Abstract
Background: Double-lumen bronchial tubes (DLBT) and bronchial blockers (BB) are commonly used in the anesthesia for clinical thoracic surgery. But there are few systematic clinical comparisons between them. In this study, the effects of BB and DLBT on one-lung ventilation (OLV) are studied.
Methods: The 200 patients with thoracic tuberculosis undergoing thoracic surgery, were randomly assigned to group A (DLBT) and group B (BB). Intubation time, hemodynamic changes (mean arterial pressure [MAP], heart rate [HR]), and arterial blood gas indicators (arterial partial pressure of carbon dioxide [PaCO2], arterial partial pressure of oxygen [PaO2], airway plateau pressure [Pplat], and airway peak pressure [Ppeak]) at 4 time points were recorded. Complications such as hoarseness, pulmonary infection, pharyngalgia, and surgical success rate were also evaluated postoperatively.
Results: Intubation times were shorter in group B. Both MAP and HR in group A were significantly higher 1 minute after intubation than before, but also higher than those in group B. PaO2 levels were lower in both groups during (OLV) than immediately after anesthesia and after two-lung ventilation (TLV), with PaO2 being lower after 60 minutes of OLV than after 20 minutes of OLV. Furthermore, at both points during OLV, PaO2 was lower in group A than in group B. No significant differences in PaCO2 were found between the 2 groups. Ppeak and Pplat were increased in both groups during OLV, with both being higher in group A than in group B. The incidence of postoperative hoarseness, pulmonary infection, and pharyngalgia were lower in group B. There was no significant difference in the success rate of operation between the 2 groups.
Conclusions: Compare with using DLBT, implementation of BB in general anesthesia has less impact on hemodynamics, PaO2 and airway pressures, and achieves lower incidence of postoperative complication.
Keywords: anesthesia, bronchial blockers, double-lumen bronchial tubes
1. Introduction
The main difference between one-lung ventilation (OLV) and two-lung ventilation (TLV) is that the former blocks one end of the tracheal catheter and only uses one lung for ventilation, providing a better field of vision for surgery, and isolating affected lung areas from healthier areas in order to prevent exposure to deleterious secretions.[1,2] At present, OLV is mainly used for thoracoscopic lung resection and esophagectomy.[3,4] OLV can also better control the ventilation quantity of healthy lung areas, as well as guarantee basic oxygenation and complete removal of carbon dioxide in patients during the operation. In addition, it can reduce airway peak pressure and the incidence of postoperative hoarseness, pulmonary infection, and pharyngalgia.[5,6]
Bronchial blockers (BB) are increasingly used for OLV.[7] BB positioning is aided by fiberoptic bronchoscopy and followed by insertion of a tracheal catheter into a single lung, which facilitates operation procedures and accurate positioning.[7,8] Double-lumen bronchial tubes (DLBT) can also be utilized for achieving OLV.[7] Although both methods are commonly used in the anesthesia for clinical thoracic surgery, clinical research is scarce. In this study, the effects of BB and DLBT on OLV are studied in patients with tuberculosis undergoing thoracic surgery.
2. Methods
2.1. Case selection and grouping
This study included a total of 200 patients with thoracic tuberculosis who underwent thoracic-approach debridement combined with thoracic posterior internal fixation under general anesthesia in Cangzhou Central Hospital from January 2016 to December 2017. The sample included 102 men and 98 women aged 45 to 67 years, with weights of 45 to 80 kg, heights of 150 to 180 cm, and a body mass index <30 kg/m2. All patients were classified as American Society of Anesthesiologists grade I–II.
Inclusion criteria: age >18 years, diagnosed with thoracic tuberculosis; OLV indicated and performed by the same doctor; patients who were physically fit and able to undergo thoracoscopic surgery; patients who were informed and voluntarily chose to participate in the study; preoperative respiratory function was normal, as well as heart, liver, and kidney function.
Exclusion criteria: patients unfit to undergo thoracoscopic surgery; patients with laryngopharyngeal symptoms such as hoarseness and pharyngeal pain before surgery; patients with serious systemic diseases; patients undergoing secondary thoracic surgery or who had undergone lung surgery previously; patients who received preoperative radiotherapy, chemotherapy, or immunotherapy; misalignment of bilateral lumen bronchial catheter.
