Abstract
Introduction:
The purpose of this study was to assess pharmacy students’ awareness, knowledge, and perceptions towards human immunodeficiency virus (HIV) pre-exposure prophylaxis (PrEP), confidence and intentions to counsel patients on PrEP, and preferred PrEP training.
Methods:
A web-based cross-sectional survey was conducted with pharmacy students. Descriptive statistics and multivariate logistic regressions were performed.
Results:
Ninety-one percent of participants were aware of PrEP and 61% were familiar with PrEP prescription guidelines. In multivariate analysis, greater PrEP knowledge, attitudes towards PrEP, and familiarity with prescribing guidelines were significantly associated with confidence in PrEP counseling (p < 0.01 for all). Males had significantly higher odds of reporting confidence in PrEP counseling relative to their female counterparts (p < 0.01). Relative to fourth year students, second year students were less likely to report confidence in PrEP counseling (p < 0.01). Participants who were familiar with prescribing guidelines had significantly higher odds of PrEP counseling intentions (p < 0.05). Preferred educational topics regarding PrEP included training on side effects and adherence monitoring (65% and 51%, respectively). The most preferred modalities for receiving PrEP education were online education (47%), educational seminars in required courses (43%), and self-study modules (39%).
Conclusions:
Given the key role played by pharmacists in patient engagement, they may be presented with opportunities to provide PrEP counseling and education. The development of educational modules for pharmacy students in an effort to increase PrEP uptake should consider addressing gaps in knowledge and preferred training modalities.
Keywords: Pharmacy students, Pre-exposure prophylaxis, HIV, Prevention
Introduction
More than 30 years into the epidemic, human immunodeficiency virus (HIV) infection persists as a significant public health problem. Currently, more than 1.1 million people are living with HIV in the United States (US) and nearly 38,500 new infections occur annually.1 In the past decade, the HIV prevention field has witnessed a distinct shift, with emphasis on biomedical strategies to supplement classic behavioral interventions, such as supporting condom use. The US National HIV/acquired immunodeficiency syndrome (AIDS) Strategy has established the important goal of decreasing HIV infections by 25% by the year 2020. One pivotal strategy to achieve this goal involves the use of oral pre-exposure prophylaxis (PrEP), co-formulated antiretroviral medications (300 mg of tenofovir disoproxil fumarate and 200 mg of emtricitabine as Truvada) taken by HIV-negative individuals to lower the risk of HIV infection. Prior studies have shown that PrEP is up to 92% effective for men who have sex with men,2 heterosexual women and men,3 and injection drug users who adhere to the treatment.4 Despite clinical practice guidelines supporting its safety and efficacy, as well as increased PrEP knowledge among healthcare providers since its approval in 2012 by the Food and Drug Administration (FDA), PrEP uptake has not kept pace with expectations.5,6 While the Centers for Disease Control and Prevention (CDC) estimate that approximately 1.2 million Americans meet eligibility criteria for PrEP, only 100,000 people take it.7,8 To guide educational strategies for healthcare professionals, investigation of provider knowledge and attitudes is needed to maximize the impact of PrEP on a population level.
Previous studies have examined attitudes towards PrEP adoption among pharmacists,9–11 physicians,12,13 nurse practitioners,14 physician assistants,15 or a combination of providers.16–19 However, few studies have been conducted among students in healthcare professional training programs, and those that have been done were limited to medical students.20,21 To date, no studies have explicitly examined pharmacy students’ awareness, knowledge, and attitudes towards PrEP. Given this lack of evidence, a better understanding of awareness and attitudes towards PrEP may inform the development of educational opportunities aimed at facilitating PrEP implementation among pharmacists.
Notably, pharmacists play a key role in community engagement and may be presented with opportunities to educate patients about PrEP. Included in the CDC’s release of PrEP clinical practice guidelines is the importance of counseling not only about adherence but also HIV risk reduction, such as encouraging condom use and HIV testing. This is a critical task that is often undertaken by pharmacists in a wide variety of settings.22 Despite these recommendations, a recent study on pharmacists’ knowledge and perceptions of PrEP found that nearly two-thirds were unaware of CDC guidelines and nearly three-fourths did not possess adequate knowledge to sufficiently counsel patients about PrEP.9 In another cross-sectional survey among community pharmacists, less than half of the sample could correctly identify Truvada as the medication used in PrEP and only 46% could correctly indicate the recommended HIV testing frequency for PrEP patients.10 Another study of pharmacists found general PrEP endorsement for high-risk individuals, despite low familiarity with PrEP.11 These findings are similar to those seen in a recent study of pharmacists, which noted that 40% had poor familiarity with PrEP and only 6% had experience with dispensing it.23 Taken together, these studies indicate gaps in pharmacists’ knowledge, awareness, and dispensing experience of PrEP despite its documented safety and effectiveness in preventing HIV infection.
