Abstract
Background/Aims
The expense associated with using non-combustible nicotine products as an alternative to smoking may deter smoking reduction or cessation. This study aimed to estimate (i) how much adults in England spend each week on smoking and alternative nicotine products and (ii) the potential cost saving that could be achieved by switching from smoking to using an alternative nicotine delivery product.
Design/Setting
Data came from September to November 2018 waves of the Smoking Toolkit Study, a series of national household surveys of the adult population in England.
Participants
A total of 859 adults (≥16 years) who reported current smoking or current use of an alternative nicotine product.
Measurements
Participants reported their average weekly expenditure on smoking and alternative nicotine products (nicotine replacement therapy (NRT) or e-cigarettes).
Findings
Current smokers who did not use any alternative nicotine delivery products (n=602) reported spending on average £23.09 (95%CI £21.64-24.54) on smoking each week. Ex-smokers who used alternative nicotine products (n=91) reported spending on average £8.59 (95% CI £6.80-10.39) on these products each week; £8.03 (95%CI £6.03-10.03) on e-cigarettes and £10.05 (95%CI £5.62-14.47) on NRT. People who both smoked and used alternative nicotine products (dual users, n=166) spent on average £24.54 (95%CI £21.78-27.29) on smoking and £7.49 (95%CI £6.00-8.99) on alternative nicotine products each week. Expenditure on smoking was higher among heavier, more addicted smokers and lower among those with routine/manual occupations, non-daily smokers, and roll-your-own tobacco users. Expenditure on e-cigarettes was higher among men, users from central and southern vs. northern England, and smokers who had tried to quit in the past year, and lower among current smokers. Expenditure on NRT was lower among roll-your-own tobacco users.
Conclusions
In England, expenditure among e-cigarette and NRT users is approximately one third of the expenditure of smokers. The average smoker may save an estimated £15 per week by switching completely to e-cigarettes or £13 per week by switching to NRT, although this is likely to differ according to individual usage patterns.
Introduction
The majority of smokers want to quit (1). While concern for health is typically the primary motive, around a third of smokers also cite cost as an important reason for quitting (2). Many smokers try to quit each year (3,4), but the addictive properties of nicotine and other tobacco constituents make it difficult to remain abstinent (5). In an effort to increase their chances of success, many smokers use alternative nicotine delivery products, such as e-cigarettes and nicotine replacement therapy (NRT), to support quit attempts or to reduce the amount they smoke. This raises the question as to how much of a cost saving might be achieved. In this study, we aimed to examine self-reported expenditure on two popular categories of nicotine delivery product, e-cigarettes and medically licensed NRT, and a category growing in popularity, heated tobacco products, in relation to expenditure on smoking.
After a period of rapid growth in prevalence of e-cigarette use (‘vaping’) from 2011 to 2014, e-cigarettes are now used by around 2.6 million people in England (20% of smokers) and in over one third (31.9%) of quit attempts (6,7). Evidence from two randomised controlled trials (RCTs) indicates that using e-cigarettes compared with placebo promotes smoking cessation (8). Some governmental and medical organisations believe in the potential public health benefit of smokers switching to e-cigarettes and have made various recommendations to maximise this potential, including that health professionals should support smokers who want to use an e-cigarette to help them quit smoking (9,10). While the prevalence of e-cigarette use in England has remained fairly stable since late 2013, use among long-term ex-smokers (those who have been abstinent for >1 year) has continued to rise (6). As such, any financial benefits associated with stopping smoking may be partially or fully offset by ongoing costs associated with e-cigarette use (e.g. buying e-liquid and components) (11). Previous studies have estimated the monthly cost of using e-cigarettes to be in the region of USD $40-60 (12–14). To our knowledge there is no high-quality, population-based evidence on expenditure on e-cigarettes in England.
Traditional licensed NRT products also remain a popular option for supporting quit attempts, used by 22.3% of smokers attempting to quit (6). RCT evidence indicates that use of any licensed form of NRT in a quit attempt increases the rate of success compared with placebo by 50-60% (15). While NRT can be obtained free of charge on prescription from a prescribing healthcare professional or stop smoking service, all forms are readily available in England to buy over-the-counter, and around three-quarters of people who use NRT report buying it (16). NRT is typically used for a shorter duration than e-cigarettes so it is possible that a higher expenditure on NRT would be tolerated by smokers with a longer-term goal of reducing their expenditure on smoking and nicotine products to zero.
The recent and rapid growth in the e-cigarette market has created interest in the development of other novel nicotine products. Major tobacco companies Philip Morris International and British American Tobacco have recently launched heated tobacco products (IQOS and glo, respectively), also referred to as “heat-not-burn” tobacco products, into the UK market. Heated tobacco products are electronic devices that heat rather than combust processed tobacco and claim to deliver an aerosol with fewer toxicants than in cigarette smoke (17), although there is currently no non-industry evidence that heated tobacco products are safer than combustible tobacco (10,18). These products aim for a niche between combustible tobacco smoking and e-cigarettes. Many e-cigarette users have already accepted the notion that non-combustible devices are safer than conventional cigarettes (19) and may see heated tobacco products as offering authentic tobacco taste with lower risk to health. Smokers who are reluctant to try e-cigarettes may be willing to try heated tobacco products, but how the cost of using these products compares to cigarette smoking is not known.
It is well-established from studies across high-income countries that most smokers use strategies to reduce the cost of smoking (20–25), such as cutting down cigarette consumption, switching to a lower priced brand, switching to roll-your-own (RYO) tobacco, reducing the amount of tobacco rolled in RYO cigarettes, or evading or avoiding tobacco taxation. Much less is known about the use of cost-mitigating strategies for alternative nicotine products, but there is a clear necessity to ask directly for estimates rather relying on prices and consumption.
This study sought to quantify average self-reported weekly expenditure on smoking (cigarettes or tobacco), e-cigarettes, licensed NRT products (gum, lozenge, patch, inhaler/inhalator, mouth or nasal spray), and heated tobacco products among adults (≥16 years) in England who use these products.
Specifically, we aimed to address the following research questions:
How much do adults in England spend each week on average on smoking and alternative nicotine delivery products (overall, and separately for e-cigarettes, NRT and heated tobacco products)?
