Abstract
Objective:
The aim of this study was to verify the prevalence of uterine cavity abnormalities diagnosed by routine office hysteroscopy in women preparing to IVF.
Methods:
We carried out a retrospective cross-sectional study of 1141 consecutive women who underwent outpatient hysteroscopy before IVF at a tertiary academic center. Of these, 961 participants had a normal transvaginal sonography (TVS) of the uterine cavity. The prevalence of hysteroscopic alterations in successive age strata was submitted to Mantel-Haenzsel Chi-square test for linear trend. The diagnostic accuracy of TVS using hysteroscopy as reference was assessed by calculating the sensitivity, specificity, positive and negative likelihood ratios.
Results:
Hysteroscopic alterations were present in 265/961 of patients with a negative TVS (prevalence 27.6%, 95% confidence interval [CI] 24.8%-30.5%). The prevalence of unsuspected submucous leiomyoma was higher among older women (p=0.005, chi-square test for linear trend) and reached 7.2% (95% CI 3.5%-14.1%) after 40 years. The sensitivity of TVS ranged from 8% (95% CI 2%-20%) for uterine synechiae to 41% (95% CI 28%-56%) for submucous leiomyoma, resulting in low likelihood ratios for negative TVS results.
Conclusions:
These findings suggest a high prevalence of unsuspected alterations found by routine hysteroscopy before IVF, an age-dependent increase in the frequency of submucous leiomyoma and a low diagnostic sensitivity of TVS to detect intracavitary lesions.
Keywords: hysteroscopy, IVF, endometrial polyp, submucous leiomyoma, transvaginal ultrasound, accuracy
INTRODUCTION
It is estimated that 72.4 million couples are infertile worldwide and that 40.5 million of them are currently seeking treatment for infertility (Boivin et al., 2007). Although uterine factors represent only 2% to 3% of the primary causes of infertility, intracavitary pathology may be present in approximately one third of infertile women submitted to routine hysteroscopy before in vitro fertilization (IVF) (Bakas et al., 2014; Boivin et al., 2007; Carneiro, 2014). Even minor uterine cavity abnormalities, such as endometrial polyps, small submucous leiomyomas, adhesions, and septa are considered to have a negative impact on the chance to conceive through IVF (Smit et al., 2016). Therefore, it has been suggested that these abnormalities should be diagnosed and treated to optimize the condition of the uterine environment and thus, the outcome of IVF treatment (Elsetohy et al., 2015).
More recently, the usefulness of performing hysteroscopy in the month preceding IVF in women with normal uterine imaging has been challenged by two randomized clinical trials that showed no benefit of routine hysteroscopy to improve livebirth rates (El-Toukhy et al., 2016; Smit et al., 2016). However, both trials found intracavitary abnormalities in less than 13% of the screened patients and, therefore, their findings might not be applicable to other populations with larger prevalence of unsuspected uterine alterations. Because the frequency of intrauterine pathology in IVF candidates varies depending on the population characteristics and the diagnostic criteria (Bakas et al., 2014; Fatemi et al., 2010), more data from different populations is needed to clarify the impact of routine hysteroscopy in revealing uterine alterations before IVF.
The aim of this study was to verify the prevalence of unsuspected uterine cavity abnormalities diagnosed by routine office hysteroscopy in women preparing to IVF. We also assessed the age-related prevalence of lesions and the accuracy of transvaginal sonography (TVS) to detect the most frequent hysteroscopic alterations. We believe that this study adds to the current literature by evaluating a large sample of women undergoing both ultrasound and hysteroscopy in a single setting using a standardized protocol, which allow us to estimate the actual prevalence of unsuspected intrauterine lesions in a typical group of Brazilian women preparing to IVF in a tertiary teaching hospital.
