Abstract
Asthma is chronic inflammation of the airways characterized by airway hyper-responsiveness, wheezing, cough, and dyspnea. Asthma affects >350 million people worldwide. The Th2 immune response is a major contributor to the pathophysiology of asthma. Targeted therapy modulating cell signaling pathways can be a powerful strategy to design new drugs to treat asthma. The potential molecular pathways that can be targeted include IL-4-IL-13-JAK-STAT-MAP kinases, adiponectin-iNOS-NF-κB, PGD2-CRTH2, IFNs-RIG, Wnt/β-catenin-FAM13A, FOXC1-miR-PI3K/AKT, JNK-Gal-7, Nrf2-ROS, Foxp3-RORγt, CysLTR, AMP, Fas-FasL, PTHrP/PPARγ, PAI-1, FcɛRI-LAT-SLP-76, Tim-3-Gal-9, TLRs-MyD88, PAR2, and Keap1/Nrf2/ARE. Therapeutic drugs can be designed to target one or more of these pathways to treat asthma.
Subject terms: Immunology, Diseases, Molecular biology
Introduction
Asthma is a complex and chronic inflammatory disease of the airways characterized by airway hyper-responsiveness (AHR), eosinophilic infiltration, reversible airflow obstruction, airway remodeling, mucus hypersecretion, and goblet cell hyperplasia. The disease usually presents with wheezing, cough, and dyspnea. Allergy and atopy comprise the main causes of asthma. Genetic and environmental triggers modulating the activation and regulation of the immune system (i.e., Th2 immune response) are the main orchestrators in the pathophysiology of asthma.1,2 Asthma affects >350 million people worldwide. Owing to the heterogeneous nature of the disease, these patients usually encounter difficulties in their treatment course.3,4
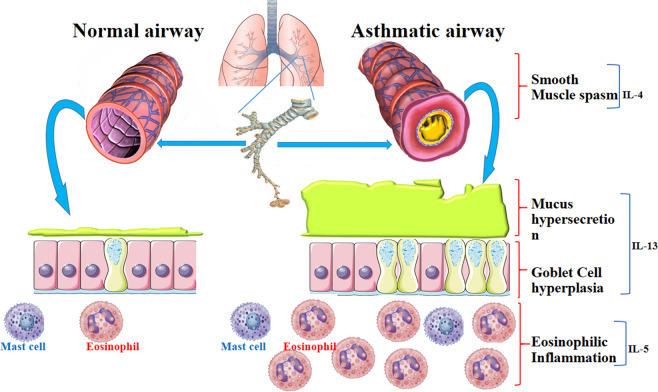
Bronchial inflammation, smooth muscle spasm, and mucus production in allergic asthma are triggered by IL-4, IL-5, and IL-13, which are released by Th2 cells. IL-13 plays the main role in the excessive secretion of mucus and AHR. IL-5 participates in the activation and migration of eosinophils to airways triggering bronchial inflammation. IL-4 induces IgE isotype switching in B cells and upregulates high-affinity IgE receptor (FcεRI) on the surface of target cells. Mast cells are activated upon allergen-induced cross-linking of FcεRI-bound IgE on their plasma membrane surface. Subsequently, mast cells release histamine and other mediators that lead to allergic symptoms. The levels of IL-4, IL-5, and IL-13 are increased in the bronchoalveolar lavage (BAL) of asthmatic patients (Fig. 1).5–8
Fig. 1.
Asthma, a chronic inflammatory airway disease, is characterized by eosinophilic inflammation, mucus hypersecretion, goblet cell hyperplasia, airway hyper-responsiveness, and breathlessness. Th2 cell immune responses are dominant in the pathophysiology of asthma. IL-4, IL-5, and IL-13 are released by Th2 cells. IL-4 has a role in B-cell IgE isotype switching and upregulation of FcεRI on mast cells, which release histamine and other mediators that lead to allergic symptoms and smooth muscle spasm. IL-5 leads to activation, migration, and accumulation of eosinophils to the airway and initiates bronchial inflammation. IL-13 has a main role in mucus hypersecretion and goblet cell hyperplasia and promotes AHR. Therefore, a focus on the mechanisms of cell signaling that are related to asthma for designing new drugs and targeted molecules can be continued with the aforementioned parameters
In recent years, targeted therapy aimed at small signaling molecules has shown promise as a novel strategy to treat diseases. Here, we reviewed cell signaling pathways and molecules that are involved in the pathogenesis of asthma and can be potential targets for developing new drugs to treat this disease. These pathways have main roles in immunomodulatory processes in asthma and are involved in the pathogenesis of all asthma clinical subtypes (i.e., intermittent, mild, moderate, and severe persistent). Acute and chronic asthma attacks can be managed by precisely identifying the regulators of these pathogenic pathways and targeting their molecular mediators.
Targeted therapy
Asthma is a multifactorial disease influenced by genetic and environmental factors. Because of its complicated nature, asthma treatment is a very difficult and exhausting process. Asthma can be categorized based on either phenotype (i.e., functional and physiopathological), severity (intermittent, mild, moderate, or severe), etiology (allergic and nonallergic or extrinsic and intrinsic), and clinical presentation (acute and chronic). Recently, there has been a focus on phenotype- and endotype-based classification approaches.9
Asthma can also be classified based on the types of inflammatory and immune cells involved. Two subtypes of inflammatory processes caused by T helper cells have recently been defined (i.e., Th2-high and Th2-low). The Th2-high subtype is characterized by marked eosinophilic infiltration of the airways, whereas the Th2-low subtype is characterized by neutrophilic infiltration.10,11 The Th2-high subtype is further associated with the predominance of type 2 cytokines (i.e., IL-4, IL-5, and IL-13). Accordingly, agents targeting the molecular participants in the Th2-high subtype (e.g., anti-IL-4, anti-IL-5, anti-IL-13, IgE blockers, and inhibitors of prostaglandin D2 (CRTH2) receptor) have recently been presented as potential drugs to treat asthma.11 Some of these targets are shown in Table 1.
Table 1.
Some of targeted therapies in control and treatment of asthma
| Target | Effects | Th2high/low | References | |
|---|---|---|---|---|
| Cell surface protein | Siglec-8 | Apoptosis of eosinophils | High | 294, 295 |
| CD300a | Activation of inhibitory receptor | High | 296 | |
| α4β1, α4β7 | Increase blood eosinophils and inhibits their tissue accumulation | High | 297 | |
| CCR3 | Block chemokine-induced eosinophils | High | 298 | |
| CXCR2 | Reduce neutrophils | Low | 16 | |
| CD52 | Deplete eosinophils | High | 299 | |
| EMR1 | Deplete primate eosinophils | High | 300 | |
| CRTH2 | Reduce tissue eosinophils | High | 301 | |
| Transcription factor | GATA3 | Reduce IL-5 | High | 302 |
| Soluble mediator antagonist | Eotaxin-1 | Inhibit eosinophil migration | High | 303, 304 |
| IgE | Reduces allergic inflammation and exacerbations and airway obstruction | High | 305, 306 | |
| IL-4 | Reduce allergic inflammation | High | 307, 308 | |
| IL-13 | Reduce airway obstruction and cough | High | 309, 310 | |
| Interleukin-17RA | Reduce Th17 response | Low | 311 | |
| TSLP | Reduce eosinophils and allergic inflammation | High | 312 | |
| PGD2 | improved Lung function | High | 313, 314 |
The Th2-low (i.e., non-Th2-driven) inflammation includes either Th1 (IFN-γ, TNF, IL-1, and IL-6) or Th17 (IL-17A, IL-17E, IL-17F, and IL-22) responses. In addition to the aforementioned molecular targets, antagonists of C-X-C-chemokine receptor (CXCR2), suppressors of IFN-γ and IL-17, as well as peroxisome proliferator-activated receptor-γ and IL-8 can be applied as novel targeting adaptors.12–16 Therefore, either allergic (i.e., Th2 high or extrinsic) or nonallergic (i.e., Th2 low or intrinsic) asthma can be treated by targeting these cell signaling mediators. The following sections briefly introduce these signaling pathways and their molecular drivers.
IL-4/IL-13 signaling pathway
The receptors of allergic cytokines, including IL-4, IL-5, IL-13, IL-31, and thymic stromal lymphopoietin (TSLP), trigger the JAK/STAT pathway.17,18 This is the main route involved in the pathogenesis of asthma.
The signaling pathways triggered by IL-4 and IL-13 recruit two distinct heterodimeric IL-4 receptors, type I IL-4R (comprising IL-4Rα and the γc common cytokine receptor chains) and type II IL-4R (comprising IL-4Rα and IL-13Rα1 chains). Although IL-4 binds to the type I receptors, IL-13 interacts with the type II IL-4Rs. The activation of both types of IL-4 receptors leads to the phosphorylation of Janus kinase (JAK) 1, Jak2, and Tyk2, activating STAT-6 transcription factors and leading to the gene expression of target inflammatory mediators.19–21 Therefore, suppressing the IL-4/IL-13 axis presents an attractive therapeutic target in asthma.
The IL-4/IL-13/STAT-6 pathway is a key modulator of asthma pathophysiology. The activation of STAT-6 can be blocked by interfering with the interaction of STAT-6-MAP kinase with ERK1/2 and p38, as well as by suppressing STAT-6 serine phosphorylation, preventing STAT-6 acetylation, and inhibiting the recruitment of the p300 transcriptional coactivator.22–25 ERK, p38 MAPK, JNK, and mTOR are serine kinases transactivating STAT-6 by phosphorylating its serine residues. Inhibitors of these adaptors can be considered as potential therapeutic agents in asthma. cAMP-response-element-binding protein-binding protein (CBP)/p300 also induces STAT-6 by phosphorylating the carboxyl terminal region of this molecule.26–29 The acetylation of STAT-6 and nuclear histones by CBP/p300 is further required for transcriptional activation of the 15-LOX-1 gene. In addition, the suppression of STAT-6 serine phosphorylation by inhibitors of p38 and MEK1/2 blocked the p300/Stat-6 interaction and suppressed IL-4/IL-13-induced expression of inflammatory chemokines such as CXCL1, CXCL3, CCL2, and CCL11 (eotaxin-1).30–32
Several therapeutics have been introduced to interfere with the IL-4/IL-13/JAK/STAT-6 pathway. These include inhibitors of JAK, dimerization suppressors, phosphopeptides targeting the SH2 domain of STAT-6, decoy oligonucleotides, siRNAs, and finally synthetic small molecules.33–36
Adiponectin signaling pathway
As a risk factor of asthma, obesity has been associated with increased airway inflammation, AHR, oxidative stress, inducible nitric oxide synthase (iNOS) expression, and elevated nitric oxide (NO) levels. On the other hand, obesity is characterized by a reduced level of adipokine, which functions as an antiinflammatory and antioxidative mediator attenuating allergic asthma severity.37–40
Adiponectin activates adiponectin receptor 1 (AdipoR1), adiponectin receptor-2 (AdipoR2), T-cadherin, and calreticulin, which are all expressed on airway epithelial cells.41,42 Adiponectin directly interacts with AdipoR1 and 2 by activating AMP-activated protein kinase (AMPK) and peroxisome proliferator-activated receptor alpha, respectively. AMPK, as a crucial energy sensor, regulates cellular metabolism (and obesity), as well as the inflammatory functions of macrophages.43–45
Nuclear factor kappa-B (NF-κB) is a part of an important inflammatory signaling pathway.26 In mammalian cells, the NF-кB family has five members, including RelA (p65), RelB, c-Rel, p50/p105 (NF-кB1), and p52/p100 (NF-кB2).46,47 According to a study by Zhu et al. in 2019, adiponectin can mitigate obesity-related asthma, improve AMPK activity, and decrease iNOS, Bcl-2, and NF-κB p65 levels within the respiratory system. These researchers showed that the level of adiponectin significantly decreased in obesity-related asthma. They also suggested that exogenous adiponectin may inhibit airway inflammation and oxidative stress in obesity-related asthma.48
Although eosinophils mainly produce eotaxin, neutrophils are the main sources of myeloperoxidase (MPO). The MPO level has been higher in obesity-related than allergic asthma, suggesting that neutrophilic and eosinophilic infiltrations are the major pathogenic processes in these subtypes, respectively. Adiponectin also downregulates the levels of both eotaxin and MPO.48
In addition, adiponectin promotes inflammatory cell apoptosis by suppressing NF-κB- and tumor necrosis factor (TNF)-α-induced expression of anti-apoptotic Bcl-2 (which contains NF-κB-binding sites in its promoter region), as well as inhibiting p50 DNA binding and p65 transactivation subunits.49–51 Adiponectin can further relieve inflammation by decreasing TNF-α production through blocking TNF-α-induced iκB-α phosphorylation and subsequent NF-κB activation.52–56 Overall, adiponectin has a main role in the control of inflammation and antioxidant processes, especially in obesity-related asthma.
Prostaglandin D2 (PGD2) receptor signaling pathway
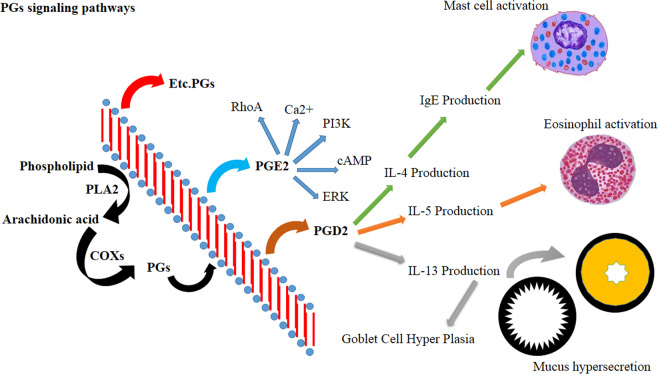
PGD2 is a proinflammatory mediator derived from arachidonic acid within the cyclooxygenase-2 (COX-2) pathway. PGD2 is released from activated immune cells, primarily from mast cells, during inflammatory reactions.57–60
PGD2 interacts with two receptors, PGD2 receptor 1 and 2 (DP1 and DP2)21, and can stimulate thromboxane receptors even at very low (µmol) concentrations. DP2 is a G-protein-coupled receptor also known as the chemoattractant receptor homologous molecule expressed on Th2 cells (CRTH2), which is expressed on the membrane surface of Th2 cells, mast cells and eosinophils.61–63 The binding of PGD2 to the DP2 receptor induces proinflammatory downstream signaling pathways culminating in the activation and migration of Th2 cells and eosinophils to the inflammatory sites in asthma.64–66 Other metabolites of PGD2, such as DK-PGD2, Δ12PGJ2, 15-deoxy- Δ12,14PGD2 and deoxy-Δ12,14PGJ2, can also activate DP2 receptors.65,67,68 The activation of the DP2 receptor on Th2 cells upregulates the expression of IL-4, IL-5, and IL-13 in a dose-dependent manner and induces Th2 migration. DP2 activation on eosinophils, on the other hand, facilitates the migration of these cells and increases eosinophil degranulation (Fig. 2).69–72
Fig. 2.
The functions of PGs and their subtypes. The subtypes of PGs have main roles in the pathophysiology of asthma. New drugs have been designed to target the PG pathway. DP2 receptor activation induces the production of proinflammatory cytokines, as well as the migration of eosinophils to the airways
In synergy with TNF-α, IL-4 enhances the expression of vascular cell adhesion molecule-1 and P selectin on vascular endothelial cells, facilitating the trans-endothelial passage of eosinophils from the blood into the respiratory system. IL-4 also stimulates the release of eotaxin, which is an eosinophil chemoattractant.73,74 IL-5 is involved in the maturation of eosinophils and inhibits apoptosis in these cells. Altogether, DP2 activation on immune cells leads to the release of IL-4, IL-5, and IL-13, which all have major roles in airway remodeling and structural damage of the pulmonary system.75–77 PGs also play important roles in allergic asthma, and their antagonists can become potent drugs for treating this condition.78
Other arachidonic acid metabolites also play a role in the pathophysiology of asthma. Increased levels of leukotriene B4 (LTB4) have been demonstrated in the BAL of asthma patients. The expression of leukotriene B4 receptor 1 (BLT1) on T cells can induce IL-13 production and promote allergic responses in airways. In accordance, asthma severity has been associated with LTB4 levels.79–82
NF-κB-iNOS-COX-2 signaling pathway
NF-κB is a ubiquitous transcription factor activated following the phosphorylation (catalyzed by IκB kinase) and dissociation of its inhibitor kappa-B subunit alpha (IκBα). NF-κB-induced iNOS and COX-2 are important mediators in the development of pulmonary inflammation. Furthermore, the expression of both iNOS and COX-2 is increased by activated NF-κB.83–86 On the other hand, iNOS and COX-2 themselves are involved in the activation of NF-κB, which can subsequently induce other inflammatory mediators and cells.87,88 Therefore, modulating iNOS and COX-2 is necessary for controlling inflammation in the lung and airways.
Interferon-virus pathway
Type I interferons (IFN-α and IFN-β) have essential roles in antiviral immune responses. Viral infections are sensed by innate immunity through pattern recognition receptors (PRRs), including Toll-like receptor 3 (TLR3), retinoic acid-inducible protein I and melanoma differentiation-associated gene 5.89–92 Zhu, et al. in 2018 reported low expression of IFN-α and IFN-β in the macrophages of airway epithelium and subepithelium in asthmatic patients. In respiratory viral infections such as rhinovirus, influenza, etc., deficiencies of IFN-α and β within the macrophages of airway epithelium and subepithelium correlated with the severities of the viral infection and asthma.93
Wnt/β-catenin signaling pathway
The Wnt signaling pathway is categorized into the canonical (β-catenin dependent) and noncanonical (β-catenin independent) pathways.58 In mammals, 19 members of the Wnt family have been recognized as having critical roles in regulating biological processes.94–96 Dysregulated Wnt signaling has been linked to the pathogenesis of airway remodeling in asthmatic patients. Intracellular aggregation and nuclear transfer of Wnt/β-catenin have further been involved in lung maturity and the development of airway smooth muscle precursor cells. The activation of the Wnt signaling pathway was also shown to accelerate the proliferation of airway smooth muscle cells, which are involved in airway remodeling.97–99
The gene encoding the family with sequence similarity 13 member A (FAM13A) has also been associated with asthma. Interestingly, FAM13A regulates β-catenin stability and augments Wnt signaling in asthma. Finally, polymorphisms in two genes related to the Wnt signaling pathway, Wnt-1-inducible-signaling pathway protein-1 and Wnt inhibitory factor-1, have been associated with persistent asthma.100–102
Vitamin D is involved in the regulation of innate and adaptive immune responses. Vitamin D deficiency exacerbates asthma severity and reduces glucocorticoid responsiveness.103–105 The bioactive form of vitamin D (1,25(OH)2D3) also promotes the translocation of β-catenin from the nucleus to the plasma membrane, represses β-catenin-TCF-4 transcriptional activity, and finally activates the transcription of the DICKKOPF-1 gene, which encodes an extracellular Wnt inhibitor.106,107 β-Catenin is crucial for adhesion to the cytoskeleton. Furthermore, vitamin D reduces the expression of Wnt5a and β-catenin and effectively inhibits the activity of the Wnt/β-catenin signaling pathway, preventing airway remodeling in asthma. Furthermore, 1,25(OH)2D3 also inhibits the proliferation of airway smooth muscle cells and reduces the content of α-SMA.108 Accordingly, elevated levels of α-SMA along with increased airway wall thickness and collagen deposition are characteristics of airway remodeling.
FOXC1-miR signaling pathway
MicroRNAs (miRNAs) are short (~ 22 nucleotides long) noncoding RNAs that are involved in the posttranscriptional regulation of genes. miRNAs target the 3′-untranslated region of mRNAs, trigger their degradation, and ultimately inhibit their translation. These small noncoding RNAs have therapeutic implications in asthma by affecting airway epithelial cells.109,110 The effects of some miRNAs on inflammatory responses are shown in Table 2.
Table 2.
