Abstract
Osteoarthritis (OA) is a common condition of the hip. Patients with hip OA often report nocturnal pain, yet little is known how it affects sleep quality. The purpose of this paper was to assess how hip arthritis affects sleep quality. We hypothesized that hip pain caused by hip OA affects sleep quality in adult patients.
This is a prospective, cross-sectional study of patients who were diagnosed with hip OA. Patients were evaluated using Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), hip outcome score (HOS), and modified Harris hip score (mHHS). Sleep quality was assessed using Pittsburgh Sleep Quality Index (PSQI). A multiple regression model was used to assess factors associated with poor sleep quality.
A total of 106 patients were analyzed. All patients had a Tonnis grade of 2 or 3 and American Society of Anesthesiologists (ASA) classification of 2. WOMAC, HOS, and mHHS were significantly and negatively correlated with PSQI. The multiple regression model, WOMAC, short form health survey vitality, ASA classification, and history of obstructive sleep apnea were associated with poor sleep quality (R = 0.60, P < .001).
Patients with hip OA, who report a symptomatic hip, are susceptible to reduced sleep quality. There is a correlation between worsening HOSs and sleep quality. The WOMAC score is a significant predictor of poor sleep quality. Patients with poor hip metrics should be screened for sleep disturbance.
Keywords: hip, osteoarthritis, Pittsburgh Sleep Quality Index, sleep quality
1. Introduction
Over 30 million United States adults are estimated to have a diagnosis of osteoarthritis (OA), which is the most common form of arthritis.[1] The hip is a frequent site for OA and the lifetime risk for developing symptomatic hip OA is 1 in 4 people.[2] It is a multifactorial degenerative joint disease and patients usually endorse pain, stiffness, and a diminished quality of life.[3] Their symptomatic hip not only affects function but has a negative impact in other areas including mental health, vocational ability, and overall energy level.[4] Furthermore, nocturnal pain in OA may increase as the disease progresses.[5,6] Total hip arthroplasty has been shown to decrease pain, improve physical functioning, and quality of life.[7–9] Recent work supports that majority of patients seeking total joint arthroplasty desire better sleep quality.[10] Sleep has been well documented as a vital element of our daily lives and its importance in mental and physical health[11,12] and disruption in sleep habits, leading to poor quality or less hours asleep, can have detrimental effects on disability, depression, pain, and overall health.[13]
It is widely accepted that pain has a negative effect on sleep quality,[14,15] but little is known how hip pain specific to OA affects sleep. There is a lack of research-based evidence on clinical populations, describing disturbances in sleep habits using hip specific self-report outcome tools and a validated sleep quality metric. Most studies group different types of arthritis pain into a single category as opposed to individualizing affects on sleep. Additionally, current publications have looked at symptomatic OA, but lacked the detail to identify specific joint affect. OA can damage any joint, which requires studies to investigate each joint's unique impact on sleep quality. Instead of grouping OA found in multiple joints into a single category we isolated the disease strictly to the hip.
This is a prospective study assessing sleep quality in patients with hip OA measured using self-reported preoperative outcome questionnaire. We hypothesized that hip pain caused by hip OA affects sleep quality in adult patients.
2. Methods
2.1. Study design
This is a prospective, cross-sectional study of 106 consecutive patients that presented to the senior author from November 2016 to September 2017 with a chief complaint of hip pain and who were diagnosed with hip OA as their main source of symptoms before undergoing total hip replacement. Study was performed through the Department of Orthopaedic Surgery at the University of Texas Southwestern Medical Center, with institutional review board approval on November 2016, STD 122016–058. All patients were provided informed consent and voluntarily completed validated outcome measures to assess their hip function, pain, and sleep quality. The patient reported outcome metrics utilized were the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), hip outcome score (HOS), modified Harris hip score (mHHS), visual analogue pain scale (EQ-VAS), short form health survey (SF-12) and the Pittsburgh Sleep Quality Index (PSQI) were analyzed.
