Supplemental Digital Content is available in the text.
Keywords: patient-centered, post intensive care syndrome, readmissions, resource utilization
Objectives:
Increasingly, patients admitted to an ICU survive to hospital discharge; many with ongoing medical needs. The full impact of an ICU admission on an individual’s resource utilization and survivorship trajectory in the United States is not clear. We sought to compare healthcare utilization among ICU survivors in each year surrounding an ICU admission.
Design:
Retrospective cohort of patients admitted to an ICU during one calendar year (2012) in a multipayer healthcare system. We assessed mortality, hospital readmissions (categorized by ambulatory care sensitive conditions and emergency department), and outpatient visits. We compared the proportion of patients with visits during the pre-ICU year versus the post-ICU year.
Patients:
People admitted to an Intermountain healthcare ICU for greater than 48 hours in the year 2012
Interventions:
None.
Measurements and Main Results:
Among 4,074 ICU survivors, 45% had increased resource utilization. Readmission rates at 30-day, 90-day, and 1-year were 15%, 26%, and 43%. The proportion of patients with a hospital admission increased significantly in the post-ICU period (43% vs 29%; p < 0.001). Of patients with a readmission in the post-ICU period, 24% were ambulatory care sensitive condition. Patients with increased utilization differed by socioeconomic status, insurance type, and severity of illness. Sixteen percent of patients had either an emergency department or inpatient admission, but no outpatient visits during the post-ICU period.
Conclusions:
An ICU admission is associated with increased resource utilization including hospital readmissions, with many due to an ambulatory care sensitive condition. Lower socioeconomic status and higher severity of illness are associated with increased resource utilization. After an ICU visit patients seem to use hospital resources over outpatient resources. Interventions to improve and coordinate care after ICU discharge are needed.
In the United States, individuals with serious medical conditions, whether chronic or terminal, make up a small fraction of the total population but account for a substantial majority of healthcare resource utilization (1, 2). Patients suffering from acute life-threatening illness have increased vulnerability to poor outcomes and high resource utilization (3–7). Multiple stakeholders have thus turned attention to methods to prevent hospital readmissions and reduce resource utilization (8–14). Development of potential interventions requires greater understanding of the burden and patterns of resource utilization among ICU survivors across an array of healthcare systems.
Every year, more Americans survive an ICU admission (12, 13); often with new or worsening disease, physical morbidities, and ongoing healthcare needs (6, 15, 16). The first years following hospital discharge are especially costly for ICU survivor families (15, 17–22). Among survivors of sepsis, an ICU stay is associated with increased hospital readmission and higher healthcare utilization compared with sepsis survivors without an ICU admission (14, 23, 24). The window between ICU discharge to 1 year is a time where preventative interventions have the potential to improve patient-centered outcomes (10).
Although population studies have begun to answer whether utilization patterns after an ICU admission are a result of pre-ICU wellness or of new disease burden (25–28), descriptions of how an ICU admission impacts an individual’s resource utilization in the United States are less granular (29, 30). An analysis of changes in individual utilization patterns and trajectories is important to develop interventions to improve patient-centered outcomes after ICU admission. We compared healthcare resource utilization before and after an ICU admission to help determine how an ICU admission alters healthcare resource utilization patterns in a United States mixed payer population.
As part of an effort to build an ICU aftercare and recovery infrastructure within Intermountain Healthcare (IHC), we sought to describe healthcare resource utilization within the IHC system among ICU survivors.
MATERIALS AND METHODS
Study Population
We retrospectively identified patients admitted to 17 ICUs at IHC hospitals during calendar year 2012. Intermountain is an integrated healthcare system operating 23 hospitals and 185 clinics in Utah and Idaho. The first ICU admission of 2012 was used as the index admission. We defined the post-ICU period as the 12 months after initial discharge. We defined the pre-ICU period as 13 months to 1 month before the index ICU admission to exclude deterioration leading to ICU admission.
We restricted our patient population to adult Utah residents who receive their medical care within the IHC system, on the basis of having been seen as an outpatient, inpatient, in an emergency department (ED), or affiliated acute care facility within the 3 years prior to the index ICU admission. Individuals with one visit or less during the 3-year period were excluded from the cohort.
We excluded all patients without insurance (i.e., self-pay), those who died during index admission and those who were transitioned to inpatient hospice or inpatient psychiatric services. To exclude patients using the ICU for observation for less severe illness, we excluded patients with an index ICU stay less than 48 hours. We further excluded those receiving solid organ transplant or cardiac mechanical support.
Classification of Healthcare Visits
We abstracted all inpatient, ED, outpatient, physical therapy (PT), occupational therapy (OT), and cognitive therapy visits. Cognitive therapy, PT, and OT visits were categorized separately from other outpatient visits. PT and OT visits on the same day were counted as a single visit. Similarly, we collapsed multiple visits on the same day to providers with the same specialty into a single visit. We prioritized and collapsed inpatient, ED, and outpatient visits on the same day as follows: A visit for a patient seen in the ED and admitted to the hospital on the same day was counted only as a hospital admission. Alternatively, if a patient had an outpatient visit and an ED visit on the same day, we counted both the outpatient visit and the ED visit. Similarly, if a patient was seen at an outpatient visit and admitted to the hospital, we counted both visits.
