Abstract
Background
Fistulas may arise as a relevant complication of Crohn’s disease (CD). Despite their clinical significance and the substantial burden imposed on patients, limited data are available on the epidemiology of fistulizing CD in the United States.
Methods
A systematic literature review was conducted to identify data published between 1970 and 2017 on the epidemiology of fistulas in patients with CD, with the aim to estimate the number of prevalent cases in the United States. Retrieved titles and abstracts were screened by 2 independent researchers for inclusion criteria (US population-based studies reporting data on the epidemiology of fistulizing CD). To validate the literature-based estimate, data from a US claims database (Truven Health MarketScan database) were analyzed. This database has broad geographic coverage, with health care data for >60 million patients during the period of the analysis.
Results
The literature search retrieved 7 articles for full-text review, and only 1 met the criteria for inclusion. This study described the cumulative incidence of fistulas in a CD population from Minnesota over 20 years. From the reported data, the estimated number of prevalent cases with fistulizing CD in the United States was ~76,600 in 2017 (~52,900 anal, ~7400 rectovaginal, ~2300 enterocutaneous, and ~14,100 internal). Analysis from the US health care database resulted in an estimated number of ~75,700 patients, confirming the robustness of the original estimate from the literature.
Conclusions
Based on 2 separate analyses, the estimated number of patients with fistulizing CD in the United States is ~77,000 patients.
Keywords: fistula, Crohn’s disease/CD, prevalence, epidemiology
This article describes a literature review and population-based database search that estimate the number of patients with fistulizing Crohn’s Disease (CD) in the United States to be ~77,000. The data indicates that fistulizing CD is an orphan condition.
INTRODUCTION
Fistula is a common and severe complication of Crohn’s disease (CD) that affects up to 50% of patients within 20 years of initial diagnosis.1, 2 It is associated with substantial morbidity and significant impairment in health-related quality of life.3 Treatment options are limited and often provide only transient benefit, with more than one-third of patients experiencing recurrent fistulas despite medical therapy.4, 5
The pathogenesis of fistula formation in patients with CD is not completely understood; however, histologic evidence suggests that fistulas arise as a consequence of an epithelial barrier defect caused by an ongoing inflammatory process.1, 4 Epithelial‒mesenchymal transition of intestinal epithelial cells results in transformation of the cells to an invasive phenotype, leading to penetration of adjacent tissue layers and the eventual establishment of a connection to other organs or the skin surface.1, 4
Fistulas in patients with CD are typically classified according to anatomic location as anal, rectovaginal, enterocutaneous, or internal.6 Anal fistulas may be further classified as either simple or complex based on the location in relation to the external anal sphincter, number of tracts, and presence or absence of associated complications, such as strictures and abscesses.7 Compared with simple fistulas, complex fistulas are associated with a worse prognosis and are more likely to require radical surgical procedures, such as stoma and proctectomy.6, 8 Studies in patients with CD suggest that 71%–84% of anal fistulas are complex.6, 8–10
Despite the burden imposed on patients, limited data are available on the epidemiology of fistulizing CD in the United States. The aim of the present study was, therefore, to estimate the US prevalence of fistulizing CD and describe the prevalence of CD-related fistulas according to type. A systematic literature review was performed to identify population-based epidemiologic data sufficient to estimate the number of prevalent cases in the United States. In addition, prevalent cases from a large US claims database were extrapolated to the US population and used as a validation approach to assess the robustness of the estimate derived from the published literature.
METHODS
Systematic Literature Review
A search of the PubMed database was performed for published articles about the epidemiology of fistulas in patients with CD in the United States between January 1, 1970, and February 15, 2017, with the aim to estimate the number of prevalent cases existing in the United States (see the Supplementary Data for the full search algorithm). The results were screened by 2 of the authors to identify potentially relevant articles for full-text review based on predefined selection criteria (population-based studies conducted in US patients with CD reporting data on the epidemiology of fistulas). Bibliographies of the selected articles were also screened to identify any additional potential sources of relevant data. Any discrepancies between authors regarding the eligibility of an article for full-text review were resolved through discussion and agreement. Articles selected for full-text review were obtained and reviewed for relevance using the same criteria noted previously.
