Abstract
For individuals living with HIV, disclosure of HIV status to their partners can be a source of psychological and emotional stress. Minimal information about serostatus disclosure is available for young men who have sex with men (YMSM). This study examined the disclosure of HIV status to social and sexual partners among YMSM using social and sexual network data. Respondent-driven sampling was used to collect data from YMSM aged 16-29 in Houston, Texas and Chicago, Illinois. Social network data from 746 respondents and 2035 social and/or sexual partners were collected from 2014 to 2016, of whom 27.9% were HIV seropositive, with 9.4% of their partners being both sexually and socially connected to respondents (overlapping network status), and 90.6% either sexually or socially connected. Generalized estimating equation analysis was conducted based on respondents’ knowledge of their sexual partners’ HIV status. Results showed that respondents with overlapping sexual and social relationships with their partners were less likely to not know their partners’ HIV status (AOR=0.26 95% CI: 0.18-0.40). Results highlight the association between overlapping partnership and knowledge of partner’s HIV status among YMSM. These findings are useful when selecting potential network members to disclose HIV status and support YMSM’s health and well-being.
Keywords: HIV, MSM, social network
Introduction
Disclosing one’s HIV status concerns not only the person living with HIV but also involves partners to whom the information may be disclosed in the sexual decision-making process. Besides other factors that facilitate HIV disclosure, it is important to consider the relationship between the person living with HIV and those to whom they may disclose their status to achieve a successful HIV disclosure. Since social and sexual networks often overlap with each other among men who have sex with men (MSM) (Bohl, Raymond, Arnold, & McFarland, 2009), it is necessary to consider this overlapped network context of social and sexual relationships in relation to knowledge/perception of partners’ HIV status.
Social network perspective addresses the issue of how individuals, organizations, or groups interact with others within the network to which they belong. Social network perspective suggests that three main factors determine individuals’ health or other behavioral outcomes: 1) network environment, 2) position in network, and 3) structural and network properties (Valente, 2015).
In the research among MSM, social network perspective was used to examine HIV disclosure in terms of both patients’ demographic characteristics and their relationships with partners, families, and friends. It has been reported that the rates of disclosure to different members of the social network differ among HIV-positive Latino gay men. (Zea, Reisen, Poppen, Echeverry, & Bianchi, 2004). More specifically, whether the disclosure targets’ awareness of an individuals’ sexual orientation was associated with patients’ disclosure to mothers, fathers, and close friends (Zea et al., 2004). Among African-American HIV-positive MSM, those who were younger and had a higher level of education were more likely to disclose their positive HIV status. In addition, they tended to disclose to older and HIV-positive individuals(Latkin et al., 2012). In a study focusing on disclosure to family members of youth living with HIV, aged 12-24, there was no association between family knowledge of their HIV status and their social support, or family socioeconomic status (Lee, Yamazaki, Harris, Harper, & Ellen, 2015).
Although the aforementioned studies provide a foundation for our current research, one limitation is that each study involved only a specific race/ethnicity. Thus, it is necessary to evaluate disclosure status across different racial/ethnic groups in order to identify the effect of race/ethnicity on HIV disclosure. One study provided addressed racial/ethnic diversity among young MSM (YMSM) by providing descriptive data in Chicago; however, they are limited in reporting HIV disclosure (Birkett, Kuhns, Latkin, Muth, & Mustanski, 2015).
To address the knowledge gap described above, we used the dataset collected by the “YMAP: Young Men’s Affiliation Project of HIV risk and prevention venue”. As the YMAP survey asks respondents whether they know their network members’ HIV status, there is a possibility that the respondent’s knowledge of the HIV status of his social or sexual network members may not be due to client level disclosure but could have originated from other network members.
Our study relied on the social network perspective and focused on network concepts of homophily and overlapping ties (multiplexity) between the respondents and their network members to examine their impact of homophily and overlapping ties on acquiring knowledge of partners’ HIV status.
Homophily refers to the principle that contact is more likely to occur among similar, rather than dissimilar, individuals (McPherson, Smith-Lovin, & Cook, 2001). “Overlapping relationships” means that individuals are connected through more than one type of relationship. Overlapping relationships may, in turn, foster greater behavioral similarity (Krohn, 1986; Krohn, Massey, & Zielinski, 1988).
