of implementation. Training on the changes will be documented.
Protected health information is only shared with research team members as required for completion of designated study tasks. Patient contact information for follow-up is only transmitted to the coordinating centre via secure network servers. All team members needing access to identifiable study data will be required to submit appropriate trainings and roster forms to request access. Logs of dates and times of database accessed will be kept, including an audit trail of data changes.
Conclusion
The RadComp trial will evaluate outcomes after proton or photon therapy for patients with breast cancer through a real-world, patient-centred pragmatic randomised clinical trial. RadComp’s goal is to generate new knowledge about the relative effects of these approaches while ensuring that treatment reflects high-quality routine clinical practice, identifies subgroups of patients that might benefit more from either treatment, and helps patients and physicians understand and apply our findings to their own experience. Patients with breast cancer considering photon or proton therapy make treatment decisions in the context of extremely sparse comparative effectiveness evidence, and then may live for years with clinically burdensome treatment-related morbidity that affects their quality of life and engagement in activities of living. The RadComp trial results will be directly relevant to many thousands of patients who confront these difficult treatment decisions every day.
Supplementary Material
Acknowledgments
The authors thank Tanya Alexander, Carole Baas, Joanne Buzaglo, Andrea Denicoff, Ashley Feriozzi, Dana Goodlett, Carolyn Hencek, Anna Hung, Holly Massett and Kim Wright for their contributions to the study.
Footnotes
Twitter: @theRadCompStudy
Collaborators: RadComp Consortium: Massachusetts General Hospital: David Gierga, RBJ, SMM, Harald Paganetti, Daniel Soto, AZT; Mayo Clinic, Arizona: Aman Anand, Michelle Halyard, Lisa A. McGee; Mayo Clinic, Rochester: Kimberly Corbin, RWM, Nicholas Remmes, Elizabeth Yan; MDAnderson Cancer Center: Elizabeth S. Bloom, Karen E. Hoffman, Falk Poenisch, Benjamin Smith, Xiaorong Ronald Zhu; Memorial Sloan Kettering Cancer LZB, OC, John Cuaron, Daphna Gelblum, Erin Gillespie, Linda Hong, AJK, Beryl McCormick, Borys Mychalczak, Preeti Parhar, SNP, Paul Romesser, KDS, Anne Marie Shepherd; Miami Cancer Institute: Jaafar Bennouna, Marcio A. Fagundes, Alonso Gutierrez, Jennifer Yu: Northwestern University: David Cella, CMK, Stephen Mihalcik, MP; Michael Stutz; Orlando Health: Tomas Dvorak, Omar Zeidan; Pinnacle Health: Eugene Fourkal, David C. Weksberg; ProCure NJ: Dennis Mah, Henry Tsai; ProCure Oklahoma: Jeffrey Campbell, Kiran Prabhu, Trevor Twyford; Provision Proton Center: Allen Meek, Niek Schreuder, J. Ben Wilkinson; Rutgers Cancer Institute of New Jersey: Sharad Goyal, BGH, Rihan Millevoi, Nisha Ohri; Texas Center for Proton Therapy: Chang Chang, Jared Sturgeon; University of Arkansas Medical School: William Bennett, FP, Lawrence Tarbox; University of California, San Diego: Jyoti Mayadev,Vitali Moiseenko, Dominique Rash, James Urbanic, Catheryn Yashar; University of Florida Proton Therapy Institute: Julie A. Bradley, Xiaoying Liang, Nancy Mendenhall, Michael Rutenberg: University Hospitals: Chee-Wai Cheng, Janice Lyons: University of Maryland: Katja Langen, MVM, Elizabeth Nichols; Perelman School of Medicine, University of Pennsylvania: Abigail Berman, Steven Feigenberg, GMF, James Kolker, Lilie Lin, Suneel Nagda, Ann Marie Siegal, Neil Taunk; University of Washington: LMF, Tony Wong; Washington University in St. Louis: Sasa Mutic, William Straube, Imran Zoberi; William Beaumont Hospital: Peter Chen, Xuanfeng Ding; Willis Knighton: Phuong Daniella Dang, Sanford Katz, Lane R. Rosen, Terry Wu.