The relationship of miRNA and inflammation response
| miRNA | Reaction and cell differentiate | Reference |
|---|---|---|
| miRNA-223 | Neutrophils mature and differentiate | 315 |
| miRNA-146, miRNA-146a | Airway epithelium, NF-kappa-B pathway | 316, 317 |
| miRNA-147 | TLR signaling pathway | 318 |
| miRNA-145 | Comparable to glucocorticoid treatment | 319 |
| miRNA-155 | TLR signaling pathway, regulation of allergic inflammation, macrophage inflammatory response, Th2 priming of dendritic cells | 320– 323 |
| miRNA-21 | TLR signaling pathway, NF-kB, IL-12p35 polarization | 324– 326 |
| miRNA-124 | M2 phenotype of monocytic cells | 327 |
| miRNA-148a, miR-148b, and miR-152 | HLA-G | 328, 329 |
| miRNA-126 | Th2 response, airway hyperresponse | 330 |
| let-7 | Il-13, regulation of allergic inflammation | 331– 333 |
| miRNA-221 | Mast cell activity regulates the production of cytokines | 334, 335 |
| miRNA-9 | Regulates steroid-resistant airway hyper-responsiveness | 336 |
| miRNA-672, miRNA-143 | Expression of metalloproteinase | 337 |
| miR-19a | Enhances proliferation of bronchial epithelial cells by targeting TGFbetaR2 gene | 338 |
| miRNA-203 | Negatively regulates c-Abl, ERK1/2 phosphorylation, and proliferation in smooth muscle cells | 339 |
| miRNA-133, miR-133a | Upregulation of Rhoa in bronchial smooth muscle cells | 340 |
| miR-192 | Decreased expression in peripheral blood of asthmatic individuals undergoing an allergen inhalation challenge | 341 |
| miR-212, miR-132, miR-182, miR-183 | upregulated Th17 cell differentiation | 342 |
| miR-106, miR-363 | downregulated Th17 cell differentiation | 342 |
| miR-18b, miR-106a, and miR-363-3p | expression of retinoid-related orphan receptor c (Rorc), Rora, IL-17a, and IL-17f and abolished secretion of Th17-mediated interleukin-17a (IL-17a) have declined | 342 |
| miR-18a | targeted Smad4, Hif1a, and Rora in the Th17 cell gene expression program | 343 |
| miRNA-34/449, let-7, miRNA-19, miRNA-21 and miRNA-455 | epithelial differentiation, mucus production, airway remodeling, and inflammation as well | 344 |
| miR-146a | modulate T-cell immunity as well as enhance class switch and secretion of IgE in B cells | 345 |
| miR-98 | suppress the expression of TSP1 (Thrombospondin 1) in the peripheral B cells | 330 |
| miR-221 | Upregulated expression promotes IgE-mediated activation of mast cell degranulation by PI3K/Akt/PLCgamma/Ca2+ signaling pathway | 346 |
| miR-223 | Downregulation promotes degranulation via the PI3K/Akt pathway by targeting IGF-1R in mast cells | 336 |
| miRNA-33b | Overexpression leads the mast cell degranulation was inhibited | 347 |
| miR-221 | Overexpression leads stimulated IL-4 secretion in mast cells through a pathway involving PTEN, p38, and NF-kappa-B | 348 |
| miR-223 | reduces IL-6 secretion in mast cells by inhibiting the IGF-1R/PI3K signaling pathway | 349 |
| miR-23b | induces tolerogenic DC and Treg through the inhibition of the Notch1 and NF-kB signaling pathways | 350 |
| miR-21 | regulates the Th1 and Th2 balance by targeting IL-12p35 expression and overexpression promotes differentiation of Th2 | 351, 352 |
| miR-139-5p, -15b-5p, 186-5p, 342-3p, 374a-5p, 409-3p, 454-3p, 660-5p, and -942-5p | lung function parameters (in males only) | 353– 355 |
| miR-1290, -142-3p, and 191-5p) with alone | lung function parameters (in females only) | |
| miR-296-5p, -548b-5p, -138-5p, -16-5p, -1227-3p, -30d-5p, -203a-3p and -128-3p | decreasing airway hyper-responsiveness | 356 |
| miR-143-3p | was shown to control TGF-b1-induced cell proliferation | 357, 358 |
| miR-181b-5p | was associated with airway eosinophilic inflammation by targeting osteopontin | 152, 359 |
| miR-223-3p, -142-3p and -629-3p | neutrophilic airway inflammation of the severe asthma | 360– 362 |
The phosphoinositide 3-kinase (PI3K)/AKT signaling pathway has a regulatory role in allergic asthma and could be indirectly regulated by miR-107. Forkhead box C1 (FOXC1), a hypoxia-induced transcription factor that belongs to the FOX transcription factor family, is upregulated in hypoxic lungs.111–113 Recent studies have reported that miR-200a participates in asthma pathogenesis by targeting FOXC1 through the PI3K/AKT signaling pathway. miR-200a also inhibits lung tissue fibrosis by suppressing TGF-β1-mediated endothelial-mesenchymal transition via reducing FOXC1 expression.114–117 FOXC1 activates the PI3K/AKT signaling pathway, leading to the phosphorylation and activation of several downstream proteins, such as NF-κB and GSK3-β.118,119 Cyclin D1 is an important regulator of the cell cycle activated by PI3K/AKT signaling through inhibiting p16INK4a, the cyclin D1 suppressor. Cyclin D1 participates in G1 phase of the cell cycle and induces cyclin-dependent kinase 2 (CDK2), CDK4, or CDK6.120–122 NF-κB is also a downstream molecule of the PI3K/AKT signaling pathway. The suppression of NF-κB activity through the pentaerythritol tetranitrate-Akt-IKKβ axis reduced cyclin D1 expression and suppressed cell proliferation.123,124 The recent phenomenon has therapeutic implications related to asthma by preventing proliferation and remodeling of smooth muscle cells. Accordingly, the inhibition of the PI3K/AKT signaling pathway reduced lung inflammation by decreasing the expression of IL-4, IL-6, IL-8, TNF-α, and IgE.117 Overall, miRNAs can have therapeutic applications in preventing airway inflammation by modulating FOXC1 and other signaling molecules, such as PI3K, AKT, NF-κB, cyclin D1, and TGF-β1.
JNK-Gal-7 signaling pathway
Damage to airway epithelial cells is an important component of asthma pathogenesis. TGF-β1 has been a mediator in cellular apoptosis and injury,125–127 as well as peribronchial fibrosis and airway remodeling in asthma.128,129
Galectin-7 (Gal-7) is a member of the galectin family. This molecule is expressed on epithelial cells and interacts with β-galactosides. The Gal-7 gene is induced by p53 and exerts proapoptotic effects. A high expression of Gal-7 has been noted in bronchial epithelium in asthma.130–132 Silencing Gal-7 was shown to inhibit TGF-β1-induced apoptosis in airway epithelial cells. The inhibitory effect of Gal-7 on TGF-β1-induced apoptosis has been related to the activity of caspase-3 and the induction of Bax, Bcl-2, and PARP. Gal-7 is a mitochondrial partner that can bind and inactivate Bcl-2. On the other hand, caspase-3 and its downstream substrate PARP initiate early apoptotic events. PARP cleavage is a crucial marker of the activation of functional caspases and an indicator of apoptosis in bronchial epithelial cells in asthma.133,134 Studies have shown that Gal-7 siRNA reduced caspase-3 activity, PARP cleavage, and Bax expression while increasing Bcl-2 expression.135
TGF-β also affects the JNK signaling pathway. JNK, a stress-activated protein kinase and a member of the mitogen-activated protein kinase (MAPK) family, has significant roles in the apoptotic process and airway remodeling in asthma by inducing the Wnt5a/JNK signaling pathway. TGF-β1 stimulates JNK, which phosphorylates its substrate Jun, at serine residues 63 and 73.136–139 On the other hand, silencing Gal-7 suppresses JNK activation and ameliorates bronchial epithelial cell injury, presenting a potential target for treating asthma.
Nrf2-ROS signaling pathway
Reactive oxygen species (ROS) have been associated with airway inflammation and asthma. In airways, epithelial cells and neutrophils are the main sources of ROS.140,141 The nuclear factor erythroid 2-related factor 2 (Nrf2) transcription factor is a main regulator of oxidative stress, as well as pulmonary fibrosis, by activating downstream antioxidant proteins, including NADPH quinone oxidoreductase (NQO1) and hemeoxygenase (HO-1).142,143 In addition, chronic inflammation promotes Nrf2-induced TGF-β expression, which also has a main role in the progression of pulmonary fibrosis.144 Suppressing upstream signaling pathways leading to ROS production, therefore has potential therapeutic implications in asthma.
Foxp3-RORγt signaling pathway
The proportion of CD4+CD25+ Treg cells is decreased in the peripheral blood of asthmatic patients. Some studies have noted that the imbalance of Treg/Th17 correlated with the severity of asthma.145–147 Fork-like transcription factor 3 (Foxp3) is a key transcription factor regulating Treg function and development. Differentiation of Th17 cells, on the other hand, is regulated by the nuclear orphan receptor γt (RORγt). Accordingly, the balance between Foxp3 and RORγt regulates the Treg/Th17 ratio.148,149
Long noncoding RNAs (lncRNAs) are ~ 200-nucleotide-long RNAs involved in the pathogenesis of airway inflammation and asthma. lncRNAs participate in posttranscriptional regulation of various target genes and proteins.150 lncRNAs can act as competing endogenous RNAs (ceRNAs) to bind to complementary microRNAs and prevent them from binding to their target mRNAs.151–153 In asthma, lncRNAs (i.e., ceRNAs) indirectly affect the levels of Foxp3 and RORγt by targeting their specific miRNAs and therefore contribute to the Treg/Th17 imbalance, which is a hallmark of asthma pathogenesis.154 Although lncRNAs can regulate the Treg/Th17 balance, other potential mechanisms still need to be investigated.154 In conclusion, miRNAs and lncRNAs are potential regulators of immunological responses in asthma and can have potential applications in the treatment and diagnosis of this disease.
MAPK-NF-κB signaling pathway
The NF-κB and MAPK signaling pathways regulate inflammation and immune responses in asthma by controlling the gene expression of inflammatory factors such as TNF-α and IL-6.155–157 Fengjuan et al. in 2019 showed that the nuclear translocation of phosphorylated P65, the inhibition of IκB kinase (IKK) within the NF-κB signaling pathway, and phosphorylation of ERK, JNK, and P38 MAPK (i.e., activation of the MAPK signaling pathway) can control the production of IgE and IL-4 and inhibit inflammatory mediators in asthma.158
CysLTR signaling pathways
Some evidence has shown that cysteinyl leukotrienes (CysLTs) and their receptors are among the major contributors in allergic asthma. There are two types of CysLT receptors, namely, CysLTR1 and CysLTR2, which belong to the G-protein-coupled receptor family. CysLT C4, D4, and E4 have been reported to modulate airway inflammation and remodeling.159,160 Despite its low affinity for CysLTR1 and 2, CysLT E4 is the most potent mediator evoking the influx of eosinophils and basophils and enhancing AHR and mucus secretion. Although montelukast and pranlukast are two antagonists of CysLTR1 and 2, there are no known antagonists for CysLT E4.161,162 The 2-oxoglutarate receptor 1 or GPR99 is a novel receptor for CysLT E4, and its activation increases vascular permeability independent of the CysLTR1/CysLTR2 pathway.163,164
P2Y12R is another modulator of CysLT E4-induced eosinophil degranulation and airway inflammation. Antagonists of P2Y12R suppress CysLT E4-induced eosinophil degranulation and inflammation in asthma162,165,166 and can be new candidates for managing inflammation and bronchoconstriction in this condition.
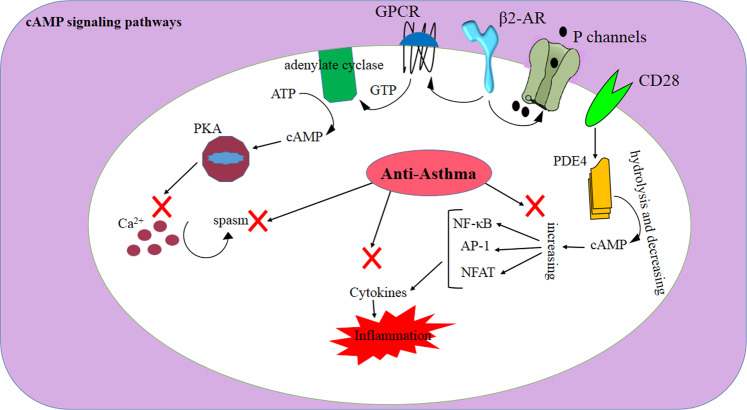
cAMP signaling pathways
Cyclic 3′5′-adenosine monophosphate (cAMP) and cyclic guanosine monophosphate (cGMP) are two main regulators of inflammation. Intracellular depletion of cAMP and cGMP following their hydrolysis by phosphodiesterase (PDE) enzymes augments inflammatory responses. In this regard, the suppression of PDE4, a subtype of PDE enzyme that is expressed in leukocytes, has promoted antiinflammatory effects in asthma.3,167–170 cAMP is also a negative regulator of T-cell activation. In this regard, PDE4 inhibitors have suppressed cytokine production by T cells, as well as biomarkers of type 2 inflammation such as periostin and serpinB2 in asthma.171,172 [173, 174]. Controlling Th2-mediated responses (i.e., the production of IL-4, IL-5, and IL-13) can have a potential therapeutic role in allergic asthma.
The activation of the costimulatory receptor CD28 induces PDE4, resulting in the hydrolysis of cAMP, the induction of NF-κB, activator protein-1 (AP-1) and NFAT, as well as the activation and proliferation of T cells. In addition, some studies showed that the level of the negative regulator of glucocorticoid receptor (GR) GRβ increased in corticosteroid-resistant asthmatic patients. The attenuated function of histone deacetylase 2 (HDAC2) further decreased GR activity, providing another corticosteroid resistance mechanism in asthma.173–175 Surpassing these glucocorticoid resistance mechanisms can be helpful in treating asthma.
β2-Agonists, which are commonly used to treat asthma, act by binding to β2-adrenoceptors (β2-AR), culminating in the activation of certain G-proteins and the generation of cAMP, which promotes smooth muscle relaxation and bronchodilation in airways.176
Similar to G-protein-coupled receptors (GPCRs), β2-AR has seven transmembrane-spanning α-helices (i.e., hepta-helical domains). This receptor couples with the Gs as a stimulatory G-protein, which is a trimeric complex consisting of one A subunit that induces adenylate cyclase (AC) and two BG subunits transducing other signals. The A subunit further activates AC, and AC catalyzes the conversion of ATP to cAMP. Subsequently, cAMP phosphorylates protein kinase A (PKA), which in turn phosphorylates other regulatory proteins involved in airway smooth muscle spasm, regulation of intracellular calcium, and bronchodilation. Nevertheless, some studies have proposed that the relaxation effect of β2-agonists might be directly mediated through the interaction of Gs with potassium channels on the plasma membrane of airway smooth muscle cells (i.e., cAMP independent pathway)176,177 (Fig. 3). Overall, the β2-AR pathway provides another viable therapeutic target in asthma.
Fig. 3.
The cAMP signaling pathway and its relationships with β2-AR, GPCR, and potassium channels. cAMP is a negative regulator of T-cell activation. Along with PDE4 inhibitors, cAMP can suppress cytokine production
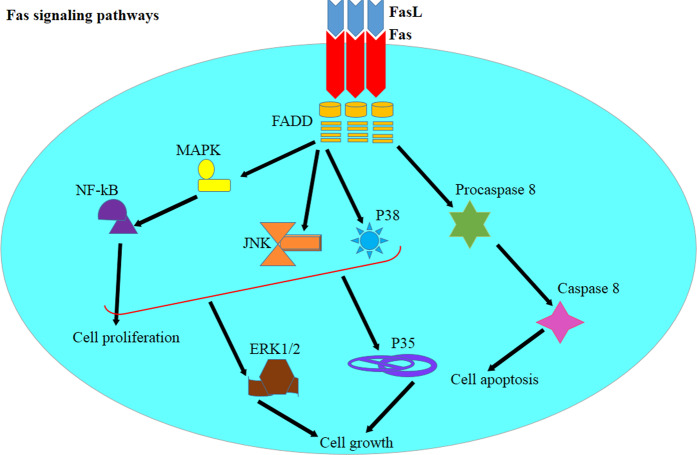
Fas-FasL signaling pathways
Fas is a member of the TNF receptor family that is involved in activation-induced cell death. Fas-mediated signaling is defective in asthma, leading to delayed resolution of inflammation. It has been shown that the expression of FasL was augmented following exposure to allergens. However, the Fas expressed on the surface of pulmonary T cells has been less sensitive to Fas-mediated apoptosis in asthma. Furthermore, the number of cells expressing the Bcl-2 antiapoptotic molecule was increased in asthmatic patients and correlated with asthma severity. Fas has also been described to regulate Th2-mediated inflammation.178–180
Fas initiates two apoptotic and nonapoptotic signaling cascades.181,182 In the apoptosis pathway, Fas ligation changes its conformational structure, allowing signaling molecules (i.e., FADD, cFLIP, and procaspase-8) to bind to the intracellular C-terminal signaling death domain of the receptor.183 The recruitment of these proteins leads to the formation of the death-inducing signaling complex, which induces the internalization of the receptor, and apoptotic reactions ensure via either caspase- or mitochondrial-mediated cascades. The Fas-mediated nonapoptotic signaling pathway involves a variety of signaling cascades independent of the death-promoting pathway.184 Fas-mediated FADD triggers the MAPK signaling cascade, which subsequently induces NF-kB translocation, as well as cell proliferation and migration.185–187 The manipulation of the Fas signaling pathway also modulates JNK, NF-kB, p38, and nonapoptotic Fas signaling pathways via both ERK1/2 and p35.185,188 Studies have described that Th2 cells are resistant to Fas-mediated apoptosis and NF-kB activation following treatment with FasL. The resistance of Th2 cells to FasL-mediated apoptosis has been attributed to the augmented baseline activities of FLIP, TRAIL, and NF-kB in these cells.189,190
Fas-mediated nonapoptotic pathways triggered by Th2 cells may also contribute to lung inflammation. Modulating Fas signaling in Th2 cells is necessary for suppressing type 2 inflammation; however, discerning Fas signaling triggered by Th2 cells is difficult from the signaling pathway originating from other T-cell populations (Fig. 4).190 Nonetheless, using antagonists to target Fas-FasL pathways may negatively affect the function of other immune cells, and more studies are warranted to resolve this issue.
Fig. 4.
The Fas-FasL pathway and its roles in cell death and cell survival. Fas signaling via the FADD adaptor triggers the MAPK signaling cascade, leading to NF-kB activation and cellular proliferation. Th2 cells are resistant to Fas-mediated apoptosis, as well as to the activation of NF-kB following attachment of FasL. Fas signaling is necessary for the resolution of type 2 inflammation. Nonapoptotic Fas signaling in Th2 cells further contributes to lung inflammation
PTHrP/PPARγ signaling pathway
Parathyroid-hormone-related protein (PTHrP) and prostaglandin E2 are secreted by alveolar type II (ATII) cells in the physiological state. Peroxisome proliferator-activated receptor gamma (PPARγ) (also known as glitazone receptor or nuclear receptor subfamily 1, group C, member 3- NR1C3-) is a type II nuclear receptor. The PTHrP/PPARγ signaling pathway has been reported to participate in nicotine-induced pulmonary dysplasia in offspring.191
Binding of PPARγ to PTHrP induces the transformation of lung fibroblasts into lipofibroblasts by absorbing neutral lipids. This interaction also upregulates PPARγ via activation of protein kinase A (PKA). PPARγ further promotes downstream adipocyte differentiation-related protein and induces lipofibroblasts and ATII cells to absorb triglycerides and secrete leptin. After the binding of leptin to ATII cells, surfactant is produced to ensure normal lung function.191,192 Downregulation of PPARγ induces the trans-differentiation of lipofibroblasts to myofibroblasts and dysregulates the differentiation of ATII cells, leading to decreased production of surfactants and therefore abnormal lung development.192 Although PPARγ agonists can support normal lung function and inhibit dyspnea, they can modulate the PTHrP-PPARγ pathway, resulting in pulmonary dysfunction, especially in allergic asthma.