Hip OA was diagnosed by clinical and radiographic evaluation. Clinical diagnosis was based on the American College of Rheumatology criteria for OA of the hip.[16] Diagnosis was made if the patient endorsed hip pain, diminished hip flexion, limited internal hip rotation, pain with internal rotation of the hip, and had radiographic evidence of hip OA. Standing anteroposterior radiograph of the pelvis was assessed for Tonnis grade by the senior surgeon without prior knowledge of the patient's self-reported pain, loss of function or sleep quality. The Tonnis classification of OA was graded as 0 (no changes), 1 (widened sclerotic zone and minimal osteophyte formation), 2 (moderate loss of joint space and cyst formation), and 3 (<1 mm of joint space or no joint space).[17] Patients were excluded from the study if they were not diagnosed with hip OA as their primary pathology or had previous hip surgery in the past year.
The PSQI is a self-reported questionnaire that evaluates sleep quality and disturbance in patients during the previous month. Patients respond to 19 self-reported questions that are collectively used in evaluation of their sleep. Their responses to the questions are used to formulate 7 individual component scores as well as a final composite score that helps differentiate their sleep quality as “poor” or “good”. The 7 component scores consist of subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each of the 7 components is scaled on a 0 to 3 interval. The sum of the components produces a global score ranging from 0 to 21, where a higher score indicates poorer sleep quality. A global score greater than or equal to 5 characterize patients as poor sleepers with a diagnostic sensitivity of 89.6% and specificity of 86.5% (kappa = 0.75, P < .001).[18]
Activity, pain, and health-related quality of life outcomes were performed with use of the UCLA activity score, EQ-VAS, mHHS, WOMAC, HOS, and SF-12. All of these are validated outcome scores for assessing patients with hip OA.[19–23]
2.2. Data analysis
Continuous measures are described as either mean and standard deviation or medians and range. Categorical measures are described using frequency and percentage and ordered categorical measures described as median and range. Pearson product moment correlations were performed between hip specific reported instruments and PSQI measures. Multiple regressions were used to predict PSQI from demographic and clinical characteristics, hip specific reported instruments, and SF-12 measurements. The variables used in the multiple regression analysis included the hip reported outcome measures and were adjusted for other significant covariates. All statistical tests were checked for violations of statistical assumptions including information on outliers, normality, multicollinearity, homoscedasticity, and independence. All analyses were conducted using IBM SPSS V25 (IBM, North America, New York, NY) and significance was set at P < .05.
3. Results
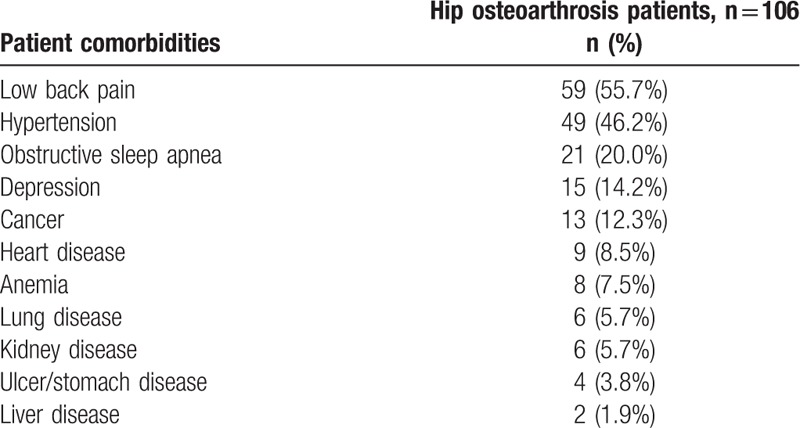
One hundred six patients were analyzed of which 63 were female. The mean age was 63 years (20–82). All patients had a Tonnis grade of 2 or 3. The median and mode for ASA physical status classification was 2 (Table 1). Concurrent comorbidities were assessed with low back pain and hypertension being the most common. Twenty percent of patients also suffered from obstructive sleep apnea and 14% had a diagnosis of depression (Table 2).
Table 1.
Patient demographics.
