Abstract
Hierarchical dimensional systems of psychopathology promise more informative descriptions for understanding risk and predicting outcome than traditional diagnostic systems, but it is unclear how many major dimensions they should include. We delineated the hierarchy of childhood and adult psychopathology and validated it against clinically relevant measures. Participants were 9987 9- and 10-year-old children and their parents from the Adolescent Brain Cognitive Development (ABCD) study. Factor analyses of items from the Child Behavior Checklist and Adult Self-Report were run to delineate hierarchies of dimensions. We examined the familial aggregation of the psychopathology dimensions, and the ability of different factor solutions to account for risk factors, real-world functioning, cognitive functioning, and physical and mental health service utilization. A hierarchical structure with a general psychopathology (‘p’) factor at the apex and five specific factors (internalizing, somatoform, detachment, neurodevelopmental, and externalizing) emerged in children. Five similar dimensions emerged also in the parents. Child and parent p-factors correlated highly (r = 0.61, p < 0.001), and smaller but significant correlations emerged for convergent dimensions between parents and children after controlling for p-factors (r = 0.09−0.21, p < 0.001). A model with child p-factor alone explained mental health service utilization (R2 = 0.23, p < 0.001), but up to five dimensions provided incremental validity to account for developmental risk and current functioning in children (R2 = 0.03−0.19, p < 0.001). In this first investigation comprehensively mapping the psychopathology hierarchy in children and adults, we delineated a hierarchy of higher-order dimensions associated with a range of clinically relevant validators. These findings hold important implications for psychiatric nosology and future research in this sample.
Subject terms: Diseases, Psychiatric disorders
Introduction
Traditional psychiatric nosologies define mental disorders as distinct categories1,2, but this is at odds with extensive evidence that disorders lie on a continuum with normality and are highly comorbid3–7. This comorbidity reflects underlying higher-order dimensions (or spectra) of psychopathology4,7–9. Dimensional classifications of these spectra have been proposed as alternative approaches to better align the nosology with empirical evidence4,7,8,10. However, available models differ in the number of spectra that they specify.
Numerous studies point to a general factor (‘p’) that represents common susceptibility to psychopathology and explains why all mental disorders tend to co-occur5,9,11–14. Other research supports a separation between broad internalizing and externalizing spectra—originally identified in studies that shaped the Achenbach System of Empirically Based Assessment (ASEBA)15,16—arguing that this is an important distinction both in adults17,18 and children19,20. However, further evidence suggests that a greater number of major dimensions are needed to characterize psychopathology8,21–25. For instance, the recently developed Hierarchical Taxonomy of Psychopathology (HiTOP)7,8 includes six spectra (internalizing, somatoform, detachment, thought disorder, antagonism, and disinhibition), which were identified based on extensive factor analytic literature (for a review, see ref. 8). Yet, the dimensions depicted in these studies may not provide full coverage of psychopathology, especially with regard to disorders common in children. For example, a neurodevelopmental spectrum—encompassing forms of psychopathology that share common genetic vulnerabilities, are associated with salient cognitive impairments, emerge in infancy or childhood, and often persist into adulthood (e.g., speech problems, motor problems, autism)—has been proposed26, but its placement among other psychopathology spectra remains unclear due to paucity of relevant factor analytic studies27,28. Furthermore, the original notion of neurodevelopmental spectrum26 did not include problems related to inattention and hyperactivity–impulsivity, which many previous factor analytic studies placed under the externalizing spectrum29–31. However, other factor analytic evidence suggests that inattention and hyperactivity–impulsivity symptoms may not cluster with externalizing problems27,28,32–36, and accumulating validity studies indicate substantial commonality with other neurodevelopmental problems37–42. Further research examining the structure of these symptoms alongside other forms of psychopathology is therefore warranted.
Models with different numbers of dimensions remain to be reconciled in order to advance psychiatric classification and its clinical utility. Simpler and more complex architectures may be integrated as different levels of a single hierarchy: from a p-factor at the apex to progressively more specific nested factors43,44. Consequently, models with different numbers of dimensions (one, two, three, etc.) can co-exist and be studied simultaneously. Initial studies, employing Goldberg’s bass-ackwards approach43 to delineate hierarchical structures, have identified a hierarchy of higher-order dimensions22,23,44–46, but were largely limited to personality pathology and focused on adults. Importantly, developmental studies suggest that some psychopathology dimensions may differ with age, and additional dimensions may emerge over development14,47, which underscores the importance of studying child samples as well.
Beyond the identification of the number of dimensions, an important step for delineating a new psychopathology classification is to validate dimensions against criteria important for clinical practice and research, such as genetic/familial and psychosocial risk factors, cognitive processes, illness course, and treatment outcome48–50. In a hierarchical structure, validity may differ across levels, as more elaborate models tend to be more informative, but are less parsimonious, and the choice between models may depend on the purpose of inquiry. Available studies show that broader spectra are associated with familiality for psychiatric disorders, childhood adversities, brain and functional impairment11,13,49, while more specific dimensions are required to adequately account for outcomes such as educational achievement and executive functioning14,19,27. However, a systematic evaluation of validity of dimensions across hierarchical levels is lacking.
In the present study, we sought to delineate higher-order dimensions of psychopathology within a hierarchical structure, and compare the validity of different levels of specificity. Our first aim was to investigate the hierarchical structure of psychopathology in 9987 children from the Adolescent Brain Cognitive Development (ABCD) study51–53—as well as in their parents—by analyzing a large and diverse set of symptoms15,16. Our second aim was to compare the validity of different levels of the childhood psychopathology hierarchy in relation to clinically informative measures of familial and developmental risk factors, current social, academic, and cognitive functioning, and service utilization11,14,50,54,55.
Methods
Sample
The ABCD sample consists of over 11,000 children and their parents who took part in a major collaboration between 21 sites across the US to investigate psychological and neurobiological development from preadolescence to early adulthood. Full details of recruitment can be found elsewhere51. Briefly, the primary method for recruiting children aged 9 or 10 at the time of the baseline assessments (between 2016 and 2018) and their parents was probability sampling of public and private elementary schools within the catchment areas of the 21 research sites, encompassing over 20% of the entire US population of 9–10 year olds. School selection was based on gender, race and ethnicity, socioeconomic status, and urbanicity. Inclusion criteria were age and attending a public or private elementary school in the catchment area. Exclusion criteria for children were limited to not being fluent in English, having a parent not fluent in English or Spanish, major medical or neurological conditions, gestational age <28 weeks or birthweight <1200 g, contraindications to MRI scanning, a history of traumatic brain injury, a current diagnosis of schizophrenia, moderate/severe autism spectrum disorder, intellectual disability, or alcohol/substance use disorder56,57. The cohort’s representation of diverse demographic and socio-economic groups was monitored through the National Center for Education Statistics databases, containing socio-demographic characteristics of the students attending each school, to enable dynamic adjustment of the accumulating sample based on demographic targets throughout recruitment. The final sample who completed the baseline assessment approached the diversity of the US population on several socio-demographic characteristics, despite not being nationally representative58: 51% of families were White, 21.4% were Hispanic, 15.2% were African American, 2.3% were Asian, and 10.01% were multiracial or from other ethnical backgrounds; household income was <$50,000 for 30.5% of families, between $50,000 and <$100,000 for 28.1% of families, and at least $100,000 for 41.3% of families; 58.9% of children had at least one parent with a bachelor’s or postgraduate degree; 73.3% parents were married or living in the same household. No weights were applied in the current study. The sample also includes twins recruited from four sites as well as a number of siblings from the same family. However, the present study is based on 9987 unrelated children (randomly selecting one child per family when more than one participated; mean age = 9.90, SD = 0.62; 47.74% females) and 9987 parents (one per child; mean age = 39.94, SD = 6.93; 89.03% females) from the Baseline ABCD 2.0 data release (NDAR-10.15154/1503209). All procedures were approved by a central Institutional Review Board (IRB) at the University of California, San Diego, and in some cases by individual site IRBs (e.g. Washington University in St. Louis)59. Parents or guardians provided written informed consent after the procedures had been fully explained and children assented before participation in the study60.
Measures
Full details on measures are presented in Supplementary Method 1. Children and parents completed assessments during an in-person visit. Psychopathology was examined in the children with the parent-reported Child Behavior Checklist (CBCL)15 and in the adults with the Adult Self-Report (ASR)16 from ASEBA, which assess problems occurring in the past 6 months on a 3-point scale.
For validation, we aimed to select a limited number of validators among those available in the ABCD dataset, based on the two criteria: (1) measures on key, clinically relevant domains, which have commonly been used for validation purposes in previous studies of the structure of psychopathology11,13,18,55,61: risk factors, real-world functioning, cognitive functioning, and service utilization; (2) measures that were maximally comprehensive and non-overlapping with each other. Validation analyses therefore focused on the following ten measures: history of developmental motor and speech delays52, conflict within the family62, social (number of friends) and academic functioning (school connectedness, average grades)63, crystalized and fluid intelligence composites from the National Institute of Health Toolbox53, utilization of physical and mental health services, and medication use52.