What is the potential cost saving that could be achieved by switching completely from smoking to using an alternative nicotine delivery product?
Among all users, to what extent does spending on these products differ according to sociodemographic characteristics?
Among past-year smokers who use these products, to what extent does spending on these products differ according to smoking characteristics, after adjustment for sociodemographic variables?
Method
Design
Data were drawn from the ongoing Smoking Toolkit Study, a monthly cross-sectional survey of a representative sample of adults (≥16 years) in England designed to provide insights into population-wide influences on smoking and cessation by monitoring trends on a range of variables relating to smoking (26). The study uses a form of random location sampling to select a new sample of approximately 1,700 adults aged ≥16 years each month. The survey typically covers 200-300 census output areas each wave, which are sampled at random (after stratification by geo-demographic analysis of the population) from more than 170,000. Interviewers travel to the selected areas and perform computer-assisted interviews with one participant aged over 16 per household until quotas based upon factors influencing the probability of being at home (working status, age and gender) are fulfilled. Random location sampling is considered superior to conventional quota sampling because the choice of properties approached is reduced by the random allocation of small output areas. However, interviewers can still choose which houses within these areas are most likely to fulfil their quotes, rather than being sent to specific households in advance. Response rates are therefore not appropriate to record, unlike random probability sampling, where interviewers have no choice as to the properties sampled and so response at each address can be recorded. Comparisons with national data indicate that key variables including sociodemographics and smoking prevalence are nationally representative (26).
For the present study, we used aggregated data from respondents between September and November 2018, as these were the only available waves to ask about spending on alternative nicotine delivery products.
Population
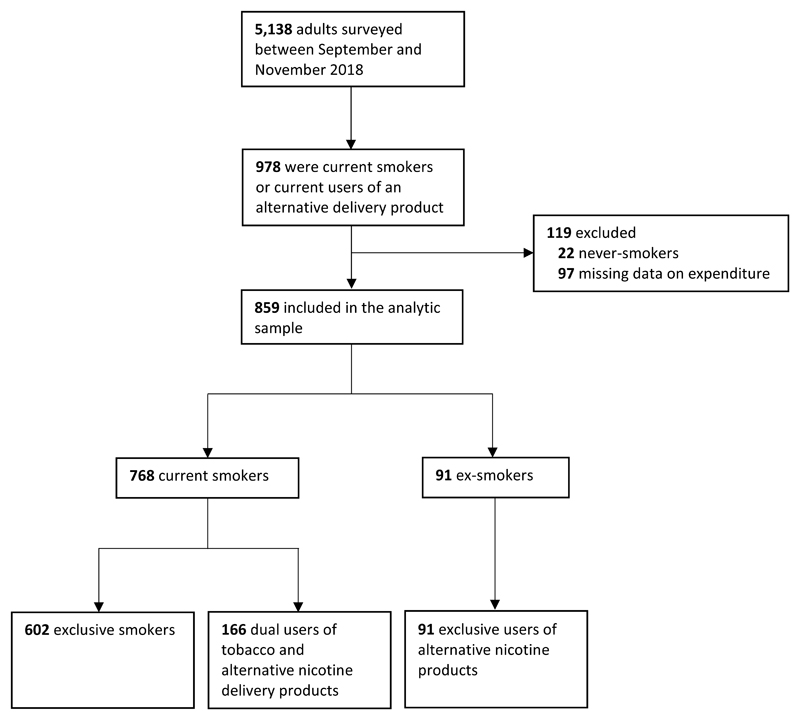
We used data from respondents in the September to November 2018 waves of the Smoking Toolkit Study who (i) reported smoking cigarettes (including hand-rolled, but excluding e-cigarettes) or other forms of tobacco (e.g. pipe or cigar) daily or occasionally at the time of the survey (‘current smokers’), and/or reported current use of (ii) e-cigarettes, (iii) any licensed NRT product (gum, lozenge, patch, inhaler/inhalator, or mouthspray) or (iv) heated tobacco products. We excluded never-smokers and those with missing data on expenditure. Figure 1 summarises the breakdown of the sample according to smoking status and use of alternative nicotine delivery products.
Figure 1.
Summary of sample selection process
Measures
Expenditure on smoking and alternative nicotine delivery products
Weekly expenditure on smoking was assessed in current smokers with the question: “On average about how much per week do you think you spend on cigarettes or tobacco?” Weekly expenditure on alternative nicotine delivery products was assessed in current users with the question: “On average about how much per week do you think you spend on using this nicotine replacement product or products?” This question followed the assessment of current use of e-cigarettes, NRT, and heated tobacco products and referred to the product(s) the respondent had reported using. Responses to both items were given to the nearest pound. Because the item on expenditure on alternative nicotine delivery products did not differentiate between the product groups, we analysed expenditure overall, and among exclusive users of e-cigarettes and NRT. We had also intended to analyse heated tobacco products and Juul, an e-cigarette product growing rapidly in popularity in the US which has recently been introduced to the UK market, but we did not have sufficient data; our sample included just one heated tobacco product user and two Juul users.
Sociodemographic characteristics
We included data on age, sex, ethnicity (dichotomised to white vs. non-white because of the small number of participants from ethnic minority groups [n=95]), social grade (dichotomised to ABC1, which includes managerial, professional and intermediate occupations, vs. C2DE, which includes small employers and own-account workers, lower supervisory and technical occupations, and semi-routine and routine occupations, never workers and long-term unemployed) and region (Government Office Region grouped into three categories: northern, central and southern England).
Smoking characteristics
Smoking characteristics assessed included current smoking status, the number of cigarettes smoked per day, daily vs. non-daily smoking, use of RYO vs. factory-made cigarettes, time to first cigarette (more than 60 minutes/30-60 minutes/6-30 minutes/within 5 minutes), and past-year quit attempts (any vs. none).
Statistical analysis
The analysis plan was pre-registered on Open Science Framework (https://osf.io/r4hfc/). All analyses were conducted using SPSS v.25, with the exception of the Bayes factors which were calculated using R.
We estimated expenditure on smoking, alternative nicotine delivery products (e-cigarettes/NRT/heated tobacco products combined), e-cigarettes, and NRT using descriptive statistics.