In an effort to increase PrEP prescription via targeted interventions aimed at healthcare professionals, one possible theoretical framework to inform such interventions is the Information Motivation Behavioral Skills (IMB) Model.24 This model has been extensively applied to antiretroviral therapy (ART) adherence among people living with HIV as a model of health behavior adoption and was recently adapted as an explanatory framework for the assessment of core factors for PrEP use.25 The model incorporates behavior-specific information, motivations, and behavioral skills as foundational elements in understanding, predicting, and explaining health behaviors. Specifically, information about a particular behavior and attitudinal motivations towards that behavior contribute to the enhancement of skills that are pertinent to performing the given behavior. In the context of PrEP uptake among healthcare professionals, knowledge of and attitudes towards PrEP provide important precursory steps towards the development of a behavioral skill such as confidence or intentions to discuss PrEP with patients in the future.
If healthcare professionals across disciplines are to maximize the potential of PrEP, efforts must be made to increase knowledge and community engagement among those who are most poised to provide these preventive services. The study goal was to explore five research questions: 1) How aware, familiar, and knowledgeable are pharmacy students about the CDC’s clinical practice guidelines for PrEP?; 2) What are their attitudes towards PrEP?; 3) What are their preferred training topics and modalities on PrEP?; 4) What are their a) confidence and b) intentions in counseling patients about PrEP?; and 5) Consistent with the IMB model, are information (knowledge about PrEP) and motivation (attitudes towards PrEP) associated with behavioral skills (confidence and intentions to counsel patients about PrEP) in the future? We believe the answers to these questions will help determine gaps that may be addressed in future educational initiatives among students in pharmacy training programs.
Methods
Procedures
Students enrolled in a doctor of pharmacy (PharmD) academic training program at the University at Buffalo were eligible for the study that aimed to examine awareness, knowledge, and attitudes towards PrEP. Between October and November 2017, potential participants received an e-mail inviting them to participate in a web-based, cross-sectional survey sent to their university-affiliated e-mail address. E-mails contained a cover letter explaining the study purpose and procedures. Those who indicated they were willing to participate in the study continued by answering the survey questions. Non-responders were sent weekly reminders to complete the survey with a maximum of three reminder emails. Participants received a $10 electronic Amazon gift card. The study protocol was approved by the university’s institutional review board.
Measures
Following a thorough literature review, we developed a survey instrument that was pilot-tested among a group of healthcare professionals (four physicians, two pharmacists, and two nurse practitioners) who suggested minimal changes to clarify questions and response options. PrEP awareness was measured with a single item that asked, “Prior to this survey, were you aware of the concept of HIV PrEP, which is prescribing regularly-scheduled oral HIV medications to HIV-uninfected individuals to help prevent them from getting HIV?” Familiarity with PrEP prescription was assessed with one item that asked, “Please rate how familiar or unfamiliar you consider yourself with regard to prescribing PrEP” on a five-point scale ranging from “very unfamiliar” to “very familiar”. The two most positive responses (very familiar and somewhat familiar) were used to designate familiarity with PrEP. PrEP knowledge was measured with five multiple choice items based on the CDC’s PrEP guidelines with responses scored as correct1 or incorrect (0). These items included knowledge of PrEP dosing frequency (i.e. daily), FDA-approved medications (i.e. a coformulated tablet containing both emtricitabine and tenofovir disoproxil fumarate, also known as Truvada), knowledge of HIV antibody testing prior to PrEP initiation (i.e. yes), knowledge of HIV testing frequency while on PrEP (i.e. every three months), and knowledge of a contraindication to prescribing PrEP (i.e. reduced creatinine clearance).
Attitudes towards PrEP measured participants’ level of agreement with eight items.26 Participants rated their responses on a five-point scale ranging from “strongly disagree” to “strongly agree” with higher scores indicating more positive attitudes. Future PrEP training needs were assessed with two items that inquired about preferred training modality and specific knowledge needed to better prepare them to counsel patients about PrEP. Confidence in PrEP counseling was measured with one item that stated, “I am confident that I could counsel patients on PrEP” on a five-point scale ranging from “strongly disagree” to “strongly agree.” The two most positive responses (strongly agree and agree) were used to designate confidence in PrEP counseling. PrEP counseling intentions were measured with one item that stated, “I intend to counsel patients about PrEP” on a five-point scale ranging from “strongly disagree” to “strongly agree.” The two most positive responses (strongly agree and agree) were used to designate intentions to counsel patients about PrEP.
Data Analyses
Using STATA version 14.2,27 descriptive statistics were used to describe the data collected in the survey. Logistic regression models were used to assess whether demographic variables, PrEP knowledge, familiarity with prescribing guidelines, and attitudes towards PrEP were associated with a) confidence and b) intentions to counsel patients on PrEP. In bivariate analyses, those variables with a p-value of < 0.2 were subsequently entered into multivariate logistic regression models to assess relationships between independent variables and the primary outcomes of interest.