MATERIALS AND METHODS
We carried out a single center, retrospective cross-sectional study of 1141 consecutive women who underwent outpatient hysteroscopy in preparation to an IVF cycle at a tertiary academic center of Belo Horizonte, Brazil, between January 2012 and December 2017. Of these, 961 participants had a negative TVS, defined as absence of visible intracavitary abnormal structures, thickening, malformation or distortion. For the purpose of this study, adnexal masses and subserous/intramural fibroids not distorting the uterine cavity were not considered as positive TVS findings. All TVS examinations were performed by a staff of 4 certified specialists during the patient's proliferative phase of menstrual cycle. The time interval between TVS and hysteroscopy ranged from 0 to 60 days.
The study was approved by the Research Ethics Committee of Universidade Federal de Minas Gerais (protocol number CAAE59731016.90000.5149) and was exempted from informed consent due to the retrospective design and anonymization of the participants.
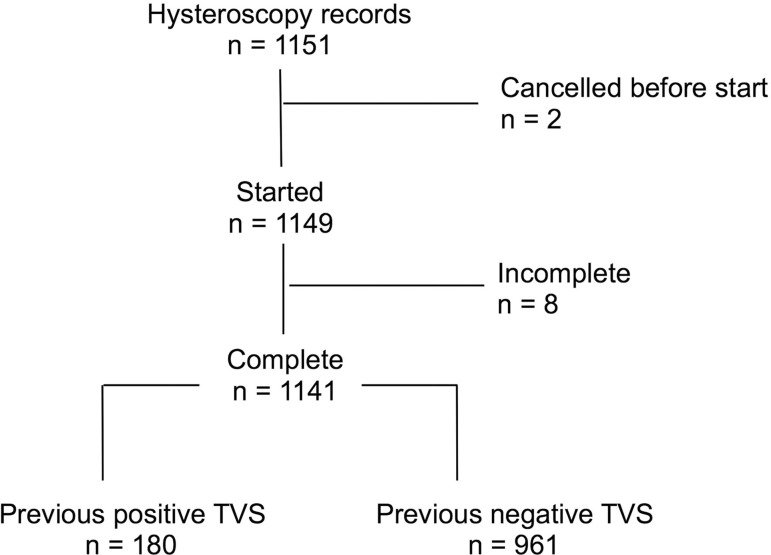
The only inclusion criterion of the study was having undergone a complete hysteroscopy in preparation to IVF (Figure 1). The total number of IVF cycles performed in our center during the study period was 914, which is inferior to the number of hysteroscopies because some women did not return after the hysteroscopy to start the IVF cycle.
Figure 1.
Study flow chart
Hysteroscopic examination
Hysteroscopy examination was performed using the vaginoscopic approach, without previous anesthesia or cervical dilatation, and was scheduled for the follicular phase of the menstrual cycle (up to the 10th day of the cycle). Patients were instructed to take oral antispasmodic medication 30 minutes before the procedure.
The examinations were performed by in training physicians under direct supervision of 3 experienced gynecologic endoscopists. The equipment used was a rigid Karl Storz Telescope with 30-degree oblique view, 2.9 mm inner diameter and a 4.1mm outer sheath. The uterine cavity was distended with 0.9% saline and a maximal pressure of 70 mmHg. The cervical canal, uterine cavity, tubal ostia and endometrial surface were inspected methodically and the findings were recorded on a standardized form.
Statistical Analysis
Categorical data (primary vs. secondary infertility, main cause of infertility, prevalence of lesions) were summarized as simple or relative frequencies and tested with Chi-square or Fisher's exact test, as appropriate. Continuous variables (age, length of infertility, menstrual cycle day) were submitted to Shapiro-Wilk normality test and departed significantly from normal distribution, therefore the inter-group differences were analyzed with the non-parametric Mann-Whitney test. The prevalence of hysteroscopic alterations in successive age strata was submitted to Mantel-Haenzsel Chi-square test for linear trend. The diagnostic accuracy of TVS using hysteroscopy as reference was assessed by calculating the sensitivity, specificity, positive and negative likelihood ratios with their respective 95% confidence intervals (CI). We used the statistical software package SPSS version 22 (IBM, Armonk, NY, USA).