We used multiple linear regression models (ordinary least squares) to test independent associations between sociodemographic and smoking characteristics and expenditure on (i) smoking among current smokers, and (ii) all alternative nicotine delivery products, (iii) e-cigarettes, and (iv) NRT among current users of these alternative nicotine delivery products. For expenditure on smoking, we ran one model that included sociodemographics (age, sex, ethnicity, social grade, dummy-coded region) and smoking characteristics (exclusive smoking vs. dual use of tobacco and alternative nicotine delivery products, number of cigarettes smoked per day, non-daily smoking, RYO use, time to first cigarette, past-year quit attempts). For expenditure on alternative nicotine delivery products, we ran two models for each of the spending outcome variables: the first examined independent associations with sociodemographic characteristics and current smoking status (i.e. exclusive use of alternative nicotine delivery products vs. dual use) in the full available sample; the second examined independent associations with smoking characteristics in past-year smokers, after adjustment for sociodemographic variables. There was no substantial multicollinearity.
In a deviation from our pre-registered analysis plan, we ran the regression models with a log transformation applied to our outcome variables to normalise the skewed distributions. Results using untransformed (raw) data are provided in Supplementary Tables for transparency.
In order to aid interpretation of the strength of the observed associations in our primary analyses, we calculated Bayes factors (BFs) to differentiate between evidence for an effect, evidence for no effect, and data insensitivity (27,28). Because we expected differences in expenditure to be considerably smaller than the maximum possible difference (i.e. it was not feasible that mean expenditure on alternative nicotine would be 100% lower than mean expenditure on smoking), we used a half-Cauchy distribution with estimated effect sizes based on Cauchy priors (29), which we calculated as the observed mean of the dependent variable divided by 7 (because the rough maximum implied by a Cauchy is 7 times its scale factor (30)) for binary independent variables, divided by the number of scale points (to get the maximum expected slope) for independent variables with a fixed number of scale points (e.g. time to first cigarette), or divided by the observed mean of the independent variable for open-ended scale independent variables (e.g. number of cigarettes smoked per day). BFs ≥3 can be interpreted as evidence for the alternative hypothesis (and against the null), BFs ≤1/3 as evidence for the null hypothesis, and BFs between 1/3 and 3 suggest the data are insensitive to distinguish the alternative hypothesis from the null (27,31).
Results
A flowchart of the sample selection process is shown in Figure 1. There were 5,138 respondents to the survey between September and November 2018, of whom 978 reported current smoking or current use of an alternative nicotine delivery product. We excluded 22 never-smokers and 97 current or ex-smokers with missing data on expenditure (of whom 83 were smokers, 43 were e-cigarette users, and 25 were NRT users), resulting in our analytic sample of 859 respondents. Of the analysed sample, 768 (89.4%) were current smokers and 91 (10.6%) were ex-smokers; 257 (29.9%) used alternative nicotine delivery products. There were 602 (70.1%) exclusive smokers, 91 (10.6%) exclusive users of alternative nicotine delivery products (all ex-smokers), and 166 (19.3%) dual users. The majority (n=235, 91.4%) of respondents who used alternative nicotine delivery products reported use of just one product category, 22 (8.6%) used two products. Table 1 summarises sociodemographic and smoking characteristics in relation to product use.
Table 1. Sample characteristics.
| Smokers | Alternative nicotine users | E-cigarette users1 | NRT users1 | |
|---|---|---|---|---|
| Sociodemographic characteristics (whole sample) | ||||
| n | 768 | 257 | 156 | 79 |
| Age, mean (SD) | 42.67 (17.39) | 43.35 (16.77) | 43.15 (16.98) | 44.26 (16.81) |
| Female sex, % (n) | 47.7 (366) | 42.8 (110) | 40.4 (63) | 48.1 (38) |
| White ethnicity, % (n) | 88.2 (674) | 89.1 (228) | 89.0 (138) | 91.1 (72) |
| Social grade C2DE, % (n) | 57.3 (440) | 46.7 (120) | 41.7 (65) | 51.9 (41) |
| Region, % (n) | ||||
| North | 32.9 (253) | 35.4 (91) | 39.7 (62) | 25.3 (20) |
| Central | 33.5 (257) | 29.6 (76) | 29.5 (46) | 31.6 (25) |
| South | 33.6 (258) | 35.0 (90) | 30.8 (48) | 43.0 (34) |
| Dual use of tobacco and alternative nicotine products, % (n) | 21.6 (166) | 64.6 (166) | 57.1 (89) | 72.2 (57) |
| Smoking characteristics (past-year smokers) | ||||
| n | 768 | 179 | 99 | 60 |
| Cigarettes per day, mean (SD) | 10.32 (7.62) | 10.50 (8.17) | 9.57 (6.96) | 11.51 (9.77) |
| Non-daily smoker, % (n) | 7.2 (55) | 4.5 (8) | 8.1 (8) | 0 (0) |
| Predominant RYO use2, % (n) | 47.1 (362) | 31.5 (81) | 31.4 (49) | 30.4 (24) |
| Time to first cigarette, % (n) | ||||
| More than 60 minutes | 36.1 (277) | 29.6 (53) | 34.3 (34) | 26.7 (16) |
| 30-60 minutes | 18.9 (145) | 21.8 (39) | 20.2 (20) | 21.7 (13) |
| 6-30 minutes | 31.3 (240) | 34.1 (61) | 34.3 (34) | 33.3 (20) |
| Within 5 minutes | 13.7 (105) | 14.5 (26) | 11.1 (11) | 18.3 (11) |
| Tried to quit in past year, % (n) | 26.5 (200) | 53.1 (95) | 52.5 (52) | 51.7 (31) |
Excludes individuals who reported using any other form of alternative nicotine.
RYO = roll-your-own cigarettes.
Note: There was a small amount of missing data for some variables so numbers do not always sum to the total sample size. Valid percentages are shown for ease of interpretation.
Table 2 presents descriptive statistics on (untransformed) weekly expenditure on smoking and alternative nicotine delivery products among all users, exclusive users, and dual users. Log-transformed descriptive data are provided in Supplementary Table 1. Overall, smokers reported spending on average £23.40 on smoking each week. Individuals who used any alternative nicotine delivery product spent on average £7.88 on these products each week. Those who used e-cigarettes spent £7.60 and NRT users £8.15.