Statistical analysis
To investigate the hierarchical structure of psychopathology, we employed an exploratory approach, given uncertainties regarding the number of dimensions and the composition of the levels of the hierarchy. Specifically, we used exploratory factor analysis (EFA) to empirically extract (with principal component analysis) and rotate (with geomin) factor solutions with an increasing number of factors. We favored an exploratory approach over a confirmatory factor analytic approach as we did not have a-priori hypotheses about the number of factors that would emerge from these data, nor on the exact loading of each item on the factors. To avoid distorting the factor structure in EFA with items that were not analyzable due to being endorsed too infrequently or too-highly correlated with other items, we removed items for which frequency was too low (>99.5% rated 0) and aggregated items that were highly correlated (polychoric r > 0.75) into composites (see Supplementary Method 1). The maximum number of factors to extract was determined with parallel analyses64 (extraction was stopped when eigenvalues fell within the 95% confidence interval of eigenvalues from simulated data; Supplementary Fig. 1). Since parallel analysis has a tendency to over-factor, we also examined the interpretability of factor solutions65,66, defined as presence of >3 clear primary loadings (highest loading ≥0.35 and at least 0.10 greater than all other loadings) for each factor65,66. All factor structures from one to the maximum number of factors were considered. To map the hierarchical structure, we correlated factor scores on adjacent levels of the hierarchy to describe transitions between levels using Goldberg’s bass-ackwards hierarchical method43. The paths between levels in the hierarchical model reflect correlations ≥0.65 between the factor scores. The bass-ackwards approach was chosen to be consistent with previous studies that investigated the hierarchical structure of psychopathology and personality22,23,44–46,67,68, and because, to our knowledge, it is the only method that allows for the delineation of multiple hierarchical levels from factors derived through EFA. Unlike alternative approaches based on bifactor models for extracting a general psychopathology factor (or p-factor) alongside residual specific factors11,34,36,55, the bass-ackwards method enables the investigation of multiple levels of a hierarchical structure and the interpretation of factors as interconnected across hierarchical levels, without statistically removing the shared effects of a general factor. In order to take sex into consideration, we further compared factor scores from each hierarchical level in females and males separately in both the child and parent sample.
To compare the utility of the factor solutions, in validation analyses, we first examined the degree of familial aggregation of the dimensions by correlating the factor scores derived for each dimension in parents and children, using both zero-order correlations and partial correlations controlling for the first general psychopathology factors in both parents and children. To examine the familial aggregation due to shared genetic and environmental factors between parent and child, 473 non-biological parent–child pairs were excluded from this analysis (245 adoptive parents, 99 custodial parents, 129 other non-biological parents). Second, we entered the factor scores from each level of the childhood hierarchy as separate blocks into a hierarchical regression model, with each of the validators as the dependent variable. We examined the predictive power and the incremental validity of each level of the hierarchy over more parsimonious structures with the significance of R2 change between blocks67. We used this stringent test, rather than comparing levels in pairs, to ensure that a significant result for models with more factors reflects new information not captured by simpler factor solutions. All analyses were run in Mplus version 7 (Muthén and Muthén, Los Angeles, CA) and SPSS version 25 (IBM Corp, Armonk, NY).
Results
Hierarchical factor structure of CBCL and ASR
CBCL
Parallel analyses indicated that up to 16 factors could be extracted from CBCL items (Supplementary Fig. 1). After examining the interpretability of these factor solutions, 1- to 5-factor solutions were found to be acceptable (Table 1, Supplementary Table 1). Solutions with more than five factors were not tenable as each included at least one factor with only three or fewer primary loadings (Supplementary Table 1).
Table 1.
Factor loadings (top) and factor correlations (bottom) for the 5-factor solution from the exploratory factor analysis of CBCL items
| F1 | F2 | F3 | F4 | F5 | |
|---|---|---|---|---|---|
| Primary loading items | |||||
| Composite (Attacks/threatens) | 0.90 | 0.03 | −0.14 | −0.03 | 0.02 |
| Cruelty, bullying, or meanness to others | 0.88 | −0.05 | −0.10 | −0.01 | −0.03 |
| Composite (Disobeys rules) | 0.81 | −0.11 | 0.16 | −0.01 | −0.07 |
| Gets in many fights | 0.78 | −0.13 | 0.02 | 0.01 | 0.05 |
| Temper tantrums or hot temper | 0.77 | 0.25 | −0.08 | 0.01 | −0.11 |
| Argues a lot | 0.76 | 0.18 | 0.02 | 0.01 | −0.19 |
| Composite (Destroys) | 0.72 | −0.06 | 0.15 | −0.01 | 0.06 |
| Screams a lot | 0.72 | 0.17 | −0.03 | 0.01 | −0.04 |
| Doesn’t seem to feel guilty after misbehaving | 0.71 | −0.11 | 0.11 | −0.03 | 0.05 |
| Swearing or obscene language | 0.70 | −0.01 | −0.04 | 0.02 | 0.02 |
| Teases a lot | 0.69 | −0.03 | 0.08 | 0.06 | −0.12 |
| Composite (Steals) | 0.69 | −0.23 | 0.12 | 0.01 | 0.10 |
| Stubborn, sullen, or irritable | 0.69 | 0.27 | −0.09 | 0.08 | −0.05 |
| Lying or cheating | 0.68 | −0.18 | 0.16 | 0.05 | 0.00 |
| Cruel to animals | 0.67 | −0.05 | −0.03 | −0.10 | 0.15 |
| Runs away from home | 0.60 | 0.11 | 0.05 | 0.00 | 0.10 |
| Sudden changes in mood or feelings | 0.60 | 0.32 | −0.02 | 0.08 | 0.03 |
| Easily jealous | 0.57 | 0.29 | 0.02 | −0.02 | −0.07 |
| Composite (Peer problems) | 0.53 | 0.07 | 0.14 | −0.03 | 0.26 |
| Suspicious | 0.53 | 0.18 | 0.08 | 0.01 | 0.14 |
| Demands a lot of attention | 0.51 | 0.27 | 0.29 | 0.00 | −0.25 |
| Thinks about sex too much | 0.51 | −0.08 | 0.12 | 0.11 | 0.03 |
| Hangs around with others who get in trouble | 0.51 | −0.18 | 0.19 | 0.04 | 0.01 |
| Feels others are out to get him/her | 0.50 | 0.36 | 0.00 | −0.05 | 0.11 |
| Sets fires | 0.50 | −0.18 | 0.19 | −0.08 | 0.06 |
| Sulks a lot | 0.49 | 0.34 | −0.09 | 0.12 | 0.12 |
| Showing off or clowning | 0.49 | −0.04 | 0.36 | 0.04 | −0.28 |
| Bragging, boasting | 0.48 | 0.05 | 0.21 | 0.08 | −0.31 |
| Whining | 0.41 | 0.27 | 0.09 | 0.09 | −0.09 |
| Too fearful or anxious | −0.13 | 0.70 | 0.33 | 0.02 | 0.03 |
| Worries | −0.06 | 0.67 | 0.18 | 0.13 | 0.00 |
| Feels he/she has to be perfect | −0.01 | 0.67 | −0.01 | 0.00 | −0.02 |
| Feels too guilty | −0.02 | 0.65 | 0.18 | 0.06 | −0.01 |
| Nervous, high-strung, or tense | 0.04 | 0.57 | 0.38 | 0.00 | −0.04 |
| Fears he/she might think or do something bad | 0.05 | 0.56 | 0.19 | −0.03 | 0.04 |
| Feels worthless or inferior | 0.28 | 0.55 | 0.04 | −0.03 | 0.14 |
| Self-conscious or easily embarrassed | 0.06 | 0.46 | 0.07 | 0.08 | 0.26 |