Results
The survey response rate was 52% (291/557). Table 1 presents participants’ demographic characteristics. Overall, 64% of participants were female with a mean age of 23.1 years (standard deviation (SD) = 2.59). In terms of race, 57% identified as white. The majority indicated their preferred future workplace setting to be either a hospital (36%) or community pharmacy (32%).
Table 1.
Participant characteristics (n = 291).
| Characteristics | n (%)a |
|---|---|
| Age [mean (SD)] | 23.1 (2.59) |
| Sex | |
| Female | 186 (63.7) |
| Male | 105 (36.3) |
| Class year | |
| First | 70 (23.9) |
| Second | 67 (22.9) |
| Third | 67 (22.9) |
| Fourth or higher | 85 (30.3) |
| Race | |
| White | 167 (57.2) |
| Asian | 101 (34.6) |
| Otherb | 12 (4.1) |
| African American | 11 (3.8) |
| Intended future workplace setting | |
| Hospital | 93 (35.9) |
| Community pharmacy | 84 (32.4) |
| Pharmaceutical industry | 24 (9.3) |
| Private practice | 11 (4.3) |
| Community health center | 10 (3.9) |
| Academia | 9 (3.5) |
| Consultant | 9 (3.5) |
| Otherc | 19 (7.2) |
SD = standard deviation.
Percentages based on number of respondents in each category; numbers may not total to 100% due to missing data.
Other includes American Indian, Alaska Native, Native Hawaiian or Pacific Islander, and other race.
Other includes administration, nuclear pharmacy, managed care, compounding pharmacy, retail pharmacy, insurance industry.
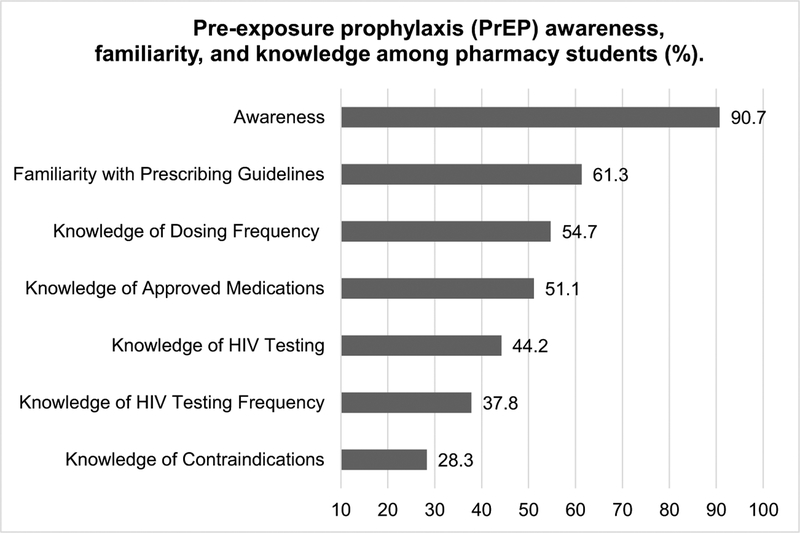
As illustrated in Fig. 1, overall PrEP awareness was high (91%). However, while reported familiarity with PrEP prescription guidelines was relatively high (61%), this did not translate into correct knowledge of PrEP. Specifically, while more than half correctly knew the daily dosing frequency and approved medication for PrEP (55% and 51%, respectively), only 44.2% knew that HIV testing was required prior to a PrEP prescription. Furthermore, slightly more than one-third knew the recommended HIV testing frequency for patients taking PrEP (38%) and slightly more than one-quarter knew that reduced creatinine clearance (< 50 mL/min) was a contraindication to prescribing PrEP (28%).
Fig. 1.
Pre-exposure prophylaxis (PrEP) awareness, familiarity, and knowledge among pharmacy students (%). HIV = human immunodeficiency virus.
