Supplemental Digital Content is available in the text.
Abstract
Patients dissatisfied with their breast implants are faced with 2 options: secondary augmentation or removal of the implants. Simple removal of breast implants often leads to wide, deflated, and laterally displaced breasts which are notoriously difficult to reconstruct. We present a surgical technique that was specifically developed to recreate the breast mound using the wide laterally displaced breast tissue left after breast implant removal.
INTRODUCTION
Breast augmentation has consistently been one of the most commonly performed plastic surgery procedures. More than 3 million breast implants have been inserted for primary augmentation in the United States since 2005.1 Recent worldwide awareness to breast implant-associated anaplastic large cell lymphoma is understandably leading more patients to seek Plastic Surgery consultation regarding the current data and perhaps aesthetically pleasing options involving removal of the breast implants.2 Any surgeon who performs aesthetic or reconstructive breast surgery will need to become increasingly familiar with techniques to manage the explantation patient.
Multiple publications have described approaches to the breast autoaugmentation patient designed to maximize aesthetic outcomes and minimize the likelihood of complications and reoperations.3–5 Breast implant explantation leaves behind a wide deflated breast with very little breast tissue barely resembling the former breast form.3–5
The Borenstein Explantation-Pexy (BEP) technique was specifically developed to recreate the breast mound immediately after the breast implant removal using the laterally displaced breast tissue, from the “bottom up.” When applied to properly selected patients, this technique may produce an aesthetically pleasing breast without the need for a breast implant. (See Video [online], which displays the surgical procedure.)
Video. This Video displays the surgical procedure.
The Breast Is Marked as for a Vertical Scar Mastopexy
De-epithelization of a smaller area than the presurgical marking is done.
A periareolar skin incision is made followed by electrocautery dissection down to the capsule. The capsule is then entered and the implant removed. After irrigation and careful hemostasis,1,2 absorbable Vicril 0 (Johnson & Johnson Medical N.V., Diegem, Belgium) is placed between the lateral part of the capsule to just medial to the breast meridian taking a good bite of the facial thickening of the IMF and the anterior rectus sheet inferior to it, narrowing the base of the breast and creating a pleasing lateral curve. Importantly, these sutures should not be tied down before their effect on the lateral curve of the breast is assessed; if they do not produce a pleasing curve or create a dimple, they should be placed again. Then the implant pocket is closed in layers. Depending on breast tissue thickness and quality, a central area of de-epithelization or skin and subcutaneous tissue excision is performed.4,6 Inverted deep dermal sutures are put between the de-epithelialized edges of the future vertical scar. Next, the Borenstein maneuver is performed; 2 thin dermal flaps, similar to facelift skin flaps, are developed on either side of the vertical incision.2,4 Horizontal figure of 8 sutures are put at the freshly exposed breast tissue edges, narrowing the breast while adding projection. The former step is repeated as needed. When the wanted breast shape is achieved, the excess thin skin strips are cut, and the tension-free dermal edges are approximated using an absorbable intradermal suture. The patient is then seated, and an external suture is put to mark the bottom of the future areola. An inked cookie cutter is placed over the nipple-areola complex and surrounding skin to mark the new areola opening. De-epithelization of the rest of the areola opening is made, and insetting of the nipple-areola complex is completed.
DISCUSSION
Breast augmentation consistently remains the most widely performed Plastic Surgery procedure, with 313,735 performed during 2018 in the United States alone, a 4% rise from 2017. Breast implants removals (29,236) were performed during 2018 in the United States, a 6% rise from 2017.1 Recent worldwide awareness to breast implant-associated anaplastic large cell lymphoma is understandably leading more patients to seek Plastic Surgery consultation regarding the current data and perhaps aesthetically pleasing options involving removal of the breast implants.2
The BEP technique described in this article is suitable for patients with enough breast tissue to recreate a breast after explantation (Fig. 1). Patient selection is important. The ideal candidate has supple, wide breasts. This technique aims to achieve upper pole fullness and control the position of the nipple-areola complex using horizontal obliteration of dead space formerly occupied by the breast implant (Fig. 1).
Fig. 1.