| Fears going to school | 0.09 | 0.40 | 0.08 | 0.10 | 0.27 |
| Fears certain animals, situations, or places, other than school | −0.05 | 0.37 | 0.24 | 0.08 | 0.08 |
| Complains of loneliness | 0.25 | 0.36 | 0.16 | 0.04 | 0.13 |
| Composite (Distracted/Hyperactive) | 0.21 | −0.04 | 0.77 | −0.06 | 0.00 |
| Daydreams or gets lost in his/her thoughts | −0.12 | 0.05 | 0.64 | 0.02 | 0.20 |
| Stares blankly | −0.03 | −0.03 | 0.60 | 0.04 | 0.36 |
| Confused or seems to be in a fog | −0.06 | 0.07 | 0.60 | −0.02 | 0.36 |
| Poorly coordinated or clumsy | −0.02 | −0.08 | 0.58 | 0.24 | 0.15 |
| Nervous movements or twitching | −0.01 | 0.24 | 0.54 | 0.00 | −0.02 |
| Fails to finish things he/she starts | 0.27 | −0.01 | 0.53 | 0.02 | 0.05 |
| Talks too much | 0.20 | 0.04 | 0.52 | 0.12 | −0.26 |
| Can’t get his/her mind off certain thoughts; obsessions | 0.16 | 0.30 | 0.50 | −0.05 | −0.02 |
| Poor school work | 0.29 | −0.14 | 0.49 | −0.04 | 0.18 |
| Repeats certain acts over and over; compulsions | 0.20 | 0.11 | 0.48 | −0.03 | 0.14 |
| Strange ideas | 0.18 | 0.04 | 0.45 | 0.04 | 0.18 |
| Acts too young for his/her age | 0.20 | 0.05 | 0.45 | −0.09 | 0.12 |
| Gets hurt a lot, accident prone | 0.04 | −0.06 | 0.41 | 0.31 | −0.02 |
| Prefers being with younger kids | 0.11 | 0.05 | 0.35 | 0.03 | 0.19 |
| Nausea, feels sick | −0.01 | 0.04 | −0.06 | 0.89 | −0.05 |
| Stomachaches | −0.01 | 0.05 | −0.08 | 0.82 | −0.03 |
| Vomiting, throwing up | 0.02 | −0.19 | −0.04 | 0.75 | 0.06 |
| Headaches | 0.02 | 0.02 | −0.02 | 0.62 | 0.01 |
| Aches or pains (not stomach or headaches) | 0.00 | 0.05 | 0.05 | 0.57 | −0.01 |
| Feels dizzy or lightheaded | −0.05 | 0.15 | 0.08 | 0.53 | 0.11 |
| Other (physical problems without known physical cause) | 0.02 | 0.04 | 0.11 | 0.48 | 0.02 |
| Problems with eyes (not if corrected by glasses) | 0.00 | −0.04 | 0.04 | 0.36 | 0.23 |
| Rashes or other skin problems | 0.01 | 0.00 | 0.10 | 0.35 | 0.04 |
| Withdrawn, doesn’t get involved with others | 0.17 | 0.17 | 0.03 | 0.05 | 0.65 |
| Would rather be alone than with others | 0.13 | 0.11 | 0.05 | 0.01 | 0.56 |
| Too shy or timid | −0.10 | 0.31 | −0.01 | 0.06 | 0.55 |
| Refuses to talk | 0.27 | 0.13 | −0.02 | 0.04 | 0.51 |
| Underactive, slow moving, or lacks energy | 0.07 | 0.00 | 0.12 | 0.34 | 0.45 |
| Non-primary loading or cross-loading items | |||||
| Secretive, keeps things to self | 0.32 | 0.08 | 0.02 | 0.08 | 0.40 |
| Strange behavior | 0.32 | 0.05 | 0.41 | −0.01 | 0.23 |
| There is very little he/she enjoys | 0.39 | 0.16 | 0.01 | 0.01 | 0.34 |
| Unhappy, sad, or depressed | 0.38 | 0.42 | −0.09 | 0.12 | 0.23 |
| Unusually loud | 0.39 | 0.08 | 0.42 | 0.11 | −0.21 |
| Deliberately harms self or attempts suicide | 0.39 | 0.37 | 0.06 | −0.08 | 0.10 |
| Feels or complains that no one loves him/her | 0.54 | 0.47 | −0.10 | −0.05 | 0.07 |
| Impulsive or acts without thinking | 0.49 | 0.02 | 0.49 | −0.05 | −0.11 |
| Talks about killing self | 0.44 | 0.38 | −0.01 | −0.03 | 0.05 |
| Overtired without good reason | 0.14 | 0.07 | 0.07 | 0.35 | 0.32 |
| Composite (Sex play) | 0.33 | −0.03 | 0.17 | 0.03 | −0.01 |
| Composite (Weight problems) | 0.14 | −0.01 | 0.04 | 0.22 | 0.16 |
| Composite (Hallucinations) | 0.16 | 0.01 | 0.26 | 0.20 | 0.18 |
| Bowel movements outside toilet | 0.13 | −0.07 | 0.12 | 0.14 | 0.19 |
| Trouble sleeping | 0.04 | 0.25 | 0.30 | 0.23 | 0.01 |
| Wets self during the day | 0.08 | −0.01 | 0.25 | 0.12 | 0.17 |
| Wets the bed | 0.13 | −0.10 | 0.15 | 0.07 | 0.06 |
| Wishes to be of opposite sex | 0.07 | 0.11 | 0.11 | −0.01 | 0.24 |
| Clings to adults or too dependent | 0.13 | 0.28 | 0.29 | 0.06 | 0.10 |
| Cries a lot | 0.31 | 0.31 | 0.10 | 0.05 | 0.08 |
| Doesn’t eat well | 0.16 | 0.08 | 0.16 | 0.12 | 0.10 |
| Gets teased a lot | 0.30 | 0.06 | 0.23 | 0.04 | 0.28 |
| Bites fingernails | 0.07 | 0.10 | 0.23 | 0.05 | −0.04 |
| Nightmares | 0.03 | 0.19 | 0.27 | 0.27 | −0.03 |
| Constipated, doesn’t move bowels | −0.01 | 0.13 | 0.11 | 0.29 | 0.09 |
| Picks nose, skin, or other parts of body | 0.17 | 0.09 | 0.33 | 0.08 | −0.04 |
| Prefers being with older kids | 0.30 | −0.02 | 0.20 | 0.11 | 0.03 |
| Sleeps less than most kids | 0.06 | 0.16 | 0.33 | 0.15 | 0.04 |
| Sleeps more than most kids during day and/or night | 0.10 | −0.01 | 0.11 | 0.21 | 0.26 |
| Speech problem | 0.00 | −0.07 | 0.34 | −0.01 | 0.23 |
| Stores up too many things he/she doesn’t need | 0.18 | 0.13 | 0.25 | 0.11 | 0.04 |
| Talks or walks in sleep | 0.02 | 0.03 | 0.24 | 0.25 | −0.14 |
| Thumb-sucking | 0.11 | −0.03 | 0.07 | 0.07 | 0.01 |
| Factor correlations | |||||
| F1 (Externalizing) | 1 | ||||
| F2 (Internalizing) | 0.33 | 1 | |||
| F3 (Neurodevelopmental) | 0.59 | 0.33 | 1 | ||
| F4 (Somatoform) | 0.38 | 0.44 | 0.38 | 1 | |
| F5 (Detachment) | 0.35 | 0.34 | 0.36 | 0.25 | 1 |
Bold indicates primary loadings (≥0.35) with at least 0.10 difference from the second largest loading. All factor correlations were statistically significant (p < 0.001, two-tailed)
CBCL Child Behavior Checklist, F1 externalizing factor, F2 internalizing factor, F3 neurodevelopmental factor, F4 somatoform factor, F5 detachment factor
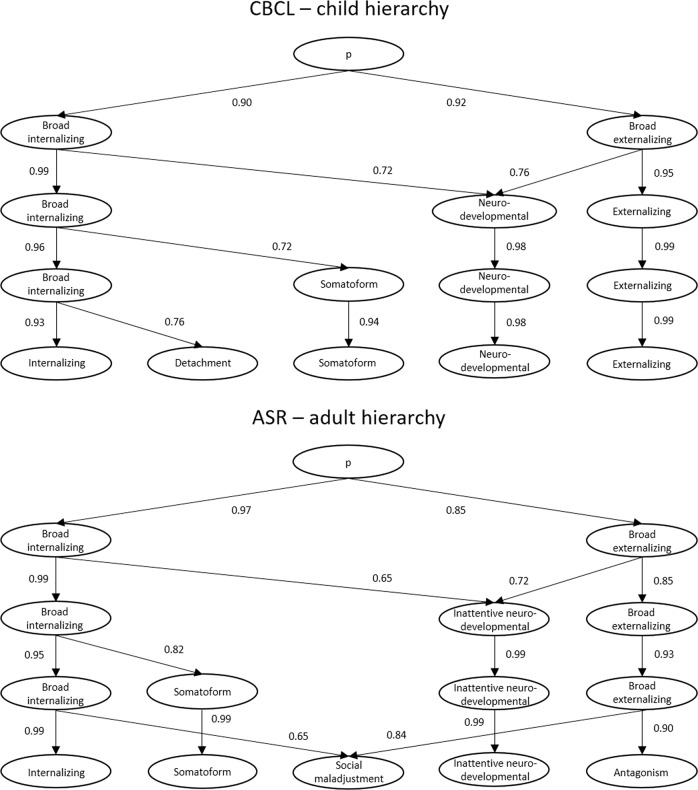
All models from 1-factor to 5-factor were interpretable and are represented as a hierarchical structure (Fig. 1), with paths showing correlations between levels. The 1-factor structure reflected a general childhood psychopathology p-factor5,14. The 2-factor solution revealed the expected broad internalizing and broad externalizing factors15,19,68. In the 3-factor structure, a neurodevelopmental factor (e.g. inattention, hyperactivity, daydreaming, clumsiness) emerged from the broad internalizing and externalizing factors. In the 4-factor solution, somatoform problems emerged from the broad internalizing factor. In the 5-factor structure, the remaining broad internalizing factor split into narrower internalizing problems (e.g. anxiety, depressive symptoms) and detachment (e.g. social withdrawal). Factors in the final 5-factor solution showed small-to-large correlations with one another (r = 0.25−0.59) (Table 1). Comparisons of factor scores across boys and girls indicated small but highly significant (all p ≤ 0.001) sex differences on all dimensions, except broad internalizing in the 2-, 3-, and 4-factor solutions (Supplementary Table 2). Boys showed slightly higher psychopathology on the p-factor, as well as externalizing, neurodevelopmental, and detachment factors in the 5-factor solution, while girls had slightly higher scores on internalizing and somatoform factors.
Fig. 1. Hierarchical models from CBCL items (top half) and ASR items (bottom half) illustrating hierarchies of child and adult psychopathology.
CBCL Childhood Behavior Checklist, ASR Adult Self Report
ASR
Parallel analyses indicated that up to 17 factors could be extracted from ASR items (Supplementary Fig. 1). The 5-factor solution was the most differentiated interpretable structure (Table 2, Supplementary Table 3), as factor solutions with more factors could not be interpreted. For example, the last factor in the 6- and 8-factor models included only two-to-three primary loadings, thus indicating no other meaningful factors beyond five (Supplementary Table 3).
Table 2.