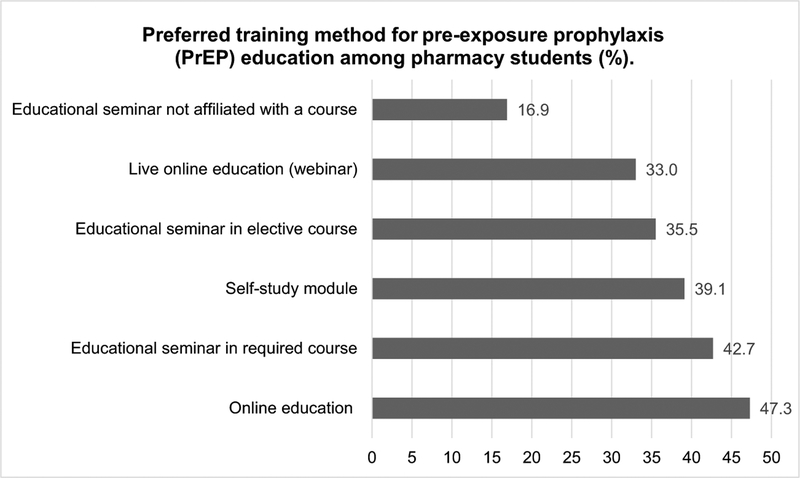
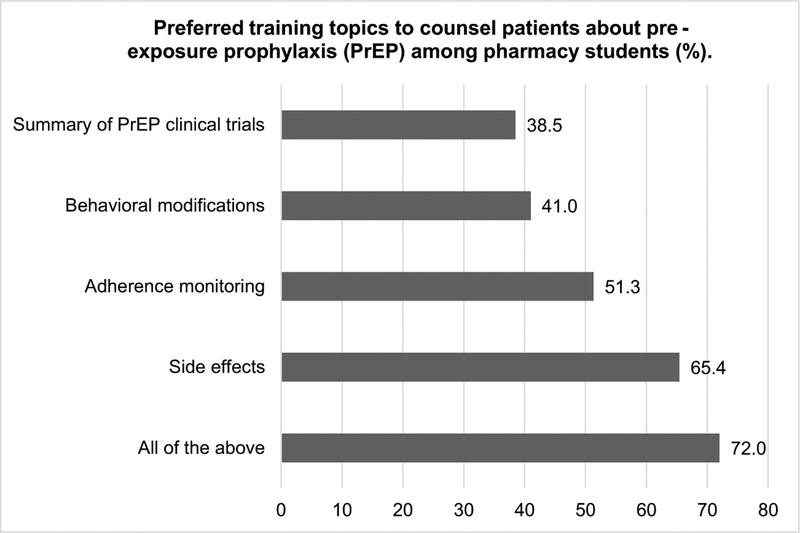
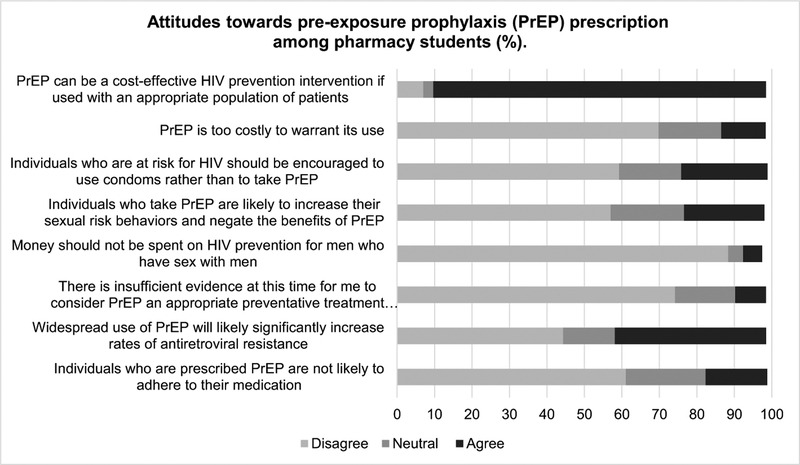
Overall, pharmacy students had generally favorable attitudes towards PrEP (Fig. 2). For example, 89% agreed that PrEP can be cost-effective to prevent HIV infection if utilized by eligible patients. Only 12% agreed that PrEP is too expensive to justify its use. Few participants agreed with the statement that individuals would be non-adherent to PrEP (16%). However, 40% believed that widespread PrEP use would considerably raise antiretroviral resistance rates. In addition, nearly one-quarter of the sample believed that sexual risk behaviors would increase among PrEP users. Fig. 3 illustrates participants’ preferences for future educational training on PrEP. Respondents indicated that in order to be better trained to counsel patients about PrEP, specific training topics would be needed. Specifically, more than half of the sample wanted training on side effects and adherence monitoring (65% and 51%, respectively) with lower percentages indicating preferences for training on behavioral modifications or a summary of PrEP clinical trials. In addition, the most preferred modalities for receiving PrEP education were online education (47%), educational seminars in required courses (42%), and self-study modules (39%) (Fig. 4).
Fig. 2.
Preferred training method for pre-exposure prophylaxis (PrEP) education among pharmacy students (%).
Fig. 3.
Preferred training topics to counsel patients about pre-exposure prophylaxis (PrEP) among pharmacy students (%).
Fig. 4.
Attitudes towards pre-exposure prophylaxis (PrEP) prescription among pharmacy students (%). HIV = human immunodeficiency virus.
