ABSTRACT
Background
Flipped learning is an approach in which core teaching is delivered using online material viewed prior to face-to-face learning, applying knowledge gained from online material. Core teaching in a module for third-year undergraduate medical students was based around a 1-week course comprising 32 hours of lectures. Feedback suggested that students were poorly engaged and attendance was poor.
Objectives
To develop and evaluate a programme of learning for medical students using flipped learning.
Methods
Core lectures were videoed and students were advised to watch online at home in the morning prior to a case-based interactive discussion session in the afternoon. Feedback was undertaken prior to and following change in delivery; changes in Likert scale feedback were assessed. Thematic assessment of free-text feedback was undertaken. Results of in-course assessment examinations were compared prior to and following change in delivery.
Results
Student feedback showed a significant improvement in satisfaction with flipped learning compared to standard lectures, both in scores and free-text feedback. Results of in-course assessments did not change between the two methods of delivery.
Conclusions
Flipped learning can improve student satisfaction and engagement with teaching, but our study has not demonstrated an improvement in assessment scores.
KEYWORDS: Medical education, flipped learning
Introduction
The aim of medical education is to enable students to turn theory into practice.1 While didactic lectures can impart information to a large audience, they may not enable students to develop knowledge application and problem-solving skills required in clinical practice.2 Therefore, there is increasing interest in ‘blended learning’ which combines classroom-based and online education.3,4 ‘Flipped learning’ or the ‘flipped classroom’ is strategy that reverses traditional learning by delivering core content outside of the classroom (often online), and moves activities more traditionally thought of as ‘homework’, into the classroom (Fig 1).5 The method often involves viewing pre-recorded material prior to attending a classroom-based session, in which students engage in a student-centred learning activity such as problem solving, applying the knowledge they have acquired beforehand. Examples of the approach are shown in Table 1. There is evidence that the approach may facilitate deeper learning as it encourages active, rather than passive learning, often seen with didactic lectures.6–8
Fig 1.
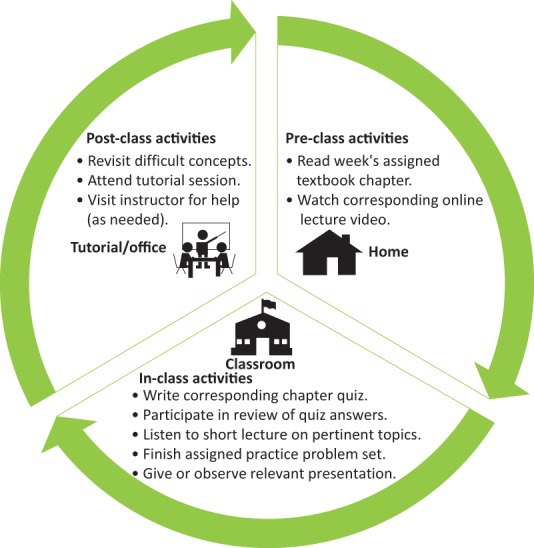
Flowchart of ‘flipped learning’ structure and settings. Adapted with permission from Moraros J, Islam A, Yu S, Banow R, Schindelka B. Flipping for success: evaluating the effectiveness of a novel teaching approach in a graduate level setting. BMC Med Educ 2015;15:27.
Table 1.
Some examples of a flipped learning in medical teaching, and our introductory week timetable using flipped learning approach
| Homework (before the class session) | Classwork | ||||
|---|---|---|---|---|---|
| Review a YouTube video of a difficult consultation. | Discuss positive and negative aspects of the consultation and what can be learnt from it. | ||||
| Read a study of an intervention published in the medical literature. | Discuss the positive and negative aspects of the study and decide what it means for clinical practice. | ||||
| Watch a videoed lecture or series of videos on a topic. | Discuss / work through clinical cases highlighting areas of importance learnt from the videos watched beforehand. | ||||
| Monday | Tuesday | Wednesday | Thursday | Friday | |
| AM | Watch videos on diabetes | Watch videos on renal medicine | Watch videos on endocrinology | Endocrinology case-based discussion | Watch videos on breast surgery / urology |
| PM | Diabetes case-based discussion | Renal medicine case-based discussion | - | Endocrinology case-based discussion | Breast surgery case-based discussion |
| Urology case-based discussion | |||||
AM = morning; PM = afternoon.
