Abstract
Medical management along with stellate ganglion block is frequently given to prevent the vasculitis of fingers in patients of systemic lupus erythematosus (SLE). Bilateral stellate ganglion block is rarely given due to the concern of phrenic and recurrent laryngeal nerve palsy. In this article, we describe the management of a recently diagnosed SLE patient presented with progressive gangrene of fingers of both upper limbs. Meticulously planned serial bilateral ultrasound-guided stellate ganglion blocks were successfully given to prevent impending loss of digits with no complications.
Key words: Bilateral, clonidine, gangrene, hoarseness, systemic lupus erythematosus, stellate ganglion block, ultrasound, vasculitis
INTRODUCTION
Systemic lupus erythematosus (SLE) is a complex autoimmune disease with a wide variety of clinical and serological manifestations that may affect any organ. Vasculitis, characterised by the presence of inflammatory cell infiltration and subsequent necrosis of blood vessel walls, is among the most characteristic processes involved in the clinical evolution towards SLE.[1] Cutaneous vasculitis in SLE was found in 19–28% of 704 European lupus patients in a descriptive analysis.[2] The histological presentation is a severe pandermal vasculitis often accompanied by thrombosis with resultant cutaneous infarction which may cause loss of digits in patients.[3] To prevent this, medical management along with stellate ganglion block is given.[4,5,6,7,8] The use of ultrasound to perform the block is more effective than landmark technique due to correct anatomical deposition of drug.[9] However, bilateral stellate ganglion block is rarely given due to the concern of phrenic and recurrent laryngeal nerve palsy.[10,11,12] In this article, we describe the management of a recently diagnosed SLE patient who presented with progressive gangrene of fingers of both upper limbs. Accordingly, meticulously planned serial bilateral guided stellate ganglion blocks were successfully given by ultrasound technique to prevent impending loss of digits with no complications.
CASE
A 22-year-old female, weighing 53 kg, with a height of 153 cm, data entry operator by profession, presented to the outpatient skin department in January. The patient reported with gangrene and black spots of multiple fingers and toes with severe pain since last one month. She was diagnosed with SLE and was started on prednisolone and hydroxychloroquine. A Doppler examination of limbs was performed with contrast injected intravenously through the left internal jugular vein to prevent venous contamination in limbs since all limbs were affected and were to be evaluated. CT angiography of upper limbs revealed attenuation of bilateral radial and ulnar arteries with poor distal run off seen in left radial artery and in left ulnar artery run off till hand was seen. No thrombus was seen. In the lower limbs, bilateral arteries below the knees were attenuated. Right anterior tibial artery and right peroneal artery were attenuated and left posterior tibial artery was totally obliterated [Figure 1a]. No thrombus was seen.
Figure 1.
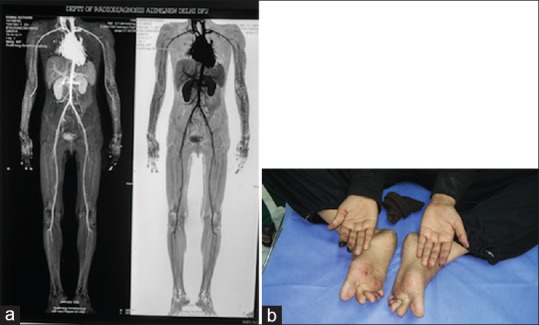
(a) Computed tomography (CT) angiogram done before sympathectomy blocks reveals attenuation of bilateral brachial arteries, bilateral radial arteries, bilateral ulnar arteries and bilateral below knee arteries (attenuation of right anterior tibial artery, right peroneal artery, total obliteration of left posterior tibial artery). (b) Wet gangrene of right index and middle finger and left index finger and thumb with multiple black spots on fingers and toes
