Abstract
Objective
Soy has been associated with lower risk of cardiovascular disease in Asian countries which consume daily soy. Our study examined whether production of equol, an estrogen metabolite, affected the ability of soy nuts to improve cardiovascular risk factors.
Materials/Methods
Sixty postmenopausal women participated in a randomized, controlled, crossover trial of a Therapeutic Lifestyle Changes (TLC) diet alone and a TLC diet in which 0.5 cups of soy nuts (25 g of soy protein and 101 mg of aglycone isoflavones) replaced 25 g of nonsoy protein daily. Each diet was followed for 8 weeks at the end of which blood pressure (BP), lipid levels, adhesion molecules and inflammatory markers were measured.
Results
Women with MetS had significantly higher baseline body mass index (BMI), BP, triglycerides (TG), and soluble intercellular adhesion molecule (sICAM) than women without MetS. In women with MetS on the soy diet, significant reductions in diastolic BP (7.7%; P=0.02), TG (22.9%; P=0.02), C-reactive protein (CRP) (21.4%; P=0.01) and sICAM (7.3%; P=0.03) were noted among equol producers compared to levels on the TLC diet. No significant changes were noted in equol nonproducers. Similarly, in women without MetS, only equol-producers had significant reductions in diastolic BP (3.3%, P=0.02) and CRP (30%, P=0.04). In contrast to women with MetS, TG and sICAM levels were not affected in women without MetS, a finding possibly related to lower baseline levels.
Conclusions
Cardiovascular risk reduction with soy nuts is not uniform and may be greater among producers of equol.
Keywords: Soy protein, isoflavones, equol, blood pressure, metabolic syndrome, inflammatory markers
1. Introduction
Coronary heart disease (CHD) is the leading cause of death among women aged 60 years and older. The incidence rises in postmenopausal women presumably due to loss of estrogen, which has vascular protective effects [1,2]. Hormone replacement therapy has been associated with increased risk of cardiovascular disease (CVD), cancer and dementia [3]; therefore, alternative vasoactive agents have been studied for their potential to decrease cardiovascular morbidity and mortality. Daily soy food intake has been associated with a reduction in CHD risk factors in Chinese women [4,5] and was inversely proportional to serum cholesterol level in Japanese adults [6]. Higher intake of dietary soy has been associated with lower cardiovascular mortality in Japanese women [7].
The metabolic syndrome (MetS) is comprised of a cluster of closely related risk factors, including visceral adiposity, insulin resistance, hypertension and dyslipidemia that increase cardiovascular risk [8]. The risk of CHD attributed to MetS is more than twice in women compared to men and more than half of all cardiovascular events in women are related to MetS [9]. Postmenopausal status is independently associated with a 60% additional risk of MetS after adjusting for age, body mass index (BMI), lifestyle-related factors and socioeconomic status [10]. This may be at least partly due to decline in circulating estrogen levels, which may increase cardiovascular risk through effects on adiposity, blood pressure (BP), lipid metabolism and prothrombotic state [11,12]. The prevalence of MetS in postmenopausal women aged 50–59 years is around 35% and increases to around 45% for women aged ≥60 [13].
We previously reported that substituting a whole soy food (soy nuts) for nonsoy protein in a therapeutic lifestyle changes (TLC) diet lowered systolic and diastolic BP in hypertensive, prehypertensive and normotensive women [14] and that the beneficial effect may be mediated via an effect on inflammation [15]. Since our original study design, the potential role of equol, an estrogen metabolite which can be formed from the soy isoflavone daidzein, in mediating beneficial effects of soy has become apparent [16]. Equol might be predicted to lower cardiovascular risk via potent inhibition of inflammation and oxidation [17]. Therefore, we performed a post-hoc analysis of our data stratified by equol production and metabolic syndrome status to test the hypothesis that equol production status affects the ability of soy nuts to lower BP and improve lipid levels and inflammatory markers in postmenopausal women.
2. Material and Methods
2.1 Subjects
Sixty healthy postmenopausal women (absence of menses for at least 12 months or irregular periods and hot flashes) without atherosclerosis or diabetes participated in this study. These are the same women in our prior report in which inclusion and exclusion criteria were described [14]. The institutional review board of the Beth Israel Deaconess Medical Center approved the protocol, and all participants gave informed consent.
2.2 Study Design
This was a randomized controlled crossover trial of the effect of one-half cup of soy nuts daily for 8 weeks on cardiovascular risk factors in postmenopausal women with and without MetS. A registered dietitian instructed the participants to consume a TLC diet, which consisted of 30% of energy from total fat (≤7% saturated fat, 12% monounsaturated fat, and 11% polyunsaturated fat), 15% from protein and 55% from carbohydrate; less than 200 mg of cholesterol per day [18]; and 1200 mg of calcium and 2 fatty fish meals per week. Those ingesting suboptimal dietary calcium were given calcium carbonate supplementation.
After a 4-week diet run-in, participants adherent to the TLC diet (from review of two 3-day food records) were randomized in a crossover design between 2 diet sequences for 8-week periods: the TLC diet without soy or the TLC diet with prepackaged daily allowances of one-half cup of unsalted soy nuts (Genisoy, Fairfield, Calif) containing 25 g of soy protein and 101 mg of aglycone isoflavones divided into 3 or 4 portions spaced throughout the day. Detailed nutritional composition of one-half cup of soy nuts has been previously published [14]. We chose a whole soy food, dry-roasted soybeans, which were administered 3 times daily to mimic Asians who consume whole soy food or fermented soy products high in aglycone isoflavones at several times throughout the day.
After a 4-week washout on the TLC diet alone, participants crossed over to the other arm for an additional 8 weeks. Participants were individually advised from which sources to decrease their protein intake to compensate for the 25 g of soy protein in the soy diet arm to keep protein amounts similar on both diet arms. At the end of each 8-week period, fasting blood was collected for measurement of lipid levels, and participants collected a 24-hour urine sample for measurement of isoflavone and creatinine levels. Dietary assessment (from 3-day food records) and exercise assessment was as previously described [14].