In published studies, flipped learning demonstrates greater student engagement and satisfaction, but does not always demonstrate higher assessment scores. A systematic review of 82 papers suggests that flipped learning is a promising approach to increasing student motivation and engagement, but that there remains a lack of evidence for its effectiveness with regards to knowledge retention and transfer.6 Meta-analysis of 46 papers with over 9,000 participants reported that the flipped learning was associated with higher academic achievement compared to a lecture-based approach.8
At Barts and the London School of Medicine and Dentistry, third-year medical students undertake a clinical module in endocrinology / nephrology. Prior to a 9-week hospital-based attachment, students have a 1-week programme of teaching, comprising 32 hours of lectures. Student feedback deemed the week to be intensive and didactic, and suggested that they were poorly engaged. Attendance was around 30%. Following literature review and discussion with a small group of students, a flipped learning approach was trialled. This report presents evaluation of flipped learning in an undergraduate module in a UK medical school.
Methods
The study was approved by Queen Mary University of London Ethics of Research Committee (reference number QMREC2098a). Students were informed that participation was anonymous and voluntary. Consideration was given to whether the students could be ‘randomised’ to flipped learning or standard teaching in a single year. Discussion with student representatives suggested that this would be deemed unfair if some students felt they were getting less teaching than others in the same year. It was therefore decided to compare one year group in whom lecture-based teaching was undertaken, to the following year group in whom flipped learning was undertaken.
Core topics were chosen from learning objectives and lectures were videoed. Nine hours of videos were recorded. Selected lecturers were approached to undertake a ‘case-based’ session to discuss clinical cases based on the video topic. All lecturers were consultants highly experienced in lecture delivery. Students were given instructions to watch a number of videos in the morning, and attend the case-based session in the afternoon. They were strongly encouraged to interact with the lecturer. The programme timetable is outlined in Table 1.
Feedback was undertaken prior to and following the change in delivery using standard forms comprising a Likert scale (minimum score = 1, maximum score = 5). Students were asked whether they preferred the flipped or lecture-based method of delivery of the programme, and were encouraged to write free-text comments, which was subjected to thematic analysis (QDA Miner Lite (Provalis Research, Montreal, Canada)).9
At the end of each module, students underwent a summative 50 question ‘single best answer’ in-course assessment (ICA). Results of ICA were compared using Student's t-tests (statistically significant if p<0.05).
Results
There were no significant differences in prior academic achievement, age distribution or percentage of graduate entry students between the groups. Videos had been accessed by 87.6% of the year group during the flipped learning week.
Student feedback scores were received from 126 of 312 students for the lectures (40.4%), and 182 of 327 students for flipped learning (53.2%). Feedback scores for flipped learning were higher compared with lectures (4.4 (standard deviation (SD) ±0.33); 3.6 (SD ±0.28), p=0.03; Fig 2). 81.3% of students stated they preferred flipped learning. Attendance over the week was maintained at over 70%.
Fig 2.
