Abstract
Physician associates (PAs) are a relatively new medical professional group working as part of the multidisciplinary team to deliver patient care. This article aims to look at how PAs can work effectively in teams, highlighting the benefits and current working practices of PAs across the NHS and address the concerns and challenges raised.
KEYWORDS: Physician associates, medical teams, multidisciplinary teams
The concept of team-based care and team working is not new in healthcare. As early as 1920, the idea was documented in a report to the UK minister for health,1 a time at which ‘doctor-centric’ service delivery was the norm. Since then, healthcare has changed significantly; patients are rarely looked after by just one healthcare professional,2 medical teams work collaboratively with other members of the multidisciplinary team (MDT) and the practice of medicine is no longer the exclusive domain of the doctor.
Over recent years, the NHS has been facing increasing challenges including concerns over funding, workforce shortages (an estimated 10,000 doctor shortages in England and a 100,000 across all staff groups, with this number predicted to rise),3 mounting inequalities in healthcare and pressures from a growing and ageing population.4 In this ever-increasing complex and changing healthcare system, effective teamwork is essential to both improve patient outcomes and experience and to support the wellbeing of the healthcare workforce.5
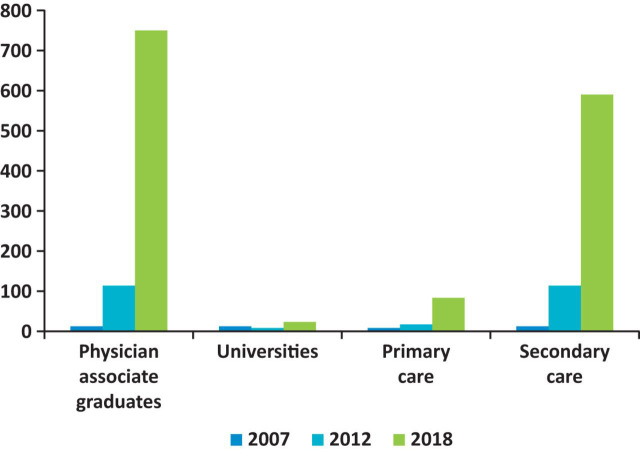
Physician associates (PAs) were introduced to the UK health service in 2003 in small numbers,6, 7 however the last 10 years has seen rapid expansion of the profession with PAs increasingly becoming an integral part of the medical team. In 2017, there were over 600 qualified PAs across the four countries of the UK.8 It is estimated currently that there are approximately 1,400 PAs and by 2020 there will be 3,200 PAs employed in the UK workforce (Fig 1).9 PAs are working across primary and secondary care in a wide variety of medical specialties and undertaking a range of clinical tasks.8
Fig 1.
Growth of physician associates in the UK.
PAs are trained as medical generalists. A UK qualified PA will have undertaken a Master's-level university programme based on a national curriculum and will have passed a national certification examination.10 PAs must also sit a national recertification examination every 6 years in order to maintain their generalist knowledge across the breadth of medicine. These elements enable PAs to remain generalists, even when working in specialties, providing a uniquely flexible workforce across the NHS.
Currently, a lack of statutory regulation and prescribing authority is restricting the PAs’ scope of practice. However, with the government’s commitment to regulation of the profession11 and further work and consultation on prescribing planned, PAs should be able to work to their full scope in future. PAs are described as dependent medical professionals. The strength of being a dependent clinician is the close team working which improves patient safety and outcomes. PAs, however, can work independently, make autonomous decisions and are professionally accountable for their practice. However, the ultimate responsibility for the patient lies with the consultant physician / general practitioner.
Although not currently statutorily regulated (the profession is going to be regulated by the General Medical Council) there is the Physician Associate Managed Voluntary Register (PAMVR) held by the Faculty of Physician Associates (FPA) at the Royal College of Physicians (RCP); it is expected that all qualified PAs should be on the register.12
How PAs can work in medical teams
As with anything new, PAs have been viewed with a degree of apprehension by the existing healthcare workforce. Recent research has shown that PAs were found to be acceptable, appropriate and safe members of the medical and surgical teams by the majority of doctors, managers and nurses.13 Forty-three PAs, 77 other healthcare professionals, 28 managers, and 28 patients and relatives participated in the study. The results showed that PAs were mainly deployed to undertake inpatient ward work in the medical/surgical team during core weekday hours. They were reported to positively contribute to continuity within their medical/surgical team, patient experience and flow, inducting new junior doctors and supporting the medical/surgical teams’ workload, which released doctors for more complex patients and their training.13
Calderdale and Huddersfield NHS Foundation Trust (CHFT) employs 19 PAs and provides a good example of how PAs can work across an organisation in a range of specialties. Below, PAs describe their scope of practice and how they currently work within their teams.
