Abstract
Near misses and unsafe conditions have become more serious for patients in emergency departments (EDs). We aimed to search the near misses and unsafe conditions that occurred in an ED to improve patient safety.
This was a retrospective analysis of a 10-year observational period from January 1, 2007 to December 31, 2016. We gained access to the adverse event notification forms (AENFs) sent to the hospital quality department from the ED. Patient age, sex, and date of presentation were recorded. The near misses and unsafe conditions were classified into 7 types: medication errors, falls, management errors, penetrative-sharp tool injuries, incidents due to institution security, incidents due to medical equipment, and forensic events. The outcome of these events was recorded.
A total of 220 AENF were reported from 294,673 ED visits. The median age of the 166 patients was 60 (21–95) years. Of these, 57.1% of the patients were females and 47.9% were males. The most commonly reported events were medication errors (32.7%) and management errors (27.3%). The median age of falling patients was 67.5 years. The nurse–patient ratio between 2007 to 2011 and 2011 to 2016 were 1/10 and 1/7, respectively. We found that when this ratio increased, the adverse events results were less significant (P < .003).
This was the 1st study investigating the adverse events in ED in Turkey. The reporting ratio of 0.07% for the total ED visits was too low. This showed that adverse events were under-reported.
Keywords: adverse events, emergency department, patient safety
1. Introduction
Near misses and unsafe conditions have become more serious for acutely hospitalized patients in emergency departments (EDs). ED is the most crowded and complex department in hospitals, especially in tertiary academic hospitals (those with a trauma center, stroke units, percutaneous intervention center, and other subspecialized units). The features of patients in EDs are very different; these patients are unique, and each patient needs different and specialized care, medical procedures, and medicines.
The quality department (QD) of the authors’ hospital initiated the activities toward Joint Commission International (JCI) accreditation in 2004. Because of these activities, the hospital was granted accreditation by JCI in 2007, and this was the 1st public and university hospital accreditation by JCI in Turkey. Then, in 2011, 2014, and 2018, our hospital was reaccredited by JCI. Hacettepe University Hospitals still keep its title as the only public university hospital accredited by JCI.[1] Because of the accreditation standards, patient safety and quality care have become more important for the hospital. For the present study, the data were obtained through the recordings of the QD. We aimed to search the near misses and unsafe conditions occurred in the ED to improve patient safety.
2. Methods
This was a retrospective analysis of a 10-year observational study from January 1, 2007 to December 31, 2016. It was approved by the Hacettepe University Ethical Committee.
The hospital QD used an “adverse event notification form” (AENF) and alerted the health care workers in the hospital to use these forms in case of adverse event occurrence. AENF is available on hospital software.
We obtained AENFs that were sent to QD from our ED. We classified the near misses and unsafe conditions into 7 groups: medication errors (wrong drug, false dosage, wrong time, false duration, inappropriate infusion rate, false route, incorrect patient, expired drug, allergic drug), falls (fall from stretcher, fall from chair, fall in the toilet, syncope, found on the floor), management errors (no identification band, administration of the procedure to incorrect patient, inappropriate procedure, wrong sample, missed sample, blood and blood products transfusion reactions, noncompliance with sterility rules, noncompliance with the transfer procedure, extravasation of the drug from the vessel, delay in prognosis and treatment), penetrative-sharp tool injuries, incidents due to institution security, incidents due to medical equipment (unessential equipment, inappropriate equipment), and forensic events. The outcomes of these events (prevented before reaching the patient; reached the patient but the patient was not affected; and reached the patient, and the patient was affected) were recorded.
The age, sex, and the presentation year of the patients were recorded.
2.1. Statistical analyses
Statistical analyses were performed with the IBM SPSS for Windows Version 22.0. Numerical variables were summarized as mean ± standard deviation. Categorical variables were given as frequencies and percentages. Categorical variables were compared by the Chi-squared test. Normality of the continuous variables was evaluated by the Kolmogorov–Smirnov test. Differences between the groups according to continuous variables were determined by independent samples t test. A P-value of <.05 was considered significant.
3. Results
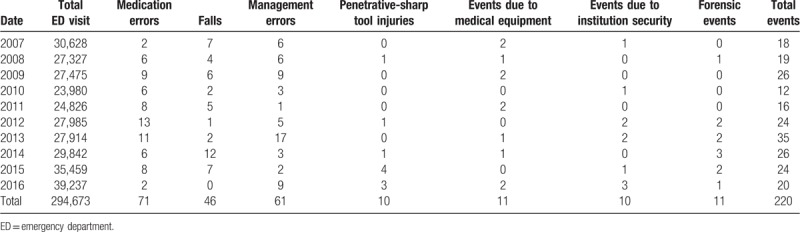
Of the total 294,673 ED visits, 220 AENF were reported from the ED during this 10-year period. The median age of the 166 patients was 60 (21–95). The ratio of the female was 57.1%, and that of the male was 47.9%. The most commonly reported events were medication errors (32.7%) and management errors (27.3%) (Fig. 1). For each year, the detailed adverse events numbers and ratios are shown in Table 1.
