Purpose of review
We present recent literature describing interventions for linkage to HIV care in the era of Universal Test and Treat (UTT) policies. We also provide information for ongoing studies of linkage to care strategies registered with ClinicalTrials.gov.
Recent findings
Differentiated service delivery for linkage to care involves implementing strategies that simplify and adapt HIV services to better serve individual needs and reduce unnecessary burdens on the health system. Recent strategies have focused not only on clinic-based populations testing for HIV but also emphasize community-based services and HIV self-testing, which create different challenges for linkage to the healthcare system. Some recent developments in linkage to care strategies include: case management, care integration with other desirable health services, financial incentives, home-based, and peer-led services. The demonstrated strategies have varying levels of success and engagement in care; further work is needed to address ongoing barriers in HIV care.
Summary
Progress towards meeting the 90–90–90 benchmarks has left gaps in linkage to care that require care-system development to facilitate increased access to care under UTT policies. Most notably, new strategies will need to focus on addressing the distinct needs of key populations and bolstering linkage to care from community-based and self-testing services.
Keywords: antiretroviral therapy initiation, barriers to care, HIV care linkage
INTRODUCTION
With the ambitious goal to end the AIDS epidemic by 2030, UNAIDS has set clear benchmarks with the 90–90–90 strategy for 2020. Reaching the second 90 requires that 90% of people living with HIV (PLWH) know their status, and 90% engage in antiretroviral therapy (ART) [1]. Global estimates report that 79% of PLWH know their status and 78% are on treatment, with 86% reaching viral suppression [2]. Although progress towards global targets has steadily increased, gaps in the cascade of care remain, including approximately 8.1 million PLWH who are unaware of their status and thus not accessing ART [2]. In addition to extending testing programs, expansion of subsequent linkage to HIV care and treatment is needed to achieve the 2020 benchmarks [3▪].
Strategies for linkage to care for HIV and initiation of ART are inherently related to the method of testing, as testing is a first step in the HIV care cascade and often serves as the initial link to the formal healthcare system. It is increasingly important to understand differentiated service delivery strategies and outcomes for linkage from different testing modalities as the endorsement of universal test and treat (UTT) has seen global expansion, whereby all PLWH are initiated on ART regardless of disease stage [4]. UTT gradually becoming standard of care has led to increased demand for linkage to ART, including for PLWH who are asymptomatic [5,6▪,7,8▪▪,9].
Moreover, as the second step of the 90–90–90 cascade, initiation of ART is a pivotal determinant of the final 90, successful maintenance of ART leading to viral suppression. With UTT and increased engagement with HIV care for those PLWH, prevention of infection also increases with the proportion of PLWH with undetectable viral loads, a strategy known as ‘Treatment as Prevention’ [10–12]. A US-based mathematical model estimates that the majority of HIV transmissions occur among people who have known HIV status but are not in care [13]. To increase uptake of HIV testing and linkage, leading to subsequent viral suppression, rapid and enhanced efforts are needed to improve linkage to care.
This review provides an overview of recently published, novel interventions for increasing linkage to HIV care grouped under the categories of: clinic-based linkage, linkage from community-based settings, and linkage from self-testing and index testing (assisted partner notification). A summary of these studies is provided in Table 1. We provide insight into the contributions of these studies to the literature on linkage to HIV care and conclude with commentary on the opportunities for further research and development of HIV care linkage programs. Selected on-going studies of linkage, registered with ClinicalTrials.gov, are presented in Table 2.
Table 1.