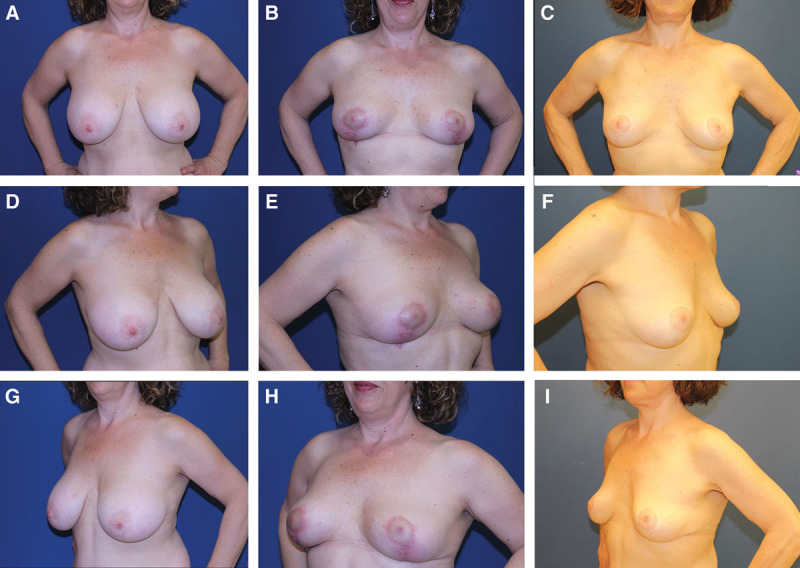
– Before and after photographs of a 45-year-old patient. A, Before BEP, AP. B, Six-month follow-up after BEP, AP. C, Six-year follow-up after BEP, AP. D, Before BEP, lateral. E, Six-month follow-up after BEP, lateral. F, Six-year follow-up after BEP, lateral. G, Before BEP, lateral. H, Six-month follow-up after BEP, lateral. I, Six-year follow-up after BEP, lateral. AP, anterior posterior.
Tips and tricks to the technique are as follows (See Video [online].):
Markings and de-epithelization are similar to those of a vertical scar mastopexy.
Periareolar incision and access enable secure closure using multiple layers, control of nipple-areola position, and IMF integrity.
The deep absorbable sutures from the lateral capsule to the IMF just medial to the breast meridian help control the lateral vector of breast ptosis.
Layered closure of the invaginated breast tissue outward to the vertical scar converts breast width to projection, aids final NAC positioning, and reduces tension of the final intradermal skin sutures.
NAC opening final de-epithelization and placement is done as the last step when the breast mound is reconstructed, and its position can be verified in a 3D manner.
There are several limitations associated with the BEP technique. First, our patient selection process excluded patients with grade IV capsular contracture or patients planned for total capsulectomy. We do, however, suspect, based on our mastopexy and reduction experience, that the method may be applied in selected cases planned for total capsulectomy if sufficient breast tissue remains. Second, patients with poor remaining breast tissue, radiated patients, and postmastectomy implant-based reconstructed patient are not candidates for this procedure. In these cases, alternative methods of breast reconstruction such as local, regional, free flaps, or multiple rounds of fat transfer may be indicated.6-8
CONCLUSIONS
Breast augmentation remains the top plastic surgery procedure performed worldwide. Natural changes in body and breast shape, device failure, malposition, and patient preference bring more patients every year to plastic surgery explantation consultations. The BEP technique is a nonimplant-based surgical option for selected patients seeking removal of their aesthetic breast implants.
Supplementary Material
Footnotes
Published online 30 September 2019
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.American Society of Plastic Surgeons. Plastic Surgery Procedural Statistics. Available at: https://www.plasticsurgery.org/documents/News/Statistics/2018/plastic-surgery-statistics-report-2018.pdf. Accessed March 23, 2019.
- 2.U.S. Food and Drug Administration. Medical Device Reports of Breast Implant-Associated Anaplastic Large Cell Lymphoma. Available at: https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/BreastImplants/ucm481899.htm. Accessed February 12, 2017.
- 3.Gurunluoglu R, Kubek E, Arton J. Dual pedicle mastopexy technique for reorientation of volume and shape after subglandular and submuscular breast implant removal. Eplasty. 2013;13:e48. [PMC free article] [PubMed] [Google Scholar]
- 4.Gurunluoglu R, Sacak B, Arton J. Outcomes analysis of patients undergoing autoaugmentation after breast implant removal. Plast Reconstr Surg. 2013;132:304–315. [DOI] [PubMed] [Google Scholar]
- 5.Hönig JF, Frey HP, Hasse FM, et al. Inferior pedicle autoaugmentation mastopexy after breast implant removal. Aesthetic Plast Surg. 2010;34:447–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graf RM, Closs Ono MC, Pace D, Balbinot P, Pazio ALB, de Paula DR. Breast auto-augmentation (Mastopexy and Lipofilling): an option for quitting breast implants. Aesthetic Plast Surg. 2019. May 7. [DOI] [PubMed] [Google Scholar]
- 7.Mess SA. Lipoaugmentation following Implant removal preferred by plastic surgeons and the general public. Plast Reconstr Surg Glob Open. 2018;6:e1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rohrich RJ, Beran SJ, Restifo RJ, et al. Aesthetic management of the breast following explantation: evaluation and mastopexy options. Plast Reconstr Surg. 1998;101:827–837. [DOI] [PubMed] [Google Scholar]