2.3 MetS criteria and blood pressure measurements
The assessment of MetS was based on the presence of three of its five components according to a modified version of the Adult Treatment Panel III guidelines [18] for women: 1. BMI ≥ 28.8 kg/m2; 2. triglyceride levels of 150 mg/dL or greater; 3. High- density lipoprotein cholesterol (HDL-C) level less than 50 mg/dL; 4. BP of 130/85 mm Hg or higher; and 5. abnormal glucose metabolism as identified by a fasting blood glucose level of 100 mg/dL or higher. Because waist circumference was not available at baseline, a cutpoint for obesity of BMI (calculated as the ratio of body mass expressed in kilograms to the square of height expressed in meters) of 28.8 kg/m2 or higher was used as a surrogate. A similar modification has been previously used [19]. BP measurements were performed with cycling dynamaps (GE Medical Systems Information Technologies, Inc, Milwaukee, Wis) at the end of each diet period as previously described [14,20,21].
2.4 Laboratory measurements
Fasting blood samples and 24-hour urines were obtained at screening and at the end of each diet period. Lipids, glucose, apolipoprotein B-100 (apoB), serum soluble vascular cell adhesion molecule 1 (sVCAM-1), sICAM-1, interleukin-6 (IL-6), matrix metalloproteinease 9 (MMP-9), high-sensitivity C-reactive protein (CRP) and isoflavones and equol were measured as previously described [14,15,22,23]. An equol producer was defined as having an equol level greater than 1000 nmol/L in the urine [24,25].
2.5 Statistical analyses
Results are expressed as mean ± SD. Continuous variables were compared using 2-tailed paired (within MetS group) and unpaired (No MetS to MetS) t tests. A repeated-measures analysis of variance was performed to examine whether there was a carryover effect from the order of diets, with order and treatment as independent variables and outcome as the dependent variable. Normality tests were conducted using the Shapiro-Wilk test. For skewed variables (all lipid levels and CRP), log-transformed values were used in all analyses and reported as geometric mean ± SD. A probability value P ≤ 0.05 was considered statistically significant.
3. Results
Baseline characteristics were compared in women with and without MetS (Table 1). Mean age and time since menopause were similar in the two groups; however, women with MetS had higher BMI, systolic BP, diastolic BP, TG, apoB and sICAM and lower HDL levels at baseline compared to women without MetS.
Table 1.
Baseline Characteristics by Metabolic Syndrome Status1
| Characteristic | No Metabolic Syndrome (n = 49) | Metabolic Syndrome (n = 11) | P value |
|---|---|---|---|
| Age (years) | 54.6±5.8 | 54.1±6.5 | 0.80 |
| BMI (kg/m2) | 24.6±3.8 | 31.8±4.6 | <0.001 |
| Years since menopause | 5.4±4.8 | 4.1±5.0 | 0.44 |
| Equol producers | 28 | 7 | |
| SBP (mmHg) | 120.0±15.0 | 136.6±24.1 | 0.005 |
| DBP (mmHg) | 71.2±10.8 | 79.3±8.6 | 0.02 |
| Exercise (min/wk) | 167.5±145.7 | 121.3±77.2 | 0.28 |
| Exercise (d/wk) | 3.9±2.4 | 3.6±2.2 | 0.40 |
| Glucose (mg/dl) | 97.7±10.7 | 100.1±7.7 | 0.48 |
| Total-C (mg/dl) | 222.33±40.2 | 240.4±59.5 | 0.20 |
| LDL-C (mg/dl) | 138.7±32.4 | 148.6±56.1 | 0.39 |
| HDL-C (mg/dl) | 59.3±13.4 | 45.6±8.7 | 0.001 |
| TG (mg/dl) | 91.2±76.4 | 192.3±109.8 | <0.001 |
| Non- HDL-C | 160.7±39.1 | 192.8±58.9 | 0.02 |
| TC/HDL-C | 3.7±1.0 | 5.3±1.6 | <0.001 |
| LDL-C/HDL-C | 2.3±0.7 | 3.3±1.1 | 0.001 |
| TG/HDL-C | 1.5±2.2 | 4.2±4.4 | <0.001 |
| Apo B (mg/dl) | 109.3±20.1 | 130.3±32.8 | 0.01 |
| sICAM-1 (ng/ml) | 276.6±57.4 | 322.1±57.0 | 0.02 |
| sVCAM-1 (ng/ml) | 600.0±125.8 | 568.4±83.2 | 0.43 |
| CRP (mg/dl) | 0.10±0.21 | 0.17±0.80 | 0.22 |
| IL-6 (ng/ml) | 2.5±1.7 | 2.7±1.6 | 0.78 |
| Fibrinogen (mg/dl) | 415.9±76.0 | 445.7±94.3 | 0.27 |
| MMP-9 (ng/ml) | 34.3±13.2 | 36.5±11.1 | 0.62 |
Values given as mean ± SD.
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; Total-C, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high- density lipoprotein cholesterol; TG, triglycerides; Apo B, Apolipoprotein B; sVCAM-1, vascular cell adhesion molecule-1; sICAM-1, soluble intercellular adhesion molecule-1; CRP, C-reactive protein; IL-6, interleukin-6; MMP-9, matrix metalloproteinase-9.
3.1 Isoflavone levels and dietary content
Soy nut compliance was assessed by urinary isoflavone levels, which were significantly higher in the soy diet arm compared with the control diet arm for daidzein, genistein and equol for both groups of women (Table 2). Glycitein levels were higher in women without MetS on a soy diet. Thirty-five women (58%) were equol producers. Levels of enterolactone, a lignan phytoestrogen found in fruits and vegetables [25], were not significantly different in the control versus soy diet arm for women with and without MetS, a finding suggesting that fruit and vegetable intake was similar in both diets.
Table 2.