Table 2. Descriptive statistics on weekly expenditure (in £) on smoking and alternative nicotine delivery products among all users, exclusive users and dual users.
| n | Mean | SD | Lower CI | Upper CI | Median | Minimum | Maximum | |
|---|---|---|---|---|---|---|---|---|
| Expenditure on smoking | ||||||||
| All smokers | 768 | 23.40 | 18.09 | 22.12 | 24.68 | 20.00 | 1.00 | 99.00 |
| Exclusive smokers | 602 | 23.09 | 18.13 | 21.64 | 24.54 | 20.00 | 1.00 | 99.00 |
| Dual users of tobacco and alternative nicotine | 166 | 24.54 | 17.96 | 21.78 | 27.29 | 20.00 | 1.00 | 80.00 |
| Expenditure on alternative nicotine products1 | ||||||||
| All alternative nicotine users | 257 | 7.88 | 9.36 | 6.73 | 9.03 | 5.00 | 1.00 | 70.00 |
| Exclusive alternative nicotine users | 91 | 8.59 | 8.60 | 6.80 | 10.39 | 6.00 | 1.00 | 50.00 |
| Dual users of alternative nicotine and tobacco | 166 | 7.49 | 9.75 | 6.00 | 8.99 | 5.00 | 1.00 | 70.00 |
| Expenditure on e-cigarettes2 | ||||||||
| All e-cigarette users | 156 | 7.60 | 9.21 | 6.14 | 9.06 | 5.00 | 1.00 | 70.00 |
| Exclusive e-cigarettes users | 67 | 8.03 | 8.22 | 6.03 | 10.03 | 5.00 | 1.00 | 50.00 |
| Dual users of e-cigarettes and tobacco | 89 | 7.28 | 9.93 | 5.19 | 9.37 | 5.00 | 1.00 | 70.00 |
| Expenditure on NRT2 | ||||||||
| All NRT users | 79 | 8.15 | 10.06 | 5.90 | 10.41 | 5.00 | 1.00 | 60.00 |
| Exclusive NRT users | 22 | 10.05 | 9.99 | 5.62 | 14.47 | 7.50 | 1.00 | 40.00 |
| Dual users of NRT and tobacco | 57 | 7.42 | 10.08 | 4.75 | 10.10 | 4.00 | 1.00 | 60.00 |
Includes individuals using more than one form of alternative nicotine product (n=22).
Excludes individuals using more than one form of alternative nicotine product.
Current smokers who did not use any alternative nicotine delivery products (exclusive smokers) spent on average £23.09 on smoking each week (Table 2). Ex-smokers who used alternative nicotine products (exclusive alternative nicotine users) spent on average £8.59 on these products each week; with spend on e-cigarettes (£8.03) slightly lower than for NRT (£10.05). Dual users of tobacco and alternative nicotine products spent on average £24.54 on smoking and £7.49 on alternative nicotine products each week, for a total weekly spend of £32.03 (95%CI £28.59 to £35.47).
Among current smokers, there was extremely strong evidence (Supplementary Table 2) that those who consumed more cigarettes per day reported significantly higher expenditure on smoking, while non-daily smokers and those who predominantly smoked roll-your-own cigarettes reported significantly lower expenditure on smoking (Table 3). Smokers from routine and manual social grades reported significantly lower expenditure on smoking and those with higher levels of addiction reported significantly greater expenditure on smoking (Table 3) but this was not strongly supported by Bayesian analysis (Supplementary Table 2). Expenditure on smoking did not differ significantly by age, sex, ethnicity, region, or past-year quit attempts after adjustment for other variables.
Table 3.
Multivariable regression models testing independent associations between sociodemographic and smoking characteristics and (log-transformed) weekly expenditure on smoking among all smokers with complete data (n=744, n=24 missing)
| B [95%CI] | p | |
|---|---|---|
| Age | 0.000 [-0.002; 0.001] | 0.438 |
| Female sex | -0.015 [-0.054; 0.025] | 0.461 |
| White ethnicity | 0.004 [-0.058; 0.067] | 0.897 |
| Social grade C2DE | -0.044 [-0.084; -0.004] | 0.031 |
| Region: central | 0.001 [-0.046; 0.048] | 0.962 |
| Region: south | -0.008 [-0.056; 0.039] | 0.734 |
| Dual use of tobacco and alternative nicotine products | 0.015 [-0.034; 0.063] | 0.556 |
| Cigarettes per day | 0.021 [0.018; 0.024] | <0.001 |
| Non-daily smoker | -0.523 [-0.603; -0.443] | <0.001 |
| Predominant RYO use1 | -0.297 [-0.336; -0.258] | <0.001 |
| Time to first cigarette2 | 0.023 [0.002; 0.045] | 0.035 |
| Tried to quit in past year | 0.028 [-0.018; 0.074] | 0.229 |
RYO = roll-your-own cigarettes.
0 = more than 60 minutes/1 = 30-60 minutes/2 = 6-30 minutes/3 = within 5 minutes.
Bayes factors for these results are shown in Supplementary Table 1.
Model R2 = 0.551.
Among current users of any alternative nicotine delivery product, there was strong evidence (Supplementary Table 3) that people from white ethnic groups reported significantly higher weekly expenditure on these products than those from non-white groups, and moderate to very strong evidence that those from central and southern England reported significantly higher weekly expenditure on these products than those in the north of England (Table 4, model 1). There was strong evidence (Supplementary Table 3) that current smokers reported significantly lower expenditure on alternative nicotine delivery products (Table 4, model 1). Expenditure on alternative nicotine delivery products did not differ significantly by age, sex, or social grade after adjustment for other sociodemographic variables. Among those who reported smoking in the past year, there was strong evidence (Supplementary Table 3) that past-year quit attempts were associated with significantly higher expenditure (Table 4, model 2). Expenditure on alternative nicotine delivery products did not differ significantly by number of cigarettes smoked per day, non-daily smoking, predominant use of roll-your-own cigarettes, or level of cigarette addiction after adjustment for other variables.
Table 4.