Reviewed interventions for linkage to HIV treatment
| Reference | Country | Intervention | Primary outcome | Primary outcome results | Secondary outcomes |
| Clinic-based linkage | |||||
| Halperin et al. [20] | United States | Immediate ART | Immediate ART initiation; viral suppression; retention in care | Immediate ART (100% newly Dx vs. 99% ART naïve); achieved viral suppression (99 vs. 94%, P = 0.0954); retention in care (92 vs. 80%, P = 0.012) | |
| Samet et al. [22▪] | Russia | Strengths-based case management | Linkage to HIV care; improved CD4 count at 12 months | 51% of intervention group and 31% of controls linked to HIV care (AOR 2.34; 95% CI 1.49-3.67; P < 0.001); no difference in CD4 count | Retention in HIV care months within 12 months; appropriate HIV care; self-reported hospitalizations |
| Solomon et al. [23▪▪] | India | Integrated care centers for MSM and PWID | Self-reported HIV testing | 31% higher at integrated center but nonsignificant, adjusted prevalence ratio 1.31, 95% CI 0.95–1.81, P = 0.09 | Awareness of status; receipt of HIV medical care in previous 6 months; CD4 cell count; use of co-trimoxazole; current use of ART and HIV RNA less than 150 copies/ ml prevalence of viraemic individuals in the population; HIV incidence estimated; stigma; alcohol use; depression; self-report spousal testing; risk behaviors; service utilization |
| Schwartz et al. [24] | South Africa | HIV care integration with reproductive services | Pregnancy incidence; HIV transmission | 99 pregnancies in 89 women; 0 transmissions | Adoption of, and sustained engagement in, safer conception care; achievement of clinical readiness for conception; HIV prevention indicators (repeat HIV testing uptake, viral suppression at pregnancy, and PrEP uptake); pregnancy outcomes |
| Community-based linkage | |||||
| MacKellar et al. [27] | Eswatini | Peer-delivered linkage case management and same day ART | Enrollment and initiation of ART care | 98% enrolled in care; 83% rapidly initiated ART; after introduction of UTT 97% initiated ART | |
| Ayieko et al. [8▪▪] | Kenya and Uganda | Comprehensive linkage with test and treat | Proportion linked within 1 year | 73.4% linked within 1 year | Factors associated with linkage at 7, 30, and 365 days after diagnosis |
| Labhardt et al. [28] | Lesotho | Same day ART | Rate of linkage to care within 3 months; viral suppression at 12 months | 68.6% in intervention group linked within 3 months; 50.4% achieved viral suppression | Viral suppression at 6 months; 12-month follow-up; 12-month mortality; 12-month changes in CD4 cell count, hemoglobin level, bodyweight, and occurrence of a new clinical WHO stage 3 or 4 event |
| Tun et al. [19] | Tanzania | Community-based ART delivery for FSW | ART Initiation | 100% ART initiation among intervention arm compared with 71.5% in control (P < 0.001) | 6-month treatment-related outcomes |
| Kuhns et al. [18] | United States | Assistance with structural barriers and determinants of care | Linkage to HIV care; engagement in care | All declined overtime and the intervention was not associated with significant group difference | |
| Linkage from self-testing and index testing | |||||
| Choko et al. [32▪▪] | Malawi | Incentives and linkage support among partners of ANC attendees | Proportion of male partners who were reported to have tested for HIV and linked into care or prevention within 28 days | Higher proportions of men linked in groups for HIVST+ $3 and HIVST + $10 (geometric mean 41 and 52%, respectively, P < 0.001) and phone reminder (22.3%, P = 0.021) | Proportion of male partners who tested for HIV within 28 days; risk of adverse or serious adverse events |
| Jubilee et al. [34] | Lesotho | Index testing among children and sexual partners | Overall HIV positivity rate among index contacts | 4.2% (454/10,854); 25.1% (114/454) children; 5.7% (26/454) adolescents; 69.2% (314/454) adults. Linkage higher among all age groups (92 vs. 65% children, 73 vs. 58% adolescents, 72 vs. 51% adults) | |
| Tafuma et al. [35] | Zimbabwe | Home-based index testing | Linkage to care | 63% (410) linked within 7 days; 85% linked within 30 days. | |
ART, antiretroviral therapy; CI, confidence interval; PrEP, pre-exposure prophylaxis; STI, Sexually Transmitted Infection.
Table 2.
Selected on-going studies of linkage to care for HIV in ClinicalTrials.gov
| Title | Clinicaltrials.gov number | Country | Intervention | Primary outcomes | Secondary outcomes | Estimated completion date |
| Clinic-based linkage | ||||||
| PlusCare: Mobile Platform to Increase Linkage to Care in Adolescents Living With HIV/AIDS | NCT03758066 | United States | PlusCare is a mobile application designed to be used by youth and young adults with HIV and case managers. | CD4 cell count; viral load; HIV medical visit frequency and gaps in medical visits | Self-report levels of adherence; quality of life; self-efficacy measurement; system usability (user satisfaction) | March 2020 |
| LEAN: Leveraging mHealth and Peers to Engage African- Americans and Latinxs in HIV Care | NCT03934437 | United States | Mobile health-enhanced linkage to care and retention | Proportion with suppressed HIV viral load | Proportion retain in care | September 2023 |
| CVCTPlus: A Couples-Based Approach to Linkage to Care and ARV Adherence | NCT01772992 | United States | MSM couples receive HIV testing and counseling as a dyad, some couples receive ARV adherence as dyad | Linkage to care within 3 months: >2 routine HIV care visits; 2+ CD4 tests; 2+ viral load tests | Retention in care | December 2019 |
| Rapid HIV Treatment Initiation, Access and Engagement in Care | NCT03512964 | United States | Rapid HIV treatment initiation for newly diagnosed and out-of-care PLWH | Number of patients who receive rapid HIV treatment initiation | Acceptability of intervention; number of patients offered intervention; number of patients with same-day-start | November 2020 |
