Abstract
Purpose
Understanding how difficulties in emotion regulation can be related to metacognitive beliefs during early abstinence, identifying which factors are associated with craving and relapse risk may be useful in residential rehabilitation treatment of alcohol addiction.
Methods
Sixty-five patients underwent a 28-day rehabilitation program for alcohol addiction. They underwent a brief semi-structured interview at admission and completed a battery of five self-report questionnaires between days 7 and 10 of alcohol abstinence (T0) and 3 days prior to discharge (T1).
Results
After rehabilitation program, all symptoms of psychological distress decreased. We found a significant improvement in all emotional, cognitive and metacognitive scales except for “Cognitive harm” (NAM), “Awareness” (DERS) and a small effect size (low statistical power) for “Emotional clarity” (DERS). Compared to those still abstinent at 1 month from discharge, we found more difficulties in “Emotional clarity” in those who had an early relapse. Difficulties in “Emotional clarity” were observed also in patients with a high level of craving at discharge.
Conclusion
Significant differences were observed between the groups “abstinence vs non-abstinence” at 1 month from discharge concerning difficulties in emotion regulation. In particular, we found difficulty in the awareness and understanding of emotion, precisely to identify correctly the emotions. The “Emotional Clarity” seems to be the emotional difficulty that characterized also the group with a high level of craving at discharge and the individuals with early relapse, suggesting the importance of this function as a preliminary factor in emotion regulation.
Keywords: emotion regulation, alcohol, abstinence, metacognitions, relapse
Introduction
Emotion dysregulation is a core feature of many mental disorders, including Alcohol Dependence.1 Several theories contend that affect regulation is the main reason for alcohol use.2–4 Alcohol can be used to regulate emotions and to cope with negative emotional states.5 Hence, it becomes a source of significant negative reinforcement to try and eliminate undesirable emotions. Emotion regulation refers to the ability to identify, understand and accept emotions, control impulsive behaviours in line with the individual’s goals and use situationally appropriate strategies in order to modulate emotional responses.6 The influence of metacognitive beliefs about alcohol use on the development and persistence of emotional dysfunction is also central. Positive and negative metacognitions motivate individuals to start and perpetuate alcohol use as a strategy of cognitive-emotional regulation.7
Alcohol abstinence, also, is associated with changes in neural stress and reward-related brain regions, that are associated with the experience and regulations of emotions.8 Moreover, early abstinence involves a distress state that may make it difficult to manage affect and impulses and lead to immediate gratification seeking during efforts to emotionally self-regulate.9
Indeed, evidence suggests that people who are able to tolerate negative affect remain abstinent for longer.10 Understanding how difficulties in emotion regulation can be related to metacognitive beliefs during early abstinence and identifying which specific aspects are associated with craving and relapse risk may be useful in guiding treatment.
In this study, we aimed to examine emotion regulation changes over time in early abstinent treatment-seeking alcohol-dependent patients, during inpatient rehabilitation, and the relationship with changes in metacognitive beliefs about alcohol use that represent the mediators of emotional dysregulation. The present analysis also aimed to investigate potential differences in emotion regulation difficulties between individuals with vs without early lapse (one-month from discharge) and craving.
Methods
Participants
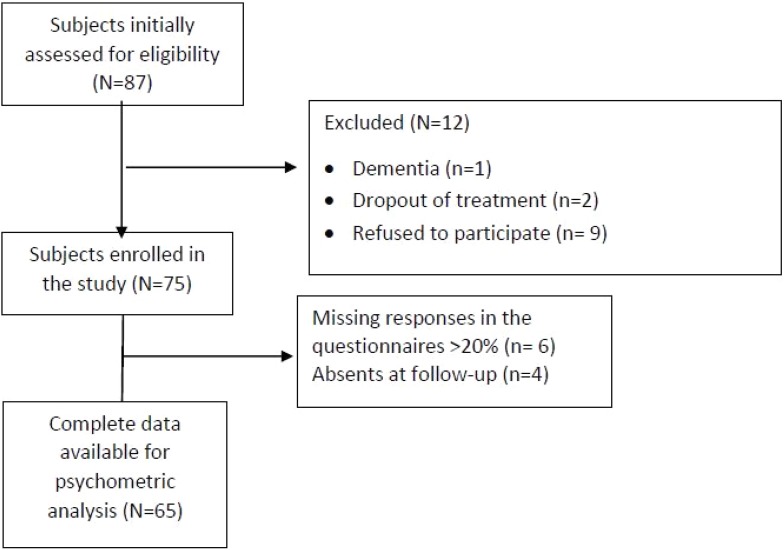
Sixty-five patients were recruited from a 28-day inpatient rehabilitation program for alcohol dependence at the Department of Physical Rehabilitation Medicine, ICS Maugeri SPA SB, and Institute of Genoa, Italy. All patients met the criteria of the Diagnostic and Statistical Manual of Mental Disorders, 4th edition revised (DSM-IV-TR),11 for diagnosis of alcohol dependence. Inclusion criteria for the study were: age >18 years, absence of dementia (Mini-Mental State Examination score ≥24), understanding of Italian language (spoken or written understanding, if foreigners), successful completion the detoxification program and participation in >80% of the planned rehabilitation sessions. The only exclusion criterion was a significant risk of suicide or suicide attempts in the two months prior to admission (as assessed during the intake interview by a trained clinician). Of the 87 patients initially screened, 12 (14%) did not meet the inclusion criteria and were excluded. Another 10 patients (11%) were later eliminated from the study sample, because of >20% of responses missing on the questionnaires or non-attendance at the follow-up (Figure 1). This study was conducted in accordance with the Declaration of Helsinki. All patients gave their written informed consent to the study and the Regional Ethics Committee of IRCCS AOU San Martino-IST (PR 430 Reg 2015) approved the research project. All authors declare no competing interests.
Figure 1.
Study flow chart with exclusion criteria.
Procedure
At the beginning of the rehabilitation stay, patients were interviewed by a trained health worker with wide experience in the field of addiction, who collected sociodemographic and clinical data for planning medical management of symptoms during withdrawal. A battery of five self-report questionnaires was administered between days 7 and 10 of rehabilitation treatment and alcohol abstinence (T0) and 3 days prior to discharge (T1). Patients remained in the unit for an average of 28 days. The treatment program included medical, nursing and psychological interventions. In particular, it involved evaluation and treatment of withdrawal symptoms with drugs, group therapy (1 hr/day) for maintenance of abstinence and CBT training to identify and modify dysfunctional beliefs about alcohol use and acquire coping skills to prevent relapse. Gymnastics, relaxation techniques and physical rehabilitation therapy took place in the afternoon. Family sessions occurred once a week. At discharge, the subjects were divided into two groups: low (PACS score ≤15) and high craving (PACS score >15). One month after discharge, patients included in the study reported to the Institute for a follow-up session and underwent a clinical interview regarding their post-rehabilitation clinical course and the maintenance of abstinence, and an alcohol test with breathalyser was performed in doubtful cases.
Measures
A brief initial semi-structured interview to collect clinical and socio-demographic information and a battery of five self-report questionnaires were administered, investigating the following areas: (a) emotion regulation; (b) craving; (c, d) positive and negative alcohol beliefs; and (e) the psychophysical state of health. We administered the battery of self-report questionnaires twice, on admission to the rehabilitation program and again 3 days before discharge.
The following evaluation scales were used:
Difficulties In Emotion Regulation Scale (DERS)
The DERS (Italian Version)12 is a brief (36-item) self-report questionnaire developed by Gratz and Roemer 2004, designed to assess multiple aspects of emotion dysregulation, scored on a 5-point Likert scale (from “almost never” to “almost always”). Higher scores indicate more difficulty in emotion regulation. The questionnaire yields a total score as well as six sub-scores derived through factor analysis:
NON-ACCEPTANCE (non-acceptance of one’s emotional responses) is composed of items that reflect the tendency to experience negative secondary emotions in response to one’s negative emotions, or to have reactions of non-acceptance with respect to one’s own discomfort.
GOALS (difficulty in adopting target-oriented behaviors) includes items that reflect difficulty in concentrating on and pursuing a task when experiencing negative emotions.
STRATEGIES (limited access to regulatory strategies) reflects a difficulty to effectively regulate the emotions that one has manifested. In the Italian validation, it was considered more as a lack of self-confidence and an inability to trust oneself in managing negative emotions.
IMPULSE (difficulty in impulse control) reflects difficulty in maintaining control of one’s behavior when experiencing negative emotions.
CLARITY (lack of emotional clarity) includes items that reflect the degree to which one can understand distinctly what emotion one is experiencing.
AWARENESS (lack of emotional awareness) contains items that emphasize the tendency to pay attention to emotions and the ability to recognize them (for this reason, the answers provided must be reversed in the phase scoring system). The Italian version of DERS showed good test–retest reliability and adequate validity, comparable to the original version, strengthening the rationale for cross-cultural utilization of DERS.13
Penn Alcohol Craving Scale (PACS)
The PACS14 is a 5-item self-administered measure (with total score from 0 to 30) assessing the frequency, intensity and duration of thoughts about drinking, average craving in the past week, and difficulty in resisting drinking if a bottle were available. PACS showed to be a valid and reliable measure of craving, able to predict the risk of relapse.
Positive Alcohol Metacognitions Scale (PAMS)
The scale consists of 12 items that investigate positive alcohol beliefs.15 Two factors represent positive metacognitions about alcohol use in: 1) emotional and 2) cognitive self-regulation. All items ranging from 1 (Do not agree) to 4 (Agree very much) are designed to determine the degree of agreement of participants with each statement, referring to the use of alcohol. PAMS possesses good psychometric properties in clinical practice.
Negative Alcohol Metacognitions Scale (NAMS)
The scale concerns 6 items that evaluate negative alcohol beliefs. Two principal components explore these variables: 1) the uncontrollability of alcohol use; and 2) the cognitive harm related to alcohol use. The total score range from 6 to 24 with higher score indicating higher levels of negative alcohol beliefs. NAMS demonstrated a good reliability and validity.16
Cognitive Behavioral Assessment – Outcome Evaluation (CBA-OE)
To evaluate the effect of the psychological treatment provided during the residential program, we used the CBA-OE tool,17 composed of 80 items scored on a 5-point Likert scale (from “not at all” to “very much”). The questionnaire has five scales: Anxiety (14 items); Well-being (15 items); Perception of positive change (11 items); Depression (19 items) and Psychological distress (21 items).
The CBA-OE has shown to have good psychometric qualities: it has a strong factor structure, good internal consistency and good ability to discriminate between nonclinical and “clinical” subjects.17
Statistical Analysis
Data analysis was performed using the software package STATA 14.0 release. Descriptive statistics (percentage, mean ± standard deviation) were used to analyze the characteristics of the study sample. The scores of scales DERS, PAMS, NAMS and PACS at T0 and T1 were reported as median and interquartile range (IQR). The scores of CBA-OE at T0 and T1 were reported as mean ± standard deviation. The assumption of normality and linearity for this scale was verified by the skewness and kurtosis normality test of STATA software. We investigated significant differences on the DERS with metacognitive and cognitive variables (PAMS, NAMS and PACS) between baseline and discharge using Wilcoxon signed rank test and calculated the effect size, using Cohen test criteria.18 We analyzed significant differences on CBA-OE through Student’s t-test (nondirectional, α=0.05) using Cohen’s d statistic to calculate the size effect.18 Possible correlations among the variables examined were evaluated with Spearman correlation coefficient,19 using Bonferroni correction for multiple comparisons.20 The Mann–Whitney test was performed to compare abstinent vs non-abstinent patients (at one month from discharge) or patients with high vs low craving at discharge. We preferred to use a nonparametric statistic, because not all scales meet normal distribution criteria and with ordinal scales, this statistic is less sensitive to the presence of outliers and the probability of error type I is lower.21
Results
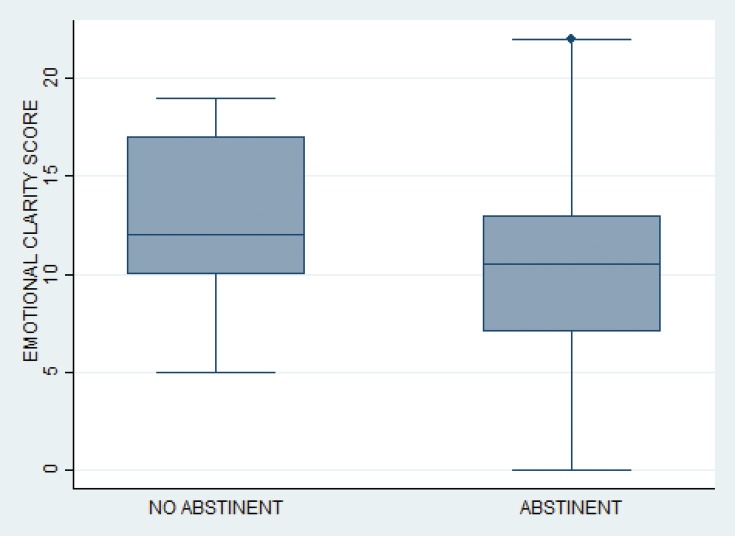
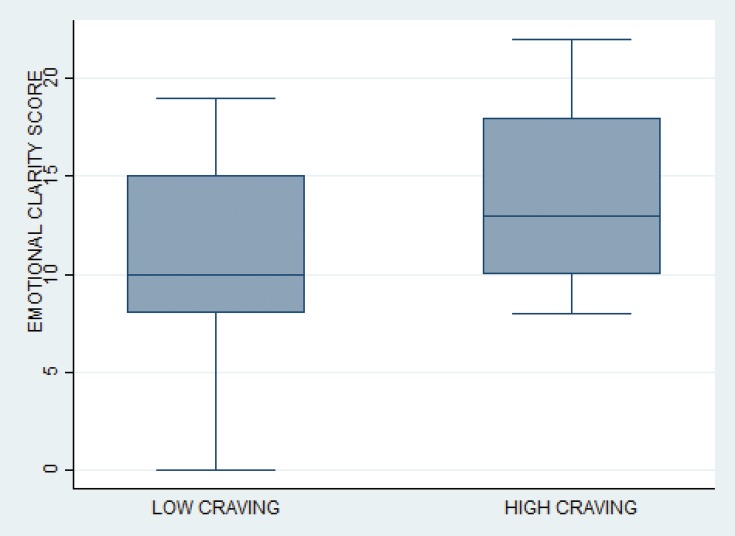
Sociodemographic and clinical characteristics of the study sample are reported in Table 1. The majority were males, unemployed (70.7%) and pure alcoholics (80%). The mean age was 51.03±8.71 years. The changes between T0 and T1 in the DERS and its subscales, cognitive variables (PAMS, NAMS and PACS), with the effect size of the difference, are reported in Tables 2 and 3. We found differences of a medium to large effect size in all the emotional, psychological, metacognitive and cognitive scales except for Awareness scale and in the “Emotional Clarity” scale the difference was closer to a small effect size. We found also no difference in the “Cognitive Harm” scale of NAM. After rehabilitation program, 36 subjects (55.3%) presented low craving and 29 (44.7%) high craving. One month after discharge, 30 subjects (46.1%) presented early relapse. Compared to those still abstinent at 1 month from discharge, we found more difficulties in “Emotional clarity” in those who had an early relapse (Figure 2). Difficulties in emotion regulation on the subscale “Emotional clarity” were observed also in patients with a high level of craving at discharge (Figure 3). Correlations during the period of early abstinence were present between DERS and psychological variables of CBA-OE, PAMS and NAMS (Table 4).
Table 1.
Sociodemographic And Clinical Characteristics Of The Total Sample (n=65)
| Variable | N (%) |
|---|---|
| Sex | |
| Male | 46 (70.7) |
| Female | 19 (29.3) |
| Education | |
| Low | 35 (53.85) |
| Middle-high | 30 (46.15) |
| Work status | |
| Employed | 19 (29.23) |
| Not employed | 46 (70.77) |
| Comorbidity | |
| Yes | 40 (61.54) |
| No | 25 (38.46) |
| Intervention | |
| Pharmaco- & Psychotherapy | 35 (53.85) |
| Psychotherapy only | 30 (46.15) |
| Alcohol dependence | |
| ≤10 years | 33 (50.77) |
| >10 years | 32 (49.23) |
| Substance dependence | |
| Pure Alcoholics | 52 (80) |
| Polyabusers | 13 (20) |
| Previous admissions | |
| Yes | 42 (64.61) |
| No | 23 (35.39) |
| Age | |
| Mean±SD | 51.03±8.71 |
| Audit | |
| Mean ±SD | 27.16±7.78 |
Abbreviation: SD, standard deviation.
Table 2.
Changes In Median Scores Of Cognitive And Metacognitive Scales Pre (T0) And Post (T1) Rehabilitation
| Admission (T0) | Discharge (T1) | z | P | Cohen’s d | |
|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | ||||
| Difficulties in emotion regulation scale (DERS) | |||||
| Non-acceptance | 14 (8–21) | 10 (6–16) | 4.39 | <0.0001 | 0.54 |
| Goals | 13 (10–19) | 10 (7–15) | 3.35 | <0.008 | 0.41 |
| Strategies | 21 (16–26) | 16 (11–23) | 3.17 | <0.005 | 0.40 |
| Impulse | 11 (8–17) | 8 (6–12) | 3.65 | <0.0002 | 0.45 |
| Clarity | 11 (8–15) | 9 (6–14) | 2.63 | <0.008 | 0.32 |
| Awareness | 6 (4–10) | 6 (3–8) | 1.50 | 0.13 | – |
| DERS Total | 88 (64–150) | 72 (52–145) | 4.36 | <0.0001 | 0.54 |
| Positive alcohol metacognitions (PAMS) | |||||
| Emotional Self Regulation | 18 (10–22) | 11 (0–18) | 4.23 | <0.0001 | 0.52 |
| Cognitive Self Regulation | 7 (4–9) | 4 (0–6) | 3.71 | <0.0002 | 0.46 |
| PAMS Total | 26 (14–31) | 15 (0–25) | 4.14 | <0.0001 | 0.51 |
| Negative alcohol metacognitions (NAMS) | |||||
| Beliefs about Uncontrollability | 6 (3–9) | 4 (0–7) | 4.5 | <0.0001 | 0.55 |
| Cognitive Harm | 9 (4–11) | 9 (0–11) | 0.85 | 0.39 | – |
| NAMS Total | 16 (7–19) | 12 (0–17) | 3.47 | <0.0005 | 0.43 |
| Penn Alcohol Craving Scale (PACS) | |||||
| Craving | 18 (15–21) | 11 (5–16) | 4.63 | <0.0001 | 0.57 |
| N, patients=65 |
Table 3.
Changes In Mean Scores Of Psychological Scales Pre (T0) And Post (T1) Rehabilitation
| Admission (T0) | Discharge (T1) | t | P | Cohen’s d | |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | ||||
| CBA-OE Subscales | |||||
| Anxiety | 24.70 (12.94) | 12.75 (8.32) | 7.773 | <0.0001 | 1.09 |
| Well-being | 21.37 (11.07) | 36.18 (10.63) | 10.460 | <0.0001 | 1.36 |
| Perception of positive change | 20.09 (7.21) | 29.37 (6.15) | 10.298 | <0.0001 | 1.38 |
| Depression | 33.07 (15.28) | 14.05 (9.97) | 9.757 | <0.0001 | 1.47 |
| Psychological distress | 30.53 (15.53) | 11.87 (10.07) | 8.982 | <0.0001 | 1.42 |
| N, patients=65 |
Figure 2.
Box-plot of difficulties in “Emotional clarity” between abstinent or not subject at one month from discharge.
Figure 3.
Box-plot of difficulties in “Emotional clarity” between subjects with low (PACS score ≤15) and high craving (PACS score >15) at discharge.
Table 4.
Correlations Of DERS Total Score And Subscales With Psychological, Cognitive And Metacognitive Factors At Admission
| DERS Total | Non-acceptance | Goals | Strategies | Impulse | Clarity | Awareness | |
|---|---|---|---|---|---|---|---|
| 2. Anxiety | 0.27* | 0.13 | 0.21 | 0.34* | 0.26* | 0.18 | 0.05 |
| 3. Well-being | −0.31* | −0.14 | −0.13 | −0.39* | −0.17 | −0.43* | −0.23 |
| 4. Perception of positive change | −0.28* | −0.16 | −0.14 | −0.33* | −0.18 | −0.37* | −0.18 |
| 5. Depression | 0.29* | 0.13 | 0.24 | 0.36* | 0.25* | 0.29* | 0.09 |
| 6. Psychological distress | 0.24 | 0.05 | 0.15 | 0.27* | 0.31* | 0.24* | 0.19 |
| 7. Positive alcohol metacognitions | 0.36* | 0.30* | 0.38* | 0.25 | 0.33* | 0.36* | 0.34* |
| 8. Negative alcohol metacognitions | 0.41* | 0.31* | 0.44* | 0.40* | 0.47* | 0.20 | 0.09 |
| 9. Craving | 0.21 | 0.15 | 0.33* | 0.22 | 0.20 | 0.04 | −0.05 |
Note: Values presented are Spearman correlation coefficient (r). *P value <0.05.
Discussion
The aim of this study was to investigate difficulties in emotion regulation during early abstinence, a period characterized by a distress state and psychological discomfort.22 In particular, the clinical symptoms of this period include emotional changes such as irritability, agitation, anxiety and dysphoria, sleep disturbances and a negative affective state. The persistence of these symptoms may constitute a significant motivational factor that leads to relapse.
Lack of emotion regulation strategies is thought to be a key feature of alcohol dependence and the main reason for alcohol use.23 Due to the psychological effort and stress involved in managing affect and impulses during early alcohol abstinence, immediate gratification seeking may occur instead of focusing on long-term priorities. This conflict in regulatory goals may have important implications for treatment outcome in alcohol-dependent patients. In this phase, after a week from admission (and abstinence from alcohol), our patients scored on the DERS values similar to subjects examined with the original version of the scale, ie, a sample of treatment-seeking adults with one or more emotional disorders,24 confirming the presence of difficulties in emotion regulation in the first period of abstinence. Comparing the median score of the total range of each subscale, we found higher values for difficulties with “Goals”, “Strategies” and “Awareness” than for the other subscales of DERS. This suggests that during early abstinence patients were less able to acknowledge their emotions25 and consequently had difficulty to apply coping strategies and avoid impulsive behaviours in a time of emotional distress. After rehabilitation treatment, we found an improvement in Emotion Regulation except for “Awareness” of emotional state, in which there was no difference between admission and discharge, while the change in “Emotional Clarity” had a small effect size, again highlighting difficulties in these skills after treatment. Awareness and clarity of emotion could represent early processing components of emotional competence.26 Indeed, only by acknowledging and identifying which emotions one is experiencing can one regulate negative affective states. Difficulties in these abilities may generate confusion about emotional experiences and the subjects may be less able to manage affect, using maladaptive regulation strategies in the presence of negative emotional states. These findings confirm a recent study on emotion differentiation (a behavioural measure of the construct “emotional clarity”) which reported that individuals with high emotion differentiation are able to distinguish among negative affective states and represent better their feelings, leading them to use less maladaptive behaviours.10 Moreover, research findings showed that lack of emotional clarity is similar to alexithymia, which was a predictor of poor outcomes in alcohol-dependent patients.27 During the first period of abstinence, we found significant positive correlations between DERS and the psychological scales of Anxiety and Depression, confirming the presence of emotional difficulties to manage these symptoms and the self-medicating hypothesis of alcohol use.28 Emotion dysregulation is known to underlie mental health conditions including anxiety and depressive disorders.25 In particular, we found high correlations with the subscales “Strategies” and “Impulse” for anxiety and with “Strategies”, “Impulse” and “Clarity” for depression. High levels of Emotion regulation difficulties also negatively correlated with the “Perception of positive change” and “Psychological well-being” scales of CBA-OE.
Another aspect we considered was the correlations with positive and negative alcohol metacognitions, which are considered potential mediators in the relationship between emotional dysregulation and problem drinking.29 Metacognitions play an executive function with regard to cognitive processing and, therefore, play a role in emotion regulation.30 Positive metacognitions are thought to motivate individuals to engage in alcohol use, with the intention of regulating affect. Negative beliefs play an important function in maintenance of alcohol use, activating negative emotional states during and following a drink episode, that push a person to continue drinking.31 In our study, during early abstinence, we found a higher total score for negative beliefs about alcohol use than for positive beliefs (if compared with the median score of the total range of each scale). These data were in agreement with emotional distress highlighted by the psychological scales.
The influence of metacognitive beliefs on the development and persistence of emotional dysregulation32 was confirmed by the significant correlation with DERS. In particular, the PAMS was correlated with all scales of DERS excluding “Strategies”, while NAMS had a positive correlation with the subscales “Non-acceptance”, “Goals”, “Strategies” and “Impulse”. Poor skills in identifying and acknowledging emotions may create difficulties to engage in emotion regulation strategies and in goal-directed behaviours, which may activate alcohol use derived from underlying dysfunctional positive metacognitions. Negative alcohol metacognitions seemed more to perpetuate maladaptive coping strategies, with difficulties to control impulse and achieve long-term goals.32 The lack of emotional clarity indicate that individuals are largely unaware of their feelings and in response to negative emotional state they avoid the development of skills such as identifying, labelling, expressing and managing emotions. This specific difficulty with emotion regulation was also found in another study among illicit substance users.28
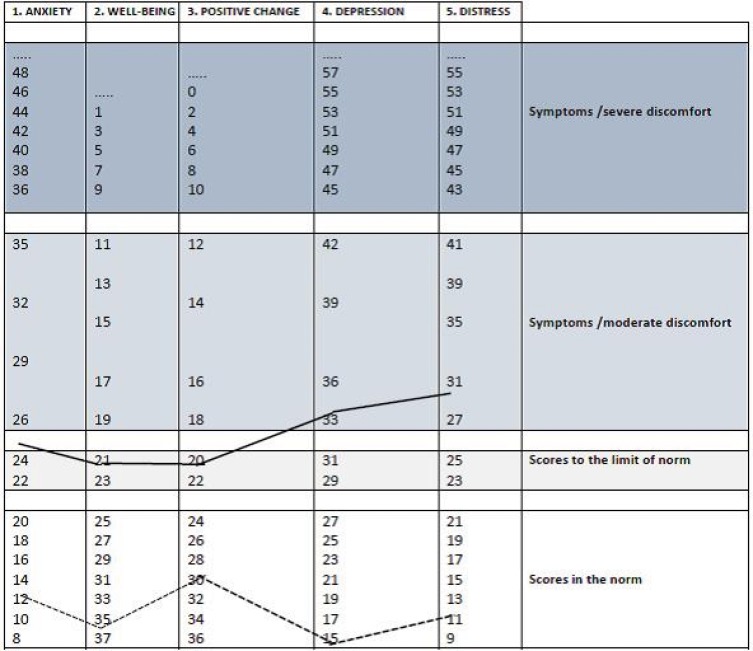
After the rehabilitation program, all symptoms of distress or psychological discomfort fell within normal values (Figure 4) as observed in our pilot study33 and the difficulties in emotion regulation also decreased, reaching values lower than the median score of the scale. With respect to the other cognitive and metacognitive variables (positive and negative alcohol beliefs and craving), we found a general significant improvement. It is likely that patients having learned to manage psychological distress without alcohol together with the intervention of rehabilitation program, have changed some of their beliefs about alcohol use. In CBT, the content of beliefs and thoughts are considered to determine the type of disorder experienced and it works mainly on the level of content of cognitions and reality tests them.31 There was also some support for the utility of the DERS for predicting treatment outcome following CBT.24 The only factor that showed no significant changes was “Cognitive Harm” perhaps also due to the increased awareness of alcohol-related health risks reached during the treatment.
Figure 4.
Clinical profile of psychological variables: T0 (admission); T1 (discharge).
Significant differences were observed between the groups “abstinence vs non-abstinence” at 1 month from discharge concerning difficulties in emotion regulation, which showed that those who relapsed were more confused about their emotional experiences, and had difficulty to identify correctly their emotions. “Emotional Clarity” seems to be the emotional difficulty that characterized also the group with a high level of craving at discharge, suggesting the importance of this function as a preliminary factor in emotion regulation.
Since emotion regulation is widely considered a main cause of alcohol abuse,34 it is interesting to explore which deficit in adaptive emotion regulation skills could be decisive for a relapse after detoxification and rehabilitation treatment. The difference between groups in the emotional clarity factor with more difficulty in this ability observed in individuals that had early relapse or had more craving at discharge could represent a fundamental target for treatment of emotion regulation skills during recovery and after discharge. The major focus on this difficulty in ER, besides these results, is an increasing number of studies that affirm a poor association of Awareness scale with the other subscales and many indices of psychopathology.27 Difficulties concerning “Emotional clarity” were found also during early abstinence in cocaine abusers,35 highlighting similarities to our sample regarding emotional disorders.
Our study has some limitations. First, the period of abstinence was limited to three weeks following withdrawal with a follow-up observation of the sample 1 month after discharge. Results are limited to the context of residential rehabilitation for alcohol addiction. Second, other variables (neuropsychological factors and biological markers) associated with alcohol abuse were not explored in this study. Finally, we did not use a control group because our intention was to explore emotional changes pre-postrehabilitation and not to test the effectiveness of treatment and it is necessary to take into consideration a potential bias in the selection criteria.
Conclusions
This study examined changes in difficulties of emotion regulation in newly abstinent alcohol-dependent subjects during inpatient rehabilitation and the possible associations with relapse at one month after discharge. The impairment of the function “Emotional Clarity” seems to represent a core factor in the early relapse of patients, as the only factor on which individuals differ on craving and relapse, suggesting the need to prioritize this emotional ability in the process of improving emotional competence. The capacity to distinguish between emotions and consequently apply adaptive coping strategies in stressful situations appears also fundamental to manage craving during alcohol abstinence.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kaufman EA, Xia M, Fosco G, Yaptangco M, Skidmore CR, Crowell SE. The Difficulties in Emotion Regulation Scale Short Form (DERS-SF): validation and replication in adolescent and adult samples. J Psychopathol Behav. 2015;38(3):443–455. doi: 10.1007/s10862-015-9529-3 [DOI] [Google Scholar]
- 2.Cox WM, Klinger E. A motivational model of alcohol use. J Abnorm Psychol. 1988;97:16–180. doi: 10.1037/0021-843X.97.2.168 [DOI] [PubMed] [Google Scholar]
- 3.Colder C, Chassin L. The stress and negative affect model of adolescent alcohol use and the moderating effects of behavioral under control. J Stud Alcohol. 1993;54:326–333. doi: 10.15288/jsa.1993.54.326 [DOI] [PubMed] [Google Scholar]
- 4.Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications? Harv Rev Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550 [DOI] [PubMed] [Google Scholar]
- 5.Norberg MM, Norton AR, Olivier J, Zvolensky MJ. Social anxiety, reasons for drinking, and college students. Behav Ther. 2010;41:555–566. doi: 10.1016/j.beth.2010.03.002 [DOI] [PubMed] [Google Scholar]
- 6.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J Psychopathol Behav Assess. 2004;26:41–54. doi: 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- 7.Dragan M. Difficulties in emotion regulation and problem drinking in young women: the mediating effect of metacognitions about alcohol use. Addict Behav. 2015;48:30–35. doi: 10.1016/j.addbeh.2015.04.008 [DOI] [PubMed] [Google Scholar]
- 8.Fox HC, Hong KA, Sinha R. Difficulties in emotion regulation and impulse control in recently abstinent alcoholics compared with social drinkers. Addict Behav. 2008;33:388–394. doi: 10.1016/j.addbeh.2007.10.002 [DOI] [PubMed] [Google Scholar]
- 9.Tice D, Bratslavsky E, Baumeister R. Emotional distress regulation takes precedence over impulse control: if you feel bad, do it! J Pers Soc Psychol. 2001;80:53–67. [PubMed] [Google Scholar]
- 10.Anand D, Chen Y, Lindquist KA, Daughters SB. Emotion differentiation predicts likelihood of initial lapse following substance use treatment. Drug Alcohol Depend. 2017;180:439–444. doi: 10.1016/j.drugalcdep.2017.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders. 4th ed. text rev Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 12.Sighinolfi C, Norcini Pala A, Chiri RL, Marchetti I, Sica C. Difficulties in emotion regulation scale (DERS): the Italian translation and adaptation. Psicoter Cogn Comport. 2010;16(2):141–170. [Google Scholar]
- 13.Giromini L, Velotti P, de Campora G, Bonalume L, Zavattini GC. Cultural adaptation of the difficulties in emotion regulation scale: reliability and validity of an Italian version. J Clin Psychol. 2012;68(9):989–1007. doi: 10.1002/jclp.21876 [DOI] [PubMed] [Google Scholar]
- 14.Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn alcohol craving scale. Alcohol ClinExp Res. 1999;23(8):1289–1295. doi: 10.1111/j.1530-0277.1999.tb04349.x [DOI] [PubMed] [Google Scholar]
- 15.Spada MM, Wells A. Metacognitive beliefs about alcohol use: development and validation of two self-report scales. AddictBehav. 2008;33(4):515–527. [DOI] [PubMed] [Google Scholar]
- 16.Di Blasi D, Benedetto L, Pacicca P. Il ruolo della metacognizione nelle manifestazioni d’ansia in preadolescenza In: Boerchi D, Camisasca E, Caravita S, et al., editors. Congresso AIP Sezione Di Psicologia Dello Sviluppo E dell’Educazione - Preatti. Milan: Vita e Pensiero; September 19–21, 2013:429–430. [Google Scholar]
- 17.Bertolotti G, Michielin P, Vidotto G, et al. Metric qualities of the cognitive behavioral assessment for outcome evaluation to estimate psychological treatment effects. Neuropsychiatr Dis Treat. 2015;11:2449–2460. doi: 10.2147/NDT.S86855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New Jersey: LEA Publishers; 1988. [Google Scholar]
- 19.Spearman C. The proof and measurement of association between two things. Am J Psychol. 1904;15:72–101. doi: 10.2307/1412159 [DOI] [PubMed] [Google Scholar]
- 20.Curtin F, Schulz P. Multiple correlations and Bonferroni’s correction. Biol Psychiatry. 1998;44(8):775–777. doi: 10.1016/s0006-3223(98)00043-2 [DOI] [PubMed] [Google Scholar]
- 21.Macdonald P. Power, type I, and type III error rates of parametric and nonparametric statistical tests. J Exp Educ. 1999;67(4):367–379. doi: 10.1080/00220979909598489 [DOI] [Google Scholar]
- 22.Becker HC. Alcohol dependence, withdrawal, and relapse. Alcohol Res Health. 2008;31(4):348–361. [PMC free article] [PubMed] [Google Scholar]
- 23.Petit G, Luminet O, Maurage F, et al. Emotion regulation in alcohol dependence. Alcoholism. 2015;39:2471–2479. doi: 10.1111/acer.12914 [DOI] [PubMed] [Google Scholar]
- 24.Hallion LS, Steinman SA, Tolin DF, Diefenbach GJ. Psychometric properties of the Difficulties in Emotion Regulation Scale (DERS) and its short forms in adults with emotional disorders. Front Psychol. 2018;9:539. doi: 10.3389/fpsyg.2018.00539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bradizza CM, Brown WC, Ruszczyk MU, Dermen KH, Lucke JF, Stasiewicz PR. Difficulties in emotion regulation in treatment-seeking alcoholics with and without co-occurring mood and anxiety disorders. Addict Behav. 2018;80:6–13. doi: 10.1016/j.addbeh.2017.12.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Salovey P, Stroud LR, Woolery A, Epel ES. Perceived emotional intelligence, stress reactivity, and symptom reports: further explorations using the Trait meta-mood scale. Psychol Health. 2002;17(5):611–627. doi: 10.1080/08870440290025812 [DOI] [Google Scholar]
- 27.Kopera M, Jakubczyk A, Suszek H, et al. Relationship between emotional processing, drinking severity and relapse in adults treated for alcohol dependence in Poland. Alcohol Alcohol. 2017;52(3):311. doi: 10.1093/alcalc/agx010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prosek EA, Giordano AL, Woehler ES, Price E, McCullough R. Differences in emotion dysregulation and symptoms of depression and anxiety among illicit substance users and nonusers. Subst Use Misuse. 2018;53(11):1915–1918. doi: 10.1080/10826084.2018.1436563 [DOI] [PubMed] [Google Scholar]
- 29.Khosravani V, Sharifi Bastan F, Ghorbani F, Kamali Z. Difficulties in emotion regulation mediate negative and positive affects and craving in alcoholic patients. Addict Behav. 2017;71:75–81. doi: 10.1016/j.addbeh.2017.02.029 [DOI] [PubMed] [Google Scholar]
- 30.Wells A. Emotional Disordersand Metacognition: Innovative Cognitive Therapy. Chichester, UK: Wiley; 2000. [Google Scholar]
- 31.Spada MM, Zandvoort M, Wells A. Metacognitions in problem drinkers. Cognit Ther Res. 2007;31(5):709–716. doi: 10.1007/s10608-006-9066-1 [DOI] [Google Scholar]
- 32.Spada MM, Caselli G, Wells A. A triphasic metacognitive formulation of problem drinking. Clin Psychol Psychother. 2013;20(6):494–500. doi: 10.1002/cpp.1791 [DOI] [PubMed] [Google Scholar]
- 33.Torselli E, Ottonello M, Franceschina E, Palagi E, Bertolotti G, Fiabane E. Cognitive and metacognitive factors among alcohol-dependent patients during a residential rehabilitation program: a pilot study. Neuropsychiatr Dis Treat. 2018;14:1907–1917. doi: 10.2147/NDT.S166669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berking M, Margraf M, Ebert D, Wupperman P, Hofmann SG, Junghanns K. Deficits in emotion-regulation skills predict alcohol use during and after cognitive-behavioural therapy for alcohol dependence. J Consult Clin Psychol. 2011;79(3):307–318. doi: 10.1037/a0023421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fox HC, Axelrod SR, Paliwal P, Sleeper J, Sinha R. Difficulties in emotion regulation and impulse control during cocaine abstinence. Drug Alcohol Depend. 2007;89(2–3):298–301. doi: 10.1016/j.drugalcdep.2006.12.026 [DOI] [PubMed] [Google Scholar]