Multivariable regression models testing independent associations between (i) sociodemographic characteristics and (log-transformed) weekly expenditure on alternative nicotine delivery products (e-cigarettes, nicotine replacement therapy, heated tobacco products) among current users with complete data (n=255 [n=2 missing]; Model 1) and (ii) smoking characteristics and (log-transformed) weekly expenditure on alternative nicotine delivery products among current users who reported smoking in the past year (n=177; Model 2)
| Model 1 |
Model 2 |
|||
|---|---|---|---|---|
| B [95%CI] | p | B [95%CI] | p | |
| Age | -0.003 [-0.006; 0.001] | 0.096 | -0.003 [-0.007; 0.002] | 0.226 |
| Female sex | -0.062 [-0.174; 0.050] | 0.280 | -0.106 [-0.246; 0.033] | 0.134 |
| White ethnicity | 0.255 [0.069; 0.440] | 0.007 | 0.225 [0.013; 0.438] | 0.038 |
| Social grade C2DE | -0.053 [-0.160; 0.054] | 0.327 | -0.067 [-0.199; 0.064] | 0.312 |
| Region: central | 0.222 [0.090; 0.354] | 0.001 | 0.320 [0.161; 0.479] | <0.001 |
| Region: south | 0.168 [0.040; 0.297] | 0.010 | 0.252 [0.097; 0.407] | 0.002 |
| Current smoker | -0.169 [-0.284; -0.054] | 0.004 | 0.071 [-0.181; 0.324] | 0.577 |
| Cigarettes per day | - | - | -0.004 [-0.013; 0.005] | 0.352 |
| Non-daily smoker | - | - | -0.206 [-0.533; 0.121] | 0.215 |
| Predominant RYO use1 | - | - | -0.111 [-0.242; 0.021] | 0.098 |
| Time to first cigarette2 | - | - | 0.000 [-0.068; 0.068] | 0.992 |
| Tried to quit in past year | - | - | 0.178 [0.046; 0.309] | 0.008 |
RYO = roll-your-own cigarettes.
0 = more than 60 minutes/1 = 30-60 minutes/2 = 6-30 minutes/3 = within 5 minutes.
Bayes factors for these results are shown in Supplementary Table 2.
Model R2 = 0.130 for Model 1, 0.235 for Model 2.
Among current e-cigarette users, there was moderate evidence (Supplementary Table 4) that women and current smokers reported significantly lower weekly expenditure on e-cigarettes than men and non-smokers, respectively, and very strong evidence that those from central and southern England reported significantly higher weekly expenditure on e-cigarettes than those in the north of England (Table 5, model 1). Expenditure on e-cigarettes did not differ significantly by age, ethnicity, or social grade after adjustment for other sociodemographic variables. Among those who reported smoking in the past year, there was moderate evidence (Supplementary Table 4) that having made a past-year quit attempt was associated with significantly higher expenditure on e-cigarettes (Table 5, model 2). Expenditure on e-cigarettes did not differ significantly by number of cigarettes smoked per day, non-daily smoking, use of roll-your-own cigarettes, or level of cigarette addiction after adjustment for other variables.
Table 5.
Multivariable regression models testing independent associations between (i) sociodemographic characteristics and (log-transformed) weekly expenditure on e-cigarettes among current users with complete data (n=154 [n=2 missing]; Model 1) and (ii) smoking characteristics and (log-transformed) weekly expenditure on e-cigarettes among current users who reported smoking in the past year (n=98; Model 2)
| Model 1 |
Model 2 |
|||
|---|---|---|---|---|
| B [95%CI] | p | B [95%CI] | p | |
| Age | -0.004 [-0.008; 0.000] | 0.050 | -0.001 [-0.006; 0.004] | 0.626 |
| Female sex | -0.133 [-0.265; -0.001] | 0.049 | -0.185 [-0.356; -0.015] | 0.034 |
| White ethnicity | 0.125 [-0.093; 0.342] | 0.258 | 0.064 [-0.180; 0.308] | 0.603 |
| Social grade C2DE | -0.057 [-0.185; 0.070] | 0.376 | -0.039 [-0.217; 0.139] | 0.664 |
| Region: central | 0.294 [0.143; 0.446] | <0.001 | 0.406 [0.211; 0.602] | <0.001 |
| Region: south | 0.253 [0.099; 0.407] | 0.001 | 0.354 [0.155; 0.554] | 0.001 |
| Current smoker | -0.177 [-0.311; -0.043] | 0.010 | -0.037 [-0.324; 0.251] | 0.800 |
| Cigarettes per day | - | - | -0.005 [-0.018; 0.009] | 0.486 |
| Non-daily smoker | - | - | -0.215 [-0.542; 0.113] | 0.196 |
| Predominant RYO use1 | - | - | -0.045 [-0.211; 0.121] | 0.595 |
| Time to first cigarette2 | - | - | 0.009 [-0.078; 0.097] | 0.831 |
| Tried to quit in past year | - | - | 0.183 [0.022; 0.343] | 0.026 |
RYO = roll-your-own cigarettes.
0 = more than 60 minutes/1 = 30-60 minutes/2 = 6-30 minutes/3 = within 5 minutes.
Bayes factors for these results are shown in Supplementary Table 3.
Model R2 = 0.187 for Model 1, 0.307 for Model 2.
Among current NRT users, expenditure on NRT did not differ significantly by age, sex, ethnicity, social grade, region, or current smoking status after mutual adjustment (Table 6, model 1). Among those who reported smoking in the past year, there was moderate evidence (Supplementary Table 5) that predominant use of roll-your-own cigarettes was associated with significantly lower expenditure on NRT (Table 6, model 2). Among past-year smokers who used NRT, expenditure on NRT did not differ significantly by number of cigarettes smoked per day, level of cigarette addiction, or past-year quit attempts after adjustment for other variables. Non-daily smoking was excluded from the model because all past-year smokers who reported using NRT were daily smokers.
Table 6.