Regarding confidence in and intentions to engage in PrEP counseling, 64% of participants felt confident that they could counsel patients about PrEP while 87% reported that they intended to counsel patients about PrEP. As illustrated in Table 2, greater PrEP knowledge, attitudes towards PrEP, and familiarity with prescribing guidelines emerged as significant correlates of confidence in counseling about PrEP [adjusted odds ratio (AOR) 1.61, (95% CI 1.29, 2.02), p < 0.01; AOR 1.06, (95% CI 1.01, 1.12), p < 0.05; AOR 2.51, (95% CI 1.28, 4.92), p < 0.01, respectively]. Males had significantly higher odds of reporting confidence in PrEP counseling relative to their female counterparts [AOR 2.70, (95% CI 1.38, 5.26), p < 0.01]. Relative to fourth year students, second year students were less likely to report confidence in PrEP counseling (AOR 0.26, (95%CI 0.11, 0.61), p < 0.01]. In addition, those who were familiar with prescribing guidelines had significantly higher odds of PrEP counseling intentions [AOR 2.82, (95% CI 1.16, 6.87), p < 0.05].
Table 2.
Factors associated with confidence in pre-exposure prophylaxis (PrEP) counseling and intentions to counsel on PrEP among pharmacy students (n = 260).
| Confidence in PrEP counseling aOR (95% CI) | PrEP counseling intentions aOR (95% CI) | |
|---|---|---|
| PrEP knowledge | 1.61 (1.29, 2.02)c | 1.07 (0.79, 1.44) |
| Attitudes towards PrEP | 1.06 (1.01–1.12)b | 1.05 (0.99–1.12)a |
| Familiarity with PrEP guidelines | 2.51 (1.28, 4.92)c | 2.82 (1.16, 6.87)b |
| Age (years) | 0.96 (0.84, 1.10) | 1.33 (0.98, 1.79) |
| First year | 0.89 (0.34, 2.26) | 2.05 (0.55, 7.59) |
| Second year | 0.26 (0.11,0.61)c | 2.47 (0.63, 9.75) |
| Third year | 0.67 (0.26, 1.68) | 0.58 (0.19, 1.77) |
| Fourth year | Ref | Ref |
| Male | 2.70 (1.38, 5.26)c | 0.67 (0.30, 1.47) |
aOR = adjusted odds ratio; CI = confidence interval; Ref = reference.
p < 0.10.
p < 0.05.
p < 0.01.
Discussion
Given the absence of research about pharmacy students’ knowledge on PrEP, the primary purpose of this study was to assess their knowledge and awareness of PrEP, familiarity with prescribing guidelines, their attitudes towards it, and their intentions and confidence in counseling patients on PrEP in the future. Results from this study demonstrate that pharmacy students were highly aware of PrEP and reported relatively high familiarity with prescribing guidelines. The high level of awareness is consistent with previous studies of HIV specialists and primary care providers12,16,17,28,29 yet higher than in other studies of pharmacists23 and medical providers.19,30 A key finding in the analysis pertains to the connection between reported familiarity with PrEP prescribing guidelines and knowledge. While the majority indicated being familiar with PrEP prescribing guidelines, this did not translate to correct responses on the knowledge items. In particular, slightly more than half could correctly identify PrEP dosing frequency and the FDA-approved medication, while less than half correctly identified the recommended HIV testing frequency, the necessity of HIV antibody testing prior to PrEP prescription, and contraindications to prescribing PrEP. These results are similar to previous findings of community pharmacists which noted relatively low knowledge of the CDC’s PrEP guidelines.10 Our results indicate that educational efforts are needed not only to increase PrEP awareness, but also to improve knowledge of prescription guidelines which can have a positive impact on broad patient education practices and PrEP dispensing.
Pharmacists can play a meaningful role in PrEP access, uptake, and adherence. Consequently, it is critical to understand pharmacy students’ attitudes towards its use. In our study, 40% of respondents erroneously believed that widespread use of PrEP could significantly increase rates of antiretroviral resistance, which is higher than found in previous studies of healthcare providers.29,31 This finding is critical as it may not be common knowledge among healthcare professional students in academic training programs and may inadvertently lead healthcare professionals to support the notion that the potential risk of antiretroviral resistance overshadows the public health benefits of reducing new infections. The CDC’s release of PrEP clinical practice guidelines provides detailed evidence from several randomized clinical trials demonstrating that drug-resistant mutations were rare. Consistent with prior studies of pharmacists23 and healthcare providers12,29 nearly 25% of respondents believed that PrEP users are likely to engage in sexual risk behaviors. However, a recent systematic review reported no conclusive evidence to support the notion that PrEP use leads to increased sexual risk behaviors.32 A promising finding is that most respondents believed that PrEP is a cost-effective intervention for preventing HIV and few held the attitude that PrEP is too expensive to justify its use. This finding is inconsistent with results from a 2013 study of pharmacists that found that 92% of respondents believed that PrEP is too costly to promote access to patients.9 It is possible that the five-year difference in data collection between these two studies resulted in the divergent findings. When PrEP gained FDA approval, cost was considered a significant potential barrier to its use. However, PrEP is currently covered by virtually every health insurance program and is also available through manufacturer medication assistance programs and state-sponsored programs. For example, a PrEP assistance program is offered through the New York State Department of Health to reimburse providers for the costs associated with providing healthcare and laboratory services (such as testing for sexually transmitted infections) to both uninsured and under-insured PrEP patients.