| LINC-II: Linking Infectious and Narcology Care-Part II | NCT03290391 | Russia | Strengths-based case management, rapid ART initiation, 13 months of pharmacological treatment for opioid use disorder | Undetectable HIV viral load | Initiation of ART; change in CD4 count; retention in HIV care; undetectable HIV viral load | December 2021 |
| Community-based linkage | ||||||
| VIBRA: Village-based vs Clinic-based ART Care - a Cluster Randomized Controlled Trial in Lesotho | NCT03630549 | Lesotho | Home-based same-day ART initiation, village-based ART refill, and customizable SMS reminder and result delivery | 12-month viral suppression | 6-month viral suppression; alternative viral suppression at 12 and 6 months (viral load <1000 copies/ml); sustained viral suppression (VL <20 copies/ml at 6 and 12 months); 1-month and 3-month linkage to care; 6 and 12 months retention in care; all-cause mortality at 12 months; LTFU at 12 months; transfer out at 12 months | September 2020 |
| GIRLS: High-yield HIV Testing, Facilitated Linkage to Care, and Prevention for Female Youth in Kenya | NCT02735642 | Kenya | Referral to care with and without SMS reminders and incentives. Choice to self-test, test in community, or test in facility | Newly diagnosed HIV infection; uptake of recruitment strategies; uptake of different testing modalities; HIV diagnosis; high-risk HIV-negative persons identified | Linkage to care percentage; time to linkage to care; retention in care; completion of VL testing; proportion reporting HIV risk behaviors, and condom use; re-testing uptake and results | July 2020 |
| Enhanced Linkage to HIV Care Following Home-Based HIV Testing in Rural Uganda | NCT02545673 | Uganda | Enhanced linkage to care behavioral intervention guided by the HIV Stigma Framework, paper-based referrals with CD4 test results delivered in home | HIV viral load suppression | Linkage to HIV care; time to HIV care; receipt of co-trimoxazole; time to receipt of co-trimoxazole; receipt of ART; time to receipt of ART; short-term retention in care (missed visits), short-term retention in care (kept/scheduled visits and 4-month constancy) | May 2021 |
| CHIEDZA: Community Based Interventions to Improve HIV Outcomes in Youth: A Cluster Randomised Trial in Zimbabwe | NCT03719521 | Zimbabwe | Community-based package of comprehensive reproductive health services offered to youth, including ART initiation and adherence support | Viral suppression among HIV-positive individuals | Knowledge of HIV-positive status; coverage of antiretroviral therapy (ART) among those who know their status; viral suppression among those reporting ART | September 2020 |
| iSTAR: Intervention for Sustained Testing and Retention Among HIV-infected Patients | NCT03018002 | Nigeria | Community-based testing, church-based Heath Advisors and integrated network of case management for HIV-infected pregnant women identified during baby showers | Linkage in care (percent of participants with >1 HIV medical care visit following diagnosis); retention in care (percent of participants with 2+ viral load measurements in 12 months) | ART initiation at 1 month; viral suppression (% of participants whose two most recent viral loads are suppressed) | March 2020 |
| Bringing South African Men Into HIV Counseling and Testing and Care | NCT03794245 | South Africa | Men-centric community or clinic-based testing with accompaniment to clinic by community health worker | Percentage of men testing for HIV | Percentage of HIV+ men initiating HIV treatment; percentage of men with suppressed VL | April 2020 |
| HITS: Home-based Intervention to Test and Start | NCT03757104 | South Africa | Microincentives to test and link-to-care among male and female community members, male-sensitive support application to facilitate testing and linkage | HIV test uptake at point of offer; HIV treatment linkage at 1 year; population-level HIV viral suppression in men; population-level HIV-related mortality in men; population-level HIV incidence in young women | HIV testing uptake at point of test offer in women; HIV treatment linkage at 1 year in women; population-level HIV viral suppression (both sexes); population-level viral suppression (both sexes) [reference clinicaltrials.gov for additional secondary outcomes] | December 2022 |
| Linkage from self-testing and index testing | ||||||
| SHARP: Study of HIV, HCV, APS and Phylogenetics for PWID | NCT03447210 | Kenya | Assisted partner notification and linkage services for the needle sharing partners of PWID | Sexual partners tested; injecting partners tested; partners diagnosed with HIV and HCV; HIV-infected partners linked to HIV care; HCV-infected partners linked to HCV care; index participants linked to HIV and HCV care | May 2022 | |
| Project Nexus: Providing Online Counseling for Home-Based HIV Testing | NCT02335138 | United States | MSM couples receive HIV videocounseling service with self-test at home | Process and use of communal coping (outcome efficacy, couple efficacy, and communal coping to reduce HIV threat); changes in sexual agreements; changes in sexual behaviour | Linkage to care [within 3 months): attend more than one clinical care appointment; more than one CD4 test; more than one viral load | May 2019 |
| FastTrack: Improving Prevention Systems to Reduce Disparities for High Priority Populations | NCT03778164 | United States | Enhanced HIV/STI testing, immediate field-based ARV/PrEP start, clinic navigation, and enhance linkage support provided in the existing partner notification system | Acceptance of HIV testing; PrEP/ARV initiation; linkage to PrEP/HIV care | STI testing | September 2022 |
ARV, antiretroviral therapy; HBV, hepatitis B virus; HCV, HBV, hepatitis C virus.