Factor loading (top) and factor correlations (bottom) for the 5-factor solution from the exploratory factor analysis on ASR items
| F1 | F2 | F3 | F4 | F5 | |
|---|---|---|---|---|---|
| Primary loading items | |||||
| I lack self-confidence | 0.73 | 0.05 | 0.22 | −0.07 | −0.13 |
| I worry a lot | 0.72 | −0.11 | −0.04 | 0.15 | 0.18 |
| I am self-conscious or easily embarrassed | 0.72 | 0.06 | 0.06 | −0.05 | −0.08 |
| I feel worthless and inferior | 0.69 | 0.22 | 0.11 | −0.03 | −0.04 |
| Composite (Anxious) | 0.67 | −0.12 | 0.12 | 0.13 | 0.13 |
| I feel too guilty | 0.65 | −0.09 | 0.15 | 0.03 | 0.13 |
| I feel that I have to be perfect | 0.62 | −0.10 | −0.04 | −0.09 | 0.16 |
| I am jealous of others | 0.58 | −0.04 | 0.19 | −0.24 | 0.18 |
| I am too shy or timid | 0.55 | 0.26 | −0.01 | −0.03 | −0.27 |
| I am unhappy, sad, or depressed | 0.54 | 0.22 | 0.06 | 0.20 | −0.02 |
| I feel overwhelmed by my responsibilities | 0.54 | −0.13 | 0.25 | 0.07 | 0.13 |
| I worry about my family | 0.53 | −0.06 | −0.08 | 0.15 | 0.17 |
| I feel lonely | 0.52 | 0.30 | 0.04 | 0.05 | −0.03 |
| I worry about my future | 0.52 | 0.06 | −0.02 | 0.06 | 0.09 |
| I feel that I can’t succeed | 0.46 | 0.20 | 0.22 | 0.01 | −0.07 |
| I can’t get my mind off certain thoughts | 0.40 | 0.06 | 0.14 | 0.15 | 0.19 |
| I blame others for my problems | 0.39 | 0.10 | 0.18 | −0.24 | 0.24 |
| I cry a lot | 0.39 | 0.20 | −0.03 | 0.18 | 0.12 |
| I refuse to talk | 0.21 | 0.60 | −0.01 | 0.09 | −0.04 |
| I have trouble making or keeping friends | 0.38 | 0.58 | 0.05 | −0.08 | −0.12 |
| I do things that may cause me trouble with the law | −0.15 | 0.57 | 0.24 | −0.05 | 0.20 |
| I am not liked by others | 0.28 | 0.57 | 0.00 | −0.05 | 0.06 |
| I don’t get along with other people | 0.15 | 0.56 | −0.06 | −0.01 | 0.15 |
| My relations with the opposite sex are poor | 0.25 | 0.54 | −0.01 | 0.01 | −0.02 |
| I am secretive or keep things to myself | 0.20 | 0.54 | −0.07 | 0.11 | −0.02 |
| I keep from getting involved with others | 0.25 | 0.53 | −0.02 | 0.03 | −0.13 |
| Composite (Hallucinations) | −0.03 | 0.52 | −0.05 | 0.34 | 0.09 |
| I steal | −0.07 | 0.51 | 0.23 | −0.13 | 0.14 |
| Composite (Vandalism) | 0.02 | 0.49 | 0.00 | 0.07 | 0.29 |
| I have trouble keeping a job | 0.04 | 0.48 | 0.22 | 0.05 | 0.03 |
| My relations with neighbors are poor | 0.11 | 0.48 | 0.02 | 0.06 | 0.00 |
| I hang around people who get into trouble | −0.13 | 0.47 | 0.19 | 0.08 | 0.20 |
| I feel that others are out to get me | 0.32 | 0.46 | −0.06 | 0.09 | 0.17 |
| I lie or cheat | 0.02 | 0.44 | 0.20 | −0.10 | 0.19 |
| Composite (Oddness) | −0.01 | 0.43 | 0.19 | 0.10 | 0.15 |
| I would rather be with older people than with people of my own age | 0.04 | 0.43 | −0.04 | 0.22 | 0.04 |
| I think about sex too much | −0.06 | 0.43 | 0.13 | −0.02 | 0.21 |
| I would rather be alone than with others | 0.30 | 0.42 | −0.02 | 0.06 | −0.12 |
| I get along badly with my family | 0.26 | 0.42 | −0.04 | 0.00 | 0.15 |
| I wish I were of the opposite sex | 0.08 | 0.41 | 0.11 | 0.14 | 0.01 |
| I break rules at work or elsewhere | −0.08 | 0.39 | 0.29 | −0.12 | 0.24 |
| I use drugs (other than alcohol, nicotine) for nonmedical purposes | −0.12 | 0.39 | 0.14 | −0.06 | 0.10 |
| I repeat certain acts over and over | 0.10 | 0.38 | 0.07 | 0.18 | 0.16 |
| I don’t feel guilty after doing something I shouldn’t | −0.10 | 0.38 | 0.06 | −0.02 | 0.14 |
| I have a speech problem | −0.03 | 0.36 | 0.19 | 0.16 | −0.07 |
| People think I am disorganized | −0.01 | 0.00 | 0.75 | 0.07 | 0.01 |
| I have trouble setting priorities | 0.18 | 0.06 | 0.72 | −0.04 | −0.05 |
| I fail to finish things I should do | 0.19 | 0.05 | 0.68 | 0.01 | −0.05 |
| I tend to lose things | 0.03 | −0.03 | 0.59 | 0.22 | 0.06 |
| I am not good at details | 0.03 | 0.09 | 0.56 | −0.01 | 0.00 |
| I have trouble concentrating or paying attention for long | 0.09 | −0.06 | 0.56 | 0.21 | 0.09 |
| I am too forgetful | 0.06 | −0.07 | 0.54 | 0.24 | 0.01 |
| My work performance is poor | 0.21 | 0.26 | 0.49 | 0.04 | −0.10 |
| I tend to be late for appointments | 0.01 | −0.04 | 0.49 | 0.02 | 0.08 |
| I have trouble planning for the future | 0.29 | 0.20 | 0.46 | 0.07 | −0.07 |
| I rush into things without considering the risks | −0.05 | 0.23 | 0.40 | 0.04 | 0.27 |
| Composite (Money management) | 0.09 | 0.22 | 0.36 | 0.11 | 0.05 |
| Composite (Nausea) | −0.02 | 0.11 | 0.02 | 0.73 | 0.00 |
| Stomachaches | 0.02 | 0.03 | 0.00 | 0.69 | 0.03 |
| Aches or pains (not stomach or headaches) | −0.06 | 0.05 | 0.08 | 0.67 | 0.03 |
| Headaches | 0.08 | −0.06 | −0.05 | 0.64 | 0.02 |
| Numbness or tingling in body parts | 0.00 | 0.08 | 0.05 | 0.62 | 0.04 |
| I feel dizzy or lightheaded | 0.14 | 0.04 | 0.06 | 0.55 | 0.01 |
| Heart pounding or racing | 0.20 | 0.04 | 0.03 | 0.52 | 0.04 |
| Problems with eyes (not if corrected by glasses) | −0.09 | 0.20 | −0.02 | 0.48 | 0.01 |
| I feel tired without good reason | 0.26 | 0.04 | 0.25 | 0.45 | −0.08 |
| I don’t have much energy | 0.29 | 0.00 | 0.27 | 0.43 | −0.11 |
| Rashes or other skin problems | 0.02 | 0.04 | 0.07 | 0.38 | 0.02 |
| I have trouble sleeping | 0.23 | 0.04 | 0.05 | 0.37 | 0.07 |
| Parts of my body twitch or make nervous movements | 0.12 | 0.17 | 0.16 | 0.37 | 0.09 |
| I am louder than others | −0.05 | −0.09 | 0.22 | 0.05 | 0.63 |
| I have a hot temper | 0.29 | 0.12 | −0.07 | 0.02 | 0.61 |
| I talk too much | −0.01 | −0.22 | 0.29 | 0.08 | 0.56 |
| I argue a lot | 0.31 | 0.06 | −0.03 | −0.09 | 0.55 |
| I scream or yell a lot | 0.31 | 0.08 | −0.07 | 0.04 | 0.54 |
| I am too impatient | 0.32 | −0.03 | 0.17 | 0.00 | 0.49 |
| I tease others a lot | 0.00 | 0.05 | 0.25 | −0.12 | 0.47 |
| I try to get a lot of attention | 0.02 | 0.10 | 0.26 | −0.16 | 0.45 |
| I show off or clown | −0.17 | 0.12 | 0.26 | −0.06 | 0.42 |
| I brag | −0.03 | 0.14 | 0.17 | −0.13 | 0.40 |
| Non-primary loading or cross-loading items | |||||
| I have trouble sitting still | 0.03 | −0.03 | 0.32 | 0.17 | 0.30 |
| I feel restless or fidgety | 0.19 | 0.03 | 0.28 | 0.30 | 0.25 |
| I dislike staying in one place for very long | −0.03 | 0.23 | 0.11 | 0.16 | 0.19 |
| I feel that no one loves me | 0.53 | 0.47 | −0.11 | 0.03 | 0.00 |
| There is very little I enjoy | 0.37 | 0.44 | 0.08 | 0.13 | −0.09 |
| Composite (Suicidality) | 0.37 | 0.42 | 0.06 | 0.06 | −0.03 |
| I get in many fights | 0.08 | 0.37 | −0.01 | 0.07 | 0.43 |
| I am mean to others | 0.09 | 0.37 | −0.03 | −0.07 | 0.40 |
| I sleep more than most other people during day and/or night | 0.08 | 0.17 | 0.19 | 0.30 | −0.06 |
| I stay away from my job even when I’m not sick or not on vacation | −0.04 | 0.35 | 0.26 | 0.09 | 0.02 |
| I worry about my relations with the opposite sex | 0.34 | 0.35 | 0.07 | 0.00 | 0.05 |