Figure 1.
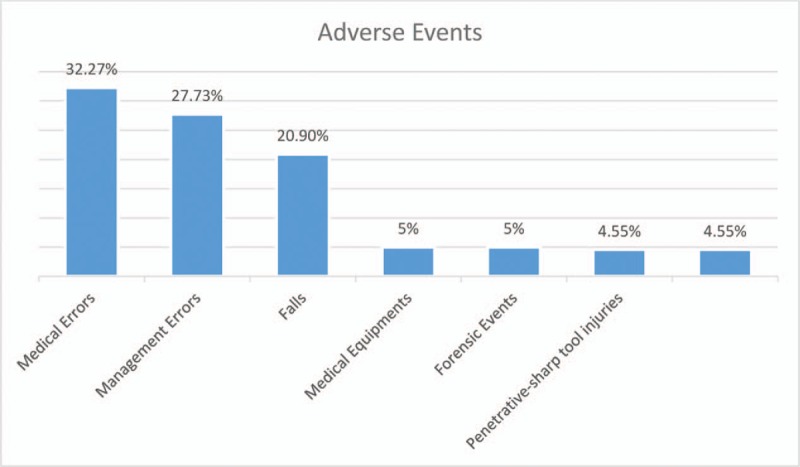
The distribution of the adverse event ratios.
Table 1.
The distribution of the adverse events classification according to the year.
While the median age of falling patients was 67.5 years, the median age of the patients who did not fall was 57 years. There was a statistically significant difference between these 2 groups (P < .001).
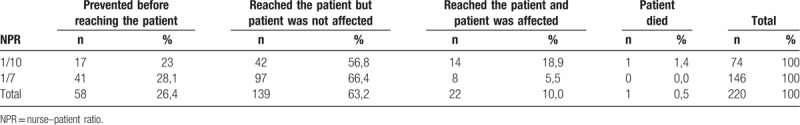
During the years 2007 to 2011, 3 nurses were working per 12 hours, while between 2011 and 2016, 5 nurses were working per 12 hours in the ED. The nurse–patient ratio (NPR) between 2007 to 2011 and 2011 to 2016 was 1/10 and 1/7, respectively. There was a statistical significance on a comparison of these periods with the adverse events results (P < .003) (Table 2).
Table 2.
The distributions of the results of the events according to the NPR.
4. Discussion
During patient management, patient safety has become more crucial in terms of medical care quality. CHARMED (cross-checking to reduce adverse events resulting from medical errors in the ED) study was the 1st study that aimed to reduce the adverse events in the ED.[2] The present study was the 1st to investigate the adverse events in ED in Turkey.
The total reporting number of 220 adverse events was too low for this 10-year period, and the ratio was 0.07% for the total ED visits. This showed that the adverse events from ED were under-reported. Aaronson et al found 750 adverse events reports for a year, and the ratio was 0.69% per annual ED visits. Ruddy et al reported 487 events for a year from 18 pediatric ED.[3,4] Schultz et al reported the notification ratio of 0.08% by using an online incident reporting system.[5] The cross-sectional observation study by Maroto et al reported the medication errors collected by 4 professional observer nurses from an ED in September 2016. The reporting number from these observers was 150 for a month, vs the 14 total notification in the hospital system, from 2013 to 2016.[6] All studies reported that the adverse events ratio was below the estimated value.
Aaronson et al reported medication safety as the 1st incident report during 1 year in their ED.[3] Ruddy et al also reported the medication-related events in their study designed in 18 pediatric ED.[4] Calder et al, however, determined that management issues were the most common type of adverse events.[7] Medication errors were also the 1st incident reports from our ED.
We found the median age of falling patients, that is, 67 years, was higher than the patients who did not fall. McErlean and Hughes reported that patient under 65 years old fell in ED, while younger patients fell in other hospital wards.[8] They attributed this finding to alcohol intake; young patients who took alcohol fell much more than other patients. The authors’ hospital is the most preferred university hospital in Turkey. Patients from all around the country come to the hospital for treatment. Malign and geriatric patients who need multidisciplinary approach are mostly admitted to the hospital and to the ED. Hence, the patients in the hospital are mostly geriatric and also bedridden, with high risk for falls.
There are no adequate studies on NPR and patient safety in the ED. We found that when the NPR increased, there were less adverse events. California Department of Public Health recommended the maximum NPR of 1:1 for trauma resuscitation patients, 1:2 for critical patients, and 1:4 for all other ED patients in 2009.[9] Chan et al found that ED waiting time and ED care time were shorter upon increasing the nurse staff in ED.[10] In the present study, the NPR was 1:10 and 1:7. The hospital still continues to work with the same NPR (1:7). Although more ED nurses are required, because of the insufficient economic sources, nurse staffing cannot be increased.