PAI-1 signaling pathway
Plasminogen activator inhibitor-1 (PAI-1) has been associated with asthma severity and airway remodeling. Tissue-type plasminogen activator (t-PA) or urokinase type PA (u-PA) converts plasminogen to plasmin. Plasminogen activators are involved in the dissolution of fibrin polymers and the degradation of extracellular matrix (ECM) components.193,194 PAI-1 can inhibit both t-PA and u-PA. PAI-1 deficiency prevents ECM deposition and reduces airway inflammation and remodeling, as well as AHR.195,196 Therefore, focusing on PAI-1 antagonists can be a viable therapeutic strategy in asthma.
FcɛRI signaling pathway
Basophils express high-affinity IgE receptor (FcɛRI) on their plasma membrane. The activation of FcɛRI leads to the release of chemical mediators such as histamine. Basophils drive the differentiation of naive T cells to Th2 cells in lymph nodes by producing TSLP and IL-4 in response to protease allergens. Basophils also augment humoral memory responses through stimulation of memory B and T cells.197–200
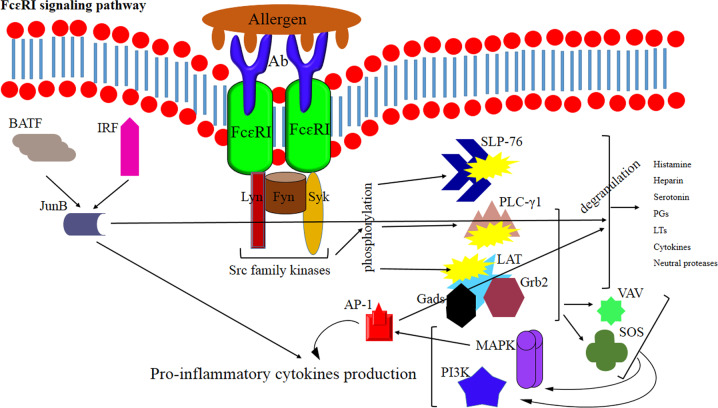
Mast cells also play an important role in allergy by releasing histamine and other mediators after activation by IgE-allergen complexes that bind to FcɛRI on these cells. The attachment of IgE-allergen immune complexes to FcεRI activates tyrosine kinases such as Lyn, Fyn, and Syk that subsequently phosphorylate a variety of signaling molecules such as LAT, SLP-76, and PLC-γ1 and lead to mast cell degranulation. The granules of mast cells contain a variety of highly active mediators, including histamine, prostaglandins, leukotrienes, heparin, serotonin, inflammatory cytokines (such as IL-6, TNF-α, MCP-1, etc.), and neutral proteases.201–204
FcεRI-mediated signaling enhances the phosphorylation of Syk, LAT, SLP-76, PLC-γ1, Akt, and ERK1/2 or p38. Following the aggregation of FcεRI –IgE–allergen complexes and the activation of Src family kinases (such as Fyn, Lyn, and Syk), downstream signaling molecules (such as LAT and SLP-76) are phosphorylated and activated. After being phosphorylated, LAT binds to Grb2, Gads, PLC-γ1, and the guanine exchange factors, VAV and SOS, leading to the activation of PI3K and MAPK-dependent pathways and production of inflammatory cytokines (Fig. 5).201,203,205 In general, pathways involved in the activation of mast cells are potential targets to design effective drugs to control allergic asthma attacks.
Fig. 5.
Allergen-IgE-mediated signaling via FcɛRI during allergic attacks of asthma. The activation of FcεRI recruits Lyn, Fyn, and Syk kinases, which subsequently phosphorylate LAT, SLP-76, and PLC-γ1, leading to mast cell degranulation. Following the aggregation of FcεRI by IgE-allergen complexes, Src family kinases are activated that subsequently phosphorylate LAT and SLP-76. LAT binds to Grb2, Gads, and PLC-γ1, as well as VAV and SOS, the guanine exchange factors. This event then induces PI3K and MAPK-dependent pathways and cytokine production
The proliferation and differentiation of Th2 cells require the AP-1 transcription factor and JunB. Ap1 is activated through the MAPK pathway, whereas JunB is a part of a trimolecular complex comprising basic leucine zipper ATF-like and interferon regulatory factor 4.206,207 Th2 cells induce the production of IgE by B cells through the action of IL-4. IgE-mediated cross-linking of FceRI further activates mast cells. The Lyn, Fyn, and Syk kinases further phosphorylate and activate the LAT adaptor molecule following FceRI aggregation. This event results in the binding of cytosolic adaptor molecules, including SLP-76, GRB2, SOS VAV, and PLCγ1, to the LAT. The activation of these molecules then leads to the recruitment of more downstream molecules, the degranulation of mast cells, and the release of cytokines and eicosanoids. The phosphorylation of Src family kinases such as Fyn and Lyn recruits Syk kinase, which in turn phosphorylates some cellular target proteins and activates multiple signaling pathways. Syk is an intracellular tyrosine kinase and a key regulator of inflammatory cells. In accordance, Syk antagonists exude potent anti-inflammatory effects.205,208,209
Tim-3-Gal-9 signaling pathway
During inflammation, macrophages differentiate into two subtypes: M1 (i.e., classically activated) and M2 (i.e., alternatively activated). M1 macrophages express CD86, secrete proinflammatory cytokines, and activate iNOS to promote inflammatory responses. M2 macrophages, on the other hand, express CD206 and are involved in immune regulation and tolerance. M2 macrophages also promote tissue repair and release anti-inflammatory cytokines, as well as Arginase-1.210–213
T-cell immunoglobulin mucin 3 (Tim-3) is an immunomodulatory molecule highly expressed on Th1 cells and cytotoxic T cells. Tim-3 induces apoptosis in Thl and cytotoxic T cells and regulates the function of NK cells, NKT cells and macrophages. Galectin-9 (Gal-9) is a ligand of Tim-3-driving apoptosis and peripheral immune tolerance when it specifically binds to Tim-3 on Th1 cells. The Tim-3/Gal-9 pathway also inhibits the function of macrophages and downregulates the release of inflammatory factors.214–216 Nevertheless, different immune responses may ensue based on the type of macrophage (i.e., M1 or M2), which needs to be clarified by further studies.
Gal-9 is a type of β-galactoside lectin that phosphorylates tyrosine residues at the tail of Tim-3. On the other hand, peptides derived from Tim-3 interact with the SH2 domain of p85, the adaptor subunit of phosphatidylinositol 3-kinase (PI3K), which induces immune pleiotropism.217,218 A study revealed extracellular Gal-9 and Tim-3 interactions on macrophages. The activation of the PI3K/Akt pathway upon Tim-3 recruitment suppresses NF-kB and MAPK signaling cascades in Th1 cells and macrophages, leading to a reduction in TNF-α expression.219,220 The activation of the Tim-3/Gal-9 signaling pathway on M1 macrophages leads to the production of proinflammatory cytokines, while in M2 macrophages, the recruitment of this pathway leads to the induction of anti-inflammatory cytokines. Therefore, M2 macrophages can be specifically targeted to alleviate inflammation in asthma.
In allergic diseases, eosinophils can be recruited by IL-4- and IL-10-stimulated M2 macrophages. Eosinophils in turn can reduce inflammation by accelerating the polarization of M2 cells via IL-4 and IL-13 and by inhibiting the NF-κB/P38 MAPK signaling pathway.221,222 IKK phosphorylates IκB, which subsequently undergoes ubiquitylation and degradation, inducing NF-κB and inflammatory reactions.223–225
The elevated expression levels of p-IκB and p-P38 in eosinophils shift the polarization of macrophages from M1 to M2 and decrease inflammation via reducing TNF-α, IL-6, and IL-12 levels, as well as the number of CD68-positive macrophages.226 On the other hand, eosinophils can also trigger type 2 inflammation, which is the main pathological process in allergic asthma.
Type 2 cytokines, such as IL-5 and IL-33, increase the numbers of eosinophils and M2 macrophages. In addition, eosinophils respond to these cytokines by decreasing the expression of CD68, iNOS, TNF-α, IL-6, and IL-12 and increasing CD163, Arg-1, TGF-β, IL-10, and IL-13.227,228 Therefore, attention should be dedicated to eosinophils as important contributors to the pathogenesis of allergic asthma.
The development of eosinophils requires IL-5. The receptor of IL-5 shares a common β-chain that is also expressed in IL-3 and GM-CSF receptors. In this regard, studies demonstrated that GM-CSF signaling promoted the recruitment of eosinophils to asthmatic lungs. Likewise, deficiencies of either GM-CSF or its receptor (GM-CSFR) led to pulmonary alveolar proteinosis. GM-CSF directly controls granulocyte trafficking and induces chemokines of eosinophils (such as eotaxins) within allergic lungs.229–232 Therefore, GM-CSF can be a potential factor in designing new drugs against asthma.
TLR signaling pathways
In atopic individuals, antigen presenting cells, especially dendritic cells (DCs), recognize allergens. After migration to lymph nodes, these cells present antigens to naive CD4 T cells and induce their differentiation into Th2 cells. The Th2 immune response is associated with the pathogenesis and progression of allergic asthma.233,234 In this process, toll-like receptors (TLRs) and NF-кB play important roles. TLRs recognize antigens through pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs). TLR signaling pathways activate NF-κB (via IKKα/IKKβ), AP-1 (via MAPKs), and IRF 3 (via TBK1, IKKε, and IKKα).235,236 Genetic polymorphisms and mutations in genes related to TLR signaling pathways such as NOD1, NOD2, IL1RL1, MAP3K7IP1, and BPI have been related to the development of asthma.237,238
Signaling pathways triggered by TLRs following antigen recognition through PAMPs or DAMPs induce cytokines, chemokines, and costimulatory molecules. The activation of TLRs causes conformational changes in the TIR domain and allows the recruitment of cytoplasmic adapter proteins such as TIR domain-containing adaptor protein (TIRAP, MAL), myeloid differentiation primary response protein MyD88 (MyD88), TIR domain-containing adapter-inducing interferon-β (TRIF, TICAM1) and TRAM that anchor the TIR domain.47,239 Based on the recruited adapter proteins, TLR signaling pathways have been classified into two distinct categories: MyD88-dependent (in all TLRs except TLR3) and MyD88-independent (also known as the TIR domain-containing adapter-inducing interferon-β (TRIF)-dependent pathway). The MyD88-dependent pathway activates NF-кB and mitogen-activated protein (MAP) kinases, inducing the expression of inflammatory cytokine genes, while the TRIF-dependent pathway activates NF-кB, IRF 3 and MAPKs inducing type I interferons and inflammatory cytokines.240
In association with Syk tyrosine kinase, the suppressor of cytokine signaling 1 and casitas B-lineage lymphoma-b (Cbl-b) regulate MyD88-dependent pathways. On the other hand, sterile α- and armadillo-motif-containing protein and its splice variant TAG are regulators of the TRIF-dependent pathway.241–244 NF-кB is an important mediator involved in inflammation and can be a potent target for developing novel therapeutics to control and treat asthma.
The stimulation of TLRs in airways induces local inflammation via the recruitment of innate and adaptive immune cells. TLRs have main roles in priming cells involved in regulating innate immunity and cytokine release. Therefore, TLRs can act as novel vaccines against allergic asthma.245,246
PAR2 signaling pathways
Protease-activated receptor-2 (PAR2) participates in bronchodilation in asthma. This molecule has been explored as a therapeutic target in asthma. Similar to β2-AR, PAR2 triggers intracellular signaling through G-protein-dependent mechanisms.247–249 Therefore, designing specific ligands to target this pathway can present therapeutic implications in asthma.
β-Arrestins are adaptor proteins recruited by GPCRs to promote receptor desensitization and internalization. These adaptor proteins can also trigger G-protein-independent signals247,248 through uncoupling GPCRs from their cognate heterotrimeric Gα subunits and decreasing their responsiveness to agonistic stimulation.250 Regarding β-arrestin-dependent signaling, G-protein signaling is a downstream pathway. In other words, β-arrestins can turn off G-protein-induced signal transduction. Furthermore, β-arrestins can promote inflammatory signals as well.251–253
Inducing β2-AR using agonists recruits Gas and stimulates membrane-bound adenylyl cyclase. This leads to cAMP generation and activates cAMP-dependent protein kinase (PKA), which in turn promotes the relaxation of airway smooth muscle cells through phosphorylation of cross-bridge cycling regulatory proteins. β2-AR also mediates cellular responses via Gai-induced generation of cGMP and intracellular elevation of Ca2+. Nevertheless, the cAMP/PKA pathway remains the predominant mechanism in the relaxation of airway smooth muscle cells.254,255
Keap1/Nrf2/ARE signaling pathways
As mentioned, the NF-κB, MAPK, and JAK-STAT (signal transducers and activators of transcription) signaling pathways are involved in the development of inflammation. On the other hand, the transcription factor Nrf2 (NF-E2 p45-related factor 2) regulates the expression of anti-inflammatory and antioxidant NADPH, NAD(P)H quinone oxidoreductase 1, glutathione peroxidase, ferritin, hemeoxygenase-1 (HO-1) and other detoxifying enzyme genes.256–259
Nrf2 belongs to the Cap ‘n’ Collar (CNC) subfamily and comprises seven functional domains: Neh (Nrf2-ECH homology) 1–7. Neh1, as a CNC-bZIP domain, permits Nrf2 to heterodimerize with the small musculoaponeurotic fibrosarcoma (Maf) protein and to form a nuclear complex with the UbcM2 ubiquitin-conjugating enzyme.260,261 The Neh2 domain contains two motifs (i.e., DLG and ETGE), which are essential for the interaction between Nrf2 and its negative regulator, Kelch-like ECH associated protein (Keap) 1.262,263 The carboxy-terminus of the Neh3 domain, on the other hand, has a role as the transactivation domain and interacts with the transcription coactivator chromo-ATPase/helicase DNA-binding protein (CHD6). Neh4 and Neh5 are also transactivation domains that bind to another transcriptional coactivator, CBP. The interaction between Neh4 and Neh5 with the nuclear cofactor RAC3/AIB1/SRC-3 enhances the expression of antioxidant response element (ARE)-containing genes. Neh5 also regulates the cellular localization of Nrf2 through a redox-sensitive nuclear-export signal motif.264–266
Keap1 is an adaptor of cullin-based E3 ubiquitin ligase that suppresses the transcriptional activity of Nrf2 via inducing its ubiquitination and proteasomal degradation. The KELCH domain of the Keap1 homodimer binds to the DLG and ETGE motifs (ETGE acts as a hinge, and DLG acts as a latch) of the Neh2 domain of Nrf2 in the cytosol.267,268 Under oxidative stress conditions, Nrf2 dissociates from Keap1 following thiol modifications of its cysteine residues, preventing Nrf2 ubiquitination and proteasomal degradation. Nrf2 then translocases into the nucleus and heterodimerizes with small Maf proteins to transactivate genes containing ARE.269,270
The β-transducin repeat-containing protein (β-TrCP) presents another regulating mechanism of Nrf2. The β-TrCP binds to two motifs (i.e., DSGIS and DSAPGS) within the serine-rich Neh6 domain of Nrf2. β-TrCP is a substrate receptor of the Skp1-Cul1-Rbx1/Roc1 ubiquitin ligase complex and therefore targets Nrf2 for ubiquitination and proteasomal degradation. Glycogen synthase kinase-3, as a regulator of Nrf2, phosphorylates Nrf2 on the Neh6 domain to facilitate the attachment of β-TrCP and recognition of Nrf2 by the ubiquitin ligase complex.271,272 These pathways can be manipulated using agonists/antagonists, as well as molecular adaptors such as miRNAs to alleviate inflammatory reactions.
HO-1 is an inducible enzyme catalyzing the degradation of heme into carbon monoxide (CO) and free iron. HO-1 also promotes the degradation of biliverdin to bilirubin. The degradation of free heme as a proinflammatory mediator indicates the anti-inflammatory effects of HO-1.273,274 In addition, CO and bilirubin have powerful antioxidant effects and protect airway cells against oxidant assaults.
The NLR family pyrin domain-containing 3 (NLRP3) inflammasome complex recognizes microbial and oxidative stress signals, such as PAMPs, ROS, and DAMPs, through its PRR. The activation of the NLRP3 inflammasome mediates the cleavage of caspase-1 and the secretion of the IL-1β proinflammatory cytokine, ultimately inducing cell death through a process known as pyroptosis. Nrf2 negatively regulates the NLRP3 inflammasome through NQO1 expression. Furthermore, NQO1 inhibits the cleavage of caspase-1 and the production of IL-1β.275,276 The efficacy of Nrf2 activators in treating asthma is unclear and should be divulged in future studies.
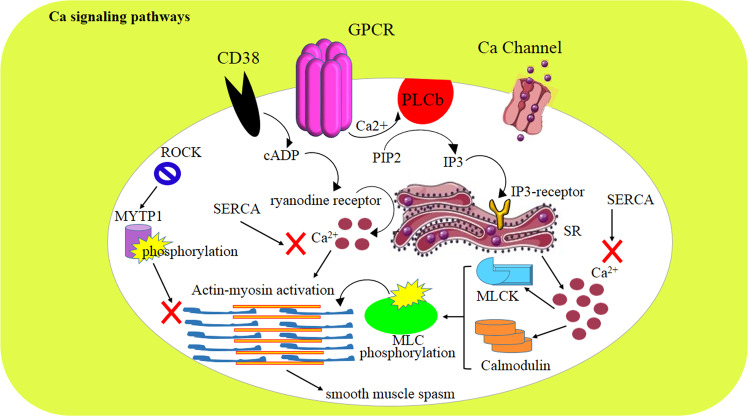
Ca2+ signaling pathways
GPCR agonists and calcium (Ca2+)-dependent and -independent pathways modulate airway smooth muscle spasm. In the Ca2+-dependent pathway, phospholipase b generates the inositol triphosphate (IP3) that binds to the IP3 receptor on the sarcoplasmic reticulum (SR) and induces Ca2+ release to the cytosol. Intracellular Ca2+ then induces calmodulin and myosin light chain kinase to phosphorylate myosin light chain and activate actin-myosin cross-bridge cycling, leading to smooth muscle spasm. In parallel with the mentioned pathway, CD38 expression evokes the generation of cyclic ADP-ribose, which binds to the ryanodine receptor and promotes the release of Ca2+i from the SR. On the other hand, the sarco/endoplasmic reticulum Ca2+-ATPase refills the SR with cytosolic Ca2+i and inhibits smooth muscle spasm. In allergic reactions, methacholine, histamine, thrombin, and leukotriene D4 have elicited Ca2+i releasing effects.277,278
After the release of intracellular Ca2+, cell surface channels facilitate the refilling of cytosolic stores by extracellular Ca2+. In this regard, the activation of Orai/STIM as well as store-operated Ca2+ entry pathways mediates Ca2+ influx through plasma membrane channels following the depletion of intracellular Ca2+ stores via IP3 receptor-mediated Ca2+i release from the SR.277
The Ca2+-independent pathway is mediated through the activation of RhoA and the stimulation of Rho kinase, which phosphorylates and inactivates the myosin light chain phosphatase target subunit. Under resting conditions, MYPT1 limits smooth muscle spasm (Fig. 6);277 therefore, activating MYPT1 during asthma attacks can be beneficial for controlling dyspnea.
Fig. 6.
