Abstract
Acute esophageal necrosis (AEN) is a serious disease which can causes gastrointestinal bleeding and death. Although black color change is not essential factor of organ necrosis, AEN is also known as “black esophagus.” Because of its rarity, there are limited studies regarding risk factors of mortality and recurrence. Thus, we conducted a multicenter retrospective study in order to evaluate the clinical characteristics of AEN. Method Clinical datum of AEN patients from 7 tertiary hospitals located in Daejeon-Choongcheong province were evaluated based on medical records. Our primary endpoint was risk factors for mortality and the secondary endpoint was risk factors for recurrence and clarifying whether “black esophagus” is a right terminology.
Fourty one patients were enrolled. Thirty six patients were male, mean age was 69.5 years. Nine patients had died, and 4 patients showed recurrence. Sepsis and white color change in endoscopy were related to high mortality (Chi-Squared test, P < .05). Old age, high pulse rate, low hemoglobin, and low albumin were also related to high mortality. Unexpectedly, heavy drinking showed favorable a mortality. Septic condition and high pulse rate showed poor mortality in logistic regression test (P < .05). Coexisting duodenal ulcer was related to recurrence (Chi-Squared test, P < .05). There was no difference in the underlying condition except patients with a coexisting cancer and white-form displayed lower hemoglobin level. Conclusion: Our results imply that white color change, septic condition, high pulse rate, and low hemoglobin & albumin are poor prognostic factors in AEN. Further evaluation may help clarify the findings of our study.
Keywords: acute esophageal necrosis, prognostic factor, white esophagus
1. Introduction
Acute esophageal necrosis (AEN) is a rare disease characterized by gastrointestinal bleeding and characteristic endoscopic features, such as diffuse circumferential black mucosa, broad mucosal detachment, and necrotic tissue. These endoscopic findings stop abruptly at the gastroesophageal junction (GEJ).[1] Even after the first report by Goldenberg, only few studies have focused on this disease due to its rarity.[2] A systemic case series was reported in 2007 that reported the clinical features and mortality rate of AEN.[1] In this study, mortality was associated with the severity of the underlying disease. However, other clinical factors for mortality were not assessed because this study was based on literature searched from Medline and Pubmed. Clinical situations and laboratory data of patients at the time of initial admission can provide a more precise and accurate data for evaluating the association of the severity of AEN with mortality.
Another important issue regarding AEN is the term “black esophagus.” Necrosis is defined as cellular injury resulting in permanent cellular death in the living tissue by autolysis.[3] AEN has been well known as the “black esophagus” due to the associated color change. However, color change depends on location of lesion, degree of necrosis, and pattern of necrosis. One Romanian study reported acute esophageal necrosis with whitish color change associated with alcoholic hepatitis.[4] We also experienced a recurrent AEN case in a 55-year-old male patient with heavy alcoholic consumption (Fig. 1). He displayed a black esophagus and severe ulceration with whitish exudates that appeared alternatively. Thus, black color may not be an essential factor for AEN. To further understand AEN, we evaluated the risk factors of mortality and the significance of color change in AEN. We wanted to know which clinical factors (laboratory data at admission, vital signs, or underlying comorbidities) had a significant impact on the prognosis of AEN.
Figure 1.
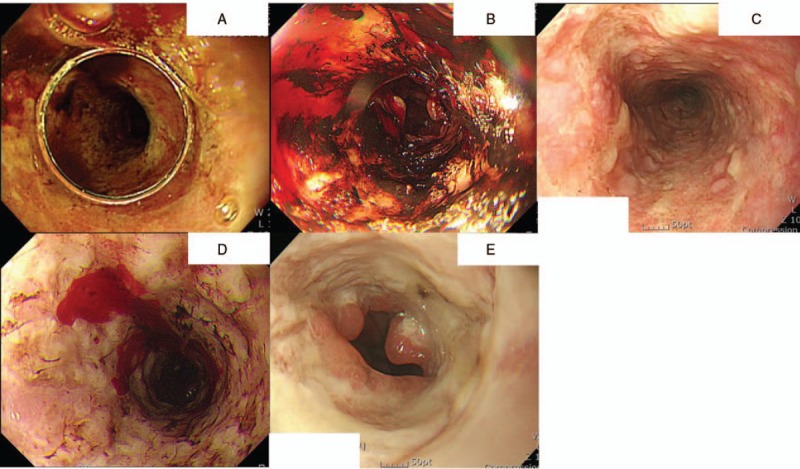
Endoscopic features of a 55-years-old-male patient who was a heavy drinker. All endoscopic images were taken at the ER with a 3 to 6 months interval. At every visit, his chief complaint was hematemesis and black and white esophageal necrosis was discovered alternatively.