Box 1.
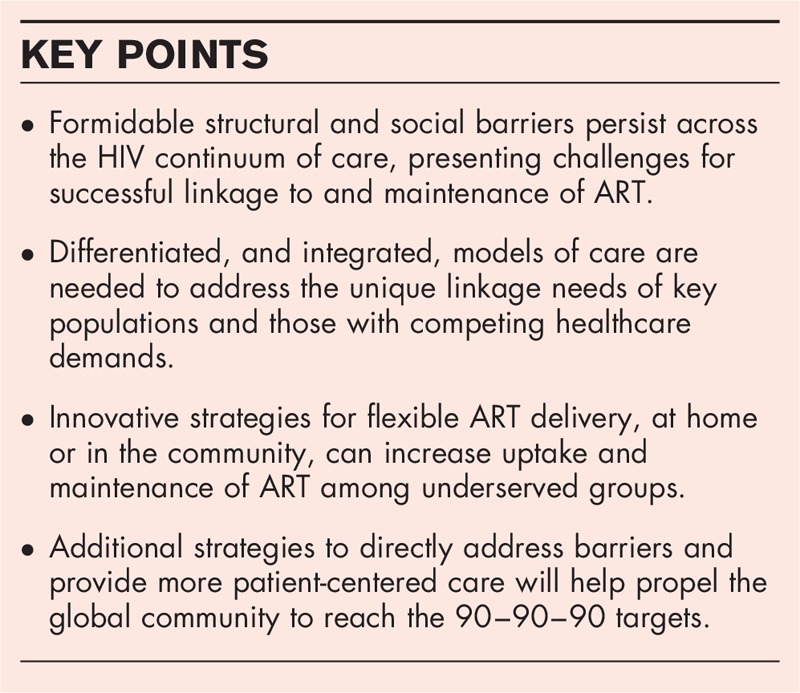
no caption available
CLINIC-BASED LINKAGE
HIV testing and linkage to ART within traditional clinical settings serves as the bedrock for many HIV care programs. Clinic-based testing often engages symptomatic patients with lower CD4 counts and a more urgent need to evaluate for opportunistic infections and promptly start ART [14]. Additionally, clinic-based testing often leads to better linkage outcomes, as compared with community-based testing, because testing and service provision may be in closer proximity [14,15]. However, engagement in HIV care programs in clinical settings are subject to multiple formidable and interacting barriers, including stigma and transportation costs, which may result in delays or deferral of testing and linkage [16]. Furthermore, key populations, such as people who inject drugs (PWID), transgender persons, or females who engage in sex-work (FSWs), may experience additional situational stigma and increased barriers preventing linkage to care [17–19]. Novel strategies to address some of these barriers modify access to HIV care, from testing to linkage, within clinic settings.
Halperin et al.[20] assessed care outcomes for an immediate ART program in a clinic in the Southern United States where more than 50% of patients were participating in Medicaid (public health insurance safety net). Rapid ART was provided in two groups: patients who were newly diagnosed, linked immediately, and offered same-day ART and those who were ART-naïve, diagnosed greater than 72 h (range, 4 days to 25 years), linked on the day of contact and offered same-day ART. Among the newly diagnosed, 100% were started on immediate ART, 99% achieved viral suppression, and 92% were retained in care. Among PLWH that were diagnosed previously, 99% initiated same-day ART, 94% achieved viral suppression, and 80% were retained in care. Those in the previously diagnosed group experienced higher rates of mental health diagnoses (20 vs. 33%, P = 0.039), perhaps indicative of competing needs. This intervention is notable for its success in maintaining patients in the cascade of care with an immediate initiation of ART and little attrition.
Case management, often facilitated by peer-counselors, endorses HIV referral and linkage to care as an ongoing process rather than a one-time event. A study of case management performed in St. Petersburg, Russia, used a modified ARTAS (Antiretroviral Treatment Access Study) case management intervention [21], tailored to the Russian context, to address societal and structural barriers to linkage for HIV care for PWID in an urban center [22▪]. These barriers included stigmatization of drug use and resource siloes for addiction and infectious diseases treatment services. The LINC intervention (Linking Infectious and Narcology Care) integrated a peer-led, strengths-based case management strategy with infectious disease and narcology care. Although the LINC intervention group had higher rates of linkage at 6 months compared with standard of care (51 vs. 31%, P < 0.001), the difference was not maintained at 12 months. A second LINC study underway is offering concurrent pharmacologic treatment for opioid use disorder (ClinicalTrials.gov #NCT03290391). These studies highlight the importance of transcending the separation between HIV care and other medical services and the need to improve durability of linkage and retention in these integrated programs.