Friedman et al recommended that engaging patients and their families in the identification of errors might improve patient safety in ED.[11] Glickman et al also supported the patient-reported approach.[12] Schultz et al designed an online incident reporting system for Australian EM, Emergency Medicine Events Register (EMER). They concluded that although the EMER system was easy, the usage of the system by the doctors must be encouraged because nurses used the system more than doctors.[5] Zhu recommended that hospital leaders should prioritize actions for patient safety in EDs and in operating rooms in intensive care units in Chinese hospitals.[13] They supported that reporting of the errors might lead to improvement in patient safety. Maroto et al recommended that declaring medication administration errors might lead to effective prevention actions against these errors.[6] All these studies stated above used different methods for reporting, but there was no priority for any particular method, and reporting was highlighted as the most important aspect in all the studies.
This study was set up in one academic tertiary medical center. This was the limitation of this study.
In conclusion, the reporting ratio of 0.07% for the total ED visits was too low. This could be considered an under-reporting of the adverse events. Through this study, we gained the practice of reporting of the unexpected events occurring in the ED. We have learnt lessons from these feedbacks, and we will improve patient care quality in the ED and patient safety accordingly. Future studies about the medical errors in the ED will be designed to investigate the root cause and to improve the approachment of the adverse events. The adverse events reporting systems have to be evolved to more simple and usable to encourage the health care worker to report the adverse events
Acknowledgment
The authors thank Dr Sevilay Karahan for the contribution of the statistical analyses. Dr Sevilay Karahan gave permission to be named in this manuscript.
Author contributions
Conceptualization: Nalan Metin Metin Aksu.
Data curation: Nalan Metin Metin Aksu, Meltem Akkaş.
Investigation: Nalan Metin Metin Aksu, Meltem Akkaş.
Methodology: Nalan Metin Metin Aksu.
Supervision: Nalan Metin Metin Aksu, Meltem Akkaş.
Validation: Meltem Akkaş.
Writing – review & editing: Nalan Metin Metin Aksu, Meltem Akkaş.
Footnotes
Abbreviations: AENF = adverse event notification form, CHARMED = cross-checking to reduce adverse events resulting from medical errors in emergency department, ED = emergency department, EMER = Emergency Medicine Events Register, JCI = Joint Commission International, NPR = nurse–patient ratio, QD = quality department.
How to cite this article: Aksu NM, Akkaş M. Where are we in patient safety in the ED in Turkey? Medicine. 2019;98:41(e17569).
The authors have no funding and conflicts of interest to disclose.
References
- [1].Available at: www.international.hastane.hacettepe.edu.tr Accessed January 2, 2019. [Google Scholar]
- [2].Freund Y, Goulet H, Leblanc J, et al. Effect of systematic physician cross-checking on reducing adverse events in the emergency department: the CHARMED cluster randomized trial. JAMA Intern Med 2018;178:812–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Aaronson EA, Brown D, Benzer T, et al. Incident reporting in emergency medicine: a thematic analysis of events. J Patient Saf 2017;doi: 10.1097/PTS.0000000000000399. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [4].Ruddy RM, Chamberlain JM, Mahajan PV, et al. Pediatric emergency care applied research network. Near misses and unsafe conditions reported in a pediatric emergency research network. BMJ Open 2015;5:e007541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Schultz TJ, Crock C, Hansen K, et al. Piloting an online incident reporting system in Australasian emergency medicine. Emerg Med Australas 2014;26:461–7. [DOI] [PubMed] [Google Scholar]
- [6].Maroto MM, Carpintero S. Medication administration errors at an emergency service: knowing to decrease risk. Rev Esp Salud Publica 2018;92:e201806038. [PMC free article] [PubMed] [Google Scholar]
- [7].Calder LA, Forster A, Nelson M, et al. Adverse events among patients registered in high-acuity areas of the emergency department: a prospective cohort study. CJEM 2010;12:421–30. [DOI] [PubMed] [Google Scholar]
- [8].McErlean DR, Hughes JA. Who Falls in an adult emergency department and why-a retrospective review. Australas Emerg Nurs J 2017;20:12–6. [DOI] [PubMed] [Google Scholar]
- [9].California Department of Public Health. Nurse-to-patient sataffing Ratio REGULATIONS. Available at: https://www.cga.ct.gov/2004/rpt/2004-R-0212.htm Accessed August 31, 2018. [Google Scholar]
- [10].Chan TC, Killeen JP, Vilke GM, et al. Effect of mandated nurse-patient ratios on patient wait time and care time in the emergency department. Acad Emerg Med 2010;17:545–52. [DOI] [PubMed] [Google Scholar]
- [11].Friedman SM, Provan D, Moore S, et al. Errors, near misses and adverse events in the emergency department: what can patients? CJEM 2008;10:421–7. [DOI] [PubMed] [Google Scholar]
- [12].Glickman SW, Mehrotra A, Shea CM, et al. A patient reported approach to identify medical errors and improve patient safety in the emergency department. J Patient Saf 2016;Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [13].Zhu J, Li L, Zhou Z, et al. Variations in patient safety climate in Chinese hospitals. J Patient Saf 2016;Epub ahead of print. [DOI] [PubMed] [Google Scholar]