2. Materials and methods
2.1. Patients and review methods
We reviewed the endoscopic data of AEN or black esophagus from the electronic medical records of 7 tertiary hospitals (Daejeon and Chungcheong province, South Korea) from January 2011 to May 2018. AEN can be misdiagnosed as severe reflux esophagitis, reflux esophagitis LA classification D degree, or corrosive esophagitis when endoscopy is performed by an inexperienced endoscopist without relevant knowledge. Thus, we also reviewed the endoscopic images of patients with these diagnoses. Researchers collected suspected cases of AEN and had discussion meetings about endoscopic pictures 3 times.
AEN was diagnosed when typical endoscopic findings are present (black color mucosal change, severe ulceration with whitish exudates, and necrotic change with mucosal detachment that stop abruptly in the GEJ) (Fig. 2). Mucosal breaks with or without ulceration, focal and shallow ulceration, and clear history of drug intoxication, such as alkali or acidic agent, were excluded. Comorbidities and laboratory and clinical data, including vital signs at the initial time of admission, were evaluated from electronic medical records. Due to our retrospective design, we could not assess exact amount of alcohol consumption. So, heavy alcohol drinker was diagnosed when patients had these clinical situations: alcoholic ketoacidosis, chronic pancreatitis, and alcoholic liver cirrhosis. Recurrence was defined as having a combination of both symptom (melena or hematemesis) and typical endoscopic findings in the follow-up endoscopy. Primary endpoint of this study was risk factors for mortality, and the secondary endpoint was risk factors of recurrence and clarifying whether the blackish discolored esophageal mucosa is essential in the diagnosis of AEN.
Figure 2.
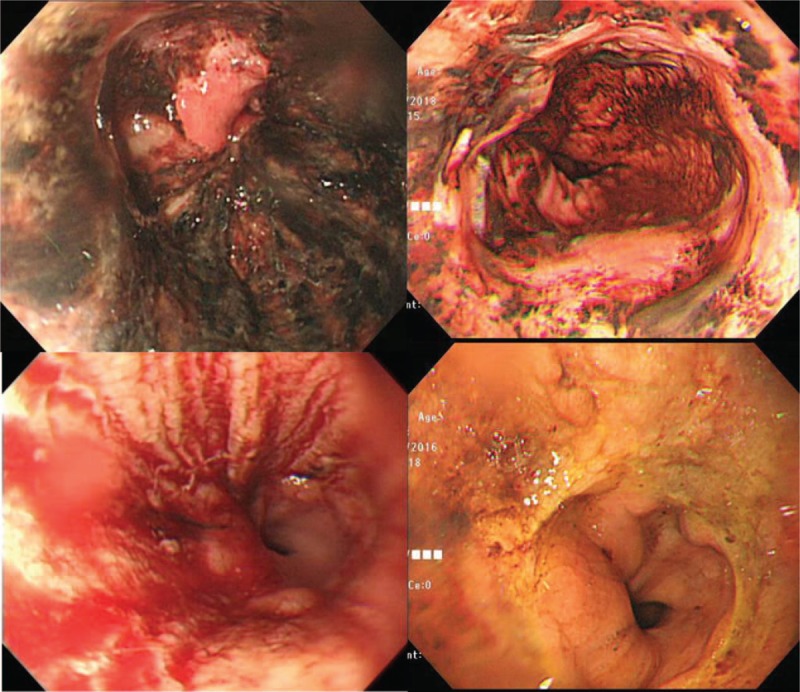
Endoscopic features of acute esophageal necrosis (AEN). Black color change (upper panel) or severe ulceration with whitish exudates (lower panel) were diagnosed with AEN.
2.2. Statistical methods
Statistical analysis was performed using the SPSS software (version 18.0, Chicago, IL, USA). The patients were divided into the survival and death groups. Univariate analysis was performed using the Chi-Squared test and Mann–Whitney U test for detection of risk factor of mortality. Color difference (black vs white) were evaluated using the same method. Multivariate logistic regression analysis was performed to calculate the odds ratio (OR) of mortality. The accepted level of statistical significance was P < .05.