In response to low uptake of HIV testing and linkage services, Solomon et al.[23▪▪] investigated the use of integrated care centers for key populations in 11 cities in India. Six care centers were created within opioid agonist treatment centers and five MSM centers within government-sponsored health services. After implementation, recent HIV testing was 31% higher at integrated care centers, when compared with usual care sites (nonsignificant). At the individual level, participants at integrated care centers were more likely to report recent testing for HIV [adjusted prevalence ratio (PR) 3.46, 95% confidence interval (CI) 2.94–4.06] and receiving ART (adjusted PR 1.25, 95% CI 2.94–4.06), and significantly higher rates of prevention strategies (needle and syringe exchange 2.27, 1.76–2.94; opioid agonist treatment 4.25, 3.17–5.69; STI evaluation at MSM sites 3.71, 2.05–6.73; partner testing 1.61, 1.36–1.91). Although the research design did not have the population effects expected by the investigators, 94% of PWID and 99% of MSM who received care at an integrated center either strongly agreed or agreed with the statement ‘I am satisfied with the services I received today’.
HIV care integration with reproductive health services is a strategy for preventing vertical and horizontal transmission of HIV in cases of serodiscordant couples with pregnancy intentions. A study in Johannesburg, South Africa, demonstrated the use of safer conception care integrated with ART and PrEP provision for couples with at least one partner living with HIV [24]. ART was initiated in 91% (73/80) of the HIV-positive participants not on ART and PrEP was initiated by about one-quarter of HIV-negative participants (28%, 28/101). The comprehensive intervention package was adjusted to individual participant's needs. Adoption of the services was high, and there were no incidents of onward transmission to either partners or infants.
Case management and integration of care with other health services improves HIV care for PLWH by reducing barriers to care. Modifications to the clinical setting, such as those described above, addresses the demonstrated need to make the linkage process more patient-centered.
COMMUNITY-BASED LINKAGE
Testing services offered in homes or within community settings offer many benefits with regard to privacy and convenience and are acceptable in many settings [14,15,19]. However, testing outside of traditional clinic facilities presents the formidable challenge of providing access to care to PLWH, most often necessitating a link to formal health systems [8▪▪,16]. Even large trials with wide access to treatment and implementation of referral for linkage strategies have yielded delays in ART uptake [8▪▪,25,26].
An intervention in Eswatini offering the CDC recommended package of peer-delivered linkage services saw similar success in linkage to ART among patients tested in community versus facility settings (overall time periods, 87 vs. 86%, respectively). The intervention included peer-supported case management, escort, and reimbursement for transportation costs, treatment navigation, appointment reminders, and other psychosocial support. Among those joining the study during the period of Test and Start, 97% of participants diagnosed in a community setting enrolled in HIV care within 90 days of program consent [27]. The findings support the acceptability of the CDC recommended package, and the utility in helping programs reach near universal linkage to HIV care and initiation of ART.
Ayieko et al.[8▪▪] assessed linkage outcomes of a patient-centered strategy as part of the SEARCH study, a community-based test-and-treat trial in Kenya and Uganda. The strategy included personal introduction to clinic staff member at time of positive test, access to a resource ‘hotline’, one-time reimbursement for transportation to clinic, appointment reminders, and telephone and in-person tracing if the first appointment was missed. Nearly three-quarters of the participants were linked after 1 year, and 50% linked within the accelerated linkage window of 7 days. Those who tested through home-based testing were about 25% less likely to link within a month, as compared with those tested through multidisease community health campaigns. Of note, those who previously knew their HIV status (427, 21%) were slower to link to care.
A randomized trial in Lesotho (CASCADE) sought to understand the effect of offering same-day ART vs. referral to a clinic after positive home-based HIV test. Among those provided same-day ART, 69% were linked to care at 90 days compared with 43% in the standard-of-care health facility referral group. The differences in outcomes remained statistically significant for viral suppression 11–14 months after enrollment with 50% in the same-day ART and 34% in standard-of-care group [28]. The authors posit that immediate linkage following home-based testing may be a more scalable strategy than multicomponent facility-based interventions for endemic areas.
An intervention for community-based ART delivery was demonstrated for FSW in Tanzania, in a setting of high-disease prevalence (27% compared with 6.5% among general population adult women), high levels of stigma, and low levels of ART access [19]. Participants in the intervention arm received immediate adherence counseling and 1-month supply of ART with ongoing ART delivery at a community location of their choosing, the comparison received facility-based ART services [19]. Participants in the intervention arm were more likely to have initiated ART (100 vs. 72%, P = 0.04), to be taking ART at 6 months (100 vs. 95%, P < 0.001), and less likely to have stopped taking ART for more than 30 days continuously (0.9 vs. 5.7%, P = 0.008). The FSWs receiving community-based ART were also less likely to report high internalized HIV stigma. This intervention addressed social and structural barriers by allowing immediate ART initiation and ongoing ART provision in community venues, supporting community-based ART not only for those deemed stable at the facility-level (as per current Tanzanian guidelines) but also for those initiating treatment.