Data Analysis
Relevant data from the literature search were used to calculate the number of prevalent cases of fistulas according to type (anal, rectovaginal, enterocutaneous, or internal) in US patients with CD. The calculation methods used were not predefined a priori, as they needed to be decided based on the type of data identified from the literature search. As the relevant data obtained from this search were about the cumulative incidence of fistulas over time in the CD population (see the Results), we derived from this the incident cases of fistulas in the incident CD population and in the rest of the CD population. Then, using the US incidence and prevalence of CD derived from published literature, and projected to 2017, the overall incidence of fistulizing CD was estimated. Incident cases according to the type of fistula were calculated from the estimated total incidence for fistulizing CD and from the distribution of fistulas reported by Schwartz et al.2 (Table 1).
TABLE 1.
Summary of Results Derived From the Population-Based Epidemiologic Study2
| CD diagnosis, No. | 169a |
| Fistula diagnosis, No. | |
| Patients | 59 |
| Episodes | 88 |
| Fistula episodes/patient, No. (%) | |
| 1 | 39 (66) |
| 2 | 13 (22) |
| ≥3 | 7 (12) |
| Cumulative incidence of fistulizing CD, % | |
| Year 1 after diagnosis | 21.0 |
| Year 5 after diagnosis | 26.0 |
| Year 10 after diagnosis | 33.0 |
| Year 20 after diagnosis | 50.0 |
| Type of fistula, No. (%) | |
| Anal | 48 (55) |
| Rectovaginal | 8 (9) |
| Enterocutaneous | 5 (6) |
| Internalb | 27 (31) |
aExcludes 6 residents with diagnosis of CD who declined consent.
bIncludes enteroenteric (n = 21), enterovesical (n = 3), and entero-intraabdominal (n = 3).
Prevalent cases of fistula were derived from the incident cases and the duration of fistula episodes according to the following formula: point prevalence = incidence * duration of condition.
Because the duration of fistula episodes varies according to the type of fistula, prevalent cases were calculated separately for each type. For each type of fistula, duration was based on the distribution of patients across a number of episodes, the median duration of the episodes of that type of fistula, and the median time between episodes, as previously reported.2, 6 Further details are provided in the Supplementary Data.
After the estimations were done, new evidence from a population-based epidemiologic study evaluating the incidence and prevalence of CD was published.11 To assess the stability of the original estimate, a post hoc sensitivity analysis based on the new published data was performed. This study evaluated the incidence and prevalence of CD in Olmsted County, Minnesota, from 1970 to 2010, and reported an age- and sex-adjusted incidence of 10.7/100,000 person-years in the period 2009‒2010 and a prevalence of 246.7/100,000 persons in 2011. The 2017 local incidence and prevalence of CD were derived from the reported local incidence and prevalence using a logistic regression model; the resulting estimates were extrapolated to the US population based on the 2017 population estimate published by the US Census Bureau.12 The estimated prevalent cases of fistulizing CD were then recalculated using the revised incidence and prevalence estimates for CD.
Population-Based Database Analysis
To validate the prevalence estimate derived from the published literature, the prevalence of fistulizing CD among individuals in a population-based US claims database was extrapolated to the US population and compared with the literature-based estimate. The analysis was performed using the Truven Health MarketScan Database (Truven Health Analytics, Ann Arbor, MI, USA), which included patient-level claims for 62.7 million individuals with active records during the period of analysis. This database is aligned to the US census, so it represents a faithful representation of the US population with employer-provided health insurance. At the time of the analysis, the database included claims data through December 31, 2014.