The Ca2+ signaling pathway and the roles of CD38, Ca2+ channels, and G-protein-coupled receptors. In the Ca2+-dependent signaling pathway, PLCb generates IP3 that binds to its receptor on the sarcoplasmic reticulum (SR) membrane and induces Ca2+i release. Ca2+i activates calmodulin and myosin light chain kinase (MLCK) to induce actin-myosin cross-bridge cycling and subsequently smooth muscle spasm. CD38 expression evokes the generation of cyclic ADP-ribose, which binds to the ryanodine receptor and stimulates the SR to release Ca2+i. SERCA refills the SR with cytosolic Ca2+i and inhibits smooth muscle spasm. The Ca2+-independent pathway is mediated by RhoA and ROCK, which phosphorylate and inactivate MYTP1, leading to airway smooth muscle spasm
IL-13 is overexpressed during allergic asthma attacks, augmenting canonical calcium mobilization pathways, enhancing calcium sensitization, and aggravating asthma presentation. In addition, suppression of RhoA has been reported to relax airway smooth muscles.279–281 These modulators can be useful in alleviating and treating asthma symptoms.
Limitations of the therapeutic targeting of cell signaling pathways
There are some concerns regarding the therapeutic targeting of cell signaling pathways. First, targeting one pathway can affect the function of other signaling pathways (i.e., a pleotropic phenomenon). On the other hand, blocking or activating a specific pathway may augment the compensatory functions of other signaling pathways, thus counteracting the therapeutic effects of the interference (i.e., redundancy function). Specifically, these problems are highlighted when targeting cytokine pathways. One solution may be targeting the last molecule within the signaling pathway.
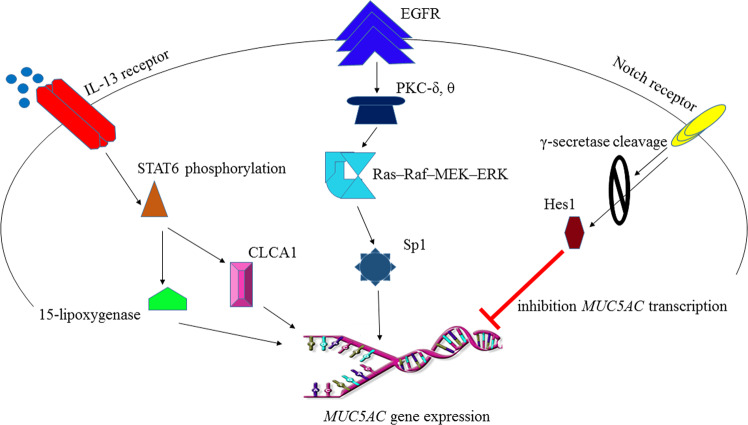
For example, mucus secretion is mediated by the induction of the MUC5AC gene in goblet cells through several independent pathways, including the CLCA1 (a Serpin)- and 15-lipoxygenase-1-dependent pathways. These pathways are activated following the binding of IL-13 to its receptor and the phosphorylation and translocation of STAT-6 to the nucleus. The SPDEF transcription factor is another regulator of goblet cell differentiation by inhibiting FOXA2 and activating other genes in these cells.282 Another mechanism regulating mucus secretion through the STAT-6 pathway involves the protein calcium-activated chloride channel 1 (CLCA1).283 CLCA1 can induce MUC5AC gene expression via the MAP kinase pathway and MAPK13 (p38δ-MAPK).284 IL-13-mediated STAT-6 activation increases the expression of SAM-pointed domain-containing Ets-like factor (SPDEF), which also shares an important role in regulating mucus production.285 The activity of SPDEF, however, is also modulated in part by FOXM1, a member of the Forkhead box (FOX) family.286,287 This indicates that therapeutic targeting of STAT-6 affects different pathways. The complicated nature of the cellular signaling network presents a major challenge in designing new drugs to target signaling molecules.
The expression of the MUC5AC gene in airways is also regulated by signaling triggered by epidermal growth factor receptor (EGFR). Nevertheless, EGFR has multiple ligands (e.g., EGF, heparin-binding EGF, β-cellulin, amphiregulin, epiregulin, and TGF-α). Binding of these ligands, on the other hand, activates the EGFR kinase domain and induces signaling cascades, leading to the expression of the MUC5AC gene.288 The EGFR signaling cascade is initiated by the activation of the PKC δ and PKC θ isoforms.289 EGFR ligand binding also activates the Ras–Raf–MEK1/2–ERK1/2 pathway, which ultimately leads to the expression of MUC5AC via the Sp1 transcription factor.290,291 Based on these findings, the Sp1 transcription factor represents a potential target to promote mucus production. On the other hand, blocking mucus production by silencing the IL-13 pathway can be compensated by the EGFR-dependent pathway (Fig. 7, Table 3, and Table 4).
Fig. 7.
Signaling pathways contributing to mucus production. The CLCA1 (a Serpin) and 15-lipoxygenase-1-dependent pathways are triggered following the binding of IL-13 to its receptor. These pathways lead to the phosphorylation of STAT-6, leading to MUC5AC gene expression and mucus production. EGFR signaling is initiated following the activation of the PKC δ and PKC θ isoforms. The activation of EGFR kinase induces the Ras–Raf–MEK1/2–ERK1/2 pathway and the transcription of MUC5AC gene in airways via binding of the Sp1 transcription factor to specific binding sites within the gene promoter. Notch activates γ-secretase-mediated proteolytic processes, and Hes1 inhibits MUC5AC expression and mucus production
Table 3.
Signaling Pathways, related targets, and molecules are interacted in asthma pathophysiology
| Pathway | Related molecules and actions | References |
|---|---|---|
| JAK-STAT | IL-4, IL-5, IL-13, IL-31 and TSLP | 17– 21 |
| Adiponectin | AMPK and NF-κB | 43– 45, 50 |
| prostaglandin receptor | CRTH2 and LTB4 | 58, 61, 62, 80, 82 |
| NF-κB | iNOS and COX-2 | 85, 86, 88, 93 |
| Type I interferon | PRRs, TLR, RIG-I and MDA5 | 89, 91, 93 |
| Wnt | WISP-1 and WIF-1 | 94, 95, 98, 99, 101, 102 |
| Vit. D, glucocorticoid, DICKKOPF | 104, 106– 108 | |
| PI3K/AKT | miRs | 111, 112, 114, 118 |
| JNK-Gal-7 | TGF-β | 133, 134, 136, 137, 139 |
| Nrf2 | ROS | 140, 142, 144 |
| Foxp3- RORγt | LncRs ceRs and miRs | 146, 147, 149, 152, 153 |
| MAPK | IgE and IL-4 | 155, 158 |
| CysLT | eosinophil degranulation | 162, 164, 166 |
| cAMP | IL-4, 5, 13 and β2-AR | 165, 171, 176 |
| Fas | apoptotic Fas signaling: JNK, NF-kB, p38 | 185, 186, 188, 189 |
| nonapoptotic Fas signal: ERK1/2 and p35 | ||
| PTHrP/PPARγ | Leptin | 191, 192 |
| PAI-1 | t-PA, u-PA, ECM and remodeling | 193, 195, 196 |
| FcɛRI | TSLP, IL-4, IgE and mast cell degranulation | 197, 199, 202– 204 |
| Tim-3-Gal-9 | PI3K/Akt, Th1 apoptosis and inflammation | 214, 216, 219, 220 |
| TLRs | NF-κB, AP-1, IRF, SOCS1 and MyD88 | 235, 236, 241, 243, 244 |
| PAR2 | b-Arrestins, cAMP/PKA | 248, 254, 255 |
| Keap1/Nrf2/ARE | CHD6, CBP, ARE | 256, 258, 265, 268, 270 |
| Ca | PLCb, ROCK, RhoA | 277, 278, 280, 281 |
Table 4.
Role of the cytokines in pathophysiology of asthma and related signaling molecules
Notch is a transmembrane receptor that binds to ligands from the Delta-like and Jagged families. This interaction activates γ-secretase-mediated proteolytic cleavage of the Notch intracellular domain, which ultimately targets Hes1 and inhibits MUC5AC transcription. Nonetheless, studies have shown that Hes1 inactivation is not sufficient to induce mucus production.292,293 This fact indicates the redundant functions of various signaling pathways that limit the therapeutic efficiency of targeting signaling molecules.
Another problem with targeted therapy of signaling pathways is that these therapeutics should be designed to act locally. For example, in the case of mucus production, systemic drugs can lead to dysfunction of other organs (e.g., digestion problems because of reduced mucus production in the gastrointestinal tract).
Concluding remarks
Cell signaling pathways can be important targets for the treatment of diseases. Designing new ligands either as agonists or antagonists for adaptor molecules of signaling pathways provides a new approach for the treatment of asthma as well. Recent knowledge about cell signaling pathways, especially within the cells that have main roles in the pathophysiology of asthma, has provided new hope for developing novel, efficient, and safe targeted therapies. Several pathways have been suggested as potential targets to design either therapeutic or prophylactic drugs against asthma. To develop highly efficient drugs, however, the interactions of these pathways with other signaling routes should be divulged in future studies.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Athari SS, et al. Critical role of Toll-like receptors in pathophysiology of allergic asthma. Eur. J. Pharmacol. 2017;808:21–27. doi: 10.1016/j.ejphar.2016.11.047. [DOI] [PubMed] [Google Scholar]
- 2.Athari SS. Immune response shifting of asthma in aging. Middle-East J. Sci. Res. 2013;13:489–498. [Google Scholar]
- 3.Soriano JB, et al. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir. Med. 2017;5:691–706. doi: 10.1016/S2213-2600(17)30293-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boyman O, et al. EAACI IG Biologicals task force paper on the use of biologic agents in allergic disorders. Allergy. 2015;70:727–754. doi: 10.1111/all.12616. [DOI] [PubMed] [Google Scholar]
- 5.Brightling C, Bradding P, Pavord I, Wardlaw A. New insights into the role of the mast cell in asthma. Clin. Exp. Allergy. 2003;33:550–556. doi: 10.1046/j.1365-2222.2003.01636.x. [DOI] [PubMed] [Google Scholar]
- 6.Taghavi M, et al. Role of pathogen-associated molecular patterns (PAMPS) in immune responses to fungal infections. Eur. J. Pharmacol. 2017;808:8–13. doi: 10.1016/j.ejphar.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 7.Foster PS, et al. Modeling TH 2 responses and airway inflammation to understand fundamental mechanisms regulating the pathogenesis of asthma. Immunological Rev. 2017;278:20–40. doi: 10.1111/imr.12549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Athari SS, Athari SM. The importance of eosinophil, platelet and dendritic cell in asthma. Asian Pac. J. Trop. Dis. 2014;4:S41–S47. doi: 10.1016/S2222-1808(14)60413-8. [DOI] [Google Scholar]
- 9.Galeone, C. et al. Precision Medicine in Targeted Therapies for Severe Asthma: Is There Any Place for “Omics” Technology? BioMed research international. 2018, 1–15 (2018). [DOI] [PMC free article] [PubMed]
- 10.Swedin L, et al. Patient stratification and the unmet need in asthma. Pharmacol. Ther. 2017;169:13–34. doi: 10.1016/j.pharmthera.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 11.Stokes JR, Casale TB. Characterization of asthma endotypes: implications for therapy. Ann. Allergy, Asthma Immunol. 2016;117:121–125. doi: 10.1016/j.anai.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 12.Chung KF. Asthma phenotyping: a necessity for improved therapeutic precision and new targeted therapies. J. Intern. Med. 2016;279:192–204. doi: 10.1111/joim.12382. [DOI] [PubMed] [Google Scholar]
- 13.Lea S, et al. The effect of peroxisome proliferator-activated receptor-γ ligands on in vitro and in vivo models of COPD. Eur. Respiratory J. 2014;43:409–420. doi: 10.1183/09031936.00187812. [DOI] [PubMed] [Google Scholar]
- 14.O'Byrne PM, et al. Efficacy and safety of a CXCR2 antagonist, AZD5069, in patients with uncontrolled persistent asthma: a randomised, double-blind, placebo-controlled trial. Lancet Respiratory Med. 2016;4:797–806. doi: 10.1016/S2213-2600(16)30227-2. [DOI] [PubMed] [Google Scholar]
- 15.Svenningsen S, Nair P. Asthma endotypes and an overview of targeted therapy for asthma. Front. Med. 2017;4:158. doi: 10.3389/fmed.2017.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nair P, et al. Safety and efficacy of a CXCR 2 antagonist in patients with severe asthma and sputum neutrophils: a randomized, placebo‐controlled clinical trial. Clin. Exp. Allergy. 2012;42:1097–1103. doi: 10.1111/j.1365-2222.2012.04014.x. [DOI] [PubMed] [Google Scholar]
- 17.Hsieh Y-Y, et al. JAK-1 rs2780895 C-related genotype and allele but not JAK-1 rs10789166, rs4916008, rs2780885, rs17127114, and rs3806277 are associated with higher susceptibility to asthma. Genet. Test. Mol. Biomark. 2011;15:841–847. doi: 10.1089/gtmb.2011.0002. [DOI] [PubMed] [Google Scholar]
- 18.Howell MD, Fitzsimons C, Smith PA. JAK/STAT inhibitors and other small molecule cytokine antagonists for the treatment of allergic disease. Ann Allerg Asthma Immunol. 2018;120:367–375. doi: 10.1016/j.anai.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 19.Wurster AL, Tanaka T, Grusby MJ. The biology of Stat4 and Stat6. Oncogene. 2000;19:2577. doi: 10.1038/sj.onc.1203485. [DOI] [PubMed] [Google Scholar]
- 20.Rudolph A-K, Walter T, Erkel G. The fungal metabolite cyclonerodiol inhibits IL-4/IL-13 induced Stat6-signaling through blocking the association of Stat6 with p38, ERK1/2 and p300. Int. Immunopharmacol. 2018;65:392–401. doi: 10.1016/j.intimp.2018.10.033. [DOI] [PubMed] [Google Scholar]
- 21.McCormick SM, Heller NM. Commentary: IL-4 and IL-13 receptors and signaling. Cytokine. 2015;75:38–50. doi: 10.1016/j.cyto.2015.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walford HH, Doherty TA. STAT6 and lung inflammation. Jak.Stat. 2013;2:e25301. doi: 10.4161/jkst.25301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lambrecht BN, Hammad H. The immunology of asthma. Nat. Immunol. 2015;16:45. doi: 10.1038/ni.3049. [DOI] [PubMed] [Google Scholar]
- 24.Makinde T, Murphy RF, Agrawal DK. The regulatory role of TGF‐β in airway remodeling in asthma. Immunol. cell Biol. 2007;85:348–356. doi: 10.1038/sj.icb.7100044. [DOI] [PubMed] [Google Scholar]
- 25.Wen F-Q, et al. Interleukin-4–and interleukin-13–enhanced transforming growth factor-β 2 production in cultured human bronchial epithelial cells is attenuated by interferon-γ. Am. J. Respir. Cell Mol. Biol. 2002;26:484–490. doi: 10.1165/ajrcmb.26.4.4784. [DOI] [PubMed] [Google Scholar]
- 26.Zhuang S. Regulation of STAT signaling by acetylation. Cell. Signal. 2013;25:1924–1931. doi: 10.1016/j.cellsig.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schindler C, Levy DE, Decker T. JAK-STAT signaling: from interferons to cytokines. J. Biol. Chem. 2007;282:20059–20063. doi: 10.1074/jbc.R700016200. [DOI] [PubMed] [Google Scholar]
- 28.So E-Y, et al. Ras/Erk pathway positively regulates Jak1/STAT6 activity and IL-4 gene expression in Jurkat T cells. Mol. Immunol. 2007;44:3416–3426. doi: 10.1016/j.molimm.2007.02.022. [DOI] [PubMed] [Google Scholar]
- 29.Wang Y, Malabarba MG, Nagy ZS, Kirken RA. Interleukin 4 regulates phosphorylation of serine 756 in the transactivation domain of Stat6 roles for multiple phosphorylation sites and Stat6 function. J. Biol. Chem. 2004;279:25196–25203. doi: 10.1074/jbc.M313668200. [DOI] [PubMed] [Google Scholar]
- 30.Yeganeh B, et al. Emerging mediators of airway smooth muscle dysfunction in asthma. Pulm. Pharmacol. Ther. 2013;26:105–111. doi: 10.1016/j.pupt.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 31.Ip W, Wong C, Lam C. Interleukin (IL)‐4 and IL‐13 up‐regulate monocyte chemoattractant protein‐1 expression in human bronchial epithelial cells: involvement of p38 mitogen‐activated protein kinase, extracellular signal‐regulated kinase 1/2 and Janus kinase‐2 but not c‐Jun NH2‐terminal kinase 1/2 signalling pathways. Clin. Exp. Immunol. 2006;145:162–172. doi: 10.1111/j.1365-2249.2006.03085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pope SM, et al. The eotaxin chemokines and CCR3 are fundamental regulators of allergen-induced pulmonary eosinophilia. J. Immunol. 2005;175:5341–5350. doi: 10.4049/jimmunol.175.8.5341. [DOI] [PubMed] [Google Scholar]
- 33.Schwartz DM, et al. JAK inhibition as a therapeutic strategy for immune and inflammatory diseases. Nat. Rev. Drug Discov. 2017;16:843. doi: 10.1038/nrd.2017.201. [DOI] [PubMed] [Google Scholar]
- 34.Morlacchi P, Mandal PK, McMurray JS. Synthesis and in vitro evaluation of a peptidomimetic inhibitor targeting the Src homology 2 (SH2) domain of STAT6. ACS medicinal Chem. Lett. 2013;5:69–72. doi: 10.1021/ml4003919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mandal PK, et al. Targeting the Src homology 2 (SH2) domain of signal transducer and activator of transcription 6 (STAT6) with cell-permeable, phosphatase-stable phosphopeptide mimics potently inhibits Tyr641 phosphorylation and transcriptional activity. J. Med. Chem. 2015;58:8970–8984. doi: 10.1021/acs.jmedchem.5b01321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miklossy G, Hilliard TS, Turkson J. Therapeutic modulators of STAT signalling for human diseases. Nat. Rev. Drug Discov. 2013;12:611. doi: 10.1038/nrd4088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lugogo NL, Bappanad D, Kraft M. Obesity, metabolic dysregulation and oxidative stress in asthma. Biochim. Biophys. Acta. 2011;1810:1120–1126. doi: 10.1016/j.bbagen.2011.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.André DM, et al. Therapy with resveratrol attenuates obesity-associated allergic airway inflammation in mice. Int. Immunopharmacol. 2016;38:298–305. doi: 10.1016/j.intimp.2016.06.017. [DOI] [PubMed] [Google Scholar]
- 39.Tilg H, Moschen AR. Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat. Rev. Immunol. 2006;6:772. doi: 10.1038/nri1937. [DOI] [PubMed] [Google Scholar]
- 40.Shore SA, et al. Adiponectin attenuates allergen-induced airway inflammation and hyperresponsiveness in mice. J. Allergy Clin. Immunol. 2006;118:389–395. doi: 10.1016/j.jaci.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 41.Miller M, et al. Adiponectin and functional adiponectin receptor 1 are expressed by airway epithelial cells in chronic obstructive pulmonary disease. J. Immunol. 2009;182:684–691. doi: 10.4049/jimmunol.182.1.684. [DOI] [PubMed] [Google Scholar]
- 42.Williams AS, et al. Role of the adiponectin binding protein, T-cadherin (Cdh13), in allergic airways responses in mice. PloS ONE. 2012;7:e41088. doi: 10.1371/journal.pone.0041088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hardie DG, Ross FA, Hawley SA. AMPK: a nutrient and energy sensor that maintains energy homeostasis. Nat. Rev. Mol. Cell Biol. 2012;13:251. doi: 10.1038/nrm3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yamauchi T, et al. Targeted disruption of AdipoR1 and AdipoR2 causes abrogation of adiponectin binding and metabolic actions. Nat. Med. 2007;13:332. doi: 10.1038/nm1557. [DOI] [PubMed] [Google Scholar]
- 45.Sag D, Carling D, Stout RD, Suttles J. Adenosine 5′-monophosphate-activated protein kinase promotes macrophage polarization to an anti-inflammatory functional phenotype. J. Immunol. 2008;181:8633–8641. doi: 10.4049/jimmunol.181.12.8633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gilmore TD. Introduction to NF-κB: players, pathways, perspectives. Oncogene. 2006;25:6680. doi: 10.1038/sj.onc.1209954. [DOI] [PubMed] [Google Scholar]
- 47.Mishra V, Banga J, Silveyra P. Oxidative stress and cellular pathways of asthma and inflammation: therapeutic strategies and pharmacological targets. Pharmacol. Ther. 2018;181:169–182. doi: 10.1016/j.pharmthera.2017.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhu L, et al. Adiponectin alleviates exacerbation of airway inflammation and oxidative stress in obesity-related asthma mice partly through AMPK signaling pathway. Int. Immunopharmacol. 2019;67:396–407. doi: 10.1016/j.intimp.2018.12.030. [DOI] [PubMed] [Google Scholar]
- 49.Catz SD, Johnson JL. Transcriptional regulation of bcl-2 by nuclear factor κB and its significance in prostate cancer. Oncogene. 2001;20:7342. doi: 10.1038/sj.onc.1204926. [DOI] [PubMed] [Google Scholar]
- 50.Viatour P, et al. NF-κB2/p100 induces Bcl-2 expression. Leukemia. 2003;17:1349. doi: 10.1038/sj.leu.2402982. [DOI] [PubMed] [Google Scholar]
- 51.Akita K, Kawata S, Shimotohno K. p21WAF1 modulates NF-κB signaling and induces anti-apoptotic protein Bcl-2 in Tax-expressing rat fibroblast. Virology. 2005;332:249–257. doi: 10.1016/j.virol.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 52.Ajuwon KM, Spurlock ME. Adiponectin inhibits LPS-induced NF-κB activation and IL-6 production and increases PPARγ2 expression in adipocytes. Am. J. Physiol.Regul. Integr. Comp. Physiol. 2005;288:R1220–R1225. doi: 10.1152/ajpregu.00397.2004. [DOI] [PubMed] [Google Scholar]
- 53.Ouchi N, et al. Obesity, adiponectin and vascular inflammatory disease. Curr. Opin. Lipidol. 2003;14:561–566. doi: 10.1097/00041433-200312000-00003. [DOI] [PubMed] [Google Scholar]
- 54.Lovren F, et al. Adiponectin primes human monocytes into alternative anti-inflammatory M2 macrophages. Am. J. Physiol. Heart Circ. Physiol. 2010;299:H656–H663. doi: 10.1152/ajpheart.00115.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Masaki T, et al. Adiponectin protects LPS‐induced liver injury through modulation of TNF‐α in KK‐Ay obese mice. Hepatology. 2004;40:177–184. doi: 10.1002/hep.20282. [DOI] [PubMed] [Google Scholar]
- 56.Ouchi N, et al. Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-κB signaling through a cAMP-dependent pathway. Circulation. 2000;102:1296–1301. doi: 10.1161/01.CIR.102.11.1296. [DOI] [PubMed] [Google Scholar]
- 57.Xue L, et al. Prostaglandin D2 activates group 2 innate lymphoid cells through chemoattractant receptor-homologous molecule expressed on TH2 cells. J. Allergy Clin. Immunol. 2014;133:1184–1194. doi: 10.1016/j.jaci.2013.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Domingo C, et al. The prostaglandin D 2 receptor 2 pathway in asthma: a key player in airway inflammation. Respir. Res. 2018;19:189. doi: 10.1186/s12931-018-0893-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Matsuda K, et al. Monomeric IgE enhances human mast cell chemokine production: IL-4 augments and dexamethasone suppresses the response. J. Allergy Clin. Immunol. 2005;116:1357–1363. doi: 10.1016/j.jaci.2005.08.042. [DOI] [PubMed] [Google Scholar]
- 60.Townley RG, Agrawal S. CRTH2 antagonists in the treatment of allergic responses involving TH2 cells, basophils, and eosinophils. Ann. Allerg. Asthma Immunol. 2012;109:365–374. doi: 10.1016/j.anai.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 61.Nagata K, et al. CRTH2, an orphan receptor of T‐helper‐2‐cells, is expressed on basophils and eosinophils and responds to mast cell‐derived factor (s) FEBS Lett. 1999;459:195–199. doi: 10.1016/S0014-5793(99)01251-X. [DOI] [PubMed] [Google Scholar]
- 62.Pettipher R. The roles of the prostaglandin D2 receptors DP1 and CRTH2 in promoting allergic responses. Br. J. Pharmacol. 2008;153:S191–S199. doi: 10.1038/sj.bjp.0707488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Coleman R, Sheldrick R. Prostanoid‐induced contraction of human bronchial smooth muscle is mediated by TP‐receptors. Br. J. Pharmacol. 1989;96:688–692. doi: 10.1111/j.1476-5381.1989.tb11869.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kupczyk M, Kuna P. Targeting the PGD 2/CRTH2/DP1 signaling pathway in asthma and allergic disease: current status and future perspectives. Drugs. 2017;77:1281–1294. doi: 10.1007/s40265-017-0777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sykes DA, et al. Fevipiprant (QAW039), a slowly dissociating CRTh2 antagonist with the potential for improved clinical efficacy. Mol. Pharmacol. 2016;89:593–605. doi: 10.1124/mol.115.101832. [DOI] [PubMed] [Google Scholar]
- 66.Xue, L. et al. in C35. ASTHMA AND ALLERGY CELLULAR INVESTIGATIONS A5301-A5301 (American Thoracic Society, 2017).