The education of pharmacy students as part of their academic training has important implications for their preparation in counseling patients about obtaining a PrEP prescription and understanding of potential side effects. They also play an important role in adherence monitoring and the management of clinically significant drug interactions. In a concerted, collaborative effort to increase PrEP uptake, training considerations for future pharmacists are of critical importance as they aid their patients in making choices about PrEP initiation and adherence. Our findings indicate that pharmacy students have a broader preference for online education, seminars in required courses, and self-study modules as the ideal means to gain greater knowledge about PrEP. These suggestions could be taken into consideration when instructors are developing foundational coursework including but not limited to infectious disease courses. For example, pathophysiology courses could include general HIV content such as screening guidelines and testing protocols as well as specific prevention methods including PrEP. In addition, the infectious disease section of a pharmacotherapeutics course could include coverage of medications to treat HIV infection as well as the use of PrEP for HIV prevention. Course content could also include strategies to counsel patients on appropriate use of these medications, management of adverse events, and drug-drug interactions. Furthermore, providing resources for online tutorials on PrEP would be a valuable training resource for students who are interested in continuing education efforts.
In regression models, males had significantly higher odds of reporting confidence in PrEP counseling relative to females. While this finding may be surprising, it is in harmony with previous studies of medical students that found females are less likely to report confidence in their clinical decision-making abilities.33,34 Results also demonstrated that participants with greater PrEP knowledge and more positive attitudes had higher odds of reporting confidence in counseling about PrEP in line with the IMB model. In addition, participants who were familiar with prescribing guidelines had higher odds of both confidence and intentions to engage in PrEP counseling. These findings bring notable attention to the importance of increasing knowledge of PrEP prescribing guidelines. In fact, recent studies among healthcare providers found that greater knowledge of the CDC guidelines is associated not only with actual PrEP prescription but also greater willingness and intentions to prescribe it in the future for adults12,29 and adolescents.35 Though class year was not significant in the PrEP counseling intentions model, it emerged in the PrEP counseling confidence model where second year students had lower odds of confidence relative to their fourth year counterparts. This finding may have been influenced by factors which were not measured in our study, such as specific coursework taken in a particular semester that may have impacted PrEP counseling confidence.
Given the demonstrated effectiveness of clinical pharmacists in improving medication adherence among people living with HIV, pharmacists can be vital team players to aid in PrEP adherence counseling and monitoring.36 One recent key change in the CDC’s approach to HIV prevention, treatment, and care is the use of an HIV Care Continuum.37 This framework provides a multi-step approach with goals to increase HIV diagnosis rates so people are aware of their infection, to facilitate prompt linkage to a healthcare provider within one month of HIV diagnosis, to improve retention in medical care over time, and to achieve viral suppression goals to keep HIV at very low levels in the blood. Analogous to the HIV Care Continuum is the PrEP cascade, the idea that there are stages in which individuals pass through to help them be aware of PrEP and ultimately prepare to initiate the medication and adhere to it over time.5,38 Pharmacists can be part of an interdisciplinary team of healthcare professionals that aid PrEP patients at multiple levels of the cascade. First, pharmacists may be approached by patients who are seeking answers to general PrEP questions (i.e. safety, efficacy, tolerability) as they often are for other medications. They can assist by providing basic knowledge about the purpose of PrEP as a biomedical preventive tool and serve as a point of referral for patients looking to obtain PrEP from local prescribers. Second, for those patients who are intending to initiate PrEP, pharmacists can aid in assisting their decision-making by reviewing the importance of medication adherence. For example, they can educate patients, particularly those who have limited experience taking daily medications, about tools or strategies to increase adherence such as pill boxes or text reminders. Third, for PrEP users, pharmacists can reiterate the importance of adherence and provide supportive counseling on the prevention and management of drug-drug interactions as well as adverse events.
Limitations
The study included pharmacy students at one university in one state, which may not be representative of all pharmacy students across the country and limits the external validity of our findings. Future studies would benefit from multi-institution data collection methods to determine the extent to which our study findings can be replicated among pharmacy students in other academic training programs in different geographic areas. As the sample was comprised exclusively of students, we were unable to assess their actual PrEP counseling behaviors and therefore used confidence and intentions to counsel patients about PrEP as an indicator of future behaviors. While achieving a response rate of > 50% is noteworthy for an online survey, there is a potential for non-response bias. We cannot determine if non-responders viewed the e-mail invitation but chose not to respond or never opened the e-mail. That said, the response rate is higher than previous online PrEP surveys conducted with community pharmacists,10 medical students,21 and primary care providers.16
Conclusions
Given the substantial burden of HIV incidence and prevalence and the underutilization of PrEP, this research study has significance because it directly addresses factors affecting PrEP uptake from the perspective of pharmacy students as key stakeholders in PrEP engagement. Findings suggest that students are generally aware of the concept of PrEP but lack knowledge about prescribing guidelines. Important opportunities exist for pharmacists to address HIV prevention during patient encounters. These discussions can include counseling and education about PrEP and the importance of adherence as well as its safety and efficacy in the prevention of HIV infection. In addition, pharmacists are well-situated to link patients with providers who offer PrEP, navigate insurance concerns or patient assistance programs, and educate about adverse drug events or drug interactions when dispensing the medication. Future studies may consider educational strategies to enhance the position of pharmacists in the education and promotion of PrEP as a biomedical tool to prevent HIV infection.