Prevalent cases of CD were identified by screening for at least 1 claim with an International Statistical Classification of Diseases and Related Health Problems (ICD)–9 code related to CD (555.0, 555.1, 555.2, and 555.9) using 5 years of history to ensure that patients with quiescent disease were not excluded. Patients with fistulizing disease were then identified using the ICD-9 code (see the Supplementary Data for a full list of codes). To maximize the probability of identifying cases of fistulizing CD, relevant surgical codes were also used. From identified incident cases of each type of fistula, the respective prevalent cases were calculated considering their duration according to published data.6
Cases identified in 2014 were screened against those from prior years to identify duplicates. Given that no ICD-9 or surgical codes are available for enterocutaneous fistulas, the prevalence was estimated by multiplying the number of records with the ICD-9 code for “intestinal fistulas excluding the rectum/anus” by 19%, based on the proportion of intestinal nonanal fistulas that were classified as enterocutaneous in a prior study.2 The prevalence of internal fistulas was adjusted accordingly to reflect the assignment of cases to enterocutaneous fistulas. The estimated prevalence of each type of fistula was extrapolated to the 2017 US population using the population projection published by the US Census Bureau.12
RESULTS
Systematic Literature Review
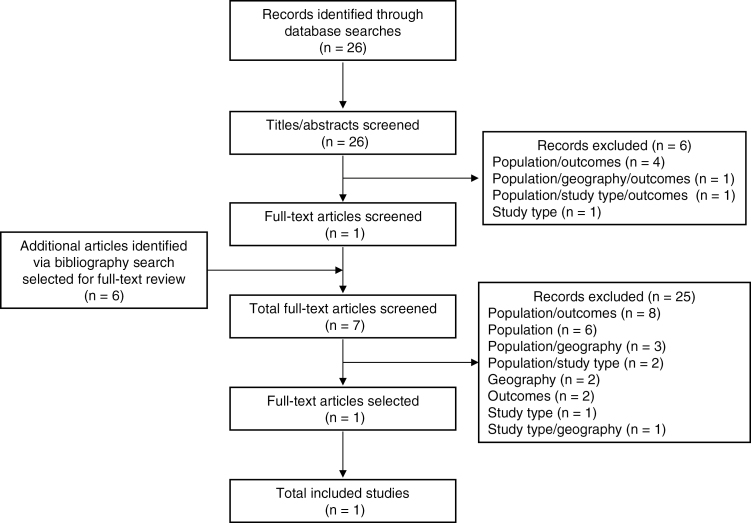
The literature search retrieved a total of 26 records, 1 of which was judged to be potentially eligible for inclusion and selected for full-text review. A manual review of the references identified an additional 6 articles (Fig. 1), resulting in a total of 7 articles undergoing formal full-text review. Finally, only 1 study met the criteria for inclusion (see the Supplementary Data for a list of excluded studies and the corresponding reasons for exclusion).
FIGURE 1.
Literature review flow diagram (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).
In the study selected for inclusion, Schwartz et al.2 analyzed the medical records of all Olmsted County residents who were diagnosed with CD from 1970 to 1993 and who developed a fistula before December 31, 1995. The findings of the study are summarized in Table 1. The reported incidence of fistulas was 21% at 1 year after CD diagnosis. However, the cumulative incidence at 20 years after diagnosis was 50%, and thus it can be concluded that the cumulative incidence of fistulas between years 2 and 20 after diagnosis was 29% (ie, 50% minus 21%). As analysis of the cumulative incidence of fistulas during years 2 to 20 following the diagnosis of CD was linear,2 it was concluded that the incidence of fistulas was 1.5% every year over this period (29%/19 years). Thus, at a given calendar year, the overall incidence of fistulizing CD is 21% of the incident CD population plus 1.5% of the rest of the CD population (ie, prevalent minus incident CD patients). This approach was followed to estimate the overall incidence of fistulizing CD, and, for that, the US incidence and prevalence of CD were derived from the published literature. In summary, the number of incident cases of CD was estimated using a weighted average incidence of 8.2/100,000 person-years. This was based on the age-stratified incidence of CD reported in a large and geographically diverse US population,13 under the assumption that the US incidence of CD has stabilized since the 1970s, as previously described.14, 15 Prevalent cases of CD in 2017 were estimated projecting the most recent countrywide prevalence rates available (2004‒2009),16 assuming that the increasing trend has continued through to the present (see the Supplementary Data for the projected US prevalence). For estimating both incident and prevalent cases of fistulizing CD, rates were projected to 2017 using population estimates from the US Census Bureau (326.6 million).12 The calculation resulted in a total of 15,732 (95% confidence interval [CI], 2302–29,162) incident cases with fistulizing CD (Table 2). Incident cases according to the type of fistula are summarized in Table 3. Prevalent cases for each type of fistula derived from the incident cases and the duration of each type of fistula are also shown in Table 3. The addition of the prevalent cases for each type of fistula yielded a total of 76,616 (95% CI, 11,209–142,026) prevalent cases for fistulizing CD.
TABLE 2.