The objective of this study was to examine the relative importance of network factors, i.e., homophily in terms of demographic and other characteristics, and overlapping relationships in determining HIV disclosure among HIV-positive YMSM in Chicago and Houston. In addition, we analyzed data from HIV-positive YMSM in Chicago and Houston in preparation for presenting descriptive information about sexual networks.
Our hypotheses were as follows: H1) the greater the homophily/similarity between HIV patients and disclosure targets with respect to race and age, the greater the likelihood that targets will be informed of their partner’s HIV status; and H2) the rate of disclosure will be higher in overlapping sexual and social relationships than in non-overlapping ones, which implies that overlapping moderates the effect of homophily in H1 (Figure 1).
Figure 1:
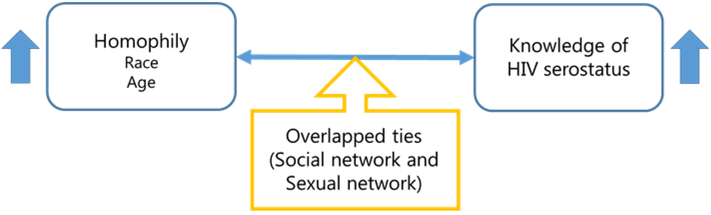
Conceptual framework of this study
Methods
Study design and setting
The YMAP is a prospective cohort study from 2014 to 2017 that evaluates risk and protective behaviors regarding HIV and sexually transmitted infections (STIs), and venue-based affiliation, social, and sexual networks of YMSM in both Chicago, IL and Houston, TX. This study used cross-sectional data collected from December 2014 to June 2016. Recruitment of respondents and data collection took place at the University of Chicago, Ann & Robert H. Lurie Children’s Hospital of Chicago, and the University of Texas Health Science Center at Houston. These three sites that participated in YMAP received approval from their respective institutional review boards.
Study participants and data collection
The criteria for selecting the respondents in this study were being MSM, between the ages of 16 and 29 years, and residing in Chicago or Houston. MSM was defined as a person: 1) assigned male sex at birth and self-identifying as male, and 2) reporting oral or anal sex with another male within the past year. The YMAP sample was drawn using the respondent-driven sampling (RDS) method (Heckathorn, 2011). Initial “seeds” were identified, recruited and enrolled via representatives at healthcare and other venues frequented by YMSM, such as clinics, and community-based organizations or social venues, such as bars and sports groups. Seeds could only refer up to four sprouts and were provided $20 for each sprout respondent. We collected biological data such as HIV status via standard HIV testing protocols at each site and employed computer-based personal interviewing using Qualtrics (Qualtrics LLC, Provo, Utah).A more detailed description of data collection procedures and survey items are available elsewhere (Fujimoto, Cao, Kuhns, Li, & Schneider, 2018; Fujimoto, Flash, Kuhns, Kim, & Schneider, 2018).
Measures
Dependent variable: Knowledge of partner’s HIV status
Network members were identified by respondents listing the names of individuals they considered to be a part of their close social network. Subsequently, respondents were asked to list sexual partners over the last 6 months. Lastly, respondents checked whether the names they listed appeared in both lists. If the name was duplicated, this individual was recognized as a duplicate network member: that is, a socially and sexually connected member.
We assessed respondents’ HIV status using a site-specific algorithm that detailed in elsewhere (Fujimoto, Flash, et al., 2018). Those with reactive samples were confirmed by using HIV-1/HIV-2 multispot differentiation and HIV RNA (viral load) tests, then referred to a clinic for care. To assess respondents’ knowledge of network members’ HIV status, we asked the question, “Is/Was your network member HIV-positive or negative?” Respondents chose one of the following answers: positive, negative, or unknown.
Independent variable: Network measures
In order to collect social network data, social ties were identified by having respondents nominate up to five individuals with whom they shared personal information. Sexual ties were determined by asking respondents to nominate up to five individuals with whom they had anal, oral, or vaginal sex within the past 6 months.
Control variables
Respondents’ age was assessed by date of birth, and the respondents provided information on network members’ ages. Race and ethnicity were evaluated by: 1) answering whether or not they were “Hispanic,” and 2) selecting among “Black/African American,” “White/Caucasian,” “American Indian or Alaskan Native,” “Asian or Pacific Islander,” or “Other.”