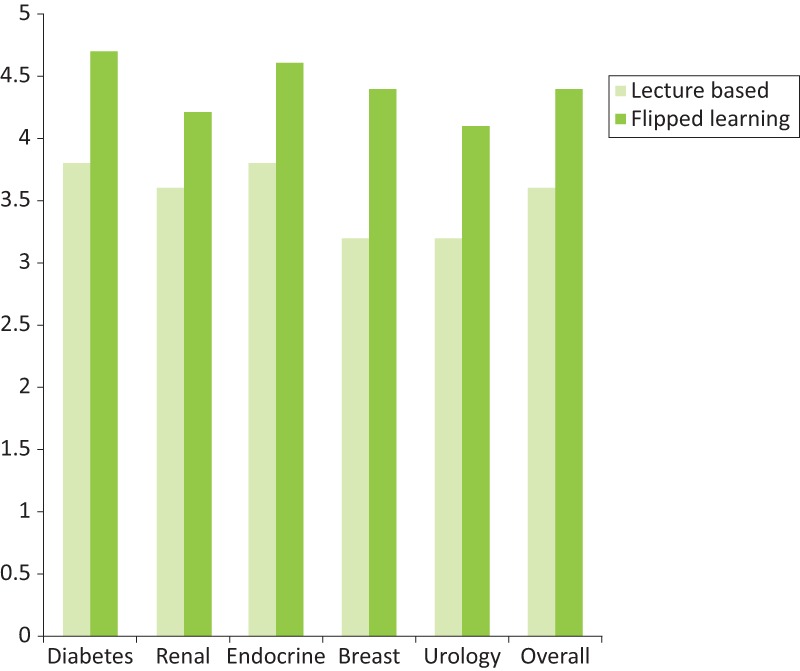
Feedback scores for lecture-based / flipped learning teaching methods. The question asked was ‘Please give an overall score for this session’. Feedback was given on a Likert scale, where 1 = very poor; 2 = poor; 3 = average; 4 = good; 5 = excellent. Mean scores improved in all subjects (Student's t-test p values were all <0.05).
Three-hundred and ten students undertook the ICA prior to flipped learning, and 324 undertook the ICA after the change. Mean score before flipped learning was 67.3% (SD 12.1), and post was 69.5% (SD 11.3; p=0.121).
Free-text themes are shown in Figs 3 and 4. Students felt more able to participate actively in learning, gained a greater understanding of basic concepts and valued being treated ‘like adults’. Students valued having the videos for revision. The main negative theme emerged around the length of the videos, and insufficient time to view them all prior to the case-based sessions.
Fig 3.
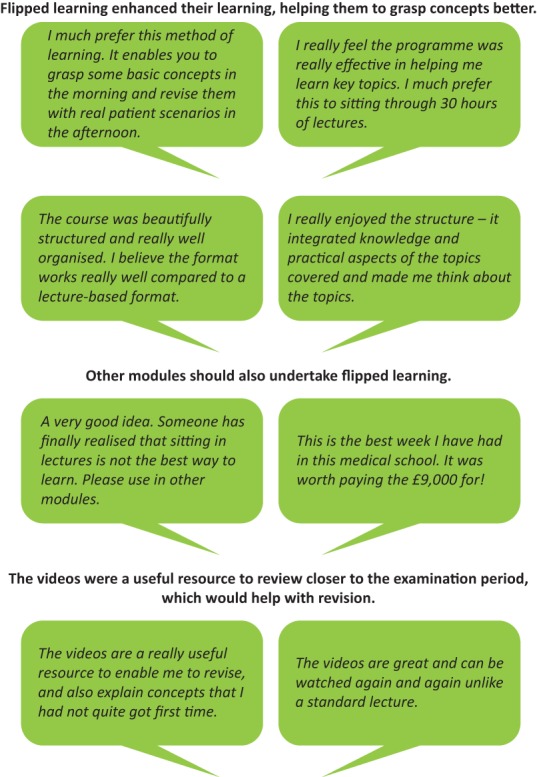
Positive themes emerging from qualitative analysis of feedback from students that attended the flipped learning module.
Fig 4.

Negative themes emerging from qualitative analysis of feedback from students that attended the flipped learning module.
Discussion
We describe the implementation and evaluation of a model of flipped learning in an undergraduate medical programme. Feedback both quantitatively and qualitatively was highly positive for flipped learning. We were unable to demonstrate improvements in assessment scores.
Flipped learning does not just entail moving lectures outside of the classroom for students to watch in their own time. It is important to ensure that face-to-face and online sections of the course are coherent. This is not always achievable, as shown by some of our student feedback, which suggested that some of the online material was overly long, and did not feel relevant. Orthodox versions of flipped learning involve a lecture which itself leads on to specific cases or worked examples. Our method of flipped learning was more loosely defined according to the topic teacher. The ‘flipped learning method’ as described in the literature may mean many different things in practice and may be applied with variations that are not apparent from the descriptions in the literature. It is possible that we need to be more rigorous with our definition of flipped learning, and this may have had an impact on subsequent assessment scores.