For the management of pain and gangrene of her fingers and toes, she was referred to the pain clinic of the anaesthesia department. On examination, she had gangrene in the right index and middle finger, left thumb and index finger with multiple black spots in rest of the fingers and toes [Figure 1b]. She had rest pain of numerical rating score (NRS) 8 in upper limbs and NRS 6 in lower limbs. She was very anxious and being a data entry operator required her to primarily use her fingers while working on the computer. After taking her consent, she was admitted for sympathectomy blocks. All blocks were performed in the pain clinic block room after securing an intravenous cannula on the wrist and attaching pulse rate and non-invasive blood pressure monitors and pulse oximeter. The monitors were attached on ear lobes as none of her fingers and toes showed any waveform or value on pulse oximetry. She was given ultrasound-guided stellate ganglion nerve block (USGNB) with a linear probe of 13–6 MHz (Fujifilm SonoSite Edge) with 5 ml of 0.25% ropivacaine and clonidine 15 μg on the more-affected right side. Clonidine was added as an adjuvant to prolong the effect of ropivacaine and for its vasodilatory effects as demonstrated previously.[13] The block was performed in long axis with 26 gauge 1.5 inches hypodermic needle attached to a 10-cm extension line without giving prior local anaesthetic because of the small-gauge needle used to perform the block [Figure 2]. The needle was inserted from lateral to medial side of the neck, placing the needle tip between longus colli muscle and carotid sheath at level C7 vertebra—the anatomical location of stellate ganglion. Before injecting the drug, saline was injected to ensure the needle tip is not placed either in longus colli muscle or within the carotid sheath [Figure 3]. After monitoring for any untoward side effects for an hour, a left-sided USGNB with the same drug volume was injected, and the patient was observed for another 1 hour. Her NRS decreased to 3 but, after 5 hours, she again complained of pain of similar intensity. Therefore, a bilateral USGNB was repeated in the evening with similar drug injectate and precautions. The next morning, she reported NRS >5, and thus a continuous stellate ganglion block on the more-affected right side with plain 0.25% ropivacaine 2 ml/h was planned with left side USGNB planned twice a day. For continuous infusion under ultrasound guidance, an epidural needle was used to perform the block and epidural catheter was threaded to place the catheter tip between longus colli muscle and carotid sheath at level C7 vertebra. The catheter was also tunnelled at the skin entry point. Left-sided USGNB was performed twice a day, both times, after stopping the infusion of the right side for an hour before and after the block. Catheter was inserted thrice in the course of treatment of 35 days. Catheter tip was checked for correct position twice a day, and infusion was disconnected at night between 12 and 4 am for the patient to sleep comfortably. The average time of correct position of the catheter tip was 3–5 days. At every block, the spread of local anaesthetic was looked for to prevent deposition of drug either in the adjoining vessels or inside the carotid sheath to avoid phrenic nerve palsy. In addition, precaution was taken to avoid deposition of drug in longus colli muscle, which would result in an ineffective block. In about a week, the gangrene of the patient's fingers started improving. She was admitted for 35 days during which a total of 64 USGNB injections were given. For lower limbs, a single epidural injection block was given twice with 8 ml of 0.25% ropivacaine and a continuous epidural infusion was given once with 3 ml/h of 0.125% ropivacaine for 3 days. None of this resulted in any motor weakness. With this treatment, the blackness of toes of lower limbs and pain completely regressed. Upper and lower limb infusions were never given simultaneously, and the total dose of ropivacaine was calculated at all times and kept within safe limits with intense monitoring during the peri-block period. 20% lipid and resuscitative equipment were kept in stand-by at all times. Supportive treatment to keep all limbs warm with gloves/socks was ensured and enforced at all times. Medical management was continued.
Figure 2.
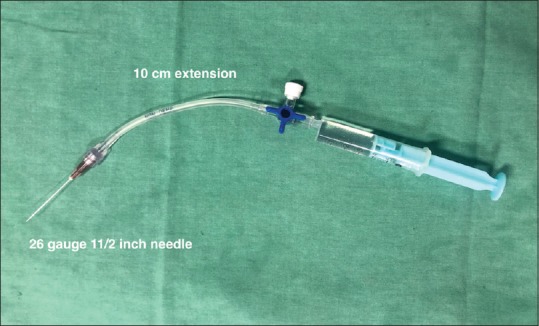
26 G 1.5 inches hypodermic needle attached to 10 cm extension line to perform the block
Figure 3.