Contributors: JEB, SP, KB, ABdG, WB, CC, BK, CL, H-ML, CDM, MP, FWP, SMM and OC each made substantial contributions to the conception or design of the study protocol. JEB conceived the overall study and wrote the first draft of the protocol and with HL, the first draft of this manuscript. KB, CDB, ABdG, WB, CC, EAH, H-ML, CDM, MP, FWP, SMM and OC provided critical input regarding the design of the study intervention, study outcomes and study procedures; JEB, SP and SE designed the data analysis and management plan. JEB, HL, SP, KB, WB, SE, H-ML, CDM, MP, SMM and OC revised the protocol critically for important intellectual content and approved the final version to be published. LZB, L-MF, GMF, BGH, AJK, RBJ, CK, MVM, RWM, SN, SNP, KS, AGT, JBW, SMM and OC and RadComp Consortium all contributed to the data collection. JEB, HL, SP, SE, SMM and OC agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: This work was funded through a Patient-Centered Outcomes Research Institute (PCORI) Award (PCS-1403-12804).
Disclaimer: The views, statements and opinions presented in this work are solely the responsibility of the author(s) and do not necessarily represent the views of the PCORI, its Board of Governors or Methodology Committee.
Competing interests: JEB, SE, CDM and BK report grants from PCORI, during the conduct of the study. SNP, WB, L-MF, BGH, CK, MVM, RWM, FWP, SMM and OC report grants from University of Pennsylvania subcontracts as study investigator, during the conduct of the study.
Patient consent for publication: Not required.
Ethics approval: University of Pennsylvania Perelman School of Medicine Institutional Review Board (IRB) and the IRBs or Research Ethics Boards (REBs) of 23 participating US institutions.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
RadComp (Radiotherapy Comparative Effectiveness Consortium):
David Gierga, Harald Paganetti, Daniel Soto, Aman Anand, Michele Halyard, Lisa A. McGee, Kimberly Corbin, Nicholas Remmes, Elizabeth Yan, Elizabeth S. Bloom, Karen E. Hoffman, Falk Poenisch, Benjamin Smith, Xiaorong Ronald Zhu, John Cuaron, Daphna Gelblum, Erin Gillespie, Linda Hong, Beryl McCormick, Borys Mychalczak, Preeti Parhar, Paul Romesser, Anne Marie Shepherd, Jaffa Bennouna, Marcio Fagundes, Alonso Gutierrez, Jennifer Yu, David Cella, Stephen Mihalcik, Michael Stutz, Tomas Dvorak, Omar Zeidan, Eugene Fourkal, David C. Weksberg, Dennis Mah, Henry Tsai, Jeffrey Campbell, Kiran Prabhu, Trevor Twyford, Allen Meek, Niek Schreuder, Sharad Goyal, Rihan Millevoi, Nisha Ohri, Chang Chang, Jared Sturgeon, William Bennet, Lawrence Tarbox, Jyoti Mayadev, Vitali Moiseenko, Dominique Rash, James Urbanic, Catheryn Yashar, Julie A. Bradley, Xiaoying Liang, Nancy Mendenhall, Michael Rutenberg, Chee-Wai Cheng, Janice Lyons, Katja Langen, Elizabeth Nichols, Abigail Berman, Steven Feigenberg, James Volker, Lilie Lin, Suneel Nagda, Ann Marie Siegal, Neil Taunk, Tony Wong, Sasa Music, William Straube, Imran Zoberi, Peter Chen, Xuanfeng Ding, Phuong Daniella Dang, Sanford Katz, Lane R Rosen, and Terry Wu
References
- 1. Ollendorf DA, Colby J. Proton beam therapy: ICER final evidence report Washington State Health Technology Assessment Program; 2014. http://www.hca.wa.gov/hta/Documents [Google Scholar]
- 2. Urie M, Goitein M, Wagner M. Compensating for heterogeneities in proton radiation therapy. Phys Med Biol 1984;29:553–66. 10.1088/0031-9155/29/5/008 [DOI] [PubMed] [Google Scholar]
- 3. National Academies Initial national priorities for comparative effectiveness research: report brief, 2009. Available: https://www.nap.edu/read/12648/chapter/1 [Accessed 5 Sep 2017].