Acknowledgment
Funding for this research was supported in part by the University of Rochester Center for AIDS Research grant P30AI078498 (NIH/NIAID) and the University of Rochester School of Medicine and Dentistry through a grant awarded to Sarahmona Przybyla (UB) and Diane Morse (UR).
Footnotes
Conflict of Interest
None.
Disclosures
None.
Appendix A. Supplementary Data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cptl.2019.01.011.
References
- 1.Centers for Disease Control and Prevention. Estimated HIV incidence and prevalence in the United States, 2010–2015. HIV Surveillance Supplemental Report. Published March 2018; Published March 2018 Number 1 https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-supplemental-report-vol-23-1.pdf, Accessed date: 17 February 2019. [Google Scholar]
- 2.Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baeten JM, Donnell D, Ndase P, et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choopanya K, Martin M, Suntharasamai P, et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–2090. [DOI] [PubMed] [Google Scholar]
- 5.Parsons JT, Rendina HJ, Lassiter JM, Whitfield TH, Starks TJ, Grov C. Uptake of HIV pre-exposure prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States. J Acquir Immune Defic Syndr. 2017;74(3):285–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu H, Mendoza MC, Huang YA, Hayes T, Smith DK, Hoover KW. Uptake of HIV preexposure prophylaxis among commercially insured persons-United States, 2010–2014. Clin Infect Dis. 2017;64(2):144–149. [DOI] [PubMed] [Google Scholar]
- 7.Mera Giler R, Magnusen D, Trevor H, Bush S, Rawlings S, McCallister S. Changes in Truvada (TVD) for HIV pre-exposure prophylaxis utilization in the USA: (2012–2016) Paper Presented at the 9th International AIDS Society Conference on HIV Science. July 23–26, 2017; July 23–26, 2017. Paris, France. [Google Scholar]
- 8.Smith DK, Van Handel M, Wolitski RJ, et al. Vital signs: estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition—United States, 2015. MMWR Morb Mortal Wkly Rep. 2015;64(46):1291–1295. [DOI] [PubMed] [Google Scholar]
- 9.Shaeer KM, Sherman EM, Shafiq S, Hardigan P. Exploratory survey of Florida pharmacists’ experience, knowledge, and perception of HIV pre-exposure prophylaxis. J Am Pharm Assoc (2003). 2014;54(6):610–617. [DOI] [PubMed] [Google Scholar]
- 10.Unni EJ, Lian N, Kuykendall W. Understanding community pharmacist perceptions and knowledge about HIV preexposure prophylaxis (PrEP) therapy in a Mountain West state. J Am Pharm Assoc. 2016;56(5):527–532.e1. [DOI] [PubMed] [Google Scholar]
- 11.Yoong D, Naccarato M, Sharma M, Wilton J, Senn H, Tan DH. Preparing for pre-exposure prophylaxis: perceptions and readiness of Canadian pharmacists for the implementation of HIV pre-exposure prophylaxis. Int J STD AIDS. 2016;27(8):608–616. [DOI] [PubMed] [Google Scholar]
- 12.Blumenthal J, Jain S, Krakower D, et al. Knowledge is power! Increased provider knowledge scores regarding pre-exposure prophylaxis (PrEP) are associated with higher rates of PrEP prescription and future intent to prescribe PrEP. AIDS Behav. 2015;19(5):802–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edelman EJ, Moore BA, Calabrese SK, et al. Primary care physicians’ willingness to prescribe HIV pre-exposure prophylaxis for people who inject drugs verus other risk groups. AIDS Behav. 2017;21(4):1025–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith DK, Mendoza MC, Stryker JE, Rose CE. PrEP awareness and attitudes in a national survey of primary care clinicians in the United States, 2009–2015. PLoS One. 2016;11(6) 10.1371/journal.pone.0156592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adams LM, Balderson BH, Brown K, Bush SE, Packett 2nd BJ. Who starts the conversation and who receives preexposure prophylaxis (PrEP)? A brief online survey of medical providers’ PrEP practices. Health Educ Behav. 2018;45(5):723–729. [DOI] [PubMed] [Google Scholar]
- 16.Blackstock OJ, Moore BA, Berkenblit GV, et al. A cross-sectional online survey of HIV pre-exposure prophylaxis adoption among primary care physicians. J Gen Intern Med. 2017;32(1):62–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petroll AE, Walsh JL, Owczarzak JL, McAuliffe TL, Bogart LM, Kelly JA. PrEP awareness, familiarity, comfort, and prescribing experience among US primary care providers and HIV specialists. AIDS Behav. 2017;21(5):1256–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weiser J, Garg S, Beer L, Skarbinski J. Prescribing of human immunodeficiency virus (HIV) pre-exposure prophylaxis by HIV medical providers in the United States, 2013–2014. Open Forum Infect Dis. 2017;4(1) 10.1093/ofid/ofx003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wood BR, McMahan VM, Naismith K, Stockton JB, Delaney LA, Stekler JD. Knowledge, practices, and barriers to HIV preexposure prophylaxis prescribing among Washington state medical providers. Sex Transm Dis. 2018;45(7):452–458. [DOI] [PubMed] [Google Scholar]