The study was approved by Ethics Committee of Cangzhou Central Hospital, and all enrolled patients signed informed consent. Patients were randomly assigned into group A or group B; DLBT were used in the former, while BB were used in the latter.
2.2. Anesthesia methods
After entering the operating room, peripheral IV lines were obtained in all patients, along with initiation of the monitoring of multi-lead electrocardiograph, oxygen saturation, and blood pressure, which was measured by puncture of the left radial artery and right internal jugular vein under local anesthesia.
Anesthesia induction was performed by administering oxygen for 2 minutes, followed by intravenous injection of midazolam (2 ml, Jiangsu Enhua Pharmaceutical Co., Ltd.), propofol ( Beijing Fresenius Kabi Pharmaceutical Co. Ltd. , China), cistracurium besilate (Jiangsu Hengrui Pharmaceutical Co., Ltd., China), and fentany (Yichang Renfu Pharmaceutical Co., Ltd., China), which allowed patients to enter the anesthetic state smoothly. Next, endotracheal intubation and mechanical exhalation were performed.
Anesthesia maintenance: Intraoperative target-controlled infusion of propofol and remifentanil maintained plasma propofol concentration of 1.5 to 3.0 μg/L and remifentanil plasma concentration of 8 ng/L. At the same time, 2% sevoflurane (Jiangsu Hengrui Medicine Co., Ltd., China) and 30% oxygen inhalation combined anesthesia was maintained.
Intubation methods: Before surgery, endotracheal endoscopy was performed in both groups through x-ray chest radiographs, and appropriate DLBT or BB type were selected.
In group A (DLBT), endotracheal intubation was conducted after anesthesia induction and under direct vision by laryngoscopy, followed by insertion of the DLBT(Tampa, Hangzhou, China) (37 Fr for men, 35 Fr for women). The front end of the catheter was bent upward and inserted into the glottis, approximately 21 to 23 cm from the incisors. The tube core was pulled out, and the bronchial catheter was positioned towards the target bronchial side under the guidance of fiberoptic bronchoscopy.
In group B (BB), a single-lumen bronchial (Tampa, Hangzhou, China) tube (man: ID 7.0–7.5 mm, woman: 6.5–7.0 mm) was inserted and fixed into the patients, at a depth of 22 to 24 cm. The BB was inserted through the tracheal tube. Then, under the guidance of fiberoptic bronchoscopy, the blocking device was inserted into the carina. The fiberoptic bronchoscope was stabilized, and the end of the BB was rotated under direct observation. The BB was then pushed into the main tracheal trunk to be blocked, the cuff was inflated, and the BB was fixed with a clip. During the procedure, chest ventilation was stopped and CO2 (2 L/min) was pumped into the right thoracic cavity. Intrathoracic pressure was maintained at 8 to 10 mmHg (1 mmHg = 133.3 Pa) to induce artificial pneumothorax. Compression of the right lung was performed in order to achieve collapse. If necessary, pulmonary forceps were used to assist in the elimination of residual air in the lung.
The parameters of OLV in both groups were set at a tidal volume of 6 to 8 mL/kg and breathing frequency 12 to 16 times/min. Related parameters were adjusted according to blood oxygen saturation and blood gas analysis during operation.
Maintenance of anesthesia depth: The correlation between the anesthesia depth of propofol and BIS value is excellent, which can accurately monitor the anesthesia depth of propofol alone. The correlation between BIS and sevoflurane uptake concentration is good. When sevoflurane is used for anesthesia, it is reliable for BIS to monitor the depth of anesthesia. BIS value is 100, awake state; BIS value is 0, completely without EEG activity (cerebral cortex inhibition), generally considered that BIS value 85 to 100 is normal state; 65 to 85 is sedative state; 40 to 65 is anesthetic state; and <40 may present explosive inhibition. Anesthesia recovery: Remaining muscle relaxation should be antagonized to restore spontaneous breathing, deoxygenation in quiet state for >15 minutes. When the patient's oxygen saturation is above 95%, the tracheal tube should be removed.