- 67.Gazi L, et al. Δ12-Prostaglandin D2 is a potent and selective CRTH2 receptor agonist and causes activation of human eosinophils and Th2 lymphocytes. Prostaglandins Other Lipid Mediat. 2005;75:153–167. doi: 10.1016/j.prostaglandins.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 68.Sawyer N, et al. Molecular pharmacology of the human prostaglandin D2 receptor, CRTH2. Br. J. Pharmacol. 2002;137:1163–1172. doi: 10.1038/sj.bjp.0704973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Sandham DA, et al. Discovery of fevipiprant (NVP-QAW039), a potent and selective DP2 receptor antagonist for treatment of asthma. ACS Med. Chem. Lett. 2017;8:582–586. doi: 10.1021/acsmedchemlett.7b00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Xue L, et al. Leukotriene E4 activates human Th2 cells for exaggerated proinflammatory cytokine production in response to prostaglandin D2. J. Immunol. 2012;188:694–702. doi: 10.4049/jimmunol.1102474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gervais FG, et al. Selective modulation of chemokinesis, degranulation, and apoptosis in eosinophils through the PGD2 receptors CRTH2 and DP. J. Allergy Clin. Immunol. 2001;108:982–988. doi: 10.1067/mai.2001.119919. [DOI] [PubMed] [Google Scholar]
- 72.Xue L, et al. Prostaglandin D2 causes preferential induction of proinflammatory Th2 cytokine production through an action on chemoattractant receptor-like molecule expressed on Th2 cells. J. Immunol. 2005;175:6531–6536. doi: 10.4049/jimmunol.175.10.6531. [DOI] [PubMed] [Google Scholar]
- 73.Patel KD. Eosinophil tethering to interleukin-4–activated endothelial cells requires both P-selectin and vascular cell adhesion molecule-1. Blood. 1998;92:3904–3911. doi: 10.1182/blood.V92.10.3904. [DOI] [PubMed] [Google Scholar]
- 74.Moore PE, et al. IL-13 and IL-4 cause eotaxin release in human airway smooth muscle cells: a role for ERK. Am. J. Physiol.Lung Cell. Mol. Physiol. 2002;282:L847–L853. doi: 10.1152/ajplung.00245.2001. [DOI] [PubMed] [Google Scholar]
- 75.Farne, H., Jackson, D. J. & Johnston, S. L. Are emerging PGD2 antagonists a promising therapy class for treating asthma? Expert Opin. Emerg. Drugs 21, 359–364 (2016). [DOI] [PubMed]
- 76.Aceves SS, Ackerman SJ. Relationships between eosinophilic inflammation, tissue remodeling, and fibrosis in eosinophilic esophagitis. Immunol. allergy Clin. North Am. 2009;29:197–211. doi: 10.1016/j.iac.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Molfino N, et al. Molecular and clinical rationale for therapeutic targeting of interleukin‐5 and its receptor. Clin. Exp. Allergy. 2012;42:712–737. doi: 10.1111/j.1365-2222.2011.03854.x. [DOI] [PubMed] [Google Scholar]
- 78.Wood BL, et al. The effects of caregiver depression on childhood asthma: pathways and mechanisms. Ann. Allergy, Asthma Immunol. 2018;121:421–427. doi: 10.1016/j.anai.2018.06.031. [DOI] [PubMed] [Google Scholar]
- 79.Zaitsu M, et al. Direct evidence that LTC4 and LTB4 but not TXA2 are involved in asthma attacks in children. J. Asthma. 1998;35:445–448. doi: 10.3109/02770909809048953. [DOI] [PubMed] [Google Scholar]
- 80.Gelfand EW. Importance of the leukotriene B4-BLT1 and LTB4-BLT2 pathways in asthma. Semin. Immunol. 2017;33:44–51. doi: 10.1016/j.smim.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sampson A, Castling D, Green C, Price J. Persistent increase in plasma and urinary leukotrienes after acute asthma. Arch. Dis. Child. 1995;73:221–225. doi: 10.1136/adc.73.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Montuschi P, Barnes PJ. Exhaled leukotrienes and prostaglandins in asthma. J. Allergy Clin. Immunol. 2002;109:615–620. doi: 10.1067/mai.2002.122461. [DOI] [PubMed] [Google Scholar]
- 83.Sheller JR, et al. Nuclear factor kappa B induction in airway epithelium increases lung inflammation in allergen-challenged mice. Exp. Lung Res. 2009;35:883–895. doi: 10.3109/01902140903019710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Schuliga M. NF-kappaB signaling in chronic inflammatory airway disease. Biomolecules. 2015;5:1266–1283. doi: 10.3390/biom5031266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Chen GG, et al. Increased inducible nitric oxide synthase in lung carcinoma of smokers. Cancer. 2008;112:372–381. doi: 10.1002/cncr.23166. [DOI] [PubMed] [Google Scholar]
- 86.Anto RJ, et al. Cigarette smoke condensate activates nuclear transcription factor-κB through phosphorylation and degradation of IκBα: correlation with induction of cyclooxygenase-2. Carcinogenesis. 2002;23:1511–1518. doi: 10.1093/carcin/23.9.1511. [DOI] [PubMed] [Google Scholar]
- 87.Kim J-B, et al. Inhibition of LPS-induced iNOS, COX-2 and cytokines expression by poncirin through the NF-κB inactivation in RAW 264.7 macrophage cells. Biol. Pharm. Bull. 2007;30:2345–2351. doi: 10.1248/bpb.30.2345. [DOI] [PubMed] [Google Scholar]
- 88.Shin N-R, et al. Galgeun-tang attenuates cigarette smoke and lipopolysaccharide induced pulmonary inflammation via IκBα/NF-κB signaling. Molecules. 2018;23:2489. doi: 10.3390/molecules23102489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Contoli M, et al. Role of deficient type III interferon-λ production in asthma exacerbations. Nat. Med. 2006;12:1023. doi: 10.1038/nm1462. [DOI] [PubMed] [Google Scholar]
- 90.Edwards M, et al. Impaired innate interferon induction in severe therapy resistant atopic asthmatic children. Mucosal Immunol. 2013;6:797. doi: 10.1038/mi.2012.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kato H, et al. Differential roles of MDA5 and RIG-I helicases in the recognition of RNA viruses. Nature. 2006;441:101. doi: 10.1038/nature04734. [DOI] [PubMed] [Google Scholar]
- 92.Yamamoto M, et al. Role of adaptor TRIF in the MyD88-independent toll-like receptor signaling pathway. Science. 2003;301:640–643. doi: 10.1126/science.1087262. [DOI] [PubMed] [Google Scholar]
- 93.Zhu J, et al. Bronchial mucosal IFN-α/β and pattern recognition receptor expression in patients with experimental rhinovirus-induced asthma exacerbations. J. Allergy Clin. Immunol. 2019;143:114–125. doi: 10.1016/j.jaci.2018.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sharma R, Chopra V. Effect of the Wingless (wg1) mutation on wing and haltere development in Drosophila melanogaster. Dev. Biol. 1976;48:461–465. doi: 10.1016/0012-1606(76)90108-1. [DOI] [PubMed] [Google Scholar]
- 95.Yurt M, et al. Vitamin D supplementation blocks pulmonary structural and functional changes in a rat model of perinatal vitamin D deficiency. Am. J. Physiol. Lung Cell. Mol. Physiol. 2014;307:L859–L867. doi: 10.1152/ajplung.00032.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Baarsma HA, Königshoff M, Gosens R. The WNT signaling pathway from ligand secretion to gene transcription: molecular mechanisms and pharmacological targets. Pharmacol. Ther. 2013;138:66–83. doi: 10.1016/j.pharmthera.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 97.Hussain M, et al. Wnt/β-catenin signaling links embryonic lung development and asthmatic airway remodeling. Biochim. Biophys. Acta. 2017;1863:3226–3242. doi: 10.1016/j.bbadis.2017.08.031. [DOI] [PubMed] [Google Scholar]
- 98.Huo Y, et al. Tiotropium inhibits methacholine-induced extracellular matrix production via β-catenin signaling in human airway smooth muscle cells. Int. J. Chronic Obstr. Pulm. Dis. 2018;13:1469. doi: 10.2147/COPD.S158552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jia XX, Zheng YR, Huang Y. Effects of Wnt/β-catenin signal pathway on asthma airway remodeling. Chinese. J. Pathophysiol. 2017;33:1683–1689. [Google Scholar]
- 100.Royer J, et al. A novel antagonist of prostaglandin D2 blocks the locomotion of eosinophils and basophils. Eur. J. Clin. Investig. 2008;38:663–671. doi: 10.1111/j.1365-2362.2008.01989.x. [DOI] [PubMed] [Google Scholar]
- 101.Vatrella A, et al. Dupilumab: a novel treatment for asthma. J. Asthma Allerg. 2014;7:123. doi: 10.2147/JAA.S52387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kuna P, Bjermer L, Tornling G. Two phase II randomized trials on the CRTh2 antagonist AZD1981 in adults with asthma. Drug Des. Dev. Ther. 2016;10:2759. doi: 10.2147/DDDT.S105142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Tromp II, et al. 25-Hydroxyvitamin D concentrations, asthma and eczema in childhood: the generation R study. Clin. Nutr. 2018;37:169–176. doi: 10.1016/j.clnu.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 104.Brehm JM, et al. Serum vitamin D levels and severe asthma exacerbations in the Childhood Asthma Management Program study. J. Allergy Clin. Immunol. 2010;126:52–58. doi: 10.1016/j.jaci.2010.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sypniewska, G. et al. 25-Hydroxyvitamin D, biomarkers of eosinophilic inflammation, and airway remodeling in children with newly diagnosed untreated asthma. Allergy Asthma Proceedings38, 29–36 (2017). [DOI] [PubMed]
- 106.Pálmer HG, et al. Vitamin D3 promotes the differentiation of colon carcinoma cells by the induction of E-cadherin and the inhibition of β-catenin signaling. J. Cell Biol. 2001;154:369–388. doi: 10.1083/jcb.200102028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Aguilera O, et al. The Wnt antagonist DICKKOPF-1 gene is induced by 1α, 25-dihydroxyvitamin D 3 associated to the differentiation of human colon cancer cells. Carcinogenesis. 2007;28:1877–1884. doi: 10.1093/carcin/bgm094. [DOI] [PubMed] [Google Scholar]
- 108.Huang Y, et al. Vitamin D alleviates airway remodeling in asthma by down-regulating the activity of Wnt/β-catenin signaling pathway. Int. Immunopharmacol. 2019;68:88–94. doi: 10.1016/j.intimp.2018.12.061. [DOI] [PubMed] [Google Scholar]
- 109.Solberg OD, et al. Airway epithelial miRNA expression is altered in asthma. Am. J. Respir. Crit. Care Med. 2012;186:965–974. doi: 10.1164/rccm.201201-0027OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Pua HH, Ansel KM. MicroRNA regulation of allergic inflammation and asthma. Curr. Opin. Immunol. 2015;36:101–108. doi: 10.1016/j.coi.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Aich J, et al. Resveratrol attenuates experimental allergic asthma in mice by restoring inositol polyphosphate 4 phosphatase (INPP4A) Int. Immunopharmacol. 2012;14:438–443. doi: 10.1016/j.intimp.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 112.Xia H, Li Y, Lv X. MicroRNA-107 inhibits tumor growth and metastasis by targeting the BDNF-mediated PI3K/AKT pathway in human non-small lung cancer. Int. J. Oncol. 2016;49:1325–1333. doi: 10.3892/ijo.2016.3628. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 113.Lin Y-J, et al. Tumor hypoxia regulates forkhead box C1 to promote lung cancer progression. Theranostics. 2017;7:1177. doi: 10.7150/thno.17895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zhang H, Hu J, Liu L. MiR-200a modulates TGF-β1-induced endothelial-to-mesenchymal shift via suppression of GRB2 in HAECs. Biomed. Pharmacother. 2017;95:215–222. doi: 10.1016/j.biopha.2017.07.104. [DOI] [PubMed] [Google Scholar]
- 115.Zhu X, et al. FoxC1 promotes epithelial-mesenchymal transition through PBX1 dependent transactivation of ZEB2 in esophageal cancer. Am. J. Cancer Res. 2017;7:1642. [PMC free article] [PubMed] [Google Scholar]
- 116.Lin Z, et al. miR‐639 regulates transforming growth factor beta‐induced epithelial–mesenchymal transition in human tongue cancer cells by targeting FOXC 1. Cancer Sci. 2014;105:1288–1298. doi: 10.1111/cas.12499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Liu Y, et al. MicroRNA-200a affects the proliferation of airway smooth muscle cells and airway remodeling by targeting FOXC1 via the PI3K/AKT signaling pathway in ovalbumin-induced asthmatic mice. Cell. Physiol. Biochem. 2018;50:2365–2389. doi: 10.1159/000495097. [DOI] [PubMed] [Google Scholar]
- 118.Huang L, et al. FOXC1 promotes proliferation and epithelial-mesenchymal transition in cervical carcinoma through the PI3K-AKT signal pathway. Am. J. Transl. Res. 2017;9:1297. [PMC free article] [PubMed] [Google Scholar]
- 119.Feng X-J, et al. The PTEN/PI3K/Akt signaling pathway mediates HMGB1-induced cell proliferation by regulating the NF-κB/cyclin D1 pathway in mouse mesangial cells. Am. J. Physiol. Cell Physiol. 2014;306:C1119–C1128. doi: 10.1152/ajpcell.00385.2013. [DOI] [PubMed] [Google Scholar]
- 120.Li C, et al. Involvement of cyclin D1/CDK4 and pRb mediated by PI3K/AKT pathway activation in Pb2+-induced neuronal death in cultured hippocampal neurons. Toxicol. Appl. Pharmacol. 2008;229:351–361. doi: 10.1016/j.taap.2008.01.039. [DOI] [PubMed] [Google Scholar]
- 121.Sun, Y., Luo, D. & Liao, D. J. CyclinD1 protein plays different roles in modulating chemoresponses in MCF7 and MDA-MB231 cells. J. Carcinog.11, 12 (2012). [DOI] [PMC free article] [PubMed]
- 122.Gao N, et al. G1 cell cycle progression and the expression of G1 cyclins are regulated by PI3K/AKT/mTOR/p70S6K1 signaling in human ovarian cancer cells. Am. J. Physiol.Cell Physiol. 2004;287:C281–C291. doi: 10.1152/ajpcell.00422.2003. [DOI] [PubMed] [Google Scholar]
- 123.Wu H, et al. A negative feedback loop between miR‐200b and the nuclear factor‐κB pathway via IKBKB/IKK‐β in breast cancer cells. FEBS J. 2016;283:2259–2271. doi: 10.1111/febs.13543. [DOI] [PubMed] [Google Scholar]
- 124.Bera A, et al. NFκB-mediated cyclin D1 expression by microRNA-21 influences renal cancer cell proliferation. Cell. Signal. 2013;25:2575–2586. doi: 10.1016/j.cellsig.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Chagani T, et al. Fas (CD95) and FasL (CD95L) expression in airway epithelium of subjects with fatal and non-fatal asthma. Am. J. Respir. Crit. Care Med. 2001;163:A739. [Google Scholar]
- 126.Rahimi RA, Leof EB. TGF‐β signaling: a tale of two responses. J. Cell. Biochem. 2007;102:593–608. doi: 10.1002/jcb.21501. [DOI] [PubMed] [Google Scholar]
- 127.Pittet J-F, et al. TGF-β is a critical mediator of acute lung injury. J. Clin. Investig. 2001;107:1537–1544. doi: 10.1172/JCI11963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Miller M, et al. Corticosteroids prevent myofibroblast accumulation and airway remodeling in mice. Am. J. Physiol. Lung Cell. Mol. Physiol. 2006;290:L162–L169. doi: 10.1152/ajplung.00252.2005. [DOI] [PubMed] [Google Scholar]
- 129.Cohn L, Elias JA, Chupp GL. Asthma: mechanisms of disease persistence and progression. Annu. Rev. Immunol. 2004;22:789–815. doi: 10.1146/annurev.immunol.22.012703.104716. [DOI] [PubMed] [Google Scholar]
- 130.Kaur M, Kaur T, Kamboj SS, Singh J. Roles of galectin-7 in cancer. Asian Pac. J. Cancer Prev. 2016;17:455–461. doi: 10.7314/APJCP.2016.17.2.455. [DOI] [PubMed] [Google Scholar]
- 131.Yin G, et al. Galectin-7 is associated with bronchial epithelial cell apoptosis in asthmatic children. Zhonghua er ke za zhi Chin. J. Pediatrics. 2006;44:523–526. [PubMed] [Google Scholar]
- 132.Kuwabara I, et al. Galectin-7 (PIG1) exhibits pro-apoptotic function through JNK activation and mitochondrial cytochrome cRelease. J. Biol. Chem. 2002;277:3487–3497. doi: 10.1074/jbc.M109360200. [DOI] [PubMed] [Google Scholar]
- 133.Vizetto-Duarte C, et al. Isololiolide, a carotenoid metabolite isolated from the brown alga Cystoseira tamariscifolia, is cytotoxic and able to induce apoptosis in hepatocarcinoma cells through caspase-3 activation, decreased Bcl-2 levels, increased p53 expression and PARP cleavage. Phytomedicine. 2016;23:550–557. doi: 10.1016/j.phymed.2016.02.008. [DOI] [PubMed] [Google Scholar]
- 134.Villeneuve C, et al. Mitochondrial proteomic approach reveals galectin-7 as a novel BCL-2 binding protein in human cells. Mol. Biol. Cell. 2011;22:999–1013. doi: 10.1091/mbc.e10-06-0534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sun X, Zhang W. Silencing of Gal-7 inhibits TGF-β1-induced apoptosis of human airway epithelial cells through JNK signaling pathway. Exp. Cell Res. 2019;375:100–105. doi: 10.1016/j.yexcr.2018.12.017. [DOI] [PubMed] [Google Scholar]
- 136.Liu J, Minemoto Y, Lin A. c-Jun N-terminal protein kinase 1 (JNK1), but not JNK2, is essential for tumor necrosis factor alpha-induced c-Jun kinase activation and apoptosis. Mol. Cell. Biol. 2004;24:10844–10856. doi: 10.1128/MCB.24.24.10844-10856.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Li C, et al. Role of c-Jun N-terminal kinase signal transduction pathway in the course of airway remodeling of asthma rat. Zhonghua er ke za zhi Chin. J. Pediatrics. 2008;46:535–539. [PubMed] [Google Scholar]
- 138.Han T, et al. Enhanced expressions of Wnt5a/JNK signaling pathway-related molecules in the lung tissues of asthmatic rats. Xi bao yu fen. zi mian yi xue za zhi Chin. J. Cell. Mol. Immunol. 2015;31:325–327. [PubMed] [Google Scholar]
- 139.De Wever O, et al. Critical role of N-cadherin in myofibroblast invasion and migration in vitro stimulated by colon-cancer-cell-derived TGF-β or wounding. J. cell Sci. 2004;117:4691–4703. doi: 10.1242/jcs.01322. [DOI] [PubMed] [Google Scholar]