Urinary Isoflavone Concentrations in the Control vs Soy Diet Arms in Women by Metabolic Syndrome Status1
| Isoflavone | No Metabolic Syndrome (n=49) | Metabolic Syndrome (n=11) | ||||
|---|---|---|---|---|---|---|
| Control Diet | Soy Diet | P value2 | Control Diet | Soy Diet | P value2 | |
| Genistein | 0.47±0.99 | 6.39±8.21 | <0.001 | 0.03±0.07 | 4.10±4.37 | 0.01 |
| Daidzein | 0.27±0.66 | 21.63±14.26 | <0.001 | 0.17±0.172 | 12.64±8.67 | 0.0001 |
| Glycitein | 0.11±0.42 | 1.62±1.05 | <0.001 | 0.36±1.14 | 0.95±0.65 | 0.21 |
| Equol | 0.05±0.19 | 4.22±7.05 | <0.001 | 0.002±0.004 | 4.92±6.02 | 0.02 |
| Enterolactone | 2.30±3.69 | 2.34±3.54 | 0.95 | 3.01±8.62 | 1.83±3.28 | 0.52 |
Values given as mean ± SD μg/mg creatinine;
Paired samples t test in women on the soy diet compared to the control diet in each group according to the metabolic syndrome status.
Analysis of dietary content revealed that total and saturated fat levels were significantly lower and protein significantly higher on the soy diet compared with the control diet in both groups of women (Table 3). Polyunsaturated fat content was higher on the soy diet in both groups of women but reached significance only in those without MetS. Cholesterol levels were less than 200 mg per day in each diet arm and saturated fat content was close to goal (7%), suggesting compliance with the TLC diet.
Table 3.
Dietary Content in the Control vs Soy Diet Arms in Women by Metabolic Syndrome Status1
| Component | No Metabolic Syndrome (n=49) | Metabolic Syndrome (n=11) | ||||
|---|---|---|---|---|---|---|
| Control | Soy | P value | Control | Soy | P value | |
| Kilocalories | 1385±325 | 1591±389 | <0.001 | 1587±275 | 1780±521 | 0.06 |
| Total Fat (g) | 24.6±7.3 | 19.9±6.6 | <0.001 | 27.1±5.9 | 19.2±5.6 | 0.02 |
| Saturated Fat (g) | 7.45±3.2 | 6.3±2.5 | 0.002 | 9.4±2.0 | 6.2±2.1 | 0.001 |
| Monounsaturated Fat (g) | 7.9±4.4 | 7.3±2.3 | 0.18 | 8.2±2.7 | 6.8±2.1 | 0.42 |
| Polyunsaturated Fat (g) | 5.2±2.8 | 7.8±2.1 | <0.001 | 4.8±2.0 | 6.0±1.1 | 0.40 |
| Protein (g) | 17.2±3.9 | 20.64±3.3 | <0.001 | 16.2±2.6 | 19.5±2.9 | 0.02 |
| Carbohydrate (g) | 55.7±8.6 | 52.2±7.0 | 0.001 | 52.8±10.3 | 52.1±5.9 | 0.84 |
| Cholesterol (mg) | 149±63.0 | 134±65.7 | 0.12 | 170±45.9 | 145±123 | 0.37 |
Values are mean ± SD
3.2 Effect on blood pressure, lipids and inflammatory markers
Table 4 compares changes in women with MetS compared to those without MetS. Diastolic BP was significantly lowered by soy compared to the control diet in women with MetS (5.4%, P = 0.03) and in women without MetS (3.4%, P = 0.008). In women without MetS, systolic BP was significantly lowered (5.9%, P < 0.001) whereas there was a similar % reduction in women with MetS (6.7%) of borderline significance (P = 0.10). CRP was lowered 11.8% (P = 0.04) and 30% (P = 0.01) in women with and without MetS, respectively, on the soy diet compared to control. Otherwise, there were no significant changes in women without MetS. In contrast, women with MetS had significant reductions in TG (17.8%, P = 0.04) and sICAM (5.2%, P = 0.04) on the soy diet compared to the control diet. Of note, VCAM approached significance but there were no changes in apoB, IL-6, fibrinogen or MMP-9 (data not shown). Order of diets did not affect response in either group of women stratified by MetS status. There was no statistically significant change in either BMI or exercise on the soy diet vs the control diet for women with or without MetS; therefore, neither weight change nor exercise level accounts for the beneficial effects observed in the soy diet arm.
Table 4.
Pre- (Control) and Post- (Soy) Dietary Intervention Results in Women With and Without Metabolic Syndrome1
| Variable (unit) | No Metabolic Syndrome (n=49) | Metabolic Syndrome (n=11) | P at baseline4 | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Control | Soy | Change (%) | P value2 | Control | Soy | Change (%) | P value3 | ||
| BMI (kg/m2) | 24.6±3.8 | 24.7±3.8 | None | 0.14 | 31.8±4.6 | 31.4±4.9 | 1.3↓ | 0.09 | <0.001 |
| SBP (mmHg) | 120.0.±15.0 | 112.9±14.8 | 5.9↓ | <0.001 | 136.6±24.1 | 127.4±17.3 | 6.7↓ | 0.10 | 0.005 |
| DBP (mmHg) | 71.2±10.8 | 68.8±9.8 | 3.4↓ | 0.008 | 79.3 ±8.6 | 75.0±8.0 | 5.4↓ | 0.03 | 0.02 |
| Exercise (min/wk) | 167.5±145.7 | 160.6±137.6 | 4.1↓ | 0.39 | 121.3±77.2 | 110.0±87.0 | 9.3↓ | 0.51 | 0.28 |
| Glucose (mg/dl) | 97.7±10.7 | 96.5±9.7 | 1.2↓ | 0.26 | 100.1±7.7 | 98.0±8.5 | 2.1↓ | 0.35 | 0.48 |
| Total-C (mg/dl) | 222.3±40.2 | 222.33±36.4 | None | 0.96 | 240.4±59.5 | 223.9±48.8 | 6.9↓ | 0.09 | 0.20 |
| LDL-C (mg/dl) | 138.7±32.4 | 139.6±31.8 | 0.6↑ | 0.63 | 148.6±56.1 | 140.3±44.3 | 5.6↓ | 0.34 | 0.39 |
| HDL-C (mg/dl) | 59.3±13.4 | 60.7±12.1 | 2.3↑ | 0.12 | 45.6±8.7 | 45.0±9.1 | 1.3↓ | 0.56 | 0.001 |
| TG (mg/dl) | 91.2±76.4 | 88.9±65.7 | 2.5↓ | 0.59 | 192.3±109.8 | 158.1±74.5 | 17.8↓ | 0.04 | <0.001 |
| TG/HDL-C | 1.5±2.2 | 1.4±1.4 | 6.7↓ | 0.22 | 4.2±4.4 | 3.5±2.5 | 16.7↓ | 0.06 | <0.001 |
| sICAM-1 (ng/ml) | 276.6±57.4 | 280.5±55.3 | 1.4↑ | 0.40 | 322.1±57.0 | 305.5±45.9 | 5.2↓ | 0.04 | 0.02 |
| sVCAM-1 (ng/ml) | 600.0±125.8 | 579.4±107.6 | 3.4↓ | 0.06 | 568.4±83.2 | 541.2±77.6 | 4.8↓ | 0.08 | 0.43 |
| CRP (mg/dl) | 0.10±0.21 | 0.07±0.09 | 30.0↓ | 0.01 | 0.17±0.80 | 0.15±0.72 | 11.8↓ | 0.04 | 0.22 |
Values given as mean ± SD;
Post-dietary intervention values in women without metabolic syndrome on the soy diet compared to the control diet;
Post-dietary intervention values in women with metabolic syndrome on the soy diet compared to the control diet;
Baseline values in women with metabolic syndrome compared to women without metabolic syndrome.