2.3. Follow-up and observation indicators
The primary observation indicators: arterial partial pressure of carbon dioxide (PaCO2), arterial partial pressure of oxygen (PaO2), airway platform pressure (Pplat), and airway peak pressure (Ppeak), which were determined by blood gas analysis on samples taken from the patients’ radial artery at 4 points in time: immediately after anesthesia, at 20 minutes of OLV, at 60 minutes of OLV, and 10 minutes after recovery from TLV; the incidence of hoarseness, pharyngalgia, cough, pulmonary infections, and other adverse reactions, which were observed and recorded within 1 week after surgery; hemodynamic changes during tube positioning: mean arterial pressure (MAP) and heart rate (HR). Secondary observation indicators included intubation time, lung block time, and intraoperative bleeding.
2.4. Statistical analysis
The SPSS17.0 (SPSS Inc., Chicago, IL,USA) was used for statistical analysis of the data. The enumeration data was expressed as frequencies; the Chi-squared test was used for comparison between groups. The measurement data were expressed as means ± standard deviations. Comparisons of data from each group at each time point were performed with the t test for independent samples. Comparisons of data within each group at multiple time points were performed with Analysis of Variance combined with Bonferroni post-hoc test. Differences were considered statistically significant when P < .05.
n = σ2/(e2/Z2 + σ2/N), (95% confidence requires the statistic of Z to be 1.96, the estimated population standard deviation to be 150, and the population unit number to be 1000). Sample size calculation: (n = 150 × 150/[30 × 30/{1.96 × 1.96}] + 150 = 100 × 150/1000).
3. Results
3.1. Comparison of basic data
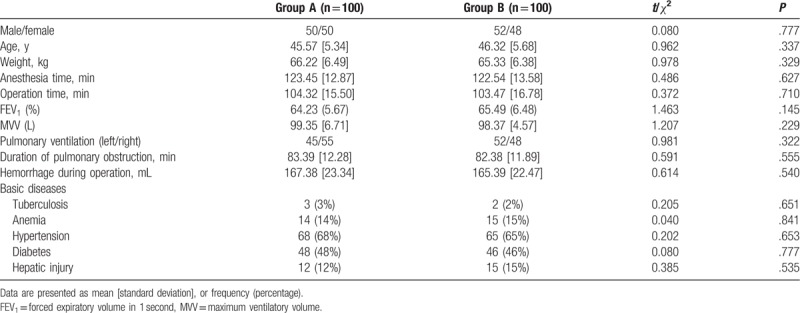
No statistically significant differences were found between the groups regarding sex ratio, age, weight, and duration of pulmonary obstruction (all P > .05, Table 1).
Table 1.
Comparison of general information.
3.2. Intubation-related indicators
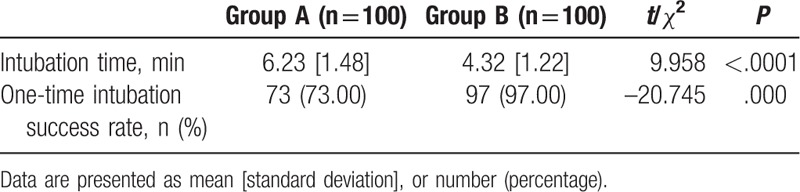
Intubation times were shorter in group B than in group A. And also there was a significantly higher one-time intubation success rate in group B in comparison to group A (both P < .05, Table 2).
Table 2.
Comparison of intubation-related indicators.
3.3. Hemodynamic changes before and after intubation
In group A, MAP and HR were found to be higher at 1 minute after intubation than before (both P < .05). In contrast, in group B, there was no statistically significant difference in MAP and HR before and after intubation (both P > .05). However, group A showed significantly lower MAP and HR at each time point compared with group B (both P < .05, Fig. 1).
Figure 1.