2.3. Ethics statement
This study was approved by the Institutional Review Board of Chungnam National University Hospital (IRB number; 2018-11-059), and written consent was waived because of the retrospective design.
3. Results
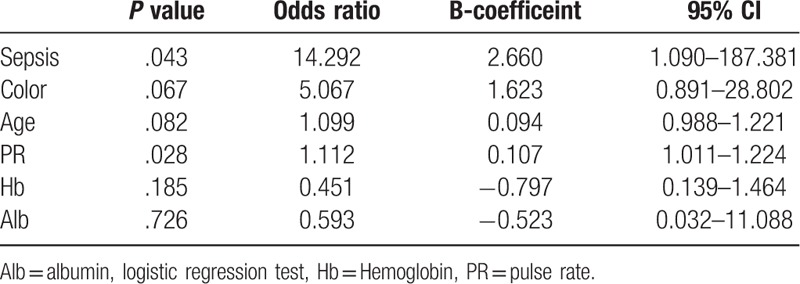
We enrolled 41 patients after reviewing the endoscopic images of 1969 patients classified with black esophagus, severe esophagitis, corrosive esophagitis, ulcer of the esophagus, burn of the esophagus, or esophageal necrosis. They had no history of intoxication with alkali or acidic agents. Thirty six patients were men, and the mean age was 69.5 years. Presumed etiologies were alcohol abuse, malignancies, sepsis, shock, pneumonia, intracranial hemorrhage, and unknown etiology (Table 1). Seven malignancies were found in our patients (3 pancreatic cancers, 1 bladder cancer, 1 gall bladder cancer, 1 cholangiocarcinoma, and 1 hepatocellular carcinoma). Nine patients died due to multi-organ failure, and 4 patients had recurrence. Gastrointestinal bleeding was the most common presenting symptom (31/41, 75.6%). Compared with survival group, septic condition and white esophageal color change were more common in the death group (Table 2). Heavy drinkers were more common in the survival group, and no difference was observed in other comorbidities between the 2 groups. The survival group consisted of younger patients and showed lower pulse rate and higher hemoglobin and albumin levels (Table 3). Logistic regression showed sepsis and pulse rate as significant factors of mortality (Table 4).
Table 1.
Demographics of patients.
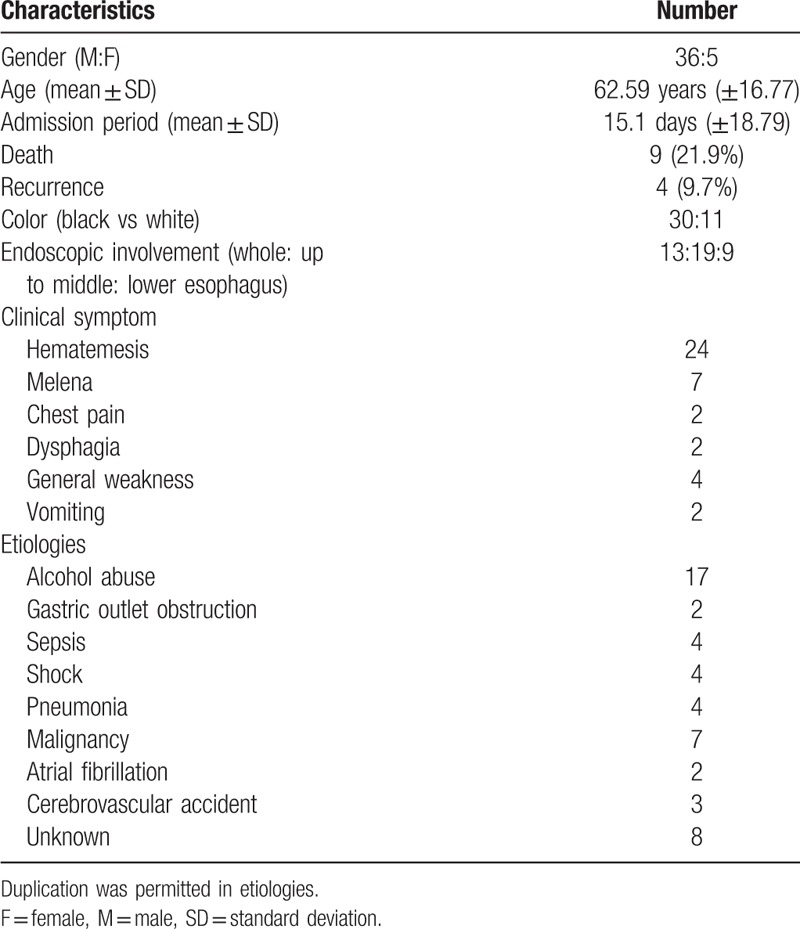
Table 2.