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; Total-C, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; sVCAM-1, vascular cell adhesion molecule-1; sICAM-1, soluble intercellular adhesion molecule-1; CRP, C-reactive protein; ↓, percent decrease; and ↑, percent increase on soy nuts versus control.
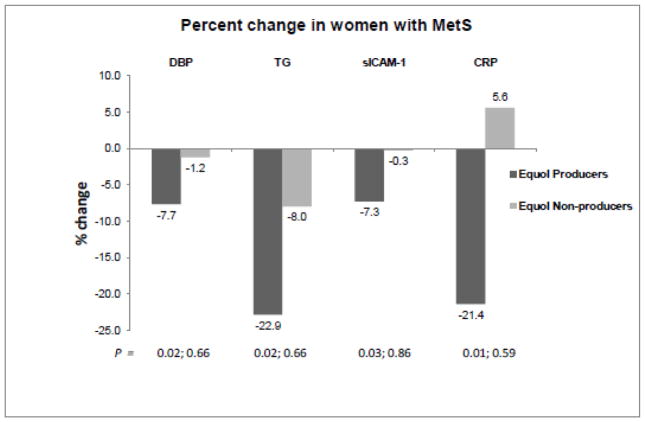
When women with MetS were stratified by equol production status, equol producers had significant reductions in diastolic BP (7.7%; P = 0.02), TG (22.9%; P = 0.02), C-reactive protein (CRP) (21.4%; P = 0.01) and sICAM (7.3%; P = 0.03) on the soy diet compared to levels on the TLC diet whereas nonproducers did not (Figure 1 and Table 5).
Figure 1.
Percent change on soy diet compared to control diet in women with metabolic syndrome among equol producers (dark bars) and equol nonproducers (lighter bars). P values are for soy vs control diet.
Table 5.
Pre- (Control) and Post-(Soy) Dietary Intervention Levels in Women with Metabolic Syndrome Stratified by Equol-Production1
| Variable (unit) | Equol producers (n=7) | Equol non-producers (n=4) | P at baseline4 | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Control | Soy | Change (%) | P value2 | Control | Soy | Change (%) | P value3 | ||
| BMI (kg/m2) | 31.4±5.4 | 30.9±5.7 | 1.6↓ | 0.10 | 32.5±3.4 | 32.3±3.8 | 0.6↑ | 0.65 | 0.73 |
| SBP (mmHg) | 133.2±27.7 | 123.2±20.1 | 7.5↓ | 0.22 | 142.5±17.9 | 134.6±8.9 | 5.5↓ | 0.30 | 0.57 |
| DBP (mmHg) | 79.1±9.9 | 73.0±8.7 | 7.7↓ | 0.02 | 79.6±6.8 | 78.6±6.2 | 1.2↓ | 0.66 | 0.94 |
| Exercise (min/wk) | 80.0±56.7 | 80.2±45.3 | 0.2↑ | 0.99 | 173.0.0±59 | 147.2±122.2 | 14.9↓ | 0.51 | 0.02 |
| Glucose (mg/dl) | 101.7±9.2 | 101.7±6.7 | None | 1.00 | 97.3±3.2 | 91.5±8.1 | 6.0↓ | 0.11 | 0.38 |
| Total-C (mg/dl) | 237.1±71.4 | 228.0±56.9 | 3.8↓ | 0.25 | 246.0±39.7 | 216.3±35.6 | 12.1↓ | 0.26 | 0.81 |
| LDL-C (mg/dl) | 140.6±68.1 | 141.2±54.0 | 0.4↑ | 0.93 | 162.9±32.3 | 138.7±25.6 | 14.8↓ | 0.27 | 0.51 |
| HDL-C (mg/dl) | 44.2±10.8 | 45.0±11.6 | 1.8↑ | 0.60 | 48.2±3.3 | 44.9±2.7 | 6.8↓ | 0.11 | 0.53 |
| TG (mg/dl) | 199.5±137.0 | 153.8±88.3 | 22.9↓ | 0.02 | 180.7±17.3 | 166.3±53.9 | 8.0↓ | 0.66 | 0.29 |
| TG/HDL-C | 4.5±5.4 | 3.4±3.2 | 24.4↓ | 0.01 | 3.8±0.5 | 3.7±1.1 | 2.6↓ | 0.97 | 0.68 |
| sICAM-1 (ng/ml) | 341.3±51.7 | 316.3±46.4 | 7.3↓ | 0.03 | 288.5±55.5 | 286.7±44.3 | 0.3↓ | 0.86 | 0.15 |
| sVCAM-1 (ng/ml) | 567.8±95.4 | 542.8±89.2 | 4.4↓ | 0.19 | 569.2±69.6 | 538.3±64.3 | 5.4↓ | 0.32 | 0.98 |
| CRP (mg/dl) | 0.14±1.00 | 0.11±0.92 | 21.4↓ | 0.01 | 0.34±0.24 | 0.36±0.20 | 5.6↑ | 0.59 | 0.47 |
Values given as mean ± SD;
Post-dietary intervention values in equol-producing women on the soy diet compared to the control diet;
Post-dietary intervention values in non-equol-producing women on the soy diet compared to the control diet;
Baseline values in women with metabolic syndrome stratified by equol production status.