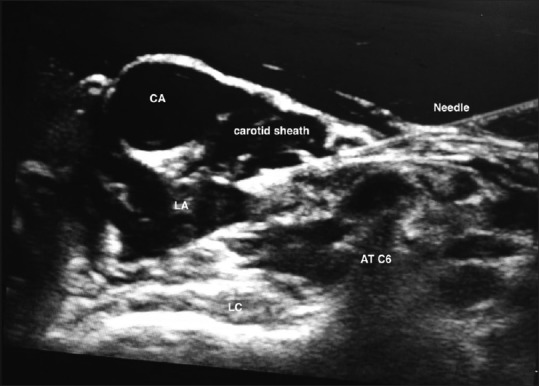
Spread of saline between longus colli muscle and carotid sheath. CA: Carotid artery; AT: Anterior tubercle; LC: Longus colli muscle; LA: Local anaesthetic
At every block, the pulse oximeter probe was attached to all fingers and toes, which showed improvement in the quality of waveform and/or pulse oximeter value after every block. Thirteen days after the commencement of blocks (around halfway through the 35-day treatment), repeat computed tomography (CT) angiography revealed bilateral ulnar arteries to be unremarkable in contrast to previous report. Right radial artery was normal and there was increase in calibre of left radial artery, both showing improvement from previous reports. Similarly there was marked improvement seen in lower limbs with normal bilateral anterior tibial arteries, bilateral peroneal arteries and right posterior tibial artery. Only posterior tibial artery remained attenuated [Figure 4a].
Figure 4.
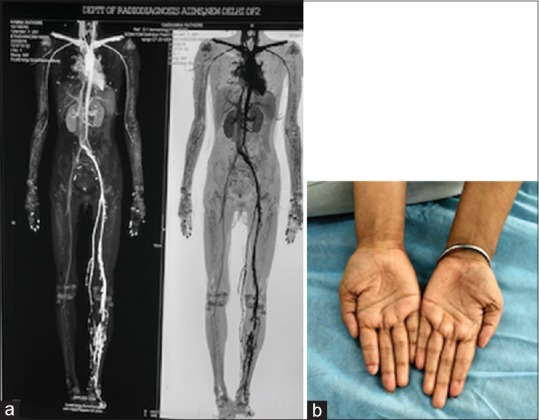
(a) Repeat CT angiography after 13 days of sympathectomy block reveals unremarkable bilateral brachial arteries, bilateral ulnar arteries, normal right radial artery and increase in calibre of left radial artery. In lower limbs bilateral anterior tibial arteries, bilateral peroneal arteries, right posterior arteries were normal and posterior tibial artery was attenuated. (b) At 7 months follow up, no gangrene or black spots on any fingers; loss of one half of the terminal phalanx of the right index finger, the most affected finger
By the end of 35 days, she had no rest pain in any of the fingers and toes. All her fingers with wet gangrene had dried. No repeat CT angiography was done due to financial constraints of the patient. Pulse oximetry waveform pattern improved in all fingers and toes with improvement in waveform and a value of >95% in all fingers.
At the 7-month follow-up, there was no pain or blackening of her fingers and toes, however, she had lost the distal part of the terminal phalanx of the right finger which was worst affected when she had first reported to us [Figure 4b]. Nevertheless, this did not affect her profession and she was happy to return to her job successfully. She is under follow-up with us since the last 2 years with no similar complaints.