RESULTS
The study flow is depicted in Figure 1. A total of 1151 hysteroscopy reports were initially available. Two cases were excluded because the examination had been cancelled before starting and 8 cases had incomplete examination due to patient intolerance and/or technical difficulties, e.g. cervical stenosis with failed access and excess bleeding or mucus. The final sample comprised 1141 completed hysteroscopies of which 180 were associated with a positive TVS and 961 with a negative TVS (Figure 1). The two groups had similar age, length of infertility and proportion of primary to secondary infertility (Table 1).
Table 1.
Characteristics of the study participants
| All (n=1141) |
TVS positive (n=180) |
TVS negative (n=961) |
p-value | |
|---|---|---|---|---|
| Age (years) | 35.4±4.7 | 36.1±4.9 | 35.3±4.7 | 0.031 |
| Length of infertility (years) | 7.7±4.2 | 7.5±4.7 | 7.7±4.1 | 0.611 |
| Menstrual cycle day | 8.7±1.9 | 8.7±2.2 | 8.7±1.9 | 0.221 |
| Infertility | ||||
| Primary | 613/901 (68%) | 85/134 (63%) | 528/767 (69%) | 0.255 |
| Secondary | 288/901 (32%) | 49/134 (37%) | 239/767 (31%) | |
| Main Cause* | ||||
| Male factor | 290 (25%) | 28 (16%) | 262 (27%) | 0.000 |
| Tubal | 97 (9%) | 11 (6%) | 86 (9%) | |
| Endometriosis | 90 (8%) | 12 (7%) | 78 (8%) | |
| PCOS | 30 (3%) | 1 (1%) | 29 (3%) | |
| Unexplained | 627 (55%) | 126 (70%) | 501 (52%) | |
| Other | 7 (1%) | 2 (1%) | 5 (1%) |
Continuous variables are shown as mean±standard variation. p-values refer to the comparison between TVS positive and TVS negative groups (Mann-Whitney test for continuous variables and Chi-square test for categorical variables).
according to annotations in the hysteroscopy report.
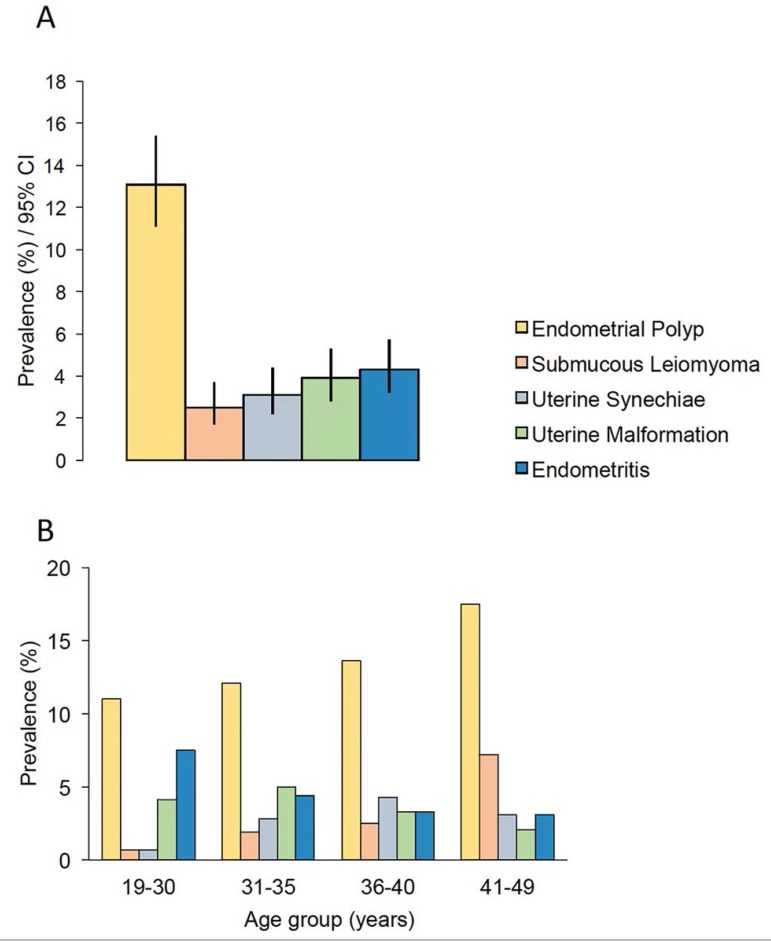
Uterine alterations were found by hysteroscopy in 351/1141 patients of the whole cohort (prevalence 30.7%, 95% CI 28.2%-33.5%) and in 265/961 patients with a negative TVS (prevalence 27.6%, 95% CI 24.8%-30.5%, Table 2). These included 126 cases of endometrial polyp (13.1% [95% CI 11.1% to 15.4%]), 24 cases of submucous leiomyoma (2.5% [1,7% to 3.7%]), 30 cases of uterine synechiae (3.1% [2.2% to 4.4%]), and 37 cases of uterine malformations such as septate, arcuate and bicornuate uterus (3.9% [2.8% to 5.3%]; Figure 2A and Table 2). In addition, there were 41 cases of suspected endometritis (4.3%) and 33 cases of nonspecific endometrial "thickening" (3.4%), defined by elevated endometrial surface upon contact with the hysteroscope (Table 2). The number of hysteroscopies needed to detect one unsuspected lesion in this population was 3.6 (95% CI 3.3 to 4.0).
Table 2.
Hysteroscopic findings
| All (n=1141) |
TVS positive (n=180) |
TVS negative (n=961) |
p-value | |
|---|---|---|---|---|
| Any alteration | 351 (30.7%) | 86 (47.8%) | 265 (27.6%) | 0.000 |
| Endometrial Polyp | 170 (17.9%) | 44 (24.4%) | 126 (13.1%) | 0.000 |
| Submucous Leiomyoma | 44 (3.9%) | 20 (11.1%) | 24 (2.5%) | 0.000 |
| Uterine Synechiae | 39 (3.4%) | 9 (5.0%) | 30 (3.1%) | 0.260 |
| Uterine Malformation | 53 (4.6%) | 16 (8.9%) | 37 (3.9%) | 0.006 |
| Suspected Endometritis | 42 (3.7%) | 1 (0.6%) | 41 (4.3%) | 0.009 |
| Endometrial "thickening" | 42 (3.7%) | 9 (5.0%) | 33 (3.4%) | 0.285 |
| Other | 15 (1.3%) | 1 (0.6%) | 14 (1.4%) | 0.490 |
The sum of all alterations is higher than the number of hysteroscopies with “any alteration” because some patients had more than one type of lesion. p-values refer to the comparison between TVS positive and TVS negative groups (Chi-square or Fisher’s exact test, as appropriate).
p-values refer to the comparison between TVS positive and TVS negative groups (Chi-square or Fisher’s exact test, as appropriate).
Figure 2.
Prevalence of hysteroscopic alterations with 95% confidence interval (A) and according to age (B) in women with normal TVS imaging of the uterine cavity (n=961)
The prevalence of uterine cavity abnormalities in the group with a negative TVS changed according to the woman's age, as shown in Figure 2B. Older women had non-significant increases in the frequency of endometrial polyp (p=0.133) and uterine synechiae (p=0.083) and decrease in uterine malformation (p=0.237). However, the prevalence of submucous leiomyoma increased significantly with age (p=0.005, Chi-square test for linear trend) and reached 7.2% (95% CI 3.5%-14.1%) after 40 years, whereas that of endometritis decreased (p=0.044, Figure 2B). A similar age trend was seen in the group with a positive TVS (not shown).