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; Total-C, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high- density lipoprotein cholesterol; TG, triglycerides; sVCAM-1, vascular cell adhesion molecule-1; sICAM-1, soluble intercellular adhesion molecule-1; CRP, C-reactive protein; ↓, percent decrease; and ↑, percent increase on soy nuts versus control.
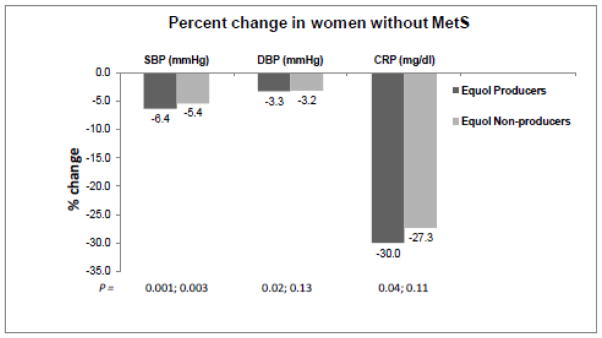
Similarly, in women without MetS, only equol producers had significant reductions in diastolic BP (3.3%, P = 0.02) and CRP (30%, P = 0.04) (Figure 2 and Table 6). In contrast to their counterparts with MetS, TG and sICAM were not affected in women without MetS, a finding possibly related to lower baseline levels of these molecules. Systolic BP was significantly lowered in both producers and nonproducers without MetS (Table 6).
Figure 2.
Percent change on soy diet compared to control diet in women without metabolic syndrome among equol producers (dark bars) and equol nonproducers (lighter bars). P values are for soy vs control diet.
Table 6.
Pre- (Control) and Post-(Soy) Dietary Intervention Levels in Women Without Metabolic Syndrome Stratified by Equol-Production1
| Variable (unit) | Equol producers (n=28) | Equol non-producers (n=21) | P at baseline4 | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Control | Soy | Change (%) | P value2 | Control | Soy | Change (%) | P value3 | ||
| BMI (kg/m2) | 23.3±2.8 | 23.3±2.8 | None | 0.425 | 26.5±4.3 | 26.6±4.3 | 0.4↑ | 0.16 | 0.003 |
| SBP (mmHg) | 118.8±14.7 | 111.2±15.4 | 6.4↓ | <0.001 | 121.6±15.5 | 115.0±13.9 | 5.4↓ | 0.003 | 0.53 |
| DBP (mmHg) | 70.4±11.2 | 68.1±10.3 | 3.3↓ | 0.02 | 72.1±10.2 | 69.8±9.3 | 3.2↓ | 0.13 | 0.60 |
| Exercise (min/wk) | 174.4±161.5 | 161.6±147.6 | 7.3↓ | 0.32 | 157.6±123.3 | 159.0±126.1 | 0.9↑ | 0.83 | 0.71 |
| Glucose (mg/dl) | 94.9±9.4 | 94.6±8.4 | 0.3↓ | 0.81 | 101.4±11.4 | 99.1±10.8 | 2.3↓ | 0.20 | 0.03 |
| Total-C (mg/dl) | 216.8±33.9 | 217.2±31.8 | 0.2↑ | 0.89 | 230.7±47.9 | 230.1±41.9 | 0.3↓ | 0.92 | 0.29 |
| LDL-C (mg/dl) | 133.6±25.1 | 135.5±27.2 | 1.4↑ | 0.58 | 146.8±40.8 | 146.5±37.7 | 0.2↓ | 0.96 | 0.15 |
| HDL-C (mg/dl) | 59.2±14.6 | 61.1±13.3 | 3.1↑ | 0.09 | 58.3±11.7 | 58.6±10.2 | 0.5↑ | 0.82 | 0.91 |
| TG (mg/dl) | 87.7±82.6 | 80.2±63.1 | 8.5↓ | 0.19 | 96.6±69.0 | 103.0±68.5 | 6.2↑ | 0.28 | 0.43 |
| TG/HDL-C | 1.5±2.5 | 1.3±1.3 | 13.3↓ | 0.05 | 1.6±1.6 | 1.7±1.6 | 5.9↑ | 0.43 | 0.78 |
| sICAM-1 (ng/ml) | 279.0±61.3 | 282.0±54.1 | 1.1↑ | 0.29 | 273.0±52.6 | 278.3±58.5 | 1.9↑ | 0.29 | 0.73 |
| sVCAM-1 (ng/ml) | 578.4±115.5 | 564.5±87.8 | 2.4↓ | 0.34 | 629.3±136.3 | 599.7±129.7 | 4.7↓ | 0.07 | 0.18 |
| CRP (mg/dl) | 0.10±0.25 | 0.07±0.10 | 30.0↓ | 0.04 | 0.11±0.13 | 0.08±0.06 | 27.3↓ | 0.11 | 0.91 |
Values given as mean ± SD;
Post-dietary intervention values in equol-producing women on the soy diet compared to the control diet;
Post-dietary intervention values in non-equol-producing women on the soy diet compared to the control diet;
Baseline values in women without metabolic syndrome stratified by equol production status.