| I get upset too easily | 0.51 | 0.05 | −0.01 | 0.05 | 0.48 |
| I am too dependent on others | 0.36 | 0.09 | 0.32 | −0.02 | 0.04 |
| I drive too fast | −0.01 | 0.04 | 0.26 | −0.03 | 0.26 |
| I feel confused or in a fog | 0.32 | 0.10 | 0.31 | 0.28 | 0.00 |
| I daydream a lot | 0.11 | 0.15 | 0.27 | 0.09 | 0.05 |
| I don’t eat as well as I should | 0.21 | 0.00 | 0.21 | 0.18 | 0.05 |
| I am afraid of certain animals, situations, or places | 0.19 | 0.20 | −0.08 | 0.20 | 0.03 |
| I am afraid I might think or do something bad | 0.38 | 0.33 | 0.06 | −0.01 | 0.09 |
| I am impulsive or act without thinking | 0.07 | 0.22 | 0.32 | 0.07 | 0.34 |
| I pick my skin or other parts of my body | 0.18 | 0.01 | 0.22 | 0.05 | 0.09 |
| My behavior is irresponsible | 0.05 | 0.40 | 0.39 | 0.00 | 0.14 |
| I have trouble making decisions | 0.45 | −0.05 | 0.47 | −0.03 | −0.06 |
| My behavior is very changeable | 0.06 | 0.31 | 0.10 | 0.07 | 0.21 |
| I am easily bored | 0.04 | 0.30 | 0.12 | 0.12 | 0.23 |
| I am stubborn, sullen, or irritable | 0.37 | 0.15 | −0.03 | 0.08 | 0.38 |
| I drink too much alcohol or get drunk | −0.02 | 0.17 | 0.23 | −0.09 | 0.15 |
| Composite (Clumsiness) | 0.09 | 0.03 | 0.33 | 0.28 | 0.06 |
| Composite (Moods wings) | 0.31 | 0.29 | 0.03 | 0.24 | 0.26 |
| Composite (Overt aggression) | 0.01 | 0.45 | −0.01 | 0.17 | 0.43 |
| Factor correlations | |||||
| F1 (Internalizing) | |||||
| F2 (Social maladjustment) | 0.43 | ||||
| F3 (Inattentive neurodevelopmental) | 0.44 | 0.45 | |||
| F4 (Somatoform) | 0.50 | 0.40 | 0.32 | ||
| F5 (Antagonism) | 0.19 | 0.41 | 0.31 | 0.27 | |
Bold indicates primary loadings (≥0.35) with at least 0.10 difference from the second largest loading. All factor correlations were statistically significant (p < 0.05, two-tailed)
ASR Adult Self Report, F1 internalizing factor, F2 social maladjustment factor, F3 inattentive neurodevelopmental factor, F4 somatoform factor, F5 antagonism factor
All models from 1-factor to 5-factor are represented in Fig. 1. The 1-factor structure reflected p-factor11. The 2-factor solution showed the broad internalizing and externalizing factors17. In the 3-factor structure, a factor encompassing inattentive neurodevelopmental problems (e.g. inattention, poor planning) emerged from the broad internalizing and externalizing factors. In the 4-factor solution, the broad internalizing factor split into separate internalizing and somatoform dimensions. In the 5-factor structure, rule-breaking behaviors from the broad externalizing factor joined detachment/oddity problems from the broad internalizing factor to form a social maladjustment factor, leaving distinct antagonism and narrower internalizing dimensions. Factors in the final 5-factor solution showed small-to-large correlations with one another (r = 0.19−0.50) (Table 2). Comparisons of factor scores across women and men indicated small but highly significant (all p ≤ 0.001) sex differences on all but the inattentive neurodevelopmental factor in the 3-, 4-, and 5-factor solutions (Supplementary Table 2). Women scored higher than men on the p-factor, as well as on the internalizing, somatoform factors in the 5-factor solution, while men showed higher scores on the social maladjustment and antagonism factors.
Validation analyses
Familial aggregation
Zero-order correlations between the child and adult factor scores from the 5-factor solutions ranged between r = 0.20−0.48 (p < 0.001, two-tailed) (Table 3). The correlation between child and parent p-factor scores was r = 0.61 (p < 0.001, two-tailed). This pattern suggested substantial familial aggregation of a dimension of general psychopathology, explaining co-occurrence across psychopathology dimensions. Controlling for these two p-factors revealed a more specific pattern of familial aggregation between corresponding parent and child dimensions (i.e. convergent correlations). Convergent partial correlations ranged between r = 0.09−0.21 (p < 0.001, two-tailed) and were significantly larger than all partial correlations between non-corresponding factors (i.e. discriminant correlations), based on Fisher’s z tests (Table 3).
Table 3.
Zero-order (top half) and partial correlations (bottom half) between the dimensions in the 5-factor structures from CBCL and ASR items, controlling for childhood and adult p-factors
| ASR | |||||
|---|---|---|---|---|---|
| Internalizing | Social maladjustment | Inattentive neurodevelopmental | Somatoform | Antagonism | |
| Zero-order correlations | |||||
| CBCL | |||||
| Externalizing | 0.42 | 0.44 | 0.40 | 0.38 | 0.38 |
| Internalizing | 0.45 | 0.27 | 0.33 | 0.33 | 0.24 |
| Neurodevelopmental | 0.42 | 0.41 | 0.43 | 0.40 | 0.34 |
| Somatoform | 0.42 | 0.34 | 0.37 | 0.48 | 0.27 |
| Detachment | 0.34 | 0.38 | 0.31 | 0.31 | 0.20 |
| Partial correlations | |||||
| CBCL | |||||
| Externalizing | −0.09 | 0.12 | −0.01 | −0.06 | 0.11 b |
| Internalizing | 0.19 a,b | −0.17 | −0.04 | −0.02 | −0.07 |
| Neurodevelopmental | −0.09 | 0.04 | 0.09 a,b | 0.01 | 0.01 |
| Somatoform | 0.00 | −0.09 | −0.03 | 0.21 a,b | −0.07 |
| Detachment | 0.00 | 0.13 a | −0.02 | 0.00 | −0.10 |
Bold denotes convergent correlations between child and parent dimensions. All zero-order correlations are statistically significant (p < 0.001, two-tailed). Partial correlations r ≥ |0.03| are significant (p < 0.05, two-tailed)
ASR Adult Self Report, CBCL Childhood Behavior Checklist
aIndicates a partial correlation that is significantly higher than all others in the row based on Fisher’s z tests
bIndicates a partial correlation that is significantly higher than all others in the column based on Fisher’s z tests
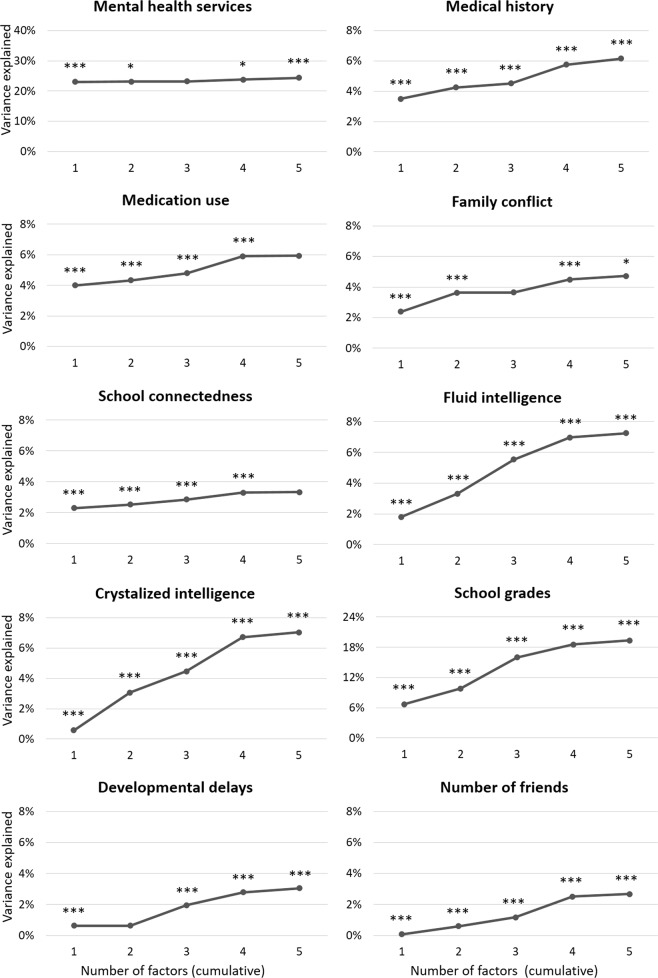
Validity of childhood hierarchical structure
The 1-factor solution was significantly associated with all validators (Fig. 2, Supplementary Table 4). The p-factor alone explained 23.02% of the variance in utilization of mental health services, and the addition of more differentiated factors, although statistically significant, produced minimal improvement in R2 (up to 24.41%). For medication use, medical history, family conflict, and school connectedness, the p-factor alone explained 2.30–4.00% of the variance, and the addition of more complex factor structures provided a moderate increase, contributing up to 3.33–6.16% of variance. The 1-factor model accounted for a relatively small proportion of the variance compared to the more complex factor solutions for fluid intelligence (from 1.79% for p-factor to 7.24% total), crystalized intelligence (0.58% to 7.02%), average grades (6.72% to 19.34%), number of friends (0.08% to 2.67%), and history of developmental delays (0.63% to 3.05%).