DISCUSSION
About 70% of SLE patients report with skin symptoms. In the present case, the patient suffered from cutaneous vasculitis that manifested in the winter months possibly due to lack of central heating in the region.[11] If the progression of vasculitis is not halted in such patients, it results in digit loss which was the chief concern of the young patient as she was a computer analyst. The stellate ganglion is a cervical sympathetic ganglion which when blocked by local anaesthetic agents halts its sympathetic discharge resulting in dilatation of peripheral vessels preventing progression of gangrene in digits.[4,5,6,7,8] Stellate ganglion block is performed by depositing local anaesthetic between longus colli muscle and carotid sheath at level C6 or C7 vertebra—the anatomical location of the ganglion.[9] The use of ultrasound to perform this block has been found to be more effective and safer than landmark technique because of the prevention of drug deposition in closely located blood vessels like carotid artery, vertebral artery and inferior thyroid vessels. Ultrasound technique avoids needle injury to oesophagus when performed on the left side. Drug deposition in longus colli muscle is avoided which would result in an ineffective block. Incidence of hoarseness, which is caused by blockade of vagus nerve in carotid sheath or of recurrent laryngeal nerve, which lies medial to carotid sheath, is also decreased as one can visualise the needle tip position.[9] Phrenic nerve injury is infrequent, as it lies lateral to location of stellate ganglion.
The description of bilateral stellate ganglion block is scarce in literature. In one patient, the block was given by ultrasound twice in a ventilated patient for vasculitis secondary to sepsis with the authors justifying the bilateral block as the patient was ventilated negating concern for bilateral blockade of phrenic and recurrent laryngeal nerves.[10] In the other two described patients, ultrasound bilateral block was given only once for refractory ventricular arrhythmias and burning mouth syndrome.[11,12]
In the present case, the bilateral block was considered, as there was gangrene in the fingers of both limbs which if not treated immediately would have resulted in the loss of digits. Bilateral blocks were performed under ultrasound guidance with necessary precautions, meticulous planning, timing and monitoring as has been previously recommended.[14] All blocks were performed by a single senior experienced anaesthetist under monitoring in the block room and were meticulously planned. The first single-shot right USGNB did not alleviate the symptoms completely; and as the right side digits were maximally affected with gangrene in the present patient, a continuous infusion was planned with continuous monitoring of heart rate, blood pressure and oxygen saturation. Patient was also monitored for any difficulty in breathing and hoarseness. The catheter tip was checked with an ultrasound twice a day. Though the average time of correct catheter tip position was not more than 5 days, it arrested the progression of gangrene of right index finger. An interval of 1 hour was kept between the continuous right-side infusion and left-side blocks to observe any complications. The volume of drug in USGNB is considerably less than when landmark block is given, as was done in the present patient.
The only minor complication which the patient had was transient hoarseness which is reported previously and, in the present patient, the hoarseness occurred in 6 out of 64 blocks.[14] All resuscitative equipment and 20% lipid were always available in the event of any catastrophe. Supportive treatment to keep all limbs warm with gloves/socks was ensured and enforced at all times. Medical management was continued.
To treat vasculitis of lower limbs, lower limb sympathectomy blocks were not given due to the requirement of bilateral blocks which would have crossed the upper limit of the recommended ropivacaine dose. A previous study has concluded a similar degree of sympathetic blockade with both lumbar sympathetic blockade and epidural anaesthesia.[13] Thus, to achieve sympathectomy of both limbs, epidural infusion and boluses were planned which resulted in a good effect in the present patient. It was ensured that both epidural infusion and right stellate ganglion nerve block infusions were not administered at the same time to avoid a local anaesthetic overdose.
Sympathectomy blocks were required in all four limbs; thus, local anaesthetic overdosing was prevented by calculating the total dose of ropivacaine being administered whenever more than one block was planned in a day. All single-shot USGNBs were performed with clonidine 15 μg as an adjuvant to prolong the duration of the action of local anaesthetic and for its vasodilatory properties which was beneficial in this patient.[15]
To conclude, if bilateral stellate ganglion block is to be given in a patient it should always be with ultrasound guidance under strict monitoring. Block should be performed by experienced personnel.