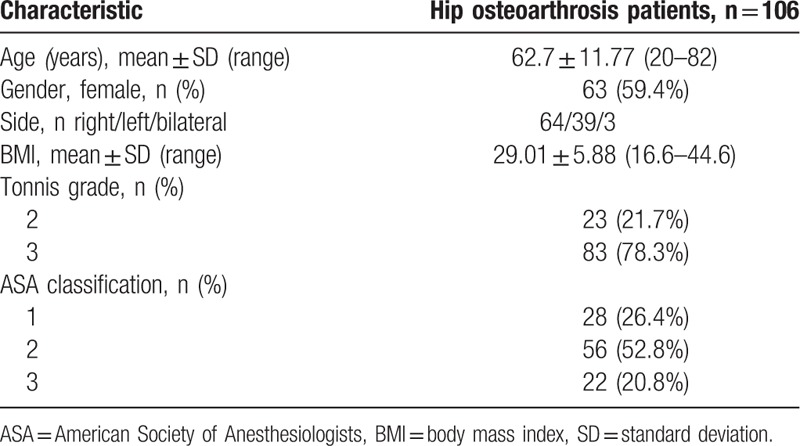
Table 2.
Comorbidity prevalence.
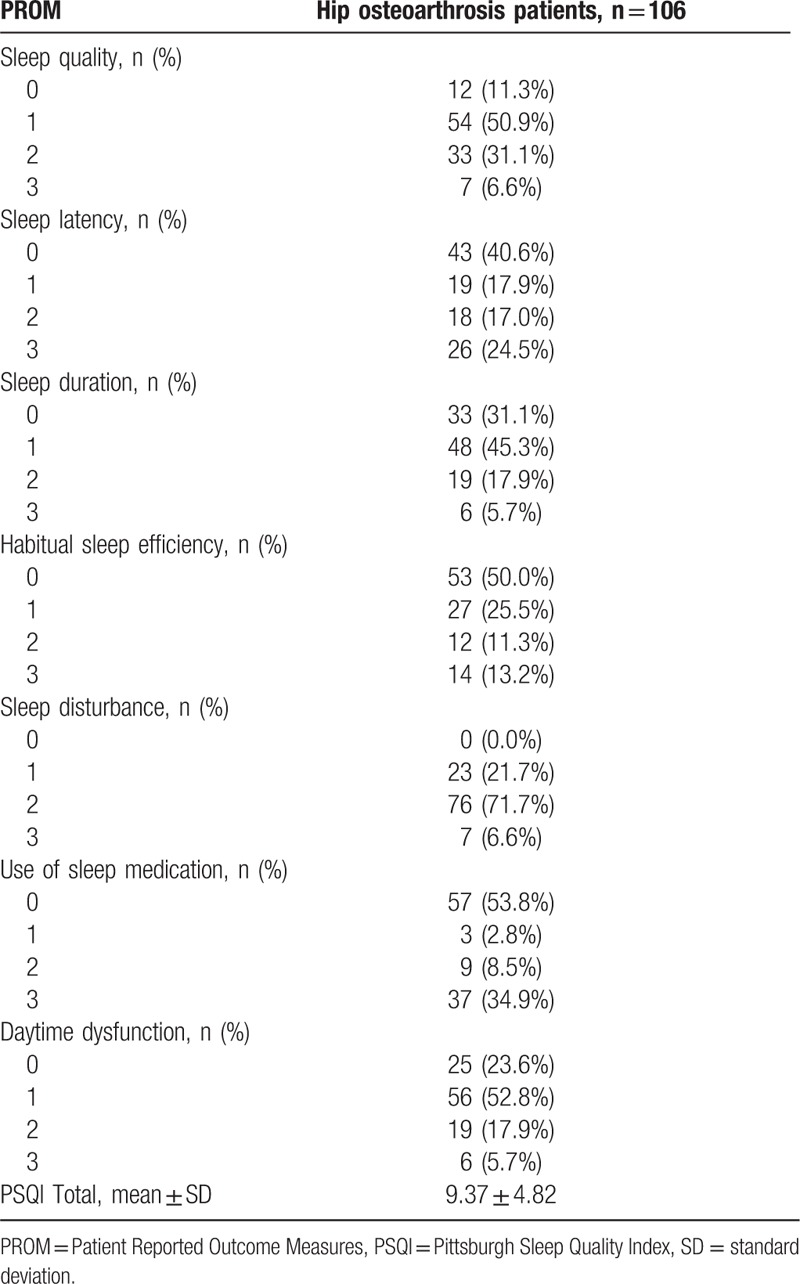
The mean mHHS, WOMAC, and HOS were 43, 41, and 44, respectively, indicating significant hip pain and diminished function (Table 3). On the SF-12, the average scores for physical function, bodily pain, role limitation due to physical health, and vitality were below 50, while scores of general health perception, social function, and mental health were above 50. The mean PSQI was 9.37, with 83% having a score of 5 or greater. The majority had some degree of dysfunction in their subcomponent scores, except for the use of prescribed or over the counter medication to aid in sleep as 53.8% denied any use in the past month. This patient cohort did report 100% of some degree of sleep disturbance. Habitual sleep efficiency was split evenly with 50% reporting issues. However, in sleep quality (88.7%), sleep latency (59.4%), sleep duration (68.9%), and daytime dysfunction (76.4%) the majority reported some level of difficulty (Table 4).