Melissa Prior-Ong, PA in medicine:
I take part in the ward round as it gives me the opportunity to be visible, get to know staff, patients and their management plans and discuss differentials. I also clerk, diagnose and formulate management plans for patients. My responsibilities have grown with competency and experience. I now help to support new junior colleagues, provide teaching to all professionals across the MDT and students, review acutely unwell patients, and admit and discharge patients with senior support. The presence of PAs on the team enables continuity and support particularly during the junior doctor change-over periods.
Rehma Sayed, Zuby Hasan and Sunita Gurung, PAs in general surgery:
In addition to the busy day-to-day workings of surgical inpatient care, we have been running telephone triage clinics for fast-track referrals and are increasingly involved in audit meetings, mortality, and morbidity reviews and research.
Ben Calow, PA in general medicine, has outlined the range of clinical skills that the PAs undertake which helps support the team and provide timely patient care:
PAs in the trust have gained competency in catheterisation, nasogastric tube insertion and placement interpretation, cannulation and venepuncture including ultrasound guided cannulation, arterial blood gas and analysis, abdominal aspiration and paracentesis, lumbar puncture both diagnostic and therapeutic, joint aspirations, chest drain management including flushing and talc pleurodesis, airway management (acute situations) including oropharyngeal, nasopharyngeal and supraglottic airway insertion, and advanced life support. One of our PAs has been trained to perform bone marrow biopsies.
The trust has seen and reaped the benefits of having PAs as part of their medical workforce. Dr Sarah Hoye, medical consultant and trust lead for PAs, states:
The PAs have become an integral part of the CHFT workforce both in medicine and surgery. They have become accustomed to working in an MDT as they rotate through a variety of specialties, and provide excellent support to ward rounds and the jobs generated as a result. They are an important part of our team, and the workforce stability is welcomed.
Although PAs are trained as generalists and expected to maintain this generalism throughout their career, they do work in specialty areas and obtain additional specialist knowledge and skills to deliver the care required in their teams.
Christopher Meally, PA in cardiology at George Eliot Hospital, gives an example of his role in this specialty:
I have worked as PA in cardiology since 2014 on a 12 bedded coronary care unit where I manage patients with acute coronary syndromes, heart failure and arrhythmias. I am closely involved with supporting students, nurses and junior doctors. With increasing experience, I have been able to help with several service developments (cardioversion and inpatient angiography).
This has been of benefit to the medical team and the MDT that he works with. The junior doctor working with Chris advised:
Prior to working with the cardiology team, I had not had any experience of working with PAs and knew very little of their day-to-day role. The PA has proven to be a valuable asset to the medical team and it appears clear that PAs can function at the same level or above their junior doctor counterparts.
The matron on the ward stated:
Nurses on the ward have confidence in the role of the PA. The PA has become an excellent role model for the junior doctors due to his specialist knowledge. His role enables him to do tasks that assist both the nurses and junior doctors, which frees up their valuable time. He has devoted a lot of time into end-stage heart failure and has been heavily involved with end-of-life care planning for the safe and supported discharge of these patients. The nursing staff find him approachable and we would class him as a valued member of our ward team.
It is abundantly clear that while a PA practices medicine, they are not a doctor, with no like-for-like equivalency and therefore cannot replace a doctor. However, working in the medical team will mean that there is overlap of knowledge and skills between professional groups. Acknowledgement and maximisation of this overlap can be advantageous for the team in the redistribution of the workload, provision of training opportunities for all staff and, ultimately, benefit patients, ensuring that the right person, with the right skills, sees the right patient at the right time.
Surrey and Sussex Healthcare NHS Trust employs over 15 PAs across the organisation in a variety of specialties and have been trailblazing in how they employ, integrate, support and develop PAs within their trust.
Moni Choudhury, PA in acute medicine, describes how her role has developed over the last 6 years and how working as part of the medical team helps with workload distribution ensuring that quality patient care is delivered in a timely manner by the most appropriate person:
In my first year, I was largely ward based working directly with the consultants to deliver ward rounds and seeing new patients. Over the last 5 years, my clinical development has been steep but thoroughly enjoyable. I have been able to deal with more complex patients and developed my role further by training in focused acute medical ultrasound. This has enabled me to support my colleagues in diagnosis and management and in delivering excellent patient-centred care. My experience in clinical practice has been invaluable in working as part of an MDT. Over the busy winter period and bank holidays I have worked additional hours to support the on-call ward cover team. I have worked alongside the on-call medical registrar assisting them with patient reviews and ward tasks such as scribing for them, taking bloods and arterial gases and supporting the crash team. This has been valuable for my own learning but also for relieving some of the work pressures the doctors experience. As a result, I am someone who knows the hospital well and my contribution has helped junior doctors, locum doctors, consultants, new PAs and students in optimising patient care and understanding the hospital system.
