Abstract
Introduction: This systematic review assessed the impact of race/ethnicity, education, and income on transgender individual's lifetime experience of suicidal thoughts and behaviors (SITB) in gray and published literature (1997–2017).
Methods: Sixty four research projects (108 articles) were identified in WorldCat, PubMed, and Google Scholar. Articles were included if they were published in Canada or the United States, included original quantifiable data on transgender SITBs, and had ≥5 participants, at least 51% of whom were ≥18 years.
Results: Across all projects suicide ideation averaged 46.55% and attempts averaged 27.19%. The majority of participants were Caucasian, whereas the highest rate of suicide attempts (55.31%) was among First Nations, who accounted for <1.5% of participants. Caucasians, by contrast, had the lowest attempt rate (36.80%). More participants obtained a bachelor's degree and fewer an associate or technical degree than any other level of education. Suicide attempts were highest among those with ≤some high school (50.70%) and lowest among those with an advanced degree (30.25%). More participants made an income of $20–$50,000/year and less $10–$20,000 than any other income bracket.
Conclusion: SITBs, among the transgender population, are both universally high and impacted by race/ethnicity, educational attainment, and income. These findings may be useful in creating culturally and factually informed interventions for transgender individuals experiencing SITBs and in informing future research on this topic.
Keywords: gender identity, health disparities, mental health, minority stress, suicide, transgender/transsexual
Introduction
Transgender people—whose gender identity is incongruent with the sex assigned to them at birth—are increasingly publicly visible.1 Despite, or perhaps because of this, they are extremely vulnerable to discrimination, violence, and marginalization, the experience of which has extremely negative impacts on their health and well-being.2 Shockingly high rates of suicidal thoughts and behaviors (SITBs), previously identified as averaging 55% for ideation and 29% for attempts over the lifetime, are a clear indication of these negative impacts.3 What relationship do race/ethnicity, educational attainment, and income have with SITBs among transgender adults? We address this question through a systematic review of 21 years of peer-reviewed and gray literature on the topic and, in doing so, update and provide an added analysis to the lead author's previous publication on the matter.3 To do so, we used data on transgender participants from 64 distinct research projectsi published in 108 articles between 1997 and 2017 (Table 1).4–110
Table 1.
Studies in This Meta-Synthesis
| No. | Author/s | # | Ideation | Attempt | Description |
|---|---|---|---|---|---|
| 1 | Cole et al.4 | 435 | Ever: 14.48% | Analyzed incidence of Axis 1 or 2 diagnoses through retrospective chart review of self-diagnosed transsexuals who presented to Texas gender clinic since 1980. Charts included information from 1 to 2 h clinical interviews, biographical and medical questionnaires and, in some cases, psychometric inventories. The previous publication on this dataset3 reported the time period as “before treatment.” This was changed to “ever” as no patients had GRS at data collection and, in any case, none attempted after GRS. The attempt rate was also changed from 15% to 14.48% to maintain consistency in reporting findings to two decimal places wherever possible | |
| 2 | Devor5,6 | 45 | Ever: 28.89% | Ever: 22.22% | Investigated life experiences of FTM individuals using qualitative interviews conducted from 1998 to 2002. Suicidality information volunteered during the interview. This is the first needs assessment conducted on the topic of transgender health |
| 3 | Rehman et al.7 | 28 | After surgery: 7.14% | Explored post-GRS sex and surgery satisfaction among MTF patients of a New York City Hospital that received GRS from 1980 to 1994, using a mail-in questionnaire and, in some cases, interviews. Only information on the postsurgical period is reported, although it was noted that there was a marked decrease in attempts postsurgery | |
| 4 | Mathy8 | 73a | Ever: 37% | Ever: 23.30% | Examined transgender suicidality among respondents to two human sexuality surveys on MSNBC website over 1 month (2000). First was selected random sample and second invited every thousandth. Given choice between male, female, and transgender, 0.2% of each sample selected the latter and were psychosocially matched to cis male and cis female controls and lesbian and gay comparison groups |
| 5 | Singer et al.,9 Kenagy10,11 | 103 | Ever: 38.83% | Needs assessment that explored physical and mental health among Philadelphia-area transgender individuals for approximately a year (1996–1997) | |
| 6 | Kenagy and Bostwick12 | 111 | Ever: 62.16% | Ever: 26.12% | Community-based needs assessment that explored health and social service needs of Chicago transgender individuals recruited over 6 months (2000–2001). Replicated Singer et al.9 and Kenagy.10,15 Suicidality findings here amend those published in Adams et al.3 to correct for small rounding error |
| 7 | Bockting, et al.,13,14 | 181 | Past 3 years: 52% | Analyzed the impact of a Minnesotan sexual health seminar on LGBT health-risk factors by following a cohort through an intervention using a case–control element to compare transgender and cis gender respondents. All participants in the 8 seminars conducted from 1997 to 2002 were asked to complete a survey pre and postintervention and after 3 months | |
| 8 | Kenagy10,11,15 | 81 | Ever: 46.91% | Ever: 19.75% | Needs assessment that investigated health and social service needs of a Philadelphia-area transgender community using data collected over 6 months (1997) |
| 9 | Risser et al.16 | 67a | Ever: 58.21%, past 30 days: 16.42% | Ever: 29.85% | Community-based needs assessment that investigated the sexual health risks and social and sexual health status of a group of transgender women in Houston over 2 months (2002–2003) |
| 10 | Xavier,17 Xavier and Simmons,18 Xavier et al.19 | 252a | Ever: 34.92% | Ever: 16.27% | Community-based needs assessment that investigated the health and social service needs of transgender people in Washington, DC recruited over 4 months (1999–2000) |
| 11 | Clements et al.,20 Clements-Nolle et al.,21,22 | 515 | Ever: 32.23% | Examined HIV, risk behaviors, mental health, and health care use of transgender individuals in San Francisco over 5 months in 1997 | |
| 12 | Zians23 | 136 | Past year: 31.62% | Ever: 17.65% | Community-based needs assessment of the health care and social service needs of transgender individuals in San Diego conducted over 7 months in 2004 |
| 13 | Taylor24,25 | 73a | Ever: 54% | Ever: 28% | Community-based needs assessment conducted over 6 months in 2006 on transgender Manitoban and Northwestern Ontarian health and social service needs. As two-spirit encompasses Aboriginal LGB and/or transgender individuals there may be a small number of non-transgender respondents in the dataset. Participants given a choice of long or short-form questionnaire and survey party held for aboriginals |
| 14 | Landers and Gilsanz26 | 52 | Past year: 30.77% | Survey conducted for the Massachusetts Department of Public Health over 10 days in 2009 using respondents from MassEquality's e-mail list to explore the impact of the State's equal marriage law on LGBT health and security. Perhaps because of a short data collection period, the response rate was 4.2%. Transgender respondents were also forced to select either LGB or transgender and thus likely under sampled | |
| 15 | McDuffie and Brown27 | 70 | Ever: 48.57% | Ever: 8.57% | Chart review of US Veterans examined for “gender identity disturbances” by second author at Tennessee VA office from 1987 to 2007. Study likely has great deal of participant overlap with Blosnich et al.,41 Brown et al.,65 and Bukowski et al.110 In contrast with Adams et al.3 the denominator used in our analysis includes those with missing ideation data. |
| 16 | Nuttbrock et al.28 | 571 | Ever: 53.50% | Ever: 27.90% | Explored psychiatric impact of gender-related abuse across New York transwomen's life course via 2004–2009 longitudinal study. Data gathered from psychometric inventories and interviews using the Life Review of Transgender Experiences (LRTE) to obtain responses for 5 time periods (early/late adolescence, early adult/young adult, early middle age). Figures used here are for the total population's lifetime suicidality |
| 17 | Maguen and Shipherd,29 Shipherd et al.30 | 153 | Ever: 17.65% | Investigated suicidality among participants at a transgender conference in New England known to focus on ‘cross-dressers’ using a questionnaire completed at the conference. Unlike Adams et al.3 our analysis includes all respondents, regardless as to whether they answered suicidality questions | |
| 18 | Effrig et al.,31 Hayes et al.32 | 108 | Ever: 48.15% | Ever: 25% | Investigated victimization and psychological distress among transgender college students using clinical and nonclinical samples. Clinical sample comprised college counseling center patients where ‘other’ not a gender option. Nonclinical sample consisted of respondents to survey conducted by colleges aligned with counseling centers. Both used the same survey measure, but institutions varied in incentives and completion prompts. Effrig et al.31 contains contradictory figures for number and suicidality of nonclinical and clinical participants. We rationalized them to reveal a probable 108 participants in both samples. In a previous article,3 a different rate of suicidality was arrived at, because of the use of only participants that answered suicidality questions |
| 19 | Meier et al.33 | 431 | Ever: 42.69% | Investigated gender confirming hormonal treatment on FTM individuals over 3 months (2008) using primarily US respondents. Suicidality findings were calculated to be accurate to 2 decimal points and therefore differ from Adams et al.3 | |
| 20 | House et al.34 | 164 | Ever: 34.80% | Explored social and psychological experiences of sexual minorities via internet survey of LGBT respondents conducted over 1 month (2004). 14.6% of respondents were transgender and this group was compared to LGB respondents. | |
| 21 | Beemyn and Rankin,35 Testa et al.36 | 3087 | First felt transgender: 16.62% | Explored transgender individuals' life experiences with an online survey conducted over 3 months (2005–2006). Investigated if respondents felt suicidal when they first realized they were transgender and if it was negatively correlated with exposure to positive representations of transgender individuals | |
| 22 | Heinz and MacFarlane37 | 54 | Ever: 35.19% | Ever: 27.78% | Explored health and social service needs of transgender people on Vancouver Island by survey from 2010 to 2011 |
| 23 | Brown et al.38,39 | 9 | Ever: 55.56% | Ever: 11.11% | Investigated life experiences of transfeminine individuals in the Missouri-Kansas City area by semistructured qualitative interviews conducted over an unspecified time period. Suicidality information was spontaneously shared and always in the context of being pretransition |
| 24 | Moody and Smith40 | 133a | Ever: 65.41%; past year: 74.44% | Ever: 26.32% | Explored suicidality and resilience among transgender Canadians (majority from Quebec and Ontario) through online survey that used verified psychometric inventories |
| 25 | Blosnich et al.41 | 1326 | 2011: 5.13% | Tracked suicidality among transgender veterans with ICD-9 code indicating transgender-related diagnosis through analysis of US VA EHRs. Records searched from 2000 to 2011, although “suicide related-behaviors” or “events” only available for 2009–2011. Overlapping data were provided for each of these years and 2011 is reported here. a lot of overlap with McDuffie et al.,27 Brown et al.,65 and Bukowski et al.,110 although the way they collected and reported patient data differ | |
| 26 | Grant et al.,42,43 Haas et al.44 | 6456 | Ever: 39.92% | Community needs assessment that examined health and social service needs of the transgender population of the US from 2008 to 2009 using a survey conducted primarily online, as well as at survey parties to increase participation of hard to find populations. These figures were calculated using an n of 6456, which represents all study participants, in contract with Adams et al.3 | |
| 27 | Mereish et al.45 | 16 | Ever: 68.75% | Ever: 31.25% | Explored LGBT victimization, substance use, and suicidality among individuals at New England community health center with large LGBT practice. All patients asked to complete a 25-question survey while waiting for physical or mental health appointment over 2 years (2001–2003). Respondents identified gender as male, female, or transgender (1.10% identified as “transgender” and “sexual minority”) |
| 28 | Reisner et al. 201446 | 31 | Ever: 58.06% | Ever: 29.03% | Massachusetts community health center research on transgender health disparities using data from patient questionnaires completed before medical appointment during 1 year (2001–2002). Transgender mutually exclusive to male or female and paired with cis gender controls, matched for age (within 3 years), ethnicity, education, and income. Possible crossover with Reisner et al.;47 Reisner et al.;66 and Beckwith et al.109 |
| 29 | Reisner et al.47 | 23 | Ever: 21.74% | Boston community health center study that examined suicidality in a cohort of FTM patients screened for STDs from July to December 2007. Data obtained through a retrospective chart review and past suicide attempts documented in the EHR. Likely some crossover with Reisner et al.66 | |
| 30 | Wilson et al.,48 Santos et al.,49 de Haan et al.50 | 314 | Ever: 53.18% | Investigated access to physical, mental health and transition-related health care among transgender women in San Francisco. The data was obtained from a behavioral survey conducted via a handheld computer over 4 months in 2010. | |
| 31 | Rosser et al.,51 Perez-Brumer et al.52 | 1229 | Ever: 28.89%; past year: 4.15% | Reports on the social demographics of hidden sexual minorities and transgender-specific individual and structural suicidality risk factors by a sample recruited through an internet-based assessment of US transgender adults. The suicidality figures reported here are slightly different from Adams et al.,3 as raw participant figures were previously calculated as fractions | |
| 32 | Scanlon et al.,53 Rotondi et al.,54,55 Bauer et al.,56, 57 Scheim and Bauer,58 Bauer et al.59 | 433 | Ever: 77%; past year: 36% | Ever: 43%; past year: 10% | Trans Pulse was a community needs assessment of Ontario transgender health and social service needs conducted from 2009 to 2010 using respondent-driven sampling and data gathered by survey completed online or in person |
| 33 | Edelman et al.60 | 521 | Ever: 60% | Ever: 34%; past year: 10% | Needs assessment conducted from May 2012 to 2013 that investigated transgender residents of the Washington, DC Metro Area and update of previous study conducted in 2000 (Xavier).17 The survey questionnaire was self-administered in most cases |
| 34 | Mustanksi et al.,61 Liu and Mustanski,62 Mustanski and Liu,63 Birkett et al.64 | 21 | Ever: 52.40%; past year: 19.00% | Explored LGBT youth suicidality (33.3% <18 years), 8.86% of whom identified as MTF or FTM which, because of small size, were collapsed into a single sample. Respondents completed self-report measures and structured and administered psychiatric interviews at initial contact and after 12 months. Data were collected from 2007 to 2011. | |
| 35 | Brown and Jones65 | 5135 | Ever: 19.36% | Reports health disparities in transgender veterans who received VA health care from 1996 to 2013 and whose sex marker changed after enrolment. Suicidality determined through diagnostic code in patient file and transgender and non-transgender veterans compared 1–3. Overlap with McDuffie et al.,27 Blosnich et al.,41 and Bukowski et al.,110 although they differ in data collection and reporting. | |
| 36 | Reisner et al.66 | 180 | Ever: 31.11% | Ever: 17.22% | Assessed mental health among transgender youth (mean age 19.7), seen at Boston-area community health center from 2002 to 2011 using EHRs. Transgender respondents (FTM and MTF) matched to cis gender controls within 3 months of being noted as transgender in file and by gender identity, age, and race/ethnicity. Data used included patient registration, behavioral intake, case notes, and suicidality according to patient self-report. Possible crossover with Reisner et al.;47 Reisner et al.;46 and Beckwith et al.109 |
| 37 | Olson et al., 2015,67 Olson68 | 96 | Ever: 51.04% | Ever: 30.21% | Investigated physiological and psychological health among transgender youth (age 12–24, mean 19.2) who presented for gender services at Los Angeles children's hospital (Feb 2011–June 2013). Psychosocial health assessed with computer-assisted self-administered survey and psychometric items and physiologic health from patient files |
| 38 | Kuper69 | 1956 | Ever: 95.50%; past year: 80.20% | Ever:: 32.30%; Past year: 10.40% | Reported on suicidality and gender development among gender nonconforming youth and young adults from across the United States through an online survey. These findings are slightly different from Adams et al.3 because of an error in transcription |
| 39 | Weir70 | 5 | Ever: 40% | Ever: 20% | Examined impact of violence on trans people and their supports using participants from Alberta and Saskatchewan recruited through online snowball sampling online. Data obtained from administered questionnaires and semistructured interviews. Suicidality data appear to have arisen during interviews |
| 40 | Tebbe and Moradi71 | 335a | Past year: 71.90% | Ever: 28.10% | Compared US transgender and cis gender college students stress coping strategies using data from national intercollegiate study that distributed surveys to random selection of over 100,000 college students at 73 different institutions in Spring 2011. Transgender cohort consisted of those who identified as neither male nor female. Three participants appeared to be intersex |
| 41 | Lehavot et al.72 | 212 | Ever: 54.72%; past year: 56.60% | Ever: 32.08% | Examined the life experiences of US transgender veterans recruited online through an anonymous online survey (Feb–May 2014) |
| 42 | Grossman et al.73 | 129 | Ever: 40.31% | Ever: 22.48% | Explored suicidality among transgender and gender nonconforming youth from three US cities (Nov 2011–Oct 2012) using snowball sampling and an administered survey. Suicidality data obtained through components of Interpersonal Needs Questionnaire |
| 43 | Reisner et al.,74 Katz-Wise et al.75 | 452 | Ever: 32.74% | Investigated change in attraction and social determinants of mental health in Massachusetts transgender adults from August to December 2013 using an online survey | |
| 44 | Lytle et al.76 | 174 | Past year: 31.03% | Past year: 17.82% | Explored transgender college students self-violence and depression with data from US National College Health Assessment survey (Fall 2008–Spring 2009) |
| 45 | Dowshen et al.77 | 66 | Past year: 15.60% | Past year: 7.80% | Investigated behavioral risk factors and health status of HIV-positive youth using a sample of adolescents and young adults from select US cities. Data were gathered using “computer-assisted self-interviews” from December 2009 to June 2012 |
| 46 | James et al.78 | 27,715 | Ever: 82%; past year: 48% | Ever: 40%; past year: 7% | Compared US transgender and cis gender college students stress coping strategies using data from national intercollegiate study that distributed surveys to random selection of >100,000 college students at 73 different institutions in Spring 2011. Transgender cohort consisted of those who identified as neither male nor female |
| 47 | Nemoto et al.,79 Operario and Nemoto,80 Nemoto et al.,81Glynn et al.82 | 573 | Ever: 54.97% | Ever: 33.33% | Study undertaken over 8 months (2000–2001) and from 2004 to 2006 that recruited primarily San Franciscan transgender women of color (African American, Latina, Asian/Pacific Islander) with histories of sex work. The research focused on the HIV impact, socioeconomic status, victimization, and physical and mental health |
| 48 | Xavier et al.,83 Goldblum et al.,84 Testa et al.,85 Barboza et al.86 | 350 | Ever: 63.71% | Ever: 25.43% | Explored the health and service needs of transgender Virginians through online and paper questionnaires administered over 10 months (2005–2006) |
| 49 | Trujillo et al.87 | 78 | Ever: 38.46% | Reported on beneficial effects of social support on transgender mental health using data obtained from a US national online survey (Feb 2013–April 2014) | |
| 50 | Brown et al.88 | 11 | Ever: 18.18% | An extension of an earlier study completed by the lead author (Brown et al.38.39 this publication reports on Mid-Western trans masculine individuals. Suicidality information was garnered from the semistructured interviews | |
| 51 | Fredriksen-Goldsen et al.,89 Fredriksen-Goldsen et al.,90 Hoy-Ellis et al.91 | 174 | Ever: 71.10% | Explored social and psychological experiences of sexual minorities in an internet survey of LGBT respondents over 1 month (2004). The transgender and lesbian, gay, and bisexual respondents were compared | |
| 52 | Irwin et al.,92 Su et al.,93 Brennan et al.94 | 83 | Ever: 73.49% | Ever: 44.58% | Community-based participatory research project arising out of a 2010 analysis of LGBT suicidal ideation and health disparities (11.9% transgender, where options were male, female, and/or transgender) |
| 53 | Kattari et al.,95 Seelman et al.,96 Seelman et al.97 | 417 | Past year: 34.05% | Past year: 9.35% | Examined health disparities among Colorado transgender adults using a self-completed survey conducted over 7 months in 2014 |
| 54 | Veale et al.98,99,100 | 600 | Ever: 55.67%; past year: 51.00% | Ever: 25.50%; past year: 26.17% | Investigated Canadian transgender youths health using a self-administered online survey conducted from Oct 1, 2013 to May 31, 2014. The older youth (19–25) are reported on here |
| 55 | Swanbrow Becker et al.101 | 47 | Ever: 55%; past year: 24% | Ever: 34%; past year: 4.30% | This case–control study reported on the stress coping strategies of US transgender college students in comparison with their cis gender peers. Data were collected from a national intercollegiate study that distributed electronic surveys to a random selection of >100,000 college students at 73 different institutions in the Spring of 2011. The transgender cohort consisted of those who identified as neither male nor female. Suicidality was assessed over the life time and “recently” using single questions |
| 56 | Testa et al.102 | 816a | Ever: 79.20%; past year: 56.10% | Ever: 45.80% | Investigated effects of stress and resilience among transgender and gender nonconforming individuals on mental and physical health using data obtained from Canadian and US adults through online surveys. Seven intersex participants were included in this dataset |
| 57 | Bouris and Hill103 | 28 | Past year: 17.86% | Chicago study compared gender and sexual minority participants to investigate relationship between youth and their mother figure as means of promoting resilience and exploring minority stress. Participants completed interviewer-administered questionnaire between August 2013 and 2014 | |
| 58 | Lytle et al., 2017104 | 18 | Past year: 61.11% | Explored suicidality and help seeking behavior among transgender youth from the Trevor Project's social network using an online questionnaire during August 2012. Individuals who experienced suicidality in past 14 days were excluded | |
| 59 | Gowin et al.105 | 45 | Ever: 55.56% | First attempt to investigate transgender suicidality solely among asylum seekers. Reviewed 2012 US asylum files of Mexican transwomen identified according to stated gender identity or behaviors. Suicidality data garnered from these records | |
| 60 | Redinger106 | 252 | Past year: 11.9% | Recruited transgender Montana High School students to complete a questionnaire on Montana sex education curriculum. Data collected from 2015 to 2016. Respondents were asked to comment on their suicidality in relation to being a high school student. | |
| 61 | Gaither et al.107 | 330 | Ever: 2.12% | Retrospectively reviewed the charts of MTF patients presented for primary GRS to a US high volume surgeon from 2011 to 2015. Patient charts were reviewed pre, intra, and postoperatively for medical morbidities, including a history of suicidality | |
| 62 | Herman et al.108 | 92,000 | Ever: 34% | Ever: 22% | Reports data obtained from telephone interview survey (2015–2016 California Health Interview Survey). Findings extrapolated to statistically valid California-wide estimate of transgender health data |
| 63 | Beckwith et al.109 | 145 | Ever: 13.79% | Investigated relationship between GRS and suicide using EHRs of binary gendered patients from larger randomly selected sample of transgender patients that presented to at least 1 health care visit to a Boston community health center (July 1, 2010 to June 30, 2015). Possible crossover with Reisner et al.46,47,66 | |
| 64 | Bukowski et al.110 | 5072 | Ever: 18.36% | Explores health of transgender veterans who received VA treatment from 1997 to 2014 using data from EHRs where records indicated any of 4 ICD-9 transgender-related diagnostic codes. Suicidality determined from diagnostic code in patient file. Study has quite a bit of overlap with McDuffie et al.,27 Blosnich et al.,41 and Brown et al.,65 although they differ in how they collected and reported on data |
In all cases, the y-axis of each figure represents the proportion of the cohort population. The data sets are organized from left to right, by increasing suicidality figure found by each study.
These studies seem to have included intersex and/or cis gender respondents, without allowing for their suicidality data to be individually assessed.
EHR, electronic health record; FTM, female to male; GRS, gender reassignment surgery, alternatively known as gender affirming surgery; ICD, International Classification of Diseases; MTF, male to female; VA, veterans administration.
Historical trends
As previously noted, the scientific and clinical approach to transgender health has generally evolved from the use of a disease-based model, prevalent from the 1950s to the 1990s,6,111 to the one that uses an identity-based lens.3,112 Under this lens, transgender SITBs can be understood as significantly being influenced by anti-transgender discrimination and minority stress.22,28,53 Within the disease-based lens, however, transgender SITBs are attributed to individualized psychopathology or neurobiology.8,113 The literature on transgender health has, therefore, increasingly moved from viewing transgender people as aberrant and pathological, to affirming gender identity as part of a varied spectrum and, where appropriate, offering supportive interventions. In this context, practitioners provide medical and therapeutic interventions that affirm rather than “correct” an individual's gender identity.114 Nevertheless, the disease-based lens continues to be employed in some cases.112,115
Meta-analyses and systematic reviews
There are 25 meta-analyses and systematic reviews summarizing the literature on transgender SITBs. However, 20 address the issue primarily among youth or children; as secondary or incidental to another issue (e.g., HIV), a single aspect of a larger topic (e.g., transgender health); or among sexual minorities writ large (e.g., LGBT). The five meta-analyses and systematic reviews that primarily assessed SITBs among transgender adults are Marshall et al.,116 Virupaksha et al.,117 McNeil et al.,118 Wolford-Clevenger et al.,119 and Adams et al.3 Two116,118 account for review parameters (exclusion of gray literature) but fail to identify a number of studies and, in one case, count a single data set multiple times. One117 includes gray literature, but only selects articles freely available online and relevant to the review title, without explaining how the latter was systematized. One119 identifies factors (attempts, behavior, and deaths) correlated with transgender SITBs in literature published between 1991 and January 2017 but does not analyze data on SITBs in this literature. One3 presents an earlier stage of this research, which excludes literature published since February 2016 and does not focus on the impact of ethnicity, income, or education on SITBs. Therefore, this systematic review provides a more robust synthesis and analysis of the available data on transgender SITBs.
Methodology
Eligibility criteria
As in the previous publication on this topic,3 studies were included in the systematic review if they took place in Canada or the United States; published in English-language journals, theses, or project/institutional reports between 1997 and 2017; reported original participant research on transgender suicide attempts and/or ideation; and included quantitative data on SITBs among ≥5 participants, at least ≥51% of whom were 18 years or older at the time of participation. In addition, this systematic review incorporated studies on both clinical and nonclinical populations (Table 1). The former typically required participants to have a diagnosis of gender dysphoria120 and/or be receiving transitional health care services (e.g., hormones and surgery). The latter, by contrast, tended to include participants based on self-identification as any of several transgender identities. Articles were excluded if they reported only on suicide deaths or nonsuicidal self-injury, single case reports, or subsumed transgender data into a larger population (e.g., LGBT). Although research published multiple times was only counted once, all reports were assessed for useful data. Nonwritten reports like poster presentations were excluded. The inclusion of gray literature helped to increase the data pool, reduce the impact of publication bias, and incorporate thesis research that may ultimately result in peer-reviewed publications. Note, however, that only 9%, or 14% of all studies, were non-peer reviewed by the end of the review inclusion period. Given the observed tendency for these publications to achieve peer review over time, it can be assumed that the majority will gain this status, particularly the 6 published since 2015.
Data collection
Of the 64 distinct research projects (and 108 articles) that make up this systematic review, 7 originated in Canada and 57 in the United States. Where possible we excluded participants <18 years; however, as data on SITBs was usually presented for the totality of participants, this was not always possible. Of these 64 projects, 55 were peer reviewed, 3 were theses, and 6 were project or institutional reports. We then extracted partial or complete data on transgender participants' race/ethnicity (n=56), education (n=49), and income (n=33). In some cases, we supplemented this through interviews with the study authors, which the first author conducted as part of his MSW thesis. Specifically, the first author interviewed 18 authors of publications on transgender SITBs and, in some cases, minor additional statistical information was reported in these interviews. We have not indicated where this occurred to ensure the confidentiality guaranteed in the initial research ethics board approval from Dalhousie University.121
Literature review
This literature review is the culmination of three sequential reviews: the lead author's thesis,121 an update3 focused on 1997 to February 2016, and the one conducted for this article that focused on 21 years of research on transgender SITBs (1997–2017 inclusive). Literature was identified primarily by keyword searching WorldCat, Google Scholar, and Google Search. WorldCat, as one of the largest catalogs of cross-referenced and multidisciplinary academic literature, was the primary source of material. The following keywords were used: “transgender suicide”; “transsexual suicide”; “FTM suicide”; “MTF suicide”; “transsexual suicidality”; “transgender suicidality”; “transgender suicide attempt”; and “transsexual suicide attempt.” This was supplemented by hand searching the reference lists of identified articles and looking for new publications from previously identified research projects.3,121 The latter were identified by searching named projects (e.g., The Trans PULSE Project)53 and checking the outputs of identified authors on Google Scholar, Google Search, PubMed, LinkedIn, and ResearchGate. We also reviewed Ramsay's collated list of publications on transgender SITBs.122
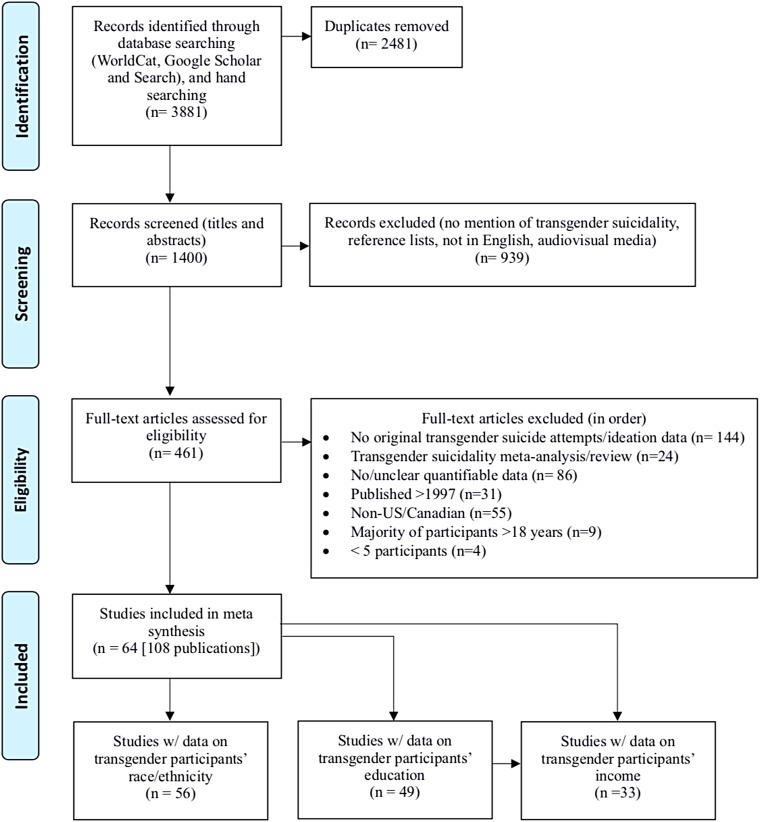
We initially identified 3,881 articles, of which 2,481 duplicates were eliminated (Fig. 1). Upon reviewing titles and abstracts of the remaining 1,400 articles, we excluded a further 939 that failed to mention transgender SITBs, consisted exclusively of reference lists or audiovisual material, or were not in English. The full texts of the remaining 461 were reviewed and the following eliminations made: reported no original data on transgender suicide attempts and/or ideation (n=144), meta-analyses/reviews of transgender SITBs (n=24), no/unclear quantitative data (n=n=86), published before 1997 (31), not from the United States or Canada (n=55), the majority of participants were <18 years (n=9), and had ≤5 participants (n=4). The remaining 108 articles, representing 64 distinct research projects, were included in this systematic review.
FIG. 1.
PRISMA Chart.
Data analysis
We extracted data on suicide attempts, ideation, and demographic details (race/ethnicity [n=56],ii education [n=49],iii and income [n=33]iv) from 64 research projects. Whenever possible we recalculated these data using all study participants as the denominator, rather than only those that answered the given question, positioning nonrespondents as “negative cases' and our findings as conservative. SPSS v. 23 and Microsoft Excel 2016 were used to conduct two analyses. The first examined race/ethnicity, education, and income of transgender participants compared with US Census data. The US Census was used as a baseline because 89% of these projects originated in the US Census and, as a result, most took their demographic categories from it. The second analysis examined lifetime transgender suicide attempt statistics reported according to race/ethnicity and education. Other analyses (income and ideation) of SITBs were excluded for lack of sufficient data.
Of the 56 projects that reported data on race/ethnicity, four (7, 35, 59, 64)v were excluded from further analysis for reporting an amalgamation of ideation and attempts; three (9, 21, 60) for specifying SITBs over a nonstandard time period (e.g., when participants ‘first felt transgender’); six (19, 32, 38, 42, 52, 56) because race/ethnicity data were not collected using mutually exclusive categories, such that the proportions of each racial/ethnic group could not be considered in relation to the study's population size; and five (14, 44–45, 53, 57) for recording SITBs over participant's last year rather than their lifetime. The race/ethnicity data of the remaining 38 projects (n=26 for ideation, n=35 for attempts) was assessed. Our second race/ethnicity analysis began with the 19 projects that analyzed data on SITBs specific to participants' race/ethnicity. Seven of these (20, 36, 43, 48, 52–53, 56) were excluded because data were reported as a statistical analysis or model, one (42) because ethnic-specific data on SITBs were recorded differently than overall demographic data, and one (44) because SITBs were recorded over a fixed period. The ethnic/race-specific SITBs data of the remaining 10 (6, 11, 19, 26, 31–33, 41, 46–47) projects were compared.
Of the 49 projects that reported on participant educational data, eight (1, 2, 6, 14–16, 28, 52) were excluded for doing so in a manner (e.g., Hollingshead average) inconsistent with the majority, seven (3, 7, 44–45, 53, 57, 60) for recording SITBs during a fixed time, one (59) for conflating suicidal ideation and attempts, and one (18) because being a college student was a requirement. The education data of the remaining 32 projects (n=20 ideation, n=29 for attempts) were assessed. Our second educational analysis began with the 10 projects that analyzed SITBs with regard to participants' educational level. We eliminated five (20, 41, 43, 48, 52) that reported on this in a statistical model. The educational data of the remaining five (11, 19, 26, 31, 46) were assessed.
Of the 33 projects that reported on participant income, 16 (1, 2, 7–8, 11, 14, 28, 30, 32, 35, 40, 47–48, 53) were eliminated for doing so in a nonstandard format (e.g., relation to poverty line). The income data of the remaining 17 projects (10 for lifetime ideation and 16 for attempts) were assessed. Important to note, however; only five projects provided comparable income data for ideation and seven for attempts using the same five common income ranges from ≤ $10,000 to ≥ $100,000. Our analysis of income was, as a result, limited.
Results
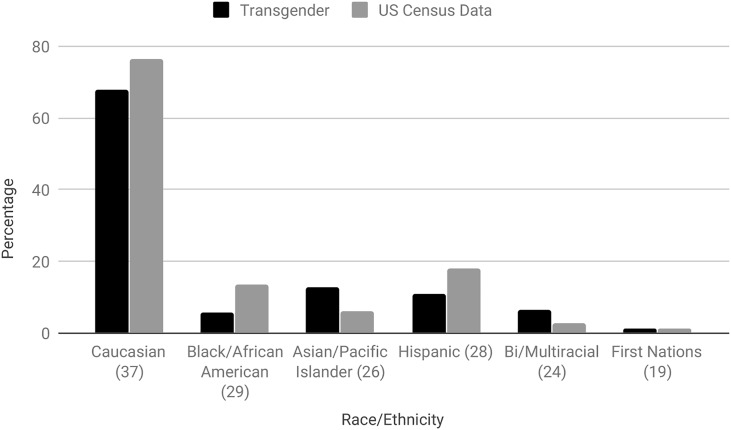
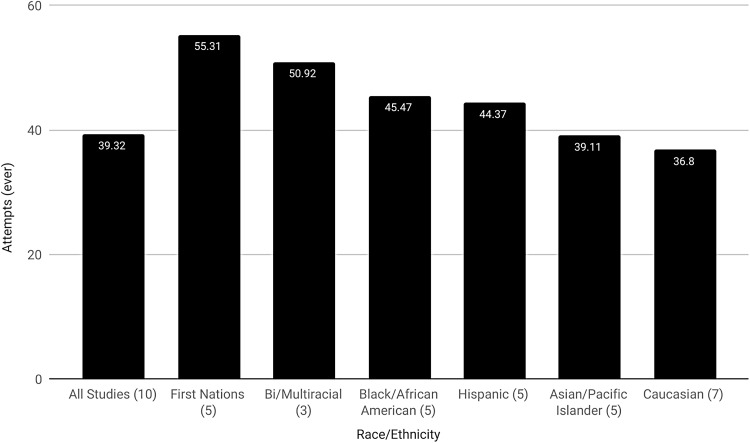
Lifetime suicidal ideation was reported in 34 studies (average=46.55%; range=18.18–95.50%) and attempts in 46 studies (average=27.19%; range=8.57–52.40%). Average lifetime SITBs in the 38 projects that reported comparable data on both suicide and race/ethnicity was 45.44% for ideation (range=18.18–82%) and 27.88% (0–40.00%) for attempts. An average of 67.75% (3.70–96.73%)vi of these participants were Caucasian and 28.05% (0–95.63%) were nonwhite. Participants in 12.78% (0–21.74%) of the projects were Asian/Pacific Islanders; 11.03% (0–43.90%) Hispanics; 6.57% (0–28%) and 5.58% (0–69.43%) Black/African American and biracial/multiracial, respectively; and 1.46% (0–27.40%) First Nations. A final 0.79% (0.15–18.15%) were classified as “other,” whereas the ethnicity of 4.44% (0–68.52%) was unknown. In comparison with US Census data (Fig. 2),123 our findings show fewer Caucasian (67.75% vs. 76.6%), Black/African American (5.58% vs. 13.4%), and Hispanic (11.03% vs. 18.1%), greater Asian/Pacific Islanders (12.78% vs. 6%) and biracial/multiracial (6.57% vs. 2.7%), and roughly equal First Nations participants (1.46% vs. 1.3%). Average lifetime suicide attempts using data on SITBs specific to race/ethnicity (Fig. 3) was 39.32%. First Nations reported the highest rate of lifetime suicide attempts (55.31%), followed by biracial/multiracial individuals (50.92%), Black/African Americans (45.47%), Hispanics (44.37%), Asian/Pacific Islanders (39.11%), and Caucasians (36.80%).
FIG. 2.
Transgender race/ethnicity versus US Census data. Figures in parenthesis specify the number of individual studies used in the calculation of transgender race/ethnicity.
FIG. 3.
Lifetime transgender suicide attempts according to race/ethnicity. Figures in parenthesis specify the number of individual studies used in the calculation of suicide attempts specific to transgender race/ethnicity.
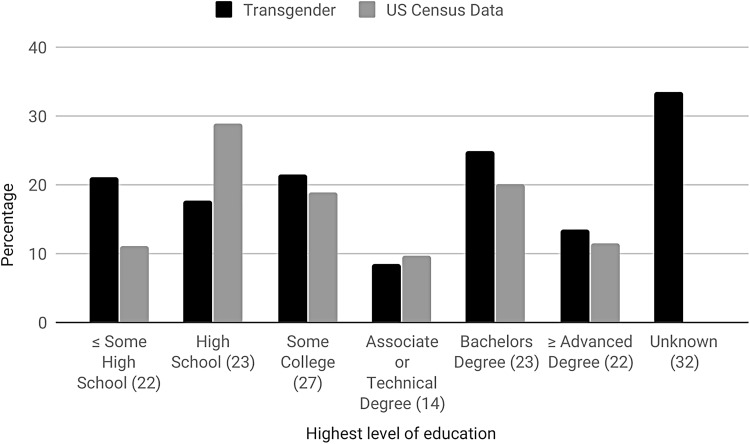
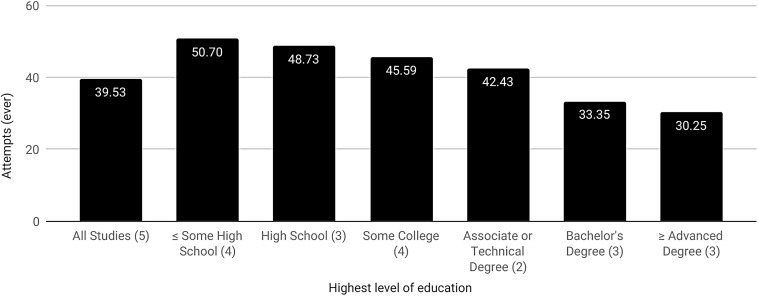
The average rate of lifetime SITBs in the 32 projects that reported comparable data on both suicide and education was 46.26% (18.18–95.50%) for ideation and 27.16% (11.11–43%) for attempts. An average of 24.79% (2.87–36.90%) of participants completed a bachelor's degree, 21.5% (7.32–100%) some college, 21.06% ≤ (0.47–40.08%) some high school, 17.59% (6.40–63.06%) high school, 13.53% (7.32–100%) ≥ an advanced degree,vii and 8.58% (1.15–27.27%) an associate or technical degree. The educational achievement of 33.55% (0–80.80%) of participants was unknown. Compared with the US Census (Fig. 4),124 transgender participants had lower rates of high school (17.59% vs. 28.89%) completion and higher attainment of ≤ some high school (21.06% vs. 11.04%), some college (21.5% vs. 18.86%), a bachelor's degree (24.79% vs. 20.04%), and ≥ an advanced degree (13.53% vs. 11.4%). Associate or technical degree attainment was comparable with the general population (8.58% vs. 9.77%). Average lifetime suicide attempts using SITB data on SITBs specific to education (Fig. 5) was 39.53% and appears to drop with the level of education achieved. Specifically, attempts peak among those that had ≤ some high school (50.7%), followed by completed high school (48.73%), some college (45.59%), an associate or technical degree (42.43%), a bachelor's degree (33.35%), and ≥ an advanced degree (30.25%).
FIG. 4.
Transgender educational attainment versus US Census data. Figures in parenthesis specify the number of individual studies used in the calculation of transgender educational attainment.
FIG. 5.
Lifetime transgender suicide attempts according to educational attainment. Figures in parenthesis specify the number of individual studies used in the calculation of suicide attempts specific to transgender educational attainment.
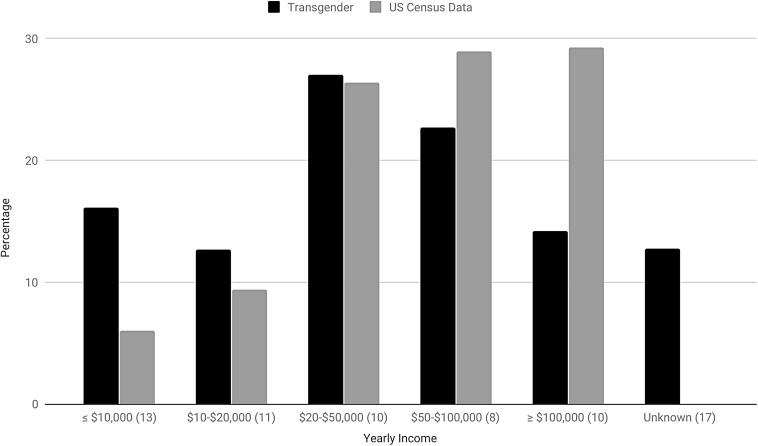
The average rate of SITBs in the 17 projects that reported comparable data on both suicide and income was 80.76% (34.92–82%) for ideation and 39.25% for attempts (16.27–45.80%). About 26.98% (19.96–40.74%) made $20–50,000, 22.72% (8.45–32.53%) made $50–100,000, 16.14% (8.43–60.32%) made ≤$10,000, 14.17% (2.32–15.21%) made ≥$100,000, and 12.67% (11.68–29.63%) made $10–$20,000. The income of 12.78% (0–89.18%) was unknown. Compared with the US Census (Fig. 6),125 transgender participants reported lower overall income. Specifically, more made ≤$10,000 (16.14% vs. 6.05%) and $10–$20,000 (12.67% vs. 9.38%), whereas fewer made $50–$100,000 (22.72% vs. 28.97%) and ≥$100,000 (14.17% vs. 29.25%). The proportion of the transgender and general population making $20–$50,000 was roughly equal (26.98% vs. 26.35%).
FIG. 6.
Transgender yearly income versus US Census data. Figures in parenthesis specify the number of individual studies used in the calculation of transgender income.
Discussion
Findings
The methodological rigor of studies on transgender SITBs continues to increase and, although cross-sectional studies are most common, a small but increasing number utilize the more rigorous case–control design. The amount of research on this topic is also increasing, with 14 projects first published from 1997 to 2007 and the remainder since. In fact, following the authors' previous study on this subject, which included studies published to February 2016,3 22 projects, or 34% of the total, have been added. We can expect this trend, which may partially result from the heightened profile of transgender issues and civil rights, to continue. Similarly, although 49 of the studies included fewer than 500 participants, there has been a trend toward exceptionally high cohorts in more recent studies; for instance, n=1,250,51 n=6,456,43 n=5135,65 n=27,715,78 and n=92,000.108
Our findings of an average rate of 46.55% lifetime suicidal ideation and 27.19% attempts among transgender participants are similar to those found in the authors' previous study (56% ideation, 29% attempts), although obviously lower with regard to ideation.3 The preponderance of evidence suggests that high rates of SITBs, rather than being inherent to transgender individuals, result from barriers to transitional care, stigma, and discrimination.11,44,59,126 In addition, by definition, lifetime experience of SITBs is cumulative and while a person may cease to be actively suicidal they will still have had the experience of being suicidal.
It is difficult to make any strong statements on the recruitment and representation of diverse populations in research on transgender SITBs and the relationship between the racial/ethnic diversity of these projects and that of the general population. It is, however, possible to make some basic observations. Online recruitment, although often unable to incorporate the cultural and situational needs of African American participants,127 is increasingly seen as an ideal way to access hidden populations like the transgender community.128 Employment of key informants and snowball sampling, addressing reluctance to participant in research, and the use of incentives and in person recruitment may help to counter African Americans and other marginalized groups' suspicion of research (p. 3).129
Our observation that relatively low rates of suicide attempts occur among Caucasian participants is inconsistent with previous research demonstrating higher rates in this population (Fig. 3).130 There is, however, variation in the research literature on this point131,132 and evidence exists that capture of Black/African American SITBs, in particular, suffers from data disparities and misclassification.132,133 Indeed, we noted relatively high rates of SITBs among Black/African American participants, a group for which SITBs, where police are involved, are sometimes miscategorized as “suicide by cop.”133,134 This is one potential explanation for the observation that low rates of SITBs among Black/African American is at odds with other findings of negative comparative race-based health outcomes.134 Our findings may suggest that Black/African American transgender individuals are less likely to attempt suicide in a manner that invites misclassification, or possibly that their transgender status itself causes their SITBs to be correctly classified. It should also be noted that we are discussing attempted suicides in which, by definition, the individual has survived and can clarify their intent. However, it should be noted that self-report is not without its limitations, as participants often give different responses to this question depending on the presence of and definition of “attempt” and whether a single question is used.135
Our observation of higher rates of SITBs among First Nations individuals136 is consistent with other findings that attribute this to colonization-based trauma.137,138 Likewise, we observed comparatively low rates among Hispanics and Asian/Pacific-Islanders.132 However, there is evidence that SITBs vary greatly within ethnic categories. Puerto Ricans, for instance, have been noted to experience a greater incidence of SITBs than other Hispanics.132 Nevertheless, there is comparatively little research on SITBs within racial/ethnic groupings and, depending on the study, conflation of existing categories (e.g., Asian Americans and American Indians). Variable racial/ethnic definitions are also a problem.132
Consistent with the rapid increase in biracial/multiracial people in the United States, several studies include information on this population, although few report findings on SITBs specific to them. This is also the case in research on SITBs among nontransgender individuals.139,140 Research that does exist tends to focus on youth which, like our own observations, show heightened attempts among biracial/multiracial compared with monoethnic groups.141 This may result from experiencing racial discrimination from multiple locations and the stress caused by conflict between one`s internal self and external world.142 Nevertheless, the lack of data makes it difficult for us to compare our observations with others and future research into SITBs among biracial/multiracial transgender adults is clearly called for.
Research on transgender individuals' educational attainment is relatively scarce, highly variable, and lacking a clear consensus. As a result, the findings in these projects cannot be presented as typical or generalizable. Comparison of our observations to data from the US Census is made more difficult by variation in the categorization of education within these research projects and with the US Census (Fig. 4). For instance, recent US Census data does not record the category of ‘some high school.’143 Nevertheless, the categorization of US Census educational data more closely mirrors the projects in this systematic review than Canadian Census data,144 and our own observations grossly compare with the general population. This systematic review also suggests that lower rates of SITBs may be associated with higher levels of educational attainment (Fig. 5), which is largely consistent with other findings of fewer SITBs among individuals with at least a college degree and more among those with less.145,146
Many transgender students experience a hostile educational environment that can jeopardize or even disrupt their education. Students so affected may opt out of or be refused access to education because of, for instance, their gender presentation.147,148 Although a number of transgender individuals return to school and achieve advanced education later in life, it can be difficult after early and often traumatic disruption,43 which may explain some findings of low educational achievement.147,149 Given the high number of convenience samples, this may particularly be the case in research that is overrepresented by especially vulnerable participants.148 Addressing gender diversity in education and increasing scholarship on this subject will help to challenge the disparities that prevent transgender people from full educational participation and, given the protective effect of educational achievement, may lead to a reduction in their experience of SITBs.150
The lack of individual project data on transgender SITBs according to income, and a complete absence of research into lifetime income among transgender individuals, limits our ability to comment on the relationship between these factors. It should also be noted that, although this systematic review found a lifetime suicide ideation rate of 80.76%, it also included a single study that had 27,715 participants and high suicidal ideation. We did, however, observe that several studies noted a relationship between transgender SITBs and high rates of poverty or un/underemployment and,43,151 within the literature, transgender individuals were observed to be four times more likely than the general population to make <$10,000/year.44,151 This is consistent with the observations of our systematic review that transgender participants are almost three times more likely to make ≤$10,000 (Fig. 6). Similarly, transgender unemployment, discrimination, and poverty are also strongly associated with workplace discrimination and, in turn, lack of education and self-harm.114 Another key consideration is that poverty curtails a transgender individual's access to medical transition, which is a known protective factor.59 This is especially true in environments, like the United States and some parts of Canada, without transgender-inclusive universal health care.
Implications for future research
The myth that transition leads to SITBs continues to be used to deny transgender health care access and legislative rights, despite a lack of empirical support for this position and repeated research debunking it.3,152–159 A more productive avenue for addressing the phenomenon of transgender SITBs might be to investigate the protective factors inherent in transgender health care,33,160–163 and the negative impacts of denied access.40,57,126 In particular, research is needed on the impact of resiliency, minority stress,164 and culturally protective factors on transgender SITBs. An exploration of syndemic factors, particularly with regard to interrelated issues like racism, poverty, and education, would also be a fruitful avenue for research. For instance, only one study has reported on SITBs among transgender refugees.105 We recommend that researchers explore transgender SITBs among various ethnicities, rather than flattening it into a comparison between whites/Caucasians and people of color, ethnic minorities, or racialized individuals. Methods of gathering these data include asking participants to write in their race/ethnicity, reporting on ethnicity and race separately,124 using census categories, and/or allowing for the selection of multiple ethnicities.165,166 Regardless, the choice should be clearly explained and rationalized in the resulting publications.
We further recommend that, where practical, participants be allowed to write in their actual or estimated income, which will allow comparison across a variety of monetary brackets. Where participants are asked to self-report SITBs, we suggest that a definition be provided of the item being measured and, where possible, multiple questions be asked.135 Finally, the creation of project websites will allow findings to be collected and disseminated from a central location. In revising the literature review from the previous publication,3 these websites were invaluable in helping us identify project updates and data published across multiple studies. Giving the project a unique and distinct name, ideally with an available website URL, and using it in promotion and branding will assist in making them easily locatable (e.g., The Trans PULSE Project53).
Limitations
These findings are preliminary and lack generalizability for several reasons. The included studies rely heavily on self-reported SITBs and individual definition of “attempt” and “ideation” can vary a great deal, particularly when a definition is not provided and only a single question is used.135 Second, because the majority of the 64 projects that make up this systematic review use convenience samples, which do not tend to result in representative or easily replicable data.147 There is also a high degree of heterogeneity between these projects; for instance, the categorization of race/ethnicity, education, and income and the size of cohorts (n=5–92,000 participants), the latter of which obscures the impact of small samples and overemphasizes the representativeness of large ones. Studies 46 (n=27,715) and 62 (n=92,000) have a particularly disproportionate impact on the results presented here.167 Another concern is the small-study effect, whereby small cohort studies of lower methodological rigor report different effects than larger ones.167,168 To some degree, concerns of heterogeneity are mitigated by aggregating these projects into a systematic review, although caution should still be taken in interpreting and applying findings. Indeed, the fact that this is a systematic review is itself limiting, as it is bound to exclude unpublished results because of publication bias,167 although this is also mitigated by our inclusion of gray literature.
In addition, income, educational attainment, and race/ethnicity are also often correlated. For instance, one's race/ethnicity directly impacts their income and access to education.169 It is, therefore, difficult to observe or discuss these factors in isolation of one another and our findings should be interpreted in light of this limitation. We suggest that future research on the subject of transgender SITBs, in relation to race/ethnicity, education, and income, collect discrete data on each of these factors and subject them to statistical tests, like stepwise regression, to determine the impact of each factor alone and together on SITBs.
Participation bias, particularly in mental health research, is also an issue in recruitment and reporting of participants.170 Other research has demonstrated that men and individuals with a substance abuse or dependence history are more likely to participate in research on suicide attempts.171 More broadly, people who have experienced SITBs, or are in greater distress generally, may be more likely to participate in studies on this subject. Likewise, research undertaken on clinical populations, or only those with specific presenting issues, may find higher rates of SITBs than population or community-based samples. This is mitigated somewhat by our inclusion of both clinical and nonclinical samples, the latter of which often used population and community-based recruitment. On the contrary, stigma related to SITBs and/or gender identity may prevent individuals from participating in or accurately reporting on their experiences in research on this subject.
As noted in the lead author's previous study,3 gender identity definitions and terms are in flux,172 differ among individual projects, and documentation of nonbinary genders continues to be limited.173 The way individual projects inquire into SITBs is also a concern. It has, for instance, been noted that yes/no questions like “have you ever attempted suicide” tend to overestimate SITBs by combining self-harming behavior with and without suicidal intent (p. 3).44 There is some evidence that in-person interviewing reduces reports of attempts among adults, although this is an uncommon methodology within research on transgender SITBs, possibly because of cost and privacy concerns.3,174,175
Conclusion
This systematic review supports findings of high, if heterogeneous and widely variant, rates of SITBs among transgender adults in the past 21 years. With regard to transgender individuals, it observes that Caucasians experience lower rates of SITBs than other groups; that high levels of educational achievement seem to protect against SITBs; and that they may be at risk of higher SITBs because of relatively low income. Research on the topic of transgender SITBs would be improved by greater consistency in data collection and improved research methodology.
Acknowledgment
The authors thank Dr. Laura Kuper, Cheri Moody, and Maaya Hitomi for their comments on early versions of this article.
Abbreviations Used
- FTM
female to male
- MTF
male to female
- SITB
suicidal thoughts and behaviors
Author Disclosure Statement
The authors have no conflicts of interest to disclose.
Funding Information
No funding was received for this article.
Cite this article as: Adams NJ, Vincent B (2019) Suicidal thoughts and behaviors among transgender adults in relation to education, ethnicity, and income: a systematic review, Transgender Health 4:1, 226–246, DOI: 10.1089/trgh.2019.0009
Projects were included dependent on their last publication on the data set. Devor5,6 was the only project to occur partially outside of the 20-year window.
The projects not reporting any race/ethnicity data were 1, 3–4, 25, 27, 34, 58, 61.
The projects not reporting any educational attainment data were 4, 21, 25, 27, 34–37, 42, 54, 56, 58, 61, 63–64.
The projects not reporting any income data were: 3–4, 9, 15–18, 21, 23, 25, 27, 29, 34, 36–39, 41–42, 44–45, 49–50, 54–55, 57–61, 64.
All bracketed numbers are taken from Table 1.
Figures for ethnicity/race, education, and income do not add to 100%, because of differences in the manner that projects classified racial/ethnic categories and because they are not always mutually exclusive.
The category of advanced degree consists of at least graduate school or a professional degree.
References
- 1. Gillig TK, Rosenthal EL, Murphy ST, Folb KL. More than a media moment: the influence of televised storylines on viewers' attitudes toward transgender people and policies. Sex Roles. 2017;78:515–527 [Google Scholar]
- 2. McCann E, Brown M. Vulnerability and psychosocial risk factors regarding people who identify as transgender. A Systematic Review of the Research Evidence. Issues Ment Health Nurs. 2018;39:3–15 [DOI] [PubMed] [Google Scholar]
- 3. Adams N, Hitomi M, Moody C. Varied reports of adult transgender suicidality: synthesizing and describing the peer-reviewed and gray literature. Transgend Health. 2017;2:60–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cole CM, O'Boyle MO, Emory LE, Meyer WJ. Comorbidity of gender dysphoria and other major psychiatric diagnoses. Arch Sex Behav. 1997;26:13–26 [DOI] [PubMed] [Google Scholar]
- 5. Devor H. Transsexualism, dissociation, and child abuse: an initial discussion based on nonclinical data. J Psychol Hum Sex. 1994;6:49–72 [Google Scholar]
- 6. Devor H. FTM: Female-to-male Transsexuals in Society. Bloomington, IN: University Press, 1997 [Google Scholar]
- 7. Rehman J, Lazer S, Benet AE, et al. . The reported sex and surgery satisfactions of 28 postoperative male-to-female transsexual patients. Arch Sex Behav. 1999;28:71–89 [DOI] [PubMed] [Google Scholar]
- 8. Mathy RM. Transgender identity and suicidality in a nonclinical sample: sexual orientation, psychiatric history, and compulsive behaviors. J Psychol Hum Sex. 2003;14:47–65 [Google Scholar]
- 9. Singer TB, Cochran M, Adamec R. Final report by the Transgender Health Action Coalition (THAC) to the Philadelphia Foundation Legacy Fund. 1997. Philadelphia, PA: Transgender Health Action Coalition [Google Scholar]
- 10. Kenagy GP. Exploring an oppressed group: a study of the health and social service needs of transgendered people in Philadelphia [Dissertation]. [Philadelphia: ]: University of Pennsylvania; 1998, p. 255 [Google Scholar]
- 11. Kenagy GP. The health and social service needs of transgender people in Philadelphia. Int J Transgend. 2005;8:49–56 [Google Scholar]
- 12. Kenagy GP, Bostwick WB. Health and social service needs of transgender people in Chicago. Int J Transgend. 2005;8:57–66 [Google Scholar]
- 13. Bockting W, Huang CY, Ding H, et al. . Are transgender persons at higher risk for HIV than other sexual minorities? A comparison of HIV prevalence and risks. Int J Transgend. 2005;8:123–131 [Google Scholar]
- 14. Bockting W, Robinson B, Forberg J, Scheltema K. Evaluation of a sexual health approach to reducing HIV/STD risk in the transgender community. AIDS Care. 2005;17:289–303 [DOI] [PubMed] [Google Scholar]
- 15. Kenagy GP. Transgender health: findings from two needs assessment studies in Philadelphia. Health Soc Work. 2005;30:19–26 [DOI] [PubMed] [Google Scholar]
- 16. Risser JMH, Shelton A, McCurdy S, et al. . Sex, drugs, violence, and HIV status among male-to-female transgender persons in Houston, Texas. Int J Transgend. 2005;8:67–74 [Google Scholar]
- 17. Xavier JM. The Washington DC Transgender Needs Assessment Survey: Final Report for Phase Two. 2000. Washington, DC: Administration for HIV and AIDS of the District of Columbia Government [Google Scholar]
- 18. Xavier JM, Simmons R. The Washington Transgender Needs Assessment Survey: executive summary. 2000. Washington, DC, Administration for HIV and AIDS of the District of Columbia Government; Available at www.glaa.org/archive/2000/tgneedsassessment1112.shtml Accessed April4, 2017 [Google Scholar]
- 19. Xavier JM, Bobbin MB, Singer B, Budd E. A needs assessment of transgendered people of color living in Washington, DC. Int J Transgend. 2005;8:31–47 [Google Scholar]
- 20. Clements K, Katz M, Marx R. The Transgender Community Health Project: Descriptive Results. San Francisco, CA: San Francisco Department of Public Health, 1999 [Google Scholar]
- 21. Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviours, health care use, and mental health status of transgender persons: implications for public health intervention. Am J Public Health. 2001;91:915–921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Clements-Nolle K, Marx R, Katz M. Attempted suicide among transgender persons: the influence of gender-based discrimination and victimization. J Homosex. 2006;51:53–69 [DOI] [PubMed] [Google Scholar]
- 23. Zians J. The San Diego County Transgender Assessment Report. 2006. San Diego, CA: The California Endowment and Family Health Centers of San Diego's Transgender Health Project [Google Scholar]
- 24. Taylor C. Nowhere near enough: A needs assessment of health and safety services for transgender and two spirit people in Manitoba and Northwestern Ontario. 2006, Winnipeg, Manitoba, Crime Prevention Branch Public Safety and Emergency Preparedness Canada; Available at www.turtleisland.org discussion/viewtopic.php?p=7927 Accessed April4, 2017 [Google Scholar]
- 25. Taylor C. Health and safety issues for aboriginal transgender/two spirit people in Manitoba. Can J Aborig Comm Based HIV/AIDS Res. 2009;2:63–84 [Google Scholar]
- 26. Landers SJ, Gilsanz P. The health of Lesbian, Gay, Bisexual and Transgender (LGBT) persons in Massachusetts: a survey of health issues comparing LGBT persons with their heterosexual and non-transgender counterparts. 2009. Boston, MA, Massachusetts Department of Public Health; Available at www.masstpc.org/wp-content/uploads/2012/10/DPH-2009-lgbt-health-report.pdf Accessed April4, 2017 [Google Scholar]
- 27. McDuffie E, Brown GR. 70 U.S. veterans with gender identity disturbances: a descriptive study. Int J Transgend. 2010;12:21–30 [Google Scholar]
- 28. Nuttbrock L, Hwahng S, Bockting W, et al. . Psychiatric impact of gender-related abuse across the life course of male-to-female transgender persons. J Sex Res. 2010;47:12–23 [DOI] [PubMed] [Google Scholar]
- 29. Maguen S, Shipherd JC. Suicide risk among transgender individuals. Psychol Sex. 2010;1:34–43 [Google Scholar]
- 30. Shipherd JC, Maguen S, Skidmore WC, Abramovitz SM. Potentially traumatic events in a transgender sample: frequency and associated symptoms. Traumatology. 2011;17:56–67 [Google Scholar]
- 31. Effrig JC, Bieschke KJ, Locke BD. Examining victimization and psychological distress in transgender college students. J Coll Couns. 2011;14:143–157 [Google Scholar]
- 32. Hayes JA, Locke BD, Castonguay LG. Introduction to the special issue: the centre for collegiate mental health: practice and research working together. J Coll Couns. 2011;14:101–104 [Google Scholar]
- 33. Meier SLC, Fitzgerald KM, Pardo ST, Babcock J. The effects of hormonal gender affirmation treatment on mental health in female-to-male transsexuals. J Gay Lesbian Ment Health. 2011;15:281–299 [Google Scholar]
- 34. House AS, Van Horn E, Coppeans C, Stepleman LM. Interpersonal trauma and discriminatory events as predictors of suicidal and nonsuicidal self-injury in gay, lesbian, bisexual, and transgender persons. Traumatology. 2011;17:75–85 [Google Scholar]
- 35. Beemyn G, Rankin S. The Lives of Transgender People. New York: Columbia University Press, 2011 [Google Scholar]
- 36. Testa RJ, Jimenez CL, Rankin S. Risk and resilience during transgender identity development: the effects of awareness and engagement with other transgender people on affect. J Gay Lesbian Ment Health. 2013;18:31–46 [Google Scholar]
- 37. Heinz M, MacFarlane D. Island lives: a trans community needs assessment for Vancouver Island. SAGE Open. 2013;3:1–13 [Google Scholar]
- 38. Brown C, Dashjian LT, Acosta TJ, et al. . The career experiences of male-to-female transsexuals. Couns Pschol. 2012;40:868–894 [Google Scholar]
- 39. Brown C, Dashjian LT, Acosta TJ, et al. . Learning from the life experiences of male-to-female transsexuals. J GLBT Fam Study. 2013;9:105–128 [Google Scholar]
- 40. Moody C, Smith NG. Suicide protective factors among trans adults. Arch Sex Behav. 2013;42:739–752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Blosnich JR, Brown R, Shipherd JC, et al. . Prevalence of gender identity disorder and suicide risk among transgender veterans utilizing Veterans Health Administration care. Am J Public Health. 2013;103:e27–e32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Grant JM, Mottet LA, Tanis J, et al. . National Transgender Discrimination Survey Report on health and health Care. 2010. Washington, DC, National Center for Transgender Equality and National Gay and Lesbian Task Force; Available at https://cancer-network.org/wp-content/uploads/2017/02/National_Transgender_Discrimination_Survey_Report_on_health_and_health_care.pdfpdf Accessed January5, 2019 [Google Scholar]
- 43. Grant JM, Mottet LA, Tanis J, et al. . Injustice at every turn: A report of the National Transgender Discrimination Survey. 2011. Washington, DC, National Center for Transgender Equality and National Gay and Lesbian Task Force; Available at https://transequality.org/sites/default/files/docs/resources NTDS_Report.pdf Accessed January5, 2019 [Google Scholar]
- 44. Haas AP, Rodgers PL, Herman JL, et al. . Suicide attempts among transgender and gender non-conforming adults: Findings of the National Transgender Discrimination Survey. 2014. Los Angeles, CA, The Williams Insitute; Available at https://queeramnesty.ch/docs/AFSP-Williams-Suicide-Report-Final.pdf Accessed December31, 2018 [Google Scholar]
- 45. Mereish EH, O'Cleirigh C, Bradford JB. Interrelationships between LGBT based victimization, suicide, and substance use problems in a diverse sample of sexual and gender minorities. Psychol Health Med. 2014;19:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Reisner SL, White JM, Bradford JB, Mimiaga MJ. Transgender health disparities: comparing full cohort and nested matched-pair study designs in a community health center. LGBT Health. 2014;1:177–184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Reisner SL, White JM, Mayer KH, Mimiaga MJ. Sexual risk behaviors and psychosocial health concerns of female-to-male transgender men screening for STDs at an urban community health center. AIDS Care. 2014;26:857–864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wilson EC, Chen YH, Arayasirikul S, et al. . Connecting the dots: examining transgender women's utilization of transition-related medical care and associations with mental health, substance use, and HIV. J Urban Health. 2014;92:182–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Santos GM, Rapues J, Wilson EC, et al. . Alcohol and substance use among transgender women in San Francisco: prevalence and association with human immunodeficiency virus infection. Drug Alcohol Rev. 2014;33:287–295 [DOI] [PubMed] [Google Scholar]
- 50. de Haan G, Santos GM, Arayasirikul S, Raymond HF. Non-prescribed hormone use and barriers to care for transgender women in San Francisco. LGBT Health. 2015;2:313–323 [DOI] [PubMed] [Google Scholar]
- 51. Rosser BRS, Oakes JM, Bockting WO, Miner M. Capturing the social demographics of hidden sexual minorities: an internet study of transgender population in the United States. Sex Res Soc. 2007;4:50–64 [Google Scholar]
- 52. Perez-Brumer A, Hatzenbuehler ML, Oldenburg CE, Bockting W. Individual and structural-level risk factors for suicide attempts in transgender adults. Behav Med. 2015;41:164–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Scanlon K, Travers R, Coleman T, et al. . Ontario's trans communities and suicide: transphobia is bad for our health. Trans PULSE E-Bulletin. 2010;1:1–2 [Google Scholar]
- 54. Rotondi NK, Bauer GR, Scanlon K, et al. . Prevalence of and risk and protective factors for depression in female-to-male transgender Ontarians: trans PULSE project. Can J Comm Ment Health. 2011;30:135–155 [Google Scholar]
- 55. Rotondi NK, Bauer GR, Travers R, et al. . Depression in male-to-female transgender Ontarians: results from the trans PULSE project. Can J Comm Ment Health. 2011;30:113–133 [Google Scholar]
- 56. Bauer G, Anjali K, Pyne J, et al. . Improving the Health of Trans Communities: Findings from the Trans PULSE Project. Paper presented at: Rainbow Health Ontario Conference; 2012 Mar 22; Ottawa, Canada [Google Scholar]
- 57. Bauer GR, Pyne J, Francino MC, Hammond R. Suicidality among trans people in Ontario: implications for social work and social justice. Serv Soc. 2013;59:35–62 [Google Scholar]
- 58. Scheim AI, Bauer GR. Sex and gender diversity among transgender persons in Ontario, Canada: results from a respondent-driven sampling surgery. J Sex Res. 2015;52:1–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bauer GR, Scheim AI, Pyne J, et al. . Intervenable factors associated with suicide risk in transgender persons: a respondent driven sampling study in Ontario, Canada. BMC Public Health. 2015;15:1–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Edelman EA, Corado R, Lumby, et al. . Access Denied: Washington, DC Trans Needs Assessment Report. Washington, DC: DC Trans Coalition, 2015 [Google Scholar]
- 61. Mustanksi BS, Garofalo R, Emerson EM. Mental health disorders, psychological distress, and suicidality in a diverse sample of lesbian, gay, bisexual and transgender youths. Am J Public Health. 2010;100:2426–2432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Liu RT, Mustanski B. Suicidal ideation and self-harm in gay, bisexual, and transgender youth. Am J Prev Med. 2012;42:221–228 [DOI] [PubMed] [Google Scholar]
- 63. Mustanski B, Liu RT. A longitudinal study of predictors of suicide attempts among lesbian, gay, bisexual, and transgender youth. Arch Sex Behav. 2013;42:437–448 [DOI] [PubMed] [Google Scholar]
- 64. Birkett M, Newcomb ME, Mustanski B. Does it get better? A longitudinal analysis of psychological distress and victimization in lesbian, gay, bisexual, transgender, and questioning youth. J Adolesc Health. 2015;56:280–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Brown GR, Jones KT. Mental health and medical health disparities in 5135 transgender veterans receiving healthcare in the Veterans Health Administration: a case-control study. LGBT Health. 2016;3:122–131 [DOI] [PubMed] [Google Scholar]
- 66. Reisner SL, Vetters R, Leclerc M, et al. . Mental health of transgender youth in care at an adolescent urban community health center: a matched retrospective cohort study. J Adolesc Health. 2015;56:1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Olson J, Schrager SM, Belzer M, et al. . Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria. J Adolesc Health. 2015;57:374–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Olson JL. Baseline physiologic and psychosocial characteristics of transgender youth seeking care for gender dysphoria [Dissertation]. [Los Angeles,]: University of Southern California, 2015. p. 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kuper LE. Gender development and suicidality among transgender and gender non-conforming youth and young adults [Dissertation]. [Chicago: ]: University of Illinois at Chicago, 2015, p. 123 [Google Scholar]
- 70. Weir C. Violence and experience of transgender individuals: How this impacts their supports [master's thesis]. [Lethbridge: ]: University of Lethbridge, 2016, p. 211 [Google Scholar]
- 71. Tebbe EA, Moradi B. Suicide risk in trans populations: an application of minority stress theory. J Couns Psychol. 2016;63:520–533 [DOI] [PubMed] [Google Scholar]
- 72. Lehavot K, Simpson TL, Shipherd JC. Factors associated with suicidality among a national sample of transgender veterans. Suicide Life Threat Behav. 2016;46:507–524 [DOI] [PubMed] [Google Scholar]
- 73. Grossman AH, Park JY, Russell ST. Transgender youth and suicidal behaviors: applying the interpersonal psychological theory of suicide. J Gay Lesbian Men Health. 2016;20:329–349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Reisner SL, White JM, Dunham EE, et al. . Discrimination and health in Massachusetts: A statewide survey of transgender and gender nonconforming adults. 2014. Boston, MA: Fenway Health; Available at http://fenwayfocus.org/wp-content/uploads/2014/07/The-Fenway-Institute-MTPC-Project-VOICE-Report-July-2014.pdf Accessed December31, 2018 [Google Scholar]
- 75. Katz-Wise SL, Reiser SL, White Hughto JM, Budge SL. Self-reported changes in attractions and social determinants of mental health in transgender adults. Arch Sex Behav. 2017;46:1425–1439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Lytle MC, Blosnich JR, Kamen C. The association of multiple identities with self-directed violence and depression among transgender individuals. Suicide Life Threat Behav. 2016;46:535–544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Dowshen N, Matone M, Luan X, et al. . Behavioral and health outcomes for HIV + young transgender women linked to and engaged in medical care. LGBT Health. 2016;3:162–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. James SE, Herman JL, Rankin S, et al. . The report of the 2015 U.S. Transgender Survey. 2016. Washington, DC, National Center for Transgender Equality; Available at www.transequality.org/sites/default/files/docs/USTS-Full-Report-FINAL.PDF Accessed December31, 2018 [Google Scholar]
- 79. Nemoto T, Keatley JG, Operario D, Soma T. Psychosocial factors affecting HIV risk behaviours among Male-to-Female transgenders (MTF TGs) in San Francisco. San Francisco, CA: The University of California, San Francisco Center for AIDS Prevention Studies [CAPS], 2002 [Google Scholar]
- 80. Operario D, Nemoto T. Sexual risk behavior and substance use among a sample of Asian Pacific Islander transgendered women. AIDS Educ Prev. 2005;17:430–443 [DOI] [PubMed] [Google Scholar]
- 81. Nemoto T, Bodeker B, Iwamoto M. Social support, exposure to violence and transphobia and correlates of depression among male-to-female transgender women with a history of sex work. Am J Public Health. 2011;101:1980–1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Glynn TR, Gamarel KE, Kahler CW et al. The role of gender affirmation in psychological well-being among transgender women. Psychol Sex Orientat Gend Divers. 2016;3:336–344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Xavier J, Honnold JA, Bradford J. The health, health-related needs, and life course experiences of transgender Virginians. 2007. Richmond, VA, Virginia HIV Community Planning Committee and Virginia Department of Health; Available at www.vdh.virginia.gov/content/uploads/sites/10 2016/01/THISFINALREPORTVol1.pdf Accessed January5, 2019 [Google Scholar]
- 84. Goldblum P, Testa RJ, Pflum S, et al. : The relationship between gender-based victimization and suicide attempts in transgender people. Prof Psychol Res Pract. 2012;43:468–475 [Google Scholar]
- 85. Testa RJ, Sciacca LM, Wang F, et al. . Effects of violence on transgender people. Prof Psychol Res Pract. 2012;43:452–459 [Google Scholar]
- 86. Barboza GE, Dominguez S, Chance E. Physical victimization, gender identity and suicide risk among transgender men and women. Preventative Med Rep. 2016;4:385–390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Trujillo MA, Perrin PB, Sutter M, et al. . The buffering role of social support on the associations among discrimination, mental health, and suicidality in a transgender sample. Int J Transgenderism. 2017;18:39–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Brown C, Maragos A, Lee R, et al. . Female to male transsexuals: giving voice to their experience. J LGBT Issues Couns. 2016;10:1–39 [Google Scholar]
- 89. Fredriksen-Goldsen KI, Kim H, Emlet CA, et al. . The aging and health Report: Disparities and resilience among lesbian, gay, bisexual, and transgender older adults. Seattle, WA: Institute for Multigenerational Health, 2011 [Google Scholar]
- 90. Fredriksen-Goldsen KI, Cook-Daniels L, Kim HY, et al. . Physical and mental health of transgender older adults: an at-risk and underserved population. Gerontologist. 2013;54:488–500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Hoy-Ellis CP, Fredriksen-Goldsen KI. Depression among transgender older adults: general and minority stress. Am J Community Psychol. 2017;59:295–305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Irwin JA, Coleman JD, Fisher CM, Marasco VM. Correlates of suicide ideation among LGBT Nebraskans. J Homosex. 2014;61:1172–1191 [DOI] [PubMed] [Google Scholar]
- 93. Su D, Irwin JA, Fisher C, Ramos A, et al. . Mental health disparities within the LGBT population: a comparison between transgender and nontransgender individuals. Transgend Health. 2016;1:12–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Brennan SL, Irwin J, Drincic A, et al. . Relationship among gender-related stress, resilience factors, and mental health in a Midwestern U.S. transgender and gender-nonconforming population. Int J Transgen. 2017;18:433–445 [Google Scholar]
- 95. Kattari SK, Walls E, Speer SR, Kattari L. Exploring the relationship between transgender-inclusive providers and mental health outcomes among transgender/gender variant people. Soc Work Health Care. 2016;55:635–650 [DOI] [PubMed] [Google Scholar]
- 96. Seelman KL, Young SR, Tesene M, et al. . A comparison of health disparities among transgender adults in Colorado (USA) by race and income. Int J Transgend. 2017;18:199–214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Seelman KL, Colon-Diaz MJP, LeCroix RH, et al. . Transgender noninclusive healthcare and delaying care because of fear: connections to general health and mental health among transgender adults. Transgend Health. 2017;2:17–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Veale K, Saewyc E, Frohard-Dourlent H, et al. . Being safe, being me: Results of the Canadian Trans Youth Health Survey. 2015. Vancouver, Canada, University of British Columbia; Available at http://apsc-saravyc.sites.olt.ubc.ca/files/2018/03/SARAVYC_Trans-Youth-Health-Report_EN_Final_Web2.pdf Accessed December31, 2018 [Google Scholar]
- 99. Veale JF, Watson RJ, Peter T, Saewyc EM. Mental health disparities among Canadian transgender youth. J Adolesc Health. 2017;60:44–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Veale JF, Peter T, Travers R, Saewyc EM. Enacted stigma, mental health, and protective factors among transgender youth in Canada. Transgend Health. 2017;2:207–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Swanbrow Becker MA, Nemeth Roberts SF, Ritts SM, et al. . Supporting transgender college students: implications for clinical intervention and campus prevention. J Coll Stud Psychother. 2017;31:155–176 [Google Scholar]
- 102. Testa RJ, Michaels MS, Bliss E, et al. . Suicidal ideation in transgender people: gender minority stress and interpersonal theory factors. J Abnorm Psychol. 2017;126:125–136 [DOI] [PubMed] [Google Scholar]
- 103. Bouris A, Hill BJ. Exploring the mother-adolescent relationship as a promotive resource for sexual and gender minority youth. J Soc Issues. 2017;73:618–636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Lytle MC, Silenzio VMB, Homan CM, et al. . Suicidal and help-seeking behaviors among youth in an online lesbian, gay, bisexual, transgender, queer, and questioning social network. J Homosex. 2017;65:1–32 [DOI] [PubMed] [Google Scholar]
- 105. Gowin M, Taylor EL, Dunnington J, et al. . Needs of a silent minority: mexican transgender asylum seekers. Health Promot Pract. 2017;18:332–340 [DOI] [PubMed] [Google Scholar]
- 106. Redinger EA. Sex education in Montana schools: An assessment of the needs of sexual and gender minority youth [master's thesis]. [Missoula: ]: University of Montana; 2017. p. 91 [Google Scholar]
- 107. Gaither TW, Awad MA, Osterberg EC. Impact of sexual orientation identity on medical morbidities in male-to-female transgender patients. LGBT Health. 2017;0:1–6 [DOI] [PubMed] [Google Scholar]
- 108. Herman JL, Wilson BD, Becker T. Demographic and health characteristics of transgender adults in California: Findings from the 2015–2016 California Health Interview Survey. Policy Brief UCLA Cent Health Policy Res. 2017;8:1–10 [PubMed] [Google Scholar]
- 109. Beckwith N, Reiser SL, Zaslow S, et al. . Factors associated with gender-affirming surgery and age of hormone therapy initiation among transgender adults. Transgend Health. 2017;2:156–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Bukowski LA, Blosnich J, Shipherd JC, et al. . Exploring rural disparities in medical diagnoses among veterans with transgender-related diagnoses utilizing Veterans Health Administration Care. Med Care. 2017;55:s07–s103 [DOI] [PubMed] [Google Scholar]
- 111. Hamburger C, Stürup GK, Dahl-Iversen E. Transvestism: hormonal, psychiatric, and surgical treatment. J Am Med Assoc. 1953;152:391–396 [DOI] [PubMed] [Google Scholar]
- 112. Bockting W. Transforming the paradigm of transgender health: a field in transition. Sex Relation Ther. 2009;24:103–107 [Google Scholar]
- 113. Kruijver FP, Zhou J-N, Pool CW, et al. . Male-to-female transsexuals have female neuron numbers in a limbic nucleus. J Clin Endocrinol Metab. 2000;85:2034–2041 [DOI] [PubMed] [Google Scholar]
- 114. Winter S, Diamond M, Green J, et al. . Transgender people: health at the margins of society. Lancet. 2016;388:390–400 [DOI] [PubMed] [Google Scholar]
- 115. Dhejne C, Lichtenstein P, Boman M, et al. . Long-term follow-up of transsexual persons undergoing sex reassignment surgery: cohort study in Sweden. PLoS One. 2011;6:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Marshall E, Claes L, Bouman WP, et al. . Non-suicidal self-injury and suicidality in trans people: a systematic review of the literature. Int Rev Psychiatry. 2015;28:58–69 [DOI] [PubMed] [Google Scholar]
- 117. Virupaksha H, Muralidhar D, Ramakrishna J. Suicide and suicidal behavior among transgender persons. Indian J Psychol Med. 2016;38:505–509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. McNeil J, Ellis SJ, Eccles FJ. Suicide in trans populations: a systematic review of prevalence and correlates. Psychol Sex Orientat Gend Divers. 2017;4:341–353 [Google Scholar]
- 119. Wolford-Clevenger C, Frantell K, Smith PN, et al. . Correlates of suicide ideation and behaviors among transgender people: a systematic review guided by ideation-to-action theory. Clin Psychol Rev. 2018;63:93–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Arlington, VA: American Psychiatric Publishing, 2013 [Google Scholar]
- 121. Adams N. Finding order in chaos: Accounting for variation in estimates of suicidality among transgender adults [master's thesis]. [Halifax: ]: Dalhousie University, 2015. p. 161 [Google Scholar]
- 122. Ramsay R. Increasing awareness of GLBTTsQQA suicide issues: Transgender people generally have the highest ‘attempted suicide’ incidences among sexual minority groups. n.d. Available at https:people.ucalgary.ca/~ramsay/transgender-transsexual-suicide-studies-world.htm Accessed January5, 2019
- 123. United States Census Bureau. Quick facts: United States. 2017a. Available at www.census.gov/quickfacts/fact/table/US/PST045217 Accessed November23, 2018
- 124. United States Census Bureau. Educational attainment in the United States: 2017. 2017b. Available at www.census.gov/data/tables/2017/demo/education-attainment/cps-detailed-tables.html Accessed November292018
- 125. United States Census Bureau. HINC-06. Income distribution to $250,000 or more for households. 2017c. Available at www.census.gov/data/tables/timeseries/demo/income-poverty/cps-hinc/hinc-06.2017.html Accessed November20, 2018
- 126. Moody C, Fuks N, Peláez S, Smith NG. Without this, I would for sure already be dead: a qualitative inquiry regarding suicide protective factors among trans adults. Psychol Sex Orientat Gend Divers. 2015;2:266–280 [Google Scholar]
- 127. Watson B, Robinson DHZ, Harker L, Jacob Arriola KR. The inclusion of African-American study participants in web-based research studies: viewpoint. J Med Internet Res. 2016;18:1–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Miner MH, Bockting WO, Romine RS, Raman S. Conducting internet research with the transgender population: reaching broad samples and collecting valid data. Soc Sci Comput Rev. 2012;30:202–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Im E-O, Chee W. Methodological issues in the recruitment of ethnic minority subjects to research via the Internet: a discussion paper. Int J Nurs Stud. 2005;42:923–929 [DOI] [PubMed] [Google Scholar]
- 130. Centers for Disease Control and Prevention. Suicide. Facts at a glance, 2015. CDC Stacks: Public Health Publications. Centers for Disease Control, 2015. Available at https://stacks.cdc.gov/view cdc/34181 Accessed December31, 2018
- 131. Borges G, Orozco R, Rafful C, et al. . Suicidality, ethnicity and immigration in the USA. Psychol Med. 2012;42:1175–1184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Perez-Rodriguez MM, Baca-Garcia E, Oquendo MA, Blanco C. Ethnic differences in suicidal ideation and attempts. Prim Psychiatry. 2008;15:44–53 [PMC free article] [PubMed] [Google Scholar]
- 133. Rockett IRH, Wang S, Stack S, et al. . Race/ethnicity and potential suicide misclassification: window on a minority suicide paradox? BMC Psychiatry. 2010;10:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Rockett RH, Samora JB, Coben JH. The black-white suicide paradox: possible effects of misclassification. Soc Sci Med. 2006;63:2165–2175 [DOI] [PubMed] [Google Scholar]
- 135. Hom MA, Joiner TE, Bernert RA. Limitations of a single-items assessment of suicide attempt history: implications for standardized suicide risk assessment. Psychol Assess. 2016;28:1026–1030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Hunter E, Harvey S. Indigenous suicide in Australia, New Zealand, Canada and the United States. Emerg Med (Fremantle). 2002;14:14–23 [DOI] [PubMed] [Google Scholar]
- 137. Curtin SC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999–2014. NCHS Data Brief. 2016;241:1–8 [PubMed] [Google Scholar]
- 138. Elias B, Mignone J, Hall M, et al. . Trauma and suicide behaviour histories among a Canadian indigenous population: an empirical exploration of the potential role of Canada's residential school system. Soc Sci Med. 2012;74:1560–1569 [DOI] [PubMed] [Google Scholar]
- 139. Wong SS, Sugimoto-Matsuda J, Chang JY, Hishinuma ES. Ethnic differences in risk factors for suicide among American high school students, 2009: the vulnerability of multiracial and Pacific Islander adolescents. Arch Suicide Res. 2010;16:159–173 [DOI] [PubMed] [Google Scholar]
- 140. Paniagua FA. Some comments to further improve the DoDSER. Mil Med. 2010;175:80–81 [DOI] [PubMed] [Google Scholar]
- 141. Subica AM, Wu LT. Substance use and suicide in Pacific Islander, American Indian, and multiracial youth. Am J Prev Med. 2018;54:795–805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Cheref S, Lane R, Polanco-Roman L, et al. . Suicidal ideation among racial/ethnic minorities: moderating effects of rumination and depressive symptoms. Cultur Diver Ethnic Minor Psychol. 2015;21:31–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Ryan CL, Bauman K. Educational attainment in the United States: 2015. 2016. Available at www.census.gov/content/dam/Census/library/publications/2016/demo/p20–578.pdf Accessed November23, 2018
- 144. Statistics Canada. Table 1: Number and proportion of the population aged 25 to 64 by highest level of educational attainment, Canada, 2011. 2011. Available at www12.statcan.gc.ca/nhs-enm/2011/as-sa/99-012-x/2011001/tbl/tbl01-eng.cfm Accessed November23, 2018
- 145. Phillips JA, Hempstead K. Differences in U.S. suicide rates by educational attainment, 2000–2014. Am J Prev Med. 2017;53:e123–e130 [DOI] [PubMed] [Google Scholar]
- 146. Abel EL, Kruger M. Educational attainment and suicide rates in the United States. Psychol Rep. 2005;97:25–28 [DOI] [PubMed] [Google Scholar]
- 147. Crissman HP, Berger MB, Graham LF, Dalton VK. Transgender demographics: a household probability sample of US adults, 2014. Am J Public Health. 2017;107:213–215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Graham LF, Crissman HP, Tocco J, et al. . Navigating community institutions: black transgender women's experiences in schools, the criminal justice system, and churches. Sex Res Social Policy. 2014;11:274–287 [Google Scholar]
- 149. Downing JM, Przedworski JM. Health of transgender adults in the U.S., 2014–2016. Am J Prev Med. 2018;55:336–344 [DOI] [PubMed] [Google Scholar]
- 150. Rands KE. Considering transgender people in education. J Teach Educ. 2009;60:419–431 [Google Scholar]
- 151. Center for American Progress, Movement Advancement Project. Paying an unfair price: The financial penalty for being transgender in America. Washington, DC, Center for American Progress, 2015 [Google Scholar]
- 152. McNeil J, Bailey L, Ellis S, et al. . Trans Mental Health Study 2012. 2012. Edinburgh, Scotland, EqualityNetwork; Available at http://worldaa1.miniserver.com/~gires/assets/Medpro-Assets/trans_mh_study.pdf Accessed January5, 2019 [Google Scholar]
- 153. Michel A, Ansseau M, Legros J-J, et al. . The transsexual: what about the future? Eur Psychiatry. 2002;17:353–362 [DOI] [PubMed] [Google Scholar]
- 154. Mate-Kole C, Freschi M, Robin A. Aspects of psychiatric symptoms at different stages in the treatment of transsexualism. Br J Psychiatry. 1988;152:550–553 [DOI] [PubMed] [Google Scholar]
- 155. Lundström B, Pauly I, Wålinder J. Outcome of sex reassignment surgery. Acta Psychiatr Scand. 1984;70:289–294 [DOI] [PubMed] [Google Scholar]
- 156. Pauly IB. Male psychosexual inversion: transsexualism: a review of 100 cases. Arch Gen Psychiatry. 1965;13:172–181 [DOI] [PubMed] [Google Scholar]
- 157. Pauly IB. Female transsexualism: Part 1. Arch Sex Behav. 1974;3:487–507 [DOI] [PubMed] [Google Scholar]
- 158. Pauly IB. Female Transsexualism: Part II. Arch Sex Behav. 1974;3:509–526 [DOI] [PubMed] [Google Scholar]
- 159. Pauly IB. Outcome of sex reassignment surgery for transsexuals. Aust N Z J Psychiatry. 1981;15:45–51 [DOI] [PubMed] [Google Scholar]
- 160. Keo-Meier CL, Herman LI, Reisner SL, et al. . Testosterone treatment and MMPI–2 improvement in transgender men: a prospective controlled study. J Consult Clin Psychol. 2015;83:143–156 [DOI] [PubMed] [Google Scholar]
- 161. Davis SA, Colton Meier S. Effects of testosterone treatment and chest reconstruction surgery on mental health and sexuality in female-to-male transgender people. Int J Sex Health. 2014;26:113–128 [Google Scholar]
- 162. Gómez-Gil E, Zubiaurre-Elorza L, Esteva I, et al. . Hormone-treated transsexuals report less social distress, anxiety and depression. Psychoneuroendocrinology. 2012;37:662–670 [DOI] [PubMed] [Google Scholar]
- 163. Murad MH, Elamin MB, Garcia MZ, et al. . Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol (Oxf). 2010;72:214–231 [DOI] [PubMed] [Google Scholar]
- 164. Claes L, Bouman WP, Witcomb G, et al. . Non-suicidal self-injury in trans people: associations with psychological symptoms, victimization, interpersonal functioning, and perceived social support. J Sex Med. 2015;12:168–179 [DOI] [PubMed] [Google Scholar]
- 165. Statistics Canada. Census profile, 2016 census: Canada [country] and Canada [country]. 2017a. Available at www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm ?Lang=E&Geo1=PR&Code1=01&Geo2=&Code2=&Data=Count&SearchText=Canada&SearchType=Begins&SearchPR=01&B1=All&TABID=1 Accessed November23, 2018
- 166. Statistics Canada. Ethnic origin reference guide, census of population 2016. 2017b. Available at www12.statcan.gc.ca/census-recensement/2016/ref/guides/008/98-500-x2016008-eng.cfm Accessed November23, 2018
- 167. Greco T, Zangrillo A, Biondi-Zoccai G, Landoni G. Meta-analysis: pitfalls and hints. Heart Lung Vessel. 2013;5:219–225 [PMC free article] [PubMed] [Google Scholar]
- 168. Turner RM, Bird SM, Higgins JPT. The impact of study size on meta-analyses: examination of underpowered studies in Cochrane Reviews. PLoS One. 2013;8:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. American Psychological Association. Ethnic and racial minorities & socioeconomic status. n.d. Available at www.apa.org/pi/ses/resources/publications/minorities Accessed September7, 2019
- 170. Patten SB. Selection bias in studies of major depression using clinical subjects. J Clin Epidemiol. 2000;53:351–357 [DOI] [PubMed] [Google Scholar]
- 171. Stirman SW, Brown GK, Ghahramanlou-Holloway M, et al. . Participation bias among suicidal adults in a randomized controlled trial. Suicide Life Threat Behav. 2012;4:203–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Coleman E, Bockting W, Botzer M, et al. . Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgend. 2012;13:165–232 [Google Scholar]
- 173. Richards C, Bouman WP, Seal L, et al. . Non-binary or genderqueer genders. Int Rev Psychiatry. 2016;28:95–102 [DOI] [PubMed] [Google Scholar]
- 174. Nock MK, Kessler RC. Prevalence of and risk factors for suicide attempts versus suicide gestures: analysis of the National Comorbidity Survey. J Abnorm Psychol. 2006;115:616–623 [DOI] [PubMed] [Google Scholar]
- 175. Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–626 [DOI] [PubMed] [Google Scholar]