Table 3 shows that TVS had low sensitivity in diagnosing the main intrauterine alterations detected by hysteroscopy. The sensitivity of TVS ranged from 8% (95% CI 2%-20%) for uterine synechiae to 41% (95% CI 28%-56%) for submucous leiomyoma, resulting in low likelihood ratios for negative TVS results. Conversely, TVS findings had very high specificity in all types of lesion evaluated, ranging from 95% specificity (95% CI 93%-96%) for submucous leiomyoma to 100% (95% CI 99%-100%) for uterine malformation. This specificity translated into high likelihood ratios for positive TVS results (Table 3).
Table 3.
Diagnostic accuracy of transvaginal sonography to detect uterine lesions using hysteroscopy as reference
| Endometrial Polyp | Submucous Leiomyoma | Uterine Synechiae | Uterine Malformation | |
|---|---|---|---|---|
| Sensitivity | 15 (11-21) | 41 (28-56) | 8 (2-20) | 17 (9-29) |
| Specificity | 97 (96-98) | 95 (93-96) | 99 (99-99) | 100 (99-100) |
| LR+ | 4.8 (2.9-7.9) | 7.5 (4.9-11.5) | 10.6 (2.9 (38.4) | 36.9 (12.8-106.4) |
| LR- | 0.9 (0.8-0.9) | 0.6 (0.5-0.8) | 0.9 (0.8-1.0) | 0.8 (0.7-0.9) |
Data are presented as percentage with 95% confidence interval.
LR+: positive likelihood ratio; LR-: negative likelihood ratio.
DISCUSSION
The gold standard technique for evaluating the uterine cavity is hysteroscopy, since it allows direct visualization of the lesions and treatment of the main abnormalities found, in contrast to other diagnostic methods such as TVS (Di Spiezio Sardo et al., 2016a). In the present study, the overall prevalence of uterine abnormalities found by hysteroscopy after a negative TVS in IVF candidates was 27.6%. The prevalence of intrauterine abnormalities identified in hysteroscopy in cases of previous normal findings in TVS has been estimated to vary from 11% (Fatemi et al., 2010) to 32% (Bakas et al., 2014), a broad range of prevalence that may translate differences in participants' age, ethnicity, anthropometry and general health. In addition, the prevalence of unsuspected lesions may vary depending on the diagnostic performance of TVS. Therefore, the TVS sensitivity in our hands might have been lower than in other studies, resulting in a higher prevalence of hysteroscopic findings not detected by a previous TVS.
In the present study we detected endometrial polyps more often in women older than 40 compared to the younger age strata, although the prevalence did not increase as a linear function of age. Confirmatory diagnosis of endometrial polyp in women in preparation for IVF is important because of its possible association with implantation failure (Pérez-Medina et al., 2005). Moderate quality evidence from a single clinical trial suggests that hysteroscopic polypectomy increases the odds of pregnancy following intrauterine insemination (Bosteels et al., 2015; Pérez-Medina et al., 2005).
The prevalence of hysteroscopic images compactible with submucous leiomyoma increased significantly with increasing age suggesting that older women, particularly after 40 years, are more likely to have this lesion detected by hysteroscopy despite a negative TVS. Considering that IVF success rates are low in women over 40 due to oocyte/embryo factors, detecting submucous leiomyoma may be an opportunity to act on a modifiable risk factor that contributes to IVF failure (Ezzati et al., 2009). Based on consistent findings of cohort studies, an American Society of Reproductive Medicine (ASRM) expert group found grade B evidence that performing myomectomy of submucosal leiomyoma improves clinical pregnancy rates (Practice Committee of the American Society for Reproductive Medicine, 2017). In this study, TVS detected only 41% of the cases in whom hysteroscopy eventually identified a submucous leiomyoma, suggesting that TVS missed most of the possible cases; on the other hand, the 95% specificity of TVS means that in 5% of the cases where hysteroscopy was negative for submucous leiomyoma there was a previous TVS indicating the presence of this lesion. This inconsistency between the two methods suggests that many true fibroids may have escaped from TVS view (false negatives), while some TVS images recorded as possible submucous leiomyomas were actually false positives. However, we cannot rule out the possibility that some true submucous fibroids have been overlooked at hysteroscopy.