Table 3.
Patient characteristics and hip reported outcome measures.
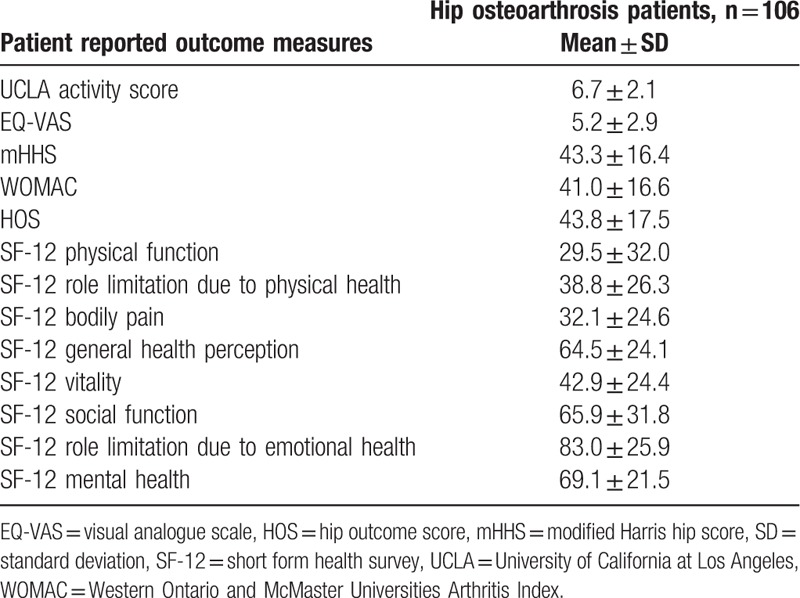
Table 4.
Pittsburgh Sleep Quality Index total and subcomponent scores.
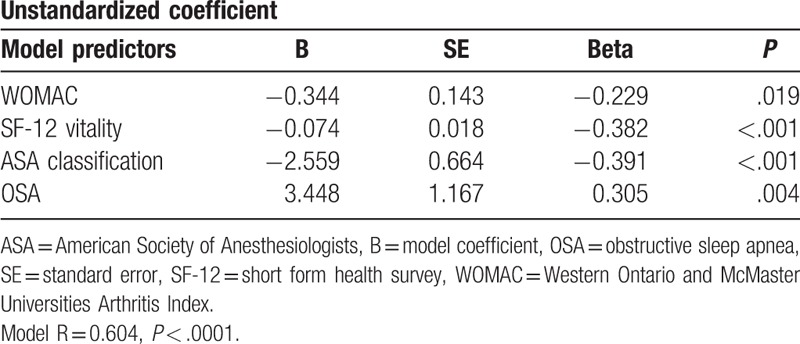
Patients with worse hip pain and dysfunction as measured by the mHHS (P = .002), WOMAC (P < .001), and HOS (P = .013) also significantly reported poor sleep quality. Pearson product moment correlation coefficients are designated as small (0.10–0.29), medium (0.30–0.49), and large (≥0.50).[24] The PSQI correlation for mHHS, WOMAC, and HOS were −0.301, −0.382, and −0.296, respectively (Table 5). Based on the multiple regression model, WOMAC, SF-12 vitality, ASA classification, and presence of obstructive sleep apnea were significant predictors of poor sleep quality (R = 0.60, P < 0.0001; P = .019, P < .001, P < .001, P = .004, respectively) (Table 6). All other multiple regression models utilizing HOS or mHHS with the model predictors resulted in nonsignificant outcomes.