Data analysis
Respondents’ demographics
A Chi-square test was used to assess the relationship between the baseline characteristics (age, gender, race/ethnicity, sexual orientation, and HIV status) of the respondents and those of their social network members.
Regression analysis
The unit of analysis for this study was the dyad (the pair of the respondent and each of his network members/partners). Homophily by age was evaluated using the value of age difference between a respondent and his network member. Race/ethnicity was assessed using a dichotomous scale (1=same race/ethnicity, 0=discordant race/ethnicity). Moreover, dyadic overlap was assessed using a dichotomous scale (1= social and sexual network overlap, 0=no overlap.)
These respondent-partner dyadic data were treated as correlated binary data clustered on the respondent. To account for clustering, a generalized estimating equation (Zeger & Liang, 1986) with a logit link function and an exchangeable correlation structure were specified to estimate the odds of knowing the sexual partner’s HIV status as a function of the factors/covariates in the model. We specified the following three models to examine the factors of knowledge of partner’s HIV status: Model A: Knowing partner’s HIV status is positive vs. other; Model B: Knowing partner’s HIV status is negative vs. other; and Model C: Not knowing partner’s HIV status vs. other.
Our regression analysis generated parameter estimates both with and without RDS-adjustment. For the RDS-adjustment, we computed Voltz-Heckahorn estimator (RDS-II) that approximates the inclusion probability as being inversely proportional to the personal network size (Volz, 2008) . We reported RDS-unadjusted results as little is known about the statistical properties of RDS-adjustment in the multilevel analysis (Volz, 2008). We also provided RDS-adjusted results as online supplemental material.
All statistical analyses were conducted using STATA version 14 (StataCorp LP, College Station, TX).
Results
Respondents’ demographics
Table 1 shows descriptive statistics concerning respondents’ demographic information.
Table 1:
Demographics of the respondents
| Chicago (n=372) |
Houston (n=374) |
p | |
|---|---|---|---|
| Age(mean, (SD)) | 24.3 (2.9) | 24.9 (2.9) | 0.046 |
| Race (%) | |||
| Hispanic | 10.5 | 18.7 | 0.009 |
| Non-Hispanic White/Caucasian | 20.2 | 15.2 | |
| Non-Hispanic Black/African American | 63.7 | 59.9 | |
| Other | 5.7 | 6.2 | |
| Sexual Orientation (%) | |||
| Gay | 65.6 | 82.9 | <0.001 |
| Heterosexual | 0.8 | 1.6 | |
| Bisexual | 28.2 | 13.1 | |
| Other | 5.4 | 2.4 | |
| Education (%) | |||
| Grade K-High school or GED | 38.4 | 37.2 | 0.434 |
| Some college or higher | 61.3 | 62.8 | |
| Unknown | 0.3 | 0 | |
| HIV prevalence (%) | 25.0 | 30.8 | 0.080 |
| History of housing instability (%) | 30.4 | 17.7 | <0.001 |
| Condom use (%) | |||
| Consistent | 29.0 | 27.8 | 0.152 |
| Inconsistent | 66.4 | 64.2 | |
| Unknown | 4.6 | 8.0 | |
| Number of sex partners (mean, (SD)) | 6.9 (13.1) | 6.0 (12.7) | 0.322 |
A total of 755 respondents took part in this study (N=377 for Chicago and N=378 for Houston). Our samples were restricted to 746 respondents (N=372 for Chicago and N=374 for Houston) by excluding nine respondents without partner information.
The mean age was higher in Houston (24.3 years-old [Chicago], 24.9 years-old [Houston], p<0.05). As for race, there was a significant difference between the two cities. The rate of Hispanic respondents was significantly higher in Houston (10.5% [Chicago], 18.7% [Houston], p<0.05), and the rate of bisexual respondents was higher in Chicago (28.2% [Chicago], 13.1% [Houston], p<0.001). Additionally, the rate of gay-identified respondents was higher in Houston (65.6% [Chicago], 82.9% [Houston], p<0.001). As for HIV prevalence, 25.0% and 30.8% of the respondents in Chicago and Houston were HIV positive, respectively (p=0.08). A history of housing instability was more frequent among respondents in Chicago (30.4% [Chicago], 17.7% [Houston], p<0.001)
Partners’ demographics
Table 2 reports descriptive statistics concerning partners’ demographic information.