Uterine malformations (such as septate uterus) and uterine synechiae were found in more than 3% of our study population with a negative TVS. Both conditions are associated with a high risk of miscarriage (Cholkeri-Singh & Sasaki, 2015; Practice Committee of the American Society for Reproductive Medicine, 2016; Tomaževič et al., 2010). However, hysteroscopy alone is not able to evaluate the external format of the uterus and therefore it does not allow the differential diagnosis between a septate and a bicornuate uterus and thus the best approach for this differentiation is hysteroscopy associated with laparoscopy (Practice Committee of the American Society for Reproductive Medicine, 2016). According to a Cochrane review, high quality evidence is still needed to support the surgical treatment of septate uterus (Rikken et al., 2017), but a current ASRM guideline concludes, based on Grade C evidence, that it is reasonable to consider septum incision in infertile women (Practice Committee of the American Society for Reproductive Medicine, 2016). Treating uterine synechiae may also reduce the risk of miscarriage in women with recurrent abortions (Goldenberg et al., 1995).
We also found hysteroscopic signs of endometritis in 4% of the patients. While diagnosis is made by histology, endometritis can be suspected by TVS based on endometrial thickening, presence of free fluid in the pelvis and painful uterine mobilization during imaging, or at hysteroscopy by the presence of edema and focal or diffuse hyperemia. Chronic endometritis is often asymptomatic and some studies have shown an association with implantation failure and recurrent miscarriage (Cholkeri-Singh & Sasaki, 2015). Another uncommon hysteroscopic finding in our patients was nonspecific endometrial "thickening", which had similar prevalence in the positive and negative TVS groups, suggesting no association with the endometrial thickness objectively measured by TVS.
The value of hysteroscopy as a routine investigation in the management of infertile women is a matter of debate. There is evidence that performing hysteroscopy prior to initiating IVF treatment may increase the chances of pregnancy in the subsequent IVF cycle in women who had one or more unsuccessful treatment cycles (Fatemi et al., 2010). A systematic review with meta-analysis including seven studies and 2545 women found moderate quality evidence of a beneficial effect of routine hysteroscopy on the IVF pregnancy rate, but the same review found only very low-quality evidence that such procedure increases the live birth rate (Di Spiezio Sardo et al., 2016b). Afterwards, two randomized clinical trials were concluded and showed no benefit of routine hysteroscopy to improve the live birth rate among women undergoing their first IVF cycle (Smit et al., 2016) or with a history of IVF failure (El-Toukhy et al., 2016). However, the prevalence of hysteroscopic alterations in these two clinical trials was low (<13%) compared to our study population (27.6%). This suggests that in our population the potential benefit of performing hysteroscopy before IVF might be underestimated by extrapolating the last clinical trial results.
The main methodological strengths of this study are the large number of participants, which allowed us to calculate the prevalence of uterine abnormalities with narrow confidence intervals, and the standardized hysteroscopic procedures performed with the same equipment and interpreted by the same staff, which reduced the risk of performance bias. Data accuracy was improved by using only standardized medical reports from a single center. The hysteroscopies were interpreted considering the clinical history and imaging findings of the patients, which is a more realistic scenario than if they had been performed blindly.
Some limitations of our research should also be noted. This is a retrospective study, which limits the quality and amount of data and increases the risk of selection bias. It was not possible to obtain data from the histological analysis of the lesions identified. Therefore, the main evaluation of the lesions was based on visual findings in hysteroscopy. Another limitation of the study is that the inter-operator variation of the diagnostic performance could not be measured retrospectively. Finally, our evaluation of TVS sensitivity to detect intrauterine lesions was based only on the record of ultrasound images compatible with the hysteroscopic aspect of the uterine cavity. The complexity of information used in clinical decision is difficult to address in a retrospective study. Since we had no access to the full medical history of the patients, we did not calculate the predictive value of TVS in this context because this would only be informative if we knew the expected prevalence of each lesion according to the patient's signs and symptoms.