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; Total-C, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high- density lipoprotein cholesterol; TG, triglycerides; sVCAM-1, vascular cell adhesion molecule-1; sICAM-1, soluble intercellular adhesion molecule-1; CRP, C-reactive protein; ↓, percent decrease; and ↑, percent increase on soy nuts versus control.
When stratified by equol production, TG/HDL ratio, a measure of insulin resistance, was significantly lower in equol-producing women both with and without MetS (24% reduction and 13.3% reduction on soy compared to control, P = 0.01 and P = 0.05, respectively) (Tables 5 and 6, respectively).
4. Discussion
The new finding in this post-hoc analysis of our randomized, controlled crossover trial of soy nuts consumed several times daily for 8 weeks is that only equol producers among women with MetS had significant reductions in diastolic BP, TG, TG/HDL ratio, CRP and sICAM-1 on a soy diet compared to the TLC diet without soy. Similarly, among those without MetS, only equol producers had significant reductions in diastolic BP, CRP and TG/HDL ratio; however, the differential effect was less marked compared to women with MetS. The lack of effect on TG and sICAM in those without MetS is probably due to lower baseline levels of these biomarkers in women without MetS compared to the higher levels in those with MetS, a finding which suggests that soy may have more effect when cardiovascular risk factors and inflammation are higher. Taken together, these findings suggest a role of equol in mediating beneficial effects of soy.
Equol is a biologically active estrogenic metabolite produced from the soy isoflavone daidzein by microbial biotransformation in the intestine usually in less than 50% of subjects consuming soy [16]. Inflammatory mechanisms underlie atherosclerosis with endothelial injury caused by hypertension and/or hypercholesterolemia leading to activation of NF-κB which in turn causes expression of cellular adhesion molecules as VCAM-1 and ICAM-1 on the endothelial wall [26]. Circulating leukocytes and monocytes bind to these adhesion molecules and are taken up into the subendothelial space where they become macrophages and foam cells, which take up oxidized LDL and develop into fatty streaks, the precursor of the atheromatous lesion. Equol is a potent inhibitor of oxidation and therefore, may protect against CVD by preventing oxidation of LDL [reviewed in ref 27]. Equol has also been shown to block LPS-induced NF-κB activation in RAW 264.7 cells and thus, may be predicted to lower CVD risk by inhibiting inflammation [17]. In the current study, the significant reductions in CRP and sICAM-1 in women with MetS who produced equol in response to soy suggests that equol may mediate a beneficial effect through a favorable effect on inflammation and adhesion molecules in women with high cardiometabolic risk. Among postmenopausal women in the Women’s Health study, CRP was the most powerful predictor of cardiovascular risk, and the relative risk of cardiovascular events was greater in subjects with elevated CRP compared to those with abnormal serum lipids [28]. In this context, it could be predicted that the significant reductions in CRP with soy in the current study in equol producers both with and without MetS may indicate a reduction in inflammation which may lower cardiovascular risk in postmenopausal women.
Hypertension, one component of MetS, alone conveys a 4-fold risk of CHD compared to normotensive women [29,30]. Equol may protect against CVD by increasing the transcription of endothelial nitric oxide synthase and increasing levels of nitric oxide, a vasodilator which may lower blood pressure [reviewed in ref 27]. Soy lowered systolic BP in the current study in women with and without MetS. The ability to produce equol was a more important factor in lowering diastolic BP in those with MetS than those without MetS, a finding suggesting that equol production may be especially important in women with high cardiometabolic risk.
The Lipid Research Clinic data showed that TG and HDL-C are better predictors of cardiovascular risk in women than LDL-C [31]. Moreover, in a meta-analysis of 17 population-based studies, a TG level increase of 1 mmol/l (89 mg/dl) was associated with a 76% increase in the risk of CVD in women [32]. Therefore, modalities lowering TG would be predicted to lower risk of CVD in women. In the present study, we observed a significant 17.8% reduction in TG levels with the soy diet in women with MetS, a finding possibly related to the higher baseline TG (192±109.8 mg/dL) in women with MetS compared to women without MetS (baseline TG 91.2±76.4 mg/dL). Moreover, only those with MetS who produced equol had a significant reduction in TG level (22.9%). Therefore, the current study suggests that whole dietary soy is most effective in lowering TG in women with MetS who produce equol. Our observation on TG levels is in line with results from a cross-sectional study of 572 Chinese adults (362 women and 210 men) in which equol secretors had a 38.2% lower serum triglyceride level (p=0.012) compared to nonproducers [33]. Equol producers also had a 4.9% lower carotid intima-media thickness (P = 0.033) compared to equol nonproducers. Moreover, the equol excretors with higher daily isoflavone intakes had significantly lower carotid intima-media thickness (16.2 % lower, p-0.035) and a trend toward higher HDL-C levels than those with lower isoflavone intakes whereas no association was observed between isoflavone intake and serum lipids or carotid intima-media thickness in nonproducers.
Three additional soy studies have analyzed results by equol status. Clerici et al. [34] observed that in 62 subjects with a baseline LDL of 186.8 mg/dL, a pasta enriched with 33 mg isoflavone aglycones (but without soy protein) reduced TC and LDL-C by 7.3% and 8.6%, respectively, lowered CRP 42% and increased brachial arterial flow-mediated vasodilatation 2.3 ± 0.8% (P=0.003) from baseline whereas there was no change in the control group which consumed conventional pasta. When stratified by equol production, only the equol producers had significant changes. In a 12-month, double-blind randomized trial, 202 postmenopausal women were randomized to isolated soy protein with 99 mg isoflavones/day or milk protein (placebo). Post-hoc analysis revealed that equol producers had lower systolic BP (P=0.09) and diastolic BP and better endothelial function on soy compared to nonproducers in whom systolic BP and diastolic BP actually increased and endothelial function deteriorated although these results were not significant [35]. Finally, in the Women’s Isoflavone Soy Health study of 350 postmenopausal women randomized to 25 g soy protein containing 91 mg isoflavones or placebo, subclinical atherosclerosis progression assessed by carotid artery intima-media thickness (CIMT) was reduced by 16% in the soy group, although the treatment effect was not statistically significant [36]. In contrast to the present and prior studies, there was no difference in CIMT progression by equol production status. Interestingly, soy supplementation appeared to be more beneficial among recently postmenopausal women as compared to a neutral effect when initiated distant from menopause with a 68% (p=0.05) lower CIMT progression among women postmenopausal within the past 5 years (n = 68) and a 46% lower CIMT progression in those aged ≤ 55 years (n = 82) versus placebo. A much larger proportion of women (almost half) in our study were ≤ 55 years of age and recently postmenopausal, which could explain the differences in our findings compared to this previous study.