Table 2:
Demographics of the partners
| Chicago (n=1089) |
Houston (n=946) |
p | |
|---|---|---|---|
| Age (mean, (SD)) | 27.0(6.7) | 27.2(6.3) | 0.577 |
| Gender (%) | |||
| Male | 81.6 | 59.1 | <0.001 |
| Female | 6.3 | 0.8 | |
| Transgender | 2.6 | 0.5 | |
| unknown | 9.3 | 39.4 | |
| Race (%) | |||
| Hispanic | 9.2 | 9.3 | 0.183 |
| Non-Hispanic White/Caucasian | 14.6 | 11.1 | |
| Non-Hispanic Black/African American | 25.7 | 22.8 | |
| Other | 4.0 | 3.2 | |
| Education (%) | |||
| Grade K-High school or GED | 30.6 | 30.6 | 0.920 |
| Some college or higher | 51.2 | 51.9 | |
| Unknown | 18.2 | 17.6 | |
| Relationship type (%) | |||
| Sex | 88.2 | 70.0 | <0.001 |
| Sex and Social | 11.9 | 30.0 | |
| HIV prevalence (%) | 11.9 | 12.4 | 0.720 |
Initially, 4,407 social and sexual network contacts were identified. However, respondents were not asked about the HIV status of all individuals included in their social network. Therefore, social network members were excluded from this analysis. Ultimately, 2,035 sexual partners were analyzed. The majority of partners were male (81.6% [Chicago], and 59.1% [Houston]). However, in Houston, respondents either did not know or refused to provide gender information for 39.4% of the partners. There was a significant difference between the two cities in terms of relationship type. In Chicago and Houston, 11.9% and 30.0% of partners, respectively, had socially and sexually overlapping relationships with respondents.
Relationship categories between respondents and partners
Respondents were asked about their relationships with each partner, as shown in Table 3.
Table 3:
Relationship categories between the respondents and their partners
| Relationship | Sexual network (%) (N=1622) |
|---|---|
| Non-romantic sex partner | 23.0 (n=373) |
| Friend | 20.7 (n=335) |
| Acquaintance | 18.1 (n=293) |
| Relationship | Overlapped network (%) (N=413) |
| Close friend | 24.5 (n=101) |
| Friend | 19.1 (n=79) |
| Roommate/housemate | 13.3 (n=55) |
The three most common categories of sexual network partnership were non-romantic sex partner (23.0%), friend (20.7%), and acquaintance (18.1%). The top three categories for overlapping network partners were close friend (24.5%), friend (19.1%), and roommate/housemate (13.3%). The mean number of years since the respondents met their partner(s) was 2.6 (SD=2.3, range 0.5-21.8).
Factors predicting HIV perception
Results of the generalized estimating equation analyses are reported in Table 4.
Table 4:
Regression analysis for demographics on HIV status perception
| Model A: Partner's HIV positive vs. others dyad=1983, YMSM=686 |
Model B: Partner's HIV negative vs. others dyad=1983, YMSM=686 |
Model C: Partner's HIV unknown vs. others dyad=1983, YMSM=686 |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | Std. Err. | p-value | 95%CI | OR | Std. Err. | p-value | 95%CI | OR | Std. Err. | p-value | 95%CI | ||||