Fig. 2. Cumulative explanatory power (R2) for a given factor structure (1- to 5-factor solutions) derived from CBCL data to predict validators.
Nagelkerke R2 is plotted for binary outcomes (mental health service utilization, medical history, medication history). Asterisks indicate significant change in R2 for that structure versus all simpler structures combined (*p < 0.05, **p < 0.01, ***p < 0.001, two-tailed). CBCL Childhood Behavior Checklist
In the 5-factor solution, utilization of mental health services showed the highest but generally non-specific correlations with psychopathology dimensions (r = 0.28–0.46) (Supplementary Table 4). The strongest association for medical history was with the somatoform factor (r = 0.26). Medication use was associated to the same extent with the neurodevelopmental and somatoform factors (both r = 0.22). Crystalized intelligence and school connectedness were associated to a similar extent with the externalizing (r = −0.12), neurodevelopmental, and detachment factors (both r = −0.11). The highest correlation for family conflict was with the externalizing factor (r = 0.19). Fluid intelligence and average grades showed the highest correlations with the neurodevelopmental factor (r = −0.18 and r = −0.33, respectively). Developmental delays were mostly associated with the detachment and neurodevelopmental factors (r = 0.14 and r = 0.10, respectively), while number of friends were mostly associated with detachment (r = −0.13).
Discussion
This study provides the most comprehensive examination of the hierarchy of psychopathology spectra to date—analyzing a wide range of symptoms and maladaptive behaviors, systematically explicating it across multiple hierarchical levels, considering both children and adults, and validating the structure against various clinically relevant measures. In children, we found five spectra at the lowest level of the hierarchy: internalizing, somatoform, detachment, externalizing, and neurodevelopmental. In adults, we observed similar dimensions: internalizing, somatoform, social maladjustment, inattentive neurodevelopmental, and antagonism. We further found substantial familiality of the identified psychopathology factors, largely explained by familial aggregation of the p-factor. Yet, the five childhood dimensions also showed specific links to the corresponding parental dimensions. The p-factor was sufficient to account for some clinical validators (e.g., service utilization), but all five dimensions were needed to explain other validators, such as developmental delays, and social, cognitive, and academic functioning. These findings support the value of explicating multiple higher-order dimensions of psychopathology. They further suggest that the neurodevelopmental spectrum should be considered for inclusion in dimensional models of both childhood and adult psychopathology. Overall, the identified hierarchy depicts robust and informative dimensional phenotypes for the ABCD study baseline assessment, paving the way for future research on this cohort.
In both children and adults, we observed that the p-factor at the top of the hierarchy separates into broad internalizing and broad externalizing spectra. These dimensions mirror the higher-order dimensions first identified by Achenbach and colleagues32. At lower hierarchical levels, the broad internalizing dimension differentiated into internalizing, detachment, and somatoform factors in children. The broad externalizing factor differentiated into narrower externalizing and neurodevelopmental factors in children (the latter originating from both broad externalizing and internalizing). The narrow externalizing factor included aggressive and rule-breaking behaviors, whereas the neurodevelopmental factor encompassed inattention, hyperactivity, and related problems (e.g. clumsiness, daydreaming, obsessions). In adults, instead of detachment as a distinct factor, we found a broader social maladjustment factor encompassing both detachment and antisocial behavior (from the externalizing factor). The differentiation of the externalizing spectrum in adults narrowed to one of its core components, antagonism, which emerged separately from the social maladjustment and inattentive neurodevelopmental factors (both partly originating from the broad internalizing spectrum). This is in line with research showing a separation of antagonism from other externalizing and neurodevelopmental dimensions8,69,70. All observed dimensions are consistent with prior studies, which have identified these factors among major dimensions of psychopathology8,25,32,71. Overall, similar but not identical dimensions were delineated in children and parents, which does not support the hypothesis that psychopathology becomes more differentiated with age14,47.
Our findings are largely consistent with the HiTOP model7,8,72, in that internalizing, antagonism, somatoform, and detachment dimensions were identified in children and/or adults. The adult social maladjustment dimension identified here has the HiTOP detachment spectrum at its core, along with additional content relating to antisocial behavior and a few symptoms of thought disorder (e.g. hallucinations). A thought disorder spectrum was not found either in adults or in children, likely because of the limited number of psychosis symptoms included in the CBCL and ASR, the very low scores on these symptoms in this population-based sample, and the exclusion of children with a diagnosis of schizophrenia based on ABCD recruitment procedures. We observed an additional factor in children that is currently not included in the HiTOP model: a neurodevelopmental dimension that includes inattention, hyperactivity, clumsiness, autistic-like traits, and atypical ideation (e.g. obsessions). Many of the symptoms included in this dimension have previously been proposed to be part of a neurodevelopmental spectrum26 and are consistent with initial factor analytic evidence in children27,28,49. Our results indicate that inattentive and hyperactive symptoms (common in attention-deficit/hyperactivity disorder (ADHD)) also belong to this spectrum, despite previous studies that included ADHD as part of the externalizing spectrum29,31. One explanation for this finding is that many previous EFA studies placing ADHD under the externalizing spectrum examined scale total scores or diagnoses, rather than individual symptoms, and did not include other neurodevelopmental problems—thereby not allowing the delineation of a separate dimension. The emergence of a similar, though narrower, inattentive neurodevelopmental factor in adults is novel, as most previous structural studies of adults have not considered enough attention or neurodevelopmental problems to allow the delineation of this dimension. This finding provides the strongest evidence to date for the inclusion of the neurodevelopmental spectrum in dimensional models of psychopathology. More generally, these findings delineating dimensions of psychopathology both in children and in adults in one of the largest samples available to date represent an important contribution to ongoing efforts seeking to understand the hierarchical structure of psychopathology. Future studies on this cohort and other samples may employ alternative analytic approaches (e.g. bifactor models)11,34,36,55 and instruments (e.g. diagnostic interviews) to examine the reproducibility of the identified dimensions and further advance knowledge of the structure of psychopathology.
By mapping multiple hierarchical levels, we showed that the familial aggregation of psychopathological dimensions in parents and children is largely accounted for by familial influences on the p-factor. This is consistent with the established pleiotropy in the genetic vulnerability to psychopathology19,73,74 and prior evidence of substantial heritability of the p-factor5. In children, the p-factor also accounted for the majority of psychopathology-related variance in several validators, especially utilization of mental health services, which underscores the value of this general dimension for public health and planning of clinical services. However, more specific dimensions also proved to be informative. Familial aggregation between specific dimensions remained significant, albeit reduced, when controlling for child and parent p-factors, and all levels of the hierarchy showed incremental validity, with five dimensions necessary to maximize the explanatory power of psychopathology for most criteria. This supports the importance of examining multiple levels of the psychopathology hierarchy, and is consistent with the view that fine-grained understanding of psychopathology is necessary to fully explicate its etiology75,76 and identify maximally effective treatment77. Further, different dimensions were most important for different validators. For example, the neurodevelopmental dimension had particularly strong links to intelligence and academic achievement, consistent with previous evidence78,79, and the externalizing factor with family conflict, as expected54. These results confirm previous studies showing that both a general factor and specific dimensions are necessary for characterizing youth psychopathology19, school grades, school and neighborhood deprivation14, and executive functioning27. They are inconsistent with studies linking cognitive abilities primarily to the p-factor11,55, potentially because these studies did not model the neurodevelopmental dimension, the strongest correlate of fluid intelligence in this study.
The present study had the following limitations. First, it was limited to one assessment system, thus generalizability of the findings needs to be tested with other measures. Nevertheless, the hierarchy is largely consistent with previous studies using different measures21,23,44,69, suggesting at least partial generalizability. Second, the same parent completed both the CBCL about the child and the ASR about themselves, which may have inflated the similarity between childhood and adult psychopathology structures due to rater biases. In addition, most of the ASR data were provided by mothers or female guardians, therefore the results in the adult sample may not generalize to both sexes. Although these limitation are common to much of the existing literature on parent and offspring psychopathology when children are too young to provide comprehensive self-reports, and a number of our validators were objective (e.g. cognitive testing) or child self-report (e.g. number of friends) measures, future research should replicate the current results with child self-reports and additional co-informant reports. Third, only one time point was included, as longitudinal data were not yet available from the ABCD study at the time of writing. Future waves of data in this unique sample will provide the unprecedented opportunity to examine the hierarchy of psychopathology over the course of development and the predictive validity of childhood factors on a variety of adolescent and young adult outcomes.
In conclusion, the present results clarify the hierarchy of psychopathology dimensions in children and adults using data from one of the largest initiatives to study youth development and psychopathology to date. The study replicates higher-order dimensions identified previously8, and suggests the addition of the neurodevelopmental spectrum to dimensional models of psychopathology. The identified higher-order dimensions represent valid constructs able to explain various clinically relevant risk factors and outcomes, such as developmental delays and academic achievement. Our investigation further provides a guide for future research to use these higher-order psychopathology dimensions in the ABCD sample. New data releases will allow researchers to apply the identified hierarchy to additional clinical, functional, and neuroimaging measures to study psychopathological dimensions during adolescent development.