- 140.Di Rosanna P, Salvatore C. Reactive oxygen species, inflammation, and lung diseases. Curr. Pharm. Des. 2012;18:3889–3900. doi: 10.2174/138161212802083716. [DOI] [PubMed] [Google Scholar]
- 141.Park SJ, et al. L-2-Oxothiazolidine-4-carboxylic acid or α-lipoic acid attenuates airway remodeling: involvement of nuclear factor-κB (NF-κB), nuclear factor erythroid 2p45-related factor-2 (Nrf2), and hypoxia-inducible factor (HIF) Int. J. Mol. Sci. 2012;13:7915–7937. doi: 10.3390/ijms13077915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Zeng H, et al. Polydatin attenuates reactive oxygen species-induced airway remodeling by promoting Nrf2-mediated antioxidant signaling in asthma mouse model. Life Sci. 2019;218:25–30. doi: 10.1016/j.lfs.2018.08.013. [DOI] [PubMed] [Google Scholar]
- 143.Huang K, et al. Polydatin promotes Nrf2-ARE anti-oxidative pathway through activating Sirt1 to resist AGEs-induced upregulation of fibronetin and transforming growth factor-β1 in rat glomerular messangial cells. Mol. Cell. Endocrinol. 2015;399:178–189. doi: 10.1016/j.mce.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 144.Lachapelle P, Li M, Douglass J, Stewart A. Safer approaches to therapeutic modulation of TGF-β signaling for respiratory disease. Pharmacol. Ther. 2018;187:98–113. doi: 10.1016/j.pharmthera.2018.02.010. [DOI] [PubMed] [Google Scholar]
- 145.Zissler U, et al. Current and future biomarkers in allergic asthma. Allergy. 2016;71:475–494. doi: 10.1111/all.12828. [DOI] [PubMed] [Google Scholar]
- 146.Ding F, Fu Z, Liu B. Lipopolysaccharide exposure alleviates asthma in mice by regulating Th1/Th2 and Treg/Th17 balance. Med. Sci. Monit. 2018;24:3220. doi: 10.12659/MSM.905202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Liang P, et al. Huai Qi Huang corrects the balance of Th1/Th2 and Treg/Th17 in an ovalbumin-induced asthma mouse model. Biosci. Rep. 2017;37:BSR20171071. doi: 10.1042/BSR20171071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Na, H. et al. Concomitant suppression of TH2 and TH17 cell responses in allergic asthma by targeting retinoic acid receptor–related orphan receptor γt. J. Allergy Clin. Immunol.141, 2061–2073 (2018). [DOI] [PMC free article] [PubMed]
- 149.Chen, T. et al. The imbalance of FOXP3/GATA3 in egulatory T cells from the peripheral blood of asthmatic patients. J. Immunol. Res.2018, 1–10 (2018). [DOI] [PMC free article] [PubMed]
- 150.Zhu Y, et al. Analysis of lncRNA expression in patients with eosinophilic and neutrophilic asthma focusing on LNC_000127. Front. Genet. 2019;10:141. doi: 10.3389/fgene.2019.00141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zhang X-y, et al. GAS5 promotes airway smooth muscle cell proliferation in asthma via controlling miR-10a/BDNF signaling pathway. Life Sci. 2018;212:93–101. doi: 10.1016/j.lfs.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 152.Zhu, Y.-J., Mao, D., Gao, W. & Hu, H. Peripheral whole blood lncRNA expression analysis in patients with eosinophilic asthma. Medicine97, e9817 (2018). [DOI] [PMC free article] [PubMed]
- 153.Narożna B, Langwiński W, Szczepankiewicz A. Non-coding RNAs in pediatric airway diseases. Genes. 2017;8:348. doi: 10.3390/genes8120348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Qiu Y-y, et al. LncRNA-MEG3 functions as a competing endogenous RNA to regulate Treg/Th17 balance in patients with asthma by targeting microRNA-17/RORγt. Biomed. Pharmacother. 2019;111:386–394. doi: 10.1016/j.biopha.2018.12.080. [DOI] [PubMed] [Google Scholar]
- 155.Paplińska M, et al. Expression of eotaxins in the material from nasal brushing in asthma, allergic rhinitis and COPD patients. Cytokine. 2012;60:393–399. doi: 10.1016/j.cyto.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 156.Shieh Y-H, et al. Zerumbone enhances the Th1 response and ameliorates ovalbumin-induced Th2 responses and airway inflammation in mice. Int. Immunopharmacol. 2015;24:383–391. doi: 10.1016/j.intimp.2014.12.027. [DOI] [PubMed] [Google Scholar]
- 157.Gui-min, G. The progress of eotaxin and the association with ashtma. Int J. Immunol.2, 93–96 (2006).
- 158.Yuan F, et al. JAX2, an ethanol extract of Hyssopus cuspidatus Boriss, can prevent bronchial asthma by inhibiting MAPK/NF-κB inflammatory signaling. Phytomedicine. 2019;57:305–314. doi: 10.1016/j.phymed.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 159.Henderson WR, Jr, et al. A role for cysteinyl leukotrienes in airway remodeling in a mouse asthma model. Am. J. Respir. Crit. Care Med. 2002;165:108–116. doi: 10.1164/ajrccm.165.1.2105051. [DOI] [PubMed] [Google Scholar]
- 160.Dahlen S-E. Pharmacological characterization of leukotriene receptors. Am. J. Respir. Crit. Care Med. 2000;161:S41–S45. doi: 10.1164/ajrccm.161.supplement_1.ltta-9. [DOI] [PubMed] [Google Scholar]
- 161.Gauvreau GM, Parameswaran KN, Watson RM, O'BYRNE PM. Inhaled leukotriene E4, but not leukotriene D4, increased airway inflammatory cells in subjects with atopic asthma. Am. J. Respir. Crit. Care Med. 2001;164:1495–1500. doi: 10.1164/ajrccm.164.8.2102033. [DOI] [PubMed] [Google Scholar]
- 162.Suh DH, et al. P2Y12 antagonist attenuates eosinophilic inflammation and airway hyperresponsiveness in a mouse model of asthma. J. Cell. Mol. Med. 2016;20:333–341. doi: 10.1111/jcmm.12727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kanaoka Y, Boyce JA. Cysteinyl leukotrienes and their receptors; emerging concepts. Allerg. Asthma Immunol. Res. 2014;6:288–295. doi: 10.4168/aair.2014.6.4.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Kanaoka Y, Maekawa A, Austen KF. Identification of GPR99 protein as a potential third cysteinyl leukotriene receptor with a preference for leukotriene E4 ligand. J. Biol. Chem. 2013;288:10967–10972. doi: 10.1074/jbc.C113.453704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Trinh HKT, et al. Characterization of cysteinyl leukotriene-related receptors and their interactions in a mouse model of asthma. Prostaglandins, Leukotrienes Essent. Fat. Acids. 2019;141:17–23. doi: 10.1016/j.plefa.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 166.Paruchuri S, et al. Leukotriene E4–induced pulmonary inflammation is mediated by the P2Y12 receptor. J. Exp. Med. 2009;206:2543–2555. doi: 10.1084/jem.20091240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Raker VK, Becker C, Steinbrink K. The cAMP pathway as therapeutic target in autoimmune and inflammatory diseases. Front. Immunol. 2016;7:123. doi: 10.3389/fimmu.2016.00123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ahmad F, et al. Cyclic nucleotide phosphodiesterases: important signaling modulators and therapeutic targets. Oral. Dis. 2015;21:e25–e50. doi: 10.1111/odi.12275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Bateman, E. D., Goehring, U.-M., Richard, F. & Watz, H. Roflumilast combined with montelukast versus montelukast alone as add-on treatment in patients with moderate-to-severe asthma. J. Allergy Clin. Immunol.138, 142–149 (2016). [DOI] [PubMed]
- 170.Southworth T, et al. Anti-inflammatory effects of the phosphodiesterase type 4 inhibitor CHF6001 on bronchoalveolar lavage lymphocytes from asthma patients. Cytokine. 2019;113:68–73. doi: 10.1016/j.cyto.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 171.Woodruff PG, et al. Genome-wide profiling identifies epithelial cell genes associated with asthma and with treatment response to corticosteroids. Proc. Natl Acad. Sci. 2007;104:15858–15863. doi: 10.1073/pnas.0707413104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Grundy S, et al. Additive anti-inflammatory effects of corticosteroids and phosphodiesterase-4 inhibitors in COPD CD8 cells. Respiratory Res. 2016;17:9. doi: 10.1186/s12931-016-0325-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Goleva E, et al. The effects of airway microbiome on corticosteroid responsiveness in asthma. Am. J. Respi. Crit. Care Med. 2013;188:1193–1201. doi: 10.1164/rccm.201304-0775OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Bjørgo E, Taskén K. Novel mechanism of signaling by CD28. Immunol. Lett. 2010;129:1–6. doi: 10.1016/j.imlet.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 175.Barnes PJ. Corticosteroid resistance in patients with asthma and chronic obstructive pulmonary disease. J. Allergy Clin. Immunol. 2013;131:636–645. doi: 10.1016/j.jaci.2012.12.1564. [DOI] [PubMed] [Google Scholar]
- 176.Matera MG, Page C, Rinaldi B. β2-Adrenoceptor signalling bias in asthma and COPD and the potential impact on the comorbidities associated with these diseases. Curr. Opin. Pharmacol. 2018;40:142–146. doi: 10.1016/j.coph.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 177.Johnson M. Molecular mechanisms of β2-adrenergic receptor function, response, and regulation. J. Allergy Clin. Immunol. 2006;117:18–24. doi: 10.1016/j.jaci.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 178.Krug N, et al. Enhanced expression of fas ligand (CD95L) on T cells after segmental allergen provocation in asthma. J. Allergy Clin. Immunol. 1999;103:649–655. doi: 10.1016/S0091-6749(99)70238-1. [DOI] [PubMed] [Google Scholar]
- 179.Müller M, et al. Altered apoptosis in bronchoalveolar lavage lymphocytes after allergen exposure of atopic asthmatic subjects. Eur. Respir. J. 2006;28:513–522. doi: 10.1183/09031936.06.00118505. [DOI] [PubMed] [Google Scholar]
- 180.Druilhe A, et al. Apoptosis, proliferation, and expression of Bcl-2, Fas, and Fas ligand in bronchial biopsies from asthmatics. Am. J. Respir. C ell Mol. Biol. 1998;19:747–757. doi: 10.1165/ajrcmb.19.5.3166. [DOI] [PubMed] [Google Scholar]
- 181.Le Gallo M, Poissonnier A, Blanco P, Legembre P. CD95/Fas, non-apoptotic signaling pathways, and kinases. Front. Immunol. 2017;8:1216. doi: 10.3389/fimmu.2017.01216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Peter ME, et al. The role of CD95 and CD95 ligand in cancer. Cell Death Differ. 2015;22:549. doi: 10.1038/cdd.2015.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Krammer PH, Arnold R, Lavrik IN. Life and death in peripheral T cells. Nat. Rev. Immunol. 2007;7:532. doi: 10.1038/nri2115. [DOI] [PubMed] [Google Scholar]
- 184.Park S-M, Schickel R, Peter ME. Nonapoptotic functions of FADD-binding death receptors and their signaling molecules. Curr. Opin. Cell Biol. 2005;17:610–616. doi: 10.1016/j.ceb.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 185.Desbarats J, et al. Fas engagement induces neurite growth through ERK activation and p35 upregulation. Nat. Cell Biol. 2003;5:118. doi: 10.1038/ncb916. [DOI] [PubMed] [Google Scholar]
- 186.Neumann, L. et al. Dynamics within the CD95 death‐inducing signaling complex decide life and death of cells. Mol. Syst. Biol. 6 (2010). [DOI] [PMC free article] [PubMed]
- 187.Kleber S, et al. Yes and PI3K bind CD95 to signal invasion of glioblastoma. Cancer Cell. 2008;13:235–248. doi: 10.1016/j.ccr.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 188.Wisniewski P, Ellert-Miklaszewska A, Kwiatkowska A, Kaminska B. Non-apoptotic Fas signaling regulates invasiveness of glioma cells and modulates MMP-2 activity via NFκB-TIMP-2 pathway. Cell Signal. 2010;22:212–220. doi: 10.1016/j.cellsig.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 189.Fang Y, et al. Comparison of sensitivity of Th1, Th2, and Th17 cells to Fas‐mediated apoptosis. J. Leukoc. Biol. 2010;87:1019–1028. doi: 10.1189/jlb.0509352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Williams JW, et al. Non-apoptotic Fas (CD95) signaling on T cells regulates the resolution of Th2-mediated inflammation. Front. Immunol. 2018;9:2521. doi: 10.3389/fimmu.2018.02521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Liu Y, et al. Protective effect of electro-acupuncture at maternal different points on perinatal nicotine exposure-induced pulmonary dysplasia in offspring based on HPA axis and signal transduction pathway. Biochem. B iophys. Res. Commun. 2018;505:586–592. doi: 10.1016/j.bbrc.2018.09.145. [DOI] [PubMed] [Google Scholar]
- 192.Rehan, V. K. & Torday, J. S. PPARγ signaling mediates the evolution, development, homeostasis, and repair of the lung. PPAR Res.2012 (2012). [DOI] [PMC free article] [PubMed]
- 193.Rijken D, Sakharov D. Basic principles in thrombolysis: regulatory role of plasminogen. Thrombosis Res. 2001;103:S41–S49. doi: 10.1016/S0049-3848(01)00296-1. [DOI] [PubMed] [Google Scholar]
- 194.Cho SH, Ryu CH, Oh CK. Plasminogen activator inhibitor-1 in the pathogenesis of asthma. Exp. Biol. Med. 2004;229:138–146. doi: 10.1177/153537020422900202. [DOI] [PubMed] [Google Scholar]
- 195.Lee SH, et al. A plasminogen activator inhibitor-1 inhibitor reduces airway remodeling in a murine model of chronic asthma. Am. J. Respir. C ell Mol. Biol. 2012;46:842–846. doi: 10.1165/rcmb.2011-0369OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Miyamoto S, et al. Intra-airway administration of small interfering RNA targeting plasminogen activator inhibitor-1 attenuates allergic asthma in mice. Am. J. Physiol. Lung Cell. Mol. Physiol. 2011;301:L908–L916. doi: 10.1152/ajplung.00115.2011. [DOI] [PubMed] [Google Scholar]
- 197.Denzel A, et al. Basophils enhance immunological memory responses. Nat. Immunol. 2008;9:733. doi: 10.1038/ni.1621. [DOI] [PubMed] [Google Scholar]
- 198.Mukai K, Obata K, Tsujimura Y, Karasuyama H. New insights into the roles for basophils in acute and chronic allergy. Allergol. Int. 2009;58:11–19. doi: 10.2332/allergolint.08-RAI-0059. [DOI] [PubMed] [Google Scholar]
- 199.Prussin C, Metcalfe DD. 4. IgE, mast cells, basophils, and eosinophils. J. Allergy Clin. Immunol. 2003;111:S486–S494. doi: 10.1067/mai.2003.120. [DOI] [PubMed] [Google Scholar]
- 200.Sokol CL, Barton GM, Farr AG, Medzhitov R. A mechanism for the initiation of allergen-induced T helper type 2 responses. Nat. Immunol. 2008;9:310. doi: 10.1038/ni1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Liu Y, et al. An essential role for RasGRP1 in mast cell function and IgE-mediated allergic response. J. Exp. Med. 2007;204:93–103. doi: 10.1084/jem.20061598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Zhu M, et al. Positive and negative regulation of FcεRI-mediated signaling by the adaptor protein LAB/NTAL. J. Exp. Med. 2004;200:991–1000. doi: 10.1084/jem.20041223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Zhu M, Rhee I, Liu Y, Zhang W. Negative regulation of FcϵRI-mediated signaling and mast cell function by the adaptor protein LAX. J. Biol. Chem. 2006;281:18408–18413. doi: 10.1074/jbc.M601535200. [DOI] [PubMed] [Google Scholar]
- 204.Kinet J-P. The high-affinity IgE receptor (FcεRI): from physiology to pathology. Annu. Rev. Immunol. 1999;17:931–972. doi: 10.1146/annurev.immunol.17.1.931. [DOI] [PubMed] [Google Scholar]
- 205.Gilfillan AM, Tkaczyk C. Integrated signalling pathways for mast-cell activation. Nat. Rev. Immunol. 2006;6:218. doi: 10.1038/nri1782. [DOI] [PubMed] [Google Scholar]
- 206.Li P, et al. BATF–JUN is critical for IRF4-mediated transcription in T cells. Nature. 2012;490:543. doi: 10.1038/nature11530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Lu Y, et al. The natural compound nujiangexanthone A suppresses mast cell activation and allergic asthma. Biochem. Pharmacol. 2016;100:61–72. doi: 10.1016/j.bcp.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 208.Kitaura J, et al. Regulation of highly cytokinergic IgE-induced mast cell adhesion by Src, Syk, Tec, and protein kinase C family kinases. J. Immunol. 2005;174:4495–4504. doi: 10.4049/jimmunol.174.8.4495. [DOI] [PubMed] [Google Scholar]
- 209.Weinblatt ME, et al. An oral spleen tyrosine kinase (Syk) inhibitor for rheumatoid arthritis. New Engl. J. Med. 2010;363:1303–1312. doi: 10.1056/NEJMoa1000500. [DOI] [PubMed] [Google Scholar]
- 210.Zhang W, et al. Lipopolysaccharide mediates time-dependent macrophage M1/M2 polarization through the Tim-3/Galectin-9 signalling pathway. Exp. C ell Res. 2019;376:124–132. doi: 10.1016/j.yexcr.2019.02.007. [DOI] [PubMed] [Google Scholar]
- 211.Aggarwal NR, King LS, D'Alessio FR. Diverse macrophage populations mediate acute lung inflammation and resolution. Am. J. Physiol.Lung Cell. Mol. Physiol. 2014;306:L709–L725. doi: 10.1152/ajplung.00341.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Liu G, Yang H. Modulation of macrophage activation and programming in immunity. J. Cell. Physiol. 2013;228:502–512. doi: 10.1002/jcp.24157. [DOI] [PubMed] [Google Scholar]
- 213.Tang L, et al. M2A and M2C macrophage subsets ameliorate inflammation and fibroproliferation in acute lung injury through interleukin 10 pathway. Shock. 2017;48:119–129. doi: 10.1097/SHK.0000000000000820. [DOI] [PubMed] [Google Scholar]