| Respondent's (Rt's) age | 1.05 | 0.03 | 0.14 | 0.99 | 1.11 | 0.95 | 0.02 | 0.04 | 0.91 | 1.00 | 1.03 | 0.03 | 0.33 | 0.97 | 1.09 |
| Rt's race White (W) | |||||||||||||||
| vs. Hispanic (H) | 0.78 | 0.28 | 0.49 | 0.39 | 1.58 | 1.10 | 0.29 | 0.73 | 0.66 | 1.84 | 1.07 | 0.35 | 0.83 | 0.57 | 2.02 |
| vs. Black (B) | 1.00 | 0.33 | 1.00 | 0.53 | 1.90 | 0.69 | 0.17 | 0.14 | 0.42 | 1.13 | 1.70 | 0.53 | 0.09 | 0.92 | 3.14 |
| vs. Other (O) | 1.15 | 0.51 | 0.75 | 0.48 | 2.76 | 0.76 | 0.26 | 0.43 | 0.39 | 1.50 | 1.04 | 0.48 | 0.93 | 0.42 | 2.57 |
| Rt's higher education | 0.86 | 0.16 | 0.41 | 0.61 | 1.23 | 0.92 | 0.14 | 0.60 | 0.69 | 1.24 | 1.33 | 0.25 | 0.14 | 0.91 | 1.93 |
| History of housing instability | 1.34 | 0.26 | 0.13 | 0.92 | 1.95 | 0.56 | 0.09 | <0.01 | 0.41 | 0.77 | 1.84 | 0.36 | <0.01 | 1.25 | 2.71 |
| Rt's sexuality Gay | |||||||||||||||
| vs. heterosexual | 0.17 | 0.20 | 0.14 | 0.02 | 1.74 | 2.05 | 1.49 | 0.33 | 0.49 | 8.53 | 1.09 | 0.86 | 0.91 | 0.23 | 5.13 |
| vs. bisexual | 0.36 | 0.10 | <0.01 | 0.22 | 0.61 | 1.36 | 0.25 | 0.09 | 0.95 | 1.95 | 1.36 | 0.29 | 0.16 | 0.89 | 2.07 |
| vs. other | 1.37 | 0.54 | 0.43 | 0.63 | 2.96 | 0.92 | 0.33 | 0.81 | 0.46 | 1.84 | 0.98 | 0.47 | 0.96 | 0.38 | 2.51 |
| Rt's HIV positive | 3.21 | 0.58 | <0.01 | 2.25 | 4.59 | 0.36 | 0.06 | <0.01 | 0.27 | 0.49 | 1.57 | 0.30 | 0.02 | 1.07 | 2.29 |
| City vs. Houston | 0.73 | 0.13 | 0.08 | 0.51 | 1.03 | 0.53 | 0.08 | <0.01 | 0.40 | 0.71 | 2.96 | 0.54 | <0.01 | 2.07 | 4.23 |
| Inconsistent condom use | 1.65 | 0.33 | 0.01 | 1.11 | 2.45 | 0.67 | 0.11 | 0.01 | 0.49 | 0.92 | 1.28 | 0.25 | 0.22 | 0.86 | 1.88 |
| # of sex partners | 1.00 | 0.01 | 0.83 | 0.99 | 1.01 | 1.00 | 0.01 | 0.99 | 0.99 | 1.01 | 1.00 | 0.01 | 0.64 | 0.99 | 1.01 |
| Partner's race White (W) | |||||||||||||||
| vs. Hispanic (H) | 2.65 | 0.75 | <0.01 | 1.52 | 4.63 | 0.81 | 0.15 | 0.25 | 0.57 | 1.16 | 0.69 | 0.15 | 0.09 | 0.45 | 1.06 |
| vs. Black (B) | 3.10 | 1.19 | <0.01 | 1.46 | 6.59 | 0.50 | 0.13 | 0.01 | 0.30 | 0.85 | 1.23 | 0.40 | 0.52 | 0.65 | 2.34 |
| vs. Other (O) | 1.76 | 0.67 | 0.14 | 0.83 | 3.71 | 0.92 | 0.22 | 0.75 | 0.57 | 1.49 | 0.85 | 0.24 | 0.57 | 0.48 | 1.49 |
| Age difference | 0.99 | 0.01 | 0.22 | 0.96 | 1.01 | 1.01 | 0.01 | 0.08 | 1.00 | 1.03 | 0.98 | 0.01 | 0.10 | 0.97 | 1.00 |
| Race match B-B | |||||||||||||||
| vs. O-O | 1.00 | 0.41 | 0.99 | 0.44 | 2.23 | 0.74 | 0.22 | 0.32 | 0.41 | 1.34 | 1.51 | 0.56 | 0.26 | 0.73 | 3.13 |
| Dubplicate Network | 2.11 | 0.36 | <0.01 | 1.51 | 2.95 | 1.43 | 0.20 | 0.01 | 1.09 | 1.88 | 0.26 | 0.05 | <0.01 | 0.18 | 0.40 |
HIV knowledge was significantly associated with the respondent’s HIV status and overlapped network status between the respondent and his partners in all three models.