Supplementary information
Acknowledgements
Drs. Michelini and Kotov are funded by National Institute of Mental Health (NIMH) award number MH117116. Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). The ABCD Study is supported by the National Institutes of Health (NIH) and additional federal partners under award numbers U01DA041022, U01DA041025, U01DA041028, U01DA041048, U01DA041089, U01DA041093, U01DA041106, U01DA041117, U01DA041120, U01DA041134, U01DA041148, U01DA041156, U01DA041174, U24DA041123, and U24DA041147. A full list of federal partners is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/principal-investigators.html. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. The authors would like to thank Avshalom Caspi, PhD (Duke University; King’s College London) and Terrie Moffitt, PhD (Duke University; King’s College London) for their helpful comments on an earlier draft of this manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information accompanies this paper at (10.1038/s41398-019-0593-4).
References
- 1.American Psychiatric Assocation. Diagnostic and Statistical Manual of Mental Disorders, 5th edn (American Psychiatric Publishing, Arlington, VA, 2013).
- 2.World Health Organization. The ICD-10 Classification of Mental And Behavioural Disorders: Diagnostic Criteria for Research, 10th edn (World Health Organization, Geneva, 1992).
- 3.Plomin R, Haworth CM, Davis OS. Common disorders are quantitative traits. Nat. Rev. Genet. 2009;10:872–878. doi: 10.1038/nrg2670. [DOI] [PubMed] [Google Scholar]
- 4.Insel T, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am. J. Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- 5.Caspi A, Moffitt TE. All for one and one for all: mental disorders in one dimension. Am. J. Psychiatry. 2018;175:831–844. doi: 10.1176/appi.ajp.2018.17121383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol. Psychiatry. 2010;15:868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krueger RF, et al. Progress in achieving quantitative classification of psychopathology. World Psychiatry. 2018;17:282–293. doi: 10.1002/wps.20566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kotov R, et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J. Abnorm. Psychol. 2017;126:454–477. doi: 10.1037/abn0000258. [DOI] [PubMed] [Google Scholar]
- 9.Hoertel N, et al. Mental disorders and risk of suicide attempt: a national prospective study. Mol. Psychiatry. 2015;20:718–726. doi: 10.1038/mp.2015.19. [DOI] [PubMed] [Google Scholar]
- 10.Lahey BB, Krueger RF, Rathouz PJ, Waldman ID, Zald DH. A hierarchical causal taxonomy of psychopathology across the life span. Psychol. Bull. 2017;143:142–186. doi: 10.1037/bul0000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caspi A, et al. The p factor: one general psychopathology factor in the structure of psychiatric disorders? Clin. Psychol. Sci. 2014;2:119–137. doi: 10.1177/2167702613497473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lahey BB, et al. Is there a general factor of prevalent psychopathology during adulthood? J. Abnorm. Psychol. 2012;121:971–977. doi: 10.1037/a0028355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martel MM, et al. A general psychopathology factor (P factor) in children: Structural model analysis and external validation through familial risk and child global executive function. J. Abnorm. Psychol. 2017;126:137–148. doi: 10.1037/abn0000205. [DOI] [PubMed] [Google Scholar]
- 14.Patalay P, et al. A general psychopathology factor in early adolescence. Br. J. Psychiatry. 2015;207:15–22. doi: 10.1192/bjp.bp.114.149591. [DOI] [PubMed] [Google Scholar]
- 15.Achenbach, T. M. & Rescorla, L. A. Manual for the ASEBA School-Age Forms & Profiles (University of Vermont, Research Center for Children, Youth, and Families, Burlington, VT, 2001).
- 16.Achenbach, T. M. & Rescorla, L. A. Manual for the ASEBA Adult Forms & Profiles (University of Vermont, Research Center for Children, Youth, and Families, Burlington, VT, 2003).
- 17.Krueger RF. The structure of common mental disorders. Arch. Gen. Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 18.Farmer RF, Seeley JR, Kosty DB, Olino TM, Lewinsohn PM. Hierarchical organization of axis I psychiatric disorder comorbidity through age 30. Compr. Psychiatry. 2013;54:523–532. doi: 10.1016/j.comppsych.2012.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Waldman ID, Poore HE, van Hulle C, Rathouz PJ, Lahey BB. External validity of a hierarchical dimensional model of child and adolescent psychopathology: tests using confirmatory factor analyses and multivariate behavior genetic analyses. J. Abnorm. Psychol. 2016;125:1053–1066. doi: 10.1037/abn0000183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99:1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- 21.Kotov R, et al. New dimensions in the quantitative classification of mental illness. Arch. Gen. Psychiatry. 2011;68:1003–1011. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- 22.Kim H, Eaton NR. The hierarchical structure of common mental disorders: connecting multiple levels of comorbidity, bifactor models, and predictive validity. J. Abnorm. Psychol. 2015;124:1064–1078. doi: 10.1037/abn0000113. [DOI] [PubMed] [Google Scholar]
- 23.Wright AG, et al. The hierarchical structure of DSM-5 pathological personality traits. J. Abnorm. Psychol. 2012;121:951–957. doi: 10.1037/a0027669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blanco C, et al. Mapping common psychiatric disorders: structure and predictive validity in the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry. 2013;70:199–208. doi: 10.1001/jamapsychiatry.2013.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roysamb E, et al. The joint structure of DSM-IV Axis I and Axis II disorders. J. Abnorm. Psychol. 2011;120:198–209. doi: 10.1037/a0021660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andrews G, Pine DS, Hobbs MJ, Anderson TM, Sunderland M. Neurodevelopmental disorders: cluster 2 of the proposed meta-structure for DSM-V and ICD-11. Psychol. Med. 2009;39:2013–2023. doi: 10.1017/S0033291709990274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bloemen AJP, et al. The association between executive functioning and psychopathology: general or specific? Psychol. Med. 2018;48:1787–1794. doi: 10.1017/S0033291717003269. [DOI] [PubMed] [Google Scholar]
- 28.Noordhof A, Krueger RF, Ormel J, Oldehinkel AJ, Hartman CA. Integrating autism-related symptoms into the dimensional internalizing and externalizing model of psychopathology. The TRAILS Study. J. Abnorm. Child Psychol. 2015;43:577–587. doi: 10.1007/s10802-014-9923-4. [DOI] [PubMed] [Google Scholar]
- 29.Carragher N, et al. ADHD and the externalizing spectrum: direct comparison of categorical, continuous, and hybrid models of liability in a nationally representative sample. Soc. Psychiatry Psychiatr. Epidemiol. 2014;49:1307–1317. doi: 10.1007/s00127-013-0770-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tackett JL, et al. Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. J. Abnorm. Psychol. 2013;122:1142–1153. doi: 10.1037/a0034151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blanco C, et al. The space of common psychiatric disorders in adolescents: comorbidity structure and individual latent liabilities. J. Am. Acad. Child Adolesc. Psychiatry. 2015;54:45–52. doi: 10.1016/j.jaac.2014.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Achenbach TM. The classification of children’s psychiatric symptoms: a factor-analytic study. Psychol. Monogr. 1966;80:1–37. doi: 10.1037/h0093906. [DOI] [PubMed] [Google Scholar]
- 33.Slobodskaya HR. The contribution of reinforcement sensitivity to the personality-psychopathology hierarchical structure in childhood and adolescence. J. Abnorm. Psychol. 2016;125:1067–1078. doi: 10.1037/abn0000179. [DOI] [PubMed] [Google Scholar]
- 34.Lahey, B. B. et al. Measuring the hierarchical general factor model of psychopathology in young adults. Int. J. Methods Psychiatr. Res. 27, e1593 (2018). [DOI] [PMC free article] [PubMed]
- 35.Snyder HR, Young JF, Hankin BL. Strong homotypic continuity in common psychopathology-, internalizing-, and externalizing-specific factors over time in adolescents. Clin. Psychol. Sci. 2017;5:98–110. doi: 10.1177/2167702616651076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Haltigan JD, et al. “P” and “DP:” examining symptom-level bifactor models of psychopathology and dysregulation in clinically referred children and adolescents. J. Am. Acad. Child Adolesc. Psychiatry. 2018;57:384–396. doi: 10.1016/j.jaac.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 37.Ghirardi, L. et al. The familial co-aggregation of ASD and ADHD: a register-based cohort study. Mol. Psychiatry23, 257–262 (2017). [DOI] [PMC free article] [PubMed]
- 38.Cheung CH, Frazier-Wood AC, Asherson P, Rijsdijk F, Kuntsi J. Shared cognitive impairments and aetiology in ADHD symptoms and reading difficulties. PLoS ONE. 2014;9:e98590. doi: 10.1371/journal.pone.0098590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Franke B, et al. Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. Eur. Neuropsychopharmacol. 2018;28:1059–1088. doi: 10.1016/j.euroneuro.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kuntsi J, et al. Co-occurrence of ADHD and low IQ has genetic origins. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2004;124B:41–47. doi: 10.1002/ajmg.b.20076. [DOI] [PubMed] [Google Scholar]