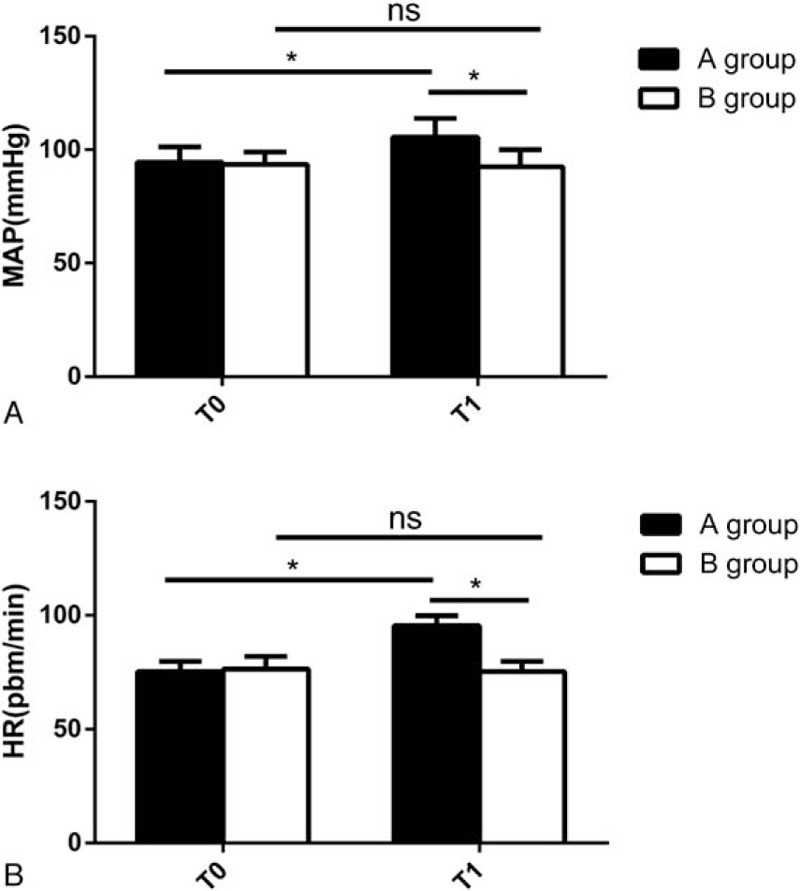
Changes of MAP and HR before and after intubation. A group: DLBT group; B group: BB group. T0: before intubation; T1: 1 minute after intubation. ∗P < .05, nsP > .05. BB = bronchial blockers, DLBT = double-lumen bronchial tubes, HR = heart rate, MAP = mean arterial pressure.
3.4. Blood gas analysis variables
In both groups, PaO2 levels during OLV were ascertained to be lower than immediately after anesthesia and after recovery from TLV in both groups, and especially PaO2 levels after 60 minutes of OLV were lower than after 20 minutes. PaO2 were found to be lower at both time point during OLV in group A than in group B (all P < .05). There were no significant differences in PaCO2 between the 2 groups at any time point (all P > .05). Ppeak and Pplat were increased immediately after anesthesia, at 20 minutes of OLV and at 60 minutes of OLV, but decreased at 10 minutes after TLV (all P < .05). In addition, Ppeak and Pplat were significantly higher in group A at 20 minutes and 60 minutes of OLV (all P < .05, Fig. 2).
Figure 2.
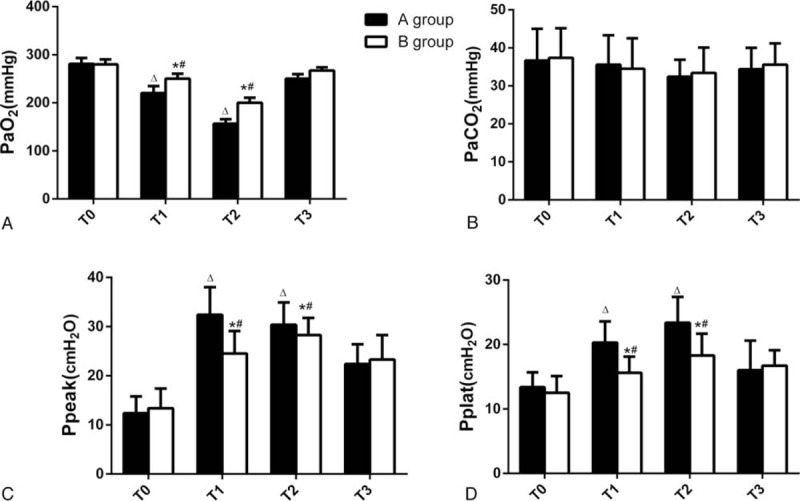
Changes of PaO2, PaCO2, Ppeak, Pplat. A group: DLBT group; B group: BB group. T0: immediately after anesthesia; T1: at 20 minutes of OLV; T2: at 60 minutes of OLV; T3: 10 minutes after recovery from TLV. ?P < .05, compared with T0 in group A; #P < .05, compared with T0 in group B; ∗P < .05, compared with group A. BB = bronchial blockers, DLBT = double-lumen bronchial tubes, OLV = one-lung ventilation, PaCO2 = arterial partial pressure of carbon dioxide, PaO2 = arterial partial pressure of oxygen, Ppeak = airway peak pressure, Pplat = airway platform pressure, TLV = two-lung ventilation.