In Model A (knowing that the partner’s HIV status was positive vs. other), bisexual respondents were less likely to know that their partner was HIV positive (AOR=0.36; p<0.01; 95% CI: 0.22-0.61), and HIV positive respondents were more likely to know that their partner was HIV positive (AOR=3.21; p<0.01; 95% CI: 2.25-4.59). Respondents who inconsistently used condoms were more likely to know that their partner was HIV positive (AOR=1.65; p<0.05; 95% CI: 1.11-2.45). Compared with white partners, respondents were more likely to know Hispanic and African American partners’ HIV status as being positive (AOR=2.65; p<0.01; 95% CI: 1.52-4.63 [Hispanic], AOR=3.10; p<0.01; 95% CI: 1.46-6.59 [Black]). Respondents connected both socially and sexually with their partners (i.e., overlapped relationships) were more likely to know that their partner was positive (AOR=2.11; p<0.01; 95% CI: 1.51-2.95).
In Model B (knowing that the partner’s HIV status was negative vs. other), older respondents were less likely to know that their partner’s HIV status was negative (AOR=0.95; p<0.05; 95% CI: 0.91-0.998). Respondents with a history of housing instability were less likely to know that their partner’s HIV status was negative (AOR=0.56; p<0.02; 95% CI: 0.41-0.77), as were HIV positive respondents (AOR=0.36; p<0.01; 95% CI: 0.27-0.49), respondents living in Houston (AOR=0.53; p<0.01; 95% CI: 0.40-0.71), and respondents who inconsistently used condom (AOR=0.67; p<0.05; 95% CI: 0.49-0.92). Compared to White partners, respondents were less likely to know that their African American partners’ HIV status was negative (AOR=0.50; p=0.01; 95% CI: 0.30-0.85).
In Model C (not knowing the partner’s HIV status vs. other), respondents with a history of housing instability (AOR=1.84; p<0.01; 95% CI: 1.25-2.71) and those living in Houston (AOR=2.96; p<0.01; 95% CI: 2.07-4.23), as well as HIV positive respondents (AOR=1.57; p<0.05; 95% CI: 1.07-2.29), were more likely to not know their partner’s HIV status. However, respondents with a partner connected both socially and sexually were less likely to not know their partner’s HIV status (AOR=0.26; p<0.01; 95% CI: 0.18-0.40).
In all three models, the age difference and racial/ethnic match between respondents and their partners were not statistically significant factors.
These results indicate the need for additional supplemental analyses to examine whether including the relationship length between respondents and partners would be a significant predictor. We conducted the additional analyses (reported in the supplemental materials), and our results indicated that the relationship length was excluded from the subset of covariates.
Discussion
This study examined the social networks of YMSM in Chicago and Houston in relation to the knowledge of their partner’s HIV status, and found that overlapping sexual and social relationships increased the likelihood of knowing a partners’ HIV status. Although we predicted that age differences and racial/ethnic matches between respondents and partners would have a significant association with knowing a partner’s HIV statuses, our data did not support this hypothesis.
Our results are consistent with previous studies. For example, among Peruvian MSM and transgender women, longer and more stable relationships were positively associated with knowledge of a partner’s serostatus (Nagaraj et al., 2013). In other words, shorter and less stable relationships, such as a casual partnership, are predictive of a diminished likelihood of knowing a partner’s HIV serostatus. Therefore, future prevention research could focus on interventions that promote disclosing accurate HIV serostatuses within even casual relationships too, in order to help facilitate safer sexual practices (Serovich, Reed, Grafsky, & Andrist, 2009). Additionally, it is important to intervene among social partners, as the enabling effects of social network members may encourage risky behaviors (Schneider et al., 2013).
Since a socially and sexually overlapping network increases the degree of contact between respondents and partners, it is reasonable that this overlapping network enhances the likelihood of knowing the partners’ HIV status. However, as we mentioned in the results and supplemental materials, the factor of net status was not associated with relationship duration. This does not necessarily imply a short time relationship with a sex partner. Thus, we concluded that relationship type does not predict the relationship duration.
This study also demonstrated that respondents with a history of housing instability were less likely to know their partners’ serostatus. This could be related to data suggesting that homeless people experience higher levels of HIV-related stigma (Wolitski, Pals, Kidder, Courtenay-Quirk, & Holtgrave, 2009). Thus, respondents with a history of housing instability may not have disclosed their own status; therefore, they were less likely to know their partners’ HIV status.