- 4. Terasawa T, Dvorak T, Ip S, et al. Systematic review: charged-particle radiation therapy for cancer. Ann Intern Med 2009;151:556–65. 10.7326/0003-4819-151-8-200910200-00145 [DOI] [PubMed] [Google Scholar]
- 5. Moya del Pina B, NCI Cancer Bulliten . Proton therapy for cancer: a new technology brief, 2009. Available: http://www.cancer.gov/ncicancerbulletin/090809/page8 [Accessed 12 Nov 2009].
- 6. Centers for Medicare and Medicaid Services Potential national coverage decision topics, 2008. Available: <http://www.cms.hhs.gov/mcd/ncpc_view_document.asp?id=19>
- 7. Brada M, De Ruysscher D, Pijls-Johannesma M. Evidence for proton therapy. J Clin Oncol 2008. [DOI] [PubMed] [Google Scholar]
- 8. Lodge M, Pijls-Johannesma M, Stirk L, et al. A systematic literature review of the clinical and cost-effectiveness of hadron therapy in cancer. Radiother Oncol 2007;83:110–22. 10.1016/j.radonc.2007.04.007 [DOI] [PubMed] [Google Scholar]
- 9. Sheehan M, Timlin C, Peach K, et al. Position statement on ethics, equipoise and research on charged particle radiation therapy. J Med Ethics 2014;40:572–5. 10.1136/medethics-2012-101290 [DOI] [PubMed] [Google Scholar]
- 10. Ellenberg S. Oversight of pragmatic clinical trials. National cancer policy forum workshop. Available: http://iom.edu/Activities/Disease/NCPF/2014-FEB-24/Day%202/Session%205/28-Ellenberg-Video.aspx
- 11. Sedrakyan A, Marinac-Dabic D, Normand S-LT, et al. A framework for evidence evaluation and methodological issues in implantable device studies. Med Care 2010;48(6 Suppl):S121–S128. 10.1097/MLR.0b013e3181d991c4 [DOI] [PubMed] [Google Scholar]
- 12. Treweek S, Zwarenstein M. Making trials matter: pragmatic and explanatory trials and the problem of applicability. Trials 2009;10:37 10.1186/1745-6215-10-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Luce BR, Kramer JM, Goodman SN, et al. Rethinking randomized clinical trials for comparative effectiveness research: the need for transformational change. Ann Intern Med 2009;151:206–9. 10.7326/0003-4819-151-3-200908040-00126 [DOI] [PubMed] [Google Scholar]
- 14. Ellenberg SS, Foulkes MA. The utility of large, simple trials in the evaluation of AIDS treatment strategies. Stat Med 1994;13:405–15. 10.1002/sim.4780130505 [DOI] [PubMed] [Google Scholar]
- 15. Thorpe KE, Zwarenstein M, Oxman AD, et al. A pragmatic-explanatory continuum indicator summary (Precis): a tool to help trial designers. J Clin Epidemiol 2009;62:464–75. 10.1016/j.jclinepi.2008.12.011 [DOI] [PubMed] [Google Scholar]
- 16. Prospective multicenter imaging study for evaluation of chest pain (promise), 2014. Available: http://projectreporter.nih.gov/project_info_description.cfm?aid=7940886&icde=5559996 [Accessed 5 Mar 2014]. [DOI] [PMC free article] [PubMed]
- 17. Bekelman J, Deye J, Vikram B. 2011. Redesigning Radiotherapy Quality Assurance: Opportunities to Develop an Efficient, Evidence-Based System to Support Clinical Trials. [DOI] [PMC free article] [PubMed]
- 18. Pettersen MN, Aird E, Olsen DR. Quality assurance of dosimetry and the impact on sample size in randomized clinical trials. Radiother Oncol 2008;86:195–9. 10.1016/j.radonc.2007.07.001 [DOI] [PubMed] [Google Scholar]