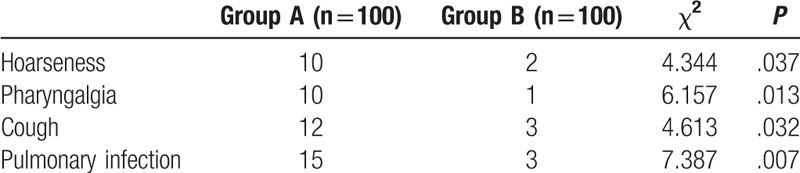
3.5. Postoperative complications
The incidence of postoperative complications was significantly lower in group B (all P < .05, Table 3).
Table 3.
Comparison of complication.
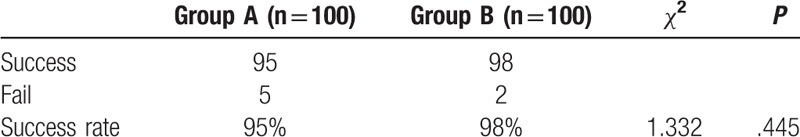
3.6. Comparison of the success rate of operation between the 2 groups
There was no significant difference in the success rate of operation between group A and group B (P = .445). See Table 4.
Table 4.
Comparison of the success rate of operation between the 2 groups.
4. Discussion
Implementation of DLBT is the most commonly used technique to achieve OLV.[9] However, clinical practice has shown this technique has relatively high requirements for operation. In addition, catheter positioning and treatment of related complications are both relatively difficult, demanding great dexterity from highly skilled physicians, and resulting in extended times for catheterization.[10]
This study found the success rate of one-time intubation to be significantly higher in the BB group than in the DLBT group. This is consistent with the results of Campos and Kernstine[11] and Ruetz et al.[12] We surmise this finding may be associated with the fact that in all the cases included in this study and the report by Cohen,[13] it was necessary to rotate the DLBT during its insertion within thoracoscopic surgery, along with its insertion into the target bronchus by blind intubation. In contrast, BB are inserted into the target healthy lung under the guidance of fiberoptic bronchoscopy, which greatly improves the success rate of one-time intubation.
We also found that in both groups, PaO2 levels during OLV were lower than immediately after anesthesia and after TLV, and PaO2 was lower after 60 minutes of OLV than after 20 minutes. PaO2 during OLV was also found to be lower in the DLBT group than in the BB group. Ppeak and Pplat were increased in both groups during OLV, being higher in the DLBT group at all time points during OLV. These results suggest utilization of BB has less impact on patients’ blood gas, especially on the PaO2, which ensures the oxygen supply of other tissues during the operation and may reduce the risk of hypoxia. This may be due to several factors: BB tube diameters are relatively smaller, and the end of the tube is flexible. Fiberoptic bronchoscopy can guide BB to the target bronchi and facilitate accurate positioning to achieve effective pulmonary collapse.[14,15]
Moreover, studies have shown that when performing OLV in a slim patient, the thinner DLBT are associated with, the greater the airway resistance will be. It hinders the improvement of oxygen saturation and the redistribution of pulmonary blood from the side under operation to the healthy side.[16–18] The BB tubes selected for this study were smaller in size than those used for DLBT, so the compression of the DLBT on the airway increased accordingly. Furthermore, because the one-time success rate of DLBT implementation is low and its positioning is cumbersome, it is often necessary to move the DLBT during intubation, further aggravating friction in the airway. This has been linked with increased incidence of discomfort in patients after the operation.[19] BB also offer better visual fields: BB retain less gas, assuring lower degree of pulmonary expansion and a wider surgical visual field; whereas DLBT are double-lumen tubes with poor ventilation which can retain much larger quantities of gas.[20] However, there are disadvantages to BB use: as the exhaust pipe and sputum suction pipe on BB are relatively thin, it is necessary to open the cuff and then the exhaust port before OLV. Therewith air in the lung is then slowly eliminated, taking a longer time than DLBT.[21] This renders BB unfit for use in patients with wet lungs, as difficulties in discharging phlegm can lead to complications such as airway obstruction and infections in patients with wet lungs. According to the blood gas analysis results of our patients, BB yields improved preservation of PaO2 in comparison to DLBT. Future studies should assess the impact of BB implementation on the incidence of hypoxic complications.