A new utilizer was defined as a patient who did not have a visit in the pre-ICU period but did in the post-ICU period. This was done for all visits, as well as ED, outpatient, and inpatient visits separately. When determining whether a patient was a new utilizer, for each type of visit we excluded patients who never had the type of visit.
Statistical Analysis
Demographics and cohort patient characteristics are presented as n (%), mean (sd), or median (interquartile range [IQR]). Our primary analysis was a comparison of the proportion of patients with at least one visit during the pre-ICU versus the post-ICU period using McNemar’s test to account for the paired nature of the data. We stratified patients by ICU admission for sepsis using a previously validated claims-based definition of severe sepsis/septic shock to identify sepsis-related admissions (31, 32). Rates of relevant outcomes (1-yr mortality, 90-d readmission, and 90-d ED visits) were compared for septic and nonseptic patients. We further report the number of patients with post-ICU hospital readmissions classified as ambulatory care sensitive conditions (ACSCs) according to primary diagnostic code for the hospital readmission (14, 33). We also present the number of visits independent of patient (i.e., a patient can have multiple visits) overall and for each visit type in the pre-ICU and post-ICU periods.
In a secondary analysis of patients alive at 1-year post-ICU discharge, we assessed which clinical variables were associated with increased utilization in a series of univariate analyses using t tests, chi-square tests, or Wilcoxon rank-sum tests as appropriate. We classified patients as increased utilizers if they experienced 1) An increase in inpatient hospital admissions of one or more from the pre-ICU to the post-ICU period or 2) New ED use or increase in ED use of at least two visits in the post-ICU period as compared with the pre-ICU period. We compared the following variables between patients with increased utilization and patients without: age, sex, insurance provider, admission Acute Physiology and Chronic Health Evaluation II score, admission Sequential Organ Failure Assessment score, mechanical ventilation, history of heart failure (9), sepsis, ICU length of stay (LOS), discharge disposition, socioeconomic status (SES) (as measured by the area deprivation index) (34, 35), and comorbid condition as measured by Charlson and Elixhauser indices (36, 37). In a sensitivity analysis, we included patients who died in the year after discharge as increased utilizers to account for mortality bias.
For enhanced detail, we performed exploratory descriptive analyses. First, we described the occurrence of specialty visits (outpatient PT, OT, or cognitive therapy and mental health visits) for the overall cohort, as well as for patients who might be at high risk for requiring such visits, defined as patients undergoing mechanical ventilation and spending at least 5 days in the ICU (17), Second, we describe the proportion of patients with opiate prescriptions in the pre- and post-ICU periods for the cohort. Third, we compared readmissions and increased utilization (by our definition) in patients with heart failure and those without because patients with heart failure have been identified as a high priority vulnerable population that benefits from intensive and tailored outpatient services (9).
The IHC privacy board and institutional review board (number 1051037) approved publication of these results, the standard method for ethical oversight for publication of operational/quality improvement efforts.
RESULTS
Demographics of Overall Cohort
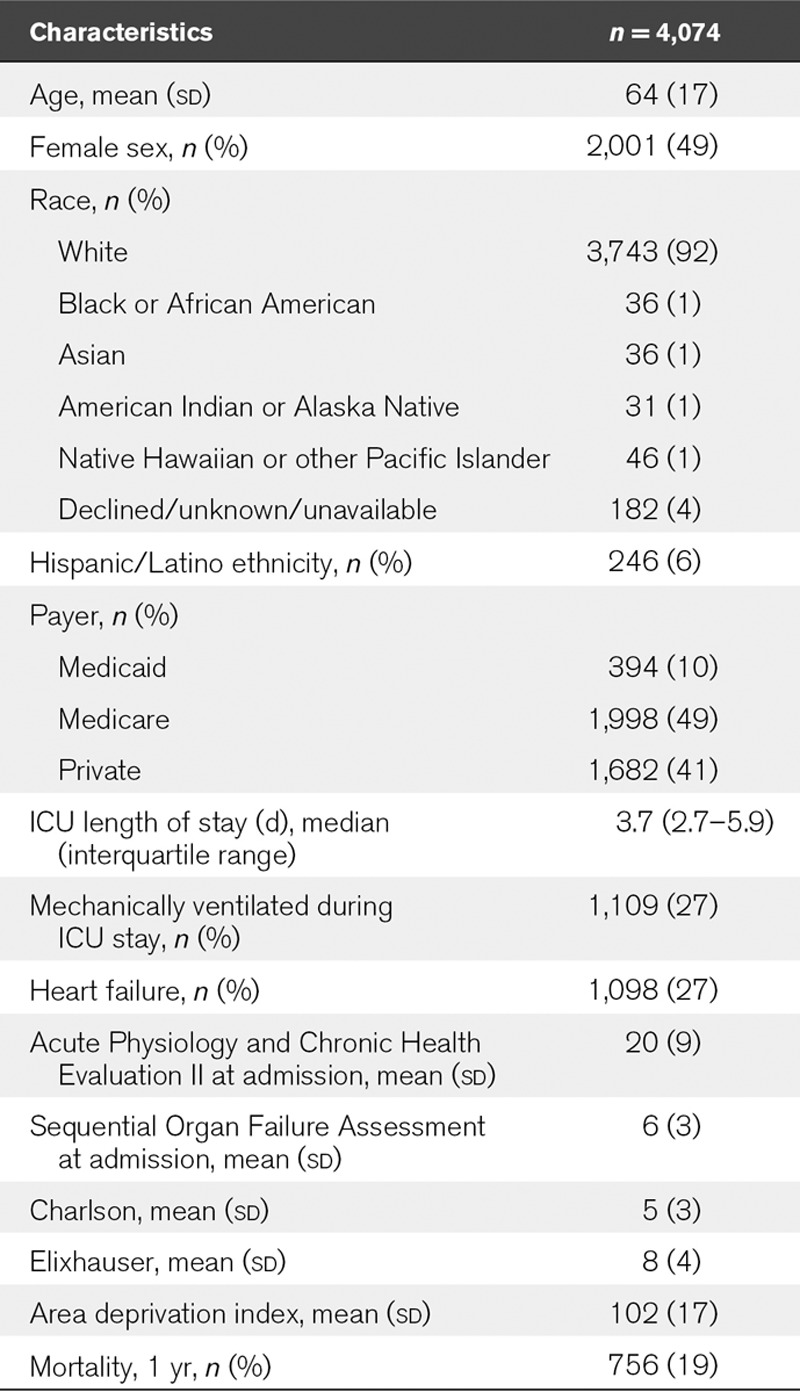
We identified 4,074 distinct patients in the overall cohort (Fig. 1); 39% 1,583 were admitted for severe sepsis or septic shock. Forty-nine percent of the cohort was female. Forty-one percent had private insurance, 10% had Medicaid, and 49% had Medicare. Median ICU LOS was 3.7 days (IQR, 2.7–5.9 d) with 27% requiring mechanical ventilation at some point during the ICU admission (Table 1). The median (IQR) for the area deprivation index by insurance status was Medicaid 110 (103–117), Medicare 106 (95–113), and private insurance 104 (94–111) (p < 0.001) (data no shown).
Figure 1.
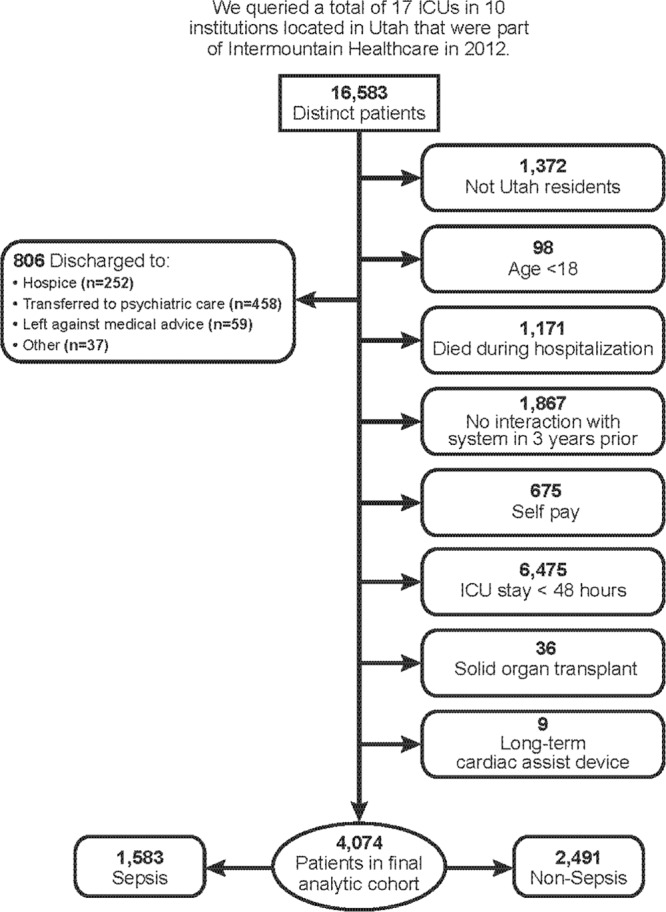
Consort diagram.
TABLE 1.
Cohort Demographics
Mortality and Readmissions.
Overall, 30-day, 90-day, and 1-year mortality rates were 4%, 9%, and 19%. Readmission rates for the cohort at 30-day, 90-day, and 1-year were 15%, 26%, and 43%. Septic patients had significantly higher mortality at all time points (p < 0.001) and higher readmission rates at 90 days (29% vs 23%; p < 0.001) and 1-year (48% vs 40%; p < 0.001), with similar readmission rates at 30 days (16% vs 14%; p = 0.07) compared with nonseptic patients (Table 2).
TABLE 2.
Mortality, Readmissions, and Emergency Department Visits Stratified by Sepsis
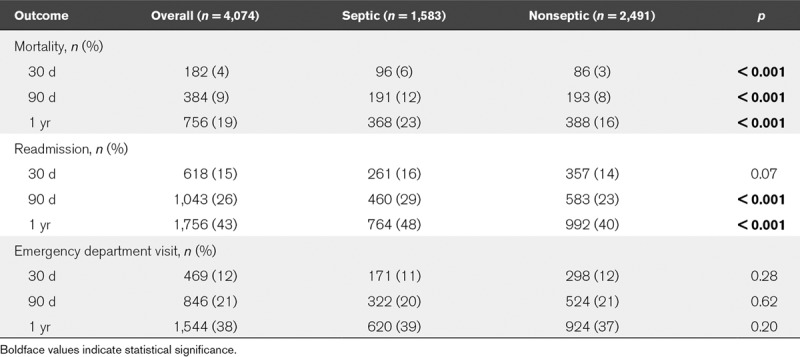
Forty-three percent (1,756) of ICU survivors experienced at least one inpatient readmission within 1 year of their index ICU hospitalization. Twenty-four percent of patients with a readmission had one categorized as a preventable admission (ACSC’s) based on the Agency for Healthcare Research Quality definitions (Supplement Table 1, Supplemental Digital Content 1, http://links.lww.com/CCM/E889). The top five ACSC’s diagnoses were congestive heart failure (8%), pneumonia (6%), complicated diabetes (3%), urinary tract infection (3%), and chronic obstructive pulmonary disease (2%).
Overall Visits and Patient Utilization.
Figure 2 depicts the number of all visits in the pre- and post-ICU periods overall and broken down by visit type. Hospital admissions increased by 60% in the post-ICU period compared with the pre-ICU period, whereas ED and outpatient visits increased by 8% and 33%, respectively, in the post-ICU period (Fig. 2).The median number of total visits in the pre-ICU period was 3 visits (IQR, 1–7), which increased to four visits (IQR, 1–9) in the post-ICU period (p < 0.001).
Figure 2.

Comparison of all types of visits in the pre- and post-ICU period. ED = emergency department.
The proportion of patients with an inpatient admission increased from 29% in the pre-ICU year to 43% in the post-ICU year (p < 0.001) (Supplement Table 2, Supplemental Digital Content 2, http://links.lww.com/CCM/E890). The increase between the pre- and post-ICU year was larger for patients admitted for sepsis (32% vs 48%; p < 0.001) than those admitted to the ICU for other diagnoses (27% vs 40%; p < 0.001).
Utilization Patterns.
There were 650 patients (16%) in the cohort who were new healthcare utilizers in that they did not have a hospital admission, ED visit, or outpatient visit in the pre-ICU period but did have at least one in the post-ICU period. Among patients who ever had a hospital admission, 47% had a hospital admission only in the post-ICU year (new inpatient utilizer). Similarly, 38% of patients with ED visits and 21% of patients with outpatient visits were new ED and new outpatient utilizers, respectively, in the post-ICU year. Of the 3,318 patients who survived to 1-year post-ICU discharge, only 472 (14%) had no visits during the post-ICU period.
Sixteen percent of the cohort (n = 639) had an ED visit or an inpatient visit in the post-ICU year without any outpatient visits in the post-ICU year. Broken down by insurance type, 22% of Medicaid, 16% of Medicare, and 13% of privately insured patients had an ED visit or a hospital admission in the post-ICU period but did not have an outpatient visit in the post-ICU year.
Increased Utilization (Secondary Analysis)
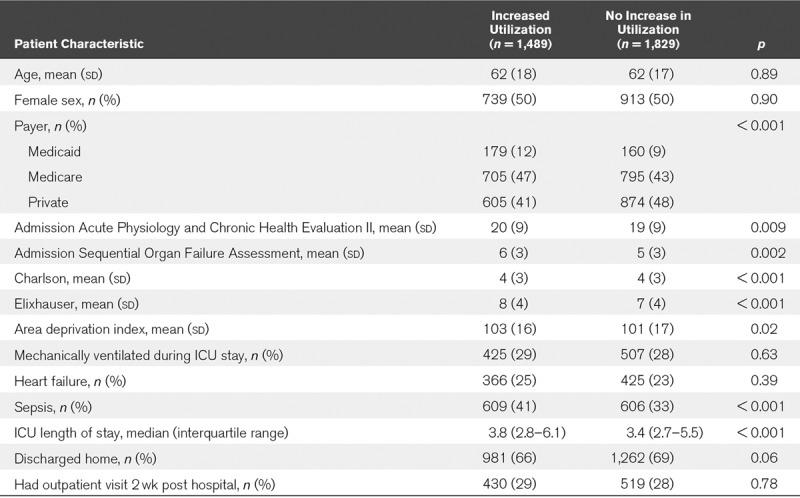
Among the 3,318 patients who survived to 1-year post-ICU discharge, 1,489 (45%) were increased utilizers according to our definition. There were significant differences in SES, payer status, severity of illness scores, and ICU LOS between increased utilizers and patients with no increase in utilization (Table 3). Neither mechanical ventilation nor having an outpatient visit 2 weeks post hospital discharge was associated with increased utilization. In a sensitivity analysis where the definition of increased utilization included patients who died within 1 year of ICU discharge, age, diagnosis of heart failure, and discharge to home were also associated with increased utilization (data not shown).
TABLE 3.
Characteristics Associated With Increased Resource Utilization Among Patients Who Survived to 1-Year Post-ICU Discharge (n = 3,318)
Exploratory Descriptive Analyses
Utilization of PT/OT, Cognitive Therapy, and Mental Health Visits.
Only 305 (8%) of all ICU survivors (primary cohort) received new support from PT/OT or cognitive/mental health clinicians in the post-ICU period. Eighty-eight percent of cognitive and 100% of psychiatric referrals were new in the post-ICU study period. Among the 617 patients who were in the ICU greater than or equal to 5 days and underwent mechanical ventilation, only 30 (5%) had a PT/OT, cognitive, or mental health visit within 90 days after ICU discharge.
Opiate Prescriptions.
A significant increase in the proportion of patients with opioid prescriptions occurred in the post-ICU period (33% in the post-ICU period vs 28% in the pre-ICU period; p < 0.001) and 17% of the cohort had new orders for opioid medication in the post-ICU period.
Patients With Heart Failure.
Among the 1,256 patients admitted to our referral center ICUs, 335 (27%) had heart failure. Patients without heart failure met our definition of increased utilizer significantly more often (24% vs 15%; p = 0.006) than patients with heart failure. However, patients with heart failure had significantly higher 30-day (21% vs 15%; p = 0.01) and 90-day (30% vs 23%; p = 0.01) readmissions compared with those without heart failure (Supplement Table 3, Supplemental Digital Content 3, http://links.lww.com/CCM/E891). A summary of all analyses and denominators is presented for easy reference in Supplement Table 4 (Supplemental Digital Content 4, http://links.lww.com/CCM/E892).
DISCUSSION
In this study of a large integrated health system in the United States, 1-year, 90-day, and 30-day hospital readmission rates were high. Almost half of patients were readmitted during the year after hospital discharge. One quarter of ICU survivors had a potentially preventable readmission within the first year. The top five ACSC’s readmission diagnoses were congestive heart failure (8%), pneumonia (6%), complicated diabetes (3%), urinary tract infection (3%), and chronic obstructive pulmonary disease (2%). Forty-five percent of ICU survivors had increased healthcare resource utilization after hospital discharge, and 16% of survivors newly began utilizing health services. Lower SES, type of insurance, higher severity of illness, and longer hospital LOS were all associated with an increase in resource utilization after hospital discharge.
This study compares general post-ICU patient’s resource utilization to pre-ICU use among a patient population that includes those with private insurance. The fact that insurance status was associated with increased resource utilization emphasizes the importance of studying patients beyond the Medicare/Medicaid population. Our study adds to the growing data on resource utilization worldwide (27–29, 38, 39) and in the United States (23, 29, 30, 40, 41). Hospital readmission rates among our cohort admitted to the ICU for sepsis are consistent with prior work (14, 23, 24). We observed that patient characteristics like severity of illness, and payer status are associated with increased utilization and extend prior work (23, 24). However, neither mechanical ventilation nor patient age were associated with increased resource utilization. The proportion of patients admitted with potentially preventable readmissions is similar to that observed in a Medicare population (14).
Our data suggest that needs and vulnerability extend across SES. Interestingly, of the non-Medicaid/Medicare (‘private payers”) patients, 13% had an ED visit or an inpatient admission and no outpatient visit in the post ICU period, while in the Medicaid population that the same percent was higher at 22%. Patients with private insurance represent a higher SES (when measured using area deprivation index), and we suspect they have easier access to outpatient services, while patients with Medicaid or no insurance represent a lower SES. Further, the lack of access to established care contributes to ED visits and hospital admissions in the post-ICU Medicaid group and in patients without insurance, but a better clarification of this pattern will require further research particularly in the uninsured. The higher than expected ED and inpatient visit use without outpatient use in the higher SES group suggests that individual factors, especially psychologic and emotional factors, play an important role in use of follow-up resources and healthcare utilization.
Patients in our cohort used costly ED and inpatient resources more than outpatient services such as PT/OT cognitive or mental health visits in the post-ICU period. This observed pattern may derive from clinician lack of awareness of the availability of such services or of relevant patient disability, or from organizational failures in the outpatient follow-up of ICU survivors. The need for specific outpatient care services designed for the post-ICU population is underscored in our data by the lack of association between an outpatient visit within 2 weeks of hospital discharge and increased resource utilization, suggesting that specific ICU aftercare and recovery activities may be needed to provide relevant and timely services to ICU survivors (2, 42, 43). The low prevalence of outpatient therapy stands in marked contrast to the high prevalence of relevant disabilities among most ICU survivors (3, 6, 44–47). Herridge et al (18) report that increased healthcare resource utilization continues up to 5 years post-ICU and is an important legacy of patients with acute respiratory distress syndrome (ARDS) admitted to the ICU for greater than 7 days.
ICU survivors often struggle to regain their pre-hospital way of life and to adjust to a new state of physical needs (11, 26, 43). The increase in opiate prescription use noted in our data are evidence of a new post-ICU circumstance similar to ICU survivors in the United Kingdom and Scotland who often report chronic pain (16, 22). Given the current opiate epidemic in the United States, our data identifies ICU survivors as a population to target for other pain control interventions. Thus, strategies and interventions designed to optimize healthcare utilization while maintaining adequate support for ICU survivors is an imperative (48, 49).
Weinberger et al (50) showed outpatient follow-up of ICU patients was able to reduce readmissions and in hospital-based costs. Ruhl et al (20, 21) demonstrated that better physical and quality of life status after an ICU admission were associated with fewer readmissions and reductions in costs in ARDS survivors. Similarly, patients with heart failure have better quality of life and fewer ED visits with a rigorous transition to home care outpatient intervention (51). Our data indicates resource utilization between heart failure patients and ICU patients is similar; it follows that a focused transition post-ICU care clinic with support and coordination services modeled after heart failure clinics may optimize outpatient resources and reduce emergency visits. An outpatient continuum of care for ICU patients including family members may enhance appropriate follow-up resource use (52, 53).
This study has several limitations. It is a retrospective investigation. We did not compare resource utilization with a matched non-ICU control group, rather we used the patient healthcare utilization prior to the ICU admission to control for comorbid conditions unrelated to the ICU admission. Due to the large sample size, statistically significant differences in characteristics like severity of illness may not represent clinically meaningful differences. We were unable to identify patients who resided in a long-term healthcare facility prior to the index ICU admission, and therefore, we were not able to include healthcare facility utilization in this study. Our utilization data are likely an underestimation of true healthcare resource utilization for ICU patients. Our population is 92% Caucasian which may limit the generalizability of our data. We defined preventable hospital readmission using AHRQ standard ACSC criteria, and we do not know if they truly represent preventable admissions. Finally, the competing risk of mortality may be a source of bias; however, a sensitivity analysis that included patients who died in the definition of increased utilizer demonstrated robust findings.
CONCLUSIONS
Almost half of all ICU survivors within a mixed payer system have increased healthcare resource utilization. An ICU admission alters an individual’s healthcare utilization patterns including increased hospital readmissions and ED visits. Patient factors including lower SES and higher severity of illness are associated with increased resource utilization. A post-ICU aftercare and recovery clinic designed to specifically address these needs may provide personalized medical therapy and anticipatory guidance thereby reducing healthcare resource utilization.
Supplementary Material
Footnotes
See also p. 1652.
Drs. Hirshberg, Hopkins, and Brown and Ms. Wilson conceptualized the article. Drs. Hirshberg, Kuttler, and Brown, Ms. Wilson, and Ms. Stanfield acquired the data. Drs. Hirshberg, Majercik, Beesley, Orme, and Brown and Ms. Wilson analyzed the data. Drs. Hirshberg, Majercik, Beesley, Orme, Hopkins, and Brown wrote the article. All authors approved the final copy and revise the article for important intellectual content.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Supported, in part, by grant from the departmental funds.
Dr. Hopkins’ institution received funding from Intermountain Research and Medical Foundation to study outcomes of family caregivers of ICU patients. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Agboola S, Golas S, Fischer N, et al. Healthcare utilization in older patients using personal emergency response systems: An analysis of electronic health records and medical alert data: Brief description: A longitudinal retrospective analyses of healthcare utilization rates in older patients using personal emergency response systems from 2011 to 2015. BMC Health Serv Res 2017; 17:282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hewner S, Wu YW, Castner J. Comparative effectiveness of risk-stratified care management in reducing readmissions in medicaid adults with chronic disease. J Healthc Qual 2016; 38:3–16 [DOI] [PubMed] [Google Scholar]
- 3.Unroe M, Kahn JM, Carson SS, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: A cohort study. Ann Intern Med 2010; 153:167–175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wunsch H. Weighing the costs and benefits of a sedative. JAMA 2012; 307:1195–1197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wunsch H, Angus DC. The puzzle of long-term morbidity after critical illness. Crit Care 2010; 14:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wunsch H, Guerra C, Barnato AE, et al. Three-year outcomes for Medicare beneficiaries who survive intensive care. JAMA 2010; 303:849–856 [DOI] [PubMed] [Google Scholar]
- 7.Elliott D, Davidson JE, Harvey MA, et al. Exploring the scope of post-intensive care syndrome therapy and care: Engagement of non-critical care providers and survivors in a second stakeholders meeting. Crit Care Med 2014; 42:2518–2526 [DOI] [PubMed] [Google Scholar]
- 8.Hacker K, Santos P, Thompson D, et al. Early experience of a safety net provider reorganizing into an accountable care organization. J Health Polit Policy Law 2014; 39:901–917 [DOI] [PubMed] [Google Scholar]
- 9.Mechanic R. Post-acute care–the next frontier for controlling Medicare spending. N Engl J Med 2014; 370:692–694 [DOI] [PubMed] [Google Scholar]
- 10.Kahn JM, Angus DC. Health policy and future planning for survivors of critical illness. Curr Opin Crit Care 2007; 13:514–518 [DOI] [PubMed] [Google Scholar]
- 11.Kahn JM, Kramer AA, Rubenfeld GD. Transferring critically ill patients out of hospital improves the standardized mortality ratio: A simulation study. Chest 2007; 131:68–75 [DOI] [PubMed] [Google Scholar]
- 12.Kahn JM, Le T, Angus DC, et al. ; ProVent Study Group Investigators: The epidemiology of chronic critical illness in the United States*. Crit Care Med 2015; 43:282–287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zimmerman JE, Kramer AA, Knaus WA. Changes in hospital mortality for United States intensive care unit admissions from 1988 to 2012. Critl Care 2013; 17:R81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prescott HC, Langa KM, Iwashyna TJ. Readmission diagnoses after hospitalization for severe sepsis and other acute medical conditions. JAMA 2015; 313:1055–1057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheung AM, Tansey CM, Tomlinson G, et al. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med 2006; 174:538–544 [DOI] [PubMed] [Google Scholar]
- 16.Griffiths J, Hatch RA, Bishop J, et al. An exploration of social and economic outcome and associated health-related quality of life after critical illness in general intensive care unit survivors: A 12-month follow-up study. Crit Care 2013; 17:R100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Herridge MS, Cheung AM, Tansey CM, et al. ; Canadian Critical Care Trials Group: One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 2003; 348:683–693 [DOI] [PubMed] [Google Scholar]
- 18.Herridge MS, Tansey CM, Matté A, et al. ; Canadian Critical Care Trials Group: Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med 2011; 364:1293–1304 [DOI] [PubMed] [Google Scholar]
- 19.Needham DM, Dowdy DW, Mendez-Tellez PA, et al. Studying outcomes of intensive care unit survivors: Measuring exposures and outcomes. Intensive Care Med 2005; 31:1153–1160 [DOI] [PubMed] [Google Scholar]
- 20.Ruhl AP, Huang M, Colantuoni E, et al. Healthcare resource use and costs in long-term survivors of acute respiratory distress syndrome: A 5-year longitudinal cohort study. Crit Care Med 2017; 45:196–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruhl AP, Lord RK, Panek JA, et al. Health care resource use and costs of two-year survivors of acute lung injury. An observational cohort study. Ann Am Thorac Soc 2015; 12:392–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McPeake J, Devine H, MacTavish P, et al. Caregiver strain following critical care discharge: An exploratory evaluation. J Crit Care 2016; 35:180–184 [DOI] [PubMed] [Google Scholar]
- 23.Liu V, Lei X, Prescott HC, et al. Hospital readmission and healthcare utilization following sepsis in community settings. J Hosp Med 2014; 9:502–507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prescott HC, Langa KM, Liu V, et al. Increased 1-year healthcare use in survivors of severe sepsis. Am J Respir Crit Care Med 2014; 190:62–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iwashyna TJ. Survivorship will be the defining challenge of critical care in the 21st century. Ann Intern Med 2010; 153:204–205 [DOI] [PubMed] [Google Scholar]
- 26.Iwashyna TJ. Trajectories of recovery and dysfunction after acute illness, with implications for clinical trial design. Am J Respir Crit Care Med 2012; 186:302–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garland A, Olafson K, Ramsey CD, et al. Distinct determinants of long-term and short-term survival in critical illness. Intensive Care Med 2014; 40:1097–1105 [DOI] [PubMed] [Google Scholar]
- 28.Szakmany T, Walters AM, Pugh R, et al. Risk factors for 1-year mortality and hospital utilization patterns in critical care survivors: A retrospective, observational, population-based data linkage study. Crit Care Med 2019; 47:15–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lone NI, Gillies MA, Haddow C, et al. Five-year mortality and hospital costs associated with surviving intensive care. Am J Respir Crit Care Med 2016; 194:198–208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hua M, Gong MN, Brady J, et al. Early and late unplanned rehospitalizations for survivors of critical illness*. Crit Care Med 2015; 43:430–438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001; 29:1303–1310 [DOI] [PubMed] [Google Scholar]
- 32.Iwashyna TJ, Odden A, Rohde J, et al. Identifying patients with severe sepsis using administrative claims: Patient-level validation of the Angus implementation of the international consensus conference definition of severe sepsis. Medl Care 2014; 52:e39–e43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agency for Healthcare Quality and Researc: Quality indicator empirical methods, 2019. Available at: https://www.qualityindicators.ahrq.gov/Modules/all_resources.aspx; https://www.qualityindicators.ahrq.gov/Downloads/Resources/Publications/2015/Empirical_Methods_2015.pdf
- 34.Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health 2003; 93:1137–1143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Knighton AJ, Savitz L, Belnap T, et al. Introduction of an area deprivation index measuring patient socioeconomic status in an integrated health system: Implications for population health. EGEMS (Wash DC) 2016; 4:1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 1987; 40:373–383 [DOI] [PubMed] [Google Scholar]
- 37.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 1992; 45:613–619 [DOI] [PubMed] [Google Scholar]
- 38.Welch CA, Harrison DA, Hutchings A, et al. The association between deprivation and hospital mortality for admissions to critical care units in England. J Crit Care 2010; 25:382–390 [DOI] [PubMed] [Google Scholar]
- 39.Garland EL. Disrupting the downward spiral of chronic pain and opioid addiction with mindfulness-oriented recovery enhancement: A review of clinical outcomes and neurocognitive targets. J Pain Palliat Care Pharmacother 2014; 28:122–129 [DOI] [PubMed] [Google Scholar]
- 40.Kramer AA, Higgins TL, Zimmerman JE. Intensive care unit readmissions in U.S. hospitals: Patient characteristics, risk factors, and outcomes. Crit Care Med 2012; 40:3–10 [DOI] [PubMed] [Google Scholar]
- 41.Hill AD, Fowler RA, Pinto R, et al. Long-term outcomes and healthcare utilization following critical illness–a population-based study. Crit Care 2016; 20:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Czerwonka AI, Herridge MS, Chan L, et al. Changing support needs of survivors of complex critical illness and their family caregivers across the care continuum: A qualitative pilot study of towards RECOVER. J Crit Care 2015; 30:242–249 [DOI] [PubMed] [Google Scholar]
- 43.McPeake J, Shaw M, Iwashyna TJ, et al. Intensive care syndrome: Promoting Independence and Return to Employment (InS:PIRE). Early evaluation of a complex intervention. PLoS One 2017; 12:e0188028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Griffiths J, Fortune G, Barber V, et al. The prevalence of post traumatic stress disorder in survivors of ICU treatment: A systematic review. Intensive Care Med 2007; 33:1506–1518 [DOI] [PubMed] [Google Scholar]
- 45.Hennessy D, Juzwishin K, Yergens D, et al. Outcomes of elderly survivors of intensive care: A review of the literature. Chest 2005; 127:1764–1774 [DOI] [PubMed] [Google Scholar]
- 46.Sacanella E, Pérez-Castejón JM, Nicolás JM, et al. Functional status and quality of life 12 months after discharge from a medical ICU in healthy elderly patients: A prospective observational study. Crit Care 2011; 15:R105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jackson JC, Hart RP, Gordon SM, et al. Post-traumatic stress disorder and post-traumatic stress symptoms following critical illness in medical intensive care unit patients: Assessing the magnitude of the problem. Crit Care 2007; 11:R27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mehlhorn J, Freytag A, Schmidt K, et al. Rehabilitation interventions for postintensive care syndrome: A systematic review. Crit Care Med 2014; 42:1263–1271 [DOI] [PubMed] [Google Scholar]
- 49.Ball C, Kirkby M, Williams S. Effect of the critical care outreach team on patient survival to discharge from hospital and readmission to critical care: Non-randomised population based study. BMJ 2003; 327:1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Weinberger M, Smith DM, Katz BP, et al. The cost-effectiveness of intensive postdischarge care. A randomized trial. Med Care 1988; 26:1092–1102 [DOI] [PubMed] [Google Scholar]
- 51.Harrison MB, Browne GB, Roberts J, et al. Quality of life of individuals with heart failure: A randomized trial of the effectiveness of two models of hospital-to-home transition. Med Care 2002; 40:271–282 [DOI] [PubMed] [Google Scholar]
- 52.Foster EM. Does the continuum of care improve the timing of follow-up services? J Am Acad Child Adolesc Psychiatry 1998; 37:805–814 [DOI] [PubMed] [Google Scholar]
- 53.Daly BJ, Douglas SL, Kelley CG, et al. Trial of a disease management program to reduce hospital readmissions of the chronically critically ill. Chest 2005; 128:507–517 [DOI] [PubMed] [Google Scholar]