- 41.Pinto R, Rijsdijk F, Ronald A, Asherson P, Kuntsi J. The genetic overlap of attention-deficit/hyperactivity disorder and autistic-like traits: an investigation of individual symptom scales and cognitive markers. J. Abnorm. Child Psychol. 2016;44:335–345. doi: 10.1007/s10802-015-0037-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Asherson P, Buitelaar J, Faraone SV, Rohde LA. Adult attention-deficit hyperactivity disorder: key conceptual issues. Lancet Psychiatry. 2016;3:568–578. doi: 10.1016/S2215-0366(16)30032-3. [DOI] [PubMed] [Google Scholar]
- 43.Goldberg LR. Doing it all bass-ackwards: the development of hierarchical factor structures from the top down. J. Res. Pers. 2006;40:347–358. doi: 10.1016/j.jrp.2006.01.001. [DOI] [Google Scholar]
- 44.Forbes MK, et al. Delineating the joint hierarchical structure of clinical and personality disorders in an outpatient psychiatric sample. Compr. Psychiatry. 2017;79:19–30. doi: 10.1016/j.comppsych.2017.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Morey LC, Krueger RF, Skodol AE. The hierarchical structure of clinician ratings of proposed DSM-5 pathological personality traits. J. Abnorm. Psychol. 2013;122:836–841. doi: 10.1037/a0034003. [DOI] [PubMed] [Google Scholar]
- 46.Tackett JL, Quilty LC, Sellbom M, Rector NA, Bagby RM. Additional evidence for a quantitative hierarchical model of mood and anxiety disorders for DSM-V: the context of personality structure. J. Abnorm. Psychol. 2008;117:812–825. doi: 10.1037/a0013795. [DOI] [PubMed] [Google Scholar]
- 47.McElroy E, Belsky J, Carragher N, Fearon P, Patalay P. Developmental stability of general and specific factors of psychopathology from early childhood to adolescence: dynamic mutualism or p-differentiation? J. Child Psychol. Psychiatry. 2018;59:667–675. doi: 10.1111/jcpp.12849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Andrews G, et al. Exploring the feasibility of a meta-structure for DSM-V and ICD-11: could it improve utility and validity? Psychol. Med. 2009;39:1993–2000. doi: 10.1017/S0033291709990250. [DOI] [PubMed] [Google Scholar]
- 49.Pettersson E, Lahey BB, Larsson H, Lichtenstein P. Criterion validity and utility of the general factor of psychopathology in childhood: predictive associations with independently measured severe adverse mental health outcomes in adolescence. J. Am. Acad. Child Adolesc. Psychiatry. 2018;57:372–383. doi: 10.1016/j.jaac.2017.12.016. [DOI] [PubMed] [Google Scholar]
- 50.Ormel J, et al. Functional outcomes of child and adolescent mental disorders. Current disorder most important but psychiatric history matters as well. Psychol. Med. 2017;47:1271–1282. doi: 10.1017/S0033291716003445. [DOI] [PubMed] [Google Scholar]
- 51.Garavan H, et al. Recruiting the ABCD sample: design considerations and procedures. Dev. Cogn. Neurosci. 2018;32:16–22. doi: 10.1016/j.dcn.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barch DM, et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: rationale and description. Dev. Cogn. Neurosci. 2018;32:55–66. doi: 10.1016/j.dcn.2017.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Luciana M, et al. Adolescent neurocognitive development and impacts of substance use: overview of the adolescent brain cognitive development (ABCD) baseline neurocognition battery. Dev. Cogn. Neurosci. 2018;32:67–79. doi: 10.1016/j.dcn.2018.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jarnecke AM, et al. The role of parental marital discord in the etiology of externalizing problems during childhood and adolescence. Dev. Psychopathol. 2017;29:1177–1188. doi: 10.1017/S095457941600122X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lahey BB, et al. Criterion validity of the general factor of psychopathology in a prospective study of girls. J. Child Psychol. Psychiatry. 2015;56:415–422. doi: 10.1111/jcpp.12300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Karcher, N. R., O’Brien, K. J., Kandala, S. & Barch, D. M. Resting-state functional connectivity and psychotic-like experiences in childhood: results from the adolescent brain cognitive development study. Biol. Psychiatry86, 7–15 (2019). [DOI] [PMC free article] [PubMed]
- 57.Thompson WK, et al. The structure of cognition in 9 and 10 year-old children and associations with problem behaviors: findings from the ABCD study’s baseline neurocognitive battery. Dev. Cogn. Neurosci. 2019;36:100606. doi: 10.1016/j.dcn.2018.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Compton, W. M., Dowling, G.J. & Garavan, H. Ensuring the best use of data: the Adolescent Brain Cognitive Development Study. JAMA Pediatr. Epub ahead of print (2019). [DOI] [PMC free article] [PubMed]
- 59.Auchter AM, et al. A description of the ABCD organizational structure and communication framework. Dev. Cogn. Neurosci. 2018;32:8–15. doi: 10.1016/j.dcn.2018.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Clark DB, et al. Biomedical ethics and clinical oversight in multisite observational neuroimaging studies with children and adolescents: the ABCD experience. Dev. Cogn. Neurosci. 2018;32:143–154. doi: 10.1016/j.dcn.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Loney J, Carlson GA, Salisbury H, Volpe RJ. Validation of three dimensions of childhood psychopathology in young clinic-referred boys. J. Atten. Disord. 2005;8:169–181. doi: 10.1177/1087054705279298. [DOI] [PubMed] [Google Scholar]
- 62.Moos RH. Conceptual and empirical approaches to developing family-based assessment procedures: resolving the case of the Family Environment Scale. Fam. Process. 1990;29:199–208. doi: 10.1111/j.1545-5300.1990.00199.x. [DOI] [PubMed] [Google Scholar]
- 63.Zucker RA, et al. Assessment of culture and environment in the Adolescent Brain and Cognitive Development Study: Rationale, description of measures, and early data. Dev. Cogn. Neurosci. 2018;32:107–120. doi: 10.1016/j.dcn.2018.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Floyd FJ, Widaman KF. Factor analysis in the development and refinement of clinical assessment instruments. Psychol. Assess. 1995;7:286. doi: 10.1037/1040-3590.7.3.286. [DOI] [Google Scholar]
- 65.Fabrigar LR, Wegener DT, MacCallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychol. Methods. 1999;4:272–299. doi: 10.1037/1082-989X.4.3.272. [DOI] [Google Scholar]
- 66.Velicer WF, Fava JL. Affects of variable and subject sampling on factor pattern recovery. Psychol. Methods. 1998;3:231. doi: 10.1037/1082-989X.3.2.231. [DOI] [Google Scholar]
- 67.Kotov R, et al. Validating dimensions of psychosis symptomatology: neural correlates and 20-year outcomes. J. Abnorm. Psychol. 2016;125:1103–1119. doi: 10.1037/abn0000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Markon KE, Krueger RF, Watson D. Delineating the structure of normal and abnormal personality: an integrative hierarchical approach. J. Pers. Soc. Psychol. 2005;88:139–157. doi: 10.1037/0022-3514.88.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wright AG, Simms LJ. A metastructural model of mental disorders and pathological personality traits. Psychol. Med. 2015;45:2309–2319. doi: 10.1017/S0033291715000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Patrick CJ, Kramer MD, Krueger RF, Markon KE. Optimizing efficiency of psychopathology assessment through quantitative modeling: development of a brief form of the Externalizing Spectrum Inventory. Psychol. Assess. 2013;25:1332–1348. doi: 10.1037/a0034864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Markon KE. Modeling psychopathology structure: a symptom-level analysis of Axis I and II disorders. Psychol. Med. 2010;40:273–288. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- 72.Kotov R, Krueger RF, Watson D. A paradigm shift in psychiatric classification: the Hierarchical Taxonomy of Psychopathology (HiTOP) World Psychiatry. 2018;17:24–25. doi: 10.1002/wps.20478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Michelini G, Eley TC, Gregory AM, McAdams TA. Aetiological overlap between anxiety and attention deficit hyperactivity symptom dimensions in adolescence. J. Child Psychol. Psychiatry. 2015;56:423–431. doi: 10.1111/jcpp.12318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Stringaris A, Zavos H, Leibenluft E, Maughan B, Eley TC. Adolescent irritability: phenotypic associations and genetic links with depressed mood. Am. J. Psychiatry. 2012;169:47–54. doi: 10.1176/appi.ajp.2011.10101549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pettersson E, Larsson H, Lichtenstein P. Common psychiatric disorders share the same genetic origin: a multivariate sibling study of the Swedish population. Mol. Psychiatry. 2016;21:717–721. doi: 10.1038/mp.2015.116. [DOI] [PubMed] [Google Scholar]
- 76.Waszczuk MA, Zavos HM, Gregory AM, Eley TC. The phenotypic and genetic structure of depression and anxiety disorder symptoms in childhood, adolescence, and young adulthood. JAMA Psychiatry. 2014;71:905–916. doi: 10.1001/jamapsychiatry.2014.655. [DOI] [PubMed] [Google Scholar]
- 77.Gershon S, Chengappa KN, Malhi GS. Lithium specificity in bipolar illness: a classic agent for the classic disorder. Bipolar Disord. 2009;11:34–44. doi: 10.1111/j.1399-5618.2009.00709.x. [DOI] [PubMed] [Google Scholar]
- 78.Michelini, G. et al. The etiological structure of cognitive-neurophysiological impairments in ADHD in adolescence and young adulthood. J. Atten. Disord. 1087054718771191 (2018). [DOI] [PMC free article] [PubMed]
- 79.Kim SH, Bal VH, Lord C. Longitudinal follow-up of academic achievement in children with autism from age 2 to 18. J. Child Psychol. Psychiatry. 2018;59:258–267. doi: 10.1111/jcpp.12808. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.