The TransLife Care (TLC) project addressed structural barriers to engagement in HIV care by providing housing, employment, legal, and out-reach based health services with HIV case management for transgender women, who experience a disproportionate burden of HIV in the United States [18]. The services were delivered by a transgender individual when possible. Over 24 months of follow-up, receiving any element from the package of services was associated with engagement in care, more visits, retention in care, and viral load testing. However, the authors also report that engagement with care and retention declined with time, and there was no significant association between receiving the intervention and viral suppression. Regardless, this notable intervention yielded improvement in linkage by directly addressing determinants of access to HIV care in transgender people in the United States.
The convenience offered by community-based and self-testing necessitates innovative solutions to linkage to the formal healthcare system. However, programs with either direct or indirect linkage support can help reduce barriers experienced by PLWH.
LINKAGE FROM SELF AND INDEX TESTING
HIV self-testing (HIVST) is increasingly recognized as a novel method for engagement in HIV treatment and prevention programs, particularly for members of key populations, as it directly addresses barriers related to stigma and discrimination in health facilities and at community venues [15,29]. HIVST expanded in Africa through policy and market changes catalyzed by the STAR (Self-Testing Africa) Initiative and endorsed by WHO in 2016. With the expansion of HIVST in six southern African countries through the STAR Initiative, multiple concerns were raised with regards to linkage to confirmatory testing and ART following HIVST [30]. Documentation of linkage is important as many studies show that expanded access to diagnosis through HIVST does not necessarily increase ART uptake [31,32▪▪,33].
In STAR, preferences for linkage to HIV care services following a reactive self-test were explored through discrete choice experiments embedded in a household survey [31]. The most important barriers cited to linkage after HIVST were costs associated with a clinic-based confirmatory testing and long wait times in clinics; facilitators were noted as follow-up phone call and follow-up care offered in the home of a counselor. The findings indicate a need for additional follow-up after a positive HIVST and creative strategies to reduce barriers to promote confirmatory testing and additional follow-up after positive HIVST.
Choko et al. evaluated the role of financial incentives after self-testing for male partners of antenatal clinic (ANC) attendees. This is a particularly important population for improved HIV testing and linkage, given the low rates of testing and linkage in men and the risk of vertical transmission during pregnancy [32▪▪]. The five-arm trial provided a standard-of-care arm and four modified interventions to incentivize linkage including: receipt of two HIVST kits, two HIVST kits and $3, two HIVST kits and $10, two HIVST kits and entry into a lottery, and 2 HIVST kits and a phone call reminder [32▪▪]. The primary outcome was the proportion of male partners who tested for HIV and linked to care or prevention within 28 days, with referral for ART or circumcision, accordingly. Seventeen percent reported testing in the standard-of-care arm whereas men in all testing arms had higher testing rates, ranging from 87 to 95% (P < 0.001 for all five arms). Meeting the primary linkage endpoint was significantly associated with financial incentive arms [HIVST + $3 geometric mean 41%, adjusted risk ratio (aRR) 3.01 (95% CI 1.63–5.57); HIVST + $10 52%, aRR 3.72 (95% CI 1.85–7.48); both P < 0.001] and phone reminder [22.3%, aRR 1.58 (95% CI 1.07–2.33), P = 0.021]. The study showed the most promise for self-testing with cash incentives for uptake of HIVST and linkage to care among men.
Jubilee et al.[34] described a program of home-based visits for index testing of biological children and sexual partners of PLWH, offering a patient-friendly strategy accommodating flexible hours in Lesotho. Seventy-five percentage of PLWH offered the intervention accepted an index visit and the trial resulted in higher HIV positivity across all groups when compared with nonindex testing. Importantly, linkage rates were higher across all groups accessed through index testing than other HIV testing services (92 vs. 65% in children, 73 vs. 58% in adolescents, and 72 vs. 51% in adults).
A second study of index testing in SSA saw 63% (410) of PLWH linked within 7 days (rapid ART initiation), and 85% linked within 30 days [35]. Participants were 4.1 times more likely to link within 7 days during a period in which ‘expert clients’ assisted with linkage (75% linkage).
The intervention included household index case testing, linkage to care, defaulter tracking, and identification and formation of community ART refill groups. Clients could link to any facility and records were reconciled to determine linkage. For the duration of the study, the number linked increased and the time to link decreased.
CONCLUSION
To maximize the impact of UTT and achieve UNAIDS targets, substantial gaps in linkage to HIV care must be addressed. Patient-centered care models can increase uptake and maintenance of ART among underserved groups and integrate care for addiction and mental health, as these become increasingly signification sources of comorbidity [17,19,36,37]. As ART programs expand and opportunities increase for PLWH to become ‘lost to follow-up’, re-engagement opportunities or ‘side-doors’ must exist [38]. By focusing on programs for key populations, as well as retention and re-engagement, the global community can directly address barriers to care and more rapidly approach the 90–90–90 targets.