Factors associated with mortality (comorbidities and clinical factors).
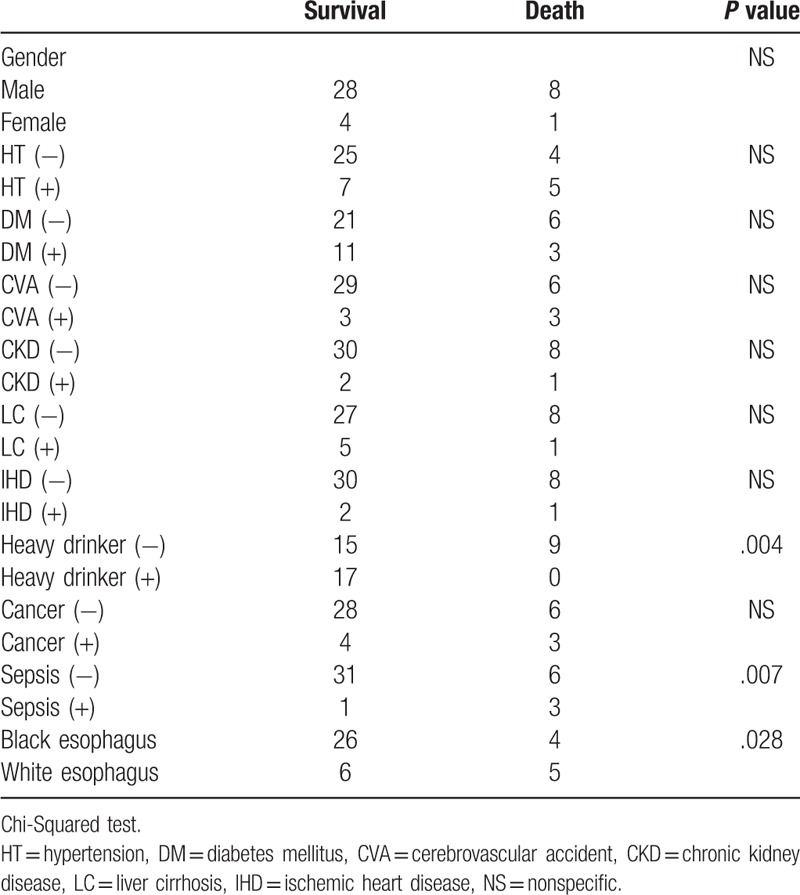
Table 3.
Factors associated with mortality (clinical situation and laboratory test at admission).
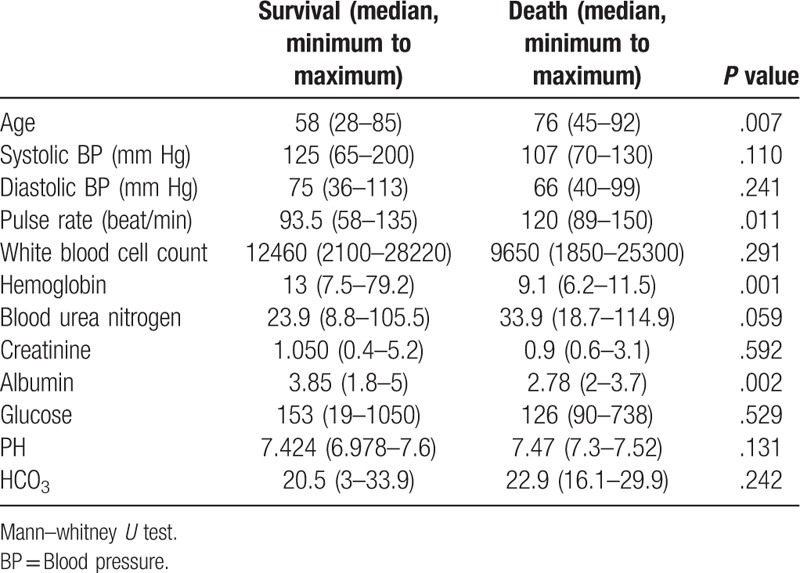
Table 4.
Multivariate analysis of mortality.