Table 5.
Pearson product moment correlation of hip metrics and Pittsburgh Sleep Quality Index change.
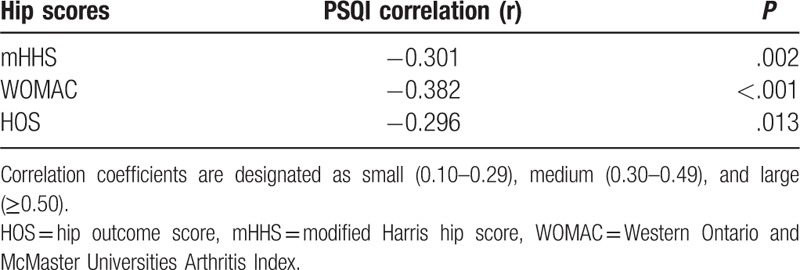
Table 6.
Multivariable model predicting Pittsburgh Sleep Quality Index.
4. Discussion
Pain and symptoms from hip OA affect sleep. All 3 patient reported outcome metrics for the hip were significant for poor sleep quality when symptomatic hip OA was present. The average total PSQI score, 9.37, was slightly under twice the indicator for poor sleep. Five or greater is the recommended benchmark for poor sleep and the majority of this patient population met the criteria at 83%. We investigated potential confounding variables, described as the patient's demographics, comorbidities, and characteristics listed in Tables 1–3, to identify if the symptomatic hip was the true reason for poor sleep and a poor WOMAC score remained an independent predictor of a high PSQI. This supports symptomatic hip OA as a major factor in reduced sleep quality. These findings are novel as it guides management for patients suffering from the chronic ailments.
Allen et al[25] found patients with hip or knee OA to be independently associated with increased odds of reporting sleep issues (odds ratio 1.25, 95% confidence interval 1.02–1.54). They risk adjusted for fair/poor health and depression finding joint OA to be independently associated with sleep problems, which support our findings that focused solely on the hip. There was no differentiation between which joint was the root cause for sleep disturbance as knee and hip OA were grouped. We aimed to delineate this uncertainty by utilizing orthopedic clinical and radiographic evaluation in diagnosing patients and specific hip outcome metrics to ensure our results were verified.
OA in other large joints has been studied to identify affect on sleep quality. Symptomatic knee OA has been found to be significantly associated with sleep disturbance, but the sleep–pain relationship was explained by baseline depressive symptoms.[26] Interestingly, when looking at symptomatic hip OA our results found a poor WOMAC score to be an independent predictor of poor sleep quality even when risk adjusted for depression. More research is needed to delineate if location of the symptomatic OA plays a critical role in depressive symptoms or other variables.
The implications of these results are an opportunity for physicians to not only address their patient's symptomatic hip OA, but potential sleep problems that can affect health and outcomes. This allows providers to take a more holistic approach when treating patients. Opening a door for the medical team to provide complete and comprehensive care instead of only treating the chief complaint and expecting the multifaceted ailments like symptomatic hip OA and poor sleep quality to resolve. Those with poor hip metrics should be screened for sleep disturbance. The positive effects of total hip arthroplasty may include a benefit to sleep quality in addition to pain control and activity. This has potential to impact patient satisfaction as it is becoming a larger component of the healthcare system's measurement of care assessment.[27] Patient's with pain show greater satisfaction about their care when the provider is more involved and offers proactive treatment options.[28] Orthopedic surgeons who spend more time counseling their patients over expected sleep quality due to their current pathology, could result in higher patient satisfaction. The more patients understand and are advised about their current health, the more autonomy over their illness they attain.