The limitations of this study include the relatively small sample size and reduced array of observation indicators. In future studies, we intend to evaluate the effect of OLV in extended periods of time; as well as assess changes in arterial xanthine oxidase levels, peroxidase activity, and polymorphonuclear count during the operation, in order to further explore the protective mechanisms of BB on OLV; and patients with heart failure affecting lung function tests were considered to be excluded.
In conclusion, we found BB implementation had less impact on blood gases when used for chest surgery, supporting it as an effective and safe technique with wide clinical applicability.
Author contributions
Conceptualization: Mengliang Zheng, Shiqiang Shan.
Formal analysis: Zhiqiang Niu, Peng Chen, Dawei Feng, Lei Wang, Zhijun Zhang.
Investigation: Zhiqiang Niu, Peng Chen.
Project administration: Mengliang Zheng, Shiqiang Shan.
Resources: Zhiqiang Niu, Benqing Wang.
Software: Lei Wang, Yu Nie, Benqing Wang, Zhijun Zhang.
Supervision: Shiqiang Shan.
Writing – original draft: Mengliang Zheng.
Writing – review & editing: Mengliang Zheng, Shiqiang Shan.
Footnotes
Abbreviations: BB = bronchial blockers, DLBT = double-lumen bronchial tubes, HR = heart rate, MAP = mean arterial pressure, OLV = one-lung ventilation, PaCO2 = arterial partial pressure of carbon dioxide, PaO2 = arterial partial pressure of oxygen, Ppeak = airway peak pressure, Pplat = airway platform pressure, TLV = two-lung ventilation.
How to cite this article: Zheng M, Niu Z, Chen P, Feng D, Wang L, Nie Y, Wang B, Zhang Z, Shan S. Effects of bronchial blockers on one-lung ventilation in general anesthesia. Medicine. 2019;98:41(e17387).
This work was supported by Cangzhou City Science and Technology Research and Development Projects (151302063).
The authors have no conflicts of interest to disclose.
References
- [1].Karzai W, Schwarzkopf K. Hypoxemia during one-lung ventilation: prediction, prevention, and treatment. Anesthesiology 2009;110:1402–11. [DOI] [PubMed] [Google Scholar]
- [2].Blank RS, Colquhoun DA, Durieux ME, et al. Management of one-lung ventilation: impact of tidal volume on complications after thoracic surgery. Anesthesiology 2016;124:1286–95. [DOI] [PubMed] [Google Scholar]
- [3].Navarromartínez J, Gálvez C, Riveracogollos MJ. Intraoperative crisis resource management during a non-intubated video-assisted thoracoscopic surgery. Ann Transl Med 2015;3:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Huang SQ, Zhang J, Zhang XX, et al. Can dexmedetomidine improve arterial oxygenation and intrapulmonary shunt during one-lung ventilation in adults undergoing thoracic surgery? A meta-analysis of randomized, placebo-controlled trials. Chin Med J (Engl) 2017;130:1707–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ku CM, Slinger P, Waddell TK. A novel method of treating hypoxemia during one-lung ventilation for thoracoscopic surgery. J Cardiothorac Vascu Anesth 2009;23:850–2. [DOI] [PubMed] [Google Scholar]
- [6].Wang KY, Yang QY, Tang P, et al. Effects of ulinastatin on early postoperative cognitive function after one-lung ventilation surgery in elderly patients receiving neoadjuvant chemotherapy. Metab Brain Dis 2017;32:427–35. [DOI] [PubMed] [Google Scholar]