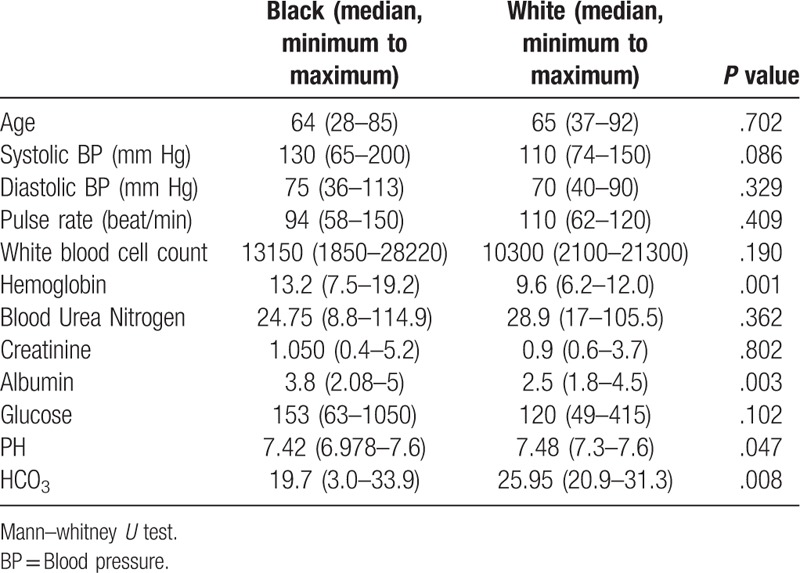
Black and white color change showed no difference in comorbidities, except for malignancy (Table 5). The white group showed lower hemoglobin and albumin levels compared with the black group (Table 6). Low hemoglobin and albumin levels at initial presentation, as well as white color change were risk factors of mortality in the univariate analysis.
Table 5.
Comparison of black vs white esophagus (comorbidities).
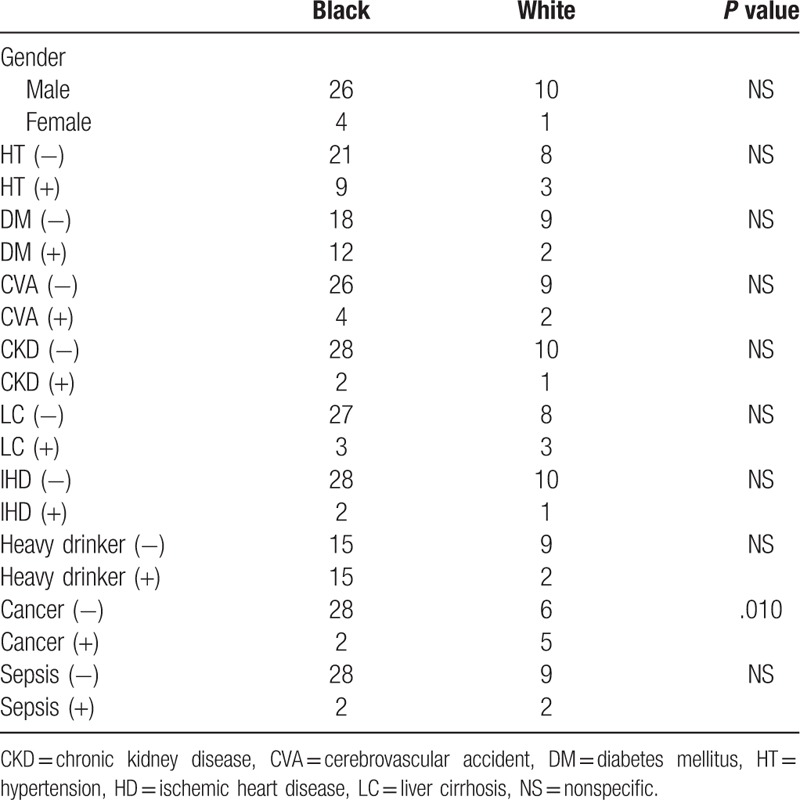
Table 6.
Comparison of black vs white esophagus (Laboratory data and clinical situation).
Four patients (4/41, 9.8%) showed recurrence. Routine follow-up endoscopy was not performed. Follow-up endoscopic evaluations were performed only in patients with symptomatic recurrences. Of 4 recurrence cases, 3 were associated with duodenal ulcer, which was statistically significant in the Chi-Squared test (3/8, 37.5% vs 1/33, 3%, P = .019).