Potential limitations to this study include the use of self-reported metrics, like PSQI, to measure sleep disturbance as a more objective instrument like polysomnography or actigraphy, could possibly report different outcomes. This is important as inconsistencies are documented between subjective and objective measurements of sleep.[29] There is potential for recall bias when the patients filled out the questionnaires. Future studies should look at hip OA treatment and their affect on sleep quality. The level and type of therapy, if any, the patient is receiving for their reported comorbidities should be further investigated and stratified to see if results are affected. Furthermore, the patients should be followed longitudinally to document change in sleep quality as the disease progresses and comorbidities and patient demographics change.
5. Conclusion
Patients with hip OA, reporting a more symptomatic and painful hip, are susceptible to reduced sleep quality. There is a direct correlation between worsening patient reported HOSs and poor sleep quality. In particular, the WOMAC score is an independent predictor of poor sleep quality. Patients with poor hip metrics should be screened for sleep disturbance.
Author contributions
Conceptualization: Edward P. Mulligan, Joel Wells.
Data curation: Nisha Reddy.
Formal analysis: Linda S. Hynan.
Methodology: Linda S. Hynan, Joel Wells.
Project administration: Joel Wells.
Supervision: Joel Wells.
Writing – original draft: J. Riley Martinez.
Writing – review & editing: Edward P. Mulligan, Joel Wells.
J. Riley Martinez orcid: 0000-0001-7106-2012.
Footnotes
Abbreviations: ASA = American Society of Anesthesiologists, BMI = body mass index, EQ-VAS = visual analogue pain scale, HOS = hip outcome score, mHHS = modified Harris hip score, OA = osteoarthritis, PSQI = Pittsburgh Sleep Quality Index, SD = standard deviation, SF-12 = short form health survey, WOMAC = Western Ontario and McMaster Universities Osteoarthritis Index.
How to cite this article: Martinez R, Reddy N, Mulligan EP, Hynan LS, Wells J. Sleep quality and nocturnal pain in patients with hip osteoarthritis. Medicine. 2019;98:41(e17464).
IRB study STD 122016-058
NIH-National Center for Advancing Translational Sciences, Award Number UL1TR001105, Hoglund Foundation.
The authors have no conflicts of interest to disclose.
References
- [1].Cisternas MG, Murphy L, Sacks JJ, et al. Alternative methods for defining osteoarthritis and the impact on estimating prevalence in a US population-based survey. Arthritis Care Res 2016;68:574–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Murphy LB, Helmick CG, Schwartz TA, et al. One in four people may develop symptomatic hip osteoarthritis in his or her lifetime. Osteoarthritis Cartilage 2010;18:1372–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].American Academy of Orthopaedic Surgeons. Diseases and Conditions, Osteoarthritis of the Hip. 2014 July. Available at: https://orthoinfo.aaos.org/en/diseases--conditions/osteoarthritis-of-the-hip Accessed May 7, 2018 [Google Scholar]
- [4].Dominick KL, Ahern FM, Gold CH, Heller DA. Health-related quality of life among older adults with arthritis. Health Qual Life Outcomes 2004;2:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Woolhead G, Gooberman-Hill R, Dieppe P, Hawker G. Night pain in hip and knee osteoarthritis: a focus group study. Arthritis Care Res 2010;62:944–9. [DOI] [PubMed] [Google Scholar]
- [6].Sasaki E, Tsuda E, Yamamoto Y, et al. Nocturnal knee pain increases with the severity of knee osteoarthritis, disturbing patient sleep quality. Arthritis Care Res 2014;66:1027–32. [DOI] [PubMed] [Google Scholar]
- [7].Elmallah RK, Chughtai M, Adib F, et al. Determining health-related quality-of-life outcomes using the sf-6d following total hip arthroplasty. J Bone Joint Surg Am 2017;99:494–8. [DOI] [PubMed] [Google Scholar]