The association between knowledge of partner’s HIV status and the relationship between respondents and their partners was confirmed in this study. Several previous studies reported knowledge of HIV status among social or sexual network members. A study indicated that a high level of trust with sex partners was a risk factor for incorrect knowledge of the sex partner’s HIV status (Fujimoto, Williams, & Ross, 2015). Even young Latino and Black men, who state that they know their partner’s HIV status, are frequently misinformed or tend to misunderstand their partner’s serostatus (Marks et al., 2009). Moreover, it has been reported that individuals rely on the nature of their relationship with a sexual partner when assessing STI/HIV status (Masaro, Dahinten, Johnson, Ogilvie, & Patrick, 2008). The extent to which these misperceptions occur and influence behavior likely differ when a partner is presumed to be uninfected rather than infected. Therefore, future interventions regarding HIV serostatus disclosure require full disclosure of one’s HIV status to help partners understand his/her correct status.
Our study has some limitations. First, the respondents were not asked about the HIV status of their social network partners, and the questions only focused on their sex partners. Therefore, it was difficult to elucidate how much the social or sexual network could impact the knowledge of HIV status of partners. Second, this study did not assess how partners’ HIV status was identified. Hence, it is possible that this knowledge might not be related to the partners themselves only, but also to other network members. If the questionnaires had asked respondents about their source of information, it could have been possible to recommend interventions to promote serostatus disclosure depending on the source. For example, if the majority of notifications of HIV status were indirect, it could be effective to encourage individuals newly infected with HIV to disclose their serostatus through health care providers, social workers, or counselors. Third, gender and HIV serostatus homophily were not assessed in this study, as partners were mostly male, and partners’ HIV serostatus was not objectively assessed. Finally, although YMAP is longitudinal network study, this study used cross-sectional data. Thus, it is possible to identify the association between each factor and knowledge of partners’ HIV status. However, it is impossible to establish causality between these factors, as the temporal order of cause and effect were not assessed (Porta, 2008).
Disclosing HIV status to more social network members is associated with retention in HIV care (Wohl et al., 2011). Therefore, our findings are useful when individuals with HIV choose potential network members to offer health-related support.
Supplementary Material
Acknowledgement
This work was supported by the National Institutes of Health (1R01MH100021, 1R01DA039934), and UT Health Innovation for Cancer Prevention Research Training Program (Cancer Prevention and Research Institute of Texas grant #RP160015). We acknowledge the contributions of the YMAP staff in both Houston and Chicago, to this study.
References
- Birkett M, Kuhns LM, Latkin C, Muth S, & Mustanski B (2015). The sexual networks of racially diverse young men who have sex with men. Archives of Sexual Behavior, 44(7), 1787–1797. doi: 10.1007/s10508-015-0485-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohl DD, Raymond HF, Arnold M, & McFarland W (2009). Concurrent sexual partnerships and racial disparities in HIV infection among men who have sex with men. Sexually Transmitted Infections, 85(5), 367–369. doi: 10.1136/sti.2009.036723 [DOI] [PubMed] [Google Scholar]
- Fujimoto K, Cao M, Kuhns LM, Li D, & Schneider JA (2018). Statistical adjustment of network degree in respondent-driven sampling estimators: venue attendance as a proxy for network size among young MSM. Social Networks, 54, 118–131. doi: 10.1016/j.socnet.2018.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujimoto K, Flash CA, Kuhns LM, Kim JY, & Schneider JA (2018). Social networks as drivers of syphilis and HIV infection among young men who have sex with men. Sexually Transmitted Infections, 94(5), 365–371. doi: 10.1136/sextrans-2017-053288 [DOI] [PubMed] [Google Scholar]