4. Discussion
AEN is a rare disease entity that is not well characterized. Although a multicenter, international study was published in 2015, not much has been revealed due to the small number of patients.[5] The present study enrolled 41 patients after reviewing unclassified cases and “white esophagus” cases. In fact, only 15 patients were diagnosed with AEN from the beginning. Most emergent endoscopies were performed by on-duty doctors who were in their course of fellowship training. Thus, the authors had to review possible cases with a different diagnosis. Thus, the present study might have selection bias in the process of patient collection. However, all researchers of the present study were expert endoscopists with experience (having performed >10,000 cases of upper endoscopies).
In epidemiologic studies, the prevalence of AEN was 0.01% to 0.28%.[5–8] Approximately 40,000 to 45,000 upper endoscopies were performed annually in our research group. During the study, approximately 280,000 to 315,000 upper endoscopies were performed, and the prevalence rate was estimated to be approximately 0.015% in this study population.
Mortality specific to AEN was only 6% in a previous study.[1] Mortality cases of the present study was mostly due to pneumonia, sepsis, multi-organ failure, and organ perforation, which were not specific to AEN. Only 3 of 9 mortality cases were directly related to AEN in our study. Gurvits suggested that the general and underlying condition of patients were the most important factor of mortality, but specific clinical prognostic factors were not reported in previous studies.[1,9] Our present study showed that laboratory data, such as hemoglobin/albumin level, and physical data, such as age, pulse rate, and sepsis, are important prognostic factors of AEN. Hypoalbuminemia and anemia might be originated from uninvestigated liver cirrhosis. However, due to our retrospective design, we could not prove this theory. These factors may act as clinical markers that reflect the medical conditions Gurvits previously described.
The etiology of AEN is known to be diverse. Combined effects of vascular compromise, impaired defense mechanism of the esophagus, and exposure to gastric acids all contribute to AEN.[10] Alcohol abuse was a common medical history in many case reports.[11,12] There are diverse clinical situations relevant to the occurrence of AEN. Alcohol, diabetic ketoacidosis, lactic acidosis, acute cholecystitis, cellulitis, bacterial infection, and organ transplantation are related to AEN.[13–22] In a recently published systemic review, alcohol and hypertension were common comorbidities, and overall mortality rate amounted to 32%.[23] While diabetic ketoacidosis had been frequently reported, there was no case with diabetic ketoacidosis in the present study.[13,14] In a case series by Gurvits, 5.7% of patients were alcohol abusers.[1] However, there has been no consensus regarding the prognostic value of the history of alcohol abuse. Interestingly, all 17 alcohol abusers (41.5%) survived in this study population. The authors are unable to propose the exact mechanism of this phenomenon. There might be some differences in terms of the race of study populations, amount of alcohol, and the type of alcohol. Alcoholic ketoacidosis is an important cause of mortality in patients with alcohol dependence.[24] We classified alcoholic ketoacidosis, alcoholic liver cirrhosis, and chronic pancreatitis as alcohol abuse. Patients with severe alcoholic ketoacidosis and AEN might have a fatal clinical course before endoscopic evaluation. Favorable prognosis of alcohol abuse in the present study might be erroneous. In a previous multicenter international study of AEN, 2 alcohol abusers of 8 patients (25%) survived.[9]
Systemic comparison between black and white color changes of AEN was conducted in the present study. Kim et al insisted that both black and white esophagus originated from ischemic injury of the esophagus.[25] Ischemic insults of the esophagus is a major etiology of AEN.[6] The present study showed no difference in the comorbidities between black and white color changes of AEN, except for malignancy. Moreover, white color change was associated with poor prognosis. Compared with black esophagus, the mortality rate of white esophagus was higher (4/30, 13.3% vs 5/11, 45.5%, P = .028). This difference of mortality was not proven in the logistic regression test. Malignancy was more associated with a white esophagus (6/11 vs 2/30, P = .010), but other clinical factors, such as cirrhosis, renal failure, ischemic heart disease, and sepsis were not different between the 2 groups. Patients with white esophagus showed lower hemoglobin and albumin levels, which were also important prognostic factors of mortality. Thus, white esophagus may be a severe form of AEN. A recent pathologic study that compared AEN and ulcerated esophagitis concluded that the combination of basophil necrosis, intravascular thrombi, and pigment deposits can effectively diagnose AEN.[26] However, in this pathologic study, only 6 AEN cases were included. Therefore, further large-scale research is needed to confirm this result.