PA working patterns
PAs across the UK work a wide range of shift patterns, including medical rotas where the appropriate support and supervision is available.
Claire McDonald and Dr Sarah Hoye at CHFT describe the benefits of PAs working on medical rotas and in shift patterns.
Claire McDonald, PA in medicine:
The PAs are on a 2-year rotational programme, changing departments every 4 months. I have found it very useful getting to know how different specialties work within our trust and meeting other members of the workforce during my rotations. All the PAs in medicine are also on a one in five rolling rota for our weekend and twilights shifts that are on the medical assessment unit across both sites. During these shifts we work alongside the on-call team, giving us the opportunity for clerking and thus ensuring we remain generalists.
Dr Sarah Hoye, consultant:
The PAs are involved in out-of-hours working and clerk new patients arriving to our acute medicine units. As their trust lead and supervisor, I have seen an increase in confidence and competence over the last few months and witnessed thoroughness and information gathering to a high standard. They are able to diagnose accurately and make sensible differentials, plus recommend an initial investigation and treatment plan. Their documentation is excellent. I always appreciate having a PA on my ward round and twilight shift, as working together with the consultant is time efficient.
Developing the PA in the medical team
The support and postgraduate education will depend on the level and experience of the PA, the area that they choose to work in, the needs of the service and what the PA might like to do. Trusts may choose to have an internship/rotational period for a new graduate PA or for the PA to work in a specific area only. What is important, however, is that adequate time is spent on preparing the organisation, patients and team in order for the PA to work effectively and that they are supported and developed. While this may be initially time intensive, it will reap its own rewards with PAs feeling valued and invested in, leading to higher retention rates, workforce stability, consistent service delivery, and continuity for both patients and the team.
Robert Deans and Sarah Vigor describe their experiences of working at Surrey and Sussex Healthcare NHS Trust.
Robert Deans, a new graduate PA working in acute medicine:
I started 2 months ago as a recent graduate. I’ve felt the integration into the team has been a really smooth process. It’s certainly a steep learning curve from being a student, however the support provided has been both excellent and necessary. While as a new PA, I can help share the workload and tasks, I feel it’s important to also have support from the team with these jobs while we get used to the system/responsibilities. The support and training we receive also means we are very aware to work within our competencies. For example, knowing when to escalate an unwell patient we can’t manage. I have found a really strong emphasis on teamwork at Surrey and Sussex Healthcare. I believe this is integral to both good patient care and making the best use of PAs. Because we can help out with jobs, I feel we are appreciated by the doctors, and PAs certainly appreciate the help and support doctors provide, such as prescribing. This feeds back into positive teamwork as we develop mutual respect.
Sarah Vigor, lead PA with 9 years’ experience:
We are fortunate to have a trust that has embraced the PA profession in its entirety and, as such, we have wonderful and supportive teams. Through this support, we have been able to develop our PA roles across the trust ensuring PAs have the opportunity to grow within their interest and demands of their departments. My colleagues and I have become relied upon team members without whom, departments would be left short staffed. We know the trust well and help induct our doctors through rotational periods, which is particularly useful in August. We have great relationships with not just our supervisors but with other specialty consultants and teams who have got to know the PAs across the trust well. This makes referrals and discussions efficient which enables us to strive for the best for our patients.
Governance structures
PAs must be able to work safely and effectively and developed to their full potential. This requires appropriate supervision, governance, polices and guidance. As medical professionals, PAs should be medically line managed, this includes annual appraisal (with evidence of personal and professional development, competencies and capabilities demonstrated through the use of a portfolio), continuing professional development (CPD) and checking of the PAMVR. The FPA have developed an employer’s guide to advise on PAs and are about to launch a toolkit for PAs to give guidance regarding portfolios, CPD and forms that may be used for appraisal purposes.14
Many organisations have a lead PA or a champion (generally a senior doctor) for PAs who oversee, coordinate and lead on the development of the PAs in the organisation, PA student placements, policy and governance, and advise the organisation on PA matters.