- 214.Han G, Chen G, Shen B, Li Y. Tim-3: an activation marker and activation limiter of innate immune cells. Front. Immunol. 2013;4:449. doi: 10.3389/fimmu.2013.00449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Sabatos CA, et al. Interaction of Tim-3 and Tim-3 ligand regulates T helper type 1 responses and induction of peripheral tolerance. Nat. Immunol. 2003;4:1102. doi: 10.1038/ni988. [DOI] [PubMed] [Google Scholar]
- 216.Toshchakov V, et al. TLR4, but not TLR2, mediates IFN-β–induced STAT1α/β-dependent gene expression in macrophages. Nat. Immunol. 2002;3:392. doi: 10.1038/ni774. [DOI] [PubMed] [Google Scholar]
- 217.Lee J, et al. Phosphotyrosine-dependent coupling of Tim-3 to T-cell receptor signaling pathways. Mol. Cell. Biol. 2011;31:3963–3974. doi: 10.1128/MCB.05297-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Anderson AC, et al. Promotion of tissue inflammation by the immune receptor Tim-3 expressed on innate immune cells. Science. 2007;318:1141–1143. doi: 10.1126/science.1148536. [DOI] [PubMed] [Google Scholar]
- 219.Guha M, Mackman N. The phosphatidylinositol 3-kinase-Akt pathway limits lipopolysaccharide activation of signaling pathways and expression of inflammatory mediators in human monocytic cells. J. Biol. Chem. 2002;277:32124–32132. doi: 10.1074/jbc.M203298200. [DOI] [PubMed] [Google Scholar]
- 220.Ma CJ, et al. Cis association of galectin-9 with Tim-3 differentially regulates IL-12/IL-23 expressions in monocytes via TLR signaling. PloS ONE. 2013;8:e72488. doi: 10.1371/journal.pone.0072488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Makita N, et al. IL-10 enhances the phenotype of M2 macrophages induced by IL-4 and confers the ability to increase eosinophil migration. Int. Immunol. 2014;27:131–141. doi: 10.1093/intimm/dxu090. [DOI] [PubMed] [Google Scholar]
- 222.Zhang, Y. et al. Eosinophils reduce chronic inflammation in adipose tissue by secreting Th2 cytokines and promoting M2 macrophages polarization. Int. J. Endocrin. 2015, 1–5 (2015). [DOI] [PMC free article] [PubMed]
- 223.Lopez-Santalla M, et al. AB0176 P38 MAPK phosphorylation as a rheumatoid arthritis biomarker. Ann. Rheum. Dis. 2013;71:647–647. doi: 10.1136/annrheumdis-2012-eular.176. [DOI] [Google Scholar]
- 224.Karin, M. & Delhase, M. The I kappa B kinase (IKK) and NF-kappa B: key elements of proinflammatory signalling. Semin Immunol. 12, 85–98 (2000). [DOI] [PubMed]
- 225.O'Sullivan AW, Wang JH, Redmond HP. NF-κB and P38 MAPK inhibition improve survival in endotoxin shock and in a cecal ligation and puncture model of sepsis in combination with antibiotic therapy. J. Surg. Res. 2009;152:46–53. doi: 10.1016/j.jss.2008.04.030. [DOI] [PubMed] [Google Scholar]
- 226.Liu L, et al. Eosinophils attenuate arthritis by inducing M2 macrophage polarization via inhibiting the IκB/P38 MAPK signaling pathway. Biochem. B iophys. Res. Commun. 2019;508:894–901. doi: 10.1016/j.bbrc.2018.12.010. [DOI] [PubMed] [Google Scholar]
- 227.Wu D, et al. Eosinophils sustain adipose alternatively activated macrophages associated with glucose homeostasis. Science. 2011;332:243–247. doi: 10.1126/science.1201475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Molofsky AB, et al. Innate lymphoid type 2 cells sustain visceral adipose tissue eosinophils and alternatively activated macrophages. J. Exp. Med. 2013;210:535–549. doi: 10.1084/jem.20121964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Schneider C, et al. Frontline science: coincidental null mutation of Csf2rα in a colony of PI3Kγ−/− mice causes alveolar macrophage deficiency and fatal respiratory viral infection. J. Leukoc. Biol. 2017;101:367–376. doi: 10.1189/jlb.4HI0316-157R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Nobs, S. P., Kayhan, M. & Kopf, M. GM-CSF intrinsically controls eosinophil accumulation in the setting of allergic airway inflammation. J. Allergy Clin. Immunol.143, 1513–1524 (2019). [DOI] [PubMed]
- 231.Schneider C, et al. Alveolar macrophages are essential for protection from respiratory failure and associated morbidity following influenza virus infection. PLoS Pathog. 2014;10:e1004053. doi: 10.1371/journal.ppat.1004053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Kopf M, et al. IL-5-deficient mice have a developmental defect in CD5+ B-1 cells and lack eosinophilia but have normal antibody and cytotoxic T cell responses. Immunity. 1996;4:15–24. doi: 10.1016/S1074-7613(00)80294-0. [DOI] [PubMed] [Google Scholar]
- 233.Gaurav R, Agrawal DK. Clinical view on the importance of dendritic cells in asthma. Expert Rev. Clin. Immunol. 2013;9:899–919. doi: 10.1586/1744666X.2013.837260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Chen K, Kolls JK. T Cell–mediated host immune defenses in the lung. Annu. Rev. Immunol. 2013;31:605–633. doi: 10.1146/annurev-immunol-032712-100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Aderem A, Ulevitch RJ. Toll-like receptors in the induction of the innate immune response. Nature. 2000;406:782. doi: 10.1038/35021228. [DOI] [PubMed] [Google Scholar]
- 236.Akira S, Takeda K, Kaisho T. Toll-like receptors: critical proteins linking innate and acquired immunity. Nat. Immunol. 2001;2:675. doi: 10.1038/90609. [DOI] [PubMed] [Google Scholar]
- 237.Eder W, et al. Toll-like receptor 2 as a major gene for asthma in children of European farmers. J. allergy Clin. Immunol. 2004;113:482–488. doi: 10.1016/j.jaci.2003.12.374. [DOI] [PubMed] [Google Scholar]
- 238.Casanova J-L, Abel L, Quintana-Murci L. Human TLRs and IL-1Rs in host defense: natural insights from evolutionary, epidemiological, and clinical genetics. Annu. Rev. Immunol. 2011;29:447–491. doi: 10.1146/annurev-immunol-030409-101335. [DOI] [PubMed] [Google Scholar]
- 239.Takeda K, Akira S. Toll-like receptors in innate immunity. Int. Immunol. 2005;17:1–14. doi: 10.1093/intimm/dxh186. [DOI] [PubMed] [Google Scholar]
- 240.Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124:783–801. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 241.Peng J, et al. SARM inhibits both TRIF‐and MyD88‐mediated AP‐1 activation. Eur. J. Immunol. 2010;40:1738–1747. doi: 10.1002/eji.200940034. [DOI] [PubMed] [Google Scholar]
- 242.Mansell A, et al. Suppressor of cytokine signaling 1 negatively regulates Toll-like receptor signaling by mediating Mal degradation. Nat. Immunol. 2006;7:148. doi: 10.1038/ni1299. [DOI] [PubMed] [Google Scholar]
- 243.Han C, et al. Integrin CD11b negatively regulates TLR-triggered inflammatory responses by activating Syk and promoting degradation of MyD88 and TRIF via Cbl-b. Nat. Immunol. 2010;11:734. doi: 10.1038/ni.1908. [DOI] [PubMed] [Google Scholar]
- 244.Palsson-McDermott EM, et al. TAG, a splice variant of the adaptor TRAM, negatively regulates the adaptor MyD88–independent TLR4 pathway. Nat. Immunol. 2009;10:579. doi: 10.1038/ni.1727. [DOI] [PubMed] [Google Scholar]
- 245.Zakeri A, Yazdi FG. Toll-like receptor-mediated involvement of innate immune cells in asthma disease. Biochim. Biophys. Acta Gen. Subj. 2017;1861:3270–3277. doi: 10.1016/j.bbagen.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 246.Matesic D, Lenert A, Lenert P. Modulating toll-like receptor 7 and 9 responses as therapy for allergy and autoimmunity. Curr. Allergy Asthma Rep. 2012;12:8–17. doi: 10.1007/s11882-011-0233-4. [DOI] [PubMed] [Google Scholar]
- 247.Lefkowitz RJ, Rajagopal K, Whalen EJ. New roles for β-arrestins in cell signaling: not just for seven-transmembrane receptors. Mol. Cell. 2006;24:643–652. doi: 10.1016/j.molcel.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 248.Lefkowitz RJ, Whalen EJ. β-arrestins: traffic cops of cell signaling. Curr. Opin. Cell Biol. 2004;16:162–168. doi: 10.1016/j.ceb.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 249.Walker JK, DeFea KA. Role for β-arrestin in mediating paradoxical β2AR and PAR2 signaling in asthma. Curr. Opin. Pharmacol. 2014;16:142–147. doi: 10.1016/j.coph.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Shenoy, S. K. & Lefkowitz, R. J. Seven-transmembrane receptor signaling through β-arrestin. Sci. Signal.2005, cm10 (2005). [DOI] [PubMed]
- 251.Nichols HL, et al. β-Arrestin-2 mediates the proinflammatory effects of proteinase-activated receptor-2 in the airway. Proc. Natl Acad. Sci. 2012;109:16660–16665. doi: 10.1073/pnas.1208881109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Walker JK, et al. β-Arrestin-2 regulates the development of allergic asthma. J. Clin. Investig. 2003;112:566–574. doi: 10.1172/JCI200317265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Hollingsworth JW, et al. Both hematopoietic-derived and non–hematopoietic-derived β-arrestin–2 regulates murine allergic airway disease. Am. J. Respir. Cell Mol. Biol. 2010;43:269–275. doi: 10.1165/rcmb.2009-0198OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Shenoy SK, et al. β-Arrestin-dependent, G protein-independent ERK1/2 activation by the β2 adrenergic receptor. J. Biol. Chem. 2006;281:1261–1273. doi: 10.1074/jbc.M506576200. [DOI] [PubMed] [Google Scholar]
- 255.Billington CK, Penn RB. Signaling and regulation of G protein-coupled receptors in airway smooth muscle. Respir. Res. 2003;4:4. doi: 10.1186/1465-9921-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Kaulmann A, Bohn T. Carotenoids, inflammation, and oxidative stress—implications of cellular signaling pathways and relation to chronic disease prevention. Nutr. Res. 2014;34:907–929. doi: 10.1016/j.nutres.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 257.Chen X-L, et al. Activation of Nrf2/ARE pathway protects endothelial cells from oxidant injury and inhibits inflammatory gene expression. Am. J. Physiol. Heart Circul. Physiol. 2006;290:H1862–H1870. doi: 10.1152/ajpheart.00651.2005. [DOI] [PubMed] [Google Scholar]
- 258.Kaplan, M. H. STAT signaling in inflammation. JAKSTAT. 2, e24198 (2013). [DOI] [PMC free article] [PubMed]
- 259.Braun S, et al. Nrf2 transcription factor, a novel target of keratinocyte growth factor action which regulates gene expression and inflammation in the healing skin wound. Mol. Cell Biol. 2002;22:5492–5505. doi: 10.1128/MCB.22.15.5492-5505.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Wang H, et al. RXRα inhibits the NRF2-ARE signaling pathway through a direct interaction with the Neh7 domain of NRF2. Cancer Res. 2013;73:3097–3108. doi: 10.1158/0008-5472.CAN-12-3386. [DOI] [PubMed] [Google Scholar]
- 261.Plafker KS, et al. The ubiquitin-conjugating enzyme UbcM2 can regulate the stability and activity of the antioxidant transcription factor Nrf2. J. Biol. Chem. 2010;285:23064–23074. doi: 10.1074/jbc.M110.121913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Wang XJ, et al. Oxaliplatin activates the Keap1/Nrf2 antioxidant system conferring protection against the cytotoxicity of anticancer drugs. Free Radic. Biol. Med. 2014;70:68–77. doi: 10.1016/j.freeradbiomed.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 263.Canning P, Sorrell FJ, Bullock AN. Structural basis of Keap1 interactions with Nrf2. Free Radic. Biol. Med. 2015;88:101–107. doi: 10.1016/j.freeradbiomed.2015.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Kim J-H, Yu S, Chen JD, Kong A-N. The nuclear cofactor RAC3/AIB1/SRC-3 enhances Nrf2 signaling by interacting with transactivation domains. Oncogene. 2013;32:514. doi: 10.1038/onc.2012.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Nioi P, Nguyen T, Sherratt PJ, Pickett CB. The carboxy-terminal Neh3 domain of Nrf2 is required for transcriptional activation. Mol. Cell. Biol. 2005;25:10895–10906. doi: 10.1128/MCB.25.24.10895-10906.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Li W, Yu S-W, Kong A-NT. Nrf2 possesses a redox-sensitive nuclear exporting signal in the Neh5 transactivation domain. J. Biol. Chem. 2006;281:27251–27263. doi: 10.1074/jbc.M602746200. [DOI] [PubMed] [Google Scholar]
- 267.Tong KI, et al. Different electrostatic potentials define ETGE and DLG motifs as hinge and latch in oxidative stress response. Mol. Cell. Biol. 2007;27:7511–7521. doi: 10.1128/MCB.00753-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Cullinan SB, et al. The Keap1-BTB protein is an adaptor that bridges Nrf2 to a Cul3-based E3 ligase: oxidative stress sensing by a Cul3-Keap1 ligase. Mol. Cell. Biol. 2004;24:8477–8486. doi: 10.1128/MCB.24.19.8477-8486.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Hayes JD, McMahon M, Chowdhry S, Dinkova-Kostova AT. Cancer chemoprevention mechanisms mediated through the Keap1–Nrf2 pathway. Antioxid. Redox Signal. 2010;13:1713–1748. doi: 10.1089/ars.2010.3221. [DOI] [PubMed] [Google Scholar]
- 270.Ahmed SMU, et al. Nrf2 signaling pathway: pivotal roles in inflammation. Biochim. Biophys. Acta. 2017;1863:585–597. doi: 10.1016/j.bbadis.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 271.Rada P, et al. SCF/β-TrCP promotes glycogen synthase kinase 3-dependent degradation of the Nrf2 transcription factor in a Keap1-independent manner. Mol. Cell Biol. 2011;31:1121–1133. doi: 10.1128/MCB.01204-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Chowdhry S, et al. Nrf2 is controlled by two distinct β-TrCP recognition motifs in its Neh6 domain, one of which can be modulated by GSK-3 activity. Oncogene. 2013;32:3765. doi: 10.1038/onc.2012.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Prestera T, et al. Parallel induction of heme oxygenase-1 and chemoprotective phase 2 enzymes by electrophiles and antioxidants: regulation by upstream antioxidant-responsive elements (ARE) Mol. Med. 1995;1:827–837. doi: 10.1007/BF03401897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Wunder C, Potter RF. The heme oxygenase system: its role in liver inflammation. Curr. Drug Targets Cardiovasc. Hematol. Disord. 2003;3:199–208. doi: 10.2174/1568006033481410. [DOI] [PubMed] [Google Scholar]
- 275.Bauernfeind FG, et al. Cutting edge: NF-κB activating pattern recognition and cytokine receptors license NLRP3 inflammasome activation by regulating NLRP3 expression. J. Immunol. 2009;183:787–791. doi: 10.4049/jimmunol.0901363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Strowig T, Henao-Mejia J, Elinav E, Flavell R. Inflammasomes in health and disease. Nature. 2012;481:278. doi: 10.1038/nature10759. [DOI] [PubMed] [Google Scholar]
- 277.Koziol-White CJ, Panettieri RA. Modulation of bronchomotor tone pathways in airway smooth muscle function and bronchomotor tone in asthma. Clin. Chest Med. 2019;40:51–57. doi: 10.1016/j.ccm.2018.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Jude JA, Wylam ME, Walseth TF, Kannan MS. Calcium signaling in airway smooth muscle. Proc. Am. Thorac. Soc. 2008;5:15–22. doi: 10.1513/pats.200704-047VS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Yoo EJ, et al. Gα12 facilitates shortening in human airway smooth muscle by modulating phosphoinositide 3‐kinase‐mediated activation in a RhoA‐dependent manner. Br. J. Pharmacol. 2017;174:4383–4395. doi: 10.1111/bph.14040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Tliba O, et al. IL‐13 enhances agonist‐evoked calcium signals and contractile responses in airway smooth muscle. Br. J. Pharmacol. 2003;140:1159–1162. doi: 10.1038/sj.bjp.0705558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Chiba Y, et al. Interleukin-13 augments bronchial smooth muscle contractility with an up-regulation of RhoA protein. Am. J. Respir. Cell Mol. Biol. 2009;40:159–167. doi: 10.1165/rcmb.2008-0162OC. [DOI] [PubMed] [Google Scholar]
- 282.Young HW, et al. Central role of Muc5ac expression in mucous metaplasia and its regulation by conserved 5′ elements. Am. J. respiratory cell Mol. Biol. 2007;37:273–290. doi: 10.1165/rcmb.2005-0460OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Hoshino M, et al. Increased expression of the human Ca2+-activated Cl− channel 1 (CaCC1) gene in the asthmatic airway. Am. J. Respir. Crit. Care Med. 2002;165:1132–1136. doi: 10.1164/ajrccm.165.8.2107068. [DOI] [PubMed] [Google Scholar]
- 284.Alevy YG, et al. IL-13–induced airway mucus production is attenuated by MAPK13 inhibition. J. Clin. Investig. 2012;122:4555–4568. doi: 10.1172/JCI64896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Park K-S, et al. SPDEF regulates goblet cell hyperplasia in the airway epithelium. J. Clin. Investig. 2007;117:978–988. doi: 10.1172/JCI29176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Ren X, et al. FOXM1 promotes allergen-induced goblet cell metaplasia and pulmonary inflammation. Mol. Cell Biol. 2013;33:371–386. doi: 10.1128/MCB.00934-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Korfhagen TR, et al. SAM-pointed domain ETS factor mediates epithelial cell–intrinsic innate immune signaling during airway mucous metaplasia. Proc. Natl Acad. Sci. 2012;109:16630–16635. doi: 10.1073/pnas.1208092109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Le Cras TD, et al. Epithelial EGF receptor signaling mediates airway hyperreactivity and remodeling in a mouse model of chronic asthma. Am. J. Physiol.Lung Cell. Mol. Physiol. 2010;300:L414–L421. doi: 10.1152/ajplung.00346.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Shao MX, Nadel JA. Dual oxidase 1-dependent MUC5AC mucin expression in cultured human airway epithelial cells. Proc. Natl Acad. Sci. 2005;102:767–772. doi: 10.1073/pnas.0408932102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Perrais, M. et al. Induction of MUC2 and MUC5AC mucin by factors of the epidermal growth factor family is mediated by EGF-R/Ras/Raf/MAPK signaling cascade and Sp1. J. Biol. Chem. 277, 32258–32267(2002). [DOI] [PubMed]