- Fujimoto K, Williams ML, & Ross MW (2015). A network analysis of relationship dynamics in sexual dyads as correlates of HIV risk misperceptions among high-risk MSM. Sexually Transmitted Infections, 91(2), 130–134. doi: 10.1136/sextrans-2014-051742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckathorn DD (2011). Snowball Versus Respondent-Driven Sampling. Sociological Methodology, 41(1), 355–366. doi: 10.1111/j.1467-9531.2011.01244.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krohn MD (1986). The web of conformity: a network approach to the explanation of delinquent behavior. Social Problems, 33(6), S81–S93. doi: 10.2307/800675 [DOI] [Google Scholar]
- Krohn MD, Massey JL, & Zielinski M (1988). Role overlap, network multiplexity, and adolescent deviant behavior. Social Psychology Quarterly, 51(4), 346–356. doi: 10.2307/2786761 [DOI] [Google Scholar]
- Latkin C, Yang C, Tobin K, Roebuck G, Spikes P, & Patterson J (2012). Social network predictors of disclosure of MSM behavior and HIV-positive serostatus among African American MSM in Baltimore, Maryland. AIDS and behavior, 16(3), 535–542. doi: 10.1007/s10461-011-0014-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Yamazaki M, Harris DR, Harper GW, & Ellen J (2015). Social Support and Human Immunodeficiency Virus-Status Disclosure to Friends and Family: Implications for Human Immunodeficiency Virus-Positive Youth. Journal of Adolescent Health, 57(1), 73–80. doi: 10.1016/j.jadohealth.2015.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks G, Millett GA, Bingham T, Bond L, Lauby J, Liau A, … Stueve A (2009). Understanding differences in HIV sexual transmission among Latino and black men who have sex with men: The Brothers y Hermanos Study. AIDS and behavior, 13(4), 682–690. doi: 10.1007/s10461-008-9380-6 [DOI] [PubMed] [Google Scholar]
- Masaro CL, Dahinten VS, Johnson J, Ogilvie G, & Patrick DM (2008). Perceptions of sexual partner safety. Sexually Transmitted Diseases, 35(6), 566–571. doi: 10.1097/OLQ.0b013e3181660c43 [DOI] [PubMed] [Google Scholar]
- McPherson M, Smith-Lovin L, & Cook JM (2001). Birds of a Feather: Homophily in Social Networks. Annual Review of Sociology, 27, 415–444. doi: 10.1146/annurev.soc.27.1.415 [DOI] [Google Scholar]
- Nagaraj S, Segura ER, Peinado J, Konda KA, Segura P, Casapia M, … Lama JR (2013). A cross-sectional study of knowledge of sex partner serostatus among high-risk Peruvian men who have sex with men and transgender women: implications for HIV prevention. BMC Public Health, 13, 181. doi: 10.1186/1471-2458-13-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porta M (2008). A Dictionary of Epidemiology (5th ed.). New York, NY: Oxford University Press. [Google Scholar]
- Schneider JA, Cornwell B, Ostrow D, Michaels S, Schumm P, Laumann EO, & Friedman S (2013). Network mixing and network influences most linked to HIV infection and risk behavior in the HIV epidemic among black men who have sex with men. American Journal of Public Health, 103(1), e28–36. doi: 10.2105/AJPH.2012.301003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serovich JM, Reed S, Grafsky EL, & Andrist D (2009). An intervention to assist men who have sex with men disclose their serostatus to casual sex partners: results from a pilot study. AIDS Educ Prev, 21(3), 207–219. doi: 10.1521/aeap.2009.21.3.207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente TW (2015). Social Network and Health Behavior In Glanz K, Rimer BK, Viswanath K (Ed.), Health Behavior Theory, Research, and Practice (pp. 207). San Francisco, CA: Jossey-Bass. [Google Scholar]
- Volz E, Heckathorn DD . (2008). Probability Based Estimation Theory for Respondent Driven Sampling. Journal of Official Statistics, 24(1), 79–97. [Google Scholar]
- Wohl AR, Galvan FH, Myers HF, Garland W, George S, Witt M, … Lee ML (2011). Do social support, stress, disclosure and stigma influence retention in HIV care for Latino and African American men who have sex with men and women? AIDS and behavior, 15(6), 1098–1110. doi: 10.1007/s10461-010-9833-6 [DOI] [PubMed] [Google Scholar]
- Zea MC, Reisen CA, Poppen PJ, Echeverry JJ, & Bianchi FT (2004). Disclosure of HIV-positive status to Latino gay men’s social networks. American Journal of Community Psychology, 33(1-2), 107–116. doi: 10.1023/B:AJCP.0000014322.33616.ae [DOI] [PubMed] [Google Scholar]
- Zeger SL, & Liang KY (1986). Longitudinal data analysis for discrete and continuous outcomes. Biometrics, 42(1), 121–130. doi: 10.2307/2531248 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