In conclusion, we have shown that equol producers experience a greater reduction in BP, inflammatory markers and adhesion molecules on a soy diet compared to a TLC diet without soy than nonproducers of equol. Limitations of our study include the post-hoc analysis for equol production status and the small number of women with MetS. If these results can be confirmed in a trial in which subjects are randomized based on equol production status to either soy or no soy, we may be able to identify those who will benefit most from dietary soy for reduction of cardiovascular risk factors and prevention of cardiovascular disease. Dietary soy could be an effective and inexpensive strategy for reducing cardiovascular risk on a population basis in both men and women although the long-term safety of such an approach requires additional study.
Acknowledgments
We thank our research participants for their time and effort. Soy nuts were donated by Genisoy Food Company Inc. (Fairfield, CA).
Funding
This study was supported by the Harvard Medical School’s Center of Excellence in Women’s Health (National Institutes of Health), contract 00T002244 from the Office on Women’s Health, Department of Health and Human Services and supported in part by grant RR 01032 to the Beth Israel Deaconess Medical Center General Clinical Research Center from the National Institutes of Health.
Abbreviations
- CVD
Cardiovascular disease
- CHD
coronary heart disease
- MetS
metabolic syndrome
- TLC
therapeutic lifestyle changes
- BMI
body mass index
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
- Total-C
total cholesterol
- LDL-C
low-density lipoprotein cholesterol
- HDL-C
high-density lipoprotein cholesterol
- TG
triglycerides
- IL-6
interleukin-6
- MMP-9
matrix metalloproteinease 9
- apoB
apolipoprotein B-100
- sVCAM-1
vascular cell adhesion molecule-1
- sICAM-1
soluble intercellular adhesion molecule-1
- CRP
C-reactive protein
Footnotes
Clinical Trials Registration: NCT01740076
Disclosure Statement
There are no conflicts of interest with any of the authors.
Author Contributions
Dr. Welty conceived and designed the study. Dr Acharjee, Dr Zhou, Dr. Elajami and Dr Welty, all have contributed to the analysis and interpretation of data, drafting the article and revising it critically for important intellectual content. All authors have approved the final version of this manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Heart Association. Heart Disease and Stroke Statistics—2005 Update. Dallas, Tx: American Heart Association; 2005. [Google Scholar]
- 2.Mendelsohn ME, Karas RH. The protective effects of estrogen on the cardiovascular system. N Engl J Med. 1999;340:1801–11. doi: 10.1056/NEJM199906103402306. [DOI] [PubMed] [Google Scholar]
- 3.Welty FK. Alternative hormone replacement regimens: Is there a need for further clinical trials? Curr Opin Lipidol. 2003;14:585–91. doi: 10.1097/00041433-200312000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Ho S, Woo J, Leung S, Sham A, Lam T, Janus E. Intake of soy products is associated with better plasma lipid profiles in the Hong Kong Chinese population. J Nutr. 2000;130:2590–3. doi: 10.1093/jn/130.10.2590. [DOI] [PubMed] [Google Scholar]
- 5.Yang G, Shu XO, Jin R, Zhang X, Li HL, Li Q, Gao YT, Zheng W. Longitudinal study of soy food intake and blood pressure among middle-aged and elderly Chinese women. Am J Clin Nutr. 2005;81:1012–17. doi: 10.1093/ajcn/81.5.1012. [DOI] [PubMed] [Google Scholar]
- 6.Nagata C, Takatsuka N, Kurisu Y, Shimizu H. Decreased serum total cholesterol concentration is associated with high intake of soy products in Japanese men and women. J Nutr. 1998;128:209–13. doi: 10.1093/jn/128.2.209. [DOI] [PubMed] [Google Scholar]
- 7.Nagata C. Ecological study of the association between soy product intake and mortality from cancer and heart disease in Japan. Int J Epidemiol. 2000;29:832–6. doi: 10.1093/ije/29.5.832. [DOI] [PubMed] [Google Scholar]
- 8.Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–16. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 9.Wilson PW, Kannel WB, Silbershatz H, D’Agostino RB. Clustering of metabolic factors and coronary heart disease. Arch Intern Med. 1999;159:1104–9. doi: 10.1001/archinte.159.10.1104. [DOI] [PubMed] [Google Scholar]
- 10.Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2003;163:427–36. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schneider JG, Tompkins C, Blumenthal RS, Mora S. The metabolic syndrome in women. Cardiol Rev. 2006;14:286–91. doi: 10.1097/01.crd.0000233757.15181.67. [DOI] [PubMed] [Google Scholar]
- 12.Schnatz PF, Schnatz JD. Dyslipidemia in menopause: mechanisms and management. Obstet Gynecol Surv. 2006;61:608–13. doi: 10.1097/01.ogx.0000235502.95332.54. [DOI] [PubMed] [Google Scholar]
- 13.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 14.Welty FK, Lee KS, Lew NS, Zhou JR. Effect of soy nuts on blood pressure and lipid levels in hypertensive, prehypertensive, and normotensive postmenopausal women. Arch Intern Med. 2007;167:1060–7. doi: 10.1001/archinte.167.10.1060. [DOI] [PubMed] [Google Scholar]