In conclusion, our findings suggest a high prevalence of unsuspected alterations found by routine hysteroscopy before IVF, an age-dependent increase in the frequency of submucous leiomyoma and a low diagnostic sensitivity of TVS to detect intracavitary lesions. International guidelines do not recommend hysteroscopy as first line method to assess uterine abnormalities in infertile women (Practice Committee of the American Society for Reproductive Medicine, 2015), but they do not make specific recommendations for women preparing to IVF. We therefore believe that additional high quality evidence is needed to define whether there are any clinical or demographic groups that might benefit from routine hysteroscopy before IVF.
Footnotes
Funding and Conflict of Interest
This study received no funding and the authors report no conflicts of interest.
REFERENCES
- Bakas P, Hassiakos D, Grigoriadis C, Vlahos N, Liapis A, Gregoriou O. Role of hysteroscopy prior to assisted reproduction techniques. J Minim Invasive Gynecol. 2014;21:233–237. doi: 10.1016/j.jmig.2013.07.023. [DOI] [PubMed] [Google Scholar]
- Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care. Hum Reprod. 2007;22:1506–1512. doi: 10.1093/humrep/dem046. [DOI] [PubMed] [Google Scholar]
- Bosteels J, Kasius J, Weyers S, Broekmans FJ, Mol BW, D'Hooghe TM. Hysteroscopy for treating subfertility associated with suspected major uterine cavity abnormalities. Cochrane Database Syst Rev. 2015;2:CD009461–CD009461. doi: 10.1002/14651858.CD009461.pub3. [DOI] [PubMed] [Google Scholar]
- Carneiro MM. What is the role of hysteroscopic surgery in the management of female infertility? A review of the literature. Surg Res Pract. 2014;2014:105412–105412. doi: 10.1155/2014/105412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cholkeri-Singh A, Sasaki KJ. Hysteroscopy for infertile women: a review. J Minim Invasive Gynecol. 2015;22:353–362. doi: 10.1016/j.jmig.2014.12.163. [DOI] [PubMed] [Google Scholar]
- Di Spiezio Sardo A, Calagna G, Laganà AS, Vitale SG, Catena U, Scutiero G, Nappi C. Is Hysteroscopy Better than Ultrasonography for Uterine Cavity Evaluation? An Evidence-Based and Patient-Oriented Approach. J Endometr Pelvic Pain Disord. 2016a;8:87–93. doi: 10.5301/je.5000252. [DOI] [Google Scholar]
- Di Spiezio Sardo A, Di Carlo C, Minozzi S, Spinelli M, Pistotti V, Alviggi C, De Placido G, Nappi C, Bifulco G. Efficacy of hysteroscopy in improving reproductive outcomes of infertile couples: a systematic review and meta-analysis. Hum Reprod Update. 2016b;22:479–496. doi: 10.1093/humupd/dmw008. [DOI] [PubMed] [Google Scholar]
- El-Toukhy T, Campo R, Khalaf Y, Tabanelli C, Gianaroli L, Gordts SS, Gordts S, Mestdagh G, Mardesic T, Voboril J, Marchino GL, Benedetto C, Al-Shawaf T, Sabatini L, Seed PT, Gergolet M, Grimbizis G, Harb H, Coomarasamy A. Hysteroscopy in recurrent in-vitro fertilisation failure (TROPHY): a multicentre, randomised controlled trial. Lancet. 2016;387:2614–2621. doi: 10.1016/s0140-6736(16)00258-0. [DOI] [PubMed] [Google Scholar]