Conclusion
As population healthcare needs change, the trend towards teams of healthcare professionals from various disciplines working together to deliver coordinated patient care is undeniable.15 There are simply not enough healthcare professionals to manage the increased activity and unmet healthcare needs. As evidenced, PAs have a lot to offer healthcare teams in terms of continuity of patient care, improved patient outcomes, redistribution of the medical workload and increased training and development opportunities for all team members. Collaboration is therefore key to creating mutually beneficial and supportive working arrangements based on skill mix and not job title.16
For PAs to work effectively, organisations and medical teams need to be prepared to integrate, support and progress the PA, enabling them to practice to their full potential. This should be in addition to and not at the expense of any other healthcare professional team member. Resources are available for organisations who want to employ PAs from the FPA and from medical teams who are successfully utilising PAs in their workforce, clearly demonstrating that there is no ‘I’ in team, but there may be a PA.
Declaration of interests
Jeannie Watkins is a founder and director of the recruitment organisation PAs Transforming Healthcare (PATH).
References
- 1.Addison C. Future provision of medical services: report of the Medical Consultative Council for England. Br Med J. 1920;1:739–743. doi: 10.1136/bmj.1.3100.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Babiker A, El Husseini M, Al Nemri A. Health care professional development: Working as a team to improve patient care. Sudan J Paediatr. 2014;14:9–16. [PMC free article] [PubMed] [Google Scholar]
- 3.Buchan J, Charlesworth A, Gershlick B, Seccome I. A critical moment: NHS staffing trends, retention and attrition. The Health Foundation; London: 2019. www.health.org.uk/publications/reports/a-critical-moment [Accessed 06 June 2019] [Google Scholar]
- 4.NHS . The NHS long term plan. NHS; 2019. [Google Scholar]
- 5.Royal College of Physicians . Improving teams in healthcare: Resource 1: Building effective teams. RCP; London: 2017. [Google Scholar]
- 6.Woodin J, McLeod H, McManus R, Jelphs K. Evaluation of US-trained Physician Assistants working in the NHS in England. University of Birmingham; Birmingham: 2005. www.birmingham.ac.uk/Documents/college-social-sciences/social-policy/HSMC/publications/2005/Evaluation-of-US-trained-Physician-Assistants.pdf [Accessed 31 May 2019] [Google Scholar]
- 7.Farmer J, Currie M, Hyman J, et al. Evaluation of physician assistants in National Health Service Scotland. Scott Med J. 2011;56:130–134. doi: 10.1258/smj.2011.011109. [DOI] [PubMed] [Google Scholar]
- 8.Ritsema T. Faculty of PAs census results. Royal College of Physicians; London: 2018. www.fparcp.co.uk/about-fpa/fpa-census [Accessed 31 May 2019] [Google Scholar]
- 9.Aiello M, Roberts KA. Development of the United Kingdom physician associate profession. JAAPA. 2017;30:1–8. doi: 10.1097/01.JAA.0000513357.68395.12. https://capa-acam.ca/wp-content/uploads/2017/05/2017-Aiello-Roberts-UK-PA-Development.pdf [Accessed 31 May 2019] [DOI] [PubMed] [Google Scholar]
- 10.Faculty of Physician Associates . Competence and curriculum framework for the physician assistant. Royal College of Physicians; London: 2012. www.fparcp.co.uk/employers/guidance [Accessed 31 May 2019] [Google Scholar]
- 11.Department of Health & Social Care . The regulation of medical associate professionals in the UK: Consultation response. DHSC; 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/777130/maps-consultation-report.pdf [Accessed 31 May 2019] [Google Scholar]
- 12.Faculty of Physician Associates . Physician Associate Managed Voluntary Register (PAMVR) Royal College of Physicians; London: 2019. www.fparcp.co.uk/employers/pamvr [Accessed 13 June 2019] [Google Scholar]
- 13.Drennan VM, Halter M, Wheeler C, et al. What is the contribution of physician associates in hospital care in England? A mixed methods, multiple case study. BMJ Open. 2019;9:027012. doi: 10.1136/bmjopen-2018-027012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Faculty of Physician Associates . An employer’s guide to physician associates. Royal College of Physicians; London: 2019. www.fparcp.co.uk/employers/guidance [Accessed 13 June 2019] [Google Scholar]
- 15.Chamberlain-Salaun J, Mills J, Usher K. Terminology used to describe health care teams: an integrative review of the literature. J Multidiscip Healthc. 2013;6:65–74. doi: 10.2147/JMDH.S40676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.King N. Medical associate professionals: we need to challenge traditional hierarchy to keep patients at the centre of what we do. BMJ. 2019;365:l. doi: 10.1136/bmj.l2394. https://blogs.bmj.com/bmj/2019/05/28/natalie-king-medical-associate-professionals-we-need-to-challenge-traditional-hierarchy-to-keep-patients-at-the-centre-of-what-we-do [Accessed 15 June 2019] [DOI] [PubMed] [Google Scholar]