Acknowledgements
None.
Financial support and sponsorship
This work was supported by the National Institutes of Health: K24 AI141036 and R01 MH108427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work was also supported by the Weissman Family Massachusetts General Hospital Research Scholar Award.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.UNAIDS. Fast-Track Ending the AIDS Epidemic by 2030 [Internet]. UNAIDS; 2014. Available at: http://www.unaids.org/en/resources/documents/2014/JC2686_WAD2014report [Accessed 11 June 2019] [Google Scholar]
- 2.UNAIDS. Fact Sheet – Global AIDS Update 2019 [Internet]. Available from: aidsinfo.unaids.org [Google Scholar]
- 3▪.Kelly N, Maokola W, Mudasiru O, McCoy SI. Interventions to improve linkage to HIV care in the era of ‘Treat All’ in sub-Saharan Africa: a systematic review. Curr HIV/AIDS Rep 2019; 16:292–303. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provides a robust overview of linkage strategies and areas for further research under UTT policies in sub-Saharan Africa.
- 4.Treat all: policy adoption and implementation status in countries. Geneva, Switzerland: World Health Organization; 2018. [Google Scholar]
- 5.Mendez-Lopez A, McKee M, Stuckler D, et al. Population uptake and effectiveness of test-and-treat antiretroviral therapy guidelines for preventing the global spread of HIV: an ecological cross-national analysis. HIV Med 2019; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6▪.Perriat D, Balzer L, Hayes R, et al. Universal Test and Treat Trials Consortium (UT3C). Comparative assessment of five trials of universal HIV testing and treatment in sub-Saharan Africa. J Int AIDS Soc 2018; 21:e25048. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provides insight and comparison of five population level studies of test and treat in sub-Saharan Africa. It provided valuable comparisons of successes and barriers between the trials.
- 7.Herce ME, Chi BH, Liao RC, Hoffmann CJ. Re-thinking linkage to care in the era of universal test and treat: insights from implementation and behavioral science for achieving the second 90. AIDS Behav 2019; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8▪▪.Ayieko J, Petersen ML, Charlebois ED, et al. A patient-centered multicomponent strategy for accelerated linkage to care following community-wide HIV testing in rural Uganda and Kenya. J Acquir Immune Defic Syndr 2019; 80:414–422. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this study, the authors provide a robust demonstration of a patient-centered strategy for improving linkage to care after population level testing by directly addressing barriers to care from community-based testing.
- 9.Yotebieng M, Brazier E, Addison D, et al. Research priorities to inform ‘Treat All’ policy implementation for people living with HIV in sub-Saharan Africa: a consensus statement from the International epidemiology Databases to Evaluate AIDS (Ie DEA). J Int AIDS Soc 2019; 22:e25218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen MS, Chen YQ, McCauley M, et al. HPTN 052 Study Team. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365:493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robertson MM, Braunstein SL, Hoover DR, et al. Timeliness of human immunodeficiency virus diagnosis and antiretroviral treatment initiation in the era of universal testing and treatment. J Infect Dis 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 12.Eisinger RW, Dieffenbach CW, Fauci AS. HIV viral load and transmissibility of HIV infection: undetectable equals untransmittable. JAMA 2019; 321:451–452. [DOI] [PubMed] [Google Scholar]
- 13.Li Z, Purcell DW, Sansom SL, et al. Vital signs: HIV transmission along the continuum of care — United States, 2016. MMWR Morb Mortal Wkly Rep 2019; 68:267–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bassett I, Regan S, Luthuli P, et al. Linkage to care following community-based mobile HIV testing compared with clinic-based testing in Umlazi Township, Durban, South Africa: mobile HIV testing in South Africa. HIV Med 2014; 15:367–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma M, Ying R, Tarr G, Barnabas R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in sub-Saharan Africa. Nature 2015; 528:S77–S85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maughan-Brown B, Kuo C, Galárraga O, et al. Stumbling blocks at the clinic: experiences of seeking HIV treatment and care in South Africa. AIDS Behav 2018; 22:765–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee MJ, Venturelli S, McKenna W, et al. Reasons for delayed antiretroviral therapy (ART) initiation in the era of early ART initiation guidelines: a retrospective service evaluation. Int J STD AIDS 2019; 30:415–418. [DOI] [PubMed] [Google Scholar]
- 18.Kuhns LM, Hotton AL, Perloff J, et al. Evaluation of Translife care: an intervention to address social determinants of engagement in HIV care among transgender women of color. AIDS Behav 2019; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 19.Tun W, Apicella L, Casalini C, et al. Community-based antiretroviral therapy (ART) delivery for female sex workers in Tanzania: 6-month ART initiation and adherence. AIDS Behav 2019; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halperin J, Conner K, Butler I, et al. A care continuum of immediate ART for newly diagnosed patients and patients presenting later to care at a federally qualified health center in New Orleans. Open Forum Infect Dis 2019; 6:ofz161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gardner LI, Metsch LR, Anderson-Mahoney P, et al. Antiretroviral Treatment and Access Study Study Group. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS Lond Engl 2005; 19:423–431. [DOI] [PubMed] [Google Scholar]
- 22▪.Samet JH, Blokhina E, Cheng DM, et al. A strengths-based case management intervention to link HIV-positive PWID in Russia to HIV care – results from a randomized controlled trial. AIDS 2019; 33:1467–1476. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study not only highlights the importance of developing linkage strategies that transcend the barriers of addiction care but also aim to increase the durability of linkage and retention.