Multivariable regression models testing independent associations between (i) sociodemographic characteristics and (log-transformed) weekly expenditure on nicotine replacement therapy among current users with complete data (n=78 [n=1 missing]; Model 1) and (ii) smoking characteristics and (log-transformed) weekly expenditure on nicotine replacement therapy among current users who reported smoking in the past year (n=58; Model 2)
| Model 1 |
Model 2 |
|||
|---|---|---|---|---|
| B [95%CI] | p | B [95%CI] | p | |
| Age | 0.001 [-0.006; 0.008] | 0.762 | -0.002 [-0.011; 0.006] | 0.579 |
| Female sex | 0.074 [-0.176; 0.324] | 0.557 | 0.109 [-0.222; 0.439] | 0.513 |
| White ethnicity | 0.350 [-0.091; 0.790] | 0.118 | 0.616 [0.041; 1.191] | 0.036 |
| Social grade C2DE | -0.070 [-0.309; 0.170] | 0.564 | -0.106 [-0.382; 0.170] | 0.445 |
| Region: central | 0.089 [-0.225; 0.403] | 0.574 | 0.217 [-0.154; 0.588] | 0.245 |
| Region: south | 0.079 [-0.212; 0.371] | 0.588 | 0.186 [-0.157; 0.530] | 0.281 |
| Current smoker | -0.147 [-0.418; 0.124] | 0.284 | 0.500 [-0.144; 1.143] | 0.125 |
| Cigarettes per day | - | - | 0.002 [-0.015; 0.019] | 0.821 |
| Non-daily smoker3 | - | - | - | - |
| Predominant RYO use1 | - | - | -0.316 [-0.606; -0.026] | 0.033 |
| Time to first cigarette2 | - | - | 0.010 [-0.127; 0.147] | 0.886 |
| Tried to quit in past year | - | - | -0.040 [-0.346; 0.267] | 0.795 |
RYO = roll-your-own cigarettes.
0 = more than 60 minutes/1 = 30-60 minutes/2 = 6-30 minutes/3 = within 5 minutes.
Excluded from Model 2 because all past-year smokers who reported using nicotine replacement therapy were daily smokers.
Bayes factors for these results are shown in Supplementary Table 4.
Model R2 = 0.086 for Model 1, 0.265 for Model 2.
BFs for non-significant associations indicated that data were generally insensitive or provided moderate evidence for the null hypothesis (Supplementary Tables 2-5).
Analyses on untransformed expenditure variables (Supplementary Tables 6-9) produced a similar pattern of results.
Discussion
In this representative survey of adults in England, smokers reported spending on average £23.40 on smoking each week, e-cigarette users reported spending £7.60, and NRT users reported spending £8.15. Sufficient data were not available to estimate expenditure on heated tobacco products. People who used to smoke and now use e-cigarettes reported spending on average £8.03 on e-cigarettes each week, while ex-smokers who now use NRT reported spending £10.05 each week. Compared with the average expenditure on smoking by those who did not use any alternative nicotine delivery product, this expenditure would represent an estimated saving of approximately £15.06 a week (£783 a year) from switching completely to e-cigarettes and approximately £13.04 a week (£678 a year) from switching completely to NRT.
Interestingly, estimates of expenditure on tobacco and alternative nicotine delivery products among dual users were similar to those in exclusive users of either product. Dual users of tobacco and alternative nicotine delivery products reported spending on average £24.54 on smoking and £7.49 on alternative nicotine products each week; comparable to the £23.09 and £8.59 spent by exclusive users of tobacco and alternative nicotine products, respectively. This suggests that (i) exclusive nicotine users appear not to be paying much more for their alternative nicotine delivery products than those who are also smoking, and (ii) smokers who are concurrently using alternative nicotine products are not spending any less on tobacco, so end up spending more on their dual use than they were on smoking alone. These findings likely reflect ex-smokers who are using alternative nicotine delivery products trying to cut down and stop using the products, while dual users are those who are heavier nicotine consumers (and indeed, may have cut down their previously above-average expenditure on smoking by introducing an alternative nicotine delivery product or who use these products in environments where combustible cigarette use is not allowed). When further data on expenditure on alternative nicotine delivery products accumulate in the Smoking Toolkit Study, it will be possible to explore differences in expenditure on these products among ex-smokers in relation to how long it has been since they quit. Prospective data on expenditure on smoking among smokers who take up dual use of an alternative nicotine delivery product could shed light on the apparent lack of cost saving on tobacco in this group.
Expenditure on smoking was higher among heavier and more addicted smokers and lower among non-daily smokers and roll-your-own tobacco users. Smokers with routine and manual occupations also reported lower expenditure on smoking, consistent with evidence that low-income smokers are most price-sensitive and use various strategies (e.g. using cheaper products or illicit tobacco) to reduce the cost of smoking (e.g. 32), although the BF was borderline for data insensitivity so this result should be interpreted with caution. Expenditure on e-cigarettes was higher among users from central and southern vs. northern England. Long-term (>12 months) use of e-cigarettes is more common in the north (33) and it may be the case that longer-term users develop strategies to reduce their expenditure. Alternatively, this could also reflect different pricing strategies for e-cigarettes across these regions. Expenditure on e-cigarettes was also higher among smokers who had tried to quit in the past year. E-cigarettes are now the most popular aid to cessation in England, with over a third of smokers using an e-cigarette in their most recent quit attempt (10), so higher expenditure among users who tried to quit is not surprising. Expenditure on NRT was lower among roll-your-own tobacco users. These smokers tend to be less motivated to quit than factory-made cigarette smokers because the cost associated with smoking is much lower (34), which may account for their lower expenditure on NRT; a product typically used to aid quit attempts.