- [8].Wiklund I, Romanus B. A comparison of quality of life before and after arthroplasty in patients who had arthrosis of the hip joint. J Bone Joint Surg Am 1991;73:765–9. [PubMed] [Google Scholar]
- [9].Laupacis A, Bourne R, Rorabeck C, et al. The effect of elective total hip replacement on health-related quality of life. J Bone Joint Surg Am 1993;75:1619–26. [DOI] [PubMed] [Google Scholar]
- [10].Manning B, Kearns S, Bohl D, et al. Prospective assessment of sleep quality before and after primary total joint replacement. Orthopedics 2017;40:e636–40. [DOI] [PubMed] [Google Scholar]
- [11].Sleep Deprivation and Deficiency. National Heart Lung and Blood Institute. U.S. Department of Health and Human Services. Available at: https://www.nhlbi.nih.gov/health-topics/sleep-deprivation-and-deficiency Accessed May 7, 2018 [Google Scholar]
- [12]. [Accessed May 7, 2018]. Harvard Health Publishing. Sleep and Mental Health–Harvard Health. Harvard Health Blog 2009 July. Available at: https://www.health.harvard.edu/newsletter_article/Sleep-and-mental-health. [Google Scholar]
- [13].McCracken L, Iverson G. Disrupted sleep patterns and daily functioning in patients with chronic pain. Pain Res Manag 2002;7:75–9. [DOI] [PubMed] [Google Scholar]
- [14].Roizenblatt M, Rosa Neto NS, Tufik S, Roizenblatt S. Pain-related diseases and sleep disorders. Braz J Med Biol Res 2012;45:792–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Mulligan EP, Brunette M, Shirley Z, Khazzam M. Sleep quality and nocturnal pain in patients with shoulder disorders. J Shoulder Elbow Surg 2015;24:1452–7. [DOI] [PubMed] [Google Scholar]
- [16].Altman R, Alarcón G, Appelrouth D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 1991;34:505–14. [DOI] [PubMed] [Google Scholar]
- [17].Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am 1999;81:1747–70. [DOI] [PubMed] [Google Scholar]
- [18].Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. [DOI] [PubMed] [Google Scholar]
- [19].Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 1990;13:227–36. [DOI] [PubMed] [Google Scholar]
- [20].Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient-relevant outcomes following total hip or knee arthroplasty in osteoarthritis. J Orthop Rheumatol 1988;1:95–108. [PubMed] [Google Scholar]
- [21].McConnell S, Kolopack P, Davis AM. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum 2001;45:453–61. [DOI] [PubMed] [Google Scholar]
- [22].Martin RL, Kelly BT, Philippon MJ. Evidence of validity for the hip outcome score. Arthroscopy 2006;22:1304–11. [DOI] [PubMed] [Google Scholar]
- [23].Ware JE, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996;34:220–33. [DOI] [PubMed] [Google Scholar]
- [24].Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edHillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- [25].Allen KD, Renner JB, Devellis B, et al. Osteoarthritis and sleep: The Johnston County Osteoarthritis Project. J Rheumatol 2008;35:1102. [PMC free article] [PubMed] [Google Scholar]
- [26].Parmelee PA, Tighe CA, Dautovich ND. Sleep disturbance in osteoarthritis: linkages with pain, disability, and depressive symptoms. Arthritis Care Res 2015;67:358–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kravitz R. Patient satisfaction with health care: critical outcome or trivial pursuit? J Gen Intern Med 1998;13:280–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Bourdillon F, Tézenas du Montcel S, Collin E, et al. Determinants of patient satisfaction regarding pain care. Rev Epidemiol Sante Publique 2012;60:455–62. [DOI] [PubMed] [Google Scholar]
- [29].Dautovich ND, Kay DB, Perlis ML, et al. Day-to-day variability in nap duration predicts medical morbidity in older adults. Health Psychol 2012;31:671–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