- 23▪▪.Solomon SS, Solomon S, McFall AM, et al. Indian National Collaboration on AIDS Study. Integrated HIV testing, prevention, and treatment intervention for key populations in India: a cluster-randomised trial. Lancet HIV 2019; 6:e283–e296. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provides data on care centers designed to address the specific needs of key populations in India, which experience a disproportionate level of stigma and face additional barriers to care.
- 24.Schwartz SR, Bassett J, Mutunga L, et al. HIV incidence, pregnancy, and implementation outcomes from the Sakh’umndeni safer conception project in South Africa: a prospective cohort study. Lancet HIV 2019; 6:e438–e446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seeley J, Bond V, Yang B, et al. HPTN 071 (PopART) study team. Understanding the Time Needed to Link to Care and Start ART in Seven HPTN 071 (PopART) Study Communities in Zambia and South Africa. AIDS Behav 2019; 23:929–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Plazy M, Farouki KE, Iwuji C, et al. Anrs 12249 Tasp Study Group. Access to HIV care in the context of universal test and treat: challenges within the ANRS 12249 TasP cluster-randomized trial in rural South Africa. J Int AIDS Soc 2016; 19:20913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.MacKellar D, Williams D, Bhembe B, et al. Peer-delivered linkage case management and same-day ART initiation for men and young persons with HIV infection — Eswatini, 2015–2017. MMWR Morb Mortal Wkly Rep 2018; 67:663–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Labhardt ND, Ringera I, Lejone TI, et al. Effect of offering same-day ART vs usual health facility referral during home-based HIV testing on linkage to care and viral suppression among adults with HIV in Lesotho: The CASCADE Randomized Clinical Trial. JAMA 2018; 319:1103–1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Neuman M, Taegtmeyer M, Hatzold K, et al. Challenges in measurement of linkage following HIV self-testing: examples from the STAR project. J Int AIDS Soc 2019; 22 Suppl 1:e25238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ingold H, Mwerinde O, Ross AL, et al. The Self-Testing AfRica (STAR) Initiative: accelerating global access and scale-up of HIV self-testing. J Int AIDS Soc 2019; 22 Suppl 1:e25249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.d’Elbée M, Indravudh PP, Mwenge L, et al. Preferences for linkage to HIV care services following a reactive self-test: discrete choice experiments in Malawi and Zambia. AIDS 2018; 32:2043–2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32▪▪.Choko AT, Corbett EL, Stallard N, et al. HIV self-testing alone or with additional interventions, including financial incentives, and linkage to care or prevention among male partners of antenatal care clinic attendees in Malawi: an adaptive multiarm, multistage cluster randomised trial. PLoS Med 2019; 16:e1002719. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this novel trial, participants were randomized to varying arms of HIV self-testing and coupled incentive interventions. This study demonstrated that incentives and appointment reminders are useful in linking partners of ANC attendees to care.
- 33.Indravudh PP. Increasing knowledge of HIV status and demand for ART using community- based HIV self-testing: a cluster randomised trial in rural Malawi. Poster presented at Conference on Retrovirals and Opportunistic Infections; 2018 July. [Google Scholar]
- 34.Jubilee M, Park FJ, Chipango K, et al. HIV index testing to improve HIV positivity rate and linkage to care and treatment of sexual partners, adolescents and children of PLHIV in Lesotho. PLOS ONE 2019; 14:e0212762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tafuma TA, Mahachi N, Dziwa C, et al. Time taken to link newly identified HIV positive clients to care following a home-base index case HIV testing: experience from two provinces in Zimbabwe. PLoS One 2018; 13:e0201018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pence BW, Mills JC, Bengtson AM, et al. Association of increased chronicity of depression with HIV appointment attendance, treatment failure, and mortality among HIV-infected adults in the United States. JAMA Psychiatry 2018; 75:379–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Remien RH, Stirratt MJ, Nguyen N, et al. Mental health and HIV/AIDS: the need for an integrated response. AIDS 2019; 33:1411–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hallett TB, Eaton JW. A side door into care cascade for HIV-infected patients? J Acquir Immune Defic Syndr 2013; 63 Suppl 2:S228–S232. [DOI] [PubMed] [Google Scholar]