- 19. Clark K, Vendt B, Smith K, et al. The cancer imaging Archive (TCIA): maintaining and operating a public information Repository. J Digit Imaging 2013;26:1045–57. 10.1007/s10278-013-9622-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kalpathy-Cramer J, Freymann JB, Kirby JS, et al. Quantitative imaging network: data sharing and competitive AlgorithmValidation Leveraging the cancer imaging Archive. Transl Oncol 2014;7:147–52. 10.1593/tlo.13862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Granger CB, Vogel V, Cummings SR, et al. Do we need to adjudicate major clinical events? Clin Trials 2008;5:56–60. 10.1177/1740774507087972 [DOI] [PubMed] [Google Scholar]
- 22. Bolland MJ, Barber A, Doughty RN, et al. Differences between self-reported and verified adverse cardiovascular events in a randomised clinical trial. BMJ Open 2013;3:e002334 10.1136/bmjopen-2012-002334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dechartres A, Boutron I, Roy C, et al. Inadequate planning and reporting of adjudication committees in clinical trials: recommendation proposal. J Clin Epidemiol 2009;62:695–702. 10.1016/j.jclinepi.2008.09.011 [DOI] [PubMed] [Google Scholar]
- 24. Marcus PM, Gareen IF, Miller AB, et al. The National lung screening trial's endpoint verification process: determining the cause of death. Contemp Clin Trials 2011;32:834–40. 10.1016/j.cct.2011.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Feldman HI, Appel LJ, Chertow GM, et al. The chronic renal insufficiency cohort (CRIC) study: design and methods. J Am Soc Nephrol 2003;14(7 Suppl 2):148S–53. 10.1097/01.ASN.0000070149.78399.CE [DOI] [PubMed] [Google Scholar]
- 26. Bild DE, Bluemke DA, Burke GL, et al. Multi-Ethnic study of atherosclerosis: objectives and design. Am J Epidemiol 2002;156:871–81. 10.1093/aje/kwf113 [DOI] [PubMed] [Google Scholar]
- 27. Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 2005;366:2087–106. 10.1016/S0140-6736(05)67887-7 [DOI] [PubMed] [Google Scholar]
- 28. Darby S, McGale P, Correa C, et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 2011;378:1707–16. 10.1016/S0140-6736(11)61629-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. McGale P, Taylor C, Correa C, et al. Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet 2014;383:2127–35. 10.1016/S0140-6736(14)60488-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. D'Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham heart study. Circulation 2008;117:743–53. 10.1161/CIRCULATIONAHA.107.699579 [DOI] [PubMed] [Google Scholar]
- 31. Cella D, Riley W, Stone A, et al. The patient-reported outcomes measurement information system (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol 2010;63:1179–94. 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Li XA, Tai A, Arthur DW, et al. Variability of target and normal structure delineation for breast cancer radiotherapy: an RTOG multi-institutional and multiobserver study. Int J Radiat Oncol Biol Phys 2009;73:944–51. 10.1016/j.ijrobp.2008.10.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Spoelstra FOB, Senan S, Le Péchoux C, et al. Variations in target volume definition for postoperative radiotherapy in stage III Non–Small-Cell lung cancer: analysis of an international contouring study. Int J Radiat Oncol Biol Phys 2010;76:1106–13. 10.1016/j.ijrobp.2009.02.072 [DOI] [PubMed] [Google Scholar]
- 34. Reeve BB, Mitchell SA, Dueck AC, et al. Recommended patient-reported core set of symptoms to measure in adult cancer treatment trials. J Natl Cancer Inst 2014;106 10.1093/jnci/dju129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Basch E, Abernethy AP, Mullins CD, et al. Recommendations for incorporating patient-reported outcomes into clinical comparative effectiveness research in adult oncology. J Clin Oncol 2012;30:4249–55. 10.1200/JCO.2012.42.5967 [DOI] [PubMed] [Google Scholar]