- 15.Nasca MM, Zhou JR, Welty FK. Effect of Soy Nuts on Adhesion Molecules and Markers of Inflammation in Hypertensive and Normotensive Postmenopausal Women. Am J Cardiol. 2008;102:84–6. doi: 10.1016/j.amjcard.2008.02.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Setchell KD, Brown NM, Lydeking-Olsen E. The clinical importance of the metabolite equol-a clue to the effectiveness of soy and its isoflavones. J Nutr. 2002;132:3577–84. doi: 10.1093/jn/132.12.3577. [DOI] [PubMed] [Google Scholar]
- 17.Kang JS, Yoon YD, Han MH, Han SB, Lee K, Park SK, Kim HM. Equol inhibits nitric oxide production and inducible nitric oxide synthase gene expression through down-regulating the activation of Akt. Int Immunopharmacol. 2007;7:491–9. doi: 10.1016/j.intimp.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2003;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 19.Ridker PM, Buring JE, Cook NR, Rifai N. C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events. An 8-year follow-up of 14 719 initially healthy American women. Circulation. 2003;107:391–7. doi: 10.1161/01.cir.0000055014.62083.05. [DOI] [PubMed] [Google Scholar]
- 20.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 21.Liebson PR, Grandits G, Prineas R, Dianzumba S, Flack JM, Cutler JA, Grimm R, Stamler J. Echocardiographic correlates of left ventricular structure among 844 mildly hypertensive men and women in the Treatment of Mild Hypertension Study (TOMHS) Circulation. 1993;87:476–86. doi: 10.1161/01.cir.87.2.476. [DOI] [PubMed] [Google Scholar]
- 22.Gamache PH, Acworth IN. Analysis of phytoestrogens and polyphenols in plasma, tissue, and urine using HPLC with coulometric array detection. Proc Soc Exp Biol Med. 1998;217:274–80. doi: 10.3181/00379727-217-44232. [DOI] [PubMed] [Google Scholar]
- 23.Nurmi T, Adlercreutz H. Sensitive high-performance liquid chromatographic method for profiling phytoestrogens using coulometric electrode array detection: application to plasma analysis. Anal Biochem. 1999;274:110–7. doi: 10.1006/abio.1999.4247. [DOI] [PubMed] [Google Scholar]
- 24.Lampe JW, Karr SC, Hutchins AM, Slavin JL. Urinary equol excretion with a soy challenge: influence of habitual diet. Proc Soc Exp Biol Med. 1998;217:335–9. doi: 10.3181/00379727-217-44241. [DOI] [PubMed] [Google Scholar]
- 25.Rowland IR, Wiseman H, Sanders TA, Adlercreutz H, Bowey EA. Interindividual variation in metabolism of soy isoflavones and lignans: influence of habitual diet on equol production by the gut flora. Nutr Cancer. 2000;36:27–32. doi: 10.1207/S15327914NC3601_5. [DOI] [PubMed] [Google Scholar]
- 26.Ross R. Atherosclerosis-an inflammatory disease. N Engl J Med. 1999;340:115–26. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 27.Jackson RL, Greiwe JS, Schwen RJ. Emerging evidence of the health benefits of S-equol, an estrogen receptor β agonist. Nutrition Reviews. 2011;69(8):432–48. doi: 10.1111/j.1753-4887.2011.00400.x. [DOI] [PubMed] [Google Scholar]
- 28.Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342:836–43. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- 29.Mosca L, Manson JE, Sutherland SE, Langer RD, Manolio T, Barrett-Connor E. Cardiovascular disease in women: a statement for healthcare professionals from the American Heart Association. Circulation. 1997;96:2468–82. doi: 10.1161/01.cir.96.7.2468. [DOI] [PubMed] [Google Scholar]
- 30.Kitler ME. Differences in men and women in coronary artery disease, systemic hypertension and their treatment. Am J Cardiol. 1992;70:1077–80. doi: 10.1016/0002-9149(92)90364-5. [DOI] [PubMed] [Google Scholar]
- 31.Bass KM, Newschaffer CJ, Klag MJ, Bush TL. Plasma lipoprotein levels as predictors of cardiovascular death in women. Arch Intern Med. 1993;153:2209–16. [PubMed] [Google Scholar]
- 32.Hokanson JE, Austin MA. Plasma triglyceride level is a risk factor for cardiovascular disease independent of high-density lipoprotein cholesterol level: a meta-analysis of population-based prospective studies. J Cardiovasc Risk. 1996;3:213–9. [PubMed] [Google Scholar]
- 33.Cai Y, Guo K, Chen C, Wang P, Zhang B, Zhou Q, Mei F, Su Y. Soya isoflavone consumption in relation to carotid intima-media thickness in Chinese equol excretors aged 40–65 years. Br J Nutr. 2012;108(9):1698–704. doi: 10.1017/S0007114511007331. [DOI] [PubMed] [Google Scholar]
- 34.Clerici C, Setchell KD, Battezzati PM, Pirro M, Guiliano V, Asciutti S, Castellani D, Nardi E, Sabatino G, Orlandi S, Baldoni M, Morelli O. Pasta naturally enriched with isoflavone aglycons from soy germ reduces serum lipids and improves markers of cardiovascular risk. J Nutr. 2007;137:2270–8. doi: 10.1093/jn/137.10.2270. [DOI] [PubMed] [Google Scholar]
- 35.Kreijkamp-Kaspers S, Kok L, Bots ML, Grobbee DE, Lampe JW, van der Schouw YT. Randomized controlled trial of the effects of soy protein containing isoflavones on vascular function in postmenopausal women. Am J Clin Nutr. 2005;81:189–95. doi: 10.1093/ajcn/81.1.189. [DOI] [PubMed] [Google Scholar]
- 36.Hodis HN, Mack WJ, Kono N, Azen SP, Shoupe D, Hwang-Levine J, Petitti D, Whitfield-Maxwell L, Yan M, Franke AA, Selzer RH Women’s Isoflavone Soy Health Research Group. Isoflavone soy protein supplementation and atherosclerosis progression in healthy postmenopausal women: a randomized controlled trial. Stroke. 2011;42:3168–3175. doi: 10.1161/STROKEAHA.111.620831. [DOI] [PMC free article] [PubMed] [Google Scholar]