- 20.Calabrese SK, Earnshaw VA, Krakower DS, et al. A closer look at racism and heterosexism in medical students’ clinical decision-making related to HIV pre-exposure prophylaxis (PrEP): implications for PrEP education. AIDS Behav. 2018;22(4):1122–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Calabrese SK, Earnshaw VA, Underhill K, Hansen NB, Dovidio JF. The impact of patient race on clinical decisions related to prescribing HIV pre-exposure prophylaxis (PrEP): assumptions about sexual risk compensation and implications for access. AIDS Behav. 2014;18(2):226–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention, US Public Health Service. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 update: a clinical practice guideline. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf; Published March 2018, Accessed date: 17 February 2019.
- 23.Sánchez-Rubio Ferrandez J, Martinez Sesmero JM, Navarro Aznárez H, Fernández Espinola S, Escobar Rodriguez I, Ventura Cerdá JM. Perceptions about HIV pre-exposure prophylaxis among healthcare professionals in Spain (PERPPRES Study). Farm Hosp. 2016;40(4):287–301. [DOI] [PubMed] [Google Scholar]
- 24.Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006;25(4):462–473. [DOI] [PubMed] [Google Scholar]
- 25.Dubov A, Altice FL, Fraenkel L. An information-motivation-behavioral skills model of PrEP uptake. AIDS Behav. 2018. 10.1007/s10461-018-2095-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walsh JL, Petroll AE. Factors related to pre-exposure prophylaxis prescription by U.S. primary care physicians. Am J Prev Med. 2017;52(6):e165–e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.STATA for Windows [Computer Program]. Version 14.2. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 28.Bacon O, Gonzalez R, Andrew E, et al. Brief report: informing strategies to build PrEP capacity among San Francisco Bay area clinicians. J Acquir Immune Defic Syndr. 2017;74(2):175–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krakower DS, Mayer KH. Pre-exposure prophylaxis to prevent HIV infection: current status, future opportunities and challenges. Drugs. 2015;75(3):243–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ross I, Mejia C, Melendez J, et al. Awareness and attitudes of pre-exposure prophylaxis for HIV prevention among physicians in Guatemala: implications for country-wide implementation. PLoS One. 2017;12(3) 10.1371/journal.pone.0173057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Desai M, Gafos M, Dolling D, McCormack S, Nardone A. PROUD study. Healthcare providers’ knowledge of, attitudes to and practice of pre-exposure prophylaxis for HIV infection. HIV Med. 2016;17(2):133–142. [DOI] [PubMed] [Google Scholar]
- 32.Freeborn K, Portillo CJ. Does pre-exposure prophylaxis for HIV prevention in men who have sex with men change risk behavior? A systematic review. J Clin Nurs. 2018;27(17–18):3254–3265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Blanch DC, Hall JA, Roter DL, Frankel RM. Medical student gender and issues of confidence. Patient Educ Couns. 2008;72(3):374–381. [DOI] [PubMed] [Google Scholar]
- 34.Theobald J, Gaglani S, Haynes MR. The association between confidence and accuracy among users of a mobile web platform for medical education. Ann Intern Med. 2015;162(5):395–396. [DOI] [PubMed] [Google Scholar]
- 35.Mullins TLK, Zimet G, Lally M, Xu J, Thornton S, Kahn JA. HIV care providers’ intentions to prescribe and actual prescription of pre-exposure prophylaxis to at-risk adolescents and adults. AIDS Patient Care STDS. 2017;31(12) 10.1089/apc.2017.0147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bruno C, Saberi P. Pharmacists as providers of HIV pre-exposure prophylaxis. Int J Clin Pharm. 2012;34(6):803–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hojilla JC, Vlahov D, Crouch PC, Dawson-Rose C, Freeborn K, Carrico A. HIV pre-exposure prophylaxis (PrEP) uptake and retention among men who have sex with men in a community-based sexual health clinic. AIDS Behav. 2018;22(4):1096–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]