- 36. DeWalt DA, Rothrock N, Yount S, et al. Evaluation of item candidates: the PROMIS qualitative item review. Med Care 2007;45(5 Suppl 1):S12–21. 10.1097/01.mlr.0000254567.79743.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Aaronson N, Alonso J, Burnam A, et al. Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res 2002;11:193–205. 10.1023/A:1015291021312 [DOI] [PubMed] [Google Scholar]
- 38. Brady MJ, Cella DF, Mo F, et al. Reliability and validity of the functional assessment of cancer Therapy-Breast quality-of-life instrument. J Clin Oncol 1997;15:974–86. 10.1200/JCO.1997.15.3.974 [DOI] [PubMed] [Google Scholar]
- 39. Coster S, Poole K, Fallowfield LJ. The validation of a quality of life scale to assess the impact of arm morbidity in breast cancer patients post-operatively. Breast Cancer Res Treat 2001;68:273–82. 10.1023/A:1012278023233 [DOI] [PubMed] [Google Scholar]
- 40. Fleissig A, Fallowfield LJ, Langridge CI, et al. Post-Operative arm morbidity and quality of life. Results of the ALMANAC randomised trial comparing sentinel node biopsy with standard axillary treatment in the management of patients with early breast cancer. Breast Cancer Res Treat 2006;95:279–93. 10.1007/s10549-005-9025-7 [DOI] [PubMed] [Google Scholar]
- 41. Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg 2009;124:345–53. 10.1097/PRS.0b013e3181aee807 [DOI] [PubMed] [Google Scholar]
- 42. Jagsi R, Li Y, Morrow M, et al. Patient-Reported quality of life and satisfaction with cosmetic outcomes after breast conservation and mastectomy with and without reconstruction. Ann Surg 2015;261:1198–206. 10.1097/SLA.0000000000000908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Garcia SF, Cella D, Clauser SB, et al. Standardizing patient-reported outcomes assessment in cancer clinical trials: a patient-reported outcomes measurement information system initiative. JCO 2007;25:5106–12. 10.1200/JCO.2007.12.2341 [DOI] [PubMed] [Google Scholar]
- 44. Butt Z, Lai J-shei, Rao D, et al. Measurement of fatigue in cancer, stroke, and HIV using the functional assessment of chronic illness therapy — fatigue (FACIT-F) scale. J Psychosom Res 2013;74:64–8. 10.1016/j.jpsychores.2012.10.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cella D, Lai J-S, Stone A. Self-reported fatigue: one dimension or more? Lessons from the Functional Assessment of Chronic Illness Therapy--Fatigue (FACIT-F) questionnaire. Support Care Cancer 2011;19:1441–50. 10.1007/s00520-010-0971-1 [DOI] [PubMed] [Google Scholar]
- 46. Pilkonis PA, Choi SW, Reise SP, et al. Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIS®): depression, anxiety, and anger. Assessment 2011;18:263–83. 10.1177/1073191111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Hahn EA, DeWalt DA, Bode RK, et al. New English and Spanish social health measures will facilitate evaluating health determinants. Health Psychol 2014;33:490–9. 10.1037/hea0000055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cella DF, Patel JD. Improving health-related quality of life in non-small-cell lung cancer with current treatment options. Clin Lung Cancer 2008;9:206–12. 10.3816/CLC.2008.n.030 [DOI] [PubMed] [Google Scholar]