- 291.Erle DJ, Sheppard D. The cell biology of asthma. J. Cell Biol. 2014;205:621–631. doi: 10.1083/jcb.201401050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Zhang S, et al. Jagged1 is the major regulator of Notch‐dependent cell fate in proximal airways. Dev. Dyn. 2013;242:678–686. doi: 10.1002/dvdy.23965. [DOI] [PubMed] [Google Scholar]
- 293.Ou-Yang H-F, Wu C-G, Qu S-Y, Li Z-K. Notch signaling downregulates MUC5AC expression in airway epithelial cells through Hes1-dependent mechanisms. Respiration. 2013;86:341–346. doi: 10.1159/000350647. [DOI] [PubMed] [Google Scholar]
- 294.Nutku E, Aizawa H, Hudson SA, Bochner BS. Ligation of Siglec-8: a selective mechanism for induction of human eosinophil apoptosis. Blood. 2003;101:5014–5020. doi: 10.1182/blood-2002-10-3058. [DOI] [PubMed] [Google Scholar]
- 295.Bochner BS. Siglec‐8 on human eosinophils and mast cells, and Siglec‐F on murine eosinophils, are functionally related inhibitory receptors. Clin. Exp. Allergy. 2009;39:317–324. doi: 10.1111/j.1365-2222.2008.03173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Munitz A, et al. The inhibitory receptor IRp60 (CD300a) suppresses the effects of IL-5, GM-CSF, and eotaxin on human peripheral blood eosinophils. Blood. 2006;107:1996–2003. doi: 10.1182/blood-2005-07-2926. [DOI] [PubMed] [Google Scholar]
- 297.Abbas M, et al. Hypereosinophilia in patients with multiple sclerosis treated with natalizumab. Neurology. 2011;77:1561–1564. doi: 10.1212/WNL.0b013e318233b391. [DOI] [PubMed] [Google Scholar]
- 298.Neighbour H, et al. Safety and efficacy of an oral CCR 3 antagonist in patients with asthma and eosinophilic bronchitis: a randomized, placebo‐controlled clinical trial. Clin. Exp. Allergy. 2014;44:508–516. doi: 10.1111/cea.12244. [DOI] [PubMed] [Google Scholar]
- 299.Wechsler ME, et al. Novel targeted therapies for eosinophilic disorders. J. Allergy Clin. Immunol. 2012;130:563–571. doi: 10.1016/j.jaci.2012.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Legrand F, et al. The eosinophil surface receptor epidermal growth factor–like module containing mucin-like hormone receptor 1 (EMR1): a novel therapeutic target for eosinophilic disorders. J. Allergy Clin. Immunol. 2014;133:1439–1447. doi: 10.1016/j.jaci.2013.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Pettipher R, et al. Heightened response of eosinophilic asthmatic patients to the CRTH 2 antagonist OC 000459. Allergy. 2014;69:1223–1232. doi: 10.1111/all.12451. [DOI] [PubMed] [Google Scholar]
- 302.Krug N, et al. Allergen-induced asthmatic responses modified by a GATA3-specific DNAzyme. New Engl. J. Med. 2015;372:1987–1995. doi: 10.1056/NEJMoa1411776. [DOI] [PubMed] [Google Scholar]
- 303.Ding C, Li J, Zhang X. Bertilimumab (Cambridge Antibody Technology Group) Curr. Opin. Investig. Drugs. 2004;5:1213–1218. [PubMed] [Google Scholar]
- 304.Ricketts HC, Cowan DC. Asthma, obesity and targeted interventions: an update. Curr. Opin. Allergy Clin. Immunol. 2019;19:68–74. doi: 10.1097/ACI.0000000000000494. [DOI] [PubMed] [Google Scholar]
- 305.Detoraki A, et al. Omalizumab in patients with eosinophilic granulomatosis with polyangiitis: a 36-month follow-up study. J. Asthma. 2016;53:201–206. doi: 10.3109/02770903.2015.1081700. [DOI] [PubMed] [Google Scholar]
- 306.Pelaia G, et al. Targeted therapy in severe asthma today: focus on immunoglobulin E. Drug Des. Dev. Ther. 2017;11:1979. doi: 10.2147/DDDT.S130743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Borish LC, et al. Interleukin-4 receptor in moderate atopic asthma: a phase I/II randomized, placebo-controlled trial. Am. J. Respir. Crit. Care Med. 1999;160:1816–1823. doi: 10.1164/ajrccm.160.6.9808146. [DOI] [PubMed] [Google Scholar]
- 308.Hart T, et al. Preclinical efficacy and safety of pascolizumab (SB 240683): a humanized anti‐interleukin‐4 antibody with therapeutic potential in asthma. Clin. Exp. Immunol. 2002;130:93–100. doi: 10.1046/j.1365-2249.2002.01973.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Blanchard C, et al. Inhibition of human interleukin‐13‐induced respiratory and oesophageal inflammation by anti‐human‐interleukin‐13 antibody (CAT‐354) Clin. Exp. Allergy. 2005;35:1096–1103. doi: 10.1111/j.1365-2222.2005.02299.x. [DOI] [PubMed] [Google Scholar]
- 310.Maselli DJ, Keyt H, Rogers L. Profile of lebrikizumab and its potential in the treatment of asthma. J. Asthma Allergy. 2015;8:87. doi: 10.2147/JAA.S69932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Busse WW, et al. Randomized, double-blind, placebo-controlled study of brodalumab, a human anti–IL-17 receptor monoclonal antibody, in moderate to severe asthma. Am. J. Respir. Crit. Care Med. 2013;188:1294–1302. doi: 10.1164/rccm.201212-2318OC. [DOI] [PubMed] [Google Scholar]
- 312.Gauvreau GM, et al. Effects of an anti-TSLP antibody on allergen-induced asthmatic responses. New Engl. J. Med. 2014;370:2102–2110. doi: 10.1056/NEJMoa1402895. [DOI] [PubMed] [Google Scholar]
- 313.Agache IO. Endotype driven treatment of asthma. Curr. Treat. Options Allergy. 2014;1:198–212. doi: 10.1007/s40521-014-0014-0. [DOI] [Google Scholar]
- 314.Canonica GW, et al. Therapeutic interventions in severe asthma. AWorld Allergy Organ. J. 2016;9:40. doi: 10.1186/s40413-016-0130-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Johnnidis JB, et al. Regulation of progenitor cell proliferation and granulocyte function by microRNA-223. Nature. 2008;451:1125. doi: 10.1038/nature06607. [DOI] [PubMed] [Google Scholar]
- 316.Liu X, et al. MicroRNA-146a modulates human bronchial epithelial cell survival in response to the cytokine-induced apoptosis. Biochem. Biophys.Res. Commun. 2009;380:177–182. doi: 10.1016/j.bbrc.2009.01.066. [DOI] [PubMed] [Google Scholar]
- 317.Taganov KD, Boldin MP, Chang K-J, Baltimore D. NF-κB-dependent induction of microRNA miR-146, an inhibitor targeted to signaling proteins of innate immune responses. Proc. Natl Acad. Sci. 2006;103:12481–12486. doi: 10.1073/pnas.0605298103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Liu G, et al. miR-147, a microRNA that is induced upon Toll-like receptor stimulation, regulates murine macrophage inflammatory responses. Proc. Natl Acad. Sci. 2009;106:15819–15824. doi: 10.1073/pnas.0901216106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Collison A, Mattes J, Plank M, Foster PS. Inhibition of house dust mite–induced allergic airways disease by antagonism of microRNA-145 is comparable to glucocorticoid treatment. J. Allergy Clin. Immunol. 2011;128:160–167. doi: 10.1016/j.jaci.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 320.Tang B, et al. Identification of MyD88 as a novel target of miR‐155, involved in negative regulation of Helicobacter pylori‐induced inflammation. FEBS Lett. 2010;584:1481–1486. doi: 10.1016/j.febslet.2010.02.063. [DOI] [PubMed] [Google Scholar]
- 321.Zhang Y, Zhong M, Zhang M, Lv K. Expression and clinical significance of miR-155 in peripheral blood CD4 (+); T cells of patients with allergic asthma. Xi bao yu fen. zi mian yi xue za zhi Chin. J. Cell. Mol. Immunol. 2012;28:540–543. [PubMed] [Google Scholar]
- 322.O'Connell RM, et al. MicroRNA-155 is induced during the macrophage inflammatory response. Proc. Natl Acad. Sci. 2007;104:1604–1609. doi: 10.1073/pnas.0610731104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Zech A, Ayata K. MicroRNA-155 modulates P2R-signaling and Th2-priming of dendritic cells during allergic airway inflammation in mice. Pneumologie. 2016;70:V163. doi: 10.1055/s-0042-118373. [DOI] [PubMed] [Google Scholar]
- 324.Lu TX, Munitz A, Rothenberg ME. MicroRNA-21 is up-regulated in allergic airway inflammation and regulates IL-12p35 expression. J. Immunol. 2009;182:4994–5002. doi: 10.4049/jimmunol.0803560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Sheedy FJ, et al. Negative regulation of TLR4 via targeting of the proinflammatory tumor suppressor PDCD4 by the microRNA miR-21. Nat. Immunol. 2010;11:141. doi: 10.1038/ni.1828. [DOI] [PubMed] [Google Scholar]
- 326.Sawant V. D. et al. Serum microRNA-21 as a biomarker for allergic inflammatory disease in children. MicroRNA. 2015;4:36–40. doi: 10.2174/2211536604666150220232507. [DOI] [PubMed] [Google Scholar]
- 327.Veremeyko T, et al. IL-4/IL-13-dependent and independent expression of miR-124 and its contribution to M2 phenotype of monocytic cells in normal conditions and during allergic inflammation. PloS ONE. 2013;8:e81774. doi: 10.1371/journal.pone.0081774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Tan Z, et al. Allele-specific targeting of microRNAs to HLA-G and risk of asthma. Am. J. Hum. Genet. 2007;81:829–834. doi: 10.1086/521200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Nicodemus-Johnson J, et al. Maternal asthma and microRNA regulation of soluble HLA-G in the airway. J. Allergy Clin. Immunol. 2013;131:1496–1503. doi: 10.1016/j.jaci.2013.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Mattes J, et al. Antagonism of microRNA-126 suppresses the effector function of TH2 cells and the development of allergic airways disease. Proc. Natl Acad. Sci. 2009;106:18704–18709. doi: 10.1073/pnas.0905063106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Kumar M, Mabalirajan U, Agrawal A, Ghosh B. Proinflammatory role of let-7 miRNAs in experimental asthma? J. Biol. Chem. 2010;285:le19–le19. doi: 10.1074/jbc.L110.145698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Polikepahad S, et al. Proinflammatory role for let-7 microRNAS in experimental asthma. J. Biol. Chem. 2010;285:30139–30149. doi: 10.1074/jbc.M110.145698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Kumar M, et al. Let-7 microRNA–mediated regulation of IL-13 and allergic airway inflammation. J. Allergy Clin. Immunol. 2011;128:1077–1085. doi: 10.1016/j.jaci.2011.04.034. [DOI] [PubMed] [Google Scholar]
- 334.Mayoral RJ, et al. MiR-221 influences effector functions and actin cytoskeleton in mast cells. PloS ONE. 2011;6:e26133. doi: 10.1371/journal.pone.0026133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Mayoral RJ, et al. MicroRNA-221–222 regulate the cell cycle in mast cells. J. Immunol. 2009;182:433–445. doi: 10.4049/jimmunol.182.1.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Li JJ, et al. MicroRNA-9 regulates steroid-resistant airway hyperresponsiveness by reducing protein phosphatase 2A activity. J. Allergy Clin. Immunol. 2015;136:462–473. doi: 10.1016/j.jaci.2014.11.044. [DOI] [PubMed] [Google Scholar]
- 337.Di Valentin E, et al. New asthma biomarkers: lessons from murine models of acute and chronic asthma. Am. J. Physiol. Lung Cell Mol. Physiol. 2009;296:L185–L197. doi: 10.1152/ajplung.90367.2008. [DOI] [PubMed] [Google Scholar]
- 338.Haj‐Salem I, et al. MicroRNA‐19a enhances proliferation of bronchial epithelial cells by targeting TGFβR2 gene in severe asthma. Allergy. 2015;70:212–219. doi: 10.1111/all.12551. [DOI] [PubMed] [Google Scholar]
- 339.Liao G, Panettieri RA, Tang DD. Micro RNA‐203 negatively regulates c‐Abl, ERK 1/2 phosphorylation, and proliferation in smooth muscle cells. Physiol. Rep. 2015;3:e12541. doi: 10.14814/phy2.12541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Chiba Y, et al. Down-regulation of miR-133a contributes to up-regulation of Rhoa in bronchial smooth muscle cells. Am. J. Respir. Crit. Care Med. 2009;180:713–719. doi: 10.1164/rccm.200903-0325OC. [DOI] [PubMed] [Google Scholar]
- 341.Yamamoto M, et al. Decreased miR-192 expression in peripheral blood of asthmatic individuals undergoing an allergen inhalation challenge. BMC Genomics. 2012;13:655. doi: 10.1186/1471-2164-13-655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.McKenzie AN, Spits H, Eberl G. Innate lymphoid cells in inflammation and immunity. Immunity. 2014;41:366–374. doi: 10.1016/j.immuni.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 343.Christianson CA, et al. Persistence of asthma requires multiple feedback circuits involving type 2 innate lymphoid cells and IL-33. J. Allergy Clin. Immunol. 2015;136:59–68. doi: 10.1016/j.jaci.2014.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Singh PB, et al. MicroRNA regulation of type 2 innate lymphoid cell homeostasis and function in allergic inflammation. J. Exp. Med. 2017;214:3627–3643. doi: 10.1084/jem.20170545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.McKenzie A, et al. MicroRNA-155 protects group 2 innate lymphoid cells from apoptosis to promote type-2 immunity. Front. Immunol. 2018;9:2232. doi: 10.3389/fimmu.2018.00796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Sharma A, et al. Antagonism of mmu-mir-106a attenuates asthma features in allergic murine model. J. Appl. Physiol. 2012;113:459–464. doi: 10.1152/japplphysiol.00001.2012. [DOI] [PubMed] [Google Scholar]
- 347.Kim RY, et al. MicroRNA-21 drives severe, steroid-insensitive experimental asthma by amplifying phosphoinositide 3-kinase–mediated suppression of histone deacetylase 2. J. Allergy Clin. Immunol. 2017;139:519–532. doi: 10.1016/j.jaci.2016.04.038. [DOI] [PubMed] [Google Scholar]
- 348.Dong J, et al. MicroRNA networks in mouse lung organogenesis. PloS ONE. 2010;5:e10854. doi: 10.1371/journal.pone.0010854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Williams AE, et al. Maternally imprinted microRNAs are differentially expressed during mouse and human lung development. Dev. Dyn. 2007;236:572–580. doi: 10.1002/dvdy.21047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Bhaskaran M, et al. MicroRNA-127 modulates fetal lung development. Physiol. Genomics. 2009;37:268–278. doi: 10.1152/physiolgenomics.90268.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Lu TX, et al. MicroRNA-21 limits in vivo immune response-mediated activation of the IL-12/IFN-γ pathway, Th1 polarization, and the severity of delayed-type hypersensitivity. J. Immunol. 2011;187:3362–3373. doi: 10.4049/jimmunol.1101235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Weidner J, Malmhäll C, Rådinger M. MicroRNAs in asthma pathogenesis-from mouse to man. J. Transl. Genet. Genom. 2019;3:2. [Google Scholar]
- 353.Davis JS, et al. Circulating microRNAs and association with methacholine PC20 in the Childhood Asthma Management Program (CAMP) cohort. PloS ONE. 2017;12:e0180329. doi: 10.1371/journal.pone.0180329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Xie Y, Merkel OM. Pulmonary delivery of siRNA via polymeric vectors as therapies of asthma. Arch. der Pharmazie. 2015;348:681–688. doi: 10.1002/ardp.201500120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Zafra, M. P. et al. Gene silencing of SOCS3 by siRNA intranasal delivery inhibits asthma phenotype in mice. PloS ONE9, e91996 (2014). [DOI] [PMC free article] [PubMed]
- 356.Kho AT, et al. Circulating microRNAs and prediction of asthma exacerbation in childhood asthma. Respiratory Res. 2018;19:128. doi: 10.1186/s12931-018-0828-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Cheng W, et al. MiR-143-3p controls TGF-β1-induced cell proliferation and extracellular matrix production in airway smooth muscle via negative regulation of the nuclear factor of activated T cells 1. Mol. Immunol. 2016;78:133–139. doi: 10.1016/j.molimm.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 358.Spurlock CF, III., et al. Expression and functions of long noncoding RNAs during human T helper cell differentiation. Nat. Commun. 2015;6:6932. doi: 10.1038/ncomms7932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359.Huo X, et al. Decreased epithelial and plasma miR‐181b‐5p expression associates with airway eosinophilic inflammation in asthma. Clin. Exp. Allergy. 2016;46:1281–1290. doi: 10.1111/cea.12754. [DOI] [PubMed] [Google Scholar]
- 360.Maes T, et al. Asthma inflammatory phenotypes show differential microRNA expression in sputum. J. Allergy Clin. Immunol. 2016;137:1433–1446. doi: 10.1016/j.jaci.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 361.Perry MM, et al. Role of non-coding RNAs in maintaining primary airway smooth muscle cells. Respir. Res. 2014;15:58. doi: 10.1186/1465-9921-15-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Heffler E, et al. MicroRNA profiling in asthma: potential biomarkers and therapeutic targets. Am. J. Respir. C ell Mol. Biol. 2017;57:642–650. doi: 10.1165/rcmb.2016-0231TR. [DOI] [PubMed] [Google Scholar]