A flipped learning model of delivery has the potential to be more satisfying for teachers. While we did not directly question teachers on their views, teachers did comment that they found the students were more engaged as they had some knowledge to contribute to the discussion. Feedback from our students showed they valued case-based interactive discussions which were of clinical relevance to cases they would see in clinical practice.
Flipped learning requires less regular teacher time, although more time was required to undertake the initial video lectures. Our original lecture programme required 26 faculty members to deliver 32 hours of lectures in 1 week, three times a year; flipped learning required core lectures to be delivered only once by video, and the number of teachers required for 1 week reduced to eight, meaning that teaching was more efficiently delivered. The course also required less timetabled lecture space. Importantly, however, material may become out of date and require refreshing with advances in therapy.
A weakness of the study was that it compared consecutive year groups, rather than students within 1 year. It proved impossible to ‘randomise’ the students in 1 year to ‘flipped’ or ‘non-flipped’ due to student concerns. A further potential weakness of the study is non-response bias, which may have had an impact on feedback results, and the fact that the authors were all participants in delivery of the flipped learning module. Evaluation undertaken by researchers not involved in delivery may have reduced such bias.
Systematic review of flipped learning has called for evaluation of higher cognitive learning and behaviour change between flipped and lecture-based learning, and longitudinal studies to examine whether flipped learning can foster learning retention over longer periods of time.10,11
In summary, we describe a method of teaching that involves flipped learning. Implementation has shown positive feedback from students, who feel more engaged and active in the learning process. We could not demonstrate an improvement in assessment scores. In our institution, flipped learning is to be extended to other clinical modules. There is no doubt that lecture-based learning is required in certain aspects of medical education,12 but we suggest that flipped learning could be considered in other areas of medical education, including postgraduate teaching, as it may offer significant advantages over lecture-based teaching.
References
- 1.Merriam SB. Updating our knowledge of adult learning. J Cont Educ Health Prof 1996;16:136–43. [Google Scholar]
- 2.Luscombe C, Montgomery J. Exploring medical student learning in the large group teaching environment: examining current practice to inform curricular development. BMC Med Educ 2016;16:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prober CG, Khan S. Medical education reimagined: a call to action. Acad Med 2013;88:1407–10. [DOI] [PubMed] [Google Scholar]
- 4.Eapen ZJ, Vavalle JP, Harrington RA. Lecture halls without lectures – a proposal for medical education. N Engl J Med 2012;367:678–9. [DOI] [PubMed] [Google Scholar]
- 5.The Flipped Learning Network What is flipped learning? FLN, 2014. https://flippedlearning.org/wp-content/uploads/2016/07/FLIP_handout_FNL_Web.pdf [Accessed 30 November 2018]. [Google Scholar]
- 6.Chen F, Lui AM, Martinelli SM. A systematic review of the effectiveness of flipped classrooms in medical education. Med Educ 2017;51:585–97. [DOI] [PubMed] [Google Scholar]
- 7.Lin Y, Zhu Y, Chen C, et al. Facing the challenges in ophthalmology clerkship teaching: Is flipped classroom the answer? PLoS One 2017;12:e0174829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen KS, Monrouxe L, Lu YH, et al. Academic outcomes of flipped classroom learning: a meta-analysis. Med Educ 2018:52:910–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology 2006;3:77–101. [Google Scholar]
- 10.Hew KF, Lo CK. Flipped classroom improves student learning in health professions education: a meta-analysis. BMC Med Educ 2018;18:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lundin M, Rensfeldt AB, Hillman T, Lantz-Andersson A, Peterson L. Higher education dominance and siloed knowledge: a systematic review of flipped classroom research. International Journal of Educational Technology in Higher Education 2018;15:20. [Google Scholar]
- 12.Jordan J, Jalali A, Clarke S, et al. Asynchronous vs Didactic education: it's too early to throw in the towel on tradition. BMC Med Educ 2013;13:105. [DOI] [PMC free article] [PubMed] [Google Scholar]