Estimated Incident Cases of Fistulizing CD in the US
| 2009 | 2017 | |||
|---|---|---|---|---|
| Patients, No. | Incidence of Fistulizing CD, % | Incident Cases of Fistulizing CD, No. (95% CI) | Incident Cases of Fistulizing CD, No. (95% CI) | |
| Incident CD cases | 25,266a | 21.0 | 5306 (3669–7064) | |
| Prevalent minus incident Crohn’s cases | 539,734b | 1.5 | 8238 (0–18,764) | |
| Total Crohn’s cases | 13,544 (1981–25,107) | 15,732c (2302–29,162) |
Rounded values displayed; calculations performed without restricting number of decimal places.
aCalculated based on weighted average incidence of 8.2/100, 000.13
cBased on estimated CD population in 2017. This estimation was based on projection of reported US prevalence of CD from 2004‒200916 to 2017 (656,264 patients), along with 2017 population statistics, from the US Census Bureau.12 Projection of reported US prevalence of CD to 2017 is shown in the Supplementary Data.
TABLE 3.
Estimated Incident Cases, Duration, and Prevalent Cases of Fistulizing CD in the United States
| Type | 2017 Incident Cases | Duration, ya | 2017 Prevalent Casesb |
|---|---|---|---|
| No. (95% CI) | No. (95% CI) | ||
| Anal | 8581 (1255–15,907) | 6.2 | 52,862 (7734–97,993) |
| Rectovaginal | 1430 (209–2651) | 5.1 | 7356 (1076–13,636) |
| Enterocutaneous | 894 (131–1657) | 2.5 | 2251 (329–4172) |
| Internal | 4827 (706–8948) | 2.9 | 14,147 (2070–26,225) |
| Total | 15,732 (2302–29,162) | – | 76,616 (11,209–142,026) |
Rounded values displayed; calculations performed without restricting number of decimal places.
aCalculated based on reported median duration of fistula episodes,6 categorical distribution of patients experiencing each quantity of episodes,2 and median time between episodes.2 Further details are provided in the Supplementary Data.
bCalculated as: incident cases * duration.
Population-Based Database Analysis
The results of the population-based database analysis are presented in Table 4. Extrapolation of claims data for fistulizing CD to the 2017 US population resulted in an estimation of 75,666 (95% CI, 73,950–77,382) prevalent cases. Consistent with the literature-based analysis, anal fistulas were the most common type of fistula, followed by internal, rectovaginal, and enterocutaneous. The close agreement between the estimates derived from the population-based database analysis and systematic literature review confirms the robustness of the literature-based estimate.
TABLE 4.
Estimated Prevalent Cases of Fistulizing CD Based on the US Claims Database Analysis
| Type | 2014 Prevalent Casesa,b | 2017 Prevalent Casesb |
|---|---|---|
| No. (95% CI) | No. (95% CI) | |
| Anal | 56,004 (54,398–57,610) | 57,359 (55,714–59,004) |
| Rectovaginal | 6064 (5656–6472) | 6211 (5793–6629) |
| Enterocutaneous | 3188 (2960–3416) | 3265 (3031–3499) |
| Internalc | 16,918 (16,303–17,533) | 17,327 (16,697–17,957) |
| Totald | 73,878 (72,203–75,553) | 75,666 (73,950–77,382) |
Rounded values displayed; calculations performed without restricting number of decimal places.
aBased on number of prevalent cases among active records as of December 31, 2014. bExtrapolated to US population based on projected population for corresponding year published by the US Census Bureau.12
cNo specific ICD-9 or surgical codes are available for enterocutaneous fistulas. Cases were estimated as an extrapolation from prior literature (please see Population-Based Database Analysis in the Methods section).
dSum of prevalent cases for different fistula types exceeds total prevalent cases due to patients with >1 type of fistula.
Post Hoc Analysis
As mentioned above, this post hoc analysis was performed to assess the effect of newly published estimates of the incidence and prevalence of CD on the estimated prevalence of fistulizing CD. Projection of the reported incidence and prevalence of CD in Olmsted County11, 14, 15, 17 to 2017 by means of logistic regression (see the Supplementary Data for the projected incidence and prevalence) and extrapolation to the 2017 US population yielded 34,965 and 969,364 incident and prevalent cases of CD, respectively. Recalculation of the number of patients with fistulizing CD using these figures resulted in a total of 105,217 prevalent cases.