Our study had 4 recurrence cases in our study. Although 1 case report is found in the literature, no study was conducted on risk factors for recurrence in AEN.[27] Of 4 recurrence cases, 3 had co-existing duodenal ulcer in our study. Duodenal bulb ulcer and edema might induce gastric outlet obstruction and potentiated regurgitation of toxic acid into the esophageal mucosa.[5,28] The authors assumed that refractory duodenal ulcer might play a role in these relapsing cases of AEN.
The present study is clinically significant and impactful. The present study was the first to evaluate the risk factors for mortality in AEN, and the first to compare white and black esophagus. Second, it was the largest study to assess the risk factors of AEN to date. AEN is a rare disease; hence, conducting large, randomized controlled studies may be difficult.
Our study has several limitations. First, it was a retrospective study with a relatively small sample size. However, due to extreme rarity, it is the largest study to date. Second, we collected patient data after reviewing past endoscopic images. Thus, selection bias may be possible during patient collection. Differential diagnosis between severe esophagitis with bleeding (grade D Los Angeles classification) and AEN is difficult. Moreover, most upper endoscopies have been performed by non-experts or trainees. However, the medical records of all patients were thoroughly reviewed, and acute alkali or acidic ingestion cases were excluded. As mentioned above, all researchers were expert endoscopists. Lastly, we did not perform thrombophilic study. AEN might be due to thrombotic situation resulted in ischemia to esophageal wall and necrosis. However, due to our retrospective design, relation between thrombophilia and AEN were not evaluated.
In conclusion, mortality of AEN was associated with the clinical situation of patients, and white esophagus may be a severe form of AEN. Additional researches are necessary to clarify nature and characteristics of AEN.
Author contributions
Conceptualization: Sun Moon Kim.
Data curation: Sun Moon Kim, Kyung Ho Song, Sun Hyung Kang, Sae Hee Kim, Young Sin Cho, Ki Bae Bang.
Formal analysis: Sae Hee Kim, Young Sin Cho.
Investigation: Hee Seok Moon, Jae Kyu Sung, Seung Woo Lee.
Methodology: Sun Hyung Kang.
Project administration: Ki Bae Kim, Seung Woo Lee.
Software: Hee Seok Moon, Jae Kyu Sung.
Supervision: Sun Hyung Kang.
Validation: Ki Bae Kim.
Visualization: Ki Bae Bang.
Writing – original draft: Sun Moon Kim, Kyung Ho Song.
Writing – review & editing: Sun Moon Kim, Kyung Ho Song, Sun Hyung Kang.
Sun Hyung Kang orcid: 0000-0002-1913-4346.
Footnotes
Abbreviations: AEN = acute esophageal necrosis, GEJ = the gastroesophageal junction.
How to cite this article: Kim SM, Song KH, Kang SH, Moon HS, Sung JK, Kim SH, Kim KB, Lee SW, Cho YS, Bang KB. Evaluation of prognostic factor and nature of acute esophageal necrosis. Medicine. 2019;98:41(e17511).
SMK and KHS both authors contributed equally to this work as first author.
The authors report no conflicts of interest.
References
- [1].Gurvits GE, Shapsis A, Lau N, et al. Acute esophageal necrosis: a rare syndrome. J Gastroetnerol 2007;42:29–38. [DOI] [PubMed] [Google Scholar]
- [2].Goldenberg SP, Wain SL, Marignani P. Acute necrotizing esophagitis. Gastroenterology 1990;98:493–6. [DOI] [PubMed] [Google Scholar]
- [3].Proskuryakov SY, Konoplyannikov AG, Gabal VL. Necrosis: a specific form of programmed cell death? Cell Res 2003;283:1–6. [DOI] [PubMed] [Google Scholar]
- [4].Săftoiu A, Cazacu S, Kruse A, et al. Acute esophageal necrosis associated with alcoholic hepatitis: is it black or is it white? Endoscopy 2005;37:268–71. [DOI] [PubMed] [Google Scholar]
- [5].Gurvits GE, Cherian K, Shami MN, et al. Black esophagus: new insight and multicenter international experience in 2014. Dig Dis Sci 2015;60:444–53. [DOI] [PubMed] [Google Scholar]
- [6].Moretó M, Ojembarrena E, Zaballa M, et al. Idiopathic acute esophageal necrosis: not necessarily a terminal event. Endoscopy 1993;25:534–8. [DOI] [PubMed] [Google Scholar]