Declaration of patient consent
The author certifies that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patients understand that her names and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Doyle M. Vasculitis associated with connective tissue disorders. Curr Rheumatol Rep. 2006;8:312–6. doi: 10.1007/s11926-006-0015-5. [DOI] [PubMed] [Google Scholar]
- 2.Vitali C, Bencivelli W, Isenberg DA, Smolen JS, Snaith ML, Sciuto M, et al. Disease activity in systemic lupus erythematosus: Report of the Consensus Study Group of the European Workshop for Rheumatology Research. I. A descriptive analysis of 704 European lupus patients. European Consensus Study Group for disease activity in SLE. Clin Exp Rheumatol. 1992;10:527–39. [PubMed] [Google Scholar]
- 3.Crowson N, Magro C. Cutaneous histopathology of lupus erythematosus. Diagn Histopathol. 2009;15:157–85. [Google Scholar]
- 4.Shiokawa Y, Morimoto M, Kamamoto H, Kamamoto H, Uchida T, Koga Y. Usefulness of perfusion index in evaluation of stellate ganglion block. Acta Medica Kinki Univ. 2009;34:83–6. [Google Scholar]
- 5.Kulkarni KR, Kadam AI, Namazi IJ. Efficacy of stellate ganglion block with an adjuvant ketamine for peripheral vascular disease of the upper limbs. Indian J Anaesth. 2010;54:546–51. doi: 10.4103/0019-5049.72645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim MK, Yi MS, Park PG, Kang H, Lee JS, Shin HY. Effect of stellate ganglion block on the regional hemodynamics of the upper extremity: A randomized controlled trial. Anesth Analg. 2018;126:1705–11. doi: 10.1213/ANE.0000000000002528. [DOI] [PubMed] [Google Scholar]
- 7.Hughes M, Herrick AL. Raynaud's phenomenon. Best Pract Res Clin Rheumatol. 2016;30:112–32. doi: 10.1016/j.berh.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Gunduz OH, Kenis-Coskun O. Ganglion blocks as a treatment of pain: Current perspectives. J Pain Res. 2017;10:2815–26. doi: 10.2147/JPR.S134775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Narouze S. Ultrasound guided stellate ganglion block: Safety and efficacy. Curr Pain Headache Rep. 2014;18:424. doi: 10.1007/s11916-014-0424-5. [DOI] [PubMed] [Google Scholar]
- 10.Bataille B, Nucci B, Mora M, Silva S, Cocquet P. Ultrasound-guided bilateral stellate ganglion blockade to treat digital ischemia in a patient with sepsis: A case report. Can J Anaesth. 2016;63:56–60. doi: 10.1007/s12630-015-0503-z. [DOI] [PubMed] [Google Scholar]
- 11.Scanlon MM, Gillespie SM, Schaff HV, Cha YM, Wittwer ED. Urgent ultrasound-guided bilateral stellate ganglion blocks in a patient with medically refractory ventricular arrhythmias. Crit Care Med. 2015;43:316–8. doi: 10.1097/CCM.0000000000001086. [DOI] [PubMed] [Google Scholar]
- 12.Walega DR, Smith C, Epstein JB. Bilateral stellate ganglion blockade for recalcitrant oral pain from burning mouth syndrome: A case report. J Oral Facial Pain Headache. 2014;28:171–5. doi: 10.11607/ofph.1165. [DOI] [PubMed] [Google Scholar]
- 13.Frank SM, El-Rahmany HK, Tran KM, Vu B, Raja SN. Comparison of lower extremity cutaneous temperature changes in patients receiving lumbar sympathetic ganglion blocks versus epidural anesthesia. J Clin Anesth. 2000;12:525–30. doi: 10.1016/s0952-8180(00)00207-5. [DOI] [PubMed] [Google Scholar]
- 14.Goel V, Patwardhan AM, Ibrahim M, Howe CL, Schultz DM, Shankar H. Complications associated with stellate ganglion nerve block: A systematic review. Reg Anesth Pain Med. 2019:pii: rapm-2018-100127. doi: 10.1136/rapm-2018-100127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kimura Y, Hamaguchi S, Okuda Y, Kitajima T. Addition of clonidine increases duration and magnitude of vasodilative effect induced by sympathetic block with mepivacaine in dogs. Reg Anesth Pain Med. 2001;26:329–32. doi: 10.1053/rapm.2001.25066. [DOI] [PubMed] [Google Scholar]