DISCUSSION
The present study estimates, from published data, that there were ~76, 600 prevalent cases and ~15,700 incident cases of fistulizing CD in the United States in 2017 (Table 3). The distribution of prevalent cases according to the type of fistula (~52,900 anal, ~7400 rectovaginal, ~2300 enterocutaneous, and ~14,100 internal) implies that 11.7% of US citizens with CD have fistulizing CD at a given time point (8.1% anal, 1.1% rectovaginal, 0.3% enterocutaneous, and 2.2% internal).
According to our results, cross-sectionally, more than two-thirds of CD patients with fistulizing disease suffer from the anal type. It is estimated that ~75% of anal fistulas in the CD population are complex.8, 9 From our results it may be inferred that, at any point in time, ~40,000 patients in the United States could be suffering from this hard-to-treat, disabling, and relapsing type of anal fistula, which commonly requires management with aggressive medical treatments and repeated surgeries.
Rectovaginal fistula in the CD population is a complication that is exceedingly difficult to treat and markedly embarrassing for patients. Traditionally, treatment of CD-associated rectovaginal fistulas has been surgical, as medical management is fraught with failure.18–20 Unfortunately, propensity to relapse makes re-repair often necessary. According to our results, at any time, more than 7000 women in the United States could be facing this significant and distressing problem.
Although enterocutaneous fistulas may be secondary to surgery in CD patients, most commonly they occur spontaneously as a consequence of an underlying bowel inflammation.21, 22 Enterocutaneous fistulas are commonly associated with malnutrition as a consequence of fistula output, wound infection, and coexisting sepsis.21, 23 Enterocutaneous fistulas rarely respond to medical treatment,21, 22 and, as a consequence, the majority of patients need surgical intervention and resection.22, 24, 25 Unfortunately, these surgeries are associated with long hospital stays and high morbidity and mortality.23 From our results, we conclude that more than 2000 US citizens are at risk of death due to CD-related enterocutaneous fistulas.
According to our findings, approximately 14,000 US CD patients could be suffering from internal fistulas at any point in time. However, internal gut-to-gut fistulas may be difficult to diagnose, particularly if only a short segment of the bowel is bypassed, and are often found incidentally during surgery.26 As a consequence, our estimates refer to diagnosed internal fistulas, rather than to existing internal fistulas.
Our literature-based findings were supported by a population-based US database analysis that yielded ~75,700 prevalent cases (Table 4). The striking agreement between the estimates derived from 2 independent sources confirms the robustness of the estimate and supports the generalizability of the findings.
The strengths of population-based studies include the near complete case ascertainment and the ability to assess longitudinal outcomes. In the study on which the present analysis was based, Schwartz et al.2 analyzed data from the Rochester Epidemiology Project, a medical records linkage system that captures and records diagnostic information for virtually all residents of Olmsted County in a central diagnostic index. In any 4-year period, it is estimated that 95% of the residents are examined at a center affiliated with 1 of the 2 participating health care systems.27, 28 Of the 175 patients with a diagnosis of CD identified in the central diagnostic index, 169 (97%) provided consent to review their medical records.2 The high ascertainment of cases of CD, coupled with the ability to review the medical records of nearly all identified cases, facilitated a precise identification of patients with fistulizing CD.
The findings of the literature-based estimations should be interpreted with due consideration of certain limitations, including the limited availability of data from published epidemiologic studies. In particular, fistula frequencies in the CD population were derived from a study conducted in Olmsted County,2 and therefore the extent to which these data are applicable to the overall US CD population is uncertain. However, the fistula frequencies reported in that study are largely consistent with those reported outside the United States (eg, the cumulative frequency of anal fistulas at 20 years in a New Zealand CD population-based cohort was 28%9 compared with 26% in Olmsted County2), which suggests that fistula frequency in the CD population does not appear to be significantly affected by geography in populations of European descent.
It should be noted that a number of assumptions have been made to estimate prevalent cases of fistulas in the CD population that may have led to overestimation. The study used as the source to estimate fistula frequencies in US patients with CD was published in 2002.2 If recent improvements in the care of CD patients have led to a reduction in the occurrence of fistulas, our numbers would be overestimated. In fact, a very recent study, also conducted in Olmsted County, has reported a decrease in the cumulative incidence of perianal fistulizing CD after 1988.29 However, the projection of US CD prevalence to 2017 was done assuming that the trend for an increase, revealed by the most recent countrywide data (2004‒2009),16 has continued through to the present. In addition, the study considered to estimate the incidence of CD, although conducted in a geographically diverse US population, did contain a female cohort.13 Although extrapolation of a female incidence rate to the overall population appears reasonable as US data from different geographic regions show that incidence rates of CD in women are essentially the same as in the overall population,11, 30, 31 the study cohort mostly consisted of white patients, which may have led to an overestimation of the incidence of CD. Disease duration was, however, estimated by including not only the duration of episodes, but also the time between episodes. This means that the reported prevalent cases include patients with fistulizing disease who were in temporal remission between 2 active phases. Lastly, the overall prevalence of fistulizing CD was obtained from the addition of the prevalence estimates for each type of fistula. This was based on the observation that the vast majority of patients do not experience fistulas of different types at the same time. However, although rare, patients suffering from 2 types of fistulas simultaneously would have led to double counting.