While this study provides useful insight into the potential cost saving that could be achieved by switching completely from smoking to an alternative nicotine delivery product, several limitations should be considered when interpreting the results. Expenditure was self-reported, introducing potential for bias. It is possible that accuracy of self-reports of expenditure may have differed between groups; for example, those with lower levels of disposable income (e.g. younger participants and those from lower social grades) may have been more mindful of the amount they were spending. Expenditure on smoking was only assessed in current smokers, so we were not able to directly calculate the cost saving made by ex-smokers who had switched to e-cigarettes or NRT. Given that heavier smokers are more likely to be dual users or to switch to e-cigarettes (35–37), estimates of expenditure among all users and dual users of e-cigarettes may be biased upwards. The assessment of expenditure on alternative nicotine delivery products did not differentiate between the product categories (i.e. NRT or e-cigarettes). As such, we restricted our analyses to those who reported use of a single product as it was not possible to accurately analyse expenditure in the small number of respondents who reported use of multiple products. However, this only excluded 23 respondents (<10% of alternative nicotine delivery product users) so it is unlikely that it had a notable impact on our results. While the majority of people who use NRT buy it over the counter, NRT is also available in England free of charge from a prescribing healthcare professional or stop smoking service. Our estimates of expenditure on NRT may therefore underestimate expenditure by those who have to pay for it. We had intended to analyse expenditure on heated tobacco products but prevalence of use in England is low (38) and was reported by just one respondent who also used another nicotine delivery product. Similarly, there were very few users of Juul, an e-cigarette product growing rapidly in popularity in the US, which precluded estimates of expenditure on this product category. As the popularity of these products in England increases, it may be possible to revisit this analysis to gain insight into their cost to users. Estimates of the cost saving that could be achieved from switching from smoking to alternative nicotine were unadjusted and derived from self-selecting groups with differing characteristics relating to their level of use. It is likely that in reality any cost saving will be affected by characteristics that influence expenditure. Estimates may also under- or overestimate the potential cost saving that could be achieved by switching to e-cigarettes because there are a great variety of products available to choose from (at a range of prices) and cost will be influenced by personal preference and availability (e.g. location of vape shops, whether people feel comfortable using the internet to order them). Evidence for cost-saving in our study is predicated on the fact that e-cigarettes are cheaper than cigarettes in England, which may not apply to different jurisdictions, such as low-middle income countries. Finally, BFs indicated that data were insensitive to detect associations between many of the sociodemographic and smoking characteristics and outcomes, so we are unable to rule out the possibility that additional associations between these variables exist.
Conclusions
One in three smokers lists cost as an important factor driving their desire to quit (2). In England, expenditure on e-cigarettes and NRT by users of these products is approximately one third of the amount smokers report spending on smoking. The average smoker could save an estimated £15 per week by switching completely from combustible tobacco to e-cigarettes or £13 per week by switching completely to NRT, although this will likely differ according to individual usage patterns. With use of alternative nicotine delivery products costing substantially less on average than smoking, the cost of alternative nicotine delivery products should not be a barrier to quit attempts.
Supplementary Material
References
- 1.Office of the Surgeon General (US), Office on Smoking and Health (US) The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2004. [cited 2018 Aug 7]. [Internet]. (Reports of the Surgeon General). Available from: http://www.ncbi.nlm.nih.gov/books/NBK44695/ [PubMed] [Google Scholar]
- 2.McCaul KD, Hockemeyer JR, Johnson RJ, Zetocha K, Quinlan K, Glasgow RE. Motivation to quit using cigarettes: A review. Addict Behav. 2006 Jan 1;31(1):42–56. doi: 10.1016/j.addbeh.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 3.Hyland A, Borland R, Li Q, Yong H-H, McNeill A, Fong GT, et al. Individual-level predictors of cessation behaviours among participants in the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006 Jun 1;15(suppl 3):iii83–94. doi: 10.1136/tc.2005.013516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults--United States, 2007. MMWR Morb Mortal Wkly Rep. 2008 Nov 14;57(45):1221–6. [PubMed] [Google Scholar]
- 5.Benowitz NL. Nicotine Addiction. N Engl J Med. 2010 Jun 17;362(24):2295–303. doi: 10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smoking in England. Electronic cigarettes in England - latest trends. [cited 2018 Oct 25];2018 [Internet]. Available from: http://www.smokinginengland.info/latest-statistics/
- 7.West R, Brown J, Shahab L. Written evidence submitted by University College London, Tobacco and Alcohol Research Group (UTARG) (ECG0047) [cited 2018 Oct 11];2017 [Internet]. Available from: http://data.parliament.uk/writtenevidence/committeeevidence.svc/evidencedocument/science-and-technology-committee/ecigarettes/written/75276.html.
- 8.Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016 Sep 14;9:CD010216. doi: 10.1002/14651858.CD010216.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Royal College of Physicians. Nicotine without smoke Tobacco harm reduction. 2016 [Google Scholar]
- 10.McNeill A, Brose LS, Calder R, Bauld L, Robson D. Evidence review of e-cigarettes and heated tobacco products 2018. [cited 2018 Jun 21];A report commissioned by Public Health England. 2018 [Internet]. Available from: https://www.gov.uk/government/publications/e-cigarettes-and-heated-tobacco-products-evidence-review/evidence-review-of-e-cigarettes-and-heated-tobacco-products-2018-executive-summary.
- 11.Liber AC, Drope JM, Stoklosa M. Combustible cigarettes cost less to use than e-cigarettes: global evidence and tax policy implications. Tob Control. 2017 Mar 1;26(2):158–63. doi: 10.1136/tobaccocontrol-2015-052874. [DOI] [PubMed] [Google Scholar]
- 12.Etter J-F. Electronic Cigarette: A Longitudinal Study of Regular Vapers. Nicotine Tob Res. 2018 Jul 9;20(8):912–22. doi: 10.1093/ntr/ntx132. [DOI] [PubMed] [Google Scholar]
- 13.Etter J-F. Explaining the effects of electronic cigarettes on craving for tobacco in recent quitters. Drug Alcohol Depend. 2015 Mar 1;148:102–8. doi: 10.1016/j.drugalcdep.2014.12.030. [DOI] [PubMed] [Google Scholar]
- 14.Yao T, Max W, Sung H-Y, Glantz SA, Goldberg RL, Wang JB, et al. Relationship between spending on electronic cigarettes, 30-day use, and disease symptoms among current adult cigarette smokers in the U.S. [cited 2019 Jan 15];PLoS ONE. 2017 Nov 7;12(11) doi: 10.1371/journal.pone.0187399. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hartmann-Boyce J, Chepkin SC, Ye W, Bullen C, Lancaster T. Nicotine replacement therapy versus control for smoking cessation. [cited 2018 Nov 8];Cochrane Database Syst Rev. 2018 (5) doi: 10.1002/14651858.CD000146. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jackson SE, Kotz D, West R, Brown J. Real-world effectiveness and effect moderators of aids to smoking cessation: a population study. doi: 10.1111/add.14656. in preparation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simonavicius E, McNeill A, Shahab L, Brose LS. Heat-not-burn tobacco products: a systematic literature review. Tob Control. 2018 Sep 4; doi: 10.1136/tobaccocontrol-2018-054419. tobaccocontrol-2018-054419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Committee on Toxicity. [cited 2019 Jun 4];Toxicological evaluation of novel heat-not-burn tobacco products. 2017 [Internet]. Available from: https://cot.food.gov.uk/sites/default/files/heat_not_burn_tobacco_summary.pdf.
- 19.Pearson JL, Richardson A, Niaura RS, Vallone DM, Abrams DB. e-Cigarette awareness, use, and harm perceptions in US adults. Am J Public Health. 2012 Sep;102(9):1758–66. doi: 10.2105/AJPH.2011.300526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choi K, Hennrikus D, Forster J, Claire AW. Use of price-minimizing strategies by smokers and their effects on subsequent smoking behaviors. Nicotine Tob Res Off J Soc Res Nicotine Tob. 2012 Jul;14(7):864–70. doi: 10.1093/ntr/ntr300. [DOI] [PubMed] [Google Scholar]
- 21.Licht AS, Hyland AJ, O’Connor RJ, Chaloupka FJ, Borland R, Fong GT, et al. How do price minimizing behaviors impact smoking cessation? Findings from the International Tobacco Control (ITC) Four Country Survey. Int J Environ Res Public Health. 2011;8(5):1671–91. doi: 10.3390/ijerph8051671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Licht AS, Hyland AJ, O’Connor RJ, Chaloupka FJ, Borland R, Fong GT, et al. Socio-Economic Variation in Price Minimizing Behaviors: Findings from the International Tobacco Control (ITC) Four Country Survey. Int J Environ Res Public Health. 2011 Jan;8(1):234–52. doi: 10.3390/ijerph8010234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White VM, Gilpin EA, White MM, Pierce JP. How do smokers control their cigarette expenditures? Nicotine Tob Res Off J Soc Res Nicotine Tob. 2005 Aug;7(4):625–35. doi: 10.1080/14622200500184333. [DOI] [PubMed] [Google Scholar]
- 24.Xu X, Pesko MF, Tynan MA, Gerzoff RB, Malarcher AM, Pechacek TF. Cigarette price-minimization strategies by U.S. smokers. Am J Prev Med. 2013 May;44(5):472–6. doi: 10.1016/j.amepre.2013.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Branston JR, McNeill A, Gilmore AB, Hiscock R, Partos TR. Keeping smoking affordable in higher tax environments via smoking thinner roll-your-own cigarettes: Findings from the International Tobacco Control Four Country Survey 2006–15. Drug Alcohol Depend. 2018 Dec 1;193:110–6. doi: 10.1016/j.drugalcdep.2018.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fidler JA, Shahab L, West O, Jarvis MJ, McEwen A, Stapleton JA, et al. “The smoking toolkit study”: a national study of smoking and smoking cessation in England. BMC Public Health. 2011 Jun 18;11:479. doi: 10.1186/1471-2458-11-479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dienes Z. Using Bayes to get the most out of non-significant results. [cited 2018 Jul 4];Front Psychol. 2014 Jul 29;5 doi: 10.3389/fpsyg.2014.00781. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.West R. Using Bayesian analysis for hypothesis testing in addiction science. Addiction. 2015;111(1):3–4. doi: 10.1111/add.13053. [DOI] [PubMed] [Google Scholar]
- 29.Rouder JN, Speckman PL, Sun D, Morey RD, Iverson G. Bayesian t tests for accepting and rejecting the null hypothesis. Psychon Bull Rev. 2009 Apr 1;16(2):225–37. doi: 10.3758/PBR.16.2.225. [DOI] [PubMed] [Google Scholar]
- 30.Dienes Z, Coulton S, Heather N. Using Bayes factors to evaluate evidence for no effect: examples from the SIPS project. Addiction. 2018;113(2):240–6. doi: 10.1111/add.14002. [DOI] [PubMed] [Google Scholar]
- 31.Jeffreys H. The Theory of Probability. Oxford: Clarendon Press; 1961. p. 474. [Google Scholar]
- 32.Action on Smoking and Health. Beyond Smoking Kills. [cited 2019 Jan 10];2010 Oct; [Internet]. Available from: http://ash.org.uk/information-and-resources/reports-submissions/reports/beyond-smoking-kills/
- 33.Jackson SE, Hill E, Shahab L, Beard E, Michie S, Brown J. Long-term e-cigarette and nicotine replacement therapy use in England: a population survey. BMJ Open. 2019 doi: 10.1136/bmjopen-2019-029252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jackson SE, Shahab L, West R, Brown J. Roll-your-own cigarette use and smoking cessation behaviour: a cross-sectional population study in England. BMJ Open. 2018 Dec 1;8(12):e025370. doi: 10.1136/bmjopen-2018-025370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vardavas CI, Filippidis FT, Agaku IT. Determinants and prevalence of e-cigarette use throughout the European Union: a secondary analysis of 26 566 youth and adults from 27 Countries. Tob Control. 2015 Sep 1;24(5):442–8. doi: 10.1136/tobaccocontrol-2013-051394. [DOI] [PubMed] [Google Scholar]
- 36.Levy DT, Yuan Z, Li Y. The Prevalence and Characteristics of E-Cigarette Users in the U.S. [cited 2018 Dec 5];Int J Environ Res Public Health. 2017 Oct;14(10) doi: 10.3390/ijerph14101200. [Internet] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brown J, West R, Beard E, Michie S, Shahab L, McNeill A. Prevalence and characteristics of e-cigarette users in Great Britain: Findings from a general population survey of smokers. Addict Behav. 2014 Jun 1;39(6):1120–5. doi: 10.1016/j.addbeh.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brose LS, Simonavicius E, Cheeseman H. [cited 2019 Jan 17];Awareness and Use of “Heat-not-burn” Tobacco Products in Great Britain. 2018 [Internet]. Available from: https://www.ingentaconnect.com/contentone/trsg/trs/2018/00000004/00000002/art00004. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.