- [7].Lacy BE, Toor A, Bensen SP, et al. Acute esophageal necrosis: report of two cases and a review of the literature. Gastrointes Endosc 1999;49:527–32. [DOI] [PubMed] [Google Scholar]
- [8].Augusto E, Fernandes V, Cremers MI, et al. Acute necrotizing esophagitis: a large retrospective case series. Endoscopy 2004;36:411–5. [DOI] [PubMed] [Google Scholar]
- [9].Gurvits GE. Black esophagus: acute esophageal necrosis syndrome. World J Gastroenterol 2010;16:3219–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Averbukh LD, Mavilia MG, Curvits GE. Acute esophageal necrosis: a case series. Cureus 2018;10:e2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Shafa S, Sharma N, Keshishian J, et al. The Black esophagus: a rare but deadly disease. ACG Case Rep J 2016;3:88–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Endo T, Sakamoto J, Sato K, et al. Acute esophageal necrosis caused by alcohol abuse. World J Gastroenterol 2005;11:5568–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Field Z, Kropf J, Lytle M, et al. Black esophagus: a rare case of acute esophageal necrosis induced by diabetic ketoacidosis in a young adult female. Case Rep Gastrointest Med 2018;7363406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].McCarthy S, Garland J, Hensby-Bennett S, et al. Black esophagus (acute esophageal necrosis) and wischnewsky lesions in a death from diabetic ketoacidosis: a possible underlying mechanism. Am J Forensic Med Pathol 2019;40:192–5. [DOI] [PubMed] [Google Scholar]
- [15].Dias E, Soares N, Macedo G. Acute esophageal necrosis in association with acute cholecystitis. Rev Esp Enferm Dig 2019;111: [DOI] [PubMed] [Google Scholar]
- [16].Tanaka S, Fujishiro M, Ichijima R, et al. Acute esophageal necrosis after cellulitis in an obese patient with diabetes mellitus. J Diabetes Investig 2019;Jun 20. doi: 10.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Khan H, Ahmed M, Daoud M, et al. Acute esophageal necrosis: a view in the dark. Case Rep Gastroenterol 2019;13:25–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Tomori M, Mukaigawara M, Narita M. Acute Esophageal Necrosis Associated with Strongyloides stercoralis hyperinfection. Am J Trop Med Hyg 2019;100:1037–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Planchard JA, Dikstein AF, Koveleskie J, et al. Acute esophageal necrosis following orthotopic liver transplantation. Cureus 2019;11:e4090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Iwuji K, Jaroudi S, Bansal A, et al. Acute necrotizing esophagitis presenting with severe lactic acidosis and shock. Proc (Bayl Univ Med Cent) 2018;31:457–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Mealiea D, Greenhouse D, Velez M, et al. Acute esophageal necrosis in an immunosuppressed kidney transplant recipient: a case report. Transplant Proc 2018;50:3968–72. [DOI] [PubMed] [Google Scholar]
- [22].Haghbayan H, Sarker AK, Coomes EA. Black esophagus: acute esophageal necrosis complicating diabetic ketoacidosis. CMAJ 2018;190:E1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Abdullah HM, Ullah W, Abdallah M, et al. Clinical presentations, management, and outcomes of acute esophageal necrosis: a systemic review. Expert Rev Gastroenterol Hepatol 2019;13:507–14. [DOI] [PubMed] [Google Scholar]
- [24].McGuire LC, Cruickshank AM, Munro PT. Alcoholic ketoacidosis. Emerg Med J 2006;23:417–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Kim DB, Bowers S, Thomas M. Black and white esophagus: rare presentations of severe esophageal ischemia. Semin Thorac Cardiovasc Surg 2017;29:256–9. [DOI] [PubMed] [Google Scholar]
- [26].Jessurun J, Cui I, Aristi-Urista G. Acute (gangrenous) esophageal necrosis (black esophagus). A rare form of injury with specific histologic features and diverse clinical associations with a common pathogenesis. Hum Pathol 2019;27:44–50. [DOI] [PubMed] [Google Scholar]
- [27].Tanaka K, Toyoda H, Hamada Y, et al. A relapse case of acute necrotizing esophagitis. Endoscopy 2007;39Suppl1:E305. [DOI] [PubMed] [Google Scholar]
- [28].Ben Soussan E, Savoye G, Hochain P, et al. Acute esophageal necrosis: a 1-year prospective study. Gastrointest Endosc 2002;56:213–7. [DOI] [PubMed] [Google Scholar]