A limitation of our literature-based estimation of prevalent cases is the relatively large size of the CIs, which is driven by the limited size of the CD population in the study used as the data source. Likewise, for the estimation of fistula duration, no CI could be derived, as they were not reported in the articles used as data sources. In any case, it should be noted that the literature-based estimate was highly consistent with a different estimate derived from a large health care database with a nationally representative patient population. This type of analysis is, however, subject to potential bias due to misclassification or underreporting of diagnoses and procedures. In addition, any potential difference in the frequency of fistulas in the employer-insured population vs the rest of the population might affect the results. Also of note, a potential source of overestimation is the identification of CD patients based on 1 CD ICD-9 code, as this could lead to the selection of patients without a properly confirmed diagnosis of CD. This was done to avoid missing quiescent cases and, above all, recently diagnosed cases, because, as shown by Schwartz et al.,2 fistulas associated with CD have the highest incidence at the time of diagnosis. Accordingly, it is crucial that recently diagnosed cases are not lost. As a reference, the estimated number of CD patients from the database in 2014 based on 1 CD ICD-9 code was 634,455 patients, compared with 506,239 when at least 2 CD ICD-9 codes are used. In our opinion, it is hard to know which figure is closer to reality.
All things considered, collectively, the results of the 2 analyses provide corroborative evidence to support the estimated US prevalence of fistulizing CD.
After completion of the study, new data from a population-based cohort study evaluating the epidemiology of CD in Olmsted County were published.11 The findings indicated that the prevalence of CD increased by 41% from 2001 to 2011, and by 31% from 1991 to 2001. However, the US prevalence of CD estimated from Olmsted County data of 785,000 patients for 2010 differed markedly from the published estimate of 565,000 for 2009, which was based on an analysis of claims data from a regionally diverse population of >12 million commercially insured individuals.16 Although the reasons for this apparent discrepancy are unknown, it may be partially attributable to the exclusion of publicly insured and uninsured individuals in the prior study, as well as potential differences in the ethnic diversity of the populations in the 2 studies. Notably, the Olmsted County population is considerably less ethnically diverse than the broader US population32; non-Hispanic white individuals represent 81% of the Olmsted County population compared with 61% of the US population.33, 34 Epidemiologic studies conducted in the United States have shown that the highest prevalence of CD is observed in non-Hispanic white individuals.30, 35, 36 Moreover, the geographic distribution of CD is heterogeneous, with higher rates observed in the Midwest than in other regions.11, 16, 35, 37 All this suggests that the extrapolation of CD prevalence from Olmsted County residents to the US population may very likely lead to a significant overestimation in the number of individuals with CD. The results of this sensitivity analysis should, therefore, be interpreted only as an upper limit for the estimated prevalence of fistulizing CD under the most extreme assumption regarding the total number of patients at risk.
CONCLUSIONS
This study is an attempt to estimate the prevalence rates for CD fistulas by validating a literature-based analysis with a large US claims database. As such, it highlights the significance of this devastating complication of CD. With >75,000 patients in the United States suffering from CD fistulas, there is a tremendous unmet need for novel therapeutic options in this subpopulation of patients with CD.