- Elsetohy KA, Askalany AH, Hassan M, Dawood Z. Routine office hysteroscopy prior to ICSI vs. ICSI alone in patients with normal transvaginal ultrasound: a randomized controlled trial. Arch Gynecol Obstet. 2015;291:193–199. doi: 10.1007/s00404-014-3397-z. [DOI] [PubMed] [Google Scholar]
- Ezzati M, Norian JM, Segars JH. Management of uterine fibroids in the patient pursuing assisted reproductive technologies. Womens Health (Lond) 2009;5:413–421. doi: 10.2217/whe.09.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatemi HM, Kasius JC, Timmermans A, van Disseldorp J, Fauser BC, Devroey P, Broekmans FJ. Prevalence of unsuspected uterine cavity abnormalities diagnosed by office hysteroscopy prior to in vitro fertilization. Hum Reprod. 2010;25:1959–1965. doi: 10.1093/humrep/deq150. [DOI] [PubMed] [Google Scholar]
- Goldenberg M, Sivan E, Sharabi Z, Mashiach S, Lipitz S, Seidman DS. Reproductive outcome following hysteroscopic management of intrauterine septum and adhesions. Hum Reprod. 1995;10:2663–2665. doi: 10.1093/oxfordjournals.humrep.a135763. [DOI] [PubMed] [Google Scholar]
- Pérez-Medina T, Bajo-Arenas J, Salazar F, Redondo T, Sanfrutos L, Alvarez P, Engels V. Endometrial polyps and their implication in the pregnancy rates of patients undergoing intrauterine insemination: a prospective, randomized study. Hum Reprod. 2005;20:1632–1635. doi: 10.1093/humrep/deh822. [DOI] [PubMed] [Google Scholar]
- Practice Committee of the American Society for Reproductive Medicine Diagnostic evaluation of the infertile female: a committee opinion. Fertil Steril. 2015;103:e44–e50. doi: 10.1016/j.fertnstert.2015.03.019. [DOI] [PubMed] [Google Scholar]
- Practice Committee of the American Society for Reproductive Medicine Uterine septum: a guideline. Fertil Steril. 2016;106:530–540. doi: 10.1016/j.fertnstert.2016.05.014. [DOI] [PubMed] [Google Scholar]
- Practice Committee of the American Society for Reproductive Medicine Removal of myomas in asymptomatic patients to improve fertility and/or reduce miscarriage rate: a guideline. Fertil Steril. 2017;108:416–425. doi: 10.1016/j.fertnstert.2017.06.034. [DOI] [PubMed] [Google Scholar]
- Rikken JF, Kowalik CR, Emanuel MH, Mol BW, Van der Veen F, van Wely M, Goddijn M. Septum resection for women of reproductive age with a septate uterus. Cochrane Database Syst Rev. 2017;1:CD008576–CD008576. doi: 10.1002/14651858.CD008576.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit JG, Kasius JC, Eijkemans MJC, Koks CAM, van Golde R, Nap AW, Scheffer GJ, Manger PAP, Hoek A, Schoot BC, van Heusden AM, Kuchenbecker WKH, Perquin DAM, Fleischer K, Kaaijk EM, Sluijmer A, Friederich J, Dykgraaf RHM, van Hooff M, Louwe LA, Kwee J, de Koning CH, Janssen ICAH, Mol F, Mol BWJ, Broekmans FJM, Torrance HL. Hysteroscopy before in-vitro fertilisation (inSIGHT): a multicentre, randomised controlled trial. Lancet. 2016;387:2622–2629. doi: 10.1016/s0140-6736(16)00231-2. [DOI] [PubMed] [Google Scholar]
- Tomaževič T, Ban-Frangež H, Virant-Klun I, Verdenik I, Požlep B, Vrtačnik-Bokal E. Septate, subseptate and arcuate uterus decrease pregnancy and live birth rates in IVF/ICSI. Reprod Biomed Online. 2010;21:700–705. doi: 10.1016/j.rbmo.2010.06.028. [DOI] [PubMed] [Google Scholar]