- [7].Bussières JS, Somma J, Del Castillo JL, et al. Bronchial blocker versus left double-lumen endotracheal tube in video-assisted thoracoscopic surgery: a randomized-controlled trial examining time and quality of lung deflation. Can J Anaesth 2016;63:818–27. [DOI] [PubMed] [Google Scholar]
- [8].Wanat-Hawthorne A, Stubblefield J, Lynch I, et al. Successful use of a double-lumen endotracheal tube and bronchial blocker for lung isolation in pulmonary mucormycosis. J Cardiothorac Vasc Anesth 2019;33:776–80. [DOI] [PubMed] [Google Scholar]
- [9].Lu Y, Dai W, Zong Z, et al. Bronchial blocker versus left double-lumen endotracheal tube for one-lung ventilation in right video-assisted thoracoscopic surgery. J Cardiothorac Vasc Anesth 2017;32:297–301. [DOI] [PubMed] [Google Scholar]
- [10].Beam MR, Bader SO. Failure of lung isolation by a double-lumen endotracheal tube rescued by the concomitant use of an arndt bronchial blocker under direct visualization. A A Case Rep 2013;1:37–8. [DOI] [PubMed] [Google Scholar]
- [11].Campos JH, Kernstine KH. A comparison of a left-sided Broncho-Cath with the torque control blocker univent and the wire-guided blocker. Anesth Analg 2003;96:283–9. [DOI] [PubMed] [Google Scholar]
- [12].Ruetzler K, Grubhofer G, Schmid W, et al. Randomized clinical trial comparing double-lumen tube and EZ-Blocker for single-lung ventilation. Br J Anaesth 2011;56:896–902. [DOI] [PubMed] [Google Scholar]
- [13].Cohen E. Methods of lung separation. Curr Opin Anaesthesiol 2002;15:69–78. [DOI] [PubMed] [Google Scholar]
- [14].Pfitzner J, Peacock MJ, Pfitzner L. Speed of collapse of the non-ventilated lung during one-lung anaesthesia: the effects of the use of nitrous oxide in sheep. Anaesthesia 2010;56:933–9. [DOI] [PubMed] [Google Scholar]
- [15].Yoshimura T, Ueda K, Kakinuma A, et al. Bronchial blocker lung collapse technique: nitrous oxide for facilitating lung collapse during one-lung ventilation with a bronchial blocker. Anesth Analg 2014;118:666–70. [DOI] [PubMed] [Google Scholar]
- [16].El-Tahan MR, Doyle DJ, Hassieb AG. High-frequency jet ventilation using the Arndt bronchial blocker for refractory hypoxemia during one-lung ventilation in a myasthenic patient with asthma. J Clin Anesth 2014;26:570–3. [DOI] [PubMed] [Google Scholar]
- [17].Ozcan PE, Sentürk M, Sungur UZ, et al. Effects of thoracic epidural anaesthesia on pulmonary venous admixture and oxygenation during one-lung ventilation. Acta Anaesthesiol Scand 2010;51:1117–22. [DOI] [PubMed] [Google Scholar]
- [18].Neustein SM. One-lung ventilation provided by anesthesiologists having minimal experience with thoracic anesthesia. Anesthesiology 2006;105:1060. [DOI] [PubMed] [Google Scholar]
- [19].Park SH. Perioperative lung-protective ventilation strategy reduces postoperative pulmonary complications in patients undergoing thoracic and major abdominal surgery. Korean J Anesthesiol 2016;69:3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Ikeda Y, Inoue T, Ogawa E, et al. Recurrent laryngeal nerve monitoring during thoracoscopic esophagectomy. World J Surg 2014;38:897–901. [DOI] [PubMed] [Google Scholar]
- [21].Craven RM, Vanner RG. Ventilation of a model lung using various cricothyrotomy devices. Anaesthesia 2004;59:595–9. [DOI] [PubMed] [Google Scholar]