Supplementary Material
Conflicts of interest: D.A.S. has received grant support from UCB and has consulted for Takeda, TiGenix, AbbVie, Genentech, Gilead, Janssen, Pfizer, and UCB. I.T. is employed by Takeda Spain (TiGenix at the time of study conduct). M.C.D. is employed by TiGenix (Takeda Group). W.J.S. has received research grants from Takeda, AbbVie, Amgen, Atlantic Healthcare, Celgene/Receptos, Genentech, Gilead Sciences, Janssen, and Lilly; has consulted for Takeda, TiGenix, AbbVie, Allergan, Amgen, Boehringer Ingelheim, Celgene, Conatus, Cosmo, Escalier, Ferring, Genentech, Gilead, Janssen, Lilly, Miraca, Nivalis, Novartis, Oppilan, Otsuka, Paul Hastings, Pfizer, Precision IBD, Progenity, Prometheus, Ritter, Robarts Clinical Trials, Salix, Seres, Shire, Seres, Sigmoid, Tillotts, UCB, and Vivelix; and owns equity in Escalier, Oppilan, Precision IBD, Progenity, and Ritter.
Supported by: TiGenix. Medical writing and editorial support were provided by Ken Glasscock and Geoff Marx of BioScience Communications, New York, New York, and were funded by TiGenix. HVH Precision Analytics (formerly Vencore) supported the analysis from the US database.
REFERENCES
- 1. Siegmund B, Feakins RM, Barmias G, et al. . Results of the Fifth Scientific Workshop of the ECCO (II): pathophysiology of perianal fistulizing disease. J Crohns Colitis. 2016;10:377–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schwartz DA, Loftus EV Jr, Tremaine WJ, et al. . The natural history of fistulizing Crohn’s disease in Olmsted County, Minnesota. Gastroenterology. 2002;122:875–880. [DOI] [PubMed] [Google Scholar]
- 3. Mahadev S, Young JM, Selby W, et al. . Quality of life in perianal Crohn’s disease: what do patients consider important? Dis Colon Rectum. 2011;54:579–585. [DOI] [PubMed] [Google Scholar]
- 4. Scharl M, Rogler G. Pathophysiology of fistula formation in Crohn’s disease. World J Gastrointest Pathophysiol. 2014;5:205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nielsen OH, Rogler G, Hahnloser D, et al. . Diagnosis and management of fistulizing Crohn’s disease. Nat Clin Pract Gastroenterol Hepatol. 2009;6:92–106. [DOI] [PubMed] [Google Scholar]
- 6. Bell SJ, Williams AB, Wiesel P, et al. . The clinical course of fistulating Crohn’s disease. Aliment Pharmacol Ther. 2003;17:1145–1151. [DOI] [PubMed] [Google Scholar]
- 7. Sandborn WJ, Fazio VW, Feagan BG, Hanauer SB; American Gastroenterological Association Clinical Practice Committee AGA technical review on perianal Crohn’s disease. Gastroenterology. 2003;125:1508–1530. [DOI] [PubMed] [Google Scholar]
- 8. Molendijk I, Nuij VJ, van der Meulen-de Jong AE, et al. . Disappointing durable remission rates in complex Crohn’s disease fistula. Inflamm Bowel Dis. 2014;20:2022–2028. [DOI] [PubMed] [Google Scholar]
- 9. Eglinton TW, Barclay ML, Gearry RB, et al. . The spectrum of perianal Crohn’s disease in a population-based cohort. Dis Colon Rectum. 2012;55:773–777. [DOI] [PubMed] [Google Scholar]
- 10. Riss S, Schwameis K, Mittlböck M, et al. . Sexual function and quality of life after surgical treatment for anal fistulas in Crohn’s disease. Tech Coloproctol. 2013;17:89–94. [DOI] [PubMed] [Google Scholar]
- 11. Shivashankar R, Tremaine WJ, Harmsen WS, et al. . Incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota from 1970 through 2010. Clin Gastroenterol Hepatol. 2017;15:857–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. US Census Bureau. 2014 National population projections https://www.census.gov/data/tables/2014/demo/popproj/2014-summary-tables.html. Accessed April 2017.