- 49. Cella D, Escudier B, Rini B, et al. Patient-Reported outcomes for axitinib vs sorafenib in metastatic renal cell carcinoma: phase III (axis) trial. Br J Cancer 2013;108:1571–8. 10.1038/bjc.2013.145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Österborg A, Brandberg Y, Molostova V, et al. Randomized, double-blind, placebo-controlled trial of recombinant human erythropoietin, epoetin beta, in hematologic malignancies. JCO 2002;20:2486–94. 10.1200/JCO.2002.08.131 [DOI] [PubMed] [Google Scholar]
- 51. Peipert JD, Beaumont JL, Bode R, et al. Development and validation of the functional assessment of chronic illness therapy treatment satisfaction (FACIT Ts) measures. Quality of Life Research 2014;23:815–24. 10.1007/s11136-013-0520-8 [DOI] [PubMed] [Google Scholar]
- 52. Aaronson NK, Ahmedzai S, Bergman B, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365–76. 10.1093/jnci/85.5.365 [DOI] [PubMed] [Google Scholar]
- 53. Kornblith AB, Huang HQ, Walker JL, et al. Quality of life of patients with endometrial cancer undergoing laparoscopic International Federation of gynecology and obstetrics staging compared with laparotomy: a gynecologic Oncology Group study. JCO 2009;27:5337–42. 10.1200/JCO.2009.22.3529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Pickard AS, Wilke CT, Lin H-W, et al. Health utilities using the EQ-5D in studies of cancer. Pharmacoeconomics 2007;25:365–84. 10.2165/00019053-200725050-00002 [DOI] [PubMed] [Google Scholar]
- 55. NIH Cancer therapy evaluation program. Available: http://ctep.cancer.gov
- 56. Hahn EA, Glendenning GA, Sorensen MV, et al. Quality of life in patients with newly diagnosed chronic phase chronic myeloid leukemia on imatinib versus interferon alfa plus low-dose cytarabine: results from the iris study. JCO 2003;21:2138–46. 10.1200/JCO.2003.12.154 [DOI] [PubMed] [Google Scholar]
- 57. Cella D, Hahn E, Webster K, et al. The FACIT treatment satisfaction measurement system. Quality of Life Research 2003;12. [Google Scholar]
- 58. Fairclough D. Design and analysis of quality of life studies in clinical trials. 2nd ed Boca Raton, FL: Chapman & Hall/CRC, 2010. [Google Scholar]
- 59. Webster K, Cella D, Yost K. The functional assessment of chronic illness therapy (FACIT) measurement system: properties, applications, and interpretation. Health Qual Life Outcomes 2003;1:79 10.1186/1477-7525-1-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Yost KJ, Eton DT. Combining distribution- and anchor-based approaches to determine minimally important differences: the FACIT experience. Eval Health Prof 2005;28:172–91. 10.1177/0163278705275340 [DOI] [PubMed] [Google Scholar]
- 61. Proposed study of proton beam and intensity modulated radiation therapy (IMRT) in the treatment of prostate cancer, agency for healthcare research and quality. Rockville, MD; 2008. [Google Scholar]
- 62. Comparative effectiveness of proton therapy and IMRT. Philadelphia, PA: University of Pennsylvania; 2008. [Google Scholar]
- 63. Comparative effectiveness of proton beam versus intensity modulated radiation therapy for treatment of early stage prostate cancer. Baltimore, MD: Maryland room, world trade Center; 2009. [Google Scholar]
- 64. Bekelman JE, Hahn SM. Reference pricing with evidence development: a way forward for proton therapy. J Clin Oncol 2014;32:1540–2. 10.1200/JCO.2014.55.6613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Bekelman JE, Denicoff A, Buchsbaum J. Randomized trials of proton therapy: why they are at risk, proposed solutions, and implications for evaluating advanced technologies to diagnose and treat cancer. J Clin Oncol 2018;36:2461–4. 10.1200/JCO.2018.77.7078 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.