Abstract
Context:
The management of renal stones of high density (>1000 Hounsfield units) on non-contrast computed tomography (NCCT), and moderate sized (15-25 mm) is still debatable.
Aims:
The aim of this study was to compare the outcomes of percutaneous nephrolithotomy (PCNL) and shock wave lithotripsy (SWL) for the high-density and moderate-sized renal stones regarding the stone-free rate (SFR), morbidity, and patients' quality of life.
Settings and Design:
This is a prospective randomized study.
Patients and Methods:
Eighty consecutive patients with renal stones, excluding those with lower calyceal stones, were randomized to receive either PCNL or SWL (40 in each arm). Patients were followed up by abdominal ultrasound and plain X-ray (NCCT if indicated) till clearance of stone. Outcomes, complications, costs, and SF-8 Health Survey scoring were recorded for each group.
Statistical Analysis:
We used Stata software, version 9.2 (Intercooled STATA®; StataCorp LP College Station, Texas, USA). Comparison of the two groups was made with regard to patient and stone criteria and the procedure details. Continuous variables were compared using the Mann–Whitney U-test with values shown as the median and interquartile range. Categorical variables were compared using the Pearson's Chi-square/Fisher's exact test. Multivariate logistic regression analysis was used to identify variables independently associated with the stone clearance after two sessions of SWL. P < 0.05 was considered statistically significant.
Results:
The basic characteristics of both groups were comparable. After a single treatment session, the SFR was 80% and 27.5% for PCNL and SWL, respectively (P < 0.001). The overall 3-month SFR was 87.5% versus 90%, respectively (P = 0.723). The median number of the required maneuvers was 1 (range: 1–3) for PCNL versus 2 (range: 1–4) for SWL (P < 0.001). The complication rate was 10% and 7.5%, respectively (P = 0.692). The cost of SWL was significantly lower (P < 0.001). On multivariate analysis, a single stone was an independent predictor for stone clearance after two sessions of SWL (odds ratio: 7.26, 95% confidence interval: 1.13–46.62, P = 0.037).
Conclusions:
PCNL for the dense, and moderate-sized renal stone provides higher initial success and lower re-treatment rates compared with SWL with comparable outcome after 3 months of therapy. However, SWL is an alternative, especially for a single stone.
Keywords: Percutaneous nephrolithotomy, renal stone, shock wave lithotripsy, stone density
INTRODUCTION
The guidelines stated that 15 mm is the cutoff size for actively treating renal stones, and shock wave lithotripsy (SWL), flexible ureteroscopy, and percutaneous nephrolithotomy (PCNL) are the treatment options for symptomatic nonlower pole renal stone <20 mm with comparable morbidity and stone-free rates (SFRs).[1,2,3]
PCNL has a higher SFR and more complications compared to SWL. In contrast, SWL has a higher retreatment rate but a shorter hospital stay.[4,5]
The cutoff Hounsfield unit (HU) value above which SWL is not recommended is still debatable, however, 900–1000 HU was reported.[6,7] Others claimed that stones with HU >1350 could be directly offered an alternative method of treatment.[8] Herein, we compare the outcomes of PCNL and SWL for high-density and moderate-sized renal stones regarding SFR and perioperative morbidity.
PATIENTS AND METHODS
A prospective randomized clinical study was conducted in our hospital with patient enrollment done between March 2012 and May 2014. The sample size was calculated using Epi Info™, version 3.5, Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia (US). To detect a 20% difference between the two groups with 90% power and a threshold of significance of 0.05, the sample size had to be 78 patients (39 per group). Eighty patients were enrolled, of which 40 patients underwent PCNL and other 40 patients underwent SWL. Adult Patients with renal stones of moderate-size (15–25 mm), and high density (>1000 HU) were included.
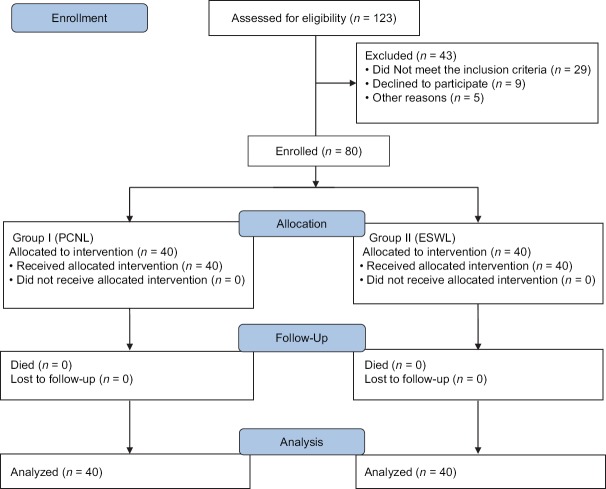
Patients were randomly assigned to either group using computer-generated random numbers (JMP, version 12.0.1; SAS Institute, Cary, NC, USA). The group into which patients allocated revealed to the operator through a sealed envelope on the day of the intervention. The study was approved by our Institutional Ethical Committee. Figure 1 shows the CONSORT flow diagram of the study.
Figure 1.
The CONSORT flow diagram of the study
The exclusion criteria were categorized into three types: first related to patients (refusing the procedure, unfit for anesthesia, bleeding diatheses, uncontrolled urinary tract infection, pregnancy, skeletal malformations making positioning and targeting impossible, renal tumor, and a typical bowel position); second related to kidney and/or urinary tract (poor ipsilateral renal function [<15%], anatomic obstruction distal to the stone, and potentially obstructed contralateral kidney); and third related to stones (renal stone length <15 mm or >25 mm, renal stone density ≤1000 or ≥1500 HU, and isolated lower calyceal renal stones).
A detailed history, clinical examination, and body mass index (BMI) were obtained. All patients did urinalysis, renal function tests, bleeding profile, complete blood count, Random blood sugar (RBS), and blood grouping performed. As regards radiological evaluation, plain kidney, ureter, and bladder (KUB), ultrasonography (US) and noncontrast computed tomography (NCCT) were done for all patients. We used the SF-8 Health Survey scoring for quality of life (QOL) assessment, which is a self-reported questionnaire divided into two parts: mental component (MC) and physical component (PC); informed written consent was obtained; and preoperative medical assessment was fulfilled.
The procedure of PCNL was started by insertion of an open-tip 6F ureteral catheter in lithotomy position under general or epidural anesthesia; then, the patient was positioned prone; and the access was created under fluoroscopy using the “Bull's eye” technique. Balloon dilation or coaxial dilators were used for the access creation, and the stone was disintegrated by the ultrasonic or pneumatic devices. Flexible ureterorenoscope was used to survey the calyces for any residuals if needed. At the end of the procedure, a nephrostomy tube (NT) and a ureteral stent were left. The NT was closed for 6 h if there was a significant bleeding.
In the first postoperative day, KUB and US were performed. If there were no residuals, the NT was removed followed by removal of the ureteral stent and urethral catheter, and a patient was discharged by the second postoperative day. If there were residual stones, then a second-look PCNL was performed in the second postoperative day under local anesthesia and general sedation. KUB, US, and/or NCCT were performed after 3 months for the evaluation of the stone clearance.
The electromagnetic lithotripter Dornier S (Dornier MedTech, Weßling, Germany) was used for SWL as an outpatient procedure. A maximum of 3000 shocks was delivered each session in a power of 60–80 (12–16 kV), and the optimal shock wave frequency was 1.0–1.5 Hz in a rate of 70 shocks/min using the ramping up technique. Localization was performed by biplanar fluoroscopy and/or US. KUB and US were performed on the first visit after 2 weeks; if there were significant residuals, then the patient underwent a second session.
All complications were graded according to the modified Clavien system. SF-8 Health Survey scoring components were reported postoperatively for both the groups.
RESULTS
Of 123 patients assessed for eligibility, 80 consecutive patients were enrolled in our study. All of them (40 in each group) completed the procedure and at least 6-months follow-up period. The median follow-up was 8 months (range: 6–30), with the last recorded follow-up visit being in November 2016. Patient characteristics including median age, gender, median BMI, and preoperative SF-8 score are similar in both the groups [Table 1].
Table 1.
Patient characteristics
| Items | PCNL (n=40) | ESWL (n=40) | P |
|---|---|---|---|
| Median years age (IQR) | 32 (25-42) | 31 (27-47) | 0.355 |
| Gender (male:female) | 27:13 | 33:7 | 0.121 |
| Median BMI kg/m2 (IQR) | 26.3 (22.7-28.2) | 24.8 (22-27) | 0.190 |
| Median PC score (IQR) | 34.2 (31.3-37.6) | 37.6 (30.6-41.2) | 0.110 |
| Median MC score (IQR) | 39.9 (37.3-43.5) | 41.2 (34.8-51) | 0.236 |
IQR: Interquartile range, BMI: Body mass index, PC: Physical component, MC: Mental component, PCNL: Percutaneous nephrolithotomy, ESWL: Extracorporeal shock wave lithotripsy
Table 2 shows the stone criteria and degree of hydronephrosis if present; there was no statistical significance between the two groups. Regarding PCNL, the lower calyx was the favorable access in 32 cases. A single puncture was required in 33 cases. The median hospital stay was 2 days (range: 2–4).
Table 2.
Stone characteristics
| Items | PCNL (n=40) | ESWL (n=40) | P |
|---|---|---|---|
| Percentage right side | 55 | 57.5 | 0.822 |
| Percentage single stone | 40 | 50 | 0.242 |
| Location | |||
| Percentage pelvicalyceal | 65 | 40 | 0.077 |
| Percentage pelvis | 30 | 40 | |
| Percentage calyceal | 5 | 20 | |
| Median stone length (mm), IQR | 25 (20-25) | 21.5 (17-25) | 0.104 |
| Median stone width (mm), IQR | 17.45 (13-22.4) | 15.5 (11.5-19.6) | 0.234 |
| Median stone burden (mm2), IQR | 345.5 (260-560) | 346.8 (220-412.25) | 0.165 |
| Percentage stone homogeneity | 45 | 57.5 | 0.263 |
| Median SSD cm (IQR) | 9.5 (7.5-11.25) | 10.52 (7.5-12.31) | 0.885 |
| Median HU (IQR) | 1250 (1010-1490) | 1262.5 (1017-1490) | 0.969 |
| Hydronephrosis | |||
| Percentage no hydronephrosis | 22.5 | 30 | 0.727 |
| Percentage mild | 57.5 | 50 | |
| Percentage moderate | 20 | 20 |
IQR: Interquartile range, PCNL: Percutaneous nephrolithotomy, ESWL: Extracorporeal shock wave lithotripsy, HU: Hounsfield unit, SSD: Skin to stone distance
Twenty-eight patients (77.5%) were rendered stone free after 2 weeks of PCNL (with residual fragments ≤4 mm), on contrary to 11 patients (27.5%) in the SWL group after the first session (P ≤ 0.001). The auxiliary procedures were performed in 9 (22.5%) and 29 (72.5%) patients in both PCNL and SWL groups, respectively (P < 0.001).
For the PCNL group, 7 cases underwent second-look PCNL and 2 SWL. For the SWL group, 13 cases cleared after the second session, 6 after the third, 6 after the fourth, and 4 cases underwent mini-PCNL for residual lower calyceal stones. The overall SFR after 3 months was similar in both PCNL and SWL patients (35 [87.5%] and 36 [90%] respectively; P = 0.723).
Postoperative complications in the PCNL group were as follows: two patients suffered urinary leakage managed conservatively; two patients suffered urinary leakage managed conservatively, and one patient with fever, one developed secondary hemorrhage, and angioembolization for uncontrolled bleeding occurred in one patient. For the SWL group, steinstrasse occurred in 3 patients, in which 2 of them were treated conservatively and the third one underwent extra SWL session for the leading stone on the lower third of the ureter.
PCNL was significantly costly than SWL (P < 0.001). There was no significant difference between SF-8 health score components (PC and MC) for both the groups. However, for each group, there was a statistically significant difference between the preoperative and postoperative (2 weeks and at 3 months) reports (P < 0.001). The postoperative outcomes for both the groups are summarized in Table 3.
Table 3.
Postoperative outcome
| Items | PCNL (n=40) | ESWL (n=40) | P |
|---|---|---|---|
| Efficacy | |||
| Percentage initial SFR after single monotherapy | 77.5 | 27.5 | <0.001 |
| Percentage retreatment (same intervention) | 7.5 | 62.5 | 0.641 |
| Percentage retreatment (different intervention) | 15 | 10 | 0.502 |
| Median maneuvers till clearance (IQR) | 1 (1) | 2 (2) | <0.001 |
| Percentage overall SFR monotherapy | 87.5 | 90 | 0.723 |
| Safety | |||
| Percentage overall complications | 10 | 7.5 | 0.692 |
| Percentage modified Clavien system | |||
| G I | 5 | ||
| G II | 2.5 | ||
| G IIIa | 7.5 | ||
| G IIIb | 2.5 | ||
| QOL | |||
| Median PC 2 weeks (range) | 48 (19-59) | 47.6 (19-59) | 0.885 |
| Median MC 2 weeks (range) | 51 (28-63) | 51.8 (28-63) | 0.658 |
| Median PC 3 months (range) | 47 (40-56) | 47 (33-59) | 0.660 |
| Median MC 3 months (range) | 50 (29-57) | 47 (36-57) | 0.540 |
QOL: Quality of life, PCNL: Percutaneous nephrolithotomy, ESWL: Extracorporeal shock wave lithotripsy, IQR: Interquartile range, PC: Physical component, MC: Mental component, SFR: Stone-free rate
On multivariate analysis using logistic regression, a single renal stone was an independent predictor for complete stone clearance after two sessions of SWL (odds ratio [OR]: 7.26, 95% confidence interval [CI]: 1.13–46.62, P = 0.037). Other factors, such as age, gender, stone burden, BMI and HU, had no statistically significant relation to the two sessions' clearance rate [Table 4].
Table 4.
Predictors of two shock wave lithotripsy sessions’ stone-free rate (multivariate analysis using logistic regression)
| Items | OR (95% CI) | P |
|---|---|---|
| Age | 1.024 (0.950-1.104) | 0.544 |
| Male | 1.001 (0.096-10.43) | 0.999 |
| BMI | 0.898 (0.703-1.070) | 0.185 |
| Stone burden | 1.001 (0.994-1.008) | 0.720 |
| Stone density (HU) | 0.995 (0.989-1.001) | 0.128 |
| Single stone | 7.258 (1.13-46.62) | 0.037 |
OR: Odds ratio, CI: Confidence interval, BMI: Body mass index, HU: Hounsfield unit
DISCUSSION
The stone size, composition, and location are important factors affecting the outcome of treating kidney stones.[9] Due to the limitations of the success rate and the complications of SWL, other minimally invasive modalities for kidney stones such as PCNL and retrograde intrarenal surgery (RIRS) are widely used.[10]
PCNL is considered the standard treatment for patients with large kidney and upper ureteral stones. The main advantages of PCNL are the higher success rate for larger stones, and it is not its independence from the stone burden or composition. However, PCNL is more invasive and has a higher associated morbidity than SWL.[11]
The treatment of medium-sized renal stones (15–25 mm) demands an expertise with minimally invasive techniques and should provide the highest SFR with the fewest procedures and the lowest complication rate.[12] The current modalities of treatment include SWL, PCNL, RIRS, and open or laparoscopic pyelolithotomy.[13]
There are a great debate and discrepancy about HU both in recent guidelines and in literature. A study concluded that obesity and increased stone density (>1000 HU) as detected by NCCT are significant predictors of failure to fragment renal stones by SWL.[14] Others stated that the cut of the level of HU for better fragmentation with SWL were 750 and 900 HU.[7,15] In our study, stones with HU >1000 were chosen in a challenge to SWL, and we obtained a comparable SFR to PCNL.
HU attenuation value may predict the success of PCNL. The Clinical Research Office of the Endourological Society (CROES) study stated that both very high and low HU values were associated with lower SFRs and long operative times.[16] Besides, stones with low HU are likely to be uric acid or struvite in composition, which is poorly visible on fluoroscopy and thus more difficult to identify during PCNL.[17] We think this can be managed using the flexible nephroscope to survey the calyces at the end of the procedure. The use of flexible cysto-nephroscope, high-resolution fluoroscopy, and perioperative CT improves the SFR after PCNL. Second-look procedure in patients with Residual fragments (RFs) >4 mm was found to be cost-effective when compared with an observational strategy.[18]
Regarding SWL technique, the stepwise voltage (ramping technique) has a lower risk of renal damage than a fixed maximal voltage with a comparable efficacy.[19] It has been shown that a pause of a few minutes can induce vasoconstriction that may provide a protective effect in reducing the rate of renal hematoma.[20] Recently, vasoconstriction has been reported to occur without a pause.[21] In our study, the stepwise voltage ramping technique, low frequency, and US guidance gave us acceptable results.
The SFR after SWL is affected by many factors including stone size, HU attenuation value, and BMI. However, the SFR after PCNL is not affected by these factors, as the intracorporeal lithotripsy devices can disintegrate any type of renal stone of any size regardless of the patient's BMI.[22]
In our study, SWL has a final SFR of 90%, which is better than other studies despite the high HU attenuation values used in our study. Several factors helped us to obtain such results as the isolated lower calyceal stone was excluded, and the electromagnetic lithotripter Dornier S is known to have high-energy flux density with a narrow focus, low-frequency disintegration, ultrasound guidance of SWL, and well-trained operators.
Our overall SFR for PCNL group was 87.5%, retreatment rate was 22.5%, and the complications rate was 10%. They were comparable to other similar studies.[4,12]
The CROES has the largest prospectively collected database of 5724 patients treated with PCNL; in 96 centers worldwide over a 1-year period, the overall complication rate was 20.5%.[23] Our overall complication rate is 10%; this is related to our patient selection criteria and experienced surgeons performed the procedure.
There was a controversy between several studies at the point of cost. In the present study and despite the greater need for retreatment and auxiliary procedures, SWL was still more cost-effective than PCNL. This might be attributed to the difference in treatment costs among different countries, the cost of inpatient hospitalization, and the higher costs of disposables for PCNL. However, the need for multiple sessions with SWL might make PCNL somewhat cost-effective.[24,25]
In the present study, on multivariate analysis using logistic regression, the single renal stone was an independent predictor for complete stone clearance after two sessions of SWL (OR: 7.26, 95% CI: 1.13–46.62, P = 0.037). In our study, and despite significant (P < 0.000) increase in the median score of both PC and MC QOL assessments in each group separately, there was no significant change (P = 0.885) pre- and postoperatively between both the groups.
Our study has some limitations such as limited numbers of patients and the restricted attenuation value of >1000 HU.
CONCLUSIONS
Patients with medium-sized (15–25 mm) high-density (HU >1000) kidney stones need an individualized approach for each case with respect to the stone site, burden, and HU density. Both PCNL and SWL have the comparable results as regards final SFR and both are complementary to each other.
PCNL has advantages of higher initial SFR with a short time of treatment and lower retreatment rate. SWL has advantages of noninvasiveness with less complication rate and higher cost-effectiveness. Although PCNL is effective, it has some limitations including invasiveness and cost. SWL is another alternative, especially for single moderate-sized high-density renal stone.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016;69:475–82. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 2.Assimos D, Krambeck A, Miller NL, Monga M, Murad MH, Nelson CP, et al. Surgical management of stones: American urological association/Endourological society guideline, PART I. J Urol. 2016;196:1153–60. doi: 10.1016/j.juro.2016.05.090. [DOI] [PubMed] [Google Scholar]
- 3.Assimos D, Krambeck A, Miller NL, Monga M, Murad MH, Nelson CP, et al. Surgical management of stones: American urological association/Endourological society guideline, PART II. J Urol. 2016;196:1161–9. doi: 10.1016/j.juro.2016.05.091. [DOI] [PubMed] [Google Scholar]
- 4.Deem S, Defade B, Modak A, Emmett M, Martinez F, Davalos J. Percutaneous nephrolithotomy versus extracorporeal shock wave lithotripsy for moderate sized kidney stones. Urology. 2011;78:739–43. doi: 10.1016/j.urology.2011.04.010. [DOI] [PubMed] [Google Scholar]
- 5.Menon M. Cost effectiveness of extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy for medium-sized kidney stones: A randomised clinical trial. J Urol. 1993;150:565. [PubMed] [Google Scholar]
- 6.El-Assmy A, El-Nahas AR, Abo-Elghar ME, Eraky I, El-Kenawy MR, Sheir KZ. Predictors of success after Extracorporeal Shock Wave Lithotripsy (ESWL) for renal calculi between 20-30 mm: A multivariate analysis model. ScientificWorldJournal. 2006;6:2388–95. doi: 10.1100/tsw.2006.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang LJ, Wong YC, Chuang CK, Chu SH, Chen CS, See LC, et al. Predictions of outcomes of renal stones after extracorporeal shock wave lithotripsy from stone characteristics determined by unenhanced helical computed tomography: A multivariate analysis. Eur Radiol. 2005;15:2238–43. doi: 10.1007/s00330-005-2742-9. [DOI] [PubMed] [Google Scholar]
- 8.Hameed DA, Elgammal MA, ElGanainy EO, Hageb A, Mohammed K, El-Taher AM, et al. Comparing non contrast computerized tomography criteria versus dual X-ray absorptiometry as predictors of radio-opaque upper urinary tract stone fragmentation after electromagnetic shockwave lithotripsy. Urolithiasis. 2013;41:511–5. doi: 10.1007/s00240-013-0596-1. [DOI] [PubMed] [Google Scholar]
- 9.Srisubat A, Potisat S, Lojanapiwat B, Setthawong V, Laopaiboon M. Extracorporeal Shock Wave Lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst Rev. 2014;11:CD007044. doi: 10.1002/14651858.CD007044.pub3. [DOI] [PubMed] [Google Scholar]
- 10.Coz F, Orvieto M, Bustos M, Lyng R, Stein C, Hinrichs A, et al. Extracorporeal shockwave lithotripsy of 2000 urinary calculi with the modulith SL-20: Success and failure according to size and location of stones. J Endourol. 2000;14:239–46. doi: 10.1089/end.2000.14.239. [DOI] [PubMed] [Google Scholar]
- 11.Ziemba JB, Matlaga BR. Guideline of guidelines: Kidney stones. BJU Int. 2015;116:184–9. doi: 10.1111/bju.13080. [DOI] [PubMed] [Google Scholar]
- 12.Hassan M, El-Nahas AR, Sheir KZ, El-Tabey NA, El-Assmy AM, Elshal AM, et al. Percutaneous nephrolithotomy vs. extracorporeal shockwave lithotripsy for treating a 20-30 mm single renal pelvic stone. Arab J Urol. 2015;13:212–6. doi: 10.1016/j.aju.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De S, Autorino R, Kim FJ, Zargar H, Laydner H, Balsamo R, et al. Percutaneous nephrolithotomy versus retrograde intrarenal surgery: A systematic review and meta-analysis. Eur Urol. 2015;67:125–37. doi: 10.1016/j.eururo.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 14.El-Nahas AR, El-Assmy AM, Mansour O, Sheir KZ. A prospective multivariate analysis of factors predicting stone disintegration by extracorporeal shock wave lithotripsy: The value of high-resolution noncontrast computed tomography. Eur Urol. 2007;51:1688–93. doi: 10.1016/j.eururo.2006.11.048. [DOI] [PubMed] [Google Scholar]
- 15.Gupta NP, Ansari MS, Kesarvani P, Kapoor A, Mukhopadhyay S. Role of computed tomography with no contrast medium enhancement in predicting the outcome of extracorporeal shock wave lithotripsy for urinary calculi. BJU Int. 2005;95:1285–8. doi: 10.1111/j.1464-410X.2005.05520.x. [DOI] [PubMed] [Google Scholar]
- 16.Anastasiadis A, Onal B, Modi P, Turna B, Duvdevani M, Timoney A, et al. Impact of stone density on outcomes in Percutaneous Nephrolithotomy (PCNL): An analysis of the Clinical Research Office of the Endourological Society (CROES) pcnl global study database. Scand J Urol. 2013;47:509–14. doi: 10.3109/21681805.2013.803261. [DOI] [PubMed] [Google Scholar]
- 17.Ghani KR, Andonian S, Bultitude M, Desai M, Giusti G, Okhunov Z, et al. Percutaneous nephrolithotomy: Update, trends, and future directions. Eur Urol. 2016;70:382–96. doi: 10.1016/j.eururo.2016.01.047. [DOI] [PubMed] [Google Scholar]
- 18.Raman JD, Bagrodia A, Bensalah K, Pearle MS, Lotan Y. Residual fragments after percutaneous nephrolithotomy: Cost comparison of immediate second look flexible nephroscopy versus expectant management. J Urol. 2010;183:188–93. doi: 10.1016/j.juro.2009.08.135. [DOI] [PubMed] [Google Scholar]
- 19.Skuginna V, Nguyen DP, Seiler R, Kiss B, Thalmann GN, Roth B. Does stepwise voltage ramping protect the kidney from injury during extracorporeal shockwave lithotripsy? Results of a prospective randomized trial. Eur Urol. 2016;69:267–73. doi: 10.1016/j.eururo.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 20.Bohris C, Bayer T, Gumpinger R. Ultrasound monitoring of kidney stone extracorporeal shockwave lithotripsy with an external transducer: Does fatty tissue cause image distortions that affect stone comminution? J Endourol. 2010;24:81–8. doi: 10.1089/end.2009.0158. [DOI] [PubMed] [Google Scholar]
- 21.Kroczak T, Scotland KB, Chew B, Pace KT. Shockwave lithotripsy: Techniques for improving outcomes. World J Urol. 2017;35:1341–6. doi: 10.1007/s00345-017-2056-y. [DOI] [PubMed] [Google Scholar]
- 22.Argyropoulos AN, Tolley DA. Evaluation of outcome following lithotripsy. Curr Opin Urol. 2010;20:154–8. doi: 10.1097/MOU.0b013e328333b68b. [DOI] [PubMed] [Google Scholar]
- 23.Labate G, Modi P, Timoney A, Cormio L, Zhang X, Louie M, et al. The percutaneous nephrolithotomy global study: Classification of complications. J Endourol. 2011;25:1275–80. doi: 10.1089/end.2011.0067. [DOI] [PubMed] [Google Scholar]
- 24.Matlaga BR, Jansen JP, Meckley LM, Byrne TW, Lingeman JE. Economic outcomes of treatment for ureteral and renal stones: A systematic literature review. J Urol. 2012;188:449–54. doi: 10.1016/j.juro.2012.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lotan Y, Pearle MS. Economics of stone management. Urol Clin North Am. 2007;34:443–53. doi: 10.1016/j.ucl.2007.04.008. [DOI] [PubMed] [Google Scholar]