- 13. Khalili H, Huang ES, Ananthakrishnan AN, et al. . Geographical variation and incidence of inflammatory bowel disease among US women. Gut. 2012;61:1686–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Loftus EV Jr, Silverstein MD, Sandborn WJ, et al. . Crohn’s disease in Olmsted County, Minnesota, 1940-1993: incidence, prevalence, and survival. Gastroenterology. 1998;114:1161–1168. [DOI] [PubMed] [Google Scholar]
- 15. Loftus CG, Loftus EV Jr, Harmsen WS, et al. . Update on the incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota, 1940-2000. Inflamm Bowel Dis. 2007;13:254–261. [DOI] [PubMed] [Google Scholar]
- 16. Kappelman MD, Moore KR, Allen JK, et al. . Recent trends in the prevalence of Crohn’s disease and ulcerative colitis in a commercially insured US population. Dig Dis Sci. 2013;58:519–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gollop JH, Phillips SF, Melton LJ 3rd, et al. . Epidemiologic aspects of Crohn’s disease: a population based study in Olmsted County, Minnesota, 1943-1982. Gut. 1988;29:49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhu YF, Tao GQ, Zhou N, et al. . Current treatment of rectovaginal fistula in Crohn’s disease. World J Gastroenterol. 2011;17:963–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Valente MA, Hull TL. Contemporary surgical management of rectovaginal fistula in Crohn’s disease. World J Gastrointest Pathophysiol. 2014;5:487–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hannaway CD, Hull TL. Current considerations in the management of rectovaginal fistula from Crohn’s disease. Colorectal Dis. 2008;10:747–755; discussion 755. [DOI] [PubMed] [Google Scholar]
- 21. Hawker PC, Givel JC, Keighley MR, et al. . Management of enterocutaneous fistulae in Crohn’s disease. Gut. 1983;24:284–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gómez-Senent S, Barreiro-de-Acosta M, García-Sánchez V. Enterocutaneous fistulas and Crohn’s disease: clinical characteristics and response to treatment. Rev Esp Enferm Dig. 2013;105:3–6. [DOI] [PubMed] [Google Scholar]
- 23. Taggarshe D, Bakston D, Jacobs M, et al. . Management of enterocutaneous fistulae: a 10 years experience. World J Gastrointest Surg. 2010;2:242–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Poritz LS, Rowe WA, Koltun WA. Remicade does not abolish the need for surgery in fistulizing Crohn’s disease. Dis Colon Rectum. 2002;45:771–775. [DOI] [PubMed] [Google Scholar]
- 25. Orangio GR. Enterocutaneous fistula: medical and surgical management including patients with Crohn’s disease. Clin Colon Rectal Surg. 2010;23:169–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Levy C, Tremaine WJ. Management of internal fistulas in Crohn’s disease. Inflamm Bowel Dis. 2002;8:106–111. [DOI] [PubMed] [Google Scholar]
- 27. Rocca WA, Yawn BP, St Sauver JL, et al. . History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87:1202–1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. St Sauver JL, Grossardt BR, Yawn BP, et al. . Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41:1614–1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Park SH, Aniwan S, Scott Harmsen W, et al. . Update on the natural course of fistulizing perianal Crohn’s disease in a population-based cohort. Inflamm Bowel Dis. 2018;25:1054–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Herrinton LJ, Liu L, Lewis JD, et al. . Incidence and prevalence of inflammatory bowel disease in a Northern California managed care organization, 1996-2002. Am J Gastroenterol. 2008;103:1998–2006. [DOI] [PubMed] [Google Scholar]
- 31. Shapiro JM, Zoega H, Shah SA, et al. . Incidence of Crohn’s disease and ulcerative colitis in Rhode Island: report from the Ocean State Crohn’s and Colitis Area Registry. Inflamm Bowel Dis. 2016;22:1456–1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. St Sauver JL, Grossardt BR, Leibson CL, et al. . Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012;87:151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. US Census Bureau. Quick facts https://www.census.gov/quickfacts/fact/table/US/PST045216. Accessed September 2017.
- 34. US Census Bureau. Quick facts https://www.census.gov/quickfacts/fact/table/olmstedcountyminnesota/RHI125216#viewtop. Accessed September 2017.
- 35. Betteridge JD, Armbruster SP, Maydonovitch C, et al. . Inflammatory bowel disease prevalence by age, gender, race, and geographic location in the U.S. Military health care population. Inflamm Bowel Dis. 2013;19:1421–1427. [DOI] [PubMed] [Google Scholar]
- 36. Wang YR, Loftus EV Jr, Cangemi JR, et al. . Racial/ethnic and regional differences in the prevalence of inflammatory bowel disease in the United States. Digestion. 2013;88:20–25. [DOI] [PubMed] [Google Scholar]
- 37. Kappelman MD, Rifas-Shiman SL, Kleinman K, et al. . The prevalence and geographic distribution of Crohn’s disease and ulcerative colitis in the United States. Clin Gastroenterol Hepatol. 2007;